Key Points
Question
Can a formulaic equation objectively classify the nasal base shapes and align with subjective classifications?
Findings
This study of 121 deidentified patient photographs supported the developed parametric model of the nasal base shape with 2 statistically significant parameters aligning with a subjective nasal base classification system.
Meaning
The nasal base can be objectively measured, described, and classified using a parametric model for preoperative planning, postoperative analysis, and objective comparison of nasal shape between patients, surgeons, and researchers.
This study assesses using an equation to quantitatively describe nasal base shape and tests it against subjective categorization.
Abstract
Importance
The nasal base view is often overlooked in rhinoplasty analysis and, unlike lateral and frontal views, lacks detailed quantitative analysis and descriptors. While shape-category analysis of the nasal base is well established, these descriptive methods remain subjective and do not facilitate quantitative analysis.
Objective
To establish a simple and quantitative classification scheme using a multiple-parameter numerical model for analyzing and describing the shape of the nasal base.
Design, Setting, and Participants
Deidentified photographs of the nasal base view were analyzed without knowledge of patients’ pathology or medical history. Each nose was classified into 1 of 6 categories derived from literature (equilateral, narrow, flat, cloverleaf, boxy, and round). Finite parametric modeling was performed on each nose, and the correlations between the resulting parameters and the 6 categories were analyzed. Photographs for this study were acquired from the practice of a single facial plastic surgeon (B.J.F.W.) at a tertiary care academic medical center. One hundred twenty-one consecutive patients who had nasal base view photographs taken were included in the study.
Main Outcomes and Measures
All of the 121 images were classified into 1 of the 6 categories by 1 reviewer (C.H.B.). The contour of each nasal base was curve fit to a 5-parameter numerical model. The 5 parameters controlled base size, deviation from the midline, projection-to-width ratio, degree of nasal alar recurvature, and anterior-posterior positioning of nasal base bulk. A numerical value for each nasal base shape type was predicted by the parametric model.
Results
In 121 patient photographs, the parametric model generated shapes that accurately matched the tracing of the actual nasal base contours with an average correlation coefficient of greater than 0.98. This finding indicates close approximation of the nasal base shape with the curve fit constructed by the PM. Parameters b (projection-to-width ratio) and e (roundedness) were shown to have significant differences among the groups (F statistic, 8.88; P < .001 and F statistic, 13.05; P < .001, respectively). These two curve-fit parameters alone could be used to classify nasal shape into 1 of the 6 clinically determined base geometries.
Conclusions and Relevance
A numerical approach to classify nasal base shape was developed using a 5-parameter model and tested against subjective analysis. This model may aid in the advancement of algorithm-driven objective nasal analysis techniques, preoperative modeling, intraoperative guidance, and surgical outcome measures beyond using Likert scales.
Level of Evidence
NA.
Introduction
Contemporary evaluation of aesthetic rhinoplasty outcomes is performed using semiquantitative grading systems incorporating Likert scales administered to either expert or lay focus groups.1,2,3,4,5 Both patient-reported and blinded-investigator analysis of rhinoplasty results are well established. However, these methods are still subjective, difficult to execute, and inefficient processes with discrepancies between patient- and surgeon-perceived results.6 While valuable for teaching, descriptive approaches lack consistency between surgeons. A more rigorous and efficient method to objectively analyze nasal shape and gauge outcomes would benefit both patients and surgeons.
Describing nasal geometry using quantitative methods at present is largely limited to linear and angular measurements,7 which do not incorporate the subtleties and features that make a nose attractive, in particular tip shape and alar curvature. Additionally, these isolated measurements alone do not allow reconstruction of the nasal base form by themselves as they are marginally descriptive and may be at variance with descriptive anatomy. Historically, the nasal base has generally been thought to be a simple geometric shape that approximates an isosceles triangle.8 Many classification systems have been developed over the years,7,9,10,11 but assignment to a particular category remains subjective. Additionally, base shape in a population varies along a spectrum without defined boundaries between shape types. Likewise, preoperative and postoperative outcomes are difficult to measure and describe quantitatively. For a classification method to be implemented, it needs to be consistent with commonly accepted nasal features, capable of recapitulating shape based on a limited set of numeric parameters, and easy to use.
Quantitative analysis of nasal shape must first start with the development of an analytic framework or model to provide numerical data in a bias-free manner. Innate pattern recognition through years of experience leads to reliable assessments by senior practitioners but is a difficult process for the neophyte. Classic anthropomorphic measurements of nasal base landmarks may be accurate and reproducible but cumbersome, leading many surgeons to forego objective analysis of the nose and rely solely on descriptive terminology, which dominates analysis strategy to date. To develop an analytic approach, the nasal base provides an ideal starting point. The classic triangular nasal base shape has been established and is generally validated among experts, and rhinoplasty surgeons strive to achieve this ideal shape with their surgical maneuvers (at least for patients of European origin).12,13,14
In this study, we developed a mathematical approach to objectively describe nasal base shape using a parametric model (PM). Then we compared the ability of this PM to segregate nasal base shapes into common clinically accepted shape categories in a population of patients.
Methods
Patient Selection and Classification
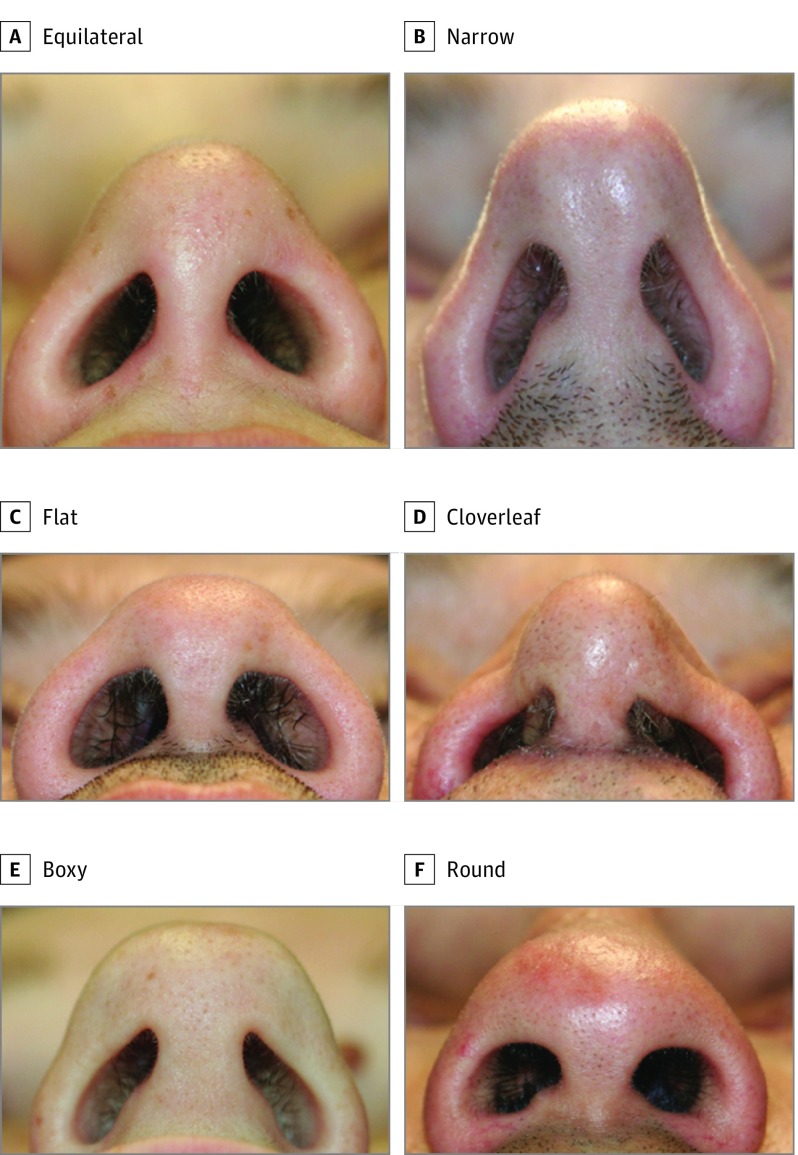
Approval for the study was obtained from the institutional review board of the University of California, Irvine. Patients provided consent to be photographed as part of patient care and documentation. The photographs were then deidentified before inclusion in the study. The medical records from the senior author (B.J.F.W.) for September 2014 to September 2015 were reviewed. Patients were included in the study if a standard nasal base view image was obtained and were excluded if an inadequate nasal base image was obtained or the patient had undergone nasal surgery in the past 6 months. Base view images for 121 consecutive patients were accumulated. Each image from the database was viewed full screen on a desktop computer monitor, analyzed, and then grouped based on similarity of shape. Shapes were clustered into 6 groups and were subsequently named based on their unifying geometric feature: equilateral, narrow, flat, cloverleaf, boxy, and round.9,10,11 Each image was assigned a category by visual inspection by a single surgeon (C.H.B.). Each category represents a nasal base shape that has fairly clear and distinct definitions (Figure 1). Categorizing into fewer groups led to dissimilar nasal types within a single group, and using more than 6 categories made accurate assignment challenging and complicated statistical analysis for the present sample size. The 6 categories are by no means exhaustive but are selected here for practical reasons and used to demonstrate parametric modeling.
Figure 1. Nasal Base Types Categorized by Perimeter Geometry.
Base view images for 121 patients were analyzed and clustered into 6 groups (A-F) based on their unifying geometric feature.
Computational Analysis
Using MATLAB (The MathWorks, Inc), the PM was empirically derived in polar coordinates that replicated the geometric features of the nasal base:
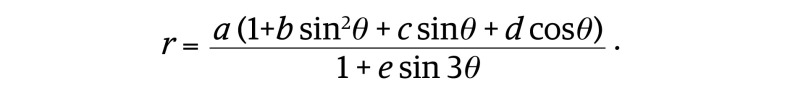 |
The equation was developed to keep the 5 parameters a through e independent except for using a (size) to normalize the other parameters. The shape of any object in nature can be empirically described using a number of curve-fitting techniques. Common examples are linear regressions and exponential curves to fit data. When objects are circlelike in shape, a change from Cartesian to polar coordinates is needed because such shapes can be defined as a function. In a mathematical function, 1 input variable precisely defines 1 output variable. The challenge here is that the shape of a given nasal base is complex. We know from descriptive anatomy that there are a limited number of archetype nasal base shapes, and that some shapes, like polygons, are extremely rare. Hence, the effort was to empirically identify a function in polar coordinates that could recapitulate the shape of each nasal base in our database. In terms of clinical use, we know of no quantitative means to define base shape or to track changes (eg, shape change after surgery).
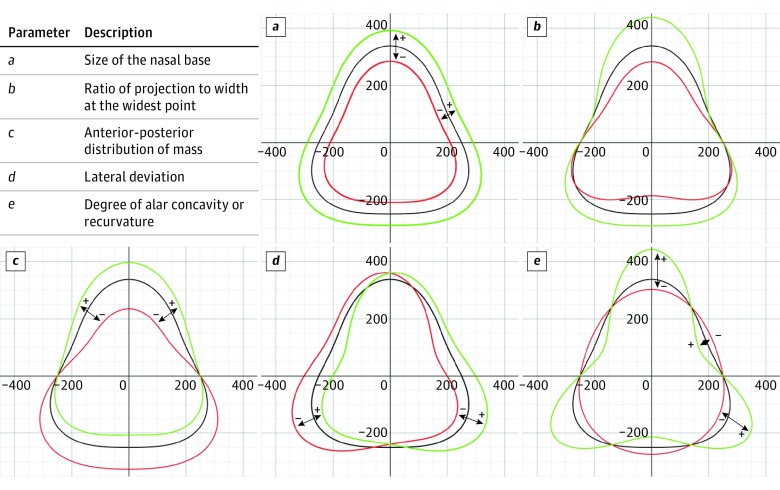
This PM replicates the shape of the nasal base using the 5 characteristic parameters. Parameter a is the scaling factor that adjusts the overall size of the base view and is used to normalize images taken from different distances or simply larger noses. Parameter b is directly proportional to the ratio of projection from the baseline to the width of the nose. Parameter c describes the anterior-posterior positioning of the tip bulk or mass of the nasal base akin to its center of gravity. As c increases, the majority of the mass of the plotted nasal base moves anteriorly, and vice versa. Parameter d delineates symmetry, where a positive value of d indicates deviation to the left side of the base, a negative value indicates deviation toward the right, and 0 is a perfectly midline nose. Parameter e describes the degree of lateral recurvature of the nasal base or presence of an alar margin furrow.15 Shapes with excess lateral recurvature are often described as similar to a 3-leaf clover. A high value of e indicates more prominent recurvature, whereas a low value of e is indicative of a simpler, rounder shape. Figure 2 summarizes the 5 scalar parameters of the PM. The effect of varying each parameter is graphically depicted in Figure 2A-E.
Figure 2. Model Parameters.
Five characteristic parameters were used to replicate the shape of the nasal base: a, size; b, projection-to-width ratio; c, tip bulk; d, lateral deviation; and e, roundedness. Plus signs (+) indicate an increase in the parameter value (green) with respect to a control (black), whereas minus signs (–) indicate a decrease in the parameter value (red).
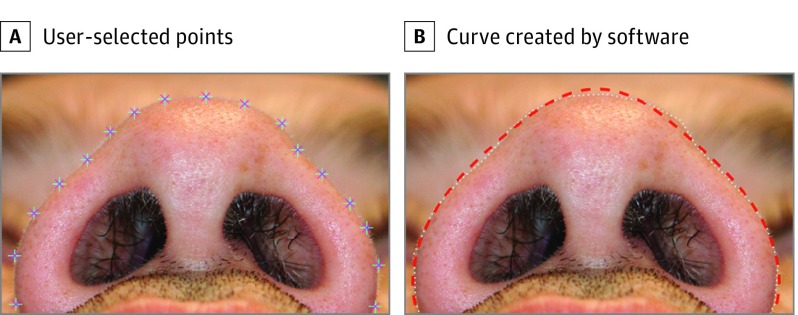
To implement the algorithm, the user imports a digital image of the nasal base into a MATLAB software program and then selects points that outline the contour of the nose using a track pad or mouse (Figure 3A) within a graphical user interface. Once the contour has been traced, the software performs a curve fit to the PM (Figure 3B) and calculates the key 5 parameters.
Figure 3. MATLAB Graphical User Interface.
A, The user can outline the contour of the nose by dotting in sequence. B, The white line represents the outline created by the user, and the red dashed line represents the result from the parametric model. After tracing the lateral anterior limits, points for the tip, base of columella, and most lateral points were selected.
All 121 images underwent this analysis, and all 5 parameters were tabulated. Regression analysis was also performed between each traced nasal base contour and the shape created by the PM to determine the accuracy of the curve fit. The parameter values were compared using ANOVA (analysis-of-variance) and t tests. ANOVA and 2-sample t tests were calculated using Microsoft Excel (Microsoft Corporation).
Results
Of the 121 images that met the inclusion criteria for parametric analysis, 25 were categorized as narrow; 24, equilateral; 24, round; 23, boxy; 14, cloverleaf; and 11, flat. Output data for the parameters of projection-to-width ratio (b), tip bulk (c), and roundedness (e) were analyzed. Parameters for total nasal base size (a) and lateral deviation (d) were not of value because they are a function of the distance of the camera to the subject and intrinsic left or right deviation of the tip, respectively.16 The mean Pearson correlation coefficient between the nasal base contour determined by the user and the nasal base contour calculated from the PM is 0.986. This finding indicates close approximation of the nasal base shape with the curve fit constructed by the PM.
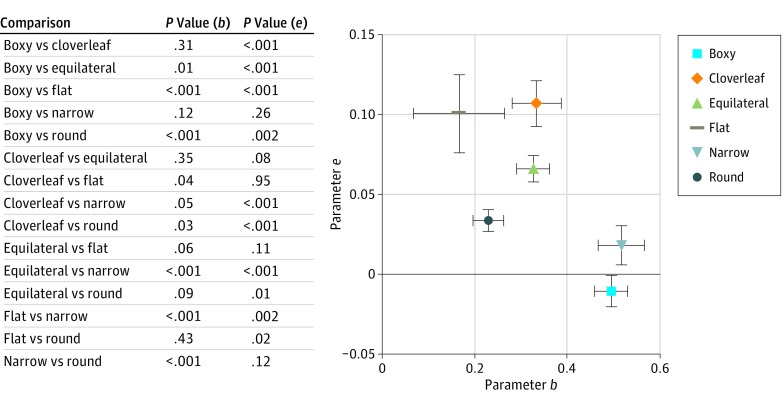
To determine whether or not the means of the 6 groups for each parameter are equal, analysis-of-variance testing was performed on each of the 3 studied parameters (ie, b, projection to width ratio; c, tip bulk; and e, roundness). Parameters b and e were shown to have significant differences among the groups (F statistic, 8.88; P < .001 and F statistic, 13.05; P < .001, respectively), while c was not significant (F statistic, 1.33; P = .32). A series of 2 sample t tests were performed for b and e to determine which nasal shape types were significantly different from one another. The multiple comparison t test results are summarized in Figure 4.
Figure 4. Results of 15 Classification Comparisons.
Multiple comparison t tests of parameters b and e. Graphical representation of the mean of each nasal base type. Error bars are shown.
On analysis, 8 of the 15 comparisons of parameter b and 10 of the 15 comparisons of parameter e demonstrate statistical significance (Figure 4). When considering both parameters, all groups were significantly different from one another except for 3 comparisons (cloverleaf vs equilateral, flat vs equilateral, and boxy vs narrow), which this numerical model fails to statistically differentiate from one another. The poorer performances for flat and cloverleaf could be due to the limited samples (nflat = 11 and ncloverleaf = 14), though a flat and cloverleaf base shape often go hand in hand.
Figure 4 displays the mean (SD) values for b and e for the 6 nasal base types. Distance between shape types on the graph is consistent with lower P values. No shape groups had high b and high e values or low b and low e values as patients with these features were not present in the tested population.
Discussion
Classification of nasal base by morphometry has been well established.17,18 However, the conventional morphometric techniques rely on the comparisons of numerous geometric measurements against an ideal or population norm. It is exceedingly time consuming, which precludes routine use and application. Ultimately, these measurements fail to provide sufficient descriptive data.
Accuracy of the PM
Numerical methods ideally must supply enough information to faithfully recreate the nasal shape. Although curve fitting is widely used to describe natural phenomena and structure across all fields of science, it is seldom used in facial aesthetic analysis. The first aim of this study was to create a numerical model that could accurately replicate the relevant traced outline of the nasal base shape. Here, the mean correlation coefficient between the hand-traced outlines and those generated by the PM is 0.986. Hence, the 5 parameters of this PM allow accurate representation of base geometry. This provides a means to potentially classify nose shape, and in practical terms provides a means to track preoperative and postoperative changes quantitatively and objectively. Such a quantitative approach is lacking in rhinoplasty analysis.
Classification of Base Shape
The second objective of this study was to determine if the 3 key model parameters can be used as a means to classify the nasal base shape into 1 of 6 commonly accepted clinical categories we selected. Classification is nonetheless a challenging task. There is no distinct boundary between groups because nasal base shape varies along a continuum. Also, a given nose may have features of more than 1 group and, hence, fit in multiple categories. For example, a nose may have both narrow and boxy features. Here, each nose was assigned to the group in line with its most prominent feature as determined by a single observer. The statistical analysis on this set of nasal base images was performed to identify potential limitations of this approach. The nasal base images used were not “textbook” shapes that fit squarely into 1 category. A real population of nasal base shapes was used without any preselection or filtering.
Figure 4 maps the distribution of base shape as a function of parameters b and e; these 2 parameters alone are valuable to categorize base shapes without the other 3 parameters in the model. The dispersion of the shapes aligns with logical expectations. The equilateral group is the least polarized and the most centrally located. It is this balance that makes this shape aesthetically attractive. It is expected that the flat nose and the narrow nose would fall in opposite ends of the graph as they are opposites in projection-to-width ratio, and this prediction is observed. Knowing the values of b and e alone, it is possible to categorize a given nasal base into its subjective shape group by using the PM. However, for the sample size analyzed here (n = 121), the standard error is large. Increasing the number of base images may reduce this variance. Of course, the large standard error also reflects that shape varies along a spectrum.
There were no base images that demonstrated a high level of recurvature with strong projection or low recurvature with underprojection. This observation is reasonable given the relatively uncommon observation of this base geometry. Noses with these values would appear largely projected with a narrow width and a high amount of recurvature or wide and underprojected yet with a very round shape.
The categorization of base shape by the PM compared well with traditional qualitative descriptions. While categorization of base shape is important for the rhinoplasty surgeon who wants to report quantitative outcomes, the PM provides a better means to document preoperative and postoperative changes, particularly those that aim to only create subtle changes in curvature, projection, or width as compared with current analysis methods. Improving the accuracy of this model can be achieved by increasing the sample population to derive more rigorous statistical classification. This refinement is an ongoing project in our group.
Limitations
While the 6 categories we selected from previously reported classification systems are to some degree arbitrary, they serve as a means to determine the accuracy of the PM to classify nasal base shape. The intergroup variability may be further reduced by increasing the number of categories, but doing so fails to simplify the historic, underused classification schemes. The size of the study, while sufficient to provide meaningful data, is inadequate to represent all possible nasal base types. Increasing the sample population numbers may increase statistical power to better detect differences among the groups and thus improve diagnostic yield. To this end specifically, we were limited by a paucity of flat and cloverleaf nasal base types.
One limitation of this PM is weaker correlation coefficients for noses with severe deformities, such as lateral deviation, sharp contour irregularities (such as those from trauma), or very concave alar margin furrows. However, the number of such noses was limited in this study, and more samples are needed to modify the model to better address uncommon base shapes. Nonetheless, the graphical user interface developed for analysis is simple to use and effective for the majority of base shapes. The user input is minimal (selecting points), and PM is largely objective. We intend to share this software package openly as an executable file and make it available for all interested parties. This parametric model for nasal base shape measurement, description, and documentation can be a useful tool for surgeons to report and compare outcomes quantitatively and objectively.
Conclusions
This study demonstrates the utility of an easily implemented and reliable nasal base classification system authenticated by a novel, objective, computer-based analysis of the base shape. The PM and the accompanying software provide a means to curve fit nasal base contour to a simple equation implemented in polar coordinates. This equation has value in terms of classifying base shape, and may prove useful as an objective means to gauge preoperative and postoperative outcomes by correlating shape changes with improvement in function, particularly if combined with Nasal Obstruction and Septoplasty Effectiveness Scale scoring. This PM is the first step toward standardizing methods to quantitatively describe nasal shape, and our study indicates that it is an objective and consistent means to study nasal base geometry. In particular, it provides a reproducible means to compare outcomes of different techniques and surgical approaches. The basis for the PM may serve as a foundation for objective quantification of the nasal shape from other standard views and ultimately 3-dimensional reconstruction.
References
- 1.Kosowski TR, McCarthy C, Reavey PL, et al. . A systematic review of patient-reported outcome measures after facial cosmetic surgery and/or nonsurgical facial rejuvenation. Plast Reconstr Surg. 2009;123(6):1819-1827. doi: 10.1097/PRS.0b013e3181a3f361 [DOI] [PubMed] [Google Scholar]
- 2.Klassen AF, Cano SJ, East CA, et al. . Development and psychometric evaluation of the FACE-Q scales for patients undergoing rhinoplasty. JAMA Facial Plast Surg. 2016;18(1):27-35. doi: 10.1001/jamafacial.2015.1445 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Alsarraf R. Outcomes research in facial plastic surgery: a review and new directions. Aesthetic Plast Surg. 2000;24(3):192-197. [DOI] [PubMed] [Google Scholar]
- 4.Cingi C, Toros SZ, Cakli H, Gürbüz MK. Patient-reported outcomes after endonasal rhinoplasty for the long nose. J Craniofac Surg. 2013;24(3):1002-1006. doi: 10.1097/SCS.0b013e31829024db [DOI] [PubMed] [Google Scholar]
- 5.Moolenburgh SE, Mureau MAM, Duivenvoorden HJ, Hofer SOP. Validation of a questionnaire assessing patient’s aesthetic and functional outcome after nasal reconstruction: the patient NAFEQ-score. J Plast Reconstr Aesthet Surg. 2009;62(5):656-662. doi: 10.1016/j.bjps.2007.07.024 [DOI] [PubMed] [Google Scholar]
- 6.Moolenburgh SE, Mureau MAM, Hofer SOP. Aesthetic outcome after nasal reconstruction: patient versus panel perception. J Plast Reconstr Aesthet Surg. 2008;61(12):1459-1464. doi: 10.1016/j.bjps.2007.09.018 [DOI] [PubMed] [Google Scholar]
- 7.Farkas LG, Hreczko TA, Deutsch CK. Objective assessment of standard nostril types—a morphometric study. Ann Plast Surg. 1983;11(5):381-389. [PubMed] [Google Scholar]
- 8.Tardy ME, Brown RJ. Surgical Anatomy of the Nose. New York, NY: Raven Press; 1990. [Google Scholar]
- 9.Bernstein L. Esthetic anatomy of the nose. Laryngoscope. 1972;82(7):1323-1330. doi: 10.1288/00005537-197207000-00022 [DOI] [PubMed] [Google Scholar]
- 10.Becker DG, Weinberger MS, Greene BA, Tardy ME Jr. Clinical study of alar anatomy and surgery of the alar base. Arch Otolaryngol Head Neck Surg. 1997;123(8):789-795. [DOI] [PubMed] [Google Scholar]
- 11.Rohrich RJ, Adams WP Jr. The boxy nasal tip: classification and management based on alar cartilage suturing techniques. Plast Reconstr Surg. 2001;107(7):1849-1863. [PubMed] [Google Scholar]
- 12.Toriumi DM. New concepts in nasal tip contouring. Arch Facial Plast Surg. 2006;8(3):156-185. [DOI] [PubMed] [Google Scholar]
- 13.Davis RE. Lateral crural tensioning for refinement of the wide and underprojected nasal tip: rethinking the lateral crural steal. Facial Plast Surg Clin North Am. 2015;23(1):23-53. [DOI] [PubMed] [Google Scholar]
- 14.Ballin AC, Kim H, Chance E, Davis RE. The articulated alar rim graft: reengineering the conventional alar rim graft for improved contour and support. Facial Plast Surg. 2016;32(4):384-397. [DOI] [PubMed] [Google Scholar]
- 15.Goodrich JL, Wong BJ. Optimizing the soft tissue triangle, alar margin furrow, and alar ridge aesthetics: analysis and use of the articulate alar rim graft. Facial Plast Surg. 2016;32(6):646-655. [DOI] [PubMed] [Google Scholar]
- 16.Nagy K, Mommaerts MY. Analysis of the cleft-lip nose in submental-vertical view, part I—reliability of a new measurement instrument. J Craniomaxillofac Surg. 2007;35(6-7):265-277. doi: 10.1016/j.jcms.2007.04.010 [DOI] [PubMed] [Google Scholar]
- 17.Lee MR, Tabbal G, Kurkjian TJ, Roostaeian J, Rohrich RJ. Classifying deformities of the columella base in rhinoplasty. Plast Reconstr Surg. 2014;133(4):464e-470e. doi: 10.1097/PRS.0000000000000022 [DOI] [PubMed] [Google Scholar]
- 18.Kim JH, Park JP, Jang YJ. Aesthetic outcomes of alar base resection in Asian patients undergoing rhinoplasty. JAMA Facial Plast Surg. 2016;18(6):462-466. doi: 10.1001/jamafacial.2016.0800 [DOI] [PubMed] [Google Scholar]