Abstract
Skilled birth attendant (SBA) utilization is low in remote and rural areas of Nepal. We designed and implemented an evaluation to assess the effectiveness of a five-component intervention that addressed previously identified barriers to SBA services in mid- and far-western Nepal. We randomly and equally allocated 36 village development committees with low SBA utilization among 1-year intervention and control groups. The eligible participants for the survey were women that had delivered a baby within the past 12 months preceding the survey. Implementation was administered by trained health volunteers, youth groups, mothers’ groups and health facility management committee members. Post-intervention, we used difference-in-differences and mixed-effects regression models to assess and analyse any increase in the utilization of skilled birth care and antenatal care (ANC) services. All analyses were done by intention to treat. Our trial registration number was ISRCTN78892490 (http://www.isrctn.com/ISRCTN78892490). Interviewees included 1746 and 2098 eligible women in the intervention and control groups, respectively. The 1-year intervention was effective in increasing the use of skilled birth care services (OR = 1.57; CI 1.19–2.08); however, the intervention had no effect on the utilization of ANC services. Expanding the intervention with modifications, e.g. mobilizing more active and stable community groups, ensuring adequate human resources and improving quality of services as well as longer or repeated interventions will help achieve greater effect in increasing the utilization of SBA.
Keywords: Cluster randomized controlled trial, maternal health, newborn health, skilled birth attendant, epidemiology, public health, intervention, evaluation, evidence-based policy, health services research, Nepal
Key Messages
Longer-term implementation of intervention activities yields a more visible increment of SBA service utilization.
Community mobilization efforts proved to be successful but required supervision and support to ensure the quality of implementation.
Improved service quality and adequate physical infrastructure of the health facilities encourage pregnant women to make the required number of ANC visits.
Remote areas require an expanded and modified intervention package, as geographic and transport barriers compound the difficulties in accessing care.
Background
Maternal deaths and disabilities are leading contributors to women’s burden of disease and maternal conditions are the second leading cause of death among women of reproductive age (Koblinsky et al. 2012). In 2015, the maternal mortality was 216 deaths per 100 000 live births which is 44% lower than in 1990 with 385 maternal deaths per 100 000 live births (WHO 2015). This global achievement is below the Millennium Development Goal (MDG) target of a 75% reduction of maternal deaths from the 1990 level (The Lancet 2016). Indeed, 303 000 women die every year worldwide due to complications of pregnancy and childbirth (WHO 2015). Almost all, i.e. 99.7% maternal deaths, occur in developing regions where the risk of pregnancy-related death is 20 times higher compared to developed regions (WHO 2015). The sub-Saharan Africa region accounts for 66.3% of global maternal deaths, followed by Southern Asia with 21.8% (WHO 2015). Furthermore, maternal mortality reveals wide gaps between rich and poor both between and within countries (WHO 2015).
Coverage gaps in maternal and newborn health care occur mostly in low-income countries and within countries populated by the most vulnerable, i.e. the poorest and least educated (Barros et al. 2012; Ruhago et al. 2012). Skilled birth care and antenatal care (ANC) are two important components of the services provided by skilled birth attendants (SBAs). In mid- and far-western Nepal, the main barriers to SBA service utilization include distance and inadequate transport to a health facility, inadequate awareness of the importance of skilled birth care, women’s lack of knowledge of pregnancy danger signs, poor economic status of the family, fewer than four ANC visits and SBA security (Choulagai et al. 2013; Onta et al. 2014).
The MDGs targeted the reduction of maternal mortality by three-fourth of the 1990 level, and use of SBA services as a means to achieve such reduction (United Nations 2011). Although Nepal’s maternal mortality ratio (MMR) decreased from 901 maternal deaths per 100 000 live births in 1990 to 258 in 2015 (WHO 2015), the Sustainable Development Goals (SDG) adopted by the United Nations General Assembly on 25 September 2015 established new targets for Nepal, i.e. MMR 70 per 100 000 live births and 90% SBA-assisted births (National Planning Commission 2015; Wikipedia 2016). Achieving those targets and reducing barriers to SBA service utilization will require further effort.
For women with no evidence of pregnancy-related complications, the 2016 WHO ANC model recommends a minimum of eight ANC contacts. The first contact is scheduled to take place up to 12 weeks of gestation in the first trimester, two contacts in the second trimester (weeks 20 and 26) and five contacts in the third trimester (weeks 30, 34, 36, 38 and 40) (WHO 2016). During ANC visits, SBAs inform women about the advantages of SBA-assisted childbirth and also about the danger signs of pregnancy, thus enabling them to recognize early symptoms and seek medical attention.
To increase SBA utilization, the government introduced a National Policy on SBAs in 2006 (Family Health Division 2006) under the broader framework of the Safe Motherhood Policy, 1998 (Family Health Division 1998). The SBA policy aims to reduce maternal and newborn morbidity and mortality by ensuring availability, access and utilization of SBA services. To minimize financial barriers to SBA service utilization, the government also introduced a Maternity Incentive Scheme (Ministry of Health and Population 2005), later named the Safe Delivery Incentive Program. In this scheme, women in the mountain, hill, and Terai regions receive a transportation incentive of Nepalese Rupees (NRP) 1500, 1000 and 500 (1 US$= NRP 107 in Mar 2017), respectively, for each birth conducted at a health facility and an additional NRP 400 to each woman who completes four ANC visits. These health care policies and programs helped increase SBA utilization from 10.1% in 1996 (New Era 1996) to 36% in 2011 (New Era 2012).
Despite an incremental increase in skilled birth care (36% in 2011 vs 10.1% in 1996) (New Era 1996, 2012), progress across the administrative regions of Nepal remains unequal. In 2011, SBA utilization in mid- and far-western Nepal was 28.7 and 30.7%, respectively (New Era 2012), lower than the eastern, central and western regions. Rural-urban variation in SBA utilization is also high (27.9 and 66.7% SBA-assisted deliveries in rural and urban areas, respectively) (New Era 2012). Our recent study in the semi-urban Health and Demographic Surveillance Site covering Jhaukhel and Duwakot determined that SBAs assisted in 93.1% of all deliveries, which is higher compared with rural areas (Choulagai et al. 2015).
This study aimed to develop an intervention that considered barriers to SBA service utilization previously identified in our baseline survey including quantitative and qualitative studies (Choulagai et al. 2013; Onta et al. 2014). We designed our intervention as a cluster randomized controlled trial and also tested its effectiveness in increasing SBA service utilization in mid- and far-western Nepal.
Methods
Study site and population
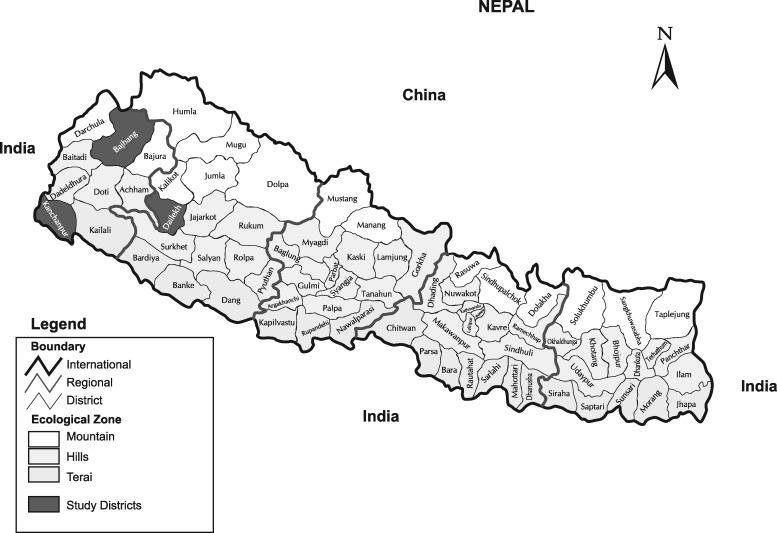
We selected three districts—Bajhang, Dailekh and Kanchanpur—from mid- and far- western regions (Figure 1), whose SBA utilization is lower than the eastern, central and mid-western regions of Nepal (New Era 2012). The districts were purposely selected to represent the three ecological zones (i.e. mountain, hill and Terai). Compared with the national average, all three districts have lower levels of education as well as health and economic development. We previously described the study site (Choulagai et al. 2013; Onta et al. 2014). Study participants were women who gave birth to a live baby within the 12 months immediately preceding the survey.
Figure 1.
Map of Nepal showing the study districts Bajhang, Dailekh and Kanchanpur in the mid- and far- western Nepal.
Study design and sampling
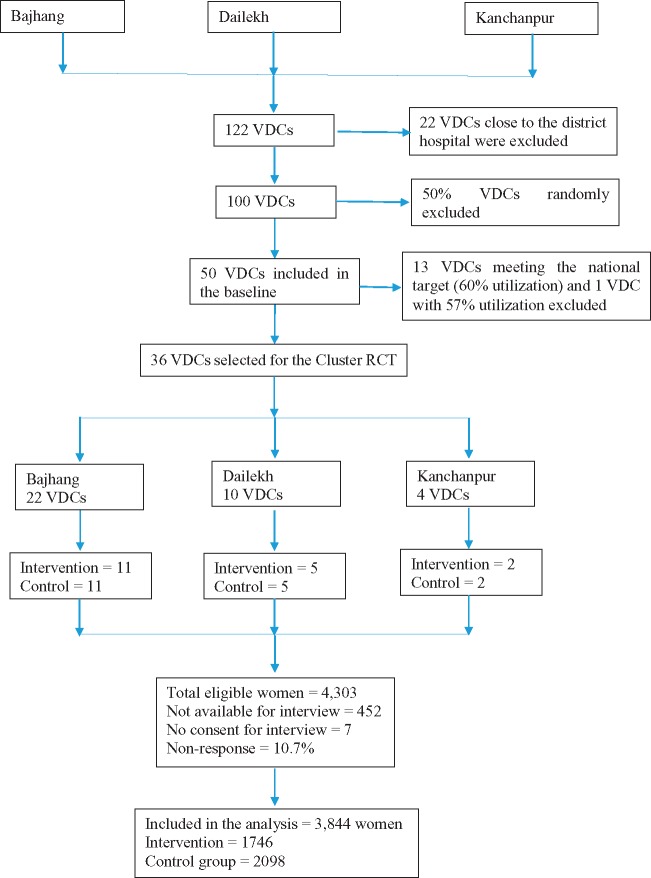
We designed this study as a cluster randomized controlled trial and used village development committees (VDCs) as the unit of randomization (Figure 2). VDCs, which are further divided into nine smaller units (i.e. wards), are the basic politicoadministrative units in each district. Together, Bajhang, Dailekh and Kanchanpur have 122 VDCs (48, 55 and 19, respectively). With an estimated 110 births per year per VDC and a 32% proportion of SBA-assisted births, we calculated sample size by assuming unmatched clusters of approximately equal size (Bhandari et al. 2014). We estimated the value of k—the between-cluster coefficient of variation—to be equal in the intervention and control groups. The value of k (0.25) was based on estimates of SBA utilization rate in the baseline survey and on experience drawn from previous field trials (Hayes and Bennett 1999).
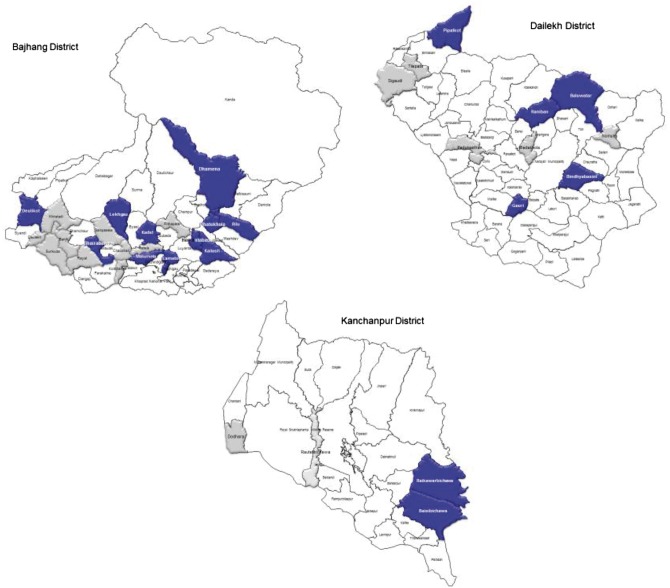
Figure 2.
Maps showing control and intervention VDCs. Note: In each of the three districts, blue-colored VDCs are intervention VDCS whereas grey-colored VDCs are control VDCs
Employing the average proportion of outcome (32%) in control group clusters, we calculated that we would need 36 clusters (110 eligible women per cluster) to detect a 10% difference in SBA utilization rate with an 80% power and 5% significance level.
Using the government’s MDG target for SBA-assisted births (60%), we randomized clusters from 36 of the 50 VDCs that participated in the baseline survey (Choulagai et al. 2013), excluding 13 VDCs that exceeded 60%. To achieve even distribution (18 VDCs each) in the intervention and control groups, we also excluded one VDC with 57% SBA utilization. Finally, our study from the Bajhang, Dailekh and Kanchanpur districts included 22, 10 and 4 VDCs, respectively (Figure 3). Prior to randomization, we discussed the intervention and selection process with stakeholders in each district. The random selection included public lottery of the study VDCs in the presence of district level stakeholders.
Figure 3.
Trial profile for measuring the utilization of skilled birth attendants‘ service. Note: VDC, Village Development Committee; RCT, Randomized Controlled Trial
Intervention
Based on barriers identified in our baseline survey (Choulagai et al. 2013; Onta et al. 2014) and following discussion with international, national and district-level stakeholders, we developed a five-component intervention to increase SBA service utilization. Project staff met with local actors including female community health volunteers (FCHVs), mothers’ groups, health facility operation and management committees (HFOMCs) and youth groups to reach a consensus on the feasibility and scalability of the components and the role of different actors. The five components included:
Increased family support to pregnant women for childbirth in a health facility. Local and locally trained FCHVs and mothers’ groups held regular meetings and discussions about promoting family support for pregnant women for seeking childbirth in a health facility. FCHVs also discussed the importance of skilled birth care during home visits and mothers’ group meetings in their respective VDCs. Further, the FCHVs encouraged mothers’ group members to invite their family to regularly attend meetings that discussed the importance of SBA assistance and to support pregnant women in reaching a health facility. Mothers’ groups also informed families about emergency funds and transport arrangements (described below).
Financial assistance for women and families who seek SBA-assisted childbirth. This component mobilized existing funds to help pregnant women reach health facilities for childbirth. In Nepal, most mothers’ groups have funds to help pay for members’ needs. We held discussions with HFOMC, FCHVs, and mothers’ groups to arrange financial support to women for covering the cost of transport. The mothers’ groups agreed to grant interest-free loans to pregnant woman to enable them to reach health facility for childbirth. The women paid back their loan to the mothers’ group after receiving transport incentive from respective health facility. Our project donated NRP 2200 to each mothers’ group in the intervention VDCs.
Transport to a health facility for childbirth. Youth groups received a 1-day orientation on the intervention component and their role in it. The youth groups prepared a list of potential contacts who agreed to transport pregnant women. If vehicles were unavailable, youths would arrange porters or transport the woman themselves to the nearest available vehicle. Our project donated NRP 2000 for each group in the intervention VDCs.
Women-friendly environment at health facilities. In the intervention VDCs, all health facility staff participated in a 2-day training on communication skills, focusing on developing friendly behaviour and a supportive attitude towards women and their families.
SBA security. Consultations with HFOMC, mothers’ groups, and youth groups helped improve SBA security. SBAs were accompanied to nighttime births by a youth group member, FCHVs, or family member.
Implementation of intervention
To develop a work and human resource mobilization plan as well as training manuals, we recruited a research coordinator in each of the three study districts and a research assistant in each intervention VDC during November 2012–April 2013. Monthly reports of service utilization and implementation progress were discussed with the health facility staff and local HFOMCs and also with the focal person from the district health office. Including training and orientation activities, the intervention was implemented during May 2013–April 2014.
Data collection and field supervision
To assess the effectiveness of the intervention, 40 enumerators and 4 supervisors attended a 4-day training and collected data using specially designed field manuals. We conducted a post-intervention survey to compare our results with the baseline findings and determine the effectiveness of the intervention.
We divided the enumerators in two groups (20 per group). Due to difficult topography and extended travel time in the mountainous Bajhang district, enumerators and two supervisors collected data there. Group 2, which included enumerators and two supervisors, covered Dailekh and Kanchanpur. Two authors (BPC and NS) supervised field data collection and met with the enumerators and supervisors.
Data were collected during May–June 2014 using a structured questionnaire to interview all women in the study VDCs who had delivered a baby the 12 months immediately preceding the survey. The enumerators visited each household of the study VDCs to identify eligible women. The questionnaire covered socioeconomic information, utilization of maternal and newborn health services and women’s knowledge of the danger signs of pregnancy and delivery. Women were considered as having knowledge of danger signs if they could state at least one of the danger signs among premature labour, prolonged labour, breech delivery, cord prolapse, postpartum haemorrhage, maternal injuries, severe headache, convulsion, high fever, foul-smelling discharge and no movement of the baby in the womb. Post-intervention data collection employed the same procedures used in the baseline survey (Choulagai et al. 2013). Among 4303 identified eligible mothers, 3844 participated which resulted in a response rate of 89.3%. Seven eligible women were not interviewed because they did not provide consent.
Data analysis
The primary outcome variable was skilled birth care utilization and the secondary outcome variable was ANC utilization. The background variables were age, education, ethnicity and occupation.
Our primary analysis focused on post-intervention changes in skilled birth care utilization and ANC services. Changes were estimated using Difference-in-differences (DiD) model. DID estimates were derived from a linear regression model with a repeated data set on the use of skilled birth care and ANC between control and intervention groups at baseline and post-intervention, expressed as:
where y is the binary outcome of interest (1 = at least one ANC visit, four or more visits, or skilled birth care utilization; 0 = other); Dp°st is the time dummy; DTr is the intervention group dummy; DpostDTr is the time and intervention interaction; β3 is the estimate of DiD; x is the vector of control variables; and ε is the error term. We included background variables (education, occupation, ethnicity, age of mother) in the model. Using a binary variable in an additive linear regression model gave us probabilities that were easy to interpret. Due to our large sample size, we could apply the central limit theorem to the model.
DiD methods are relevant when using research designs based on controlling for confounding variables and when pre-treatment information is available (Lechner 2010). This approach involves recognizing the intervention and evaluates the differences in results before and after the interventions for treated and untreated groups. We analysed the DiD to evaluate results between control and intervention groups at baseline and post-intervention (Khandker et al. 2010).
Further, we performed mixed-effects logistic regression to determine the factors associated with the utilization of SBA services. VDCs functioned as a random intercept. We included background variables (education, occupation, ethnicity, age of mother), intervention time and group in the mixed-effects logistic regression model. Data were analysed in R software and statistical significance was set at P ≤ 0.05.
Ethical considerations
The authors obtained ethical approval from their institute. Our trial was registered in the International Standard Randomized Controlled Trial Number (ISRCTN) Registry with the registration number ISRCTN78892490 (http://www.isrctn.com/ISRCTN78892490).
Results
We previously described the baseline survey findings (Choulagai et al. 2013). The post-intervention survey included 3844 women. Although we had equal number of VDCs with 18 each that were randomly allocated to intervention and control, the actual number of women we surveyed were different with 2098 (54.6%) women in the control area and 1746 (45.4%) women in the intervention area.
Sociodemographic characteristics
Nearly three-fourths (73.8%) of participants were 20–35 years of age (Table 1) (median age = 24 years). The main ethnic groups included Brahmin/Chhetri (63.5%), Dalit (lower caste, 25.2%) and Janajati (indigenous group, 10.9%). Two in every 10 of the women were illiterate, whereas 8.4% had higher secondary education or above (Table 1). Agriculture was the major primary occupation (60.4%). Median age at marriage and first childbirth was 17and 19 years, respectively.
Table 1.
Socio-demographic characteristics of women participating in the post-intervention survey of control and intervention VDCs (N = 3844)
| Variables | Intervention |
Control |
Total |
|||
|---|---|---|---|---|---|---|
| N | % | N | % | N | % | |
| Age groups (years) | ||||||
| <20 | 396 | 22.7 | 501 | 23.9 | 897 | 23.3 |
| 20–35 | 1313 | 75.2 | 1524 | 72.6 | 2837 | 73.8 |
| >35 | 37 | 2.1 | 73 | 3.5 | 110 | 2.9 |
| Ethnicity | ||||||
| Brahmin/Chhetri | 1035 | 59.3 | 1405 | 67.0 | 2440 | 63.5 |
| Dalit | 388 | 22.2 | 581 | 27.6 | 969 | 25.2 |
| Janajati | 316 | 18.1 | 102 | 4.9 | 418 | 10.9 |
| Others | 7 | 0.4 | 10 | 0.5 | 17 | 0.4 |
| Education | ||||||
| Illiteratea | 268 | 15.3 | 510 | 24.3 | 778 | 20.2 |
| Informalb | 627 | 35.9 | 637 | 30.4 | 1264 | 32.9 |
| Primaryc | 333 | 19.2 | 290 | 13.8 | 623 | 16.2 |
| Secondaryd | 390 | 22.3 | 467 | 22.3 | 857 | 22.3 |
| Higher secondary and abovee | 128 | 7.3 | 194 | 9.2 | 322 | 8.4 |
| Occupation | ||||||
| Agriculture | 1033 | 59.2 | 1288 | 61.4 | 2321 | 60.4 |
| Housewife | 645 | 36.8 | 713 | 34.0 | 1358 | 35.3 |
| Service | 31 | 1.8 | 40 | 1.9 | 71 | 1.9 |
| Business | 22 | 1.3 | 32 | 1.5 | 54 | 1.4 |
| Wage labourer | 10 | 0.6 | 10 | 0.5 | 20 | 0.5 |
| Others | 5 | 0.3 | 15 | 0.7 | 20 | 0.5 |
Note: Results are shown for 3844 women who gave birth within the 12 months immediately preceding the post-intervention survey.
Unable to read and write.
Learning not connected to formal school.
Grades 1–5.
Grades 6–10.
Grades 11 and above.
Utilization of SBA services
Most of the participants, i.e. 90.8% completed at least one ANC visit and 65% completed four or more visits (Table 2). Majority (56.7%) used skilled birth care and 51% knew at least one danger sign of pregnancy and delivery. More than three-fourths (76.5%) had to walk more than half an hour to reach the nearest health facility.
Table 2.
Utilization of SBA services by women participating in the post-intervention survey of control and intervention VDCs (N = 3844)
| Variables | Intervention |
Control |
Total |
|||
|---|---|---|---|---|---|---|
| N | % | N | % | N | % | |
| Utilization of skilled birth care | ||||||
| No | 760 | 43.5 | 903 | 43.0 | 1663 | 43.3 |
| Yes | 986 | 56.5 | 1195 | 57.0 | 2181 | 56.7 |
| Frequency of ANC visit | ||||||
| <4 | 681 | 39.1 | 663 | 31.6 | 1344 | 35.0 |
| ≥4 | 1065 | 60.9 | 1435 | 68.4 | 2500 | 65.0 |
| Distance to health facility | ||||||
| ≤30 min | 405 | 23.2 | 500 | 23.8 | 905 | 23.5 |
| >30 min | 1341 | 76.8 | 1598 | 76.2 | 2939 | 76.5 |
| Knowledge of danger signs | ||||||
| No | 800 | 45.8 | 1084 | 51.7 | 1884 | 49.0 |
| Yes | 946 | 54.2 | 1014 | 48.3 | 1960 | 51.0 |
Note: Results are shown for 3844 women who gave birth within 12 months prior to the post-intervention survey. ANC, antenatal care; VDC, Village Development Committee.
Table 3 shows the results of DiD analysis of the intervention’s effectiveness regarding skilled birth care and ANC visits. At baseline, both the skilled birth care and ANC utilization were higher in controls compared with the intervention group. Post-intervention, the rate of one or more ANC visits, increased significantly (4%). The proportion of SBA-assisted births increased in the intervention group by 5%, and four or more ANC visits decreased by 3.1%; however, both the changes were statistically insignificant.
Table 3.
Effect of intervention in increasing the use of ANC and skilled birth care services in mid- and far-western Nepal
| Baseline |
Post-intervention |
Pre difference | Post difference | Impact |
||||
|---|---|---|---|---|---|---|---|---|
| Intervention | Control | Intervention | Control | Difference in Difference | P-value | |||
| Skilled birth care (%) | 30.4 | 35.9 | 56.5 | 57.0 | −5.5 | −0.5 | 5.0 | 0.06 |
| At least one ANC (%) | 83.4 | 84.4 | 92.4 | 89.4 | −1.0 | 3.0 | 4.0 | 0.03 |
| Four or more ANC (%) | 46.4 | 50.8 | 60.9 | 68.4 | −4.4 | −7.5 | −3.1 | 0.30 |
| Mean ANC (N) | 2.8 | 3.0 | 3.3 | 3.3 | −0.2 | 0.0 | 0.2 | 0.23 |
Note: Results are shown for effect of intervention using DiD estimates from a linear regression model. ANC, antenatal care.
Table 4 shows the outcome of the mixed-effects model. As per the adjusted analysis, post-intervention women were 1.57 times more likely to use skilled birth care (95% CI 1.19–2.08) than women in the control group. There was no effect of intervention in the use of ANC services. Women in the age Group 20–35 years were 0.81 times less likely to use skilled birth care (P < 0.001) compared with women aged below 20 years. Increasing level of education associated with increased use of skilled birth care and ANC visits. Occupation and ethnicity were not associated with the use of ANC visits or use of skilled birth care. Use of skilled birth care and ANC visits increased significantly in the post-intervention survey compared with the baseline survey. During the post-intervention, the control groups were 0.54 times less likely to use skilled birth care compared with the intervention group (Table 4).
Table 4.
Effect of intervention on utilization of ANC and skilled birth care in mid- and far-western Nepal
| Parameter | Skilled birth care |
At least one ANC |
Four or more ANC |
||||||
|---|---|---|---|---|---|---|---|---|---|
| aOR | CI | P | aOR | CI | P | aOR | CI | P | |
| Age in years | |||||||||
| <20 | Ref | – | – | – | – | – | – | – | – |
| 20–35 | 0.81 | 0.70, 0.94 | <0.001 | 0.78 | 0.61, 1.01 | 0.06 | 1.06 | 0.92, 1.23 | 0.41 |
| >35 | 0.73 | 0.51, 1.06 | 0.09 | 0.49 | 0.31, 0.57 | <0.01 | 0.65 | 0.46, 0.92 | 0.02 |
| Education | |||||||||
| Illiterate | Ref | – | – | – | – | – | – | – | – |
| Non-formal education | 1.06 | 0.90, 1.26 | 0.47 | 1.27 | 1.04, 1.56 | 0.02 | 1.39 | 1.19, 1.62 | <0.001 |
| Primary level | 1.70 | 1.37, 2.10 | <0.001 | 2.95 | 2.06, 4.23 | <0.001 | 1.92 | 1.56, 2.36 | <0.001 |
| Secondary level\ | 2.02 | 1.63, 2.50 | <0.001 | 4.76 | 3.17, 7.16 | <0.001 | 2.56 | 2.08, 3.14 | <0.001 |
| Higher secondary and above | 3.90 | 2.88, 5.28 | <0.001 | 10.40 | 4.71, 22.96 | <0.001 | 4.86 | 3.54, 6.67 | <0.001 |
| Occupation | |||||||||
| Agriculture | Ref | – | – | – | – | – | – | – | – |
| Service | 1.36 | 0.82, 2.27 | 0.23 | 1.05 | 0.29, 3.78 | 0.94 | 1.16 | 0.67, 1.98 | 0.60 |
| Business | 1.55 | 0.89, 2.68 | 0.12 | 1.82 | 0.54, 6.14 | 0.33 | 1.08 | 0.63, 1.86 | 0.78 |
| Wage labour | 0.69 | 0.36, 1.34 | 0.27 | 0.62 | 0.24, 1.57 | 0.31 | 0.81 | 0.43, 1.53 | 0.52 |
| House wife | 1.19 | 1.01, 1.41 | 0.03 | 0.98 | 0.76, 1.27 | 0.89 | 0.92 | 0.79, 1.08 | 0.32 |
| Others | 0.65 | 0.33, 1.29 | 0.22 | 0.78 | 0.28, 2.14 | 0.63 | 0.68 | 0.36, 1.29 | 0.24 |
| Ethnicity | |||||||||
| Brahman/Chhetri | Ref | – | – | – | – | – | – | – | – |
| Janajati | 1.19 | 0.93, 1.53 | 0.17 | 1.86 | 1.11, 3.11 | 0.02 | 1.06 | 0.83, 1.34 | 0.63 |
| Dalit | 1.16 | 1.00, 1.35 | 0.05 | 1.26 | 1.02, 1.57 | 0.03 | 1.07 | 0.93, 1.23 | 0.36 |
| Others | 1.17 | 0.74, 1.85 | 0.49 | 0.75 | 0.39, 1.44 | 0.39 | 1.28 | 0.82, 2.01 | 0.28 |
| Intervention time (baseline vs post-intervention) | 2.12 | 1.76,2.56 | <0.001 | 1.36 | 1.05,1.74 | 0.02 | 1.95 | 1.63,2.33 | <0.001 |
| Intervention group (intervention vs control) | 0.54 | 0.29, 0.99 | 0.05 | 0.81 | 0.51,1.30 | 0.40 | 0.77 | 0.52,1.13 | 0.18 |
| Effects of intervention on SBA service utilization | |||||||||
| Post-intervention | 1.57 | 1.19, 2.08 | <0.001 | 1.42 | 0.98,2.06 | 0.06 | 0.86 | 0.67,1.10 | 0.23 |
| Coefficient of variation | 0.390 | 0.423 | 0.209 | ||||||
Note: Results are shown for effects of intervention to increase service utilization using mixed-effects model. The results are adjusted for age, education, occupation, ethnicity, intervention time and intervention group. ANC: antenatal care, aOR: adjusted odds ratio, CI: confidence interval, SBA: skilled birth attendant, Ref: Reference.
Discussion
Our study examined whether intervention increases women’s utilization of two important components of SBA services—skilled birth care and ANC. The utilization of SBA services increased in both the intervention and control areas of our study. In the intervention area, the utilization of skilled birth care and at least one ANC visit increased from 30.4 and 83.4% at baseline to 56.5 and 92.4% post-intervention, respectively. Similarly, in the control area, the utilization of skilled birth care and at least one ANC visit increased from 35.9 and 84.4% at baseline to 57.0 and 89.4% at post-intervention. At the national level the use of skilled birth care increased from 9 in 1996 to 36% in 2011 (New Era 1996, 2012). Such increment could be attributed to Nepal Government’s policies and programs that include Safe Motherhood Policy (Family Health Division 1998), Maternity Incentive Scheme (Ministry of Health and Population 2005), National Policy on SBAs (Family Health Division 2006) and National Free Delivery Policy (Ministry of Health and Population 2010).
We used DiD to measure the effect of the intervention and analysed associated factors with regression analyses. Although both intervention and control areas showed increased levels of skilled birth care, the increases were incremental in the intervention area (5 and 4%, respectively). In DiD analysis, the increase in at least one ANC visit was significant but the changes in use of four or more ANC visits and skilled birth care were not. The mixed-effects logistic regression analysis, using VDCs as random intercepts, showed that our intervention was positively associated with increased use of skilled birth care (OR = 1.57; 95% CI 1.19–2.08).
The incremental increase in initial ANC visits might result from awareness-raising activities in FCHV-facilitated mothers’ group meetings. Further, the absence of incremental increases in four or more ANC visits could relate to distance from a health facility, poor road conditions and limited means of transport (Choulagai et al. 2013; Karkee et al. 2013; Onta et al. 2014). Another study in Nepal reported that women are more likely to attend four or more ANC visits when the availability of medical equipment, rooms, and skilled providers is adequate (Karkee et al. 2014). Conversely, the inadequate number of ANC visits may result from women’s perception that ANC services were not useful to them or of low quality. In the context of recently revised guidelines by the WHO on ANC for a positive pregnancy experience (WHO 2016), more efforts are required in Nepal for achieving the recommended eight ANC contacts.
The baseline survey revealed key barriers, including distance to a health facility, inadequate transport, lower educational level, low economic status, and inadequate knowledge about the danger signs of pregnancy and childbirth (Choulagai et al. 2013). Perceived barriers included insufficient awareness of the importance of SBAs, families’ inability to predict delivery date, delayed payment of transport incentives, inadequate human resources in peripheral health facilities, quality of service and SBA security issues, especially at night (Onta et al. 2014). Other studies conducted in Nepal, Bangladesh and Afghanistan report similar barriers (Edmonds et al. 2012; Mayhew et al. 2008; Shrestha et al. 2012).
Aiming to ensure the feasibility of expanding successful interventions and thus increasing SBA utilization into other areas, we consulted with stakeholders (e.g. the Ministry of Health and Population and District Health Office) in national and district level workshops before selecting the five intervention components. The intervention focused on utilizing the existing health infrastructure and community structures—HFOMC, mothers’ groups and youth groups—rather than establishing new structures or initiating additional programs. Moreover, the intervention aimed to address pre-identified barriers: lack of family support for helping pregnant women reach a childbirth facility, inability to pay for transport costs to reach health facility to avail SBA services, unavailability of transport to a childbirth facility, lack of a women-friendly environment in health facilities and issues related to SBA security. Attaining SDG targets will require the expansion of health interventions.
Cluster RCT is an appropriate design for community-based interventions (Bhandari et al. 2003; Manandhar et al. 2004; Penny et al. 2005; Aboud and Akhter 2011). Indeed, Cluster RCT is considered the strongest design in health research when allocation of identifiable groups is necessary (Murray et al. 2004). According to the ‘CONSORT 2010 statements: extension to cluster randomized trials’ Cluster RCTs are preferable when there is threat of unintentional spill-over of intervention effects from one treatment group to another (contamination) (Campbell et al. 2012). Our use of a community-based intervention and health facility staff made Cluster RCT feasible and appropriate to prevent such contamination.
We faced some challenges during the implementation of the intervention components. Regarding increasing family support for giving birth at a health facility (component 1), FCHV-facilitated mothers’ group meetings were delayed during the harvesting season and major festivals. Regarding the financial assistance from the mothers’ group fund (component 2), our monitoring records show variable use with 20% of women utilizing such assistance in Dailekh district and 6% each in Bajhang and Kanchanpur districts.
Youth group mobilization (component 3) was also a challenge—the importance of youth participation did not meet our expectations. Instead, neighbourhood women provided transport in two-thirds of all cases in the hill and mountain districts. In Kanchanpur, a Terai district, youths helped transport only about one out of six pregnant women. Youths’ frequent mobility mainly for employment and education interfered with their contribution. Although no security issues arose during the study period (component 5), some SBAs favoured the idea of better accommodations close to the health facility.
Strengths and limitations
The strength of this five-component intervention was its rootedness in an extensive baseline survey that involved both quantitative and qualitative approaches. For scalability and sustainability of the intervention, we ensured that the components added few financial and structural demands on the existing health system. Another strength of this trial is the randomized allocation of adequate number of clusters into intervention and control groups.
Limitations included simultaneous implementation of all five components during the 1-year intervention period, thus precluding an effectiveness assessment of individual components. Although the baseline survey identified distance to the health facility and inadequate transport as important barriers, the intervention could not address distance barrier. However, transport arrangements developed during the intervention optimally utilized pre-existing transport and mobilized community groups to bring pregnant women to the health facility. Moreover, although identified barriers included several supply-side factors (e.g. insufficient human resources, inadequate capacity and motivation of health workers, inadequate infrastructure and supply logistics at health facilities and issues related to the quality of services provided), the components of our study mostly addressed demand-side issue. Although our intervention included components on promoting a women-friendly environment at health facilities and improving security issues of the SBAs, it did not address other supply-side aspects.
Conclusions
Our 1-year intervention was effective in increasing the use of skilled birth care services; however, the intervention had no effect on the utilization of ANC services. Expanding the intervention with some modifications, e.g. mobilizing more active and stable community groups, adding service-side interventions to address issues related to human resources and quality of services as well as longer or repeated interventions will help achieve greater effect in increasing the utilization of SBA.
Lessons learned
Youth group mobilization was less effective than expected in overcoming barriers related to transport arrangement and SBA security. Regular participation by pregnant women in mothers’ group meetings is crucial to effective intervention. Poor families could not afford transport because the government’s incentive was not always enough to cover the cost. Many barriers to SBA services relate to both supply- and demand-side supports, better road and improved transport services. Retention of SBAs would help enhance service utilization. Because outcome includes components of behaviour change, a longer intervention, or repeated interventions, could yield greater impact.
Acknowledgments
The research team thanks the women who participated in the trial, mothers’ group and youth group members, and the Health Facility Operation and Management Committee from the study districts. We acknowledge District Development Committees and District Health Offices of the respective districts for their cooperation in this trial. Nepal’s Ministry of Health and Population is acknowledged for its cooperation throughout the study period. We acknowledge staffs from the World Health Organization, Geneva, particularly Ms Anayda Portela and Dr Rajiv Bahl for their technical inputs and support at various stages of the research project. We are thankful to the members and staff of Nepal Public Health Foundation for their untiring efforts to meet project demands at every stage. The help of field staff, data enumerators, and supervisors was crucial in conducting the intervention and the surveys. The authors thank scientific editor Karen Williams (Kwills Editing Services, Weymouth, MA, USA) for providing professional English-language editing of this article.
Conflict of interest statement. None declared.
Funding
This study was funded by the Alliance for Health Policy and Systems Research, WHO, Geneva, with support from the Norwegian Government Agency for Development Cooperation (Norad), the Swedish International Development Cooperation Agency (Sida), and the UK Department for International Development (DFID). Technical coordination and support was provided by the Department of Maternal Newborn Child and Adolescent Health, WHO, Geneva. The funder had no role in conducting the surveys, implementing the intervention, or analysis and interpretation of the data. The corresponding author had access to all study data and had final responsibility for the decision to submit for publication.
Ethical approval
We conducted the intervention at the community and health systems level and involved health facility management committees, mothers groups, and FCHVs, focusing on strengthening capacity by reinforcing expanding the scope of the health system’s ongoing activities. The intervention was noninvasive, thus no health risks were anticipated for the women.
Health volunteers, health providers and women and youth groups were informed about the objectives of the study, the implementation package and the evaluation process. Before randomizing VDCs, we met with stakeholders in all study VDCs to share the research objectives, approaches, and duration of the intervention. Our intervention aimed to benefit the most vulnerable (women and newborn) and within that group, those with most difficult access to the health facilities. Because the selection of intervention VDCs might involve selection bias, all intervention and control VDCs were randomly chosen. The Government of Nepal committed to extending the intervention to the control clusters if the intervention was effective.
Before seeking written informed consent, enumerators explained study, its objectives, and the extent of participant involvement to everyone included in the survey. Enumerators conducted the interview with due respect to respondents’ privacy and maintained confidentiality of all information. For illiterate women, a witness read the informed consent form aloud and consenting participants applied their thumbprint on the consent form. The witness also signed the consent form.
The authors obtained ethical approval from Nepal Health Research Council and the World Health Organization in Geneva, Switzerland. The trial was registered in the International Standard Randomized Controlled Trial Registry as ISRCTN78892490.
References
- Aboud FE, Akhter S.. 2011. A cluster-randomized evaluation of a responsive stimulation and feeding intervention in Bangladesh. Pediatrics 127: e1191–7. [DOI] [PubMed] [Google Scholar]
- Barros AJD, Ronsmans C, Axelson H. et al. 2012. Equity in maternal, newborn and child interventions in Countdown to 2015: a retrospective review of survey data from 54 countries. Lancet 379: 1225–33. [DOI] [PubMed] [Google Scholar]
- Bhandari GP, Subedi N, Thapa J. et al. 2014. A cluster randomized implementation trial to measure the effectiveness of an intervention package aiming to increase utilization of skilled birth attendants by women for childbirth: study protocol. BMC Pregnancy and Childbirth 14: 109.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhandari N, Bahl R, Mazumdar S. et al. 2003. Effect of community-based promotion of exclusive breastfeeding on diarrhoeal illness and growth: a cluster randomised controlled trial. Lancet 361: 1418–23. [DOI] [PubMed] [Google Scholar]
- Campbell MK, Piaggio G, Elbourne DR, Altman DG.. 2012. Consort 2010 statement: extension to cluster randomized trials. BMJ 345: e5661.. [DOI] [PubMed] [Google Scholar]
- Choulagai B, Aryal U, Shrestha B. et al. 2015. Jhaukhel-Duwakot health demographic surveillance site, Nepal: 2012 follow-up survey and use of skilled birth attendants. Global Health Action 8: 29396.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choulagai B, Onta S, Subedi N. et al. 2013. Barriers to using skilled birth attendants' services in mid- and far-western Nepal: a cross-sectional study. BMC International Health and Human Rights 13: 49.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edmonds JK, Paul M, Sibley L.. 2012. Determinants of place of birth decisions in uncomplicated childbirth in Bangladesh: an empirical study. Midwifery 28: 554–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Family Health Division 1998. Safe Motherhood Policy 1998. Kathmandu: Department of Health Services. [Google Scholar]
- Family Health Division. 2006. National Policy on Skilled Birth Attendants. Kathmandu: Family Health Division, Ministry of Health and Population. [Google Scholar]
- Hayes RJ, Bennett S.. 1999. Simple sample size calculation for cluster randomized controlled trials. International Journal of Epidemiology 28: 319–26. [DOI] [PubMed] [Google Scholar]
- Karkee R, Lee AH, Binns CW. 2013. Why women do not utilize maternity services in Nepal: a literature review. WHO South-East Asia Journal of Public Health 2: 135–41. [DOI] [PubMed] [Google Scholar]
- Karkee R, Lee AH, Pokharel PK.. 2014. Women's perception on quality of maternity services: a longitudinal survey in Nepal. BMC Pregnancy and Childbirth 14: 45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khandker SR, Koolwal GB, Samad HA.. 2010. Handbook on Impact Evaluation: Quantitative Methods and Practices. Washington, DC: The World Bank. [Google Scholar]
- Koblinsky M, Chowdhury ME, Moran A, Ronsmans C.. 2012. Maternal morbidity and disability and their consequences: neglected agenda in maternal health. Journal of Health, Population and Nutrition 30: 124–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lechner M. 2010. The estimation of causal effects by difference-in-difference methods. Foundations and Trends in Econometrics 4: 167–223. [Google Scholar]
- Manandhar DS, Osrin D, Shrestha BP. et al. 2004. Effect of a participatory intervention with women’s groups on birth outcomes in Nepal: cluster-randomised controlled trial. Lancet 364: 970–9. [DOI] [PubMed] [Google Scholar]
- Mayhew M, Hansen PM, Peters DH. et al. 2008. Determinants of skilled birth attendant utilization in Afghanistan: a cross-sectional study. American Journal of Public Health 98: 1849–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ministry of Health and Population. 2005. Operational Guidelines on Incentives for Safe Delivery Services. Kathmandu: Ministry of Health and Population. [Google Scholar]
- Ministry of Health and Population. 2010. The Aama Program: an Initiative Towards Reducing Maternal and Newborn Deaths in Nepal. Kathmandu: Ministry of Health and Population. [Google Scholar]
- Murray DM, Varnell SP, Blitstein JL.. 2004. Design and analysis of group randomized trials: a review of recent methodological developments. American Journal of Public Health 94: 423–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Planning Commission. 2015. Sustainable Development Goals 2016–2030: National (Preliminary) Report. Kathmandu: National Planning Commission. [Google Scholar]
- New Era. 1996. Nepal Family Health Survey 1996. Kathmandu: Ministry of Health, New Era and Macro International Inc. [Google Scholar]
- New Era. 2012. Nepal Demographic and Health Survey 2011. Kathmandu: Ministry of Health and Population, New Era and Macro International Inc. [Google Scholar]
- Onta S, Choulagai B, Shrestha B. et al. 2014. Perceptions of users and providers on barriers to utilizing skilled birth care in mid- and far-western Nepal: a qualitative study. Global Health Action 7: 24580.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penny ME, Creed-Kanashiro HM, Robert RC. et al. 2005. Effectiveness of an educational intervention delivered through the health services to improve nutrition in young children: a cluster-randomised controlled trial. Lancet 365: 1863–72. [DOI] [PubMed] [Google Scholar]
- Ruhago GM, Ngalesoni FN, Norheim OF.. 2012. Addressing inequity to achieve the maternal and child health millennium development goals: looking beyond averages. BMC Public Health 12: 1119.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shrestha SK, Banu B, Khanom K. et al. 2012. Changing trends on the place of delivery: why do Nepali women give birth at home? BMC Reproductive Health 9: 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Lancet. 2016. The Lancet Maternal Health: An Executive Summary for The Lancet’s Series. [Online] The Lancet. Available at: http://www.thelancet.com/series/maternal-health-2016, accessed 18 February 2017
- United Nations. 2011. The Millennium Development Goals Report 2011. New York: United Nations. [Google Scholar]
- WHO. 2015. Trends in Maternal Mortality: 1990 to 2015. Geneva: WHO, UNICEF, World Bank and the United Nations Population Division. Geneva: WHO. [Google Scholar]
- WHO. 2016. WHO recommendations on Antenatal Care for a positive pregnancy experience [PubMed]
- Wikipedia 2016. Sustainable Development Goals. [Online]. Wikipedia. Available at: https://en.wikipedia.org/wiki/Sustainable_Development_Goals, accessed 12 May 2016.