Abstract
Background: Understanding patterns of injury in England is challenging due to a lack of national injury surveillance data. Through recent linkage of a large primary care research database to hospitalization and mortality data, we describe the epidemiology of poisonings, fractures and burns over a 14-year period. Methods: We used linked English primary care, hospitalisation and mortality data from the Clinical Practice Research Datalink, Hospital Episode Statistics and Office for National Statistics between 1998 and 2011 to establish a cohort of 2,106,420 0–24 year olds. Incidence rates, per 10 000 person-years (PY) were estimated by age, sex, calendar year and socioeconomic status. Using Poisson regression we estimated incidence rate ratios, adjusting for age and sex. Results: Age patterns of injury incidence varied by injury type, with peaks at age 2 (74.3/10 000 PY) and 18 (74.7/10 000 PY) for poisonings, age 13 for fractures (305.1/10 000 PY) and age 1 for burns (116.8/10 000 PY). Over time, fracture incidence increased, whereas poisoning incidence increased only among 15–24 year olds and burns incidence reduced. Poisoning and burns incidence increased with deprivation, with the steepest socioeconomic gradient for poisonings among 20–24 year olds (IRR 2.63, 95% confidence interval 2.24–3.09). Conclusion: Differing patterns according to age and injury type reflect differences in underlying injury mechanisms, highlighting the importance of developing tailored preventative interventions across the life course. Inequalities in injury occurrences support the targeting of preventative interventions to children and young people living in the most deprived areas.
Introduction
Injuries among children and young people continue to be a public health priority across Europe, remaining the leading cause of death, and accounting for an estimated 16.2 million hospital attendances each year among those aged 0–24.1 Three of the commonest injuries of childhood and adolescence are poisonings, fractures and burns; injuries highlighted as priorities for prevention both within the United Kingdom (UK) and Europe.2,3 There is recognition across Europe that injury data collection systems need strengthening to allow more specific targeting of interventions and monitoring of progress.4 Within the UK there is no national injury surveillance system, with existing hospitalisation and mortality data only capturing a small proportion of the injury burden.5 The recent linkage of a large population-based primary care research database to hospitalisation and mortality data offers new potential for injury surveillance in England. We therefore aimed to describe the epidemiology of poisonings, fractures and burns for children and young people aged 0–24 living in England, using these linked data sources, with the aim of informing injury prevention strategies.
Methods
Setting and study population
The Clinical Practice Research Datalink (CPRD) is a large primary care research database containing the primary care records of over 11 million patients from the UK.6 In the UK, over 98% of the resident population is registered with a general practitioner (GP).7 GPs play a central role in managing the health of their registered patients, maintaining a longitudinal health record, including recording information received about patient utilisation of secondary and tertiary health services [e.g. emergency department (ED) attendances, specialist burns units]. Medical data are recorded in CPRD using Read codes, a clinical coding system.
Using the CPRD, we conducted an open cohort study of children and young people aged 0–24 living in England, who were registered with a CPRD practice between 1998 and 2011 and had their primary care record linked to hospitalisation and mortality data. Within England, hospitalisation data are held within the Hospital Episode Statistics (HES) inpatient dataset, which captures elective and emergency hospitalisations paid for by the National Health Service. Diagnoses and procedures are coded in HES using the International Classification of Diseases revision 10 (ICD-10), and Office of Population Census and Surveys version 4 (OPCS-4), respectively. All deaths occurring in England are captured in the Office for National Statistics (ONS) mortality dataset, with ICD-10 used to record cause of death. CPRD, HES and ONS mortality data were linked by a trusted third party using the patient’s unique identifier, sex and date of birth. For the period 1998–2011, 356 general practices contributing to the CPRD had linked HES and ONS mortality data (∼4% of English practices in 2011). Data from linked CPRD-HES practices are broadly representative of the age and sex structure of the English population,6,8 but underrepresents practices from the North East, East Midlands and Yorkshire and the Humber.
The start of follow-up for each participant was the latest date of: their date of birth, practice registration date, 1st January 1998, and the date the practice met the CPRD data quality standards. The end of follow-up was the earliest date of: 31 December 2011, participant’s 25th birthday, death date, date of practice deregistration and the date medical data were last collected from the practice.
Injury outcomes
We identified all poisoning, fracture and burn events, regardless of their intent, recorded in primary care (CPRD), hospitalisation (HES) or mortality data (ONS) using comprehensive Read, ICD-10 and OPCS-4 code lists. Each injury outcome was defined according to ICD-10 categories (Supplementary table S1).
By using three linked data sources we aimed to maximise our capture of medically attended injuries, as there is no single data source in England that comprehensively captures all injury occurrences. Some injuries will however be recorded in multiple data sources; for example a child hospitalised for a fracture will have a record in HES, but may also have a record in primary care (CPRD) when the GP receives correspondence from secondary care. In addition, a child may have multiple records for the same injury when follow-up care is required. To avoid over-counting injury events we used a time-based algorithm, as previously described,5 to define incident injury events in linked CPRD-HES-ONS data. In brief, we assessed the time between the first code for an injury event and all subsequent records for that injury type. Those records occurring within a certain time-window of the event date (i.e. likely to indicate follow-up care, or the same injury recorded in multiple data sources) were considered the same event (Supplementary table S2). Those records occurring outside of the time-window were considered a new injury event. This method enabled the inclusion of repeated injury events per study participant.
Causes of injury
Within ICD-10, the external cause codes (V01-Y36, Y90-Y98) classify injuries according to how they occurred (e.g. transport accidents) or whether the injury was unintentional or intentional. For each injury recorded in HES and ONS mortality data we identified the external cause of injury, and assessed the proportions of events due to each cause by child age. We do not report injury mechanisms/intent for events only recorded in primary care, as recording is incomplete within UK primary care data (e.g. available for 2% of fractures and 4% of burns).5
Statistical analyses
Injury incidence rates were estimated per 10 000 person-years (PY) with 95% confidence intervals (95%CI) by age, sex, socioeconomic status and calendar year. We measured socioeconomic status using quintiles of the Index of Multiple Deprivation 2010, a measure of deprivation based on area of residence.9 Using Poisson regression we calculated adjusted incidence rate ratios (aIRR) for socioeconomic status and calendar year, adjusting for age and sex. Calendar time was divided into two periods (1 January 1998–31 December 2004, and 1 January 2005–31 December 2011). We estimated the burden of poisonings, fractures and burns among 0–24 year olds for the year 2011 by applying injury incidence rates by age and sex to the 2011 population estimate for England.10 All analyses were conducted using Stata version 13.0. The study was approved by the Independent Scientific Advisory Committee for the Medicines and Healthcare products Regulatory Agency (protocol 13-199R).
Results
The study cohort consisted of 2 106 420 children and young people, contributing a total of 9 814 557 PYs of follow-up. Of the study population, 1 029 379 (49%) were male and 1 077 041 (51%) were female, with similar proportions of the cohort from each socioeconomic quintile (Supplementary table S3). During study follow-up, 40 931 poisonings, 177 524 fractures, and 34 819 burns occurred among the cohort, giving incidence rates for 0–24 year olds of 41.7/10 000PY (95%CI 41.2-42.2), 180.9 (95%CI 180.0-181.8) and 35.5 (95%CI 35.1-35.9), respectively.
Age and sex
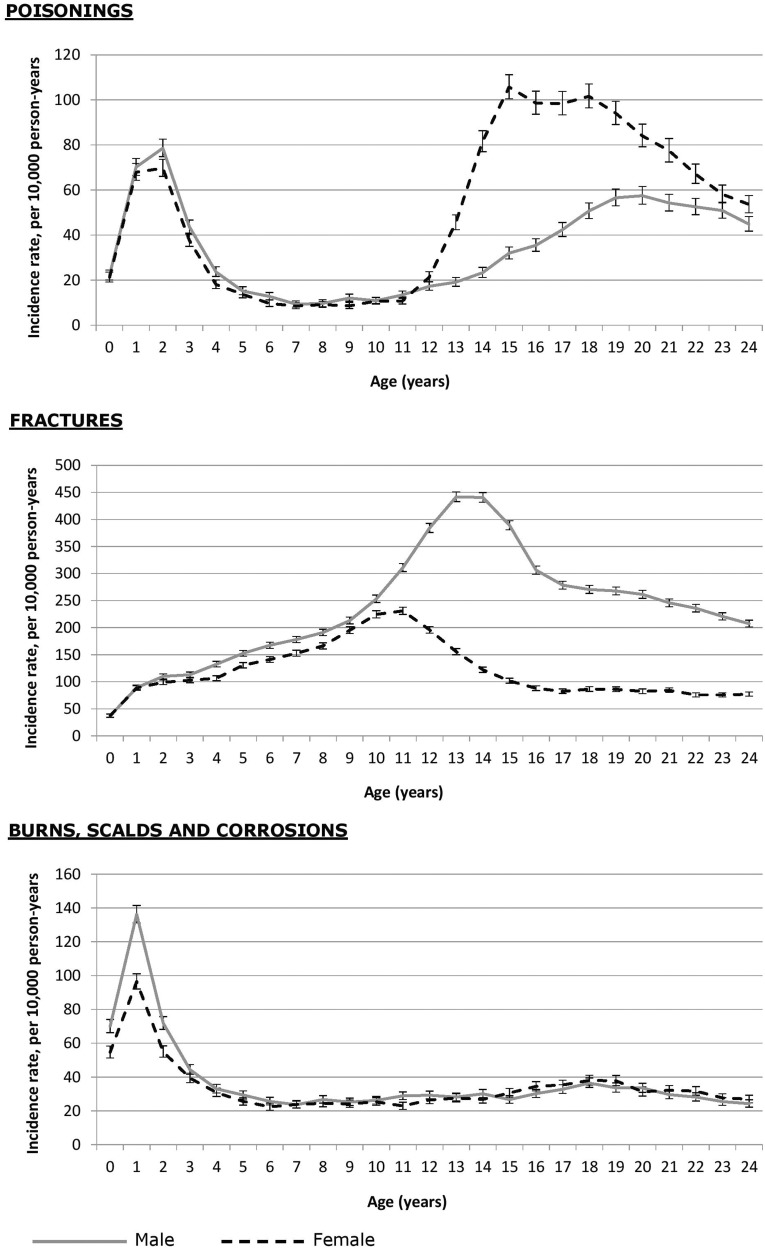
Age patterns varied by injury type (figure 1), with peaks in injury incidence at age 2 (74.3/10 000 PY) and 18 (74.7/10 000 PY) for poisonings, age 13 for fractures (305.1/10 000 PY) and age 1 for burns (116.8/10 000 PY). Among children aged 0–4, males (48.1/10 000PY, 95%CI 46.7-49.6) had a higher poisoning incidence than females (43.3/10 000PY, 95%CI 42.0–44.7). Comparatively, poisonings increased among females after the age of 12, with incidence over twice as high for females aged 15–24 compared with males of this age (females:99.8/10 000 vs. males:43.1/10 000). Across all ages, fracture incidence was higher among males than females, peaking at age 11 in females (231.0/10 000PY) and age 13 in males (441.8/10 000PY). Males aged 0–4 had a significantly higher burns incidence (71.0/10 000PY) than females (55.2/10 000PY). After the age of 5, burns incidence remained between 20 and 35/10 000PY with incidence similar between males and females.
Figure 1.
Incidence of poisonings, fractures and burns by age and sex, using linked health and mortality data 1998–2011
Socioeconomic inequalities
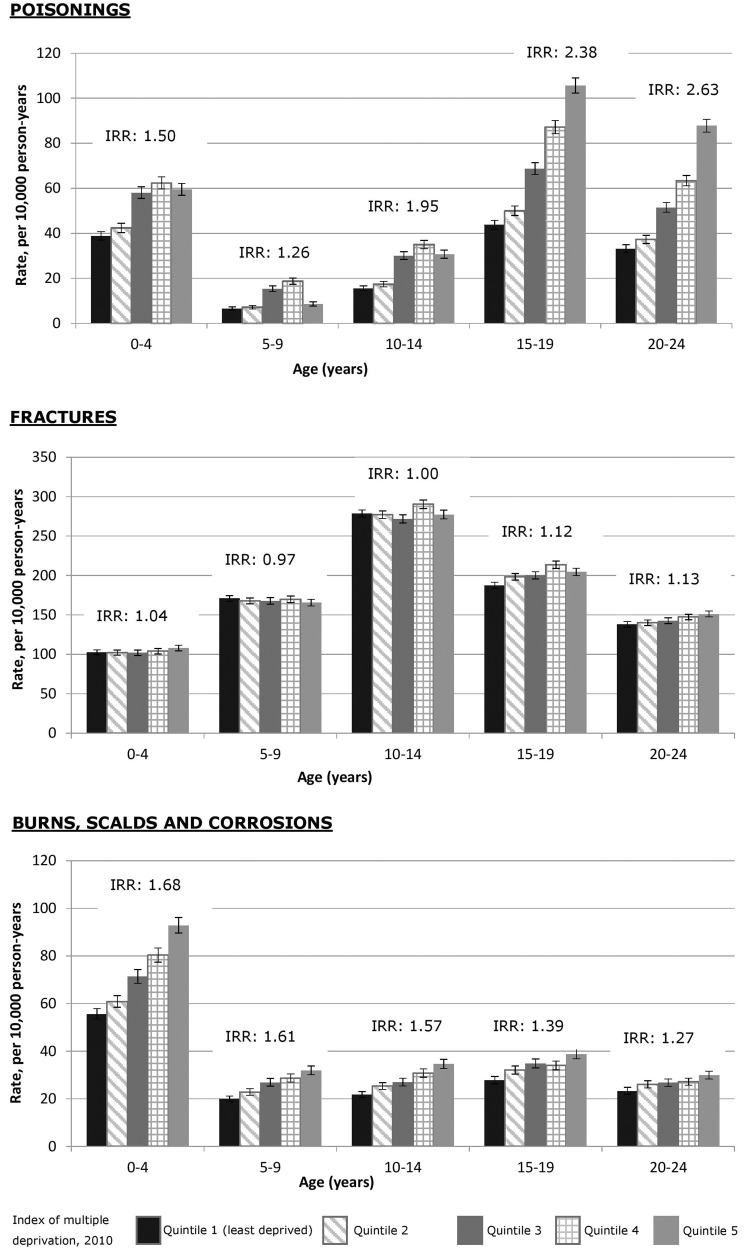
Among 0–24 year olds, those in the most deprived quintile had a 2-fold higher rate of poisonings (aIRR 2.12, 95%CI 1.68–2.69), and a 53% higher rate of burns (aIRR 1.53, 95%CI 1.40–1.68) compared to those in the least deprived quintile. Comparatively, there was no significant difference in fracture rates between the most and least deprived quintiles (aIRR 1.04, 95%CI 0.89–1.22). The strength of socioeconomic gradients varied with age (figure 2), with the steepest gradient seen for poisonings among 20–24 year olds (aIRR 2.63, 95%CI 2.24-3.09). Significant differences in fracture rates between the most and least deprived quintiles were only seen for 0–4 (aIRR 1.04, 1.02-1.07), 15–19 (aIRR 1.12, 95%CI 1.09–1.15) and 20–24 year olds (aIRR 1.13, 95%CI 1.12–1.14); considerably smaller socioeconomic gradients than seen for poisonings and burns.
Figure 2.
Incidence of poisonings, fractures and burns among children and young people by age and socioeconomic status, using linked health and mortality data 1998–2011
Incidence over time
Among 0–24 year olds, burns incidence significantly reduced between the first (1998–2004) and last (2005–11) study periods (aIRR 0.84, 95%CI 0.82–0.85; Supplementary table S1). In contrast, fracture incidence increased by 20% between these periods (aIRR 1.20, 95%CI 1.79–1.21), whereas poisoning incidence remained the same (aIRR 1.03, 95%CI 1.00–1.05). Trends over time for burns and fractures were consistent across age groups, whereas for poisonings patterns differed by age. Among 0–4 years olds, poisoning incidence reduced from 53.4/10 000PY to 40.0/10 000PY between the first and last study periods. Comparatively, poisoning incidence increased between the first and last study periods among 15–24 year olds.
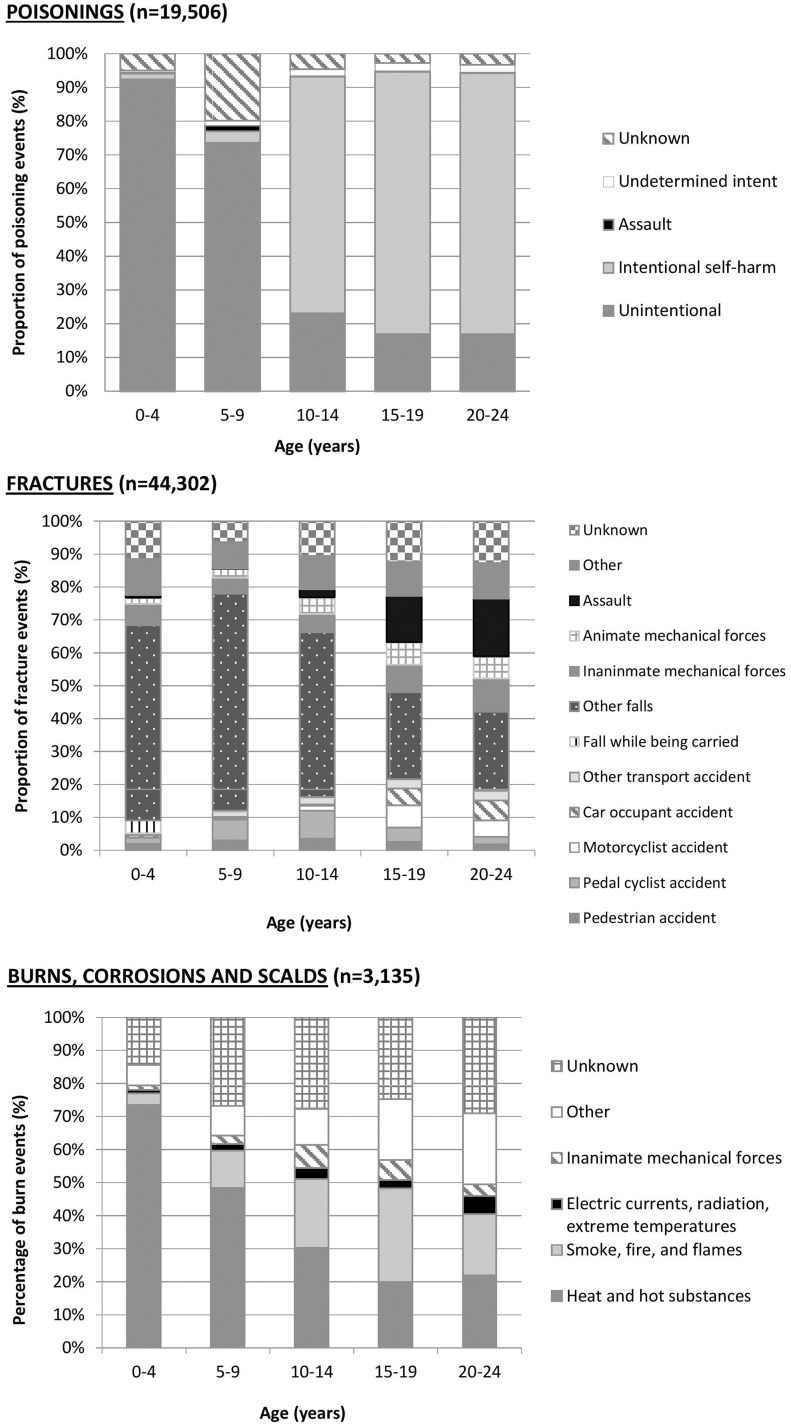
Cause of injury: hospitalisations and deaths
Among the cohort, 19 408 poisoning, 44 250 fracture and 3125 burn events led to hospitalisation, and an additional 106 poisoning, 58 fracture and 10 burn events led to death (of which some were also hospitalised prior to death) during the period 1998–2011. Figure 3 shows injury mechanisms for these hospitalisations and deaths. Among 0–4 year olds, 92.5% (n = 2864) of poisonings were recorded as unintentional, contrasting with 77.6% of poisonings among 20–24 year olds coded as intentional self-harm. Across all ages the most common fracture mechanism was a fall, although the proportion of events due to falls reduced with age (63.6% in 0–4 year olds, 24.1% in 20–24 year olds). The proportion of fractures resulting from transport accidents peaked in 15–19 year olds, accounting for 21.6% of fractures in this age group. Assault accounted for 14.0% of fractures in 15–19 year olds and 17.5% in 20–24 year olds. In 0–4 year olds, burns were most commonly due to exposure to heat and hot substances (e.g. hot drinks, bathwater scalds), accounting for 74.2% of the 1726 burns in this age group. The proportion of events due to this mechanism reduced with age (21.6% in 20–24 year olds).
Figure 3.
External causes of injury according to age, for poisoning, fracture and burn events leading to hospitalisation or death, 1998–2011
Estimates of poisonings, fractures and burns in England
Using 2011 population census data, our estimated incidence rates equate to a total of 70 918 poisonings, 340 033 fractures and 49 973 burns occurring in 2011 among 0–24 year olds living in England.
Discussion
We present the first UK study to provide detailed injury incidence estimates by child characteristics through the use of linked primary care, hospitalisation and mortality data. In 2011, at least 70 918 poisonings, 340 033 fractures and 49 973 burns occurred among 0–24 year olds in England; vital information to those planning health services and developing injury prevention programmes. We have demonstrated notably different patterns in injury incidence by age, sex, calendar year and socioeconomic status for the three injury types, reflecting differences in underlying mechanism and intent. Fracture incidence increased over time for all ages, whereas poisoning incidence increased only among 15–24 year olds, and burns incidence reduced over time. Children from more deprived areas had higher injury rates, with the strength of the socioeconomic gradient varying by age and injury type.
Strengths and limitations
By using three linked data sources, we have been able to provide more complete estimates of injury incidence than currently exist, capturing not only injuries leading to hospitalisation, but also those leading to death prior to hospitalisation and those recorded within primary care only. In addition, through using a time-based algorithm to define injury events we have been able to include repeated injury events over time. A strength of our study is the use of a large cohort of over 2 million children and young people drawn from the CPRD, which has been shown to be broadly representative of the demographics of the UK population.6 Underrepresentation of practices from the North West, Yorkshire and Humber and East Midlands may lead to some underestimation of injury incidence, as injury rates tend to be higher in these areas.11 Universal health coverage, with high GP registration,7 and emergency care almost exclusively provided by the NHS12 mean we are unlikely to be substantially underestimating injury incidence as a result of individuals being managed by the private sector.
The main limitations of this study relate to data quality and availability, as these data were primarily captured for administrative and clinical purposes. We have previously shown injury mechanism and intent are poorly recorded in primary care data,5 and so the patterns described in figure 3 reflect causes of severe injuries leading to hospitalisation and/or death. For example, the percentage of fractures due to transport accidents (15.7%) is considerably higher than estimates from ED data (1.4% of fractures in 0–14 year olds).13 Additionally, information about specific consumer products (e.g. dishwasher tablets) and where the injury occurred (e.g. playground) are poorly recorded in these data. While GPs do record correspondence from EDs in the primary care record, we cannot be certain that all injury events were captured if information was not received by the GP or if information was recorded using non-specific codes (e.g. ‘seen in ED’) or free text. In future, linkage of ED data to CPRD would ensure all medically-attended injuries are captured and may provide more comprehensive data on injury mechanisms for those injuries not leading to hospitalisation or death. We measured socioeconomic status based on area of residence, which may not accurately capture an individual’s socioeconomic position. However, as many injury prevention programmes are delivered at population levels (e.g. geographical areas), our findings are relevant to those planning and delivering services.
Comparison to existing literature
Our estimates of injury incidence and patterns by age and sex are consistent with available literature. Similar to UK and European studies,14,15 we demonstrated a higher and later peak in fracture incidence among males compared with females. A peak in burns and poisoning incidence at ages 1–2 years, higher among males than females, is consistent with studies using hospitalisation and ED data,16–18 and can largely be explained by the developmental changes and exploratory behaviour of children at this age.16,17 We found young women aged 15–24 had substantially higher rates of poisonings than males; consistent with studies of adolescent self-harm showing considerably higher rates among females.19–21
Our finding of higher poisoning and burns incidence among the most deprived groups is consistent with existing hospital-based studies.22–25 Comparatively, literature on socioeconomic differences in fracture rates is less consistent.24,26,27 For example, Stark et al.26 found children aged 0–14 from deprived areas of Glasgow had a 25% higher rate of fractures than those living in the least deprived areas; differing from Lyons et al.27 who found no association between socioeconomic status and fracture rates among children in Wales. While our finding of similar rates of fractures by socioeconomic group among 5–14 year olds, and relatively small differences in fracture rates (4–13%) amongst the other age groups is surprising, it is plausible that differing underlying mechanisms and exposures between socioeconomic groups (e.g. time and type of sport played, exposure to road hazards) may lead to an offsetting of rates between socioeconomic groups. Future studies should consider how socioeconomic gradients vary by fracture mechanism, as this may have implications for developing preventative interventions.
Similar to a recent study of poisoning hospitalisations22 and a cohort study using primary care data28 we found reductions in poisoning and burns incidence among children aged 0–4 over time. These observed reductions may reflect improved public awareness, legislative changes and successes of preventative programmes.29 In contrast, we found an increase in fracture incidence across all ages, similar to a Swedish study that found a 59% increase in fracture incidence between 1993 and 2007.30 Comparatively, a study from Finland found an 18% reduction in fracture incidence between 1983 and 2005, although trends differed by fracture site (e.g. increase in forearm fractures).15 Explanations for an increase in fracture incidence may include increasing childhood obesity, associated with both upper and lower limb fractures31,32 and changes in child leisure activities, with the clearest example being the increase in fractures related to trampolining.33 These explanations, however, may not fully explain the trend we have observed, particularly as there have been reductions in other fracture mechanisms, such as road traffic accidents.34 A possible explanation is that the trend we have observed reflects an increase in surgical stabilisation of some fractures (e.g. forearm fractures),35,36 which if leading to an increase in the proportion of children hospitalised, could result in improved capture of fracture events within the data sources we are using. Similarly, while there is some evidence to suggest our observed increase in poisoning incidence among 15–24 year olds may be genuine,37 changes to national guidance on the management of self-harm in 2004,38 recommending inpatient admission and psychiatric review for those aged <16, may have increased the proportion of poisonings resulting in hospitalisation. The use of other data sources and future linkage of ED data to CPRD (when it becomes available) will be important in verifying these trends.
Implications for research and practice
We have demonstrated that the ability to link primary care, hospitalisation and mortality data allows more comprehensive estimates of injury incidence than previously available in England, with these linked data holding potential for injury surveillance. Future linkage of ED data to CPRD will ensure all medically attended injuries are captured, allow verification of trends in incidence over time and provide further information on injury mechanism and intent.
Differing injury patterns seen within this study highlight the importance of taking a strategic, life-course approach to injury prevention, with interventions tailored according to child age and injury type. With a broad range of effective interventions available, including population-wide initiatives (e.g. product safety measures),39 community initiatives (e.g. traffic calming measures)39 and family interventions (e.g. home safety schemes),40 there is a need for a multiagency approach at both local and national levels. High rates of adolescent self-poisonings highlight the need for close links between injury prevention, mental health and substance misuse strategies. Alongside implementing universal injury prevention approaches for all children and young people, our finding of socioeconomic gradients in injury occurrences supports the targeting of preventative interventions to households in the most deprived areas.3
Supplementary Material
Acknowledgements
R.B. is funded by the National Institute for Health Research School for Primary Care Research (NIHR SPCR) and The University of Nottingham. This work has previously been presented at the School for Primary Care Research Conference, Oxford England on the 9 July 2015.
Funding
R.B. is funded by the National Institute for Health Research School for Primary Care Research (NIHR SPCR) and The University of Nottingham.
Supplementary data
Supplementary data are available at EURPUB online.
Conflicts of interest: None declared.
Disclaimer: The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health.
Key points
The ability to link longitudinal primary care, hospitalisation and mortality data offers a new opportunity to provide detailed quantification of the injury burden in England.
Patterns of injury by age, sex, socioeconomic status and calendar time vary by injury type.
Tailored injury prevention programmes should be developed across the life course based on the epidemiology described here.
Inequalities in injury occurrences support the targeting of preventative interventions to households in the most deprived areas.
References
- 1. Bauer R, Steiner M. Injuries in the European Union. Statistics Summary 2005-2007. Vienna: Euosafe. KfV, Austrian Road Safety Board, 2009. [Google Scholar]
- 2. Public Health England. Reducing Unintentional Injuries in and Around the Home Among Children Under Five Years. London: Public Health England, 2014. [PubMed] [Google Scholar]
- 3. Sethi D, Towner E, Vincenten J, et al. European report on child injury prevention. Copenhagen: World Health Organanisation, 2008. Available at http://www.who.int/violence_injury_prevention/child/injury/world_report/European_report.pdf. [Google Scholar]
- 4. MacKay M, Vincenten J. Action Planning for Child Safety. 2010 Update on the Strategic and Coordinated Approach to Reducing the Number One Cause of Death and Disability for Children in Europe—Injury. Amsterdam: European Child Safety Alliance. Eurosafe, 2010.
- 5. Baker R, Tata LJ, Kendrick D, Orton E. Identification of incident poisoning, fracture and burn events using linked primary care, secondary care and mortality data from England: Implications for research and surveillance. Inj Prev 2016;22:59–67. [DOI] [PubMed] [Google Scholar]
- 6. Herrett E, Gallagher AM, Bhaskaran K, et al. Data resource profile: Clinical practice research datalink (CPRD). Int J Epidemiol 2015;44:827–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Health and Social Care Information Centre. Attribution Data Set GP-Registered Populations 2010. 2012. Available at http://www.hscic.gov.uk/ (October 2015, date last accessed).
- 8. Crooks C. The epidemiology of upper gastrointestinal bleeding. Nottingham: University of Nottingham; 2013. [Google Scholar]
- 9. Department for Communities and Local Government. English Indices of Deprivation 2010. Guidance Document, 2011. [May 2014]. Available at: https://www.gov.uk/government/publications/english-indices-of-deprivation-2010-guidance (May 2014, date last accessed).
- 10. Office for National Statistics. 2011. Census, Population Estimates by Single Year of Age and Sex for Local Authorities in the United Kingdom, 2013. Available at: http://www.ons.gov.uk/ons/rel/census/2011-census (October 2015, date last accessed).
- 11. Public Health England. Public Health Outcomes Framework 2012. Available at: http://www.phoutcomes.info/. (October 2015, date last accessed).
- 12. Arora S, Charlesworth A, Kelly E, Stoye G. Institure for Fiscal Studies, Nuffield Trust. Understanding Competition and Choice in the NHS. Public Payment and Private Provision. The Changing Landscape of Health Care in the 2000s. London: Nuffield Trust, 2013. Available at http://www.nuffieldtrust.org.uk/sites/files/nuffield/publication/130522_public-payment-and-private-provision.pdf. [Google Scholar]
- 13. Lyons RA, Delahunty AM, Kraus D, et al. Children's fractures: a population based study. Inj Prev 1999;5:129–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Cooper C, Dennison EM, Leufkens HG, et al. Epidemiology of childhood fractures in Britain: a study using the general practice research database. J Bone Miner Res 2004;19:1976–81. [DOI] [PubMed] [Google Scholar]
- 15. Mayranpaa MK, Makitie O, Kallio PE. Decreasing incidence and changing pattern of childhood fractures: A population-based study. J Bone Miner Res 2010;25:2752–9. [DOI] [PubMed] [Google Scholar]
- 16. Agran PF, Anderson C, Winn D, et al. Rates of pediatric injuries by 3-month intervals for children 0 to 3 years of age. Pediatrics 2003;111:e683–92. [DOI] [PubMed] [Google Scholar]
- 17. Flavin MP, Dostaler SM, Simpson K, et al. Stages of development and injury patterns in the early years: A population-based analysis. BMC Public Health 2006;6:187.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Franklin RL, Rodgers GB. Unintentional child poisonings treated in United States hospital emergency departments: National estimates of incident cases, population-based poisoning rates, and product involvement. Pediatrics 2008;122:1244–51. [DOI] [PubMed] [Google Scholar]
- 19. Hawton K, Bergen H, Waters K, et al. Epidemiology and nature of self-harm in children and adolescents: Findings from the multicentre study of self-harm in England. Eur Child Adolesc Psychiatry 2012;21:369–77. [DOI] [PubMed] [Google Scholar]
- 20. Prescott K, Stratton R, Freyer A, et al. Detailed analyses of self-poisoning episodes presenting to a large regional teaching hospital in the UK. Br J Clin Pharmacol 2009;68:260–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Bateman DN, Bain M, Gorman D, Murphy D. Changes in paracetamol, antidepressants and opioid poisoning in Scotland during the 1990s. QJM 2003;96:125–32. [DOI] [PubMed] [Google Scholar]
- 22. Mbeledogu CN, Cecil EV, Millett C, Saxena S. Hospital admissions for unintentional poisoning in preschool children in England; 2000-2011. Arch Dis Child 2015;100:180–2. [DOI] [PubMed] [Google Scholar]
- 23. Groom L, Kendrick D, Coupland C, et al. Inequalities in hospital admission rates for unintentional poisoning in young children. Inj Prev 2006;12:166–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Hippisley-Cox J, Groom L, Kendrick D, et al. Cross sectional survey of socioeconomic variations in severity and mechanism of childhood injuries in Trent 1992-7. BMJ 2002;324:1132.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Brewster CT, Coyle B, Varma S. Trends in hospital admissions for burns in England, 1991-2010: A descriptive population-based study. Burns 2013;39:1526–34. [DOI] [PubMed] [Google Scholar]
- 26. Stark AD, Bennet GC, Stone DH, Chishti P. Association between childhood fractures and poverty: population based study. BMJ 2002;324:457.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Lyons RA, Delahunty AM, Heaven M, et al. Incidence of childhood fractures in affluent and deprived areas: population based study. BMJ 2000;320:149.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Orton E, Kendrick D, West J, Tata LJ. Persistence of health inequalities in childhood injury in the UK; A population-based cohort study of children under 5. PLoS One 2014;9:e111631.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. The Royal Society for the Prevention of Accidents. Safe At Home—The National Home Safety Equipment Scheme, 2014. Available at: http://www.rospa.com/home-safety/advice/child-safety/safe-at-home/. (July 2015, date last accessed).
- 30. Hedstrom EM, Svensson O, Bergstrom U, Michno P. Epidemiology of fractures in children and adolescents. Acta Orthop 2010;81:148–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Adams AL, Kessler JI, Deramerian K, et al. Associations between childhood obesity and upper and lower extremity injuries. Inj Prev 2013;19:191–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Kessler J, Koebnick C, Smith N, Adams A. Childhood obesity is associated with increased risk of most lower extremity fractures. Clin Orthop Relat Res 2013;471:1199–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Bhangal KK, Neen D, Dodds R. Incidence of trampoline related pediatric fractures in a large district general hospital in the United Kingdom: lessons to be learnt. Inj Prev 2006;12:133–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Fogarty AW, Liu C. Temporal trends in the associations between age, sex and socioeconomic status after death from motor vehicle collisions in England and Wales: 1960-2009. Emerg Med J 2015;32:203–6. [DOI] [PubMed] [Google Scholar]
- 35. Kosuge D, Barry M. Changing trends in the management of children's fractures. Bone Joint J 2015;97-B:442–8. [DOI] [PubMed] [Google Scholar]
- 36. Helenius I, Lamberg TS, Kaariainen S, Impinen A, et al. Operative treatment of fractures in children is increasing. A population-based study from Finland. J Bone Joint Surg Am 2009;91:2612–6. [DOI] [PubMed] [Google Scholar]
- 37. Hagell A, Coleman J, Brooks F. Key Data on Adolescence 2015. London: Association for Young People’s Health, 2015. Available at http://cdn.basw.co.uk/upload/basw_110253-1.pdf. [Google Scholar]
- 38. National Institute for Health and Care Excellence (NICE). Self-Harm: The Short-Term Physical and Psychological Management and Secondary Prevention of Self-Harm in Primary and Secondary Care. Clinical guideline 16: Manchester: NICE, 2004.
- 39. Towner E, Dowswell T, Mackereth C, Jarvis S. What works in preventing unintentional injuries in children and young adolescents: an updated systematic review. London: Health Development Agency, 2001. [Google Scholar]
- 40. Kendrick D, Young B, Mason-Jones AJ, et al. Home safety education and provision of safety equipment for injury prevention. Cochrane Database Syst Rev 2012;9:CD005014.. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.