Abstract
Background: Many studies have investigated how unemployment influences health, less attention has been paid to the reverse causal direction; how health may influence the risk of becoming unemployed. We prospectively investigated a wide range of health measures and subsequent risk of unemployment during 14 years of follow-up. Methods: Self-reported health data from 36 249 participants in the Norwegian HUNT2 Study (1995–1997) was linked by a personal identification number to the National Insurance Database (1992–2008). Exact dates of unemployment were available. Cox’s proportional hazard models were used to estimate hazard ratios (HR) for the association of unemployment with several health measures. Adjustment variables were age, gender, education, marital status, occupation, lifestyle and previous unemployment. Results: Compared to reporting no conditions/symptoms, having ≥3 chronic somatic conditions (HR 1.78, 95% CI 1.46–2.17) or high symptom levels of anxiety and depression (HR 1.57, 95% CI 1.35–1.83) increased the risk of subsequent unemployment substantially. Poor self-rated health (HR 1.36, 95% CI 1.24–1.51), insomnia (HR 1.19, 95% CI 1.09–1.32), gastrointestinal symptoms (HR 1.17, 95% CI 1.08–1.26), high alcohol consumption (HR 1.17, 95% CI 0.95–1.44) and problematic use of alcohol measured by the CAGE questionnaire (HR 1.32, 95% CI 1.17–1.48) were also associated with increased risk of unemployment. Conclusion: People with poor mental and physical health are at increased risk of job loss. This contributes to poor health amongst the unemployed and highlights the need for policy focus on the health and welfare of out of work individuals, including support preparing them for re-employment.
Introduction
Following the Great Recession, concerns have been raised regarding possible health effects of millions of people losing their jobs. There is a growing body of evidence suggesting adverse effects on health of the crisis, especially concerning higher rates of suicide and mental illness. 1–6 Furthermore, evidence from different countries has indicated an association between unemployment and several health outcomes, including cardiovascular mortality, cancer mortality, poorer general health, somatic complaints, altered alcohol consumption and increased use of health services and prescription drugs. 7–12 However, the causal direction between unemployment and health is not straight forward.
While health effects of unemployment (causation hypothesis) have been extensively studied 13,14 less attention has been paid to whether poor health increases the risk of job loss (health selection hypothesis). If people with impaired health are more likely to lose their jobs, i.e. ‘selected’ into unemployment, this is an important public health issue per se and should be considered in preventive health care and the design of vocational rehabilitation programs. Further, health selection may confound the association between unemployment and health.
Although some studies have found a selection of workers with ill health into unemployment, 15–18 a recent meta-analysis found the selection effects to be weak. 19 However, the existing literature on the influence of poor health on the risk of unemployment has mostly been limited to studies on poor mental health 8,14,18 and overall self-rated health measures, 16,20 whereas somatic conditions and lifestyle have received little attention. High alcohol consumption as a predictor of unemployment has been studied with mixed results. 21 Many previous studies in this field have used survey data only 18 or had short periods of follow-up. 22 The aim of our study was to prospectively investigate the associations between health and lifestyle and subsequent risk of unemployment in a Norwegian labour market context.
Methods
The HUNT Study
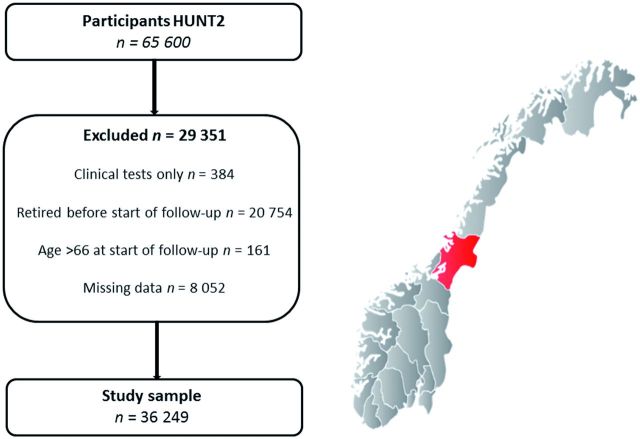
All residents of Nord-Trøndelag County in Norway aged ≥20 were invited to participate in the second wave of the HUNT Study (1995–1997, http://www.ntnu.edu/hunt/databank ). The study procedures and a non-participation study are described elsewhere. 23,24 Participants were asked to fill in questionnaires and undergo a physical examination. Of the 94 194 invited, 65 600 (70%) participated. In the present study, 36 249 were included in the analysis ( figure 1 ). Inclusion criteria were age 20–66, not pensioned before baseline or within the first year after baseline, having filled in the HUNT2 questionnaire and non-missing on exposures.
Figure 1.
Participants in the second wave of the Nord-Trøndelag Health Study (HUNT2 1995–1997), study sample and map—Norway, Nord-Trøndelag County. Map source: Wikimedia commons
The Norwegian Insurance Database (FD-trygd)
Statistics Norway’s National Insurance Database covers the entire Norwegian population since 1992 and provided entry/exit dates on all working life events for each HUNT2-participant: unemployment (registered and benefits), sick leave benefits, supplementary benefits, pensions, emigration and death.
Outcome ascertainment
The dependent variable time to unemployment was defined as time to first date of an unemployment period lasting for more than 90 days. We defined unemployed as being registered as 100% unemployed (actively job seeking, not necessarily on benefits) or fulltime participating in job creation programs. Duration of more than 90 days was chosen to avoid seasonal unemployment and students being short-term unemployed in summer holidays or after finishing studies. The median length of an unemployment episode was 99 days. We also created (i) an alternative outcome variable defined by time to unemployment lasting for >180 days, in order to capture health selection to long-term unemployment and (ii) an outcome variable measuring any unemployment, regardless of duration.
Health status at baseline
A detailed presentation of the health measures is given in appendix ( Supplementary Ttable 1 ). Symptoms of common mental disorders were measured using the 14-item Hospital Anxiety and Depression Scale (HADS, four-point Likert scale scored 0–3). 25 Seven items measured symptoms of depression and anxiety, respectively. Clinical caseness cut-off score was set to ≥8/21, concordant with validation studies reporting sensitivity and specificity for both anxiety and depression to be between 0.80 and 0.90. 25 Anxiety and depression symptoms were then combined into: No problems, anxiety only, depression only and comorbid anxiety and depression.
Chronic somatic conditions were measured as a categorical variable (0, 1, 2 and ≥3) reflecting the number of conditions reported. Participants were asked about presence of: (i) asthma; (ii) cardiovascular diseases (stroke, myocardial infarction or angina pectoris); (iii) diabetes; (iv) thyroid diseases; (v) rheumatic conditions (rheumatoid arthritis, osteoarthritis or ankylosing spondylitis); (vi) osteoporosis; (vii) epilepsy; (viii) cancer; (ix) other longstanding diseases; (x) traumas (hip fractures or other trauma necessitating hospital admission and (xii) physical handicap (vision, hearing, motor handicapped).
Somatic symptoms were measured as self-reported musculoskeletal pains (categorical, 0, 1, 2 and ≥3 depending on the number of affected joints), gastrointestinal complaints (dyspepsia, nausea, constipation or diarrhoea) and insomnia (‘How often do you suffer from insomnia?’ (about once a week or more than once a week), difficulty falling asleep or waking early (often or almost every night), insomnia to such a degree that it affected work (yes/no)).
The question ‘How is your health at the moment?’ (poor/not so good vs. good/very good) measured self-rated health.
Alcohol consumption was considered as likely to affect work ability and risk of unemployment and was included both as exposure and adjustment variable (in contrast to the other lifestyle measures). Questions of drinking frequency per month and whether teetotaller or not were combined into a categorical variable (teetotaller, 0 times (but not teetotaller), 1–4, 5–8, >8). The CAGE questionnaire was used to measure problematic alcohol use, with caseness cut-off ≥2, concordant with validation studies. 26
Adjustment variables
Age was categorized at 20–29; 30–39; 40–49; 50–59 and 60–66. Marital status and educational level measured socioeconomic position at baseline. Education was measured in three categories at start of follow-up; (i) compulsory education (primary school, lower secondary school or less), (ii) intermediate education (upper secondary school and post-secondary non-tertiary education), (iii) tertiary education (undergraduate, graduate and postgraduate). Occupation (HUNT2-questionnaire) was another measure of socioeconomic position that was considered a potential confounder, and we did a separate analysis adjusting for occupation ( Supplementary tables 3 and 4 ).
We also adjusted for lifestyle related variables: Body mass index—categorical variable (kg/m 2 , WHO standard: Normal range 18.5–24.99 (ref.), Underweight <18.5, Overweight ≥25, Obese ≥30). Physical activity—categorical variable ( high = vigorous activity for more than 1 h/week, moderate = vigorous for less than 1 h or light exercise more than 1 h/week, low = less active than moderate). Smoking status—categorical variable (never, previous, current) and alcohol consumption (described above).
As unemployment is likely to affect health, we adjusted for previous unemployment, measured as accumulated days (from 1992 to baseline).
Analysis
The association between health and risk of unemployment was investigated using Cox’s proportional hazard models with time from participation in the HUNT Study as the time axis. Start of follow-up was 90 days after participation in HUNT2, as we were concerned that some individuals may have been depressed as a result of a known upcoming redundancy (reverse causality). Similarly, those who became unemployed 90 days before or after participation in the study were left censored at the date of participation, so that none of the participants were unemployed at start of follow-up.
The participants were followed until date of first unemployment, emigration, death or permanent exit from the labour market (early/old age pension or temporary/permanent disability pension), whichever occurred first. For all main analyses the first date of unemployment was set to the first day of an unemployment episode lasting >90 days. In addition, sensitivity analyses were performed with the first day of an employment episode lasting >180 days. The statistical analyses were performed on participants with complete data on exposure variables (thus N varied between models).
Three models were analysed for each of the health indicators. Model 1 was adjusted for age, gender, education and marital status. Additional adjustment variables that could have status as both confounders and mediators were included in model 2: physical activity, body mass index, smoking and alcohol consumption (i.e. variables that could possibly be causing unemployment but also to some extent could be caused by unemployment). In model 3, we adjusted for cumulative length (days) of previous unemployment. We also investigated possible effect measure modification by age and sex for each of the health indicators, and did age-stratified analyses (< >50 years). The proportional hazards assumptions were tested based on Schoenfeld residuals. Results were reported as hazard ratios (HR) with 95% confidence intervals (CI). Statistical software: Stata 13.1.
Supplementary analyses
It is possible that individuals with underlying health problems experiencing job insecurity or job loss would go to their doctor and get a sickness absence certificate, instead of register as unemployed. Thus, sick leave could be a possible competing risk factor of unemployment and ‘mask’ a potential health selection process related to unemployment, especially in the Norwegian welfare state context with generous benefits. Unemployment benefits covers on average 62.4% of earned income the previous year and are granted conditional on several terms, the most important being that earned income the previous year exceeded €14132 (2014), and that working time is reduced by 50% or more. In contrast, Norwegian sickness benefits cover 100% of the income loss up until 1 year after first day of sick leave.
To explore potential competing risk, we analysed whether the risk of subsequent unemployment was reduced, if we took sick leave into account in a simultaneous analysis. Multinomial regression analysis was performed, comparing time to first sick leave period (≥ 8 weeks) with time to first period of unemployment (≥ 90 days). We divided follow-up time in 28 six-month periods from baseline to end of follow-up. The dependent variable took on three values; 0 = no unemployment or sick leave, 1 = unemployment (>90 days) or 2 = sick leave (>60 days). We investigated the same health and lifestyle variables as in the Cox’s proportional hazard models, and added a continuous time variable (1–28) indicating how many periods the participant contributed with data.
To explore health selection according to duration of unemployment, we performed a Cox proportional hazard analysis on time to end of unemployment with robust standard errors taking into account clustering of individuals with several unemployment periods. We hypothesized that those with several conditions or symptoms would have a lower risk of ending their unemployment spell quickly, compared to their healthier peers.
Ethics approval
The study was approved by the Regional Committee for Medical Research Ethics (ref. 2012/1941b). Written consent was given by all HUNT2 participants.
Results
Baseline characteristics are listed in table 1 . Maximum follow-up time was 13.8 years with 312 279 person-years, each person being followed for 8.6 years on average.
Table 1.
Characteristics at baseline (HUNT2, 1995–1997); study population ( N , %) and participants experiencing an unemployment period lasting for more than 90 and 180 consecutive days, respectively ( n , %). Missing values on each variable (%)
| Missing |
Total study population
|
Unemployment >90 days
|
Unemployment >180 days
|
||||
|---|---|---|---|---|---|---|---|
| % | N | % | n | % | n | % | |
| Study population | 36 249 | 100 | 3065 | 8 | 1991 | 5 | |
| Women | 0.0 | 19 345 | 53 | 1559 | 51 | 1102 | 55 |
| Mean age (SD) | 0.0 | 42 | (11.3) | 38 | (11.5) | 39 | (11.6) |
| Days of previous unemployment, mean (SD) | 0.0 | 74 | (216) | 218 | (361) | 213 | (371) |
| Mean drinking frequency per month (SD) | 3.8 | 2.7 | (2.9) | 2.7 | (3.3) | 2.5 | (3.6) |
| Mean BMI (SD) | 0.2 | 25.9 | (3.9) | 28.8 | (4.2) | 25.8 | (4.3) |
| Education | 0.2 | ||||||
| Compulsory education (or less) | 7715 | 21 | 889 | 29 | 612 | 31 | |
| Intermediate education | 20 450 | 57 | 1782 | 59 | 1134 | 57 | |
| Tertiary education | 8004 | 22 | 375 | 12 | 231 | 12 | |
| Marital status | 0.3 | ||||||
| Not married | 10 928 | 30 | 1472 | 48 | 882 | 44 | |
| Married | 22 228 | 62 | 1274 | 42 | 884 | 45 | |
| Widow(er) | 331 | 1 | 19 | 1 | 15 | 1 | |
| Divorced/separated | 2669 | 7 | 287 | 9 | 203 | 10 | |
| Anxiety and depression (HADS) | 1.6 | ||||||
| No anxiety/depression symptoms | 29 425 | 82 | 2342 | 78 | 1507 | 78 | |
| Anxiety symptoms only | 3521 | 10 | 352 | 12 | 222 | 11 | |
| Depression symptoms only | 1137 | 3 | 96 | 3 | 67 | 3 | |
| Anxiety and depression symptoms | 1604 | 5 | 212 | 7 | 151 | 8 | |
| Chronic somatic conditions | 0.9 | ||||||
| No conditions | 20 853 | 57 | 1665 | 54 | 1067 | 54 | |
| 1 condition | 11 057 | 31 | 987 | 32 | 660 | 33 | |
| 2 conditions | 3290 | 9 | 293 | 10 | 194 | 10 | |
| ≥3 conditions | 1049 | 3 | 120 | 4 | 70 | 3 | |
| Musculoskeletal pain | 0.0 | ||||||
| No symptoms | 12 788 | 35 | 1135 | 37 | 716 | 36 | |
| 1 symptom | 14 107 | 39 | 1147 | 37 | 272 | 37 | |
| 2 symptoms | 4165 | 11 | 330 | 11 | 215 | 11 | |
| ≥3 symptoms | 5180 | 14 | 452 | 15 | 314 | 16 | |
| Gastrointestinal complaints | 1.8 | 17 549 | 49 | 1626 | 54 | 1085 | 56 |
| Frequent insomnia symptoms | 0.5 | 5708 | 16 | 585 | 19 | 399 | 20 |
| Not so good/poor self-rated health | 0.7 | 5497 | 15 | 540 | 18 | 354 | 18 |
| Physical activity | 3.1 | ||||||
| Low physical activity | 5831 | 17 | 578 | 20 | 364 | 19 | |
| Moderate physical activity | 17 971 | 51 | 1407 | 47 | 946 | 49 | |
| High physical activity | 11 330 | 32 | 985 | 33 | 612 | 32 | |
| Smoking | 0.4 | ||||||
| Never smoker | 17 172 | 47 | 1252 | 41 | 787 | 40 | |
| Previous smoker | 8268 | 23 | 596 | 20 | 414 | 21 | |
| Current smoker | 10 682 | 30 | 1203 | 39 | 778 | 39 | |
| CAGE—problematic use of alcohol | 8.2 | 2902 | 9 | 362 | 13 | 221 | 12 |
Multivariable analyses
Over the follow-up period 3065 (8.4%) participants experienced one or more episodes of unemployment lasting more than 90 days; 1991 (5.4%) had periods of over 180 days unemployment. Results of the Cox’s regression analyses are presented in table 2 .
Table 2.
Hazard ratio (HR) for unemployment (>90 days) according to baseline symptoms of anxiety and depression, chronic somatic conditions, musculoskeletal pain, gastrointestinal symptoms, insomnia, self-rated health, alcohol consumption and problematic use of alcohol (CAGE)
|
Model 1
a |
Model 2
b,c |
Model 3
d |
||||
|---|---|---|---|---|---|---|
| HR | 95% CI | HR | 95% CI | HR | 95% CI | |
| Anxiety and depression (HADS) | ||||||
| No symptoms (78%) | 1.00 | Ref. | 1.00 | Ref. | 1.00 | Ref. |
| Anxiety only (12%) | 1.23 | 1.10-1.38 | 1.29 | 1.06-1.34 | 1.13 | 1.01-1.27 |
| Depression only (3%) | 1.33 | 1.08-1.63 | 1.25 | 1.01-1.55 | 1.20 | 0.98-1.49 |
| Anxiety and depression (7%) | 1.87 | 1.62-2.16 | 1.72 | 1.48-1.99 | 1.57 | 1.35-1.83 |
| Chronic somatic conditions | ||||||
| 0 (54%) | 1.00 | Ref. | 1.00 | Ref. | 1.00 | Ref. |
| 1 (32%) | 1.20 | 1.10-1.29 | 1.19 | 1.10-1.30 | 1.17 | 1.07-1.27 |
| 2 (10%) | 1.31 | 1.16-1.49 | 1.30 | 1.15-1.48 | 1.29 | 1.13-1.46 |
| ≥3 (4%) | 1.93 | 1.60-2.32 | 1.86 | 1.53-2.26 | 1.78 | 1.46-2.17 |
| Musculoskeletal pain | ||||||
| No symptoms (37%) | 1.00 | Ref. | 1.00 | Ref. | 1.00 | Ref. |
| 1 symptom (37%) | 1.08 | 0.99-1.18 | 1.05 | 0.96-1.14 | 1.05 | 0.96-1.15 |
| 2 symptoms (11%) | 0.99 | 0.88-1.12 | 0.98 | 0.86-1.12 | 0.97 | 0.85-1.10 |
| ≥3 symptoms (15%) | 1.13 | 1.01-1.27 | 1.07 | 0.94-1.19 | 1.03 | 0.91-1.15 |
| Gastrointestinal symptoms | ||||||
| No (46%) | 1.00 | Ref. | 1.00 | Ref. | 1.00 | Ref. |
| Yes (54%) | 1.25 | 1.16-1.34 | 1.20 | 1.12-1.30 | 1.17 | 1.08-1.26 |
| Insomnia | ||||||
| Not frequent (81%) | 1.00 | Ref. | 1.00 | Ref. | 1.00 | Ref. |
| Frequent (19%) | 1.37 | 1.25-1.50 | 1.27 | 1.15-1.40 | 1.19 | 1.09-1.32 |
| Self-rated health | ||||||
| Good/very good (82%) | 1.00 | Ref. | 1.00 | Ref. | 1.00 | Ref. |
| Poor/not so good (18%) | 1.51 | 1.37-1.66 | 1.43 | 1.29-1.58 | 1.36 | 1.24-1.51 |
| Alcohol consumption | ||||||
| 1–4 (59%) | 1.00 | Ref. | 1.00 | Ref. | 1.00 | Ref. |
| Teetotaller (5%) | 1.02 | 0.86-1.20 | 1.16 | 0.98-1.37 | 1.11 | 0.93-1.32 |
| 0 (but not teetotaller) (22%) | 1.07 | 0.98-1.18 | 1.09 | 0.99-1.20 | 1.07 | 0.97-1.17 |
| 5–8 (11%) | 1.13 | 0.99-1.27 | 1.09 | 0.96-1.23 | 1.08 | 0.95-1.22 |
| >8 (3%) | 1.09 | 1.00-1.51 | 1.20 | 0.98-1.48 | 1.17 | 0.95-1.44 |
| CAGE (problematic use of alcohol) | ||||||
| No (87%) | 1.00 | Ref. | 1.00 | Ref. | 1.00 | Ref. |
| Yes (13%) | 1.43 | 1.27-1.59 | 1.37 | 1.22-1.54 | 1.32 | 1.17-1.48 |
Notes: Total N = 36 249 with a maximum of 3065 unemployment episodes (failures). Percentage of unemployment episodes given in parenthesis. Complete case analysis with 95% confidence intervals (CI). Total N in the analyses varies according to missing values on exposures.
a: Adjusted for gender, age, education and marital status.
b: Adjusted for gender, age, education, marital status, physical activity, body mass index, smoking and alcohol consumption.
c: Model 2 with CAGE as exposure exclude alcohol consumption as adjustment variable.
d: Same as Model 2 + additional adjustment for accumulated days of previous unemployment (1992 to baseline).
In the age, gender, education and marital status-adjusted model there was nearly a double risk of unemployment in those having symptoms of both depression and anxiety [HR 1.87, 95% confidence interval (CI) 1.62–2.16] compared with those without such symptoms. Further adjustment for lifestyle and previous unemployment moderately attenuated the associations. The risk of job loss increased with increasing numbers of chronic somatic conditions, and was highest amongst the 4% reporting three or more conditions [fully adjusted (a) HR 1.78, 95% CI 1.46–2.17]. Elevated risk of unemployment was also found for musculoskeletal pain, gastrointestinal symptoms, insomnia, poor self-rated health and high/problematic alcohol consumption.
Results of the analysis replacing the outcome >90 days with >180 days of unemployment are presented in the appendix ( Supplementary table 2 ). It generally showed similar results compared to the original 90 days regression. As expected, the hazard ratios were slightly higher among those unemployed for a longer period of time. Adjusting for occupation did not change the results profoundly ( Supplementary tables 3 and 4 ).
We found no strong evidence that associations differed in males versus females on most of the health measures investigated ( P interaction 0.06–0.82); the exception was problematic use of alcohol assessed using CAGE ( P interaction 0.01); associations were stronger in women (aHR 1.84 (1.28–2.30) than men [aHR 1.16 (1.01–1.33), data not shown]. Likelihood-ratio tests indicated effect measure modification by age ( P interaction <0.001–0.016). Age-stratified analysis showed that those >50 had a weaker association between health and unemployment compared to those <50 years on almost all of the health measures ( Supplementary table 5 ).
Supplementary analyses
Results of the multinomial logistic regressions are presented as relative risk ratios (RRR), see Supplementary tables 6a–6g . This supplementary analysis gave close to similar results as the main analysis. The risk of sick leave were generally higher than the risk of unemployment for all the somatic conditions, while those reporting symptoms of both anxiety and depression had a higher risk of unemployment than of sick leave in all three models. The Cox analysis on unemployment length showed that those with several ill health conditions or symptoms had a higher risk of having longer unemployment spells, compared to those with fewer or no symptoms ( Supplementary table 8 ).
Discussion
We found evidence of health selection to unemployment. High symptom levels of anxiety and depression or having chronic somatic conditions nearly doubled the risk of subsequent unemployment. Having musculoskeletal pain, gastrointestinal symptoms, insomnia, high/problematic alcohol consumption or poor self-rated health were all factors associated with an increased risk of unemployment. Adjusting for lifestyle and previous unemployment slightly attenuated the estimates.
Strengths and limitations
The main strengths of this study are the detailed data on unemployment and the prospective design with longitudinal (18 years) register data on labour market status through record linkage. The analyses of sick leave as competing risk are, to the best our knowledge, a new contribution to the literature. Limitations are the lack of follow-up information on health, and potential biases related to non-response and self-reporting. 27 Further, although the assessment of anxiety and depression was based on a valid questionnaire, a (semi)structured psychiatric diagnostic interview would have given more reliable diagnostic information.
Context
The degree to which welfare benefits buffer reduced earning abilities in the unemployed is of importance for population health. 28 There are several aspects of Norway’s state benefits system that may influence the generalizability of the results to other settings. Norway has a high GDP/capita (86% above the average of EU28 in 2013, www.ssb.no/en/ppp ), generous social insurances, high degree of unionization, strong support of worker’s rights (with focus on the most vulnerable groups) and a comprehensive vocational rehabilitation system. The unemployment rate in Norway has been low for decades, and was relatively unaffected by the recession in 2007 ( Supplementary figure 1 ). However, sickness absence (7% of agreed working hours) and disability rates (10% of working age adults), both possible competing risk factors of unemployment, were reported the highest in OECD in 2014 (Organization for Economic Cooperation and Development). 29
Previous studies
A comparative study of the Scandinavian countries found no evidence of (self-reported) health selection to unemployment in Norway. 30 In keeping with our findings a systematic review and meta-analysis on health selection found that self-rated poor health was a risk factor for unemployment (RR 1.34, 95% CI 1.26–1.65). 20 Other studies have found evidence of mental health selection to unemployment in cohorts in Finland 8,31 and Australia. 18
There have been few studies on the association between unemployment and specific symptoms like musculoskeletal pain, gastrointestinal symptoms and insomnia, even though these are frequent causes of medical consultation and reduced work ability. 32 Also, gender differences in health selection are scarcely investigated. 13 Concordant to a French longitudinal study on health selection, 33 we did not find profound gender differences in the health related risk of unemployment. Our results on alcohol consumption and higher risk of subsequent unemployment, especially in women, are consistent with the results in a Swedish follow-up study. 21
Interpretation and possible mechanism
One could expect sickness benefits in Norway to filter health-related problems before they lead to unemployment. Still, those with ill health seem to have a higher risk of job loss and longer periods of unemployment following job loss, also shown in previous studies. 34 People with illness might be selected to more unstable jobs or they might lose their job more often because they are regarded less valuable to the employers. The unemployment rate will to some extent vary by socioeconomic position and occupation. However, adjusting for occupation did not alter the estimated risk of unemployment much. We interpret this as a result of educational level capturing most of these variations in a Norwegian labour market context.
We found that older workers with health problems were at lower risk of unemployment. This may be explained by a healthy worker effect—those ‘surviving’ in the labour force are the healthiest people (or they cope well with their health problems), while those with health impairment are more likely to exit earlier. It could also relate to the fact that older people have acquired skills and experience that are valued by their employers over and above health problems. Also, Norway’s employment legislation offers strong protection to older workers.
Introducing sick leave benefits as a competing risk factor of unemployment (Supplementary analysis) did not greatly alter our estimates of risk factors for unemployment. However, compared to participants reporting ill health on other health measures, those with symptoms of common mental disorders were somewhat more likely to lose their jobs than have periods of sick leave. This may indicate under-treatment, stigma and social exclusion in relation to mental health problems, as discussed in a recent review on mental health stigma, 35 and should be further investigated.
To conclude, the present study finds that poor health increases the risk of job loss. This evidence of health selection highlights the need for policy focus on the welfare of unemployed individuals, including support preparing them for re-employment.
Supplementary Material
Acknowledgements
The Nord-Trøndelag Health Study is a collaboration between the HUNT Research Centre (Faculty of Medicine, Norwegian University of Science and Technology), Nord-Trøndelag County Council, Central Norway Health Authority and the Norwegian Institute of Public Health. We would like to thank the HUNT Data Bank and Statistics Norway for providing data. We would also like to thank the two reviewers, who provided valuable comments and suggestions. Preliminary results of this study were presented orally at the 22 nd Norwegian Epidemiology Conference (NOFE) October 29-30 2014 in Trondheim, Norway, and at the European Public Health Conference (EPH), October 15 2015 in Milan, Italy.
Funding
Silje Lill Kaspersen and Kristine Pape were funded by the Liaison Committee between the Central Norway Regional Health Authority and the Norwegian University of Science and Technology. Gunnhild Åberge Vie was publicly funded by the Norwegian University of Science and Technology. David Gunnell is a NIHR Senior Investigator.
Conflicts of interest: None declared.
Key points
Health effects of unemployment have been extensively studied, while less attention has been paid to whether poor health increases the risk of job loss (selection hypothesis).
The existing literature on the influence of health on unemployment has mostly been limited to studies on poor mental health and overall self-rated health, whereas somatic conditions and lifestyle have been scarcely investigated.
This study found evidence of health selection to unemployment in Norway by linking baseline self-reported health data (1995–1997) to 14 years of follow-up in national registers.
Having chronic somatic conditions nearly doubled the risk of subsequent unemployment. Anxiety and depression, musculoskeletal pains, gastrointestinal symptoms, insomnia, high/problematic alcohol consumption or poor self-rated health were all factors associated with an increased risk of unemployment.
Our findings suggest a call for health perspectives in public employment programs.
References
- 1. Chang SS, Stuckler D, Yip P , et al. . Impact of 2008 global economic crisis on suicide: time trend study in 54 countries . BMJ 2013. ; 347 : f5239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Norstrom T, Gronqvist H . The Great Recession, unemployment and suicide . J Epidemiol Commun Health 2015. ; 69 : 110 – 6 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Stuckler D, Basu S, Suhrcke M , et al. . The health implications of financial crisis: a review of the evidence . Ulster Med J 2009. ; 78 : 142 – 5 . [PMC free article] [PubMed] [Google Scholar]
- 4. Webb RT, Kapur N . Suicide, unemployment, and the effect of economic recession . The Lancet Psychiatry 2 : 196 – 7 . [DOI] [PubMed] [Google Scholar]
- 5. Backhans MC, Hemmingsson T . Unemployment and mental health–who is (not) affected? Eur J Public Health 2012. ; 22 : 429 – 33 . [DOI] [PubMed] [Google Scholar]
- 6. Fergusson DM, Horwood LJ, Woodward LJ . Unemployment and psychosocial adjustment in young adults: causation or selection? Soc Sci Med 2001. ; 53 : 305 – 20 . [DOI] [PubMed] [Google Scholar]
- 7. Hammarstrom A, Gustafsson PE, Strandh M , et al. . It's no surprise! Men are not hit more than women by the health consequences of unemployment in the Northern Swedish Cohort . Scand J Public Health 2011. ; 39 : 187 – 93 . [DOI] [PubMed] [Google Scholar]
- 8. Heponiemi T, Elovainio M, Manderbacka K , et al. . Relationship between unemployment and health among health care professionals: health selection or health effect? J Psychosom Res 2007. ; 63 : 425 – 31 . [DOI] [PubMed] [Google Scholar]
- 9. Roelfs DJ, Shor E, Davidson KW, Schwartz JE . Losing life and livelihood: a systematic review and meta-analysis of unemployment and all-cause mortality . Soc Sci Med 2011. ; 72 : 840 – 54 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Eliason M, Storrie D . Job loss is bad for your health - Swedish evidence on cause-specific hospitalization following involuntary job loss . Soc Sci Med 2009. ; 68 : 1396 – 406 . [DOI] [PubMed] [Google Scholar]
- 11. Jin RL, Shah CP, Svoboda TJ . The impact of unemployment on health: a review of the evidence . CMAJ 1995. ; 153 : 529 – 40 . [PMC free article] [PubMed] [Google Scholar]
- 12. Ruhm CJ . Recessions, healthy no more? J Health Econ 2015. ; 42 : 17 – 28 . [DOI] [PubMed] [Google Scholar]
- 13. Norstrom F, Virtanen P, Hammarstrom A , et al. . How does unemployment affect self-assessed health? A systematic review focusing on subgroup effects . BMC Public Health 2014. ; 14 : 1310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Milner A, Page A, Lamontagne AD . Cause and effect in studies on unemployment, mental health and suicide: a meta-analytic and conceptual review . Psychol Med 2013. ; 1 – 9 . [DOI] [PubMed] [Google Scholar]
- 15. Fergusson DM, McLeod GF, Horwood LJ . Unemployment and psychosocial outcomes to age 30: A fixed-effects regression analysis . Aust N Z J Psychiatry 2014. ; 48 : 735 – 42 . [DOI] [PubMed] [Google Scholar]
- 16. Böckerman P, Ilmakunnas P . Unemployment and self-assessed health: evidence from panel data . Health Econ 2009. ; 18 : 161 – 79 . [DOI] [PubMed] [Google Scholar]
- 17. Schuring M, Robroek SJ, Otten FW , et al. . The effect of ill health and socioeconomic status on labor force exit and re-employment: a prospective study with ten years follow-up in the Netherlands . Scand J Work Environ Health 2012. . [DOI] [PubMed] [Google Scholar]
- 18. Butterworth P, Leach LS, Pirkis J , et al. . Poor mental health influences risk and duration of unemployment: a prospective study . Soc Psychiatry Psychiatr Epidemiol 2012. ; 47 : 1013 – 21 . [DOI] [PubMed] [Google Scholar]
- 19. Paul KI, Moser K . Unemployment impairs mental health: Meta-analyses . J Vocat Behav 2009. ; 74 : 264 – 82 . [Google Scholar]
- 20. van Rijn RM, Robroek SJ, Brouwer S, Burdorf A . Influence of poor health on exit from paid employment: a systematic review . Occup Environ Med 2013. . [DOI] [PubMed] [Google Scholar]
- 21. Backhans MC, Lundin A, Hemmingsson T . Binge drinking–a predictor for or a consequence of unemployment? Alcohol Clin Exp Res 2012. ; 36 : 1983 – 90 . [DOI] [PubMed] [Google Scholar]
- 22. Lundin A, Lundberg I, Hallsten L , et al. . Unemployment and mortality–a longitudinal prospective study on selection and causation in 49321 Swedish middle-aged men . J Epidemiol Commun Health 2010. ; 64 : 22 – 8 . [DOI] [PubMed] [Google Scholar]
- 23. Jostein Holmen KMØ, Krüger A, Langhammer T , et al. . The Nord-Trøndelag Health Study 1995-97 (HUNT 2):Objectives, contents, methods and participation . Norsk Epidemiologi 2003. ; 13 : 19 – 32 . [Google Scholar]
- 24. Krokstad S, Langhammer A, Hveem K , et al. . Cohort Profile: The HUNT Study, Norway . Int J Epidemiol 2013. ; 42 : 968 – 77 . [DOI] [PubMed] [Google Scholar]
- 25. Bjelland I, Dahl AA, Haug TT , et al. . The validity of the Hospital Anxiety and Depression Scale. An updated literature review . J Psychosom Res 2002. ; 52 : 69 – 77 . [DOI] [PubMed] [Google Scholar]
- 26. Skogen JC, Overland S, Knudsen AK , et al. . Concurrent validity of the CAGE questionnaire. The Nord-Trondelag Health Study . Addict Behav 2011. ; 36 : 302 – 7 . [DOI] [PubMed] [Google Scholar]
- 27. Van Loon AJ, Tijhuis M, Picavet HS , et al. . Survey non-response in the Netherlands: effects on prevalence estimates and associations . Ann Epidemiol 2003. ; 13 : 105 – 10 . [DOI] [PubMed] [Google Scholar]
- 28. Bambra C . Health inequalities and welfare state regimes: theoretical insights on a public health ‘puzzle’ . J Epidemiol Commun Health 2011. ; 65 : 740 – 5 . [DOI] [PubMed] [Google Scholar]
- 29. OECD. Mental Health and Work: Norway, Mental Health and Work, Paris, OECD Publishing, Paris, 2013. DOI: 10.1787/9789264178984-en . [DOI]
- 30. Heggebo K . Unemployment in Scandinavia during an economic crisis: cross-national differences in health selection . Soc Sci Med 2015. ; 130 : 115 – 24 . [DOI] [PubMed] [Google Scholar]
- 31. Virtanen P, Janlert U, Hammarstrom A . Health status and health behaviour as predictors of the occurrence of unemployment and prolonged unemployment . Public Health 2013. ; 127 : 46 – 52 . [DOI] [PubMed] [Google Scholar]
- 32. Ihlebaek C, Brage S, Eriksen HR . Health complaints and sickness absence in Norway, 1996–2003 . Occup Med 2007. ; 57 : 43 – 9 . [DOI] [PubMed] [Google Scholar]
- 33. Jusot F, Khlat M, Rochereau T , et al. . Job loss from poor health, smoking and obesity: a national prospective survey in France . J Epidemiol Commun Health 2008. ; 62 : 332 – 7 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Stewart JM . The impact of health status on the duration of unemployment spells and the implications for studies of the impact of unemployment on health status . J Health Econ 2001. ; 20 : 781 – 96 . [DOI] [PubMed] [Google Scholar]
- 35. Evans-Lacko S, Courtin E, Fiorillo A , et al. . The state of the art in European research on reducing social exclusion and stigma related to mental health: a systematic mapping of the literature . Eur Psychiatry 2014. ; 29 : 381 – 9 . [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.