Abstract
Background:
Concomitant radiation with BRAF inhibitor (BRAFi) therapy may increase radiation-induced side effects but also potentially improve tumour control in melanoma patients.
Methods:
A total of 155 patients with BRAF-mutated melanoma from 17 European skin cancer centres were retrospectively analysed. Out of these, 87 patients received concomitant radiotherapy and BRAFi (59 vemurafenib, 28 dabrafenib), while in 68 patients BRAFi therapy was interrupted during radiation (51 vemurafenib, 17 dabrafenib). Overall survival was calculated from the first radiation (OSRT) and from start of BRAFi therapy (OSBRAFi).
Results:
The median duration of BRAFi treatment interruption prior to radiotherapy was 4 days and lasted for 17 days. Median OSRT and OSBRAFi in the entire cohort were 9.8 and 12.6 months in the interrupted group and 7.3 and 11.5 months in the concomitant group (P=0.075/P=0.217), respectively. Interrupted vemurafenib treatment with a median OSRT and OSBRAFi of 10.1 and 13.1 months, respectively, was superior to concomitant vemurafenib treatment with a median OSRT and OSBRAFi of 6.6 and 10.9 months (P=0.004/P=0.067). Interrupted dabrafenib treatment with a median OSRT and OSBRAFi of 7.7 and 9.8 months, respectively, did not differ from concomitant dabrafenib treatment with a median OSRT and OSBRAFi of 9.9 and 11.6 months (P=0.132/P=0.404). Median local control of the irradiated area did not differ in the interrupted and concomitant BRAFi treatment groups (P=0.619). Skin toxicity of grade ≥2 (CTCAE) was significantly increased in patients with concomitant vemurafenib compared to the group with treatment interruption (P=0.002).
Conclusions:
Interruption of vemurafenib treatment during radiation was associated with better survival and less toxicity compared to concomitant treatment. Due to lower number of patients, the relevance of treatment interruption in dabrafenib treated patients should be further investigated. The results of this analysis indicate that treatment with the BRAFi vemurafenib should be interrupted during radiotherapy. Prospective studies are desperately needed.
Keywords: radiation, radiotherapy, BRAF, vemurafenib, dabrafenib
BRAF inhibitors (BRAFi) combined with MEK inhibitors are standard therapy in patients with BRAF V600 mutated metastatic melanoma (Larkin et al, 2014; Long et al, 2014). Although highly effective, radiation therapy may still be indicated, e.g., for the treatment of brain or symptomatic bone metastases (Lubgan et al, 2014; Ishihara et al, 2016; Nowak-Sadzikowska et al, 2016). A recent analysis showed an increased frequency of adverse events when BRAFi were administered concomitantly with radiotherapy (Hecht et al, 2015), which subsequently lead to a drug safety warning by the FDA and other institutions. However, an interruption of BRAFi treatment may lead to decreased tumour control with the progression of non-irradiated metastases. Furthermore, in preclinical models BRAFi sensitised melanoma cells to radiotherapy (Sambade et al, 2011; Dasgupta et al, 2013). This radiosensitising effect could improve efficacy with improved tumour control in patients treated concomitantly. Currently, no standard approach with regard to a possible interruption of BRAFi therapy during radiotherapy exists. As this question frequently appears in clinical practice, the aim of this study is to provide reliable data on local and systemic tumour control to help decide which is more beneficial: concomitant or interrupted BRAFi treatment during radiotherapy.
Material and methods
Patients
Between September 2010 and January 2017 a total of 155 patients with metastatic BRAF-mutated melanoma from 17 skin cancer centres in Germany, Austria and Switzerland were retrospectively analysed. This retrospective study was approved by the local institutional review board of the Friedrich-Alexander-Universität Erlangen-Nürnberg (nr. 358_17 Bc). Informed consent was waived since only data from standard clinical therapy were collected and analysed anonymously. All patients received conventional or stereotactic radiotherapy either with concomitant or interrupted BRAFi therapy. Analyses were performed for the entire patient cohort and for vemurafenib- and dabrafenib-treated patients separately, since retrospective analyses suggest vemurafenib to be a more effective radiosensitiser than dabrafenib (Hecht et al, 2015). Kaplan–Meier analyses for local tumour control (LC), progression free survival (PFS) and overall survival (OSRT) were performed from the beginning of radiotherapy. In addition, OS was analysed from the beginning of the BRAFi therapy (OSBRAFi). If patients received more than one series of radiotherapy treatment, the first radiotherapy was selected for all analyses. Patients’ characteristics are shown in Table 1. Median follow-up time was 8.1 months (range 0.1–51.4 months). During the follow-up 154 OS and 171 PFS events occurred. Toxicity was graded according CTCAE 4.0.
Table 1. Clinical characteristics of the patient cohort.
|
All patients |
Vemurafenib |
Dabrafenib |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Concomitant | Interrupted | Concomitant | Interrupted | Concomitant | Interrupted | ||||
| Number of patients | 87 | 68 | 59 | 51 | 28 | 17 | |||
| Mean age in years (range) | 53 (19–85) | 59 (18–83) | P=0.022 | 56 (19–85) | 58 (18–83) | P=0.683 | 48 (19–73) | 63 (40–80) | P=0.001 |
| Male | 53 (61%) | 43 (63%) | P=0.868 | 37 (63%) | 30 (59%) | P=0.699 | 16 (57%) | 13 (76%) | P=0.219 |
| Pts. with brain metastases | 54 (62%) | 44 (65%) | P=0.867 | 38 (64%) | 32 (63%) | P=1.000 | 16 (57%) | 12 (71%) | P=0.528 |
| Concomitant MEK-inhibitor | 8 (9%) | 7 (10%) | P=1.000 | 0 | 4 (8%) | P=0.043 | 8 (29%) | 3 (18%) | P=0.493 |
| LDH | P=0.213 | P=0.140 | P=0.710 | ||||||
| Elevated (>250 U l−1) | 42 (48%) | 23 (34%) | 35 (59%) | 20 (39%) | 7 (25%) | 3 (18%) | |||
| Normal (⩽250 U l−1) | 31 (36%) | 34 (50%) | 18 (31%) | 20 (39%) | 16 (57%) | 11 (65%) | |||
| Unknown | 14 (16%) | 11 (16%) | 6 (10%) | 11 (22%) | 5 (18%) | 3 (18%) | |||
| Number of pretreatments | P=0.145 | P=0.161 | P=0.589 | ||||||
| 0 | 51 (59%) | 41 (60%) | 37 (63%) | 31 (61%) | 14 (50%) | 10 (59%) | |||
| 1 | 25 (29%) | 19 (28%) | 15 (25%) | 15 (29%) | 10 (36%) | 4 (24%) | |||
| ≥2 | 11 (13%) | 2 (3%) | 7 (12%) | 1 (2%) | 4 (14%) | 1 (6%) | |||
| Unknown | 0 | 6 (9%) | 0 | 4 (8%) | 0 | 2 (12%) | |||
| ECOG | P=0.003 | P=0.008 | P=0.321 | ||||||
| 0 | 18 (21%) | 31 (46%) | 10 (17%) | 22 (43%) | 8 (29%) | 9 (53%) | |||
| 1 | 28 (32%) | 15 (22%) | 19 (32%) | 12 (24%) | 9 (32%) | 3 (18%) | |||
| ≥2 | 11(13%) | 5 (7%) | 8 (14%) | 2 (4%) | 3 (11%) | 3 (18%) | |||
| Unknown | 30 (34%) | 17 (25%) | 22 (37%) | 15 (29%) | 8 (29%) | 2 (12%) | |||
| Irradiated sites | P=0.757 | P=0.753 | P=0.750 | ||||||
| Whole-brain radiotherapy (WBRT) | 31 (36%) | 28 (41%) | 24 (41%) | 23 (45%) | 7 (25%) | 5 (29%) | |||
| Stereotactic radiotherapy (STX) brain | 23 (26%) | 16 (24%) | 14 (24%) | 9 (18%) | 9 (32%) | 7 (41%) | |||
| Bone metastases | 14 (16%) | 8 (12%) | 9 (15%) | 7 (14%) | 5 (18%) | 1 (6%) | |||
| Axillary lymph nodes | 7 (8%) | 7 (10%) | 3 (5%) | 6 (12%) | 4 (14%) | 1 (6%) | |||
| Mediastinal metastases | 5 (6%) | 1 (1%) | 4 (7%) | 1 (2%) | 1 (4%) | 0 | |||
| Soft tissue metastases | 4 (5%) | 5 (7%) | 3 (5%) | 3 (6%) | 1 (4%) | 2 (12%) | |||
| Others | 3 (3%) | 3 (4%) | 2 (3%) | 2 (4%) | 1 (4%) | 1 (6%) | |||
Abbreviations: ECOG=Eastern Cooperative Oncology Group; LDH=lactate dehydrogenase.
Statistical analysis
Data analysis was carried out using SPSS 21.0 (IBM Corporation, Armonk, NY, USA). Patients’ characteristics were checked for differences with Fisher’s exact test (categorical items) and Student’s t-test (continuous items). The Kaplan–Meier method and the log-rank test were used to analyse tumour control and survival. Univariate and multivariate regression analyses of OS were performed using Cox’s proportional hazard model. Variables associated with a P-value <0.35 in univariate analyses were considered for inclusion in multivariate analyses. The proportional hazard assumption was tested through plotting logminus-log curves. Toxicity in the subgroups was compared with the Mann–Whitney U test. A P-value below 0.05 was considered to be statistically significant.
Results
Tumour control and survival of the entire patient cohort and the subgroups
Survival of patients receiving concomitant BRAFi therapy and radiotherapy was compared to those with interrupted BRAFi therapy during radiotherapy. All analyses were performed for the entire patient cohort with 155 patients and for patients treated with vemurafenib and dabrafenib separately. Patients’ characteristics are shown in Table 1 and are balanced with respect to important prognostic parameters like frequency of brain metastases (P=0.867). ECOG was significantly better in the interrupted group than in the concomitant group (P=0.003), whereas lactate dehydrogenase (LDH) tended to be more frequently increased in the concomitant group, but the latter reached no statistical significance (P=0.140). There were no differences in the number of pretreatments (P=0.145). Concomitant MEK inhibitor treatment was rare and balanced between the groups (P=1.000).
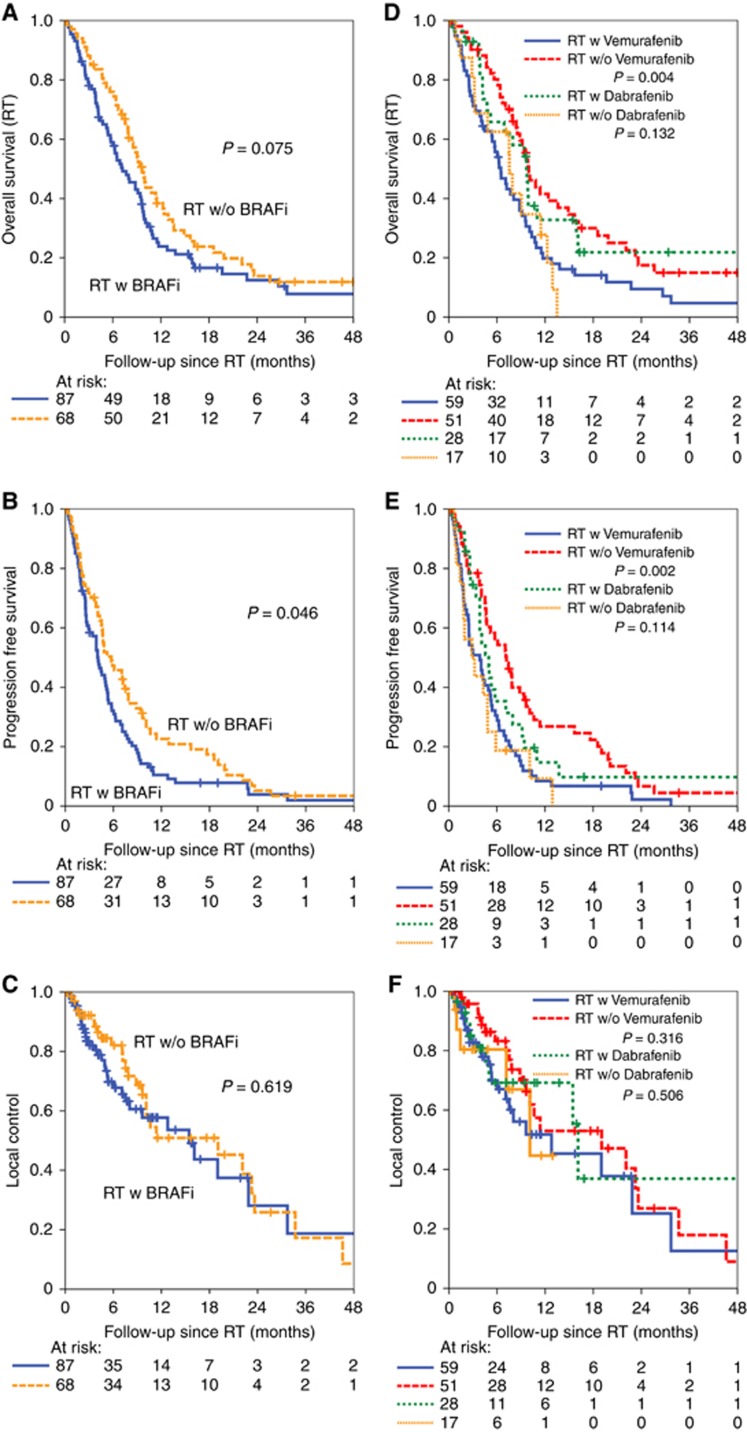
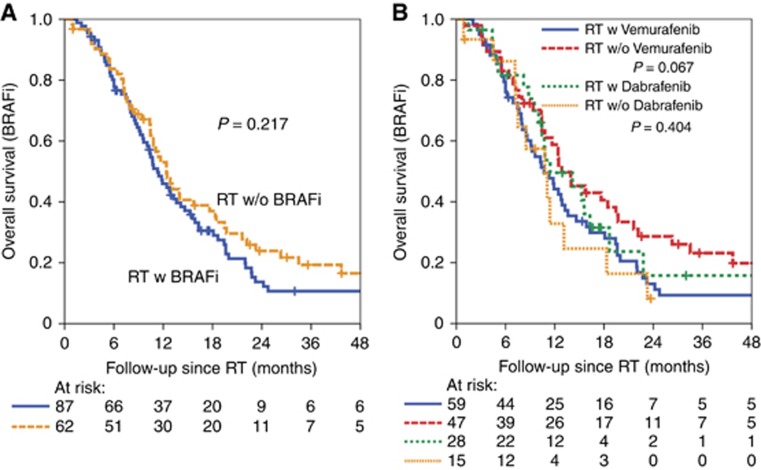
The starting point for the calculation of LC, PFS and OSRT was the start of radiotherapy and for OSBRAFi the initiation of BRAFi therapy. For the entire patient cohort the median OSRT tended to be longer in the interrupted group than in the concomitant group with 9.8 months vs 7.3 months, respectively (P=0.075, Figure 1A). The median PFS was significantly longer in the interrupted group with 5.8 months vs 4.2 months, respectively (P=0.046, Figure 1B). There was no difference in median LC of the irradiated area (P=0.619, Figure 1C). Similarly, there was no difference when the beginning of BRAF inhibitor treatment was used for the calculation (OSBRAFi interrupted 12.6 months vs concomitant 11.5 months, P=0.217, Figure 2A).
Figure 1.
Kaplan–Meier estimates of OSRT, PFS and LC calculated from the beginning of radiotherapy. Overall survival (OSRT), progression-free survival (PFS) and local tumour control of the irradiated area (LC) were calculated from start of the first radiotherapy. The patient cohort with concomitant BRAF inhibitor and radiotherapy (RT w BRAFi) was compared to the cohort with radiotherapy and interrupted BRAF inhibitor (RT w/o BRAFi). OSRT, PFS and LC were calculated for concomitant and interrupted BRAF inhibitor treatment during radiotherapy (A, B, C) and for the subgroups treated with vemurafenib and dabrafenib (D, E, F). BRAFi=BRAF inhibitor; RT=radiotherapy.
Figure 2.
Kaplan–Meier estimates of OSBRAFi calculated from the beginning of BRAFi therapy. Overall survival (OSBRAFi) was calculated from start of BRAFi therapy and was analysed for patients with concomitant and interrupted BRAFi treatment during radiotherapy (A) and separately for the subgroups treated with vemurafenib and dabrafenib (B). BRAFi=BRAF inhibitor; RT=radiotherapy.
To determine potential differences between both BRAFi, interrupted and concomitant treatment with vemurafenib and dabrafenib were analysed separately. Median OSRT and PFS were clearly longer in the subgroup of interrupted vemurafenib with 10.1 and 7.3 months, respectively, compared to 6.6 and 3.9 months in the subgroup of concomitant vemurafenib (P=0.004/P=0.002; Figure 1D and E, Supplementary Tables S1 And S2). OSRT and PFS did not significantly differ in the subgroup of interrupted dabrafenib with 7.7 and 3.3 months, respectively, compared to concomitant treatment with 9.9 and 5.1 months (P=0.132/P=0.114). Moreover, interrupted vemurafenib treatment led to a distinctly longer OSRT and PFS than interrupted dabrafenib treatment (P=0.022/P=0.004), but not than concomitant dabrafenib treatment (P=0.697/P=0.284). There was no difference in any of the subgroups for local tumour control (Figure 1F).
The mean pre-treatment period with BRAFi prior to radiotherapy was 4.2 months in the concomitant group and 2.9 months in the interrupted group. Though, the pre-treatment was 1.2 months longer in the concomitant group than in the interrupted group. It might cause a bias and therefore survival was analysed from the beginning of BRAFi treatment. In this calculation, OS also tended to be longer in the interrupted vemurafenib group than in the concomitant group (OSBRAFi interrupted 13.1 months vs concomitant 10.9 months, P=0.067, Figure 2B). In conclusion, the survival benefit in the entire patient cohort showed a longer OS in the interrupted vemurafenib subgroup compared to the concomitant vemurafenib subgroup.
In a univariate analysis of the vemurafenib subgroup the effect of interrupted vs concomitant vemurafenib was compared to other prognostic parameters of metastatic melanoma (Table 2). In this cohort ECOG performance status, brain metastases and the duration of BRAFi pretreatment had only low impact on survival. The stronger prognostic parameters (all P<0.35) as elevated LDH, radiation-associated toxicity, systemic pretreatment and interrupted vemurafenib treatment were included in a multivariate analysis. Here toxicity was the weakest variable. Systemic pretreatment (HR 1.65, 0.96–2.87, P=0.073) and elevated LDH (HR 1.70, 95% CI 0.96–3.00, P=0.070) were predictors for bad prognosis. The only independent prognostic parameter for overall survival in the multivariate analysis was interrupted vs concomitant treatment with vemurafenib during radiotherapy (HR 0.51, 0.29–0.88, P=0.015).
Table 2. Univariate and multivariate analysis of the vemurafenib subgroup.
|
Univariate analysis |
Multivariate analysis |
|||||
|---|---|---|---|---|---|---|
| Variable | Hazard ratio | 95% CI | P | Hazard ratio | 95% CI | P |
| ECOG (0 (n=29) vs >0 (n=38)) | 1.007 | 0.505–2.006 | 0.985 | — | — | — |
| LDH (⩽ 250 (n=26) v.>250 U/l (n=41)) | 1.514 | 0.805–2.849 | 0.199 | 1.698 | 0.959–3.008 | 0.070 |
| Brain metastases (no (n=26) vs yes (n=41)) | 1.194 | 0.637–2.24 | 0.580 | — | — | — |
| Period BRAFi RT (⩽58 days (n=37) vs>58 days (n=30)) | 1.155 | 0.668–1.999 | 0.606 | — | — | — |
| Toxicity (no (n=33) vs any (n=34)) | 1.656 | 0.622–4.407 | 0.312 | 1.455 | 0.635–3.334 | 0.376 |
| Drugs (only BRAFi (n=30) vs drug prior to BRAFi (n=37)) | 1.746 | 0.991–3.077 | 0.054 | 1.654 | 0.955–2.866 | 0.073 |
| Vemurafenib (concomitant (n=36) vs interrupted (n=31)) | 0.683 | 0.309–1.512 | 0.347 | 0.507 | 0.293–0.877 | 0.015 |
Abbreviations: BRAFi=BRAF inhibitor; CI=confidence interval; ECOG=Eastern Cooperative Oncology Group; LDH=lactate dehydrogenase.
Variables associated with a P-value <0.35 in univariate analyses were considered for inclusion in multivariate analyses. P-values <0.05 were considered to be statistically significant and were marked in bold.
Furthermore, survival with respect to LDH and systemic pretreatment were analysed (Supplementary Figure S1). In the subgroup of patients with elevated LDH, the OSRT was longer in the interrupted vemurafenib group compared to the concomitant treatment group (P=0.004). In the subgroup with normal LDH this was only a trend (P=0.115). Especially patients with no systemic therapy prior to vemurafenib benefited from the interruption of vemurafenib during radiotherapy (P=0.004). In pretreated patients this effect almost disappeared (P=0.325). ECOG performance status had no relevant influence on OS in the entire patient cohort (Table 2).
Except for one centre, all centres had a standard procedure to either interrupt or not BRAFi therapy thus limiting potential bias for concomitant therapy in patients with a high rate of progression. An analysis conducted with the exclusion of patients with non-standard treatment and the centre without standard procedure (Supplementary Table S3) confirmed the OSRT benefit of interrupted BRAFi in the entire patient cohort (P=0.016) and in the vemurafenib subgroup (P=0.001; Supplementary Figure S2).
Safety of concomitant BRAF inhibitor therapy and radiotherapy
Since a radiosensitising effect of BRAF inhibitors has been described previously toxicity was analysed separately for both drugs and for interrupted and concomitant therapy schemes (Table 3). The median duration of BRAFi treatment interruption prior to beginning of radiotherapy was 4 days (range 0–37 days) and lasted for 17 days (range 3–68 days). Skin toxicity grade ≥2 was significantly increased in patients with concomitant vemurafenib compared to the interrupted vemurafenib group with 35% and 14% of patients, respectively, experiencing radiodermatitis (P=0.002). The risk of radiation dermatitis grade ≥2 tended to be lower in the group of concomitant dabrafenib treatment with 21% compared to 35% in the group of concomitant vemurafenib treatment, but without statistical significance (P=0.185). Follicular cystic proliferation of the irradiated skin exclusively occurred in patients with concomitant vemurafenib therapy.
Table 3. Adverse events of patients treated with BRAF inhibitor in combination with radiotherapy.
| Concomitant vemurafenib (n=59) | Interrupted vemurafenib (n=51) | Concomitant dabrafenib (n=28) | Interrupted dabrafenib (n=17) | |
|---|---|---|---|---|
|
Radiation dermatitis | ||||
| 1° | 11 (19%) | 6 (12%) | 4 (14%) | 2 (12%) |
| 2° | 15 (25%) | 6 (12%) | 4 (14%) | 0 |
| 3° | 6 (10%) | 1 (2%) | 2 (7%) | 0 |
|
Other adverse events | ||||
| Follicular cystic proliferation | 10 (17%)a | 0 | 0 | 0 |
| Hearing disorder | 4 (7%) | 0 | 0 | 0 |
| Dysphagia | 2 (3%) | 0 | 0 | 0 |
| Hyperpigmentation | 1 (2%) | 3 (6%) | 0 | 0 |
| Impaired wound healing | 1 (2%) | 0 | 1 (4%) | 0 |
| Haemorrhagic intracranial metastasis | 1 (2%) | 0 | 1 (4%) | 0 |
| Pneumonitis | 1 (2%) | 0 | 1 (4%) | 0 |
| Othersa | 3 (5%)b | 1 (2%)c | 0 | 1 (6%)d |
Adverse events appearing in more than one patient in the entire cohort are listed in the table while adverse events occurring in only one patient are summarised in ‘Others’.
Includes one case of cutis verticis gyrate-like toxicity as the maximal form of follicular cystic proliferation.
One case each of cardiac insufficiency, hand-food syndrome and taste disorder
Radiation recall dermatitis
Pruritus.
Discussion
Currently, no standard approach exists in clinical routine with regard to continuation or interruption of BRAFi therapy during radiotherapy. A clinically relevant radiosensitisation by BRAFi has been described and even led to a recommendation of the Eastern Cooperative Oncology Group to interrupt BRAFi treatment during radiotherapy (Hecht et al, 2015; Anker et al, 2016). This radiosensitising effect could potentially also increase the response of the tumour cells to radiotherapy and thus improve tumour control. In vitro vemurafenib sensitises melanoma cells to radiotherapy (Sambade et al, 2011; Dasgupta et al, 2013). This large multicentre study was conducted to evaluate whether this effect also appears in melanoma patients and subsequently bases the decision on BRAFi interruption on in vivo data. We provide evidence that LC was equal in the BRAFi interrupted and BRAFi concomitant groups. More importantly, OS and PFS in patients taking vemurafenib were longer in the interrupted group than in the concomitant group. Thus, this study indicates that vemurafenib should be interrupted during radiotherapy, which increases efficacy and decreases toxicity. In patients taking dabrafenib OS and PFS did not differ in the interrupted and concomitant group. The lack of difference in efficacy might be attributable to the lower number of patients in the dabrafenib group. Consequently, the relevance of a treatment interruption in dabrafenib treated patients is not clear.
A limitation of this work is its retrospective design possibly resulting in unbalanced patient subgroups. However, the most important prognostic factor, the frequency of brain metastases, was equal in the subgroups. The number of patients with increased LDH tended to be higher in the concomitant group, but a subgroup analysis in patients with low and high LDH confirmed the benefit of interrupted vemurafenib in both groups. Currently, standard of therapy is combination therapy with BRAF and MEK inhibitors (Larkin et al, 2014; Long et al, 2014), whereas in this study cohort only few patients had additional MEK inhibitors and they were evenly distributed across groups. In both groups the frequency of irradiated anatomic locations was similar. Despite the significantly worse ECOG score of patients in the concomitant group the univariate analysis of the vemurafenib subgroup showed ECOG only as a very weak prognostic parameter in this patient cohort. In the multivariate analysis, only the interruption of vemurafenib had significant impact on OS. One bias of this retrospective analysis might have been the clinical strategy to continue BRAFi treatment in patients with high tumour burden. In an additional analysis of patients exclusively treated according to the centres’ standard procedure, the survival benefit of interruption of vemurafenib during radiotherapy was confirmed. The mean pre-treatment with BRAFi was 1.2 months longer in the concomitant group than in the interrupted group. Starting the analyses from the first irradiation, this could bias the results. Possibly more patients had already progressed at the time point of radiotherapy in the concomitant group. However, when survival was calculated from the beginning of BRAFi treatment, OS also tended to be longer in the interrupted vemurafenib group than in the concomitant group. Thus, patients with interrupted vemurafenib therapy during radiotherapy really seem to have an improved OS.
As local tumour control is similar and no severe toxicities appeared, the treatment interruption of vemurafenib has probably a positive effect on systemic tumour control. This finding is in line with reports of successful re-challenge with BRAFi after treatment interruption due to acquired resistance (Seghers et al, 2012; Koop et al, 2014; Mackiewicz-Wysocka et al, 2014; Roux et al, 2015). Additionally, immunological mechanisms could be the reason for the favorable effect of vemurafenib interruption. Since vemurafenib binds less specifically to mutated BRAF than dabrafenib and binding to wildtype BRAF (Menzies et al, 2013) could inhibit ERK activation in immune cells. This signalling pathway is essential for proliferation or maturation of several immune cells (Gato-Canas et al, 2015; Ohtsuka et al, 2016). Radiation therapy also changes the tumour cell phenotype and the tumour microenvironment, enhancing an anti- tumour immune response (Barker et al, 2015). In combination with immune stimulating agents such as ipilimumab this can lead to an abscopal effect with improved tumour control distant from the irradiated metastasis (Golden et al, 2013; Chandra et al, 2015). Similarly, vemurafenib might interact with radiation therapy immunologically (Schilling et al, 2014).
So far, it has not been proven that a treatment interruption of BRAFi prevents radiation-induced adverse events. In this patient cohort the median planned interruption of BRAFi was 4 days prior to beginning of radiation therapy and lasted for 17 days. This interruption of vemurafenib significantly reduced skin toxicity with similar if not enhanced efficacy compared to concomitant treatment. Since vemurafenib has a half-life of ∼57 h (Zhang et al, 2017), the median interruption period of vemurafenib prior to radiotherapy was approximately two half-life times. Based on our findings with regard to efficacy and safety, we recommend interrupting vemurafenib ∼4 days prior to the first irradiation.
Although toxicity in the concomitant treatment arm was increased, it was manageable in all cases. There appeared no severe visceral or even lethal complications as described in single case reports (Anker et al, 2016). Radiation recall dermatitis has been reported previously with BRAFi (Conen et al, 2014; Forschner et al, 2014; Houriet et al, 2014) but is rare. Consequently, BRAFi interruption after the last fraction of radiotherapy seems not necessary. Follicular cystic proliferation or the cutis verticis gyrate-like skin reaction as its maximal form appeared in 17% patients taking vemurafenib concomitantly, which is in line with other reported cases (Harding et al, 2014; Lang et al, 2014).
Conclusion
In this retrospective multicentre study investigating a large patient cohort with metastatic melanoma treated with BRAFi therapy during radiotherapy the concomitant BRAFi therapy did not improve local or distant tumour control. Survival in patients with interrupted vemurafenib was better than in patients with concomitant treatment. The interruption of vemurafenib therapy during radiotherapy reduced the risk of radiation dermatitis. Thus, it is recommended to interrupt vemurafenib during radiotherapy. Due to lower number of patients, the relevance of treatment interruption in dabrafenib treated patients should be further investigated.
Acknowledgments
MH and LH received funding from Novartis for the in vitro investigation of radiosensitisation by BRAF inhibitors and MEK inhibitors in melanoma cell lines (S2TAF-003). This funding was for preclinical experiments only. There was no funding for the design and analysis of this study or for writing the manuscript. The preclinical study has been finished.
Footnotes
Supplementary Information accompanies this paper on British Journal of Cancer website (http://www.nature.com/bjc)
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 4.0 Unported License.
MH participated in advisory boards for Merck Serono and BMS; received research funding from Novartis and MSD; travel support from Merck Serono, MSD and Teva. FM received honoraria from Roche, BMS, GSK, Novartis, MSD; travel support from Roche Pharma and BMS; research funding from Wyeth/Pfizer, MerckSerono, Novartis. LZ has served as consultant or/and has received honoraria from Roche, BMS, MSD, GSK, Novartis, Merck, and travel support from MSD, BMS, Amgen and Novartis. CL participated in advisory board from Roche, MSD, BMS, Amgen, Pierre Fabre, Novartis, Leo; received speaker honoraria from Roche, MSD, Amgen, Novartis, BMS; travel support from Roche, BMS, Amgen, Novartis. CW is principal investigator in clinical studies by Amgen, BMS, Curevac, Delcath, Kyowa, Leo Pharma, Novartis and Roche and is consultant or has received speaker fees, travel support or research funding from Amgen, BMS, Novartis, MSD, Roche and Takeda. AF reports honoraria from BMS, MSD, Roche, Novartis. She is advisory board member of Roche, Novartis and received travel support from Roche, Novartis and BMS. RG received research funding from Roche Pharma, Novartis, Pfizer, Johnson&Johnson. Honoraria from Roche Pharma, BMS, GSK, Novartis, Merck Serono, MSD, Almirall-Hermal, Amgen, Galderma, Janssen, Boehringer Ingelheim. Honoraria for advisory boards from Roche Pharma, BMS, GSK, Novartis, MSD, Almirall-Hermal, LEO, Amgen, Pfizer, Pierre Fabre. Meeting/travel support Roche Pharma, BMS. JSU is on the advisory board or has received honoraria and travel support from Amgen, BMS, GSK, LeoPharma, MSD, Novartis, Roche. SMG: Intermittent advisory board relationship and travel grant support from MSD, BMS, Novartis and Roche. Research time support by the University Hospital Zurich and medAlumni! MG has received a speaker fee from Roche. JCH is principal investigator in clinical studies by BMS, MSD, Merck, Roche, Novartis/GSK, Amgen, BioNTech and ImmunoCore and is consultant or has received speaker fees, travel grants or research funding from BMS, MSD, Merck, Roche, Novartis, Amgen and Pfizer. FK participated in symposia, advisory boards and meetings and therefore received payments and travel grants from Amgen, BMS, Merck-Serono, MSD, Novartis, Pierre-Fabre, Regeneron and Roche. RR participated in advisory boards for Novartis, received fees for lectures from Novartis and Amgen and travel support from Bristol-Myers Squibb and Amgen. CB is principal investigator in clinical studies by Amgen, BMS, MSD, Novartis, Array Pharma / Pierre Fabre, Regeneron, and Roche, she has been consultant and/or has received speaker´s honoraria and/or travel support by Amgen, AstraZeneca, BMS, MSD, Novartis, Pierre Fabre, and Roche. DS report research funding from Novartis and GSK, honoraria from Amgen and Boehringer Ingelheim, Leo Pharma, Roche MSD and BMS SG is consultant or has received speaker fees, or travel grants from AbbVie, Amgen, BMS, Beiersdorf, MSD, Merck, Novartis, Roche, Sanofi-Pasteur-MSD, Takeda. RF received honoraria from Fresenius, Merck Serono, MSD, Roche; has consulting or advisory role for Fresenius, Merck Serono, MSD, Roche; Speakers' Bureau for Fresenius, Merck, MSD, Roche; received research funding from MSD and travel support from Fresenius, Merck, MSD, Roche. LH is principal investigator in clinical studies by BMS, MSD, Merck, Roche, Amgen, GSK, Curevac and Novartis and is consultant or has received speaker fees, travel grants or research funding from BMS, MSD, Merck, Roche, Amgen, Curevacc and Novartis. The remaining authors declare no conflict of interest.
Supplementary Material
References
- Anker CJ, Grossmann KF, Atkins MB, Suneja G, Tarhini AA, Kirkwood JM (2016) Avoiding severe toxicity from combined BRAF Inhibitor and radiation treatment: consensus guidelines from the Eastern Cooperative Oncology Group (ECOG). Int J Radiat Oncol Biol Phys 95(2): 632–646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barker HE, Paget JT, Khan AA, Harrington KJ (2015) The tumour microenvironment after radiotherapy: mechanisms of resistance and recurrence. Nat Rev Cancer 15(7): 409–425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chandra RA, Wilhite TJ, Balboni TA, Alexander BM, Spektor A, Ott PA, Ng AK, Hodi FS, Schoenfeld JD (2015) A systematic evaluation of abscopal responses following radiotherapy in patients with metastatic melanoma treated with ipilimumab. Oncoimmunology 4(11): e1046028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conen K, Mosna-Firlejczyk K, Rochlitz C, Wicki A, Itin P, Arnold AW, Gross M, Zimmermann F, Zippelius A (2014) Vemurafenib-induced radiation recall dermatitis: case report and review of the literature. Dermatology 230(1): 1–4. [DOI] [PubMed] [Google Scholar]
- Dasgupta T, Haas-Kogan DA, Yang X, Olow A, Yang DX, Gragg A, Orloff LA, Yom SS (2013) Genotype-dependent cooperation of ionizing radiation with BRAF inhibition in BRAF V600E-mutated carcinomas. Invest New Drugs 31(5): 1136–1141. [DOI] [PubMed] [Google Scholar]
- Forschner A, Zips D, Schraml C, Rocken M, Iordanou E, Leiter U, Weide B, Garbe C, Meier F (2014) Radiation recall dermatitis and radiation pneumonitis during treatment with vemurafenib. Melanoma Res 24(5): 512–516. [DOI] [PubMed] [Google Scholar]
- Gato-Canas M, Martinez de Morentin X, Blanco-Luquin I, Fernandez-Irigoyen J, Zudaire I, Liechtenstein T, Arasanz H, Lozano T, Casares N, Chaikuad A, Knapp S, Guerrero-Setas D, Escors D, Kochan G, Santamaria E (2015) A core of kinase-regulated interactomes defines the neoplastic MDSC lineage. Oncotarget 6(29): 27160–27175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golden EB, Demaria S, Schiff PB, Chachoua A, Formenti SC (2013) An abscopal response to radiation and ipilimumab in a patient with metastatic non-small cell lung cancer. Cancer Immunol Res 1(6): 365–372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harding JJ, Barker CA, Carvajal RD, Wolchok JD, Chapman PB, Lacouture ME (2014) Cutis verticis gyrata in association with vemurafenib and whole-brain radiotherapy. J Clin Oncol 32(14): e54–e56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hecht M, Zimmer L, Loquai C, Weishaupt C, Gutzmer R, Schuster B, Gleisner S, Schulze B, Goldinger SM, Berking C, Forschner A, Clemens P, Grabenbauer G, Muller-Brenne T, Bauch J, Eich HT, Grabbe S, Schadendorf D, Schuler G, Keikavoussi P, Semrau S, Fietkau R, Distel LV, Heinzerling L (2015) Radiosensitization by BRAF inhibitor therapy-mechanism and frequency of toxicity in melanoma patients. Ann Oncol 26(6): 1238–1244. [DOI] [PubMed] [Google Scholar]
- Houriet C, Klass ND, Beltraminelli H, Borradori L, Oberholzer PA (2014) Localized epidermal cysts as a radiation recall phenomenon in a melanoma patient treated with radiotherapy and the braf inhibitor vemurafenib. Case Rep Dermatol 6(3): 213–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ishihara T, Yamada K, Harada A, Isogai K, Tonosaki Y, Demizu Y, Miyawaki D, Yoshida K, Ejima Y, Sasaki R (2016) Hypofractionated stereotactic radiotherapy for brain metastases from lung cancer: evaluation of indications and predictors of local control. Strahlenther Onkol 192(6): 386–393. [DOI] [PubMed] [Google Scholar]
- Koop A, Satzger I, Alter M, Kapp A, Hauschild A, Gutzmer R (2014) Intermittent BRAF-inhibitor therapy is a feasible option: report of a patient with metastatic melanoma. Br J Dermatol 170(1): 220–222. [DOI] [PubMed] [Google Scholar]
- Lang N, Sterzing F, Enk AH, Hassel JC (2014) Cutis verticis gyrata-like skin toxicity during treatment of melanoma patients with the BRAF inhibitor vemurafenib after whole-brain radiotherapy is a consequence of the development of multiple follicular cysts and milia. Strahlenther Onkol 190(11): 1080–1081. [DOI] [PubMed] [Google Scholar]
- Larkin J, Ascierto PA, Dreno B, Atkinson V, Liszkay G, Maio M, Mandala M, Demidov L, Stroyakovskiy D, Thomas L, de la Cruz-Merino L, Dutriaux C, Garbe C, Sovak MA, Chang I, Choong N, Hack SP, McArthur GA, Ribas A (2014) Combined vemurafenib and cobimetinib in BRAF-mutated melanoma. N Engl J Med 371(20): 1867–1876. [DOI] [PubMed] [Google Scholar]
- Long GV, Stroyakovskiy D, Gogas H, Levchenko E, de Braud F, Larkin J, Garbe C, Jouary T, Hauschild A, Grob JJ, Chiarion Sileni V, Lebbe C, Mandala M, Millward M, Arance A, Bondarenko I, Haanen JB, Hansson J, Utikal J, Ferraresi V, Kovalenko N, Mohr P, Probachai V, Schadendorf D, Nathan P, Robert C, Ribas A, DeMarini DJ, Irani JG, Casey M, Ouellet D, Martin AM, Le N, Patel K, Flaherty K (2014) Combined BRAF and MEK inhibition versus BRAF inhibition alone in melanoma. N Engl J Med 371(20): 1877–1888. [DOI] [PubMed] [Google Scholar]
- Lubgan D, Ziegaus A, Semrau S, Lambrecht U, Lettmaier S, Fietkau R (2014) Effective local control of vertebral metastases by simultaneous integrated boost radiotherapy: preliminary results. Strahlenther Onkol 191(3): 264–271. [DOI] [PubMed] [Google Scholar]
- Mackiewicz-Wysocka M, Krokowicz L, Kocur J, Mackiewicz J (2014) Resistance to vemurafenib can be reversible after treatment interruption: a case report of a metastatic melanoma patient. Medicine 93(27): e157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Menzies AM, Kefford RF, Long GV (2013) Paradoxical oncogenesis: are all BRAF inhibitors equal? Pigment CellMelanoma Res 26(5): 611–615. [DOI] [PubMed] [Google Scholar]
- Nowak-Sadzikowska J, Walasek T, Jakubowicz J, Blecharz P, Reinfuss M (2016) Current treatment options of brain metastases and outcomes in patients with malignant melanoma. Rep Pract Oncol Radiother 21(3): 271–277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ohtsuka S, Ogawa S, Wakamatsu E, Abe R (2016) Cell cycle arrest caused by MEK/ERK signaling is a mechanism for suppressing growth of antigen-hyperstimulated effector T cells. International immunology 28(11): 547–557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roux J, Pages C, Malouf D, Basset Seguin N, Madjlessi N, Baccard M, Comte C, Archimbaud A, Battistella M, Viguier M, Mourah S, Bagot M, Lebbe C (2015) BRAF inhibitor rechallenge in patients with advanced BRAF V600-mutant melanoma. Melanoma Res 25(6): 559–563. [DOI] [PubMed] [Google Scholar]
- Sambade MJ, Peters EC, Thomas NE, Kaufmann WK, Kimple RJ, Shields JM (2011) Melanoma cells show a heterogeneous range of sensitivity to ionizing radiation and are radiosensitized by inhibition of B-RAF with PLX-4032. Radiother Oncol 98(3): 394–399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schilling B, Sondermann W, Zhao F, Griewank KG, Livingstone E, Sucker A, Zelba H, Weide B, Trefzer U, Wilhelm T, Loquai C, Berking C, Hassel J, Kahler KC, Utikal J, Al Ghazal P, Gutzmer R, Goldinger SM, Zimmer L, Paschen A, Hillen U, Schadendorf D DeCog (2014) Differential influence of vemurafenib and dabrafenib on patients' lymphocytes despite similar clinical efficacy in melanoma. Ann Oncol 25(3): 747–753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seghers AC, Wilgenhof S, Lebbe C, Neyns B (2012) Successful rechallenge in two patients with BRAF-V600-mutant melanoma who experienced previous progression during treatment with a selective BRAF inhibitor. Melanoma Res 22(6): 466–472. [DOI] [PubMed] [Google Scholar]
- Zhang W, Heinzmann D, Grippo JF (2017) Clinical pharmacokinetics of vemurafenib. Clin Pharmacokinet 56(9): 1033–1043. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.