Abstract
The objective of this article is to assess the extent and determinants of switching delivery location between women’s first and second deliveries. We used Demographic and Health Survey data from 39 low- and middle-income countries on delivery locations from >30 000 women who had their first two deliveries in the 5-year survey recall period. Each delivery was characterized as occurring at home or in a health facility, facilities were classified as public- or private-sector. The extent of switching was estimated for each country, region and overall. Multivariable logistic regression models assessed determinants of switching (home to facility or facility to home), using four dimensions (perceived/biological need, socioeconomic characteristics, utilization of care and availability of care). Overall, 49.0% of first and 44.5% of second deliveries occurred in health facilities. Among women who had their first delivery at home, 11.8% used a facility for their second (7.0% public-sector and 4.8% private-sector). Among women who had their first delivery in a facility, 21.6% switched to a home location for their second. The extent of switching varied by country; but the overall net effect was either non-existent (n = 20) or away from facilities (n = 17) in all but two countries—Cambodia and Burkina Faso. Four factors were associated with switching to a facility after a home delivery: higher education, urban residence, non-poor household status and multiple gestation. Majority of women consistently used the same delivery location for their first two deliveries. We found some evidence that where switching occurred, women were being lost from facility care during this important transition, and that all four included dimensions were important determinants of women’s pattern of delivery care use. The relative importance of these factors should be understood in each specific context to improve retention in and provision of quality intrapartum care for women and their newborns.
Keywords: Maternal health, facility delivery care, provider switching, low- and middle-income countries, Demographic and Health Surveys, multivariate analysis
Key Messages
Understanding factors associated with retention of women in care is important to achieving universal coverage with good quality delivery care globally.
In the 39 low- and middle-income countries assessed, the majority of women consistently used the same delivery location for their first and second births; but in 17 countries more were switching away from facilities (towards home births), in 2 countries towards facilities and in the rest there was no net effect.
Factors associated with switching to a facility after a home delivery included higher education, urban residence, non-poor household status and multiple gestation.
Introduction
Considerable gains were made in reducing maternal mortality between 1990 and 2015 (Alkema et al. 2015; UNICEF and World Health Organization 2015). However, the unequal gains in ensuring skilled care at birth across and within low- and middle-income countries (LMICs) must remain a focus of research and policy at the time of transition to the Sustainable Development Goals (Barros et al. 2012; UNICEF and World Health Organization 2015). One method that can help us understand the importance of women’s previous access to, and experiences of, health services, as well as the socioeconomic context within which their decisions are made, is the life course approach (Rich-Edwards 2002; Russ et al. 2014). This study employs such approach to define the patterns of where women deliver in LMICs, quantify switching behaviour, and identify key determinants for switching.
While recognizing that quality of delivery care in health facilities can be far from ideal, obstetric emergencies are best attended there, and attending uncomplicated deliveries within the structure of health system can enable faster access to referral if needed. However, studies have also shown that delivering in a health facility does not necessarily equate to receiving good quality, respectful care (Shankar et al. 2008; Benova et al. 2015; Tripathi et al. 2015), which is not only crucial in order to reduce maternal and newborn morbidity and mortality, but also to encourage women and their families to continue engaging with preventive and curative health care services during their lifespan. Existing literature provides an extensive examination of determinants of delivering in a health facility among women in LMICs, using both quantitative and qualitative approaches (Gabrysch and Campbell 2009; Montagu et al. 2011; Guliani et al. 2012; Adjiwanou and Legrand, 2013; Moyer and Mustafa 2013; Bohren et al. 2014; Mason et al. 2015). Women’s non-use of facility-based delivery care can reflect important considerations and prior experience with care, and provide useful feedback about the accessibility, affordability and perceived quality of care provided by health facilities to guide policy and research; however, the work examining the patterns of delivery care for successive births is limited.
Bell et al. (2003) assessed consistency of delivery with or without a skilled birth attendant (SBA) in six countries, using multiple Demographic and Health Surveys (DHS) per country. They found that most women were consistent in their use of SBA over successive deliveries; the proportion of women with inconsistent care (SBA for some but not all deliveries) ranged from 7% in Bangladesh to 27% in Malawi. Highlighting the importance of long-term healthcare utilization patterns, their multivariable model showed that SBA use for the index birth was the most important predictor of SBA use for a subsequent delivery, followed by urban/rural residence and education level in some countries. Parity was unimportant in all six countries. Johnson et al. (2013) analysed DHS data from 44 LMICs to examine patterns in location (home or health facility) of successive deliveries, including quantifying the direction of switching (from home to facility or from facility to home). They concluded that 14% of women in these countries changed delivery location between the two most recent deliveries in the survey recall period, but that in all four regions the directions of switching cancelled each other. A multivariable model predicting changing from home to facility location among all women who changed location (in either direction) showed that parity, ANC use and wealth were important factors of switching in both directions.
While these two studies provide insights into the patterns of delivery care use by women over successive births, there are several avenues through which existing data can further explicate women’s patterns of delivery care use. The particular salience of parity as a determinant of delivery care utilization is widely recognized (Stephenson and Tsui 2002; Gabrysch and Campbell 2009). High parity has garnered attention due to being a marker of increased risk of adverse maternal and newborn outcomes (Bai et al. 2002; Mgaya et al. 2013) and can also be a proxy for lower socioeconomic status related to high fertility. However, studies have also highlighted the fact that primiparity carries higher risks for women and their newborns (Malkiel et al. 2008; Hashim et al. 2012). This can lead to a pattern where women use facility delivery care for their first birth but chose to deliver their second and subsequent children in home environments (Moyer and Mustafa 2013), and can be a culturally normalized practice. Early experiences with maternal health care might have important repercussions for women’s use of maternal (as well as newborn and child) health services over the life course, and can provide important feedback to health systems on the acceptability of available services. The importance of understanding and preventing this ‘loss’ of women from healthcare in the crucial transition between first and second births is also underpinned by declining fertility rates in LMICs (United Nations Department of Economic and Social Affairs - Population Division 2015), which will result in increasing proportions of all births being first- and second-order. In this article, we therefore focus specifically on changes in delivery care use occurring between women’s first and second births.
This study has two main objectives. First, we conceptually define patterns of transitions in delivery care locations over successive deliveries and suggest appropriate measurement of these patterns capturing both the extent and the direction of switching. Second, we use DHS data to estimate the prevalence of these patterns in individual countries and across two LMIC regions—Sub-Saharan Africa and South/Southeast Asia, as they relate to switching between women’s first- and second-order births. Within this objective, we assess determinants of delivery location switching to gain a better understanding of women’s decisions and access to delivery care.
Materials and methods
Population
The DHS are nationally representative population-based surveys which collect data about households and women in reproductive age (15–49 years), that include information about pregnancies, deliveries and the use of reproductive and maternal care. We used DHS data from the most recent survey conducted between 2004 and 2012 for the Sub-Saharan African and South/Southeast Asian countries which used a 5-year recall period to collect data about delivery care use. The switching analysis sample was limited to women who had their first and second live births in the survey recall period. A small proportion of women had additional deliveries during the recall period; they were retained in the analysis. We considered multiples (twins and higher) to constitute one delivery as it relates to the delivery location. For example, a woman who delivered twins and a subsequent singleton was considered to have experienced two deliveries. In addition, all women with one or more live births in the recall period were retained to compare their characteristics with those of the switching analysis sample group.
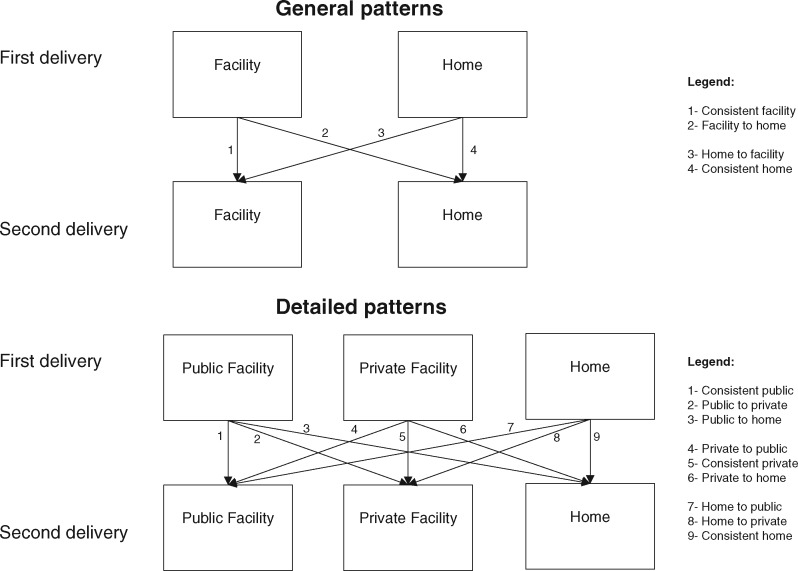
Women were asked about the location of deliveries for all live births they reported in the survey recall period. Their responses were categorized into home- vs facility-based environments. Facility deliveries were further classified as occurring in public- or the private-sector locations, using a categorization used previously (Benova et al. 2015). Two sets of delivery location patterns capturing the consistency of delivery location between the two most recent deliveries were constructed and analysed for each woman: four general and nine detailed (Figure 1).
Figure 1.
General and detailed patterns of delivery location
Statistical analysis
First, we examined the prevalence of the four general and nine detailed patterns among women in the analysis sample, by country and by region. The net direction of switching (towards home or facility) was quantified. Second, among women whose first delivery occurred at home, we assessed the determinants of switching to a facility for the second delivery, vs retention in home-based care. Among women with a first delivery in a facility we assessed the determinants of switching to a home location vs retention in facility-based care for the second delivery. Determinants of detailed patterns were not analysed due to small sample sizes within countries.
We used logistic regression to analyse determinants of the two types of switching; only variables significant at the P < 0.1 level were retained in the final models, except for age group, which was retained in all models a priori regardless of significance. Multivariable analyses were conducted for all women in the sample using individual-level weights adjusted for both country-level sampling design and regional population weights. All analyses were conducted in Stata SE 14 (College Station, TX, USA). The analysis of DHS requires the use of within-country individual weights to generate nationally representative estimates. In addition to women’s sampling weights, we also accounted for the effect of sample clustering and stratification through use of the svyset command. Regional and overall estimates were produced by weighting countries according to their population in 2008 (UN estimates).
Determinants
Variables capturing four dimensions were considered for inclusion in multivariable models. First, characteristics capturing women’s biological and perceived need for delivery care included age group in years at first delivery (10–19, 20–24, 25–29, 30–34, 35+), whether first delivery was by caesarean section or not, birth interval between the two deliveries (<24 or 24+ months), whether the second delivery was multiple (twins or more) or not, whether the first child (or, in cases of multiple first delivery, at least one child) was alive at the time of the second delivery or not, and whether the two deliveries were wanted at the time of the pregnancy (both wanted, both unwanted/mistimed, first wanted-second unwanted/mistimed or first unwanted/mistimed-second wanted). Second, women’s socioeconomic characteristics were considered in order to examine access to, autonomy and affordability of delivery care. These included women’s education (no education, primary, secondary and higher), household’s relative poverty (in the two poorest wealth quintiles or not), marital status at the time of survey (married/cohabiting or not), residence (urban/rural) and sex of the first and of the second child (in case of multiple first delivery, the sex of the child listed last was used). Third, experience with and utilization of pregnancy care was used. Specifically, whether, regardless of delivery location, the first delivery occurred in the presence of a SBA or not (Benova et al. 2015), and, as a proxy for continuity of care and counselling of delivery location options, the number ANC visits during the second pregnancy (none, 1, 2, 3, 4 or 5+). The vast majority of DHS only capture ANC utilization for the most recent live birth in the recall period, and therefore this variable was consistently only available for women whose second delivery was also their most recent. We show multivariable models for the whole switching analysis sample as well as sensitivity analyses including ANC use among the >90% of women in this sample for whom the second delivery was the most recent. Fourth, we considered the availability of delivery care in women’s area by including the percentage of births of all parities in women’s survey stratum which occurred in health facilities. The countries’ macroeconomic, social and health-system characteristics were adjusted for by including a country dummy variable in all multivariable models.
Missing data
The DHS generally have low missingness (<1%). In this analysis, we excluded women with any missing data on delivery location. In the other covariates, the extent of missing data is shown on the descriptive tables, and women with missing data were excluded from the multivariable models.
Ethical approval
The DHS received institutional review centrally (ICF International) and were approved by every participating country. The authors obtained ethical approval from their institute.
Results
The analysis was conducted on a weighted sample of 31 651 women from 39 countries who had their first two live births in the survey recall period (Supplementary Material S1). In Sub-Saharan Africa, the 30 included countries represented 83% of the population of the region; in South/Southeast Asia, the 9 included countries accounted for 84% of the region’s population. Compared with all women with one or more births in the recall period, women included in the switching analysis sample had, by definition, a lower mean number of children ever born, and were on average younger, more educated and more likely to be married/cohabiting at the time of the survey, but equally likely to reside in rural areas or belong to the 40% poorest quintile of households (Supplementary Material S2).
Prevalence and direction of delivery location switching
The percentages of women by the location of their first and second deliveries, as well as according to the general patterns, by country, region and overall are shown in Table 1. Among women in the analysis sample, 49.0% of women had their first delivery in a facility compared with 44.5% for the second delivery. The proportion of first deliveries occurring in facilities ranged widely across the countries, from 98.4% in the Maldives to 12.2% in Ethiopia. Overall, 16.6% of women changed delivery location (from home to facility or from facility to home) between the first and second deliveries; this was highest in Lesotho (38.0%) and lowest in the Maldives (2.1%). In regard to the absolute direction of switching, in 15 of the 30 countries in Sub-Saharan Africa, the direction of switching was towards home delivery locations, 14 saw no significant net effect of the directions and only 1 country (Burkina Faso) saw a net increase in facility use between first to second deliveries. Among the nine South/Southeast Asian countries, two showed a significant net decrease in facility deliveries (India and the Philippines), one showed a significant net increase (Cambodia) and the remaining six showed no net effect. For both regions as well as the overall sample of women, the net effect of switching was a significant decline in facility deliveries between the first and second deliveries (overall effect: −4.6%, 95%CI −5.4, −3.8).
Table 1.
Prevalence of delivery location switching among women with first two deliveries in survey recall period
| Country/region | Location of 1st delivery |
% of women with deliveries in facility |
General patterns of delivery location switching between first and second delivery (% of all women in switching analysis sample) |
% women in sample who switched delivery location |
Net direction of switching*(H->F minus F->H) |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Home (%) | Public facility (%) | Private facility (%) | 1st delivery (%) | 2nd delivery (%) | Consistent home (%) | Consistent facility (%) | Facility to home (%) | Home to facility (%) | Absolute difference (%) | 95% CI | ||
| Benin | 17.6 | 64.9 | 17.6 | 82.5 | 82.4 | 13.9 | 78.8 | 3.7 | 3.6 | 7.3 | −0.1 | −1.7 to 1.5 |
| Burkina Faso | 35.4 | 64.1 | 0.5 | 64.6 | 73.5 | 22.3 | 60.4 | 4.2 | 13.1 | 17.3 | 8.9 | 6.1 to 11.5 |
| Burundi | 25.0 | 68.4 | 6.7 | 75.0 | 71.3 | 13.5 | 59.7 | 15.3 | 11.5 | 26.8 | −3.8 | −8.3 to 0.8 |
| Cameroon | 32.7 | 44.5 | 22.9 | 67.4 | 66.0 | 27.3 | 60.6 | 6.7 | 5.4 | 12.1 | −1.3 | −3.9 to 1.3 |
| Chad | 83.1 | 14.2 | 2.7 | 16.9 | 13.5 | 80.2 | 10.6 | 6.3 | 2.9 | 9.2 | −3.4 | −6.8 to 0.0 |
| Republic of the Congo | 14.3 | 80.9 | 4.8 | 85.7 | 82.1 | 9.8 | 77.6 | 8.1 | 4.5 | 12.6 | −3.6 | −7.9 to 0.7 |
| Democratic Rep. of Congo | 27.8 | 54.2 | 18.0 | 72.2 | 73.2 | 19.1 | 64.5 | 7.7 | 8.7 | 16.4 | 1.0 | −3.9 to 5.8 |
| Ethiopia | 87.8 | 11.1 | 1.1 | 12.2 | 9.5 | 85.0 | 6.7 | 5.5 | 2.8 | 8.3 | −2.7 | −6.1 to 0.7 |
| Gabon | 7.4 | 71.5 | 21.2 | 92.7 | 90.4 | 4.3 | 87.4 | 5.3 | 3.0 | 8.3 | −2.3 | −5.7 to 1.2 |
| Ghana | 36.8 | 53.1 | 10.1 | 63.2 | 61.4 | 27.9 | 52.5 | 10.7 | 8.9 | 19.6 | −1.8 | −8.4 to 4.8 |
| Guinea | 65.7 | 32.0 | 2.3 | 34.3 | 27.6 | 62.2 | 24.1 | 10.2 | 3.5 | 13.7 | −6.7 | −10.8 to − 2.5 |
| Kenya | 48.4 | 44.0 | 7.6 | 51.6 | 41.7 | 41.1 | 34.4 | 17.2 | 7.3 | 24.5 | −9.9 | −15.7 to − 4.2 |
| Lesotho | 33.4 | 53.7 | 12.9 | 66.6 | 53.7 | 20.8 | 41.2 | 25.5 | 12.5 | 38.0 | −13.0 | −20.2 to − 5.7 |
| Liberia | 68.1 | 23.4 | 8.6 | 31.9 | 32.0 | 58.1 | 22.1 | 9.8 | 10.0 | 19.8 | 0.2 | −5.9 to 6.1 |
| Madagascar | 63.2 | 34.1 | 2.7 | 36.8 | 33.3 | 56.3 | 26.4 | 10.4 | 6.9 | 17.3 | −3.5 | −6.6 to − 0.4 |
| Malawi | 25.0 | 59.1 | 15.9 | 75.0 | 77.9 | 13.9 | 66.8 | 8.2 | 11.1 | 19.3 | 2.9 | 0.2 to 5.7 |
| Mali | 51.8 | 46.3 | 1.9 | 48.2 | 46.1 | 44.1 | 38.4 | 9.8 | 7.7 | 17.5 | −2.1 | −5.3 to 1.2 |
| Mozambique | 45.5 | 52.8 | 1.7 | 54.5 | 54.9 | 36.6 | 46.0 | 8.4 | 9.0 | 17.4 | 0.6 | −3.0 to 3.9 |
| Namibia | 16.1 | 81.0 | 3.0 | 83.9 | 77.5 | 9.1 | 70.5 | 13.4 | 7.0 | 20.4 | −6.4 | −11.6 to − 1.3 |
| Niger | 77.9 | 21.0 | 1.1 | 22.1 | 19.2 | 73.9 | 15.2 | 6.9 | 4.0 | 10.9 | −2.9 | −5.8 to 0.1 |
| Nigeria | 56.4 | 22.0 | 21.6 | 43.6 | 41.7 | 52.7 | 37.9 | 5.7 | 3.7 | 9.4 | −2.0 | −3.3 to − 0.6 |
| Rwanda | 16.7 | 82.6 | 0.7 | 83.3 | 84.0 | 8.2 | 75.4 | 7.9 | 8.5 | 16.4 | 0.6 | −2.3 to 3.6 |
| Sao Tome and Principe | 4.6 | 95.4 | 0.0 | 95.4 | 79.0 | 2.7 | 77.2 | 18.2 | 1.9 | 20.1 | −16.3 | −25.9 to − 6.9 |
| Senegal | 18.1 | 76.0 | 5.9 | 81.9 | 75.6 | 14.2 | 71.8 | 10.2 | 3.8 | 14.0 | −6.4 | −8.8 to − 3.8 |
| Sierra Leone | 68.0 | 28.4 | 3.6 | 32.0 | 26.4 | 62.2 | 20.6 | 11.4 | 5.8 | 17.2 | −5.6 | −10.3 to − 0.8 |
| Swaziland | 16.7 | 51.0 | 32.3 | 83.3 | 72.1 | 9.5 | 65.0 | 18.3 | 7.2 | 25.5 | −11.1 | −18.2 to − 4.2 |
| Tanzania | 38.3 | 50.1 | 11.6 | 61.7 | 54.2 | 30.9 | 46.8 | 14.9 | 7.4 | 22.3 | −7.5 | −12.0 to − 3.1 |
| Uganda | 30.6 | 54.1 | 15.4 | 69.5 | 64.4 | 21.3 | 55.2 | 14.3 | 9.2 | 23.5 | −5.1 | −9.5 to − 0.6 |
| Zambia | 42.9 | 50.9 | 6.2 | 57.1 | 52.3 | 33.2 | 42.6 | 14.5 | 9.7 | 24.2 | −4.8 | −9.4 to − 0.2 |
| Zimbabwe | 30.5 | 61.1 | 8.4 | 69.5 | 64.1 | 21.4 | 54.9 | 14.5 | 9.2 | 23.7 | −5.3 | −10.3 to − 0.4 |
| Sub-Saharan Africa | 48.7 | 39.3 | 12.0 | 51.3 | 48.7 | 42.4 | 42.4 | 8.9 | 6.3 | 15.2 | −2.6 | −3.5 to −1.7 |
| Bangladesh | 75.1 | 11.1 | 13.8 | 24.9 | 26.2 | 66.9 | 18.0 | 6.9 | 8.2 | 15.1 | 1.3 | −2.1 to 4.6 |
| Cambodia | 43.9 | 44.9 | 11.2 | 56.1 | 65.3 | 28.6 | 50.0 | 6.1 | 15.3 | 21.4 | 9.2 | 5.1 to 13.2 |
| India | 49.6 | 25.2 | 25.2 | 50.4 | 43.2 | 44.2 | 37.7 | 12.7 | 5.4 | 18.1 | −7.3 | −8.6 to − 5.9 |
| Indonesia | 52.1 | 10.4 | 37.5 | 47.9 | 47.6 | 46.4 | 41.9 | 6.0 | 5.7 | 11.7 | −0.3 | −3.3 to 2.7 |
| Maldives | 1.6 | 87.4 | 11.0 | 98.4 | 98.8 | 0.3 | 97.6 | 0.8 | 1.3 | 2.1 | 0.5 | −1.2 to2.1 |
| Nepal | 61.9 | 25.0 | 13.1 | 38.1 | 36.4 | 49.9 | 24.5 | 13.6 | 12.0 | 25.6 | −1.6 | −7.1 to 3.8 |
| Pakistan | 54.7 | 14.6 | 30.7 | 45.3 | 43.2 | 47.7 | 36.2 | 9.1 | 7.0 | 16.1 | −2.1 | −5.0 to 0.8 |
| Philippines | 44.1 | 34.5 | 21.4 | 55.9 | 46.1 | 40.1 | 42.0 | 13.8 | 4.1 | 17.9 | −9.7 | −13.4 to − 6.1 |
| Timor-Leste | 74.0 | 24.6 | 1.4 | 26.0 | 27.0 | 65.8 | 18.8 | 7.2 | 8.2 | 15.4 | 1.0 | −2.7 to 4.6 |
| South/Southeast Asia | 51.9 | 22.2 | 25.9 | 48.1 | 42.7 | 46.0 | 36.8 | 11.3 | 5.9 | 17.2 | −5.4 | −6.4 to − 4.3 |
| Overall | 50.9 | 27.2 | 21.8 | 49.0 | 44.5 | 44.9 | 38.5 | 10.6 | 6.0 | 16.6 | −4.6 | −5.4 to −3.8 |
| Country summary | ||||||||||||
| Minimum | 1.6 | 10.4 | 0.0 | 12.2 | 9.5 | 0.3 | 6.7 | 0.8 | 1.3 | 2.1 | −16.3 | |
| Maximum | 87.8 | 95.4 | 37.5 | 98.4 | 98.8 | 85.0 | 97.6 | 25.5 | 15.3 | 38.0 | 9.2 | |
| Median | 42.9 | 50.1 | 8.6 | 57.1 | 54.2 | 30.9 | 46.0 | 9.8 | 7.2 | 17.3 | −2.7 | |
Positive absolute difference shows switching pattern favours facility deliveries, negative favours switching to home delivery locations.
The detailed patterns of delivery locations for all women in the sample, and by country and region are shown in Table 2. Together with Table 1, it shows that the most common of the nine detailed patterns was to have both deliveries at home (44.9% overall, range across countries 0.3–85.0%), followed by having both deliveries in facilities (overall 38.5%, of which the largest contribution was from women who consistently used public facilities or consistently used private facilities for both deliveries).
Table 2.
Prevalence of detailed patterns of delivery location switching among women with first two deliveries in survey recall period with known delivery locations
| Country/region | Consistent home (%) | Consistent facility |
Facility to home |
Home to facility |
|||||
|---|---|---|---|---|---|---|---|---|---|
| Consistent public (%) | Consistent private (%) | Public to private (%) | Private to public (%) | Public to home (%) | Private to home (%) | Home to public (%) | Home to private (%) | ||
| Benin | 13.9 | 56.7 | 11.3 | 4.9 | 5.8 | 3.3 | 0.4 | 3.3 | 0.2 |
| Burkina Faso | 22.3 | 59.4 | 0.4 | 0.5 | 0.1 | 4.3 | 0.0 | 13.1 | 0.0 |
| Burundi | 13.5 | 52.5 | 3.9 | 1.8 | 1.7 | 14.1 | 1.1 | 10.6 | 0.9 |
| Cameroon | 27.3 | 32.9 | 17.8 | 5.6 | 4.4 | 6.0 | 0.7 | 4.5 | 0.9 |
| Chad | 80.2 | 8.4 | 2.0 | 0.0 | 0.2 | 5.8 | 0.5 | 2.8 | 0.1 |
| Republic of the Congo | 9.8 | 65.0 | 2.9 | 7.8 | 1.9 | 8.1 | 0.0 | 4.5 | 0.0 |
| Democratic Rep. of Congo | 19.1 | 46.5 | 12.7 | 2.5 | 2.8 | 5.2 | 2.6 | 8.1 | 0.6 |
| Ethiopia | 85.0 | 5.6 | 0.6 | 0.3 | 0.2 | 5.2 | 0.3 | 2.1 | 0.7 |
| Gabon | 4.3 | 60.1 | 15.1 | 6.5 | 5.7 | 4.8 | 0.4 | 2.8 | 0.3 |
| Ghana | 27.9 | 37.1 | 6.9 | 6.2 | 2.3 | 9.8 | 0.9 | 8.1 | 0.8 |
| Guinea | 62.2 | 22.3 | 1.1 | 0.2 | 0.5 | 9.6 | 0.6 | 3.6 | 0.0 |
| Kenya | 41.1 | 25.3 | 5.3 | 3.4 | 0.5 | 15.4 | 1.8 | 4.7 | 2.6 |
| Lesotho | 20.8 | 28.7 | 2.7 | 5.1 | 4.7 | 19.9 | 5.6 | 9.9 | 2.6 |
| Liberia | 58.1 | 15.3 | 2.9 | 1.3 | 2.6 | 6.8 | 3.0 | 7.9 | 2.1 |
| Madagascar | 56.3 | 23.3 | 1.9 | 0.8 | 0.4 | 10.0 | 0.5 | 6.5 | 0.4 |
| Malawi | 13.9 | 48.8 | 11.4 | 3.6 | 3.0 | 6.7 | 1.5 | 9.3 | 1.9 |
| Mali | 44.1 | 35.7 | 1.1 | 1.1 | 0.5 | 9.5 | 0.3 | 7.2 | 0.5 |
| Mozambique | 36.6 | 43.8 | 0.5 | 1.3 | 0.5 | 7.7 | 0.8 | 6.9 | 2.1 |
| Namibia | 9.1 | 66.7 | 3.0 | 0.9 | 0.0 | 13.4 | 0.0 | 7.0 | 0.0 |
| Niger | 73.9 | 14.4 | 0.4 | 0.1 | 0.3 | 6.5 | 0.4 | 4.0 | 0.0 |
| Nigeria | 52.7 | 16.5 | 18.0 | 1.2 | 2.1 | 4.3 | 1.4 | 2.6 | 1.2 |
| Rwanda | 8.2 | 73.7 | 0.4 | 1.1 | 0.1 | 7.7 | 0.1 | 8.5 | 0.0 |
| Sao Tome and Principe | 2.7 | 75.4 | 0.0 | 1.8 | 0.0 | 18.2 | 0.0 | 1.9 | 0.0 |
| Senegal | 14.2 | 65.7 | 4.2 | 0.5 | 1.4 | 9.8 | 0.3 | 3.8 | 0.0 |
| Sierra Leone | 62.2 | 17.4 | 3.2 | 0.0 | 0.0 | 11.0 | 0.4 | 5.6 | 0.3 |
| Swaziland | 9.5 | 36.2 | 17.4 | 4.1 | 7.3 | 10.7 | 7.6 | 4.9 | 2.3 |
| Tanzania | 30.9 | 35.2 | 6.5 | 2.9 | 2.2 | 12.1 | 2.8 | 5.8 | 1.6 |
| Uganda | 21.3 | 38.0 | 9.8 | 3.7 | 3.8 | 12.4 | 1.9 | 8.0 | 1.3 |
| Zambia | 33.2 | 37.8 | 3.4 | 1.1 | 0.4 | 12.1 | 2.5 | 9.0 | 0.7 |
| Zimbabwe | 21.4 | 45.2 | 4.0 | 2.5 | 3.3 | 13.4 | 1.2 | 7.3 | 1.9 |
| Sub-Saharan Africa | 42.4 | 29.8 | 8.8 | 2.0 | 1.8 | 7.5 | 1.3 | 5.3 | 1.0 |
| Bangladesh | 66.9 | 4.4 | 9.6 | 2.6 | 1.4 | 4.1 | 2.9 | 4.1 | 4.1 |
| Cambodia | 28.6 | 36.3 | 6.5 | 2.8 | 4.4 | 5.8 | 0.3 | 14.2 | 1.0 |
| India | 44.2 | 15.5 | 17.0 | 2.3 | 2.9 | 7.4 | 5.3 | 2.9 | 2.5 |
| Indonesia | 46.4 | 5.9 | 30.7 | 2.1 | 3.1 | 2.4 | 3.7 | 1.4 | 4.3 |
| Maldives | 0.3 | 80.9 | 8.3 | 5.9 | 2.4 | 0.5 | 0.3 | 1.3 | 0.0 |
| Nepal | 49.9 | 14.1 | 6.4 | 0.6 | 3.5 | 10.4 | 3.2 | 9.3 | 2.6 |
| Pakistan | 47.7 | 8.3 | 24.5 | 2.0 | 1.5 | 4.3 | 4.8 | 2.0 | 5.0 |
| Philippines | 40.1 | 20.1 | 14.3 | 3.3 | 4.4 | 11.1 | 2.7 | 3.2 | 0.9 |
| Timor-Leste | 65.8 | 17.5 | 0.9 | 0.1 | 0.2 | 7.0 | 0.2 | 7.9 | 0.2 |
| South/Southeast Asia | 46.0 | 13.3 | 18.5 | 2.3 | 2.7 | 6.5 | 4.8 | 2.9 | 3.1 |
| Overall | 44.9 | 18.2 | 15.6 | 2.2 | 2.4 | 6.8 | 3.8 | 3.6 | 2.5 |
| Country summary | |||||||||
| Minimum | 0.3 | 4.4 | 0.0 | 0.0 | 0.0 | 0.5 | 0.0 | 1.3 | 0.0 |
| Maximum | 85.0 | 80.9 | 30.7 | 7.8 | 7.3 | 19.9 | 7.6 | 14.2 | 5.0 |
| Median | 30.9 | 35.7 | 4.2 | 2.0 | 1.9 | 7.7 | 0.8 | 5.6 | 0.8 |
Each row total is 100%—any small differences are due to rounding.
Table 3 describes both general and detailed patterns of delivery location switching, expressed as probabilities of using a particular location for second delivery conditional on using a specific location for the first. The general patterns show that among women who had their first delivery at home, 88.2% had their second at home, whereas 11.8% switched to facility. Retention in home location for both deliveries varied across the countries from 21.1% (Maldives) to 96.8% in Ethiopia. Among women who had their first delivery in a facility, 78.4% overall used a facility for their second (range from 54.9% in Ethiopia to 99.2% Maldives) and the rest switched to home. The detailed patterns show that among women who switched from home to facility locations, a larger proportion of women chose public (7.0%) than private (4.8%) facilities. Among women who used public facilities for their first delivery, 66.9% returned for their second, 25.1% switched to home and 8.0% switched to private facilities. Lastly, women who had their first delivery in private facilities, 71.7% returned, 17.2% switched to home locations and 11.1% to public facilities. However, the probabilities of switching varied widely across included countries. In both regions, the most common switching pattern among women who delivered their first birth in a public facility was to have the second at home. However, among women who had their first delivery in a private facility, the most common switching pattern in Sub-Saharan Africa was to switch to a public facility, whereas in South/Southeast Asia women were most likely to switch to home locations.
Table 3.
Probabilities of remaining in or switching delivery location according to location of first delivery, general and detailed patterns
| General pattern |
Detailed pattern |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| If first delivery in: | Home |
Facility |
Home |
Public facility |
Private facility |
||||||||
| Probability of second delivery in: | Home*(%) | Facility (%) | Home (%) | Facility**(%) | Home (%) | Public facility (%) | Private facility (%) | Home (%) | Public facility (%) | Private facility (%) | Home (%) | Public facility (%) | Private facility (%) |
| Country/region | |||||||||||||
| Benin | 79.6 | 20.4 | 4.5 | 95.5 | 79.6 | 19.1 | 1.4 | 5.0 | 87.3 | 7.6 | 2.3 | 33.3 | 64.4 |
| Burkina Faso | 63.0 | 37.0 | 6.6 | 93.4 | 63.0 | 37.0 | 0.0 | 6.6 | 92.7 | 0.7 | 0.0 | 21.0 | 79.0 |
| Burundi | 54.0 | 46.0 | 20.4 | 79.6 | 54.0 | 42.3 | 3.7 | 20.7 | 76.8 | 2.6 | 17.1 | 24.9 | 58.0 |
| Cameroon | 83.5 | 16.5 | 10.0 | 90.1 | 83.5 | 13.6 | 2.8 | 13.4 | 73.9 | 12.7 | 3.2 | 19.2 | 77.6 |
| Chad | 96.5 | 3.5 | 37.3 | 62.7 | 96.5 | 3.4 | 0.1 | 40.6 | 59.2 | 0.2 | 20.1 | 6.3 | 73.6 |
| Republic of the Congo | 68.7 | 31.3 | 9.5 | 90.5 | 68.7 | 31.3 | 0.0 | 10.0 | 80.4 | 9.6 | 0.0 | 39.1 | 61.0 |
| Democratic Rep. of Congo | 68.8 | 31.2 | 10.7 | 89.3 | 68.8 | 29.2 | 2.0 | 9.5 | 85.9 | 4.6 | 14.2 | 15.3 | 70.6 |
| Ethiopia | 96.8 | 3.2 | 45.1 | 54.9 | 96.8 | 2.4 | 0.8 | 46.6 | 50.3 | 3.1 | 28.9 | 18.1 | 52.9 |
| Gabon | 58.8 | 41.2 | 5.7 | 94.3 | 58.8 | 37.3 | 3.8 | 6.7 | 84.1 | 9.2 | 2.1 | 26.7 | 71.3 |
| Ghana | 75.9 | 24.1 | 16.9 | 83.1 | 75.9 | 22.0 | 2.1 | 18.5 | 69.8 | 11.7 | 8.7 | 22.7 | 68.6 |
| Guinea | 94.6 | 5.4 | 29.8 | 70.2 | 94.6 | 5.4 | 0.0 | 29.9 | 69.5 | 0.6 | 28.3 | 24.0 | 47.8 |
| Kenya | 85.0 | 15.0 | 33.3 | 66.7 | 85.0 | 9.6 | 5.3 | 34.9 | 57.4 | 7.7 | 24.1 | 6.6 | 69.3 |
| Lesotho | 62.5 | 37.5 | 38.2 | 61.8 | 62.5 | 29.7 | 7.8 | 37.0 | 53.5 | 9.6 | 43.2 | 35.9 | 20.9 |
| Liberia | 85.4 | 14.6 | 30.8 | 69.2 | 85.4 | 11.6 | 3.1 | 29.1 | 65.5 | 5.4 | 35.4 | 30.7 | 33.9 |
| Madagascar | 89.0 | 11.0 | 28.4 | 71.6 | 89.0 | 10.3 | 0.6 | 29.3 | 68.3 | 2.4 | 16.6 | 14.3 | 69.1 |
| Malawi | 55.5 | 44.5 | 10.9 | 89.1 | 55.5 | 37.1 | 7.5 | 11.3 | 82.6 | 6.1 | 9.7 | 18.9 | 71.5 |
| Mali | 85.1 | 14.9 | 20.3 | 79.7 | 85.1 | 13.9 | 1.0 | 20.6 | 77.1 | 2.4 | 14.5 | 25.8 | 59.8 |
| Mozambique | 80.4 | 19.6 | 15.5 | 84.5 | 80.4 | 15.1 | 4.5 | 14.6 | 83.0 | 2.4 | 44.6 | 27.9 | 27.5 |
| Namibia | 56.4 | 43.6 | 16.0 | 84.0 | 56.4 | 43.6 | 0.0 | 16.6 | 82.3 | 1.1 | 0.0 | 0.0 | 100.0 |
| Niger | 94.8 | 5.2 | 31.3 | 68.7 | 94.8 | 5.2 | 0.0 | 31.0 | 68.5 | 0.5 | 36.5 | 27.4 | 36.2 |
| Nigeria | 93.3 | 6.7 | 13.1 | 86.9 | 93.3 | 4.6 | 2.1 | 19.5 | 75.2 | 5.4 | 6.5 | 9.9 | 83.5 |
| Rwanda | 48.9 | 51.1 | 9.5 | 90.5 | 48.9 | 51.1 | 0.0 | 9.4 | 89.3 | 1.4 | 19.5 | 18.4 | 62.1 |
| Sao Tome and Principe | 59.5 | 40.5 | 19.1 | 80.9 | 59.5 | 40.5 | 0.0 | 19.1 | 79.0 | 1.9 | n/a | n/a | n/a |
| Senegal | 78.8 | 21.2 | 12.4 | 87.6 | 78.8 | 21.2 | 0.0 | 12.9 | 86.4 | 0.7 | 5.7 | 23.2 | 71.1 |
| Sierra Leone | 91.4 | 8.6 | 35.5 | 64.5 | 91.4 | 8.2 | 0.4 | 38.8 | 61.2 | 0.0 | 9.9 | 0.0 | 90.1 |
| Swaziland | 57.1 | 42.9 | 22.0 | 78.0 | 57.1 | 29.0 | 13.9 | 21.0 | 70.9 | 8.1 | 23.6 | 22.6 | 53.8 |
| Tanzania | 80.8 | 19.2 | 24.2 | 75.8 | 80.8 | 15.0 | 4.2 | 24.1 | 70.2 | 5.7 | 24.4 | 19.3 | 56.3 |
| Uganda | 69.9 | 30.1 | 20.5 | 79.5 | 69.9 | 26.1 | 4.1 | 22.9 | 70.3 | 6.8 | 12.0 | 24.4 | 63.6 |
| Zambia | 77.4 | 22.6 | 25.4 | 74.6 | 77.4 | 21.0 | 1.6 | 23.7 | 74.3 | 2.1 | 39.5 | 5.9 | 54.6 |
| Zimbabwe | 70.0 | 30.0 | 20.9 | 79.1 | 70.0 | 23.8 | 6.2 | 21.9 | 74.0 | 4.1 | 13.8 | 38.8 | 47.4 |
| Sub-Saharan Africa | 87.1 | 12.9 | 17.3 | 82.7 | 87.1 | 10.8 | 2.1 | 19.2 | 75.8 | 5.0 | 11.1 | 15.0 | 73.9 |
| Bangladesh | 89.1 | 10.9 | 27.7 | 72.3 | 89.1 | 5.5 | 5.4 | 36.5 | 39.7 | 23.8 | 20.7 | 9.9 | 69.4 |
| Cambodia | 65.3 | 34.7 | 10.9 | 89.1 | 65.3 | 32.4 | 2.4 | 13.0 | 80.9 | 6.1 | 2.2 | 39.9 | 57.9 |
| India | 89.0 | 11.0 | 25.1 | 74.9 | 89.0 | 5.9 | 5.1 | 29.4 | 61.4 | 9.3 | 20.9 | 11.6 | 67.5 |
| Indonesia | 89.0 | 11.0 | 12.7 | 87.4 | 89.0 | 2.7 | 8.3 | 22.7 | 56.9 | 20.5 | 9.9 | 8.3 | 81.8 |
| Maldives | 21.1 | 78.9 | 0.9 | 99.2 | 21.1 | 78.9 | 0.0 | 0.6 | 92.6 | 6.7 | 2.7 | 22.1 | 75.2 |
| Nepal | 80.7 | 19.3 | 35.8 | 64.2 | 80.7 | 15.1 | 4.2 | 41.5 | 56.2 | 2.3 | 24.8 | 26.5 | 48.8 |
| Pakistan | 87.3 | 12.7 | 20.1 | 80.0 | 87.3 | 3.6 | 9.1 | 29.7 | 56.9 | 13.4 | 15.5 | 4.8 | 79.7 |
| Philippines | 90.8 | 9.2 | 24.7 | 75.3 | 90.8 | 7.2 | 2.1 | 32.2 | 58.3 | 9.5 | 12.6 | 20.5 | 66.9 |
| Timor-Leste | 89.0 | 11.0 | 27.8 | 72.2 | 89.0 | 10.7 | 0.3 | 28.4 | 71.1 | 0.5 | 17.4 | 17.4 | 65.3 |
| South/Southeast Asia | 88.6 | 11.4 | 23.5 | 76.5 | 88.6 | 5.5 | 5.9 | 29.5 | 60.1 | 10.4 | 18.4 | 10.4 | 71.2 |
| Overall | 88.2 | 11.8 | 21.6 | 78.4 | 88.2 | 7.0 | 4.8 | 25.1 | 66.9 | 8.0 | 17.2 | 11.1 | 71.7 |
| Country summary | |||||||||||||
| Minimum | 21.1 | 3.2 | 0.9 | 54.9 | 21.1 | 2.4 | 0.0 | 0.6 | 39.7 | 0.0 | 0.0 | 0.0 | 20.9 |
| Maximum | 96.8 | 78.9 | 45.1 | 99.2 | 96.8 | 78.9 | 13.9 | 46.6 | 92.7 | 23.8 | 44.6 | 39.9 | 100.0 |
| Median | 80.4 | 19.6 | 20.4 | 79.6 | 80.4 | 15.1 | 2.1 | 21.9 | 71.1 | 5.4 | 15.0 | 20.7 | 66.1 |
Home retention rate.
Facility retention rate.
n/a—not applicable.
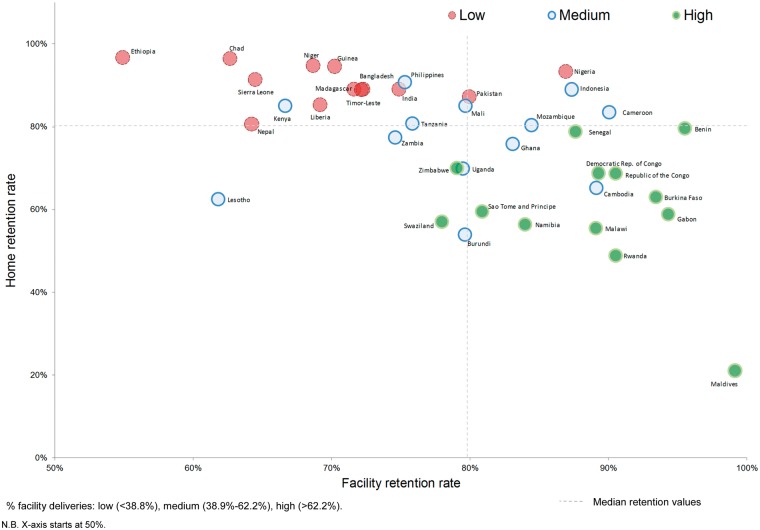
A scatter plot locating countries based on their facility and home retention rates is shown in Figure 2. It is colour-coded to show facility–delivery rates for all births in the recall period (low, medium and high tertiles in sample of 39 countries) and divided into four quadrants according to the median facility (79.6%) and home (80.4%) retention rates in included countries. On the whole, it shows that countries with relatively high home retention rates and low facility retention rates (top left quadrant) tend to be those with low overall facility delivery rates. This type of pattern may be common in circumstances where home is believed to be the norm for deliveries, where facilities are not accessible or affordable, (are seen to) provide low quality of care, or where health facilities are largely used for complications. In this type of environment, women generally deliver at home and even if they require facility delivery with their first delivery, switch to use home locations for the second. Ethiopia and Chad are examples of this type of country environment. The top right hand quadrant with relatively high home and facility retention rates contains a mix of countries with medium and low overall facility delivery rates. This type of pattern might arise in environments with large socioeconomic or geographic disparities in access/affordability or quality of care in a manner through which some women consistently use homes and other women consistently use facilities, but there are relatively low levels of switching occurring in either direction. Examples of such countries include Nigeria, Indonesia and Cameroon.
Figure 2.
Ecological scatter graph of countries by home and facility retention rates between first and second deliveries, colour coded by percentages of all births in facilities
The bottom left hand quadrant presents a scenario with relatively low levels of retention in both homes and facilities. The only country that can be seen to fit this pattern is Lesotho (∼62% retention rates), but the switching analysis sample in this country was small and net direction of switching not significant. Lastly, the bottom right hand quadrant contains countries with relatively low home retention rates but high facility retention rates. With two exceptions, all countries in this quadrant have high overall facility delivery rates. In such environments, giving birth in facilities might be the norm, and women who had their first delivery at home may have not intended to do so, as high proportions switch to facility-based delivery care for the second delivery. The Maldives represent the most extreme example of this type of context. However, this pattern might also include countries where the overall accessibility, acceptability or desirability of facility delivery is increasing rapidly over time, so that a relatively high proportion of women who intentionally had their first delivery at home accessed facility-based care for their second delivery. This scenario may be occurring in Cambodia, one of the two countries with the net direction of switching favouring facilities.
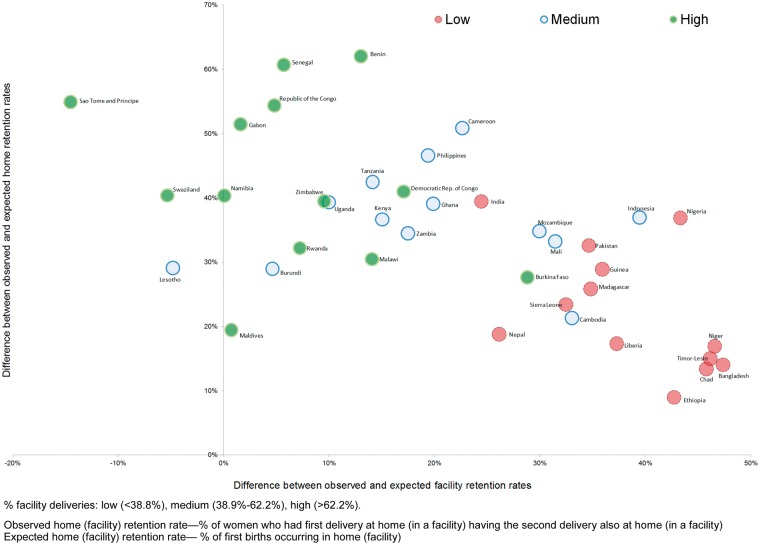
Next, we assess these observed retention rates relative to the rates that would be seen if the levels of facility/home deliveries for the second birth remained the same as those for the first birth (Figure 3). A country with facility and home retention rates close to expected levels (i.e. the probability of the second delivery location is independent on the first and follows the distribution of delivery locations for first birth) would be located at or near the 0.0 point on the graph. This figure shows that no country in the sample has observed retention rates at levels that are comparable with the distribution of locations from the first birth, possibly with the exception of the Maldives (a country with near-universal facility delivery rate). This supports the finding that women tend to consistently use the first delivery location for their subsequent birth. The point that can be clearly seen in this figure is that countries with high overall facility delivery rates tend to have near-expected facility retention rates together with high absolute home retention rates; the opposite is true for countries with low overall facility delivery rates. (The relative size of the differences in observed and expected retention rates were also assessed—not shown—and the same pattern emerged.) Three countries have lower than expected facility retention rates (Sao Tome and Principe, Swaziland and Lesotho) alongside higher than expected home retention rates—these are also countries with the highest net effect of switching away from facilities from the 39 countries in the analysis. Countries with very high retention in both homes and facilities are the same as identified in the top right quadrant in Figure 2 (Cameroon, Nigeria, Indonesia). Burkina Faso and Cambodia are outliers within their respective tertiles of overall facility delivery rates in having lower than expected home retention rates and higher than expected facility retention rates.
Figure 3.
Ecological scatter graph of countries by the difference between the observed and expected home and facility retention rates between first and second deliveries, colour coded by percentages of all births in facilities
Analysis of determinants of switching
Characteristics of women, for the sample overall as well as according to the four general patterns of delivery location switching are provided in Table 4. In crude analysis, all variables with the exception of the sex of the first child, sex of the second child and multiple gestation were significantly associated with the general pattern. Sex of the second child was explored in the South/Southeast Asia region and found to be significantly associated with the general delivery pattern in India only (Supplementary Material S3).
Table 4.
Distribution of determinants in overall sample and according to general pattern
| Determinant | 1st delivery |
All women*(%) |
Home |
Facility |
P-value** | ||
|---|---|---|---|---|---|---|---|
| 2nd delivery | Home (%) | Facility (%) | Home (%) | Facility (%) | |||
| Column % | Row % | ||||||
| Biological/perceived need | |||||||
| Woman’s age group at 1st delivery | 10-19 | 50.7 | 54.3 | 6.4 | 11.2 | 28.1 | <0.001 |
| 20-24 | 38.2 | 38.3 | 6.2 | 10.8 | 44.7 | ||
| 25-29 | 8.9 | 24.2 | 4.1 | 7.1 | 64.6 | ||
| 30-34 | 2.0 | 27.8 | 3.7 | 7.5 | 61.1 | ||
| 35+ | 0.2 | 32.0 | 1.2 | 3.4 | 63.5 | ||
| Birth interval between 1st and 2nd delivery | <24 months | 43.1 | 43.1 | 5.5 | 12.0 | 39.4 | <0.001 |
| 24+ months | 56.9 | 46.3 | 6.4 | 9.6 | 37.7 | ||
| 1st delivery by caesarean section | No | 91.6 | 49.0 | 6.6 | 10.4 | 34.0 | <0.001 |
| Yes | 8.0 | 0.0 | 0.0 | 11.9 | 88.1 | ||
| Missing | 0.4 | 0.0 | 0.0 | 33.1 | 66.9 | ||
| 2nd delivery multiple gestation | Yes | 0.8 | 33.7 | 9.6 | 8.3 | 48.5 | 0.080 |
| No | 99.2 | 45.0 | 6.0 | 10.6 | 38.4 | ||
| Child from 1st delivery alive at time of 2nd delivery | Yes | 89.1 | 44.6 | 5.5 | 10.7 | 39.3 | <0.001 |
| No | 10.9 | 47.8 | 10.6 | 9.9 | 31.8 | ||
| Sex of child from 1st delivery | Male | 50.2 | 44.6 | 5.7 | 10.9 | 38.9 | 0.262 |
| Female | 49.8 | 45.3 | 6.4 | 10.3 | 38.0 | ||
| Sex of child from 2nd delivery | Male | 51.2 | 44.6 | 6.2 | 10.0 | 39.3 | 0.083 |
| Female | 48.8 | 45.3 | 5.8 | 11.3 | 37.6 | ||
| Pattern of pregnancy wantedness | Both wanted | 70.1 | 46.8 | 6.4 | 10.1 | 36.7 | <0.001 |
| 1st wanted, 2nd unwanted/mistimed | 20.1 | 41.8 | 4.5 | 11.5 | 42.1 | ||
| 1st unwanted/mistimed, 2nd wanted | 3.6 | 38.0 | 5.6 | 11.5 | 44.8 | ||
| Both unwanted/mistimed | 6.2 | 37.2 | 7.2 | 12.4 | 43.1 | ||
| Socioeconomic | |||||||
| Woman’s education level | No education | 35.1 | 66.4 | 5.4 | 10.4 | 17.8 | <0.001 |
| Primary | 24.2 | 46.8 | 7.5 | 11.1 | 34.6 | ||
| Secondary/higher | 40.6 | 25.2 | 5.8 | 10.5 | 58.6 | ||
| Missing | <0.1 | 0.0 | 86.7 | 0.0 | 13.9 | ||
| Residence | Rural | 70.9 | 55.2 | 6.2 | 11.6 | 27.0 | <0.001 |
| Urban | 29.1 | 19.8 | 5.7 | 8.1 | 66.5 | ||
| Currently married or cohabiting | Yes | 96.9 | 45.1 | 6.0 | 10.5 | 38.3 | 0.018 |
| No | 3.1 | 38.5 | 6.5 | 13.1 | 41.9 | ||
| In two poorest wealth quintiles | Yes | 41.2 | 64.7 | 5.8 | 11.6 | 17.9 | <0.001 |
| No | 58.8 | 31.1 | 6.2 | 9.9 | 52.9 | ||
| Pregnancy care | |||||||
| Birth attendant at 1st delivery | SBA | 54.2 | 10.0 | 2.2 | 18.9 | 68.9 | <0.001 |
| Non-SBA | 45.7 | 86.3 | 10.6 | 0.7 | 2.3 | ||
| Missing | 0.1 | 47.8 | 10.4 | 12.8 | 29.0 | ||
| Number of ANC visits for 2nd delivery | None | 16.4 | 81.8 | 2.9 | 8.3 | 7.0 | <0.001 |
| 1 | 6.0 | 55.5 | 6.4 | 16.7 | 21.4 | ||
| 2 | 12.5 | 55.8 | 6.5 | 14.3 | 23.4 | ||
| 3 | 14.0 | 41.6 | 6.8 | 14.2 | 37.6 | ||
| 4 | 8.7 | 28.7 | 8.7% | 10.6 | 52.0 | ||
| 5 or more | 28.1 | 20.0 | 6.4 | 7.5 | 66.1 | ||
| Missing | 1.3 | 31.5 | 4.3 | 8.4 | 55.9 | ||
| 2nd delivery not most recent birth | 13.0 | 52.9 | 6.3 | 10.2 | 30.7 | ||
| Overall | 44.9 | 6.0 | 10.6 | 38.5 | |||
| Availability of care | |||||||
| Stratum mean | |||||||
| % of all deliveries in facilities | 41.9 | 31.1 | 43.6 | 40.5 | 54.6 | <0.001 | |
| of all deliveries in private facilities | 19.0 | 14.6 | 19.0 | 17.6 | 24.6 | <0.001 | |
| of facility deliveries in private facilities | 45.5 | 45.1 | 45.0 | 44.7 | 46.3 | <0.001 | |
Weighted sample of 31 651 women.
P-value for chi-square test for all variables other than variables capturing availability of care, where one-way ANOVA was used.
Table 4 shows that older women were more likely to have consistently delivered in facilities compared with younger women. Among women who had a first birth in a facility, those who experienced a caesarean section were more likely to use a facility for the second delivery. Women whose first child died before their second delivery were more likely to switch from home to a facility compared with women whose first child was alive. Women with no education, of rural residence and within the two poorest quintiles of household wealth were more likely to consistently deliver at home compare to women with more education, urban residence and higher wealth who were more likely to consistently deliver in facilities. Women who had an SBA at first delivery and women with higher numbers of ANC visits preceding the second birth were more likely to consistently use facilities for both births. Stratum-level percentages of all deliveries occurring in facilities were higher for women who stayed in or transitioned to facilities.
Table 5 shows the significant determinants of having the first delivery in a facility (vs at home). It shows that older women, women with multiple gestation, higher levels of education, urban residence and higher household wealth were more likely to deliver their first child in a facility. Among women with their first delivery at home (Table 6), significant determinants of switching to a facility for the second included a longer birth interval, multiple gestation, death of a child from first delivery, higher education, urban residence, higher household wealth, ANC utilization for the second pregnancy and higher stratum-level facility–delivery rates. Table 7 shows that among women with first delivery in a facility, determinants of switching to home for the second delivery included younger age, vaginal first delivery, lower educational level, rural residence, household poverty, low ANC utilization and residence in strata with lower facility delivery rates.
Table 5.
Multivariable model of having first delivery in a facility among women in switching analysis sample
| Determinant | Sample | All women |
|
|---|---|---|---|
| (n = 31,651) | |||
| OR (95CI) | P-value | ||
| Biological/perceived need | |||
| Woman’s age group at 1st delivery | 10–19 | Ref | <0.001 |
| 20–24 | 1.47 (1.33–1.63) | ||
| 25–29 | 2.55 (2.14–3.04) | ||
| 30–34 | 2.44 (1.76–3.40) | ||
| 35+ | 2.03 (1.09–3.80) | ||
| 1st delivery multiple gestation | No | Ref | <0.001 |
| Yes | 2.44 (1.10–5.42) | ||
| Socioeconomic | |||
| Woman’s education level | No education | Ref | <0.001 |
| Primary | 1.74 (1.52–1.98) | ||
| Secondary/higher | 3.81 (3.34–4.35) | ||
| Rural residence | No | Ref | <0.001 |
| Yes | 0.36 (0.32–0.41) | ||
| In two poorest wealth quintiles | No | Ref | <0.001 |
| Yes | 0.51 (0.46–0.57) | ||
Model controlled for effect of country.
P-values of likelihood ratio test.
Stratum level facility delivery rate not included due to collinearity.
Table 6.
Multivariable model of switching to facilities, among women whose 1st delivery occurred at home
| Determinant | Outcome |
Switching to facility |
|||
|---|---|---|---|---|---|
| Sample |
All women with 1st delivery at home |
Women who had exactly two deliveries and 1st delivery at home |
|||
| (n = 16,109) |
(n = 13,535) |
||||
| OR (95% CI) | P-value | OR (95% CI) | P-value | ||
| Biological/perceived need | |||||
| Woman’s age group at 1st delivery | 10–19 | Ref | 0.126 | Ref | 0.548 |
| 20–24 | 1.25 (1.03–1.52) | 1.12 (0.90–1.39) | |||
| 25–29 | 1.23 (0.83–1.84) | 1.12 (0.72–1.73) | |||
| 30–34 | 0.97 (0.48–1.93) | 0.93 (0.47–1.86) | |||
| 35+ | 0.22 (0.06–0.76) | 0.10 (0.02–0.50) | |||
| Birth interval between 1st and 2nd delivery | <24 months | Ref | 0.011 | Ref | 0.070 |
| 24+ months | 1.28 (1.06–1.55) | 1.22 (0.98–1.51) | |||
| 2nd delivery multiple gestation | No | Ref | 0.068 | Ref | 0.101 |
| Yes | 2.30 (0.94–5.61) | 2.56 (0.83–7.87) | |||
| Child from 1st delivery alive at time of 2nd delivery | No | Ref | <0.001 | Ref | <0.001 |
| Yes | 0.41 (0.31–0.52) | 0.44 (0.33–0.59) | |||
| Socioeconomic | |||||
| Woman’s education level | No education | Ref | <0.001 | Ref | <0.001 |
| Primary | 1.56 (1.21–2.01) | 1.13 (0.86–1.48) | |||
| Secondary/higher | 2.23 (1.72–2.89) | 1.53 (1.16–2.02) | |||
| Rural residence | No | Ref | <0.001 | Ref | 0.003 |
| Yes | 0.52 (0.41–0.66) | 0.53 (0.42–0.68) | |||
| In two poorest wealth quintiles | No | Ref | <0.001 | Ref | 0.001 |
| Yes | 0.63 (0.51–0.77) | 0.68 (0.55–0.85) | |||
| Pregnancy care | |||||
| Birth attendant at 1st delivery | Non-SBA | Ref | 0.042 | Ref | 0.254 |
| SBA | 1.31 (1.01–1.69) | 1.18 (0.89–1.55) | |||
| Number of ANC visits for 2nd delivery | None | Ref | <0.001 | ||
| 1 | 2.50 (1.48–4.20) | ||||
| 2 | 2.40 (1.54–3.73) | ||||
| 3 | 2.90 (1.91–4.39) | ||||
| 4 | 4.74 (3.03–7.43) | ||||
| 5 or more | 5.63 (3.77–8.41) | ||||
| Availability of care | |||||
| % Of all deliveries in facilities (stratum mean) | (Continuous variable, odds associated with 1% increase in) | 1.03 (1.02–1.03) | <0.001 | 1.02 (1.01–1.03) | <0.001 |
Models controlled for effect of country.
P-values of likelihood ratio test.
Table 7.
Multivariable model of switching to home, among women whose 1st delivery occurred in a facility
| Determinant | Outcome | Switching to home |
|||
|---|---|---|---|---|---|
| Sample | All women with 1st delivery in facility |
Women who had exactly two deliveries and 1st delivery in facility |
|||
|
(n = 15,408) |
(n = 13,489) |
||||
| OR (95% CI) | P-value | OR (95% CI) | P-value | ||
| Biological/perceived need | |||||
| Woman’s age group at 1st delivery | 10–19 | Ref | <0.001 | Ref | <0.001 |
| 20–24 | 0.77 (0.65–0.91) | 0.77 (0.64–0.93) | |||
| 25–29 | 0.46 (0.34–0.61) | 0.47 (0.34–0.64) | |||
| 30–34 | 0.48 (0.30–0.78) | 0.51 (0.30–0.86) | |||
| 35+ | 0.28 (0.06–1.43) | 0.33 (0.06–1.80) | |||
| Birth interval between 1st and 2nd delivery | <24 months | Ref | 0.054 | Ref | 0.365 |
| 24+ months | 0.85 (0.73–1.00) | 0.92 (0.77–1.10) | |||
| 1st delivery by caesarean section | No | Ref | <0.001 | Ref | <0.001 |
| Yes | 0.47 (0.36–0.62) | 0.48 (0.36–0.64) | |||
| Child from 1st delivery alive at time of 2nd delivery | No | Ref | 0.059 | Ref | 0.470 |
| Yes | 1.28 (0.99–1.65) | 1.12 (0.83–1.51) | |||
| Socioeconomic | |||||
| Woman’s education level | No education | Ref | <0.001 | Ref | <0.001 |
| Primary | 0.75 (0.60–0.95) | 0.87 (0.67–1.12) | |||
| Secondary/higher | 0.53 (0.42–0.66) | 0.75 (0.58–0.96) | |||
| Rural residence | No | Ref | <0.001 | Ref | <0.001 |
| Yes | 2.25 (1.88–2.71) | 2.04 (1.67–2.49) | |||
| In two poorest wealth quintiles | No | Ref | <0.001 | Ref | <0.001 |
| Yes | 1.80 (1.50–2.16) | 1.61 (1.31–1.97) | |||
| Pregnancy care | |||||
| Number of ANC visits for 2nd delivery (%) | None | Ref | <0.001 | ||
| 1 | 0.93 (0.60–1.47) | ||||
| 2 | 0.68 (0.47–0.99) | ||||
| 3 | 0.58 (0.40–0.83) | ||||
| 4 | 0.30 (0.20–0.44) | ||||
| 5 or more | 0.22 (0.16–0.32) | ||||
| Availability of care | |||||
| % Of all deliveries in facilities (stratum mean) | (Continuous variable, odds associated with 1% increase in) | 0.97 (0.96–0.98) | <0.001 | 0.98 (0.97–0.99) | <0.001 |
Models controlled for effect of country.
P-values of likelihood ratio test.
Lastly, Table 8 summarizes the findings on determinants of switching, first by showing the selection of women into switching analysis samples by virtue of the location of their first delivery. Four main factors were associated with having the first delivery in a facility and with switching to a facility after a home delivery: higher education, urban residence, non-poor household status and multiple gestation. Woman’s age was significantly positively associated with first delivery in a facility, but not with switching to a facility after a home delivery. Comparing the determinants of the two opposite switching directions, we found that five determinants operated in consistently reverse directions and were significant in both models: education, residence, household poverty, ANC utilization and stratum-level proportion of births occurring in facilities. In the model of determinants predicting switching from home to a facility, three other determinants were of importance—birth interval, multiple gestation and whether first child was alive at time of second delivery. In the model of switching from facility to home, older age and first delivery by caesarean section were negative predictors. Country-level effect was significant in all three models. On the other hand, sex of the child, pregnancy wantedness and marital status were not associated with delivering in a facility or switching to a facility after a home birth. SBA at first delivery was not a significant predictor of switching towards or away from facility delivery after ANC use was adjusted for, most likely because it is highly correlated with delivering in a facility.
Table 8.
Summary of effects of determinants on facility delivery (first delivery) and switching pattern for second delivery
| Determinant | First delivery in a facility | Switching to facility after home delivery | Switching to home after facility delivery | |
|---|---|---|---|---|
| Biological/perceived need | Woman’s (older) age | Positive | n.s. | Negative |
| Birth interval (longer) | Not applicable | Positive | n.s. | |
| Multiple gestation | Positive (1st delivery) | Positive (2nd delivery) | n.s. (2nd delivery) | |
| Caesarean section | Not applicable | Not applicable | Negative | |
| Child alive | Not applicable | Negative | n.s. | |
| Male child | n.s. | n.s. | n.s. | |
| Wantedness | n.s. | n.s. | n.s. | |
| Socioeconomic | Education (higher) | Positive | Positive | Negative |
| Rural residence | Negative | Negative | Positive | |
| Marital status | n.s. | n.s. | n.s. | |
| Poverty | Negative | Negative | Positive | |
| Pregnancy care | SBA at 1st delivery | Not available | n.s. | n.s. |
| ANC before 2nd delivery | Not available | Positive | Negative | |
| Availability of care | Stratum facility delivery rate (higher) | Not included | Positive | Negative |
Effect direction shown if significant at P < 0.1.
n.s.—not significant at P < 0.1 level.
Discussion
Summary of findings
In this article, we examined the extent of delivery location switching among women between their first and second deliveries in 39 LMICs in Sub-Saharan Africa and South/Southeast Asia, 2 regions where relatively recent surveys cover >80% of the population. We also developed a conceptual approach to understanding country-level patterns of switching and retention in home- or facility-based care. We found that with some exceptions, women largely tended to remain in the same location for both deliveries. This finding that the majority of women use the same level of care across subsequent pregnancies is similar to that of two previous studies (Bell et al. 2003; Johnson et al. 2013). Overall in the included countries, the net direction of switching was away from health facilities—the proportion of second deliveries in facilities was lower than the proportion of first deliveries. The magnitude of this net effect differed across the countries, but was negative (away from facility delivery) and significant in 17 countries. These results are different from Johnson et al.’s (2013) findings of no net effect, most likely because they included women of all parities in analysis. Their finding, together with our conclusion that women of low parities are switching away from facilities, implies that the net direction of switching is most likely in the opposite direction, towards facilities, among higher parity women. The question of whether facility delivery rate among women of higher parities returns to the levels seen among primiparous women was not examined in either study. However, our study highlights that in many countries, women appeared to drop out of facility-based delivery care between their first and second deliveries, a crucial transition that has the potential to wield long-term influence on the health-seeking behaviour of women and their households.
Bell’s analysis of delivery care consistency across subsequent deliveries in a small number of countries relied on delivery attendant rather than location. Yet, once women reach health facilities, it is unlikely that they can exercise a high degree of choice over the delivery attendant. From the life course perspective of women’s decisions on delivery care it might be more informative to focus such analyses on delivery location. Johnson et al. conducted such an analysis in 44 countries. However, they assessed the predictors of the direction (towards or away from facility) of switching among women who switched. Their approach could therefore not identify the factors associated with switching vs remaining in the same location. Our analysis of predictors of switching vs remaining in the same location found that variables capturing all four dimensions played an important role. The five consistent effects show that experience with care (ANC), availability/acceptability of facility-based care in the woman’s environment (stratum facility delivery rate), and socioeconomic status were important determinants of both switching to facilities and switching away from facilities.
We also found that factors associated with delivering in a certain location may differ from reasons for remaining in, or switching to, such locations. From the factors capturing perceived need, we found that older women had a higher likelihood of staying in facilities for second birth. However, older age was not associated with the likelihood of switching to a facility after a home birth. Longer birth interval was associated with switching to a facility, but not with staying in a facility, and similarly, multiple gestation was associated with switching to but not with staying in a facility. A child from first delivery dying was associated with switching to facility, but not with staying in facility. This seems to show that negative experiences, or a threat thereof, might be more important to initiating change than positive experience is to retention in facility-based care, and is seen particularly with biological/perceived need variables. However, socioeconomic factors and care availability/previous experience with care were variables most consistently associated with facility delivery at first delivery, with retention in facilities, and with switching to facilities.
Limitations
The strengths of our analysis include its focus on women’s first two births (eliminating confounding by parity), transparency on how country-level surveys were weighted to regional averages, clarity about how multiple pregnancies (twins and higher) were handled in analyses, and inclusion of sector (public or private) of delivery facilities in analysis. However, this study has some limitations. Most importantly, we relied on the 5-year recall period of DHS data to identify the sample of women for analysis. However, compared with all women with their first two deliveries, women who had these deliveries during the surveys’ recall period might be more likely to have shorter birth intervals and potentially also higher fertility and lower socioeconomic position. It is possible that due to this selection, we may have, to some extent, overestimated the net direction of change away from facilities. However, it is also likely that among women with longer birth intervals between first and second deliveries, the determinants of switching delivery location have a different magnitude and strength of association, particularly those related to previous experience with healthcare, which occurred longer in the past. Second, DHS data do not capture pregnancy outcomes (and their location) other than live births, and our analysis therefore only includes deliveries resulting in live births. However, women’s experience of care during events such as miscarriage, induced abortion and stillbirth is also likely to be important in their life course use of healthcare for reproductive and maternal/newborn health. Third, we had no information about the women’s intended location of delivery, only the actual location. It is possible that to some extent, the switching—particularly switching from facility to home—may have been unintentional, in that women who intended to again deliver in a facility had been unable to reach those facilities in time for childbirth. Fourth, the analysis of delivery location patterns, particularly the detailed patterns, relied on women’s recall of not just the location but also the sector of delivery location, for a period of up to 5 years preceding the survey. Fifth, the information capturing obstetric risk and availability of/access to care used in multivariable models was limited. Future analyses could explore the salience of determinants such as distance (or travel time) to the nearest operational health facility and pregnancy/delivery complications experienced by women to their retention in facility delivery care.
Conclusion
With continuing declines in fertility in LMICs, the focus of research and policy is shifting to low-parity women. This analysis of patterns of delivery care utilization provides broad insights into women’s choices in continuity or switching of delivery location and sheds light on the determinants of their decisions. The reasons for consistency and switching patterns might differ in each country, as the case of India showed where an crude association was found between male sex of the unborn (second) child and higher likelihood of women remaining in facilities or switching from home to facilities. Contextual factors such as the importance of the experience of care surrounding the first delivery, cultural practices and attitudes that might consider the first birth riskier than higher order births, the influence of secular trends in proportions of deliveries occurring in facilities, and effects of any demand- and supply-side interventions that influence these factors need to be better understood. Such country-specific studies, if based on longitudinal cohorts of women, will also be able to describe switching patterns and their determinants across all parities. In particular, our analysis highlights that countries with low facility retention rates should seek to understand the reasons for this phenomenon in order to ensure accessible, affordable, respectful and high-quality intrapartum care for all women. Of particular concern would be differential retention rates between public- and private-sector facilities, which may point to issues of variable quality of care and unaffordability of facility-based deliveries in general. However, one of the limitations of the DHS data is that country-level sample sizes for this type of analysis are often too small, and thus other data sources and methodologies may need to be used for this purpose.
Burkina Faso and Cambodia were exceptions in displaying net switching patterns towards facility deliveries, and in both countries might be a result of secular trends in the overall facility delivery rates. Cambodia has experienced a rapid increase in the proportion of births delivered in health facilities during the period of time examined in this study—rising from 22% in 2005 to 83% in 2014, with a particular focus on reducing socioeconomic gradients in service use (National Institute of Public Health et al. 2006; Boerma et al. 2008; Annear 2010; National Institute of Statistics et al. 2015). This increase has been a result of both demand-side (expansion of user-fee exemptions, health equity funds, vouchers and community-based health insurance) and supply-side (midwife training, midwifery incentive scheme in public facilities and ban on traditional birth attendants assisting with home births) policies and schemes (Dingle et al. 2013; Ir et al. 2015). Since Burkina Faso implemented a policy subsidizing fees for skilled birth attendance in 2007, the facility–delivery rate has increased, particularly among poor and rural women, alongside reducing household expenditures on care ( Ridde et al. 2011; FEMHealth, 2014; Langlois et al. 2015). Our analysis showed that considering women’s behaviours and choices within a life course framework—by focusing on continuity of care—can provide useful perspectives to help understand the ways in which health systems are successful in progressing toward achieving universal and equitable coverage with maternal and newborn care. In particular, our findings that women largely tend to remain in the location of the first birth highlights the importance of increasing facility delivery rates for first-order births and ensuring women delivering in health facilities receive good quality care, helping to ensure retention in facility-based care for subsequent births.
Supplementary Data
Supplementary data are available at HEAPOL online.
Funding
This study was supported by funding from MSD, through its MSD for Mothers program. Funding was used for general financial support, including staff salaries, travel, and overhead. MSD had no role in the design, collection, analysis and interpretation of data, in writing of the manuscript, or in the decision to submit the manuscript for publication. The content of this publication is solely the responsibility of the authors and does not represent the official views of MSD. MSD for Mothers is known as Merck for Mothers in the United States and Canada.
Conflict of interest statement. None declared.
Supplementary Material
References
- Adjiwanou V, Legrand T.. 2013. Does antenatal care matter in the use of skilled birth attendance in rural Africa: a multi-country analysis. Social Science & Medicine 86: 26–34. [DOI] [PubMed] [Google Scholar]
- Alkema L, Chou D, Hogan D, United Nations Maternal Mortality Estimation Inter-Agency Group et al. 2015. Global, regional, and national levels and trends in maternal mortality between 1990 and 2015, with scenario-based projections to 2030: a systematic analysis by the UN Maternal Mortality Estimation Inter-Agency Group. Lancet 387: 462–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Annear P. 2010. A comprehensive review of the literature on health equity funds in Cambodia 2001–2010 and annotated bibliography. HEALTH POLICY AND HEALTH FINANCE KNOWLEDGE HUB Working paper series. Melbourne, Australia: Nossal Institute for Global Health, The University of Melbourne.
- Bai J, Wong FW, Bauman A, Mohsin M.. 2002. Parity and pregnancy outcomes. American Journal of Obstetrics & Gynecology 186: 274–8. [DOI] [PubMed] [Google Scholar]
- Barros AJ, Ronsmans C, Axelson H. et al. 2012. Equity in maternal, newborn, and child health interventions in Countdown to 2015: a retrospective review of survey data from 54 countries. Lancet 379: 1225–33. [DOI] [PubMed] [Google Scholar]
- Bell J, Curtis SL, Alayón S.. 2003. Trends in delivery care in six countries DHS Analytical Studies No. 7. Calverton, Maryland: ORC Macro and International Research Partnership for Skilled Attendance for Everyone (SAFE). [Google Scholar]
- Benova L, Macleod D, Footman K. et al. 2015. Role of the private sector in childbirth care: cross-sectional survey evidence from 57 low- and middle-income countries using Demographic and Health Surveys. Tropical Medicine & International Health 20: 1657–73. [DOI] [PubMed] [Google Scholar]
- Boerma JT, Bryce J, Kinfu Y, Axelson H, Victora CG.. 2008. Mind the gap: equity and trends in coverage of maternal, newborn, and child health services in 54 Countdown countries. Lancet 371: 1259–67. [DOI] [PubMed] [Google Scholar]
- Bohren MA, Hunter EC, Munthe-Kaas HM. et al. 2014. Facilitators and barriers to facility-based delivery in low- and middle-income countries: a qualitative evidence synthesis. Reproductive Health 11: 71.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dingle A, Powell-Jackson T, Goodman C.. 2013. A decade of improvements in equity of access to reproductive and maternal health services in Cambodia, 2000–2010. International Journal of Equity Health 12: 51.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- FEMHealth 2014. Effects of subsidising maternal and neonatal health care in Burkina Faso: “it’s good but still not enough”!. http://www.abdn.ac.uk/femhealth/documents/Deliverables/PAC00132_Policy_Document_Burkina-ENGLISHLO.pdf, accessed 25 October 2015. Bobo-Dioulasso, Burkina Faso: AFRICSanté.
- Gabrysch S, Campbell OM.. 2009. Still too far to walk: literature review of the determinants of delivery service use. BMC Pregnancy Childbirth 9: 34.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guliani H, Sepehri A, Serieux J.. 2012. What impact does contact with the prenatal care system have on women's use of facility delivery? Evidence from low-income countries. Social Science & Medicine 74: 1882–90. [DOI] [PubMed] [Google Scholar]
- Hashim N, Naqvi S, Khanam M, Jafry HF.. 2012. Primiparity as an intrapartum obstetric risk factor. Journal of Pakistan Medical Association 62: 694–8. [PubMed] [Google Scholar]
- Ir P, Korachais C, Chheng K. et al. 2015. Boosting facility deliveries with results-based financing: a mixed-methods evaluation of the government midwifery incentive scheme in Cambodia. BMC Pregnancy Childbirth 15: 170.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson FA, Padmadas SS, Matthews Z.. 2013. Are women deciding against home births in low and middle income countries? PLoS ONE 8: e65527.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langlois EV, Karp I, Serme JD, Bicaba A.. 2015. Effect of a policy to reduce user fees on the rate of skilled birth attendance across socioeconomic strata in Burkina Faso. Health Policy and Planning 31: 462–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malkiel A, Pnina M, Aloni H, Gdansky E, Grisaru-Granovsky S.. 2008. Primiparity: a traditional intrapartum obstetric risk reconfirmed. The Israel Medicine Association Journal 10: 508–11. [PubMed] [Google Scholar]
- Mason L, Dellicour S, Ter Kuile F. et al. 2015. Barriers and facilitators to antenatal and delivery care in western Kenya: a qualitative study. BMC Pregnancy Childbirth 15: 26.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mgaya AH, Massawe SN, Kidanto HL, Mgaya HN.. 2013. Grand multiparity: is it still a risk in pregnancy?. BMC Pregnancy Childbirth 13: 241.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montagu D, Yamey G, Visconti A, Harding A, Yoong J.. 2011. Where do poor women in developing countries give birth? A multi-country analysis of demographic and health survey data. PLOS ONE 6: e17155.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moyer CA, Mustafa A.. 2013. Drivers and deterrents of facility delivery in sub-Saharan Africa: a systematic review. Reproductive Health 10: 40.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute of Public Health, National Institute of Statistics [Cambodia] & ORC MACRO 2006. Cambodia Demographic and Health Survey 2005. Phnom Penh, Cambodia and Calverton, Maryland, USA: National Institute of Public Health, National Institute of Statistics and ORC Macro. [Google Scholar]
- National Institute of Statistics, Directorate General for Health & ICF International 2015. Cambodia Demographic and Health Survey 2014. Phnom Penh, Cambodia, and Rockville, Maryland, USA: National Institute of Statistics, Directorate General for Health, and ICF International. [Google Scholar]
- Rich-Edwards J. 2002. . A life course approach to women’s reproductive health. In: Kuh D, Hardy R (eds). A Life Course Approach to Women’s Health. London: Oxford University Press. [Google Scholar]
- Ridde V, Richard F, Bicaba A, Queuille L, Conombo G.. 2011. The national subsidy for deliveries and emergency obstetric care in Burkina Faso. Health Policy and Planning 26: ii30–40. [DOI] [PubMed] [Google Scholar]
- Russ SA, Larson K, Tullis E, Halfon N.. 2014. A lifecourse approach to health development: implications for the maternal and child health research agenda. Maternal & Child Health Journal 18: 497–510. [DOI] [PubMed] [Google Scholar]
- Shankar A, Bartlett L, Fauveau V, Islam M, Terreri N. & Countdown to Maternal Health Group. 2008. Delivery of MDG 5 by active management with data. Lancet 371: 1223–4. [DOI] [PubMed] [Google Scholar]
- Stephenson R, Tsui AO.. 2002. Contextual influences on reproductive health service use in Uttar Pradesh, India. Studies in Family Planning 33: 309–20. [DOI] [PubMed] [Google Scholar]
- Tripathi V, Stanton C, Strobino D, Bartlett L.. 2015. Development and validation of an index to measure the quality of facility-based labor and delivery care processes in Sub-Saharan Africa. PLoS ONE 10: e0129491.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNICEF and World Health Organization 2015. Countdown to 2015: a decade of tracking progress for maternal, newborn and child survival. The 2015 Report. Geneva, Switzerland: WHO.
- United Nations Department of Economic and Social Affairs—Population Division 2015. World population prospects: the 2015 revision, key findings and advance tables. Working Paper No. ESA/P/WP.241. New York, NY: United Nations.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.