Key Points
Question
How does the prevalence of diabetes and hypertension in India vary by geographical area and sociodemographic characteristics?
Findings
Diabetes and hypertension prevalence varied widely among states (by more than a factor of 6 for diabetes and more than a factor of 2 for hypertension); while household wealth and urban location were positively associated with both conditions, the prevalence of diabetes and hypertension among those older than 40 years in the poorest household wealth quintile in rural areas was nonetheless high (5.9% and 30.0%, respectively).
Meaning
The prevalence of diabetes and hypertension in India varies substantially by age, rural vs urban location, and state—knowledge that could be used to target relevant programs to those most in need.
Abstract
Importance
Understanding how diabetes and hypertension prevalence varies within a country as large as India is essential for targeting of prevention, screening, and treatment services. However, to our knowledge there has been no prior nationally representative study of these conditions to guide the design of effective policies.
Objective
To determine the prevalence of diabetes and hypertension in India, and its variation by state, rural vs urban location, and individual-level sociodemographic characteristics.
Design, Setting, and Participants
This was a cross-sectional, nationally representative, population-based study carried out between 2012 and 2014. A total of 1 320 555 adults 18 years or older with plasma glucose (PG) and blood pressure (BP) measurements were included in the analysis.
Exposures
State, rural vs urban location, age, sex, household wealth quintile, education, and marital status.
Main Outcomes and Measures
Diabetes (PG level ≥126 mg/dL if the participant had fasted or ≥200 mg/dL if the participant had not fasted) and hypertension (systolic BP≥140 mm Hg or diastolic BP≥90 mm Hg).
Results
Of the 1 320 555 adults, 701 408 (53.1%) were women. The crude prevalence of diabetes and hypertension was 7.5% (95% CI, 7.3%-7.7%) and 25.3% (95% CI, 25.0%-25.6%), respectively. Notably, hypertension was common even among younger age groups (eg, 18-25 years: 12.1%; 95% CI, 11.8%-12.5%). Being in the richest household wealth quintile compared with being in the poorest quintile was associated with only a modestly higher probability of diabetes (rural: 2.81 percentage points; 95% CI, 2.53-3.08 and urban: 3.47 percentage points; 95% CI, 3.03-3.91) and hypertension (rural: 4.15 percentage points; 95% CI, 3.68-4.61 and urban: 3.01 percentage points; 95% CI, 2.38-3.65). The differences in the probability of both conditions by educational category were generally small (≤2 percentage points). Among states, the crude prevalence of diabetes and hypertension varied from 3.2% (95% CI, 2.7%-3.7%) to 19.9% (95% CI, 17.6%-22.3%), and 18.0% (95% CI, 16.6%-19.5%) to 41.6% (95% CI, 37.8%-45.5%), respectively.
Conclusions and Relevance
Diabetes and hypertension prevalence is high in middle and old age across all geographical areas and sociodemographic groups in India, and hypertension prevalence among young adults is higher than previously thought. Evidence on the variations in prevalence by state, age group, and rural vs urban location is critical to effectively target diabetes and hypertension prevention, screening, and treatment programs to those most in need.
This cross-sectional, nationally representative, population-based study determines the prevalence of diabetes and hypertension in India, and its variation by state, rural vs urban location, and individual-level sociodemographic characteristics.
Introduction
In 2011, World Health Organization (WHO) member states signed the Global Action Plan for the Prevention and Control of Noncommunicable Diseases, which aimed to halt the rise of diabetes by 2025 and reduce the prevalence of hypertension by 25% between 2010 and 2025. In 2015, as part of Sustainable Development Goal 3, the United Nations (UN) member states set the target of reducing premature mortality from noncommunicable diseases (NCDs) by one-third by 2030. Given India’s huge population, its achievements are critical to reaching these global targets.
India is in the midst of a rapid epidemiological transition: the estimated proportion of disability-adjusted life-years (DALYs) attributable to NCDs in India has risen from 31% of total DALYs in 1990 to 55% in 2016. An increasing prevalence of diabetes and hypertension is thought to be both an important driver and consequence of this transition. The NCD Risk Factor Collaboration (NCD-RisC) estimates suggest that between 1980 and 2014, the age-standardized diabetes and hypertension prevalence among men in India grew from 3.7% to 9.1% and 24.5% to 26.6%, respectively, and among women from 4.6% to 8.3% and 22.7% to 24.7%, respectively. The prevalence of both conditions is likely to continue increasing in the future given that (1) India’s population is aging and urbanizing rapidly and (2) standards of living in the country are improving, which tends to be accompanied by an increase in obesity and its associated cardiovascular disease (CVD) risk factors, including diabetes and hypertension. The latter is particularly concerning given that adults of Asian Indian ethnicity are thought to be predisposed to developing CVD when exposed to obesogenic environments and lifestyles.
For effective targeting of health system resources and services, it is essential to understand how the prevalence of diabetes and hypertension varies among population groups across this vast country. Yet, to date, there has not been a nationally representative study of diabetes and hypertension in India to provide the evidence needed to inform policymaking. Pooling data from a nationally representative sample of 1.3 million adults, this study aims to provide a new (and more accurate) diabetes and hypertension prevalence estimate for India, and to examine how the prevalence of these conditions varies by state, rural vs urban location, and individual-level sociodemographic characteristics.
Methods
Data Sources
We pooled data from 2 large household surveys in India: The District-Level Household Survey-4 (DLHS-4) and the second update of the Annual Health Survey (AHS), which were both carried out between 2012 and 2014, are representative at the district level and jointly cover all 29 states of India except (1) Jammu and Kashmir and (2) Gujarat. More details on the surveys are provided in eMethods 1, eMethods 2, and eFigure 1 in the Supplement. This analysis of an existing data set in the public domain received a determination of “not human subjects research” by the institutional review board of the Harvard T. H. Chan School of Public Health.
Ascertainment of Diabetes and Hypertension
Both the AHS and DLHS-4 measured blood glucose and blood pressure (BP) in men and nonpregnant women 18 years or older. A capillary blood sample (using a finger prick) was taken and blood glucose measured using the SD CodeFree handheld glucometer (Bionsensor Inc), which multiplied capillary glucose readings by 1.11 to display their plasma equivalent. Blood pressure was measured twice in the left upper arm (with the patient sitting) using an electronic BP monitor (Rossmax AW150, Rossmax International Ltd).
Diabetes
Diabetes was defined as having a high plasma glucose reading (≥126 mg/dL [7.0 mmol/L] if patients reported having fasted or ≥200 mg/dL [11.1 mmol/L] if patients reported not fasting per the recommendations of the International Diabetes Federation and WHO). All participants were asked to fast overnight until the time of the blood glucose measurement in the morning. Fasting status was verified by self-report in the DLHS-4 (58.4% of participants reported to have fasted) but was not recorded in the AHS. The prevalence and regression results in this article assume all AHS respondents to have fasted. However, in the Supplement, we present all prevalence and regression estimates assuming AHS participants had not fasted, as well as regression results among only those respondents in whom fasting status was verified by self-report (ie, DLHS-4 participants only).
Hypertension
Based on the mean of the 2 BP measurements taken in the AHS and DLHS-4, we defined hypertension as systolic BP of at least 140 mm Hg or diastolic BP of at least 90 mm Hg.
Ascertainment of Sociodemographic Characteristics
The independent variables for this study were state, household wealth quintile, education, marital status (currently married or not), and whether the household was located in a rural or urban area. We used household ownership of 12 assets (radio, TV, computer, phone, refrigerator, bike, scooter, car, washing machine, sewing machine, house, and land) and 5 key housing characteristics (water supply, type of toilet and whether it is shared, cooking fuel, housing material, and source of lighting) to generate a household wealth index in a principal component analysis (PCA). Following the methodology developed by Filmer and Pritchett, we extracted the first component in the PCA separately for urban and rural areas and divided this variable into quintiles (again, separately for rural and urban areas) based on the distribution in the national data set. More details on the computation of the household wealth index are provided in eMethods 3 in the Supplement.
Statistical Analysis
Diabetes and hypertension prevalence was calculated by state, rural vs urban location, sex, age group, and household wealth quintile using sampling weights to account for both the survey design and the pooling of AHS with DLHS-4 data (see eMethods 4 in the Supplement). Age-standardized prevalence estimates were weighted to the age distribution of the WHO’s standard population. We fitted multivariable linear probability models (LPMs)—run separately for rural and urban areas—to further investigate the association of diabetes and hypertension with individual-level sociodemographic characteristics. Our regressions included a binary indicator (“fixed effect”) for each of 18 126 primary sampling units (PSUs) to filter out area-level effects on diabetes and hypertension. Because there are relatively few observations in each PSU, we fitted LPMs rather than logistic or probit models to avoid the incidental parameter problem. An added advantage of the LPM is the interpretability of the regression coefficients as simple absolute differences in the probability of the outcome. To avoid the possibility of fitted probabilities greater than 1 and less than 0, we use logistic regression (with district-level fixed effects to sidestep the incidental parameter problem) for predicted probability plots. The standard errors in all regression models were adjusted for clustering at the PSU level. Statistical analyses were performed with R software (version 3.3.2; R Foundation), and all figures were created with the ggplot2 package.
Results
Sample Characteristics
A total of 1 618 359 nonpregnant adults were interviewed; 297 804 (18.4%) had a missing value for the plasma glucose measurement or at least 1 of the 2 BP readings, yielding a sample size for analysis of 1 320 555 adults. Table 1 shows the (unweighted) characteristics of the participants; 7.6% of participants had diabetes, 26.5% had hypertension, 43.4% of participants were ages 18 to 35 years, and 47.0% of women and 28.6% of men had not completed primary school. Three quarters of participants were married, and a third (32.5%) were living in urban areas.
Table 1. Sample Characteristicsa.
| Characteristic | Total | Female | Male |
|---|---|---|---|
| No. | 1 320 555 | 701 408 (53.1) | 619 147 (46.9) |
| Diabetes, No. (%) | 100 242 (7.6) | 52 019 (7.4) | 48 223 (7.8) |
| Hypertension, No. (%) | 350 273 (26.5) | 170 145 (24.3) | 180 128 (29.1) |
| Age group, No. (%), y | |||
| 18-25 | 253154 (19.2) | 131 388 (18.7) | 121 766 (19.7) |
| 26-35 | 320 018 (24.2) | 178 779 (25.5) | 141 239 (22.8) |
| 36-45 | 281 706 (21.3) | 153 249 (21.8) | 128 457 (20.7) |
| 46-55 | 212 465 (16.1) | 114 018 (16.3) | 98 447 (15.9) |
| 56-65 | 150 940 (11.4) | 75 911 (10.8) | 75 029 (12.1) |
| >65 | 102 253 (7.7) | 48 056 (6.9) | 54 197 (8.8) |
| Education, No. (%) | |||
| <Primary school | 504 829 (38.4) | 328 296 (47.0) | 176 533 (28.6) |
| Primary school | 163 953 (12.5) | 83 338 (11.9) | 80 615 (13.1) |
| Middle school | 203 128 (15.4) | 96 659 (13.8) | 106 469 (17.3) |
| Secondary school | 182 391 (13.9) | 81 380 (11.6) | 101 011 (16.4) |
| High schoolb | 128 270 (9.8) | 55 876 (8.0) | 72 394 (11.7) |
| >High schoolb | 132 544 (10.1) | 53 329 (7.6) | 79 215 (12.9) |
| Household wealth quintile, No. (%) | |||
| 1 (Poorest) | 254 652 (20.2) | 135 454 (20.2) | 119 198 (20.2) |
| 2 | 248 101 (19.7) | 130 896 (19.5) | 117 205 (19.8) |
| 3 | 245 748 (19.5) | 130 413 (19.4) | 115 335 (19.5) |
| 4 | 253 905 (20.1) | 134 977 (20.1) | 118 928 (20.1) |
| 5 (Richest) | 259 491 (20.6) | 139 077 (20.7) | 120 414 (20.4) |
| Currently married, No. (%) | 988 456 (75.0) | 532 786 (76.0) | 455 670 (73.7) |
| Urban area, No. (%) | 429 330 (32.5) | 228 954 (32.6) | 200 376 (32.4) |
These data were not weighted using sampling weights. Data are given as (number (percentage). These sample characteristics are for all participants who had nonmissing blood glucose level and blood pressure measurement. Sample characteristics stratified by whether the blood glucose or blood pressure measurement was missing are shown in eTable 1 in the Supplement. The percentage missing for all sociodemographic variables (ie, age, education, household wealth, marital status, and urban vs rural location) was less than 0.5% except for household wealth quintile (4.4% of observations were missing).
Generally referred to as “higher secondary school” in the Indian school system.
National Prevalence of Diabetes and Hypertension
The crude (weighted) prevalence of diabetes was 7.3% (95% CI, 7.1%-7.4%) and 7.8% (95% CI, 7.6%-8.0%) among women and men, respectively, and ranged from 2.4% (95% CI, 2.2%-2.5%) among men ages 18 to 25 years to 14.0% (95% CI, 13.5%-14.5%) among men older than 65 years (eTable 2 in the Supplement). Crude hypertension prevalence was 23.6% (95% CI, 23.3%-23.8%) among women and 27.4% (95% CI, 27.0%-27.7%) among men, ranging from 9.2% (95% CI, 8.9%-9.6%) among women ages 18 to 25 years to 48.6% (95% CI, 47.9%-49.3%) among women older than 65 years.
Prevalence by Individuals’ Sociodemographic Characteristics
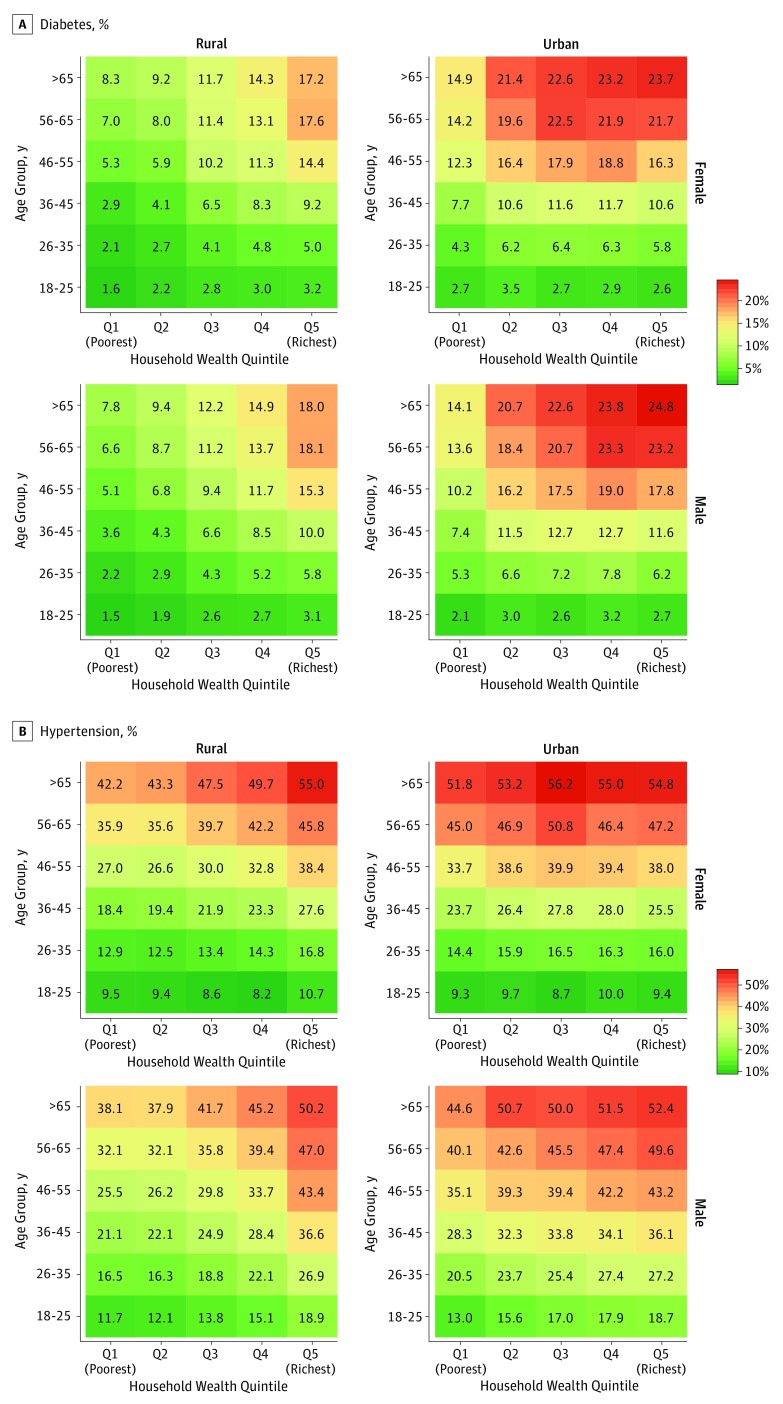
Stratification of crude prevalence by individuals’ sociodemographic characteristics (Figure 1 and eFigure 4 in the Supplement) and multivariable regressions (Table 2 and Figure 2) show that (1) household wealth quintile was positively associated with both conditions, although—compared with the poorest quintile—the richest quintile had only a modestly higher probability of diabetes (rural areas: 2.81 percentage points; 95% CI, 2.53-3.08 and urban areas: 3.47 percentage points; 95% CI, 3.03-3.91) and hypertension (rural areas: 4.15 percentage points; 95% CI, 3.68-4.61 and urban areas: 3.01 percentage points; 95% CI, 2.38-3.65); (2) the differences in the probability of both conditions by educational attainment were generally small (≤2.00 percentage points); (3) for both conditions, prevalence tended to be higher in urban than rural areas; (4) the relative differences in prevalence by urban vs rural location and household wealth quintile were markedly higher for diabetes than for hypertension; (5) the relative differences between household wealth quintiles in the probability of both conditions were higher in rural areas than in urban areas; (6) while for both diabetes and hypertension men had a greater probability of having the condition than women, the absolute difference in the probability by sex was substantially larger for hypertension; and (7) the differences in the probability of both conditions with age group were higher than for any other sociodemographic characteristic.
Figure 1. Prevalence of Diabetes and Hypertension by Rural-Urban Location, Sex, and Household Wealth Quintilea.
A, Diabetes prevalence. B, Hypertension prevalence.
aDiabetes prevalence under the assumption that all Annual Health Survey participants had not fasted are shown in eFigure 3 in the Supplement.
Table 2. Multivariable Linear Regressions of Diabetes and Hypertension on Sociodemographic Characteristics and PSU-Level Fixed Effectsa.
| Characteristic | Diabetes | Hypertension | ||||||
|---|---|---|---|---|---|---|---|---|
| Rural | Urban | Rural | Urban | |||||
| Difference in Probabilityb (95% CI) | P Value | Difference in Probabilityb (95% CI) | P Value | Difference in Probabilityb (95% CI) | P Value | Difference in Probabilityb (95% CI) | P Value | |
| Age group, y | ||||||||
| 18-25 | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | ||||
| 26-35 | 1.42 (1.28 to 1.57) | <.001 | 2.57 (2.33 to 2.81) | <.001 | 6.68 (6.39 to 6.96) | <.001 | 8.12 (7.71 to 8.52) | <.001 |
| 36-45 | 3.76 (3.57 to 3.95) | <.001 | 7.04 (6.71 to 7.36) | <.001 | 14.33 (13.98 to 14.68) | <.001 | 17.84 (17.34 to 18.34) | <.001 |
| 46-55 | 6.60 (6.36 to 6.83) | <.001 | 12.11 (11.70 to 12.52) | <.001 | 21.84 (21.41 to 22.27) | <.001 | 27.49 (26.89 to 28.08) | <.001 |
| 56-65 | 8.82 (8.53 to 9.10) | <.001 | 15.86 (15.36 to 16.36) | <.001 | 28.76 (28.26 to 29.26) | <.001 | 34.52 (33.84 to 35.19) | <.001 |
| >65 | 9.96 (9.63 to 10.29) | <.001 | 17.09 (16.51 to 17.67) | <.001 | 34.77 (34.19 to 35.35) | <.001 | 39.78 (39.00 to 40.56) | <.001 |
| Wealth quintile | ||||||||
| 1 (Poorest) | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | ||||
| 2 | 0.27 (0.11 to 0.44) | <.001 | 1.04 (0.72 to 1.36) | <.001 | 0.14 (−0.18 to 0.46) | .40 | 1.35 (0.87 to 1.83) | <.001 |
| 3 | 0.59 (0.40 to 0.79) | <.001 | 2.10 (1.73 to 2.46) | <.001 | 0.84 (0.47 to 1.20) | <.001 | 2.43 (1.90 to 2.96) | <.001 |
| 4 | 1.12 (0.90 to 1.34) | <.001 | 2.92 (2.53 to 3.32) | <.001 | 1.95 (1.55 to 2.35) | <.001 | 2.77 (2.21 to 3.34) | <.001 |
| 5 (Richest) | 2.81 (2.53 to 3.08) | <.001 | 3.47 (3.03 to 3.91) | <.001 | 4.15 (3.68 to 4.61) | <.001 | 3.01 (2.38 to 3.65) | <.001 |
| Education | ||||||||
| <Primary school | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | ||||
| Primary school | 0.63 (0.46 to 0.81) | <.001 | 0.77 (0.39 to 1.14) | .52 | 0.57 (0.27 to 0.88) | <.001 | −0.04 (−0.57 to 0.48) | .87 |
| Middle school | 0.51 (0.35 to 0.68) | <.001 | 0.66 (0.31 to 1.00) | .86 | 0.36 (0.06 to 0.67) | .02 | −0.30 (−0.81 to 0.20) | .24 |
| Secondary school | 0.57 (0.37 to 0.77) | <.001 | 0.57 (0.22 to 0.91) | .001 | 0.47 (0.13 to 0.80) | .007 | −0.29 (−0.79 to 0.21) | .26 |
| High schoolc | −0.24 (−0.46 to −0.01) | .04 | −0.16 (−0.53 to 0.20) | .38 | −0.26 (−0.67 to 0.14) | .20 | −1.61 (−2.16 to −1.06) | <.001 |
| >High schoolc | −0.40 (−0.68 to −0.12) | .005 | −0.90 (−1.28 to −0.52) | <.001 | 0.15 (−0.35 to 0.64) | .56 | −1.72 (−2.28 to −1.17) | <.001 |
| Currently married | −0.02 (−0.16 to 0.13) | .83 | 0.21 (−0.04 to 0.46) | .09 | −2.62 (−2.88 to −2.35) | <.001 | −2.14 (−2.51 to −1.78) | <.001 |
| Male | 0.31 (0.21 to 0.42) | <.001 | 0.56 (0.37 to 0.74) | <.001 | 3.46 (3.23 to 3.70) | <.001 | 5.99 (5.67 to 6.31) | <.001 |
Abbreviation: PSU, primary sampling unit.
These linear probability models included all sociodemographic variables listed in the table (age group, wealth quintile, education, marital status, and sex) and a binary indicator for each PSU (PSU-level fixed effects). Standard errors were adjusted for clustering at the PSU level. These regressions assumed all AHS participants to have fasted at the time of the blood glucose level measurement. Regression results assuming that all AHS participants had not fasted are shown in eTable 4 in the Supplement. eTable 5 in the Supplement shows the regression results when restricting the sample to those in whom fasting status was verified through self-report (ie, DLHS-4 participants only).
The regression coefficients (denoted as “difference in probability”) should be interpreted as the average absolute difference (in percentage points) in the probability of having diabetes/hypertension compared with the reference category.
Generally referred to as “higher secondary school” in the Indian school system.
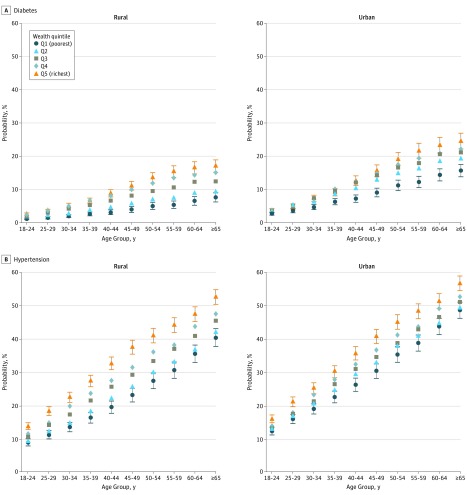
Figure 2. The Predicted Probability of Diabetes and Hypertension by Age Group, Rural or Urban Location, and Household Wealth Quintile.
A, Diabetes prevalence. B, Hypertension prevalence. Predicted probabilities were obtained from multivariable logistic regressions of diabetes and hypertension on individuals’ sociodemographic characteristics (age group, household wealth quintile, education, marital status, sex, and rural vs urban location), district-level fixed effects, and an interaction term between age group and household wealth quintile. Predicted probabilities assuming that all Annual Health Survey respondents had not fasted are shown in eFigure 6 in the Supplement.
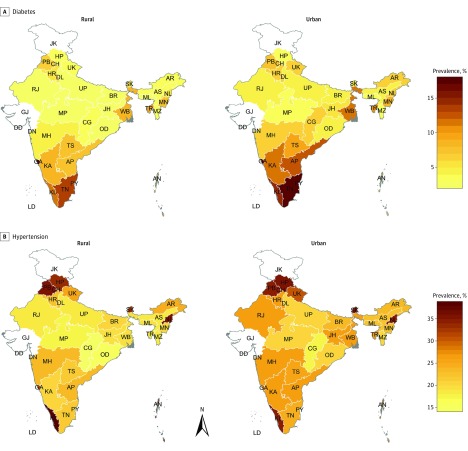
State- and District-Level Prevalence of Diabetes and Hypertension
The age-standardized prevalence of diabetes varied from 2.33% (95% CI, 1.98%-2.75%) among women in Madhya Pradesh to 17.90% (95% CI, 15.37%-20.74%) among men in Goa (eTable 6 in the Supplement). For hypertension, the age-standardized prevalence ranged from 13.50% (95% CI, 12.19%-14.93%) among women in Chhattisgarh to 43.53% (95% CI, 38.33%-48.87%) among men in Daman and Diu. While diabetes was most prevalent in the South of India (Andhra Pradesh, Goa, Karnataka, Kerala, and Tamil Nadu) as well as in Delhi and West Bengal, hypertension prevalence tended to be highest in the northern states of Punjab and Himachal Pradesh, the southern state of Kerala, and the northeastern states of Sikkim and Nagaland (Figure 3). The state- and district-level prevalence of diabetes and hypertension was positively correlated with each area’s standard of living (as measured by the state- or district-level mean household wealth quintile) (eFigure 8 and eFigure 9 in the Supplement).
Figure 3. Age-Standardized, State-Level Prevalence of Diabetes and Hypertension by Rural vs Urban Location Within Each State.
A, Diabetes prevalence. B, Hypertension prevalence. No data were available for Jammu and Kashmir, and Gujarat. The Union Territories of Chandigarh, Daman and Diu, and Puducherry are not visible in the map owing to their small area. Point estimates and 95% CIs for each state are shown in eTable 7 in the Supplement. AP indicates Andhra Pradesh; AR, Arunachal Pradesh; AS, Assam; BR, Bihar; CG, Chhattisgarh; CH, Chandigarh; DD, Daman and Diu; DL, Delhi; GA, Goa; HR, Haryana; HP, Himachal Pradesh; JH, Jharkhand; KA, Karnataka; KL, Kerala; MP, Madhya Pradesh; MH, Maharashtra; MN, Manipur; ML, Meghalaya; MZ, Mizoram; NL, Nagaland; OD, Odisha (Orissa); PB, Punjab; PY, Puducherry; RJ, Rajasthan; SK, Sikkim; TN, Tamil Nadu; TS, Telangana State; TR, Tripura; UP, Uttar Pradesh; UK, Uttarakhand (Uttaranchal); WB, West Bengal.
Discussion
To our knowledge, our study is the first to analyze nationally representative, individual-level blood glucose level and BP data in India—a country that is home to more than a sixth of the world’s population and 22% of the population in low- and middle-income countries—to provide empirical evidence on the prevalence of diabetes and hypertension and its variation among different geographical areas and sociodemographic groups. The age-standardized prevalence of diabetes was 6.1% (95% CI, 6.0%-6.3%) among women and 6.5% (95% CI, 6.4%-6.7%) among men. For comparison, NCD-RisC estimates that the age-standardized prevalence of diabetes in the United States was 6.4% among women and 8.1% among men. For hypertension, the age-standardized prevalence was considerably higher in India than estimates for the United States (20.0% among women in India compared with 10.8% in the United States, and 24.5% among men in India compared with 15.5% in the United States). While we found substantial variation in diabetes and hypertension prevalence among Indian states, we show that diabetes and hypertension are common in middle and older age across all geographical settings and population groups in the country. Specifically, even though household wealth and living in an urban area were positively associated with both diabetes and hypertension, the prevalence of these conditions in middle and old age among the lowest household wealth quintile in rural areas was still high. For instance, among those older than 40 years in the poorest wealth quintile in rural areas, 5.9% (95% CI, 5.5%-6.2%) had diabetes and 30.0% (95% CI, 29.2%-30.7%) had hypertension.
While the key strength of this study is its ability to disaggregate prevalence by state- and individual-level sociodemographic characteristics, we also provide a new diabetes and hypertension prevalence estimate for India. To date, prevalence estimates for both conditions have been obtained by extrapolating findings from subnational studies to the national level. We observed an age-standardized diabetes prevalence of 6.3% (95% CI, 6.2%-6.5%). As depicted in eFigure 14, this figure is lower than the age-standardized estimates provided by the International Diabetes Federation (which has estimated an adult prevalence of 9.3% [95% CI, 7.6%-11.4%] for 2015), NCD-RisC (estimating an adult prevalence of 9.1% [95% CI, 5.2%-14.2%] for 2014), and the Global Burden of Disease Project (estimating an age-standardized prevalence among the entire population of 6.5% [uncertainty range: 6.0%-7.1%] in 2015). The lower value for prevalence in our study is partly because we defined diabetes based on blood glucose level only (because information on diabetes medications or diagnosis was not available in the AHS and DLHS-4). While our prevalence figures are lower than these previous modeled estimates, our state-level prevalence estimates are similar to those obtained using data from the largest subnational study to date.
For hypertension, our age-standardized prevalence estimate of 24.5% (95% CI, 24.2%-24.9%) among men and 20.0% (95% CI, 19.7%-20.3%) among women is within the uncertainty intervals of the modeled estimates by WHO/NCD-RisC for India for 2015 (26.5% [95% uncertainty level, 21.2%-32.4%] among men and 24.7% [95% uncertainty level, 19.9%-29.9%] among women), which used the same definition of hypertension as was used in this study. More strikingly however, as shown in eFigure 2 in the Supplement, we found substantially higher prevalence of hypertension among age groups younger than 45 years than estimated by WHO/NCD-RisC for South Asia (India contributed 76% of the population of South Asia, as defined by WHO/NCD-RisC). In fact, in younger age groups, our hypertension prevalence estimates for India were higher than those for Central and Eastern Europe—a region that WHO/NCD-RisC identified as having the highest hypertension prevalence globally. An important finding of our study, therefore, is the unexpectedly high prevalence of hypertension among young adults in India, which—if ineffectively treated—will likely result in longer lifetime exposure to this risk factor and thus higher CVD rates in the future.
Limitations
Equity concerns have been raised about investing limited resources for health in LMICs into CVD screening and treatment because CVD is generally thought to occur more frequently in wealthier strata of society than in poorer strata. In this study, we show that the wealth and education gradients in diabetes and hypertension prevalence are relatively minor, especially when compared with age gradients. A limitation of this study, however, is that if wealthier and more educated individuals were more likely to achieve control of their diabetes or hypertension through better access to treatment, then the socioeconomic gradients in diabetes and hypertension in this analysis (which defined these conditions based on blood glucose level and BP only) are flatter than they would have been had these conditions been defined as either reporting to be on treatment or having a high blood glucose level and BP. More generally, prevalence of CVD risk factors by wealth groups can only partially inform equity-focused policy decisions because of 2 main limitations. The first is that prevalence estimates do not take into account that CVD events are likely to have more detrimental effects among the poor than among the wealthy because poorer individuals have lower access to high-quality health care services and have less financial risk protection. The second limitation is that examining a single risk factor or disease at a time does not provide information on the relative contribution of the disease to the wealth group’s total disease burden. In particular, many areas of India are still facing a substantial infectious disease burden and poor maternal and child health indicators—health problems that disproportionately affect the poor.
Our study has several additional limitations. As in any population-based survey, some adults (18.4%) had a missing value for their blood glucose measurement or at least 1 of the 2 systolic or diastolic BP measurements. Of these, 87.0% had a missing consent variable (basic sociodemographic information on these participants was still collected from the household head), suggesting that missing measurements were mostly due to some adults being absent at the time of the household visit (rather than refusal to consent or data entry errors). Second, a 1-time capillary blood glucose measurement is not recommended for the diagnosis of diabetes in clinical settings. It has, however, been shown to have an acceptable sensitivity and specificity for defining diabetes in population-based research and is the recommended method for monitoring diabetes prevalence in the WHO’s STEPwise Approach to NCD Risk Factor Surveillance. Third, the study was unable to distinguish between type 1 and type 2 diabetes. The International Diabetes Federation estimates that 72 000 children with type 1 diabetes from birth to age 14 years lived in India in 2015; 0.02% of the country’s population was in this age range. Extrapolating this percentage to adults would suggest that the proportion of adults with type 1 diabetes in our sample is likely very small. Fourth, in contrast with the DLHS-4, fasting status was not verified through self-report in the AHS. Applying a fasting blood glucose threshold to participants who had not fasted in the AHS (which covers the poorer states of India) may be partially responsible for the high diabetes prevalence among poorer individuals. We addressed this limitation by also providing prevalence estimates assuming that all AHS respondents had not fasted instead of fasted (eTables 3 and 9-11 and eFigures 5 and 6, in the Supplement). In addition, we show our regression results after restricting the sample to DLHS-4 respondents (eTable 5 and eFigure 7 in the Supplement) and find that among these participants, for whom fasting status was verified through self-report, the probability of diabetes in the lowest national household wealth quintile was even higher than among AHS respondents (eFigure 7 in the Supplement).
Conclusions
While we identified important variation in diabetes and hypertension prevalence among states and by rural vs urban location, prevalence levels in India are high across all geographical settings and socioeconomic groups in middle and old age. Major investments in targeted diabetes and hypertension prevention, detection, and treatment programs are needed across the country if India is to avert catastrophic health, social, and economic consequences of these conditions and their sequelae. Given the size, growth, rapid urbanization, and aging of India’s population, as well as the high levels of impoverishing health care expenditures caused by NCDs, the country’s success in tackling its diabetes and hypertension epidemic will be crucial to achieving Sustainable Development Goals globally.
eMethods 1. Methodology of the AHS and DLHS-4
eFigure 1. States and Union Territories covered by each survey
eMethods 2. Matching Annual Health Survey biomarker data to participants’ socio-demographic data
eMethods 3. Computation of the household wealth index
eMethods 4. Computation of sampling weights
eTable 1. Sample characteristics stratified by whether the blood glucose or blood pressure measurement was missing
eTable 2. National diabetes and hypertension prevalence by age group and sex
eTable 3. National diabetes prevalence assuming all AHS respondents were unfasted
eFigure 2. Hypertension prevalence by five-year age group for India and WHO/NCD-RisC regions
eFigure 3. Prevalence of diabetes by rural vs urban residence, sex, and household wealth quintile assuming all AHS respondents were unfasted
eFigure 4. Prevalence of diabetes and hypertension by rural vs urban residence, sex, and education
eFigure 5. Prevalence of diabetes by rural vs urban residence, sex, and education assuming all AHS respondents were unfasted
eTable 4. Regression results for diabetes assuming all AHS participants were unfasted
eTable 5. Regression results for diabetes among those in whom fasting status could be ascertained (ie, DLHS-4 participants only)
eFigure 6. The predicted probability of diabetes by age group, rural-urban location, and household wealth quintile assuming AHS participants were unfasted
eFigure 7. The predicted probability of diabetes by age group, rural-urban location, and household wealth quintile among those in whom fasting status could be ascertained (ie, DLHS-4 participants only)
eTable 6. State-level age-standardized diabetes and hypertension prevalence estimates by sex
eTable 7. State-level age-standardized diabetes and hypertension prevalence estimates by rural vs urban location
eTable 8. State-level crude diabetes and hypertension prevalence estimates by age group
eTable 9. State-level age-standardized diabetes prevalence estimates by sex assuming all AHS respondents were unfasted
eTable 10. State-level age-standardized diabetes prevalence estimates by rural vs urban location assuming all AHS respondents were unfasted
eTable 11. State-level crude diabetes prevalence estimates by age group assuming all AHS respondents were unfasted
eFigure 8. Association of the state- and district-level age-standardized prevalence of diabetes with mean household wealth quintile
eFigure 9. Association of the state- and district-level age-standardized prevalence of hypertension with mean household wealth quintile
eFigure 10. Comparison of age-standardized national diabetes prevalence reported in different studies
eReferences
References
- 1.World Health Organization Global Action Plan for the Prevention and Control of Noncommunicable Diseases 2013–2020. Geneva, Switzerland: World Health Organization; 2013. [Google Scholar]
- 2.United Nations Population Division The World Population Prospects: 2015 Revision. New York, NY: United Nations; 2015. [Google Scholar]
- 3.Institute for Health Metrics and Evaluation (IHME) GBD Compare Data Visualization. 2016; https://vizhub.healthdata.org/gbd-compare/. Accessed October 25, 2017.
- 4.Zhou B, Lu Y, Hajifathalian K, et al. . Worldwide trends in diabetes since 1980: pooled analysis of 751 population-based measurement studies with over 4.4 million participants [published online April 6, 2016]. Lancet. 2016. doi: 10.1016/S0140-6736(16)00618-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.United Nations Population Division 2014 Revision of World Urbanization Prospects. New York, NY: United Nations; 2014. [Google Scholar]
- 6.The World Bank India. 2017; https://data.worldbank.org/country/india?view=chart. Accessed May 24, 2017.
- 7.Egger G, Swinburn B, Islam FM. Economic growth and obesity: an interesting relationship with world-wide implications. Econ Hum Biol. 2012;10(2):147-153. [DOI] [PubMed] [Google Scholar]
- 8.Fernando E, Razak F, Lear SA, Anand SS. Cardiovascular Disease in South Asian Migrants. Can J Cardiol. 2015;31(9):1139-1150. [DOI] [PubMed] [Google Scholar]
- 9.Anchala R, Kannuri NK, Pant H, et al. . Hypertension in India: a systematic review and meta-analysis of prevalence, awareness, and control of hypertension. J Hypertens. 2014;32(6):1170-1177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Anjana RM, Deepa M, Pradeepa R, et al. ; ICMR–INDIAB Collaborative Study Group . Prevalence of diabetes and prediabetes in 15 states of India: results from the ICMR-INDIAB population-based cross-sectional study. Lancet Diabetes Endocrinol. 2017;5(8):585-596. [DOI] [PubMed] [Google Scholar]
- 11.Sacks DB, Arnold M, Bakris GL, et al. . Guidelines and recommendations for laboratory analysis in the diagnosis and management of diabetes mellitus. Clin Chem. 2011;57(6):e1-e47. [DOI] [PubMed] [Google Scholar]
- 12.International Diabetes Federation IDF Clinical Practice Recommendations for Managing Type 2 Diabetes in Primary Care. Brussels, Belgium: International Diabetes Federation; 2017. [Google Scholar]
- 13.Weber MA, Schiffrin EL, White WB, et al. . Clinical practice guidelines for the management of hypertension in the community a statement by the American Society of Hypertension and the International Society of Hypertension. J Hypertens. 2014;32(1):3-15. [DOI] [PubMed] [Google Scholar]
- 14.Filmer D, Pritchett LH. Estimating wealth effects without expenditure data–or tears: an application to educational enrollments in states of India. Demography. 2001;38(1):115-132. [DOI] [PubMed] [Google Scholar]
- 15.Rutstein S, Johnson K DHS Comparative Reports: The DHS Wealth Index. 2004. https://dhsprogram.com/pubs/pdf/CR6/CR6.pdf. Accessed April 3, 2017.
- 16.Ahmad OB, Boschi-Pinto C, Lopez AD, Murray CJ, Lozano R, Inoue M. Age Standardization of Rates: A New WHO Standard. Geneva, Switzerland: World Health Organization. 2001;31:1-14. [Google Scholar]
- 17.Lancaster T. The incidental parameter problem since 1948. J Econom. 2000;95(2):391-413. [Google Scholar]
- 18.NCD Risk Factor Collaboration (NCD-RisC) Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 4.4 million participants. Lancet. 2016;387(10027):1513-1530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.NCD Risk Factor Collaboration (NCD-RisC) Worldwide trends in blood pressure from 1975 to 2015: a pooled analysis of 1479 population-based measurement studies with 19·1 million participants. Lancet. 2017;389(10064):37-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.International Diabetes Federation IDF Diabetes Atlas. 7th ed Brussels, Belgium: International Diabete Federation; 2015. [Google Scholar]
- 21.Institute for Health Metrics and Evaluation GBD Results Tool. 2017; http://ghdx.healthdata.org/gbd-results-tool?params=querytool-permalink/8536320807f63b50054bc1ea29010fe9. Accessed April 4, 2017.
- 22.Anjana RM, Pradeepa R, Deepa M, et al. ; ICMR–INDIAB Collaborative Study Group . Prevalence of diabetes and prediabetes (impaired fasting glucose and/or impaired glucose tolerance) in urban and rural India: phase I results of the Indian Council of Medical Research-INdia DIABetes (ICMR-INDIAB) study. Diabetologia. 2011;54(12):3022-3027. [DOI] [PubMed] [Google Scholar]
- 23.World Health Organization Raised Blood Pressure (SBP ≥ 140 OR DBP ≥ 90), Age-Standardized (%)—Estimates by Country. Geneva, Switzerland: World Health Organization; 2017. [Google Scholar]
- 24.Bukhman G, Mocumbi AO, Horton R. Reframing NCDs and injuries for the poorest billion: a Lancet Commission. Lancet. 2015;386(10000):1221-1222. [DOI] [PubMed] [Google Scholar]
- 25.Subramanian SV, Corsi DJ, Subramanyam MA, Smith GD. Jumping the gun: the problematic discourse on socioeconomic status and cardiovascular health in India. Int J Epidemiol. 2013;42(5):1410-1426. [DOI] [PubMed] [Google Scholar]
- 26.Basu S, Millett C. Social epidemiology of hypertension in middle-income countries: determinants of prevalence, diagnosis, treatment, and control in the WHO SAGE study. Hypertension. 2013;62(1):18-26. [DOI] [PubMed] [Google Scholar]
- 27.Basu S, King AC. Disability and chronic disease among older adults in India: detecting vulnerable populations through the WHO SAGE Study. Am J Epidemiol. 2013;178(11):1620-1628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gwatidzo SD, Stewart Williams J. Diabetes mellitus medication use and catastrophic healthcare expenditure among adults aged 50+ years in China and India: results from the WHO study on global AGEing and adult health (SAGE). BMC Geriatr. 2017;17(1):14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Manne-Goehler J, Atun R, Stokes A, et al. . Diabetes diagnosis and care in sub-Saharan Africa: pooled analysis of individual data from 12 countries. Lancet Diabetes Endocrinol. 2016;4(11):903-912. [DOI] [PubMed] [Google Scholar]
- 30.Brinda EM, Kowal P, Attermann J, Enemark U. Health service use, out-of-pocket payments and catastrophic health expenditure among older people in India: the WHO Study on global AGEing and adult health (SAGE). J Epidemiol Community Health. 2015;69(5):489-494. [DOI] [PubMed] [Google Scholar]
- 31.Jaspers L, Colpani V, Chaker L, et al. . The global impact of non-communicable diseases on households and impoverishment: a systematic review. Eur J Epidemiol. 2015;30(3):163-188. [DOI] [PubMed] [Google Scholar]
- 32.GBD 2015 DALYs and HALE Collaborators Global, regional, and national disability-adjusted life-years (DALYs) for 315 diseases and injuries and healthy life expectancy (HALE), 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388(10053):1603-1658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.American Diabetes Association Diagnosis and classification of diabetes mellitus. Diabetes Care. 2014;37(suppl 1):S81-S90. [DOI] [PubMed] [Google Scholar]
- 34.Priya M, Mohan Anjana R, Pradeepa R, et al. . Comparison of capillary whole blood versus venous plasma glucose estimations in screening for diabetes mellitus in epidemiological studies in developing countries. Diabetes Technol Ther. 2011;13(5):586-591. [DOI] [PubMed] [Google Scholar]
- 35.Kruijshoop M, Feskens EJ, Blaak EE, de Bruin TW. Validation of capillary glucose measurements to detect glucose intolerance or type 2 diabetes mellitus in the general population. Clin Chim Acta. 2004;341(1-2):33-40. [DOI] [PubMed] [Google Scholar]
- 36.Riley L, Guthold R, Cowan M, et al. . The World Health Organization STEPwise approach to noncommunicable disease risk-factor surveillance: methods, challenges, and opportunities. Am J Public Health. 2016;106(1):74-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods 1. Methodology of the AHS and DLHS-4
eFigure 1. States and Union Territories covered by each survey
eMethods 2. Matching Annual Health Survey biomarker data to participants’ socio-demographic data
eMethods 3. Computation of the household wealth index
eMethods 4. Computation of sampling weights
eTable 1. Sample characteristics stratified by whether the blood glucose or blood pressure measurement was missing
eTable 2. National diabetes and hypertension prevalence by age group and sex
eTable 3. National diabetes prevalence assuming all AHS respondents were unfasted
eFigure 2. Hypertension prevalence by five-year age group for India and WHO/NCD-RisC regions
eFigure 3. Prevalence of diabetes by rural vs urban residence, sex, and household wealth quintile assuming all AHS respondents were unfasted
eFigure 4. Prevalence of diabetes and hypertension by rural vs urban residence, sex, and education
eFigure 5. Prevalence of diabetes by rural vs urban residence, sex, and education assuming all AHS respondents were unfasted
eTable 4. Regression results for diabetes assuming all AHS participants were unfasted
eTable 5. Regression results for diabetes among those in whom fasting status could be ascertained (ie, DLHS-4 participants only)
eFigure 6. The predicted probability of diabetes by age group, rural-urban location, and household wealth quintile assuming AHS participants were unfasted
eFigure 7. The predicted probability of diabetes by age group, rural-urban location, and household wealth quintile among those in whom fasting status could be ascertained (ie, DLHS-4 participants only)
eTable 6. State-level age-standardized diabetes and hypertension prevalence estimates by sex
eTable 7. State-level age-standardized diabetes and hypertension prevalence estimates by rural vs urban location
eTable 8. State-level crude diabetes and hypertension prevalence estimates by age group
eTable 9. State-level age-standardized diabetes prevalence estimates by sex assuming all AHS respondents were unfasted
eTable 10. State-level age-standardized diabetes prevalence estimates by rural vs urban location assuming all AHS respondents were unfasted
eTable 11. State-level crude diabetes prevalence estimates by age group assuming all AHS respondents were unfasted
eFigure 8. Association of the state- and district-level age-standardized prevalence of diabetes with mean household wealth quintile
eFigure 9. Association of the state- and district-level age-standardized prevalence of hypertension with mean household wealth quintile
eFigure 10. Comparison of age-standardized national diabetes prevalence reported in different studies
eReferences