Unnecessary health care at the end of life is a problem well recognized in many areas of medicine including the care of prostate cancer, breast cancer, and elective surgeries.1–3 Treatments and tests may be unnecessary or even inappropriate if they involve risks that outweigh potential benefits. For example, mammography is no longer recommended in women who have less than 10 years to live, given the known risks and limited benefits of screening.4 To target services to those who may benefit, many guidelines now recommend incorporating life expectancy into clinical decisions. 1,4,5 As dermatologists who care for patients with low-risk tumors, such as small (<1 cm) nodular and superficial basal cell carcinomas (BCCs), we need to think about this issue for our own specialty.
Some difficult questions we often face as clinicians include: Is this patient too frail to be referred for Mohs? How do I make that decisione—and what if I am wrong? What do I do when my medical recommendation does not match what the patient or family wants? Should cost ever be a consideration in treatment decision-making? How do I document this without getting sued?
Our goal in this piece is to discuss a challenge that dermatologists face daily, and propose a simple practical strategy for managing BCCs in patients with limited life expectancy.
THE PROBLEM
Some patients with limited life expectancy (eg, <1 year of life because of metastatic cancer) may not live long enough to benefit from treating asymptomatic low-risk BCCs. Most BCCs grow slowly, and some patients will die of unrelated causes before their BCCs cause symptoms. There is no doubt that many treatments for BCC are beneficial because they relieve symptoms, or remove a tumor that could cause significant problems. However, when these effective treatments are used for low-risk, asymptomatic skin lesions, the benefits are not immediate. Like treatments for hypertension and diabetes in older adults, these treatments have a time lag to benefit.6 In some patients with less than a year of life remaining, the short-term drawbacks of detection and treatment of low-risk BCCs may outweigh future benefits. In practice, patients seem to get the same types of treatment regardless of their life expectancy.7 Preliminary data from both national and single-center studies suggest similar treatments are rendered regardless of how we define life expectancy: patients who died within 1 or 2 years of biopsy; patients-with dementia; patients who cannot independently dress, feed, or bathe themselves; and patients with many medical comorbidities, all seem to receive the same treatments for BCC as healthier patients.
BALANCING HEALTH CARE QUALITY AND PATIENT AUTONOMY
Dermatologists, dermatologic surgeons, and primary care doctors share a common goal: to provide safe, effective, and responsible care for our patients. In particular, dermatologic surgeons are cutaneous oncologists, with specialized expertise on assessing and balancing the risks and benefits of treatment options for the millions of patients who have potentially harmful BCCs. Surgery may seem to be the best treatment for patients with BCC at the end of life because of convenience and efficacy. However, 1 study showed that over a quarter (27%) of patients reported a problem after skin cancer surgery of which physicians were not aware. These included medical complications like bleeding, infection, and wound dehiscence; as well as nonmedical concerns such as scar appearance, not being able to perform regular activities with bandages, and problems with insurance and follow-up appointments. This highlights the importance of explaining appropriate expectations for each treatment option and the need for ongoing communication between patient and provider. Moreover, physicians are only part of the health care decision equation. Increasingly, patients themselves—regardless of age—eexpress strong treatment preferences. We support this patient empowerment and believe that no patient should be denied an appropriate treatment for their BCC because of their age or health status and that patient preferences should be incorporated in decisions in the context of goals of care and patient prognosis. Balancing patient preferences against medical recommendations can be challenging, but hinges on communicating with patients about what is known and not known about risks, benefits, and likely prognoses.8
AGE AND ESTIMATING LIFE EXPECTANCY
Although life tables can estimate average life expectancy, we all care for healthy, active, independent 90 year olds who may live much longer. Age contributes to, but does not determine, life expectancy. Although neither a clinician nor an index can predict with absolute certainty how long a patient will live, validated prognostic indices (http://eprognosis.ucsf.edu/) can improve the accuracy and help guide individual clinical decisions.5 These online tools are accessible and user-friendly, and can be helpful during clinic visits to open the discussion with patients, and visually communicate both estimated life expectancy and the uncertainty of prediction.
LOW-RISK BCC
The National Comprehensive Cancer Network9 has defined high-risk BCCs based on location on the central aspect of the face or genital areas, size greater than 2 cm, ill-defined borders or aggressive histology, patient immunosuppression (especially organ transplant recipients), and tumors recurring or developing in previously irradiated sites. Conversely, low-risk BCCs can be defined as primary BCCs on the trunk or limbs, less than 1 cm in size, and in patients who are not organ transplant recipients or have had prior skin irradiation. Dermatologists have specialized skills and training to diagnose potential skin cancers clinically, and to identify and manage low-risk lesions that are likely BCCs, even before a biopsy is performed.
MANAGEMENT OF LIKELY LOW-RISK BCCs AT THE END OF LIFE
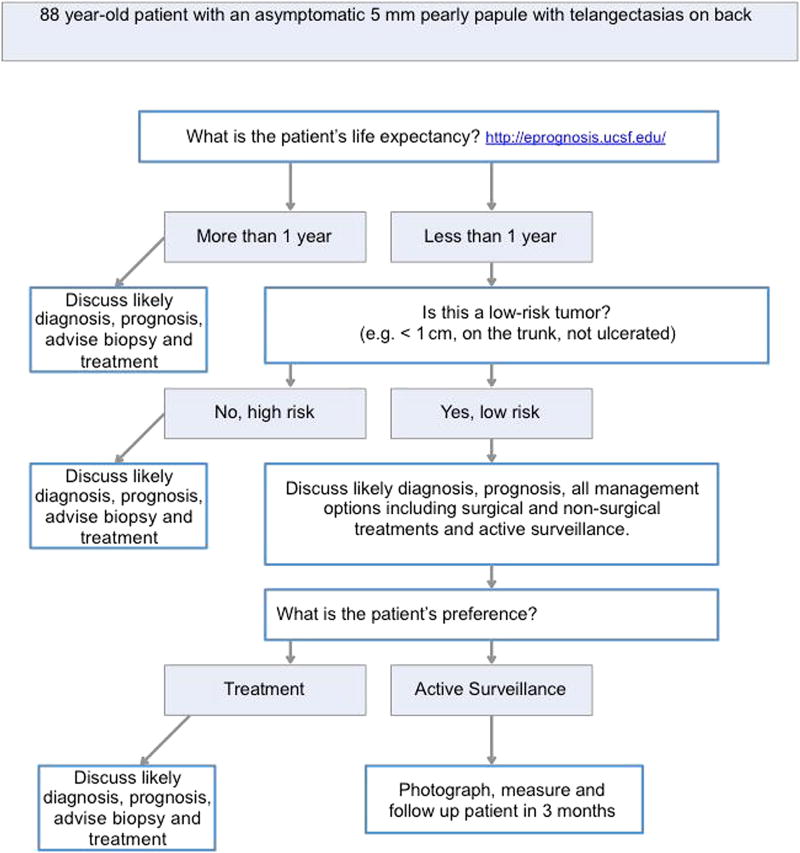
To help patients and their families make informed decisions about slow-growing skin lesions, we need more evidence on the natural history of untreated lesions, patient treatment preferences, and the risks and benefits of biopsy, referral, and treatment of potential BCCs. Accumulating this evidence will take time. Meanwhile, we present a framework (Fig 1) to guide clinicians faced with this common situation.
Fig. 1.
Framework.
For example, an 88-year-old man is referred to your office for a skin lesion on his back. He has metastatic lung cancer with recent weight loss and renal failure. He is unaware of this skin lesion. On examination, you see a 5-mm pearly papule with telangectasias that is likely a nodular BCC. With access to a user-friendly validated online tool to estimate the patient’s life expectancy (http://eprognosis.ucsf.edu/), you find that this patient has an average life expectancy of 1 year. You explain the likely diagnosis, prognosis, risks, and benefits of all management options, including doing a biopsy today to obtain histologic confirmation followed by surgical and nonsurgical treatments. In addition, you offer active surveillance (no biopsy or treatment today, but a photograph, measurement, and follow-up clinic visit in 3 months). You explain the risks of active surveillance, including not having histologic confirmation of the lesion, and the potential that the lesion would grow or become symptomatic in the future, leading to a bigger treatment and scar later. You clarify that the patient could change his mind at any point and come back sooner for a biopsy and treatment.
This suggested strategy is only the first step and based only on opinion because high-quality data are lacking. We hope that this suggested strategy will encourage discussion among our specialty about a common situation for which optimal decisions may not be obvious for patients who may have different preferences. We also hope our discussions will stimulate research that will ultimately lead to high-quality evidence-based guidelines for BCC management that incorporate patient prognosis.
Acknowledgments
This research was funded by the National Center for Advancing Translational Sciences, National Institutes of Health, through University of California San Francisco, Clinical and Translational Science Institute (UCSF-CTSI) grant number KL2TR000143; National Institute of Arthritis and Musculoskeletal and Skin Diseases K24; 5K24AR052667-09, the Dermatology Foundation Career Development Award; and the UCSF Claude D. Pepper Older Americans Independence Center P30AG044281.
Footnotes
Disclosure: Dr Mary-Margaret Chren serves as a consultant to Genentech Inc. Drs Linos and Berger have no conflicts of interest to declare.
References
- 1.Walter LC, Bertenthal D, Lindquist K, Konety BR. PSA screening among elderly men with limited life expectancies. JAMA. 2006;296(1):2336–2342. doi: 10.1001/jama.296.19.2336. [DOI] [PubMed] [Google Scholar]
- 2.Sima CS, Panageas KS, Schrag D. Cancer screening among patients with advanced cancer. JAMA. 2010;304(14):1584–1591. doi: 10.1001/jama.2010.1449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kwok AC, Semel ME, Lipsitz SR, et al. The intensity and variation of surgical care at the end of life: a retrospective cohort study. Lancet. 2011;378(9800):1408–1413. doi: 10.1016/S0140-6736(11)61268-3. [DOI] [PubMed] [Google Scholar]
- 4.Walter LC, Schonberg MA. Screening mammography in older women: a review. JAMA. 2014;311:1336–1347. doi: 10.1001/jama.2014.2834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yourman LC, Lee SJ, Schonberg MA, Widera EW, Smith AK. Prognostic indices for older adults: a systematic review. JAMA. 2012;307(2):182–192. doi: 10.1001/jama.2011.1966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lee SJ, Boscardin WJ, Stijacic-Cenzer I, Conell-Price J, O’Brien S, Walter LC. Time lag to benefit after screening for breast and colorectal cancer: meta-analysis of survival data from the United States, Sweden, United Kingdom, and Denmark. BMJ. 2013;346:e8441. doi: 10.1136/bmj.e8441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Linos E, Parvataneni R, Stuart SE, Boscardin WJ, Landefeld CS, Chren MM. Treatment of nonfatal conditions at the end of life: nonmelanoma skin cancer. JAMA Intern Med. 2013 Jun 10;173(11):1006–1012. doi: 10.1001/jamainternmed.2013.639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wenger NS. Skin cancer and shared decision making: comment on “treatment of nonfatal conditions at the end of life”. JAMA Intern Med. 2013;173(11):1012–1013. doi: 10.1001/jamainternmed.2013.6685. [DOI] [PubMed] [Google Scholar]
- 9.National Comprehensive Cancer Network (NCCN) Basal cell and squamous cell skin cancers. [Accessed April 28, 2015];National Comprehensive Cancer Network The complete library of NCCN Clinical Practice Guidelines in Oncology, version 2 2012 2012 May 18, 2010 [cited] Available from: http://www.nccn.org/professionals/physician_gls/f_guidelines.asp.