Abstract
Despite growing support for integration of frontline services, a lack of information about the pre-conditions necessary to integrate such services hampers the ability of policy makers and implementers to assess how feasible or worthwhile integration may be, especially in low- and middle-income countries (LMICs). We adopted a modified systematic review with aspects of realist review, including quantitative and qualitative studies that incorporated assessment of health system preparedness for and capacity to implement integrated services. We searched Medline via Ovid, Web of Science and the Cochrane library using terms adapted from Dudley and Garner’s systematic review on integration in LMICs. From an initial list of 10 550 articles, 206 were selected for full-text review by two reviewers who independently reviewed articles and inductively extracted and synthesized themes related to health system preparedness. We identified five ‘context’ related categories and four health system ‘capability’ themes. The contextual enabling and constraining factors for frontline service integration were: (1) the organizational framework of frontline services, (2) health care worker preparedness, (3) community and client preparedness, (4) upstream logistics and (5) policy and governance issues. The intersecting health system capabilities identified were the need for: (1) sufficiently functional frontline health services, (2) sufficiently trained and motivated health care workers, (3) availability of technical tools and equipment suitable to facilitate integrated frontline services and (4) appropriately devolved authority and decision-making processes to enable frontline managers and staff to adapt integration to local circumstances. Moving beyond claims that integration is defined differently by different programs and thus unsuitable for comparison, this review demonstrates that synthesis is possible. It presents a common set of contextual factors and health system capabilities necessary for successful service integration which may be considered indicators of preparedness and could form the basis for an ‘integration preparedness tool’.
Keywords: Integration, health services, health system, assessment, low- and middle-income countries
Key Messages
Following a decade of highly targeted (mostly communicable) disease control efforts fuelled by global health initiatives, there is growing attention to, and support for the idea of more efficient and user-friendly integrated frontline services.
However, the variable focus and scope of integration efforts have made cumulative and comparative analysis difficult, hindering development of comprehensive guidance for integration planning.
Findings from this review identify five ‘contextual enablers’ and four ‘health system capabilities’ necessary for integration.
The review makes a substantive contribution by providing the basis for developing preparedness tools or similar to assess health system readiness for future service integration.
Introduction
Health service integration—what it is, and whether it is beneficial—has been the subject of intense debate among global health practitioners and policy makers for a number of decades. Advocates of service integration have pointed to the potential for financial, operational and logistical efficiencies that promote sustainability (Msuya 2005); improve service accessibility and equity (Jacobs et al. 2012) and strengthen quality of care via service continuity and a more person-centred approach (De Maeseneer et al. 2008). Others have argued that integration may in fact reduce access and quality of care through ‘watered down’ service platforms that lack focus or data with which to monitor and evaluate (Atun et al. 2008).
Various definitions of integration reveal a range of foci and rationales. Adopting a largely technocratic and process-focussed approach, UNAIDS defines integration as the joining together of different kinds of services or operational programmes in order to maximize outcomes (UNAIDS 2011). The President's Emergency Plan for AIDS Relief (PEPFAR) similarly defines integration as the organization, coordination and management of multiple activities and resources to ensure the delivery of more efficient and coherent services (Ryan 2011). Others have indicated the importance of defining integration in relation to the broader health system. Atun et al. (2010) for example defined integration as the assimilation of health interventions into each of the critical functions of a health system, including governance, financing, planning, service delivery, monitoring and evaluations and demand generation. Such definitions highlight the different levels (e.g. service, programme and policy) at which integration may take place but pay little attention to the way in which adopting or assimilating health services is influenced by the nature of the health system problem being addressed (e.g. access, equity or efficiency), the service or intervention and the unit of adoption.
Despite its intuitive appeal, evidence of the benefits of integration remains uncertain (Shigayeva et al. 2010). In part, this stems from the above noted variability in the focus and scope of integration efforts that make cumulative and comparative analysis difficult. Further compounding this variability however is the ‘limited experience in […] conducting systematic analysis of [integration] experiences’ (Grépin and Reich 2008). Lack of information on the impact of integration as well as the necessary pre-conditions for achieving it (including assessment of the health systems within which integration must occur), continue to hamper the ability of policy makers and programme implementers to prospectively assess how feasible or worthwhile integration may be. Lack of information about the pre-conditions necessary for implementing a successful integration programme is particularly problematic in low- and middle-income countries (LMICs), as health systems vary widely in terms of the capacity and readiness to adopt and assimilate new programs, services or interventions (Dudley and Garner 2011).
Planning health service integration requires adequate assessment and preparedness. In this systematic review, we sought to identify, examine and synthesize the evidence from studies in the literature reporting on health system assessment, preparedness and planning towards integration of health services. We sought to understand the contextual factors which facilitate or act as barriers to the preparation of LMIC health systems for integration of services. The aim of this review was to identify what health system factors are critical enablers of successful health service integration in LMIC settings.
Methods
Our approach was framed by an understanding of health systems as dynamic and adaptive, characterized by interdependent relationships and constellations of power both within and outside the system (Atun 2012). Against this backdrop, we adopted the principles of a realist review (Pawson et al. 2005). Realist reviews embrace the relevance of evidence from diverse sources and use an iterative process to build and refine theory to better answer research questions. Such an approach offers a way of synthesizing literature that evaluates complex social interventions, such as that focusing on identifying and understanding how certain processes operate in each context to produce program outcomes—both intended and unintended.
Therefore, we began this systematic review with a broad definition of integration of frontline health services that involves the adoption and assimilation of one health service with another. This definition encompassed a range of integration models—including assimilation of a specialist into a generalist service (e.g. integration of voluntary HIV testing into routine outpatient checks); harmonization of two stand-alone services into one integrated service (e.g. integration of TB and HIV testing, care and treatment) or bundling of a series of services into a new package of ‘integrated’ care (e.g. Integrated Management of Childhood Illness).
Despite a large number of published articles referring in some way to integrated service-delivery, early in this review process we found a dearth of empiric research with sufficient detail to be able to carry out a true realist synthesis. We thus adopted a modified systematic review incorporating aspects of realist review, setting broader methodological parameters for inclusion than are typical in a traditional systematic review and adapting the research question to focus on evidence of circumstances and implementation strategies that contribute to the perceived success of frontline health service integration in LMICs.
Search strategy
We searched Medline via Ovid, Web of Science and the Cochrane library using the following terms: ‘needs assessment’, ‘preparedness’, ‘assessment’, ‘planning’, ‘Delivery of Health Care’, ‘Comprehensive Health Care’, ‘Continuity of Patient Care’, ‘Primary Health Care’, ‘horizontal’, ‘vertical’, ‘coordination’ and a list of LMICs as defined by the World Bank. The terms were adapted from a previous systematic review on strategies for integrating health services in LMICs at the point of delivery (Dudley and Garner 2011).
Inclusion criteria
The review included both quantitative and qualitative studies assessing preparedness and capacity to implement or integrate specific integrated interventions; studies describing the planning or preparation for frontline service integration; studies primarily on integration outcomes but with some information on assessment and planning and studies describing tools to assess preparedness for service integration. The review only included studies conducted in LMICs and included literature between 1980 and June 2015.
Exclusion criteria
The review excluded studies on preparedness for emergency or pandemics, those focused exclusively on the introduction of a new drug or diagnostic or those on interventions not intended to become routine. Studies published prior to 1980 and studies published in a language other than English were excluded.
Data review and synthesis
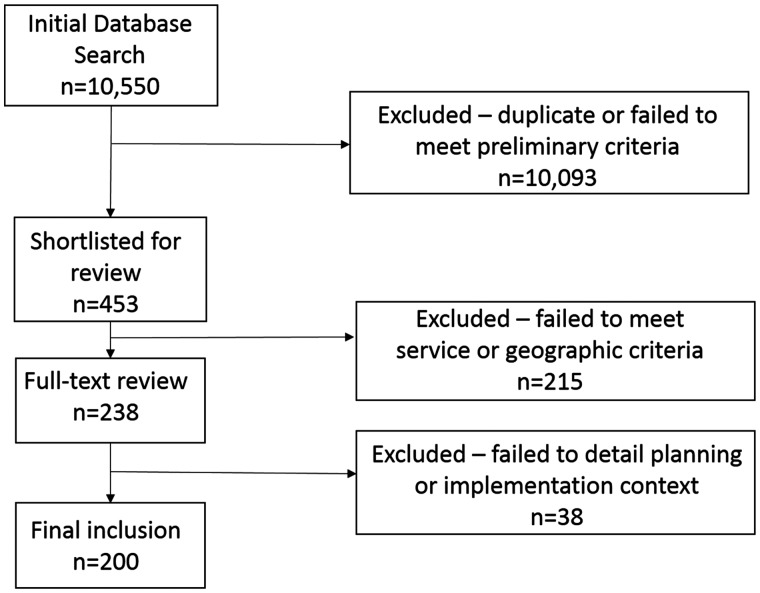
Application of the search terms during initial database searches yielded (after removal of duplicates) 6350 entries from Medline and an additional 4200 entries from Web of Science. Authors (blinded for peer review) independently reviewed titles and summaries against a criterion requiring only mention of health service integration in a LMIC. Independent selections were merged and compared and duplicates removed. Four hundred and forty-one articles were selected by both reviewers and retained; 36 articles that were identified by only one reviewer were discussed and consensus reached with 24 retained. Both reviewers independently reviewed the abstracts (where available) of short-listed articles against more explicit inclusion criteria, which required a description of the nature of the integration programme or intervention (e.g. the types of services being integrated and resourcing involved). The discordant selections were re-reviewed and discussed to reach consensus. Figure 1 illustrates the review process with 200 articles retained at the final stage. The reviewers independently synthesized and expounded on the themes of health system preparedness to produce summary descriptions which were consolidated and refined. Final interpretations were agreed upon after a final series of discussions among all the authors.
Figure 1.
Review cascade.
Data extraction and categorization
Data and insights were not uniformly reported and were thus extracted variously from the background material, description of methods, reported results and in interpretative reflections in the discussion section of different articles. A potential weakness of this methodology is that we sometimes relied on the perception of authors regarding which factors enabled or constrained their efforts to integrate health services. Hales et al. (2016) recently developed guidelines for reporting implementation and operational research, recommending that ‘contextual factors (i.e.) success factors, barriers and how they were overcome’ should be reported in the discussion section. Nonetheless, wherever located in an article, the extraction and inclusion of experiential (sometimes viewed as ‘anecdotal’) data included in this review is consistent with the realist approach to evidence synthesis reviews (Wong et al. 2013), which emphasizes a contextualized understanding of how and why interventions work, or not.
In line with our realist-informed approach, categorization of articles was also conducted inductively and in several stages. Following the general title and abstract review, a first level of categorization utilized the health system building blocks (WHO 2007) to identify and categorize five common themes in the literature relating to health system preparedness for integration. These themes were: (1) frontline service organization, (2) health care worker preparedness, (3) community and client preparedness, (4) upstream logistics and (5) policy and governance issues.
A second more nuanced synthesis took place as part of the final (full-text) review. This resulted in a sorting of evidence in the five ‘common themes’ according to four, inductively identified, cross-cutting health system capabilities, namely the need for: (1) frontline health services sufficiently functional to be able to deliver integrated services; (2) health care workers willing and capable of delivering integrated services; (3) technical tools and equipment sufficiently available and suitable to facilitate integrated frontline services and (4) decision-making processes appropriately devolved to facilitate delivery of integrated frontline services.
Findings
We present findings according to the four health system capabilities listed above. A summary matrix of the findings according to these capabilities and the five health system themes are summarized in Table 1. Systems for integrated services are often suboptimal in performance. In this presentation of findings, we were not able to cover in the narrative all the papers due to the large number of articles included in this review. Please see Table 1 for the complete list and categorization of all the studies included in this review.
Table 1.
Findings from a review of health system factors required to facilitate health service integration
| Essential capabilities for integration | Health system context enabling the capabilities for integration |
||||
|---|---|---|---|---|---|
| Service operations | Health workers | Community | Logistics | Policy | |
| Health services are sufficiently functional |
|
|
|
|
|
| Health care workers are willing and capable (polyvalent) |
|
|
|
|
|
| Technical tools are available and suitable to aid frontline service delivery |
|
|
|
|
|
| Decision-making processes are devolved |
|
|
|
|
|
Are health services sufficiently functional to deliver integrated services?
Some studies highlighted the importance of having sufficient and appropriate physical space within which to operate and deliver integrated services, especially with regard for patient privacy and smooth patient flow. Abera et al. (2014) assessed the knowledge, perceptions and willingness of health workers to deliver integrated mental health services in PHC settings in Ethiopia and identified the availability of appropriate space as a potential enabler of effective service integration. In a study by Mitashi et al. (2015) assessing the state of preparedness of PHC facilities in Democratic Republic of (DR) Congo for the integration of Human African Trypanosomiasis (HAT) diagnosis and treatment into routine PHC services, they identified that the recipient health service must be sufficiently functional in terms of physical space for service delivery. Njozing et al. (2011) and Topp et al. (2013) also identified, that although TB-HIV and HIV-outpatient co-location reduces patient waiting time and improved patient monitoring, inadequate space in the health facility limited the extent of service integration. Likewise, in their study to evaluate a policy in Ghana to integrate sexually transmitted infection (STI) services with existing family planning and maternal and child health services, Mayhew (2000) identified lack of sufficient space within health facilities to ensure privacy as a constraint on effective integration.
Another study was conducted in Kenya and Swaziland, assessing the impact on workload of integrating HIV services with sexual and reproductive health services. In the study, Sweeney et al. (2014) found that it was more likely for each health worker to take on more tasks in facilities with integrated use of physical space (i.e. where the range of services provided per room was increased as part of preparation for integration). Hermans et al. (2012) evaluated an intervention in which the service delivery space was reorganized to deliver integrated services in the form of an outdoor ‘One-Stop Shop’ TB–HIV clinic for attendees of an existing HIV clinic in Uganda. They found that this compact open-air setup allowed for easy communication and treatment continuity. The intervention led to improvements in TB treatment completion rate and reduction in deaths. In addition to space for service delivery, Chan et al. (2010) also identified the importance of space for the safe storage of medicines as enablers of the process of decentralizing HIV care from hospital to PHC facilities in Malawi.
Further, studies identified having sufficient numbers of health workers to manage the joint patient flow (including lay health workers) as a contextual enabler of service integration. Jiang et al. (2010) assessed a programme to integrate HIV/AIDS and STI control in four pilot provinces in China and identified the contextual features influencing implementation, one of which was insufficient human resources for HIV control and surveillance. Chan et al. (2010) identified the availability of medical assistants and/or nurses as a pre-requisite for integrating HIV care at PHC facilities in Malawi. Similarly, Nansera et al. (2010) found that the lack of health workers constrained the capacity of PHC facilities to integrate TB and HIV services in Uganda. One of the factors highlighted by Mitashi et al. (2015) as important for the preparedness of PHC facilities was the availability of health workers to deliver services. Harrington et al. (2012) also examined community preparedness to use family planning services among women accessing HIV treatment in Kenya and found that one of the barriers to service uptake was availability of health workers at the point of service, whether due to inadequate numbers or absenteeism. And when Mugala et al. (2010) examined barriers to incorporating and implementing HIV guidelines within the Integrated Management of Childhood Illness (IMCI) algorithm in Zambia, they found that due to workload, health workers prioritized conditions that they perceived or considered as important (e.g. potential emergencies) compared to HIV, suggesting the need for additional health workers at service delivery points to ensure effective integration of services.
Community trust in health services was another enabler of the capability of the existing system to deliver integrated services. Moran et al. (2012) developed and applied benchmark measures to quantitatively assess the readiness of LMICs to integrate and scale up newborn survival interventions, but found that factors such as the presence of a strong civil society and influence from community groups were as important although they require qualitative assessment. Mitashi et al. (2015) identified sufficient community trust in the health system as a contextual enabler of service integration. They found that community trust led to the uptake of frontline integrated PHC services, instead of bypassing these for (vertical) services at higher levels in the health system. Harrington et al. (2012) also found that community willingness to use integrated services (i.e. the use of HIV clinic as site of family planning services) in Kenya was due to convenience, familiarity (many felt like established regulars at the clinic) and provider expertize. However, they also found that the women who were seeking HIV services preferred trained clinicians, and that they do not trust volunteers and lay health workers to provide family planning services and to ensure confidentiality. And in an assessment of a community-based IMCI programme in Armenia, Thompson and Harutyunyan (2009) found that engaging clinicians already working in the community to serve as trainers of the lay health workers who would be involved in the programme demonstrated to the community that their clinicians were committed to the programme and had the additional benefit of providing the clinicians with richer perspective on community health. In a study of the performance of lay health workers delivering Integrated Community Case Management (iCCM) of malaria, pneumonia and diarrhoea in Uganda, Bagonza et al. (2014) found that community support was an important motivator of performance; a form of ‘intangible’ incentive for the lay health workers based on how the communities accept, cooperate with and appreciate services offered by health workers in their community.
Another essential component of health system functionality was having the logistical capacity to guarantee that drugs and equipment essential to integrated service-delivery was available. Mitashi et al. (2015) found that the poor provision of diagnostic tools for Trypanosomiasis constrained the successful integration of its diagnosis and treatment into routine PHC services in DR Congo. Munkhuu et al. (2009) also demonstrated that making onsite rapid diagnostic tests available (to replace laboratory referral for ante-natal syphilis screening) was a feasible strategy for integrating syphilis screening at the PHC level in Mongolia. Sibiya and Grainger (2007) also found that inadequate infrastructure and equipment to perform cervical screening constrained the integration of cervical screening with routine PHC services in rural (vs urban) health facilities in South Africa. Other studies in this category identified the importance of drug availability. Abera et al. (2014), in their assessment of health worker knowledge, perceptions and willingness to deliver integrated mental health services in PHC setting in Ethiopia, found that poor medication supply was an important challenge to effective integration. Lafort et al. (2003) assessed the integration of STI services into family planning clinics in Cote d'Ivoire and found that one of the constraints to integration was the lack of commodities, even though provision of STI drugs were integrated into existing procurement and distribution systems. In an economic modelling of the incremental cost of adding various interventions to existing maternal and child health days in Somalia, Vijayaraghavan et al. (2012) identified the need for logistical capacity to secure additional drugs and commodities for such integration of services.
In addition, Chan et al. (2010) found that the strategy for decentralization and integration of HIV services to the PHC level in Malawi required a strengthened supply chain to expand access to essential drugs and laboratory services. Nansera et al. (2010) also identified that stock availability limited provision of services as part of TB–HIV service integration in Uganda. Kayemba et al. (2012) evaluated the introduction of newborn care into iCCM in which patients were linked directly to the health facility from the community found that patients did not comply with referrals due to lack of medicines at the health facility. And in their study assessing a pilot integration of TB services with routine services at PHC facilities in Nepal, Onozaki and Shakaya (1995) found that there was low confidence in the PHC facilities without essential drugs and cold chain infrastructure. Bagonza et al. 2014 also identified drug availability is an independent predictor of good performance among lay health workers delivering iCCM of malarial, pneumonia and diarrhoea in Uganda. Lack of drugs meant their services were perceived by the community as irrelevant or unpopular, with negative effects on health workers’ motivation and performance.
Further, ensuring that services are sufficiently functional to deliver integrated services is linked to the level of government support. Lin et al. (2012) found that significantly increased detection of tuberculosis cases among patients with diabetes in China was enabled by a national policy (including locally relevant tools and guidance documents) to screen diabetes patients for tuberculosis. Efforts to integrate tuberculosis and HIV services in Uzbekistan, Tajikistan and Kyrgyzstan (Hausner et al. 2007) were facilitated by overarching policy to develop protocols, guidelines and training programmes with participation from high level stakeholders. Moran et al. (2012) found that having champions within the national government may be essential in efforts to integrate and scale up newborn survival interventions in LMICs; the authors emphasized that this was particularly the case where previously the same services had been separately planned and/or delivered. Jiang et al. (2010) also assessed a programme to integrate HIV/AIDS and STI control in China and found that one of the enablers of integration was the strong and detailed policy framework provided by the national government to guide implementation. More specifically, some studies highlighted the need for policies authorizing integrative actions at the frontline (e.g. Shelley et al. 2014; Kouam et al., 2014) and policies enabling financing mechanisms that support service integration (e.g. Sheiman and Shevski 2014; Uwimana and Jackson 2013). However, the capacity of government policy to facilitate integration may be constrained—a study by Shayo et al. (2013) found that a constraint to the effective integration of PMTCT services within PHC in Tanzania was the limited bottom-up feedback into planning decisions due to the overbearing involvement of global health agencies in decision-making.
Are health workers and managers willing and able to provide integrated services?
The second category of capabilities for integration is the willingness and ability of the health workforce to provide integrated services. Lin et al. (2012) found that training and assigning special staff to screen and record data and that supervision and site visits by local health managers strengthened the performance of a programme incorporating TB screening into diabetes treatment services in China. Conversely, Nsona et al. (2012) identified that weak supervision and monitoring of community based health workers limited the scale up of iCCM in Malawi. Abera et al. (2014) identified the need for ongoing supervision as one of the perceived challenges for integration of mental health into primary health care in Ethiopia. In an evaluation of the performance of lay health workers delivering iCCM of malaria, pneumonia and diarrhoea services in Uganda, Bazonga et al. (2014) found that receiving feedback in the form of supportive supervision from health workers in the facilities to which their work was linked was a predictor of good performance among lay health workers. Birdthistle et al. (2014) highlighted the importance of peer support by including mentoring (by more experienced health workers) as part of their intervention to train health workers to integrate HIV services delivery with existing maternal and child health services.
Abera et al. (2014) found that willingness of health workers to deliver integrated services is another potential challenge. This was linked to concerns about increased workload and competency requirements given that health workers perceive that brief stand-alone in-service training in mental health was likely insufficient. However, in a study assessing the feasibility of one-stop ante-natal syphilis testing in Mongolia, Munkhuu et al. (2009) found that in spite of increased workload occasioned by the use of rapid diagnostic tests for syphilis, the health workers were still willing to provide the services because of the clear benefits to their patients: reduction in costs as patients did not need to travel elsewhere for syphilis screening as part of their ante-natal care. Examining the link between workload and the integration of HIV services with sexual and reproductive health services in Kenya and Swaziland, Sweeney et al. (2014) found that there was no overall relationship between integration and workload at the facility level, and that to the contrary, workload may significantly reduce with integrated services, highlighting the potential for more efficient use of capacity with integration. However, Moran et al. (2012) and Topp et al. (2013) identified how the disposition of health workers, including facility managers, can influence the readiness and ease with which new tasks are introduced. Hermans et al. (2012) found that the formation of a dedicated team of health care workers who were convinced of the need for integrated care was paramount to the success of the intervention to integrate TB and HIV services in Uganda. Likewise, Mayhew (2000) found in Ghana that disrespectful and abusive care by health workers limited the efforts to integrate STI services with family planning and maternal and child health services. Indeed, some of these studies highlighted duty allocation and team dynamics as being important for the willingness of health workers to deliver integrated services (e.g. Hanson et al. 2014; Sweeney et al. 2014).
While the willingness of health workers to deliver integrated services was important, so was the need to possess the skills to do so, with adequate training and opportunity to practice the new skills (including the use of new algorithms and diagnostics). In a study to identify the opportunities and barriers in efforts to implement integrated TB and HIV care at the PHC level in Uganda, Nansera et al. (2010) found that gaps in the knowledge of health workers (on TB in children and HIV care generally) limited the delivery of integrated services. Mitashi et al. (2015) showed that having polyvalent health workers was a prerequisite for integrating the diagnosis and treatment of Trypanosomiasis into routine PHC services in DR Congo. Kayemba et al. (2012) found that sub-optimal training and skills of lay health workers limited the introduction of newborn care into an existing iCCM programme in Uganda. Similarly, Byamungu and Ogbeiwi (2002) also found that low quality of training and skills of health workers (which showed with higher levels of task complexity) limited the effective integration of leprosy services at the PHC level in DR Congo.
In a study of the integration of diabetes care with other PHC services in the Philippines, Ku and Kegels (2014) found it essential to include in-service training to improve health workers’ familiarity and competence with diabetes. Chan et al. (2010) also found that in-service training of health workers was an important contextual enabler of the decentralization and integration of HIV care at the PHC level, but effects of the training were limited due to rapid turnover of health workers and managers. Some studies highlight the effects of posting and transfer of health workers on turnover and skills retention as an important constraint to effective service integration (e.g. Sodhi et al. 2014; Uwimana and Jackson 2013).
Furthermore, Chaudhary et al. (2005) evaluated the in-service training of health workers to provide IMCI at various time points after training and follow up in India. They found that follow-up after training improved performance of both health workers and supervisors. They also found that longer gaps between supervision were associated with poor performance, and that gaps between the in-service training and work environment was partly responsible for sub-optimal performance. Also, policies linking in-service training to continuous professional development accreditation promote in-service training (Sodhi et al. 2014). Topp et al. (2013) additionally noted that frequent transfers of health workers between integrated and non-integrated facilities undermined the efficacy of such in-service training. But beyond episodic and ad hoc in-service training with its inherent weakness to prepare health workers for service integration, other studies highlighted the importance of having national policy to ensure pre-service training rather than the adhoc in-service training. In a survey of health workers conducted to assess the feasibility of integrating mental health into PHC in Ethiopia, Abera et al. (2014) found that knowledge about mental disorder diagnoses, symptoms and treatments was generally low, but that health workers with higher levels of pre-service general health training (degree vs diploma) and pre-service clinical exposure to mental health care were associated with more favourable attitudes towards delivering mental health care. Byamungu and Ogbeiwi (2002) also found that in-service training for health workers was inadequate to ensure the skills for service delivery when leprosy diagnosis and treatment was transferred to PHC facilities. Instead, services with higher levels of task complexity continued to be provided in many PHC facilities by health workers who had been previously received pre-service training to provide vertical leprosy services.
Linked to the requirement for training, is the need to maintain technical skills once gained; and this may require sufficient disease prevalence or clinical cases for health workers to maintain their technical skill. In a pilot study to assess the feasibility of integrating TB services with routine services at PHC facilities in Nepal, Onozaki and Shakaya (1995) found that it was difficult to maintain the technical skill of health workers when the number of specimens to use in TB diagnosis was small. They recommended a rethink of integration when service uptake is low and perhaps to only integrate services in higher uptake sites which can be used as referral facilities for lower uptake ones. Mitashi et al. (2015) in their study assessing the preparedness of PHC facilities in DR Congo to integrate the diagnosis and treatment of Trypanosomiasis into routine PHC services, identified the need to have sufficient disease prevalence to ensure that technical competence is maintained over time. Similarly, in an economic evaluation of the integration of family planning services into existing HIV services, Shade et al. (2013) found that larger health facilities (defined based on the number of HIV-infected women currently enrolled) enjoyed substantial economies of scale and were therefore more cost-effective. Cost per woman decreased more with increasing clinic size. The cost per additional woman using more effective family planning also decreased more with increasing clinic size. And the fixed costs were personnel and training costs and physical reorganization of health facility to facilitate integration. But on the other hand, recurring costs included training costs, notably when there was >40% staff turnover in a health facility, costs of supplies and materials. These findings further strengthen the argument against integration when service uptake is low, and where the challenge of rapid staff turnover is common.
Are technical tools available and suitable to aid frontline service delivery?
Studies frequently identified the importance of having or creating new and manageable clinical algorithms and decision making tools to aid health workers in the delivery of integrated services. Lin et al. (2012), for example, found that the creation of tools for tuberculosis symptoms screening and referral (in addition to existing diabetes tools) facilitated a significant increase in the detection of tuberculosis cases among patients with diabetes in China. Hausner et al. (2007) highlighted that the formation of new data collection tools and an electronic surveillance database facilitated efforts in Uzbekistan, Tajikistan and Kyrgyzstan to integrate tuberculosis and HIV services. Likewise, Nsona et al. (2012) found that provision and use of a job aid specifying algorithms for diagnosis and care by PHC workers facilitated the scale up of iCCM in Malawi. In a study on the integration of diabetes care with other PHC services in the Philippines, Ku and Kegels (2014) found the provision of decision tools during and after in-service training of health workers was essential for service integration. In addition to algorithms, Jiang et al. (2010) highlighted the potential for data collection and decision-making tools that minimize duplication of effort and reduce the impression of increased workloads in China, to provide an incentive for frontline health workers and managers to adopt integrated practices. These tools require information technology capability, and the existence of job aids and data tools may signal or require high level support.
Are decision-making processes for integrated services sufficiently devolved?
The fourth capability that is essential for successful integration of services relates to the devolution of decision-making processes. Lindgren et al. (2011) highlighted the need for local (i.e. district) government capacity to assess demand for and reorganize services in rural Malawi through mobile clinics providing HIV testing and treatment referral; ante-natal care, diagnosis and treatment of malaria; sputum collection for TB screening and diagnosis and treatment of sexually transmitted and opportunistic infections. Ku and Kegels (2014) also found that strong local (i.e. district) government support for a project to integrate diabetes care with other PHC services in the Philippines and decision space of sub-national health managers led to local policies being adopted beyond the scope of the project. Several, including Moran et al. (2012), highlighted that it is essential for national champions to create the policy space necessary for sub-national and facility managers to adapt newborn services for integration and scale up in LMICs. It is therefore important to have or develop a national policy or culture that enables sub-national decision making supportive of integration.
In a study to evaluate a policy in Ghana to integrate STI services with existing family planning and maternal and child health services, Mayhew (2000) identified as an important constraint on effective integration unclear government policy on what mid-level health workers (i.e. nurses) could do. Although the integration policy guidelines allow nurses to prescribe antibiotics to treat patients with STIs, doctors continued to expect nurses to refer patients to them for treatment at higher level health facilities, instead of initiating treatment at the PHC level. Another way in which the decision space for service providers may be limited is an overbearing involvement of international agencies in decision-making. Shayo et al. (2013) examined the challenge of bottom-up feedback into planning decisions (to ensure integration of PMTCT services within PHC in Tanzania) in a decentralized health system funded by an international donor agency. They found that higher levels of government (in a decentralized system) meddle in local input in planning because of their perception that planning is the responsibility of donors who leave limited decision space for local decision makers, such that there is little space to modify the programme according to the judgement and needs health workers (and in response to community needs); people who are closest to implementation and with the most relevant information.
Similar to how community trust is an enabler of functional health services, decision-making processes for service integration also requires community engagement. Indeed, community involvement in service planning is a vital contextual enabler of service integration at the PHC level. Lindgren et al. (2011) identified the importance of community engagement in the governance of a mobile clinic intervention designed to provide integrated HIV services in Malawi. The participation of existing village health committee members and other community leaders (in selecting intervention sites and organizing service delivery) was important for effective service integration and uptake. Likewise, Nsona et al. (2012) found that creating and engaging with village health committees through community dialogues and their ownership of the iCCM agenda in their communities helped facilitate the initiation, implementation and sustainability of the programme in Malawi. The village health committees supported the PHC workers who were specifically trained to implement the programme and were posted to participating communities. Committee members took responsibility for establishing housing for the health workers, identified the location of the village health clinics, assisted in constructing the buildings and in managing service delivery, including monitoring of drug supplies. Some studies also highlight the important role of community engagement in planning integrated services as it can help address previous fears, myths and misconceptions about diseases and their treatment that could undermine integration (e.g. Hanlon et al. 2014; Wallace et al. 2014).
Moran et al. (2012) highlighted that the presence of a strong civil society and the influence of community groups was important for facilitating and scaling up the integration of newborn services at the PHC level. Kayemba et al. (2012) found that integrating newborn care within the existing iCCM programme in Uganda was facilitated by community support for health workers. The community members helped the lay health workers by identifying new mothers in the community, providing transportation support and giving donations to the lay health workers involved in service delivery.
Coordination of operations among health system managers (including both local and international non-government officials) can influence the extent to which devolved decision-making can support effective service integration. Sibiya and Grainger (2007) found that weak follow-up arrangements and feedback from referral clinic limited the effective integration of cervical screening with other PHC services. Nsona et al. (2012) found that coordination of operations between district and national health managers and with international NGO officials was essential for rolling out service integration activities in the intervention districts as part of efforts to scale up of iCCM in Malawi. In their assessment of a pilot programme to integrate HIV and STI control in four provinces in China, Jiang et al. (2010), found that coordination among health system managers along the chain of decentralized governance (from the central, provincial, prefecture to the county levels) was necessary to ensure frontline service delivery. Njozing et al. (2011) also found, in a study assessing TB–HIV co-location in Cameroon, that integration was facilitated by team work among health workers, especially when the same manager was in charge of the two co-located services (or when that was not the case, by both teams having a joint committee that holds regular meetings to facilitate cross-referrals). Shayo et al. (2013) identified that the integration of PMTCT services within PHC in Tanzania was limited by poor collaboration among health managers at different levels of decentralized government and international NGO operations. This was in part because the health managers with the power to make the most important decisions were far removed from local communities and health facilities.
Discussion
In this review, we identified a broad range of capabilities and contextual enablers and constraints influencing frontline health service integration in LMICs. These findings were synthesized into five contextual enablers or constrainers, and four capability themes, summarized in Table 2. Mapping against traditional health systems building blocks or functions, contextual enablers and constrainers were categorized as: (1) the organizational characteristics of frontline services, (2) health care worker preparedness, (3) community and client preparedness, (4) upstream logistics and (5) policy and governance issues. Major health system capabilities necessary for ensuring the success of health service integration included the availability of already functional frontline health services; sufficiently trained and motivated health care workers; the availability of technical tools and equipment suitable to facilitate integrated services, and finally, appropriately devolved authority and decision-making processes to enable local adaptation.
Table 2.
Summary findings from review of health system enablers and barriers to health service integration
 |
Colours/shades indicate the number of reviewed articles providing evidence of each theme. Please see online for colour table.
Several existing reviews have examined health service decentralization and identified factors that contribute to successful integration (e.g. Atun et al. 2010; Dudley and Garner 2011; Legido-Quigley et al. 2013; Watt et al. 2017). The findings reported here may be differentiated from previous work in several ways. First, in this review we did not limit the search to examples of health service integration related to a specific disease(s) (e.g. HIV). Rather, we synthesized findings from literature covering all types of health service integration in any low- and middle-income setting. Adopting this broader scope was important, since disease-specific interventions and their evaluations often occur within chronological, institutional or geographical ‘bubbles’ where critical reflection on prevailing norms and implementation practices may be limited. By comparing evidence of health service integration spanning several decades of efforts in maternal and child health, neglected tropical diseases, outpatient, HIV, malaria and other frontline services, this review thus produces a more comprehensive synthesis of the health system pre-conditions necessary to enable health services integration of any type, in LMIC settings.
A second distinguishing feature of this review was our use of a realist-informed methodology. Existing reviews have tended to be conducted within a positivist paradigm with the aim of identifying generalizable evidence that controls for contextual factors. Such methods limit readers’ ability to reflect on ‘real world’ factors that have contributed to, or inhibited the success of efforts to integrate health services; all the more so, since in the reviewed literature, authors are often keen to demonstrate the impact of health service integration efforts, rather than to discuss reasons and contextual factors that influenced the outcomes. Adopting realist principles required us to engage with a diverse literature, including different types of integration studies—from experimental to implementation science studies and from prospective to retrospective evaluations—and different forms of evidence. This approach allowed us to move beyond the unhelpful characterizations of the extensive integration literature as being too diverse to enable meaningful synthesis.
As summarized in Table 2, which maps the number of articles supporting each sub-theme, comparatively more articles reflected on the intuitive need for material and instrumental aspects of health system preparedness particularly the role of health worker training and supervision, clinical guidelines and the availability of drugs and other technologies. Investment in the training of health workers to adopt new tasks and use new clinical tools and guidelines were mentioned in 58 articles. Yet consideration of other, important but relational aspects of health worker preparedness, such as the management of health worker transfers that impact on frontline service capacity, was less common. This relative emphasis on preparatory actions related to the most tangible aspects of a health system likely reflects policy makers’, program implementers’ and researchers’ preference for investing in areas that are more visible, and those considered easier to improve in the context in which many health service integration efforts are implemented—namely, short-term, disease-specific, donor-funded interventions.
This review also highlights several less-well recognized contextual factors and capabilities important to enabling health service integration. At the ‘macro’-level findings highlight the role that policy plays by enabling decisions and actions by mid- and lower-level health service actors. A large proportion of reviewed articles focused on instrumental aspects of policy, such as the need to develop nationally approved technical tools, clinical guidelines and information systems. But a subset of the literature underscored the value of strategic policy actions such as developing pre-service training packages to reduce the need for (time consuming, expensive and often ineffective) in-service workshops, or developing national or sub-national policies that explicitly encourage health service integration. A small group of articles additionally highlighted the importance of policy and managerial actions that enable devolved decision making at the micro-level as a pre-requisite for iterative adaptations and community consultations that typically underpin locally appropriate service models.
Following a decade of highly targeted, mostly communicable disease control efforts fuelled and driven by the investment of global health initiatives, there is growing attention to, and support for the idea of integrated frontline services that are more efficient and user friendly. Despite the manifest weaknesses in many LMIC health systems, however, less attention has been paid to the conditions necessary to establish and sustain such services. This review draws on evidence from across different geographies and countries and presents the first comprehensive synthesis of health system enablers and barriers to health service integration in low-income settings. Indeed, the findings presented here may be considered the basis for developing a set of indicators or an assessment tool for integration preparedness. Each of the five ‘context’ categories intersecting with four ‘capabilities’ generates a question that should be considered in future research and implementation efforts to assess, prepare and evaluate health service integration efforts.
For example, depending on context, ‘willing and capable health workers’ may include an indicator to capture whether the service to be integrated is sufficient to maintain the clinical skill of health workers. Similarly, a program implementer may ensure there is community engagement in planning and delivering integrated service to ensure trust. The same indicators could be used to better evaluate why integration is successful (or not)—potentially contributing to the development of more robust theory of health service integration in the process. In this way, findings presented in this review can potentially minimize the risk that policy makers and program implementers will overlook the need to ensure health system preparedness and provide a useful tool for minimizing unintended negative consequences that can arise from efforts to integrate health services which may enhance efforts to assess and prepare health systems for health service integration.
Conclusion
In summary, this review provides a synthesis of both research evidence and experiential knowledge on how a range of system ‘capabilities’ necessary for health service integration interact with contextual enablers or constrainers to influence the success or otherwise of efforts to integrate health services. By highlighting the cross-cutting enablers of short- and longer-term success, the findings highlight both the intuitive and the less obvious components of health system preparedness for health service integration. The synthesized findings of this review highlight both structural and relational enablers and constraints of service integration and could provide the basis for designing a tool for evaluating health systems prior to integration design or implementation.
Funding
No funding was received for this work. R.J. is funded by a Future Leader Fellowship funded by the Australian National Heart Foundation (APP100484).
Supplementary Data
Supplementary data are available at Health Policy and Planning Online.
Conflict of interest statement. None declared.
Supplementary Material
References
- Abera M, Tesfaye M, Belachew T, Hanlon C.. 2014. Perceived challenges and opportunities arising from integration of mental health into primary care: a cross-sectional survey of primary health care workers in south-west Ethiopia. BMC Health Services Research 14: 113.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atun RA, Bennett S, Duran A.. 2008. Policy Brief. When Do Vertical (Stand-Alone) Programmes Have a Place in Health Systems? Copenhagen: World Health Organization Regional Office for Europe; http://www.euro.who.int/document/hsm/5_hsc08_ePB_8.pdf, accessed 20 October 2017. [Google Scholar]
- Atun R, de Jongh T, Secci F, Ohiri K, Adeyi O.. 2010. A systematic review of the evidence on integration of targeted health interventions into health systems. Health Policy and Planning 25: 1–14. [DOI] [PubMed] [Google Scholar]
- Atun R. 2012. Health systems, systems thinking and innovation. Health Policy and Planning 27: iv4–8. [DOI] [PubMed] [Google Scholar]
- Bagonza J, Kibira SP, Rutebemberwa E.. 2014. Performance of community health workers managing malaria, pneumonia and diarrhoea under the community case management programme in central Uganda: a cross sectional study. Malaria Journal 13: 367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barker C, Turshen M.. 1986. ‘ Primary health care or selective health strategies’. Review of African Political Economy 13: 78–85. [Google Scholar]
- Birdthistle IJ, Mayhew SH, Kikuvi J. et al. 2014. Integration of HIV and maternal healthcare in a high HIV-prevalence setting: analysis of client flow data over time in Swaziland. BMJ Open 4: e003715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byamungu DC, Ogbeiwi OI.. Integrating leprosy control into general health service in a war situation: the level after 5 years in eastern Congo. Leprosy Review 74: 68–78. [PubMed] [Google Scholar]
- Chan AK, Mateyu G, Jahn A. et al. 2010. Outcome assessment of decentralization of antiretroviral therapy provision in a rural district of Malawi using an integrated primary care model. Tropical Medicine and International Health 15: 90–7. [DOI] [PubMed] [Google Scholar]
- Chaudhary N, Mohanty PN, Sharma M.. 2005. Integrated management of childhood illness (IMCI) follow-up of basic health workers. Indian Journal of Pediatrics 72: 735–9. [DOI] [PubMed] [Google Scholar]
- Collins PY, Insel TR, Chockalingam A, Daar A, Maddox YT.. 2013. Grand challenges in global mental health: integration in research, policy, and practice. PLoS Medicine 10: e1001434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Maeseneer J, van Weel C, Egilman D. et al. 2008. Strengthening primary care: addressing the disparity between vertical and horizontal investment. The British Journal of General Practice 58: 3–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dudley L, Garner P.. 2011. Strategies for integrating primary health services in low- and middle-income countries at the point of delivery. The Cochrane Database of Systematic Reviews CD003318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grépin KA, Reich MR.. 2008. Conceptualizing integration: a framework for analysis applied to neglected tropical disease control partnerships. PLoS Neglected Tropical Diseases 2: e174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hales S, Lesher-Trevino A, Ford N. et al. 2016. Reporting guidelines for implementation and operational research. Simplein of the World Health Organization 94: 58–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanlon C, Luitel NP, Kathree T. et al. 2014. Challenges and opportunities for implementing integrated mental health care: a district level situation analysis from five low- and middle-income countries. PLoS One 9: e88437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrington EK, Newmann SJ, Onono M. et al. 2012. Fertility intentions and interest in integrated family planning services among women living with HIV in Nyanza Province, Kenya: a qualitative study. Infectious Disease in Obstetrics and Gynecology 2012: 809682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hausner DS, Kulsharova M, Seledtsov V, Khodakevich L, Deryabina A.. 2007. Facilitating interaction between TB and AIDS medical services for better management of patients with co-infections. Global Public Health 2: 140–54. [DOI] [PubMed] [Google Scholar]
- Hermans SM, Castelnuovo B, Katabira C. et al. 2012. Integration of HIV and TB services results in improved TB treatment outcomes and earlier, prioritized ART initiation in a large urban HIV clinic in Uganda. Journal of Acquired Immune Deficiency Syndromes (1999) 60: e29–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobs B, Ir P, Bigdeli M, Annear PL, Van Damme W.. 2012. Addressing access barriers to health services: an analytical framework for selecting appropriate interventions in low-income Asian countries. Health Policy Plan 27: 288–300. [DOI] [PubMed] [Google Scholar]
- Jiang Z, Wang DB, Yang S. et al. 2010. Integrated response toward HIV: a health promotion case study from China. Health Promotion International 26: 196–211. [DOI] [PubMed] [Google Scholar]
- Kayemba CN, Sengendo HN, Ssekitooleko J. et al. 2012. Introduction of Newborn Care within Integrated Community Case Management in Uganda. The American Journal of Tropical Medicine and Hygiene 87: 46–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerschberger B, Hilderbrand K, Boulle AM. et al. 2012. The effect of complete integration of HIV and TB services on time to initiation of antiretroviral therapy: a before-after study. PLoS One 7: e46988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim JY, Farmer P, Porter ME.. 2013. Redefining global health-care delivery. Lancet 382: 1060–9. [DOI] [PubMed] [Google Scholar]
- Kouam CE, Delisle H, Ebbing HJ. et al. 2014. Perspectives for integration into the local health system of community-based management of acute malnutrition in children under 5 years: a qualitative study in Bangladesh. Nutrition Journal 13: 22.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ku GMV, Kegels G.. 2014. Integrating chronic care with primary care activities: enriching healthcare staff knowledge and skills and improving glycemic control of a cohort of people with diabetes through the First Line Diabetes Care Project in the Philippines. Global Health Action 7: 25286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lafort Y, Sawadogo Y, Delvaux T, Vuylsteke B, Laga M.. 2003. Should family planning clinics provide clinical services for sexually transmitted infections? A case study from Côte d’Ivoire. Tropical Medicine and International Health 8: 552–60. [DOI] [PubMed] [Google Scholar]
- Legido-Quigley H, Montgomery CM, Khan P. et al. 2013. Integrating tuberculosis and HIV services in low- and middle-income countries: a systematic review. Tropical Medicine and International Health 18: 199–211. [DOI] [PubMed] [Google Scholar]
- Li L, Lin Y, Mi F. et al. 2012. Screening of patients with tuberculosis for diabetes mellitus in China. Tropical Medicine and International Health 17: 1294–301. [DOI] [PubMed] [Google Scholar]
- Lindgren TG, Deutsch K, Schell E. et al. 2011. Using mobile clinics to deliver HIV testing and other basic health services in rural Malawi. Rural Remote Health 11: 1682. [PubMed] [Google Scholar]
- Mayhew SH. 2000. Integration of STI services into FP/MCH services: health service and social contexts in rural Ghana. Reproductive Health Matters 8: 112–24. [DOI] [PubMed] [Google Scholar]
- Mitashi P, Hasker E, Mbo F. et al. 2015. Integration of diagnosis and treatment of sleeping sickness in primary healthcare facilities in the Democratic Republic of the Congo. Tropical Medicine and International Health 20: 98–105. [DOI] [PubMed] [Google Scholar]
- Moran AC, Kerber K, Pfitzer A. et al. 2012. Benchmarks to measure readiness to integrate and scale up newborn survival interventions. Health Policy and Planning 27: iii29–39. [DOI] [PubMed] [Google Scholar]
- Mugala N, Mutale W, Kalesha P, Sinyinza E.. 2010. Barriers to implementation of the HIV guidelines in the IMCI algorithm among IMCI trained health workers in Zambia. BMC Pediatrics 10: 93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munkhuu B, Liabsuetrakul T, Chongsuvivatwong V, McNeil E, Janchiv R.. 2009. One-stop service for antenatal syphilis screening and prevention of congenital syphilis in Ulaanbaatar, Mongolia: a cluster randomized trial. Sexually Transmitted Diseases 36: 714–20. [DOI] [PubMed] [Google Scholar]
- Murray et al. 1999. A WHO Framework for Health Systems Performance Assessment http://www.who.int/healthinfo/paper06.pdf, accessed 22 October 2017.
- Msuya J. 2005. Horizontal and Vertical Delivery of Health Services: What Are the Tradeoffs? Washington, DC: World Bank. [Google Scholar]
- Nansera D, Bajunirwe F, Kabakyenga J, Asiimwe PKJ, Mayanja-Kizza H.. 2010. Opportunities and barriers for implementation of integrated TB and HIV care in lower level health units: experiences from a rural western Ugandan district. African Health Science 10: 312–9. [PMC free article] [PubMed] [Google Scholar]
- Njozing BN, Edin KE, Sebastián MS, Hurtig AK.. 2011. Voices from the frontline: counsellors’ perspectives on TB/HIV collaborative activities in the Northwest Region, Cameroon. BMC Health Services Research 11: 328.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nsona H, Mtimuni A, Daelmans B. et al. 2012. Scaling up integrated community case management of childhood illness: update from Malawi. The American Journal of Tropical Medicine and Hygiene 87: 54–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Onozaki I, Shakya TM.. 1995. Feasibility study of a district tuberculosis control programme with an 8-month short-course chemotherapy regimen utilizing the integrated health service network under field conditions in Nepal. Tubercle and Lung Disease 76: 65–71. [DOI] [PubMed] [Google Scholar]
- Patel V, Belkin GS, Chockalingam A. et al. 2013. Grand challenges: integrating mental health services into priority health care platforms. PLoS Medicine 10: e1001448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pawson R, Greenhalgh T, Harvey G, Walshe K.. 2005. Realist review–a new method of systematic review designed for complex policy interventions. Journal of Health Services Research and Policy 10: 21–34. [DOI] [PubMed] [Google Scholar]
- Ryan C. 2011. “The Continuum of Response. PEPFAR’s Use of Integration as a Tool to Improve the Health of Mothers and Children, Build Stronger Health Systems, and Reduce HIV Incidence” http://www.aidstar-one.com/sites/default/les/Ryan_Integration_3_Addis.pdf, accessed 22 October 2017.
- Sen K, Koivusalo M.. 1998. Health care reforms in developing countries. International Journal of Health Planning and Management 13: 199–215. [DOI] [PubMed] [Google Scholar]
- Shade SB, Kevany S, Onono M. et al. 2013. Cost, cost-efficiency and cost-effectiveness of integrated family planning and HIV services. AIDS 27(Suppl 1): S87–92. [DOI] [PubMed] [Google Scholar]
- Shayo EH, Mboera LE, Blystad A.. 2013. Stakeholders’ participation in planning and priority setting in the context of a decentralised health care system: the case of prevention of mother to child transmission of HIV programme in Tanzania. BMC Health Services Research 13: 273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheiman I, Shevski V.. 2014. Evaluation of health care delivery integration: the case of the Russian Federation. Health Policy 115: 128–37. [DOI] [PubMed] [Google Scholar]
- Shelley D, Nguyen L, Pham H, VanDevanter N, Nguyen N.. 2014. Barriers and facilitators to expanding the role of community health workers to include smoking cessation services in Vietnam: a qualitative analysis. BMC Health Services Research 14: 606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shigayeva A, Atun R, McKee M, Coker R.. 2010. Health systems, communicable diseases and integration. Health Policy and Planning 25(Suppl 1): i4–20. [DOI] [PubMed] [Google Scholar]
- Sibiya MN, Grainger L.. 2007. An assessment of the implementation of the provincial cervical screening programme in selected Primary Health Care Clinics in the Ilembe Region, KwaZulu-Natal. Curationis 30: 48–55. [DOI] [PubMed] [Google Scholar]
- Sodhi S, Banda H, Kathyola D. et al. 2014. Supporting middle-cadre health care workers in Malawi: lessons learned during implementation of the PALM PLUS package. BMC Health Services Research 14: S8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sweeney S, Obure CD, Terris-Prestholt F; Integra Research Team et al. 2014. The impact of HIV/SRH service integration on workload: analysis from the Integra Initiative in two African settings. Human Resources for Health 12: 42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson ME, Harutyunyan TL.. 2009. Impact of a community-based integrated management of childhood illnesses (IMCI) programme in Gegharkunik, Armenia. Health Policy and Planning 24: 101–7. [DOI] [PubMed] [Google Scholar]
- Topp SM, Chipukuma JM, Chiko MM. et al. 2013. Integrating HIV treatment with primary care outpatient services: opportunities and challenges from a scaled-up model in Zambia. Health Policy and Planning 28: 347–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Unger J-P, Paepe P, Green A.. 2003. A code of best practice for disease control programmes to avoid damaging health care services in developing countries. International Journal of Health Planning and Management 18: S27–39. [DOI] [PubMed] [Google Scholar]
- Uwimana J, Jackson D.. 2013. Integration of tuberculosis and prevention of mother-to-child transmission of HIV programmes in South Africa. The International Journal of Tuberculosis and Lung Disease 17: 1285–90. [DOI] [PubMed] [Google Scholar]
- Vijayaraghavan M, Wallace A, Mirza IR. et al. 2012. Economic evaluation of a Child Health Days strategy to deliver multiple maternal and child health interventions in Somalia. The Journal of Infectious Diseases 205(Suppl 1): S134–40. [DOI] [PubMed] [Google Scholar]
- Wallace A, Kimambo S, Dafrossa L. et al. 2014. Qualitative assessment of the integration of HIV services with infant routine immunization visits in Tanzania. Journal of Acquired Immune Deficiency Syndromes (1999) 66: e8–e14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walsh JA, Warren KS.. 1979. Selective primary health-care—interim strategy for disease control in developing-countries. New England Journal of Medicine 301: 967–74. [DOI] [PubMed] [Google Scholar]
- Watt N, Sigfrid L, Legido-Quigley H. et al. 2017. Health systems facilitators and barriers to the integration of HIV and chronic disease services: a systematic review. Health Policy and Planning doi: 10.1093/heapol/czw149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong G, Greenhalgh T, Westhorp G, Buckingham J, Pawson R.. 2013. RAMESES publication standards: realist syntheses. BMC Medicine 11: 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. (2007). Everybody’s Business: Strengthening Health Systems to Improve Health Outcomes: WHO’s Framework for Action. Geneva: World Health Organization. [Google Scholar]
- World Health Organization. (2008). Integrated Health Services—What and Why? Technical Brief No 1, 2008 http://www.who.int/healthsystems/service_delivery_techbrief1.pdf, accessed 22 October 2017.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.