Abstract
National Strategic Plans (NSPs) for HIV/AIDS are country planning documents that set priorities for programmes and services, including a set of targets to quantify progress toward national and international goals. The inclusion of sex-disaggregated targets and targets to combat gender inequality is important given the high disease burden among young women and adolescent girls in Sub-Saharan Africa, yet no comprehensive gender-focused analysis of NSP targets has been performed. This analysis quantitatively evaluates national HIV targets, included in NSPs from eighteen Sub-Saharan African countries, for sex-disaggregation. Additionally, NSP targets aimed at reducing gender-based inequality in health outcomes are compiled and inductively coded to report common themes. On average, in the eighteen countries included in this analysis, 31% of NSP targets include sex-disaggregation (range 0–92%). Three countries disaggregated a majority (>50%) of their targets by sex. Sex-disaggregation in data reporting was more common for targets related to the early phases of the HIV care continuum: 83% of countries included any sex-disaggregated targets for HIV prevention, 56% for testing and linkage to care, 22% for improving antiretroviral treatment coverage, and 11% for retention in treatment. The most common target to reduce gender inequality was to prevent gender-based violence (present in 50% of countries). Other commonly incorporated target areas related to improving women’s access to family planning, human and legal rights, and decision-making power. The inclusion of sex-disaggregated targets in national planning is vital to ensure that programmes make progress for all population groups. Improving the availability and quality of indicators to measure gender inequality, as well as evaluating programme outcomes by sex, is critical to tracking this progress. This analysis reveals an urgent need to set specific and separate targets for men and women in order to achieve an equitable and effective HIV response and align government planning with international priorities for gender equality.
Keywords: HIV, AIDS, National Strategic Plans, Sub-Saharan Africa, gender targets
Key Messages
National Strategic Plans (NSPs) for HIV/AIDS are critical planning documents that set priorities and targets for a country’s response to the HIV epidemic, influence donor funding priorities, and guide data collection for domestic and international monitoring and evaluation.
Given the disproportionately high HIV burden among young women and adolescent girls in Sub-Saharan Africa, disaggregation of national targets by sex and age is important for identifying priority populations and monitoring the progress towards achieving international HIV goals.
This analysis reveals that NSPs for countries in Sub-Saharan Africa, with high HIV burden in young women, do not consistently set targets for men and women separately along the HIV care continuum or create targets designed to advance gender equality.
Strengthening NSPs to include gender equality and sex-disaggregated targets is crucial for monitoring and evaluating outcomes for both men and women, aligning donor investments with highest need, improving government accountability, and achieving a more robust domestic and international response to HIV/AIDS.
Background
In 2016, the United Nations General Assembly adopted the Political Declaration on Ending AIDS and affirmed its commitment to eradicating the epidemic by 2030 (United Nations 2016). The agreement committed signatory member states to the ‘90-90-90’ treatment targets and provided a series of ‘Fast Track’ targets necessary so that by 2020, 90% of people living with human immunodeficiency virus (HIV) will know their status, 90% of people diagnosed with HIV will receive sustained antiretroviral (ARV) therapy and 90% of people receiving ARV therapy will have viral suppression (UNAIDS 2014). In parallel, the United Nations developed 169 targets to measure progress toward its 17 Sustainable Development Goals (SDGs) that included the goal of ending the HIV epidemic by 2030.
Monitoring progress toward international HIV goals is fundamentally dependent on the systematic collection and reporting of quality country-level data. In the majority of countries with high HIV disease burden, governments periodically release strategic documents detailing their national public health priorities and targets. These National Strategic Plans (NSPs) for HIV/AIDS serve as a central guide by which programmes and activities will be prioritized in a 5-year evaluation period, and identify which targets should be measured and monitored in order to quantify success toward the country’s strategic objectives. Country data collected in order to measure progress toward NSP targets serve as the basis for tracking international priorities such as the UN Fast-Track and the SDGs targets. Additionally, as part of its country-led approach, the Global Fund encourages countries to base their applications for funding on NSPs, further emphasizing their importance in driving country programming and resource allocation.
The extent to which HIV targets in NSPs are disaggregated by sex and age is a measure of quality, and has important implications for county data collection, monitoring and programming. Disaggregated targets are necessary to track how the HIV epidemic is affecting different segments of the population, and if programmatic efforts are responsive to the unique needs of those populations. The President's Emergency Plan for AIDS Relief (PEPFAR) has recommended that all country programmes should disaggregate all epidemiological and programmatic data by sex and age, as well as advocate for and support national level disaggregated data (PEPFAR 2013).
The extent to which NSPs are responsive to gender disparities in HIV can also be assessed through the inclusion of targets specifically aimed at reducing gender inequality in health outcomes. Recent WHO guidance (2016) for increasing gender responsive national monitoring and evaluation systems defines a gender inequality target as one ‘that measures gender inequality directly or through proxies’. These include targets for social or structural factors that are linked to HIV acquisition in women including economic marginalization, gender-based violence (GBV), and gender-based norms that disempower women in intimate partnerships (WHO, 2016). The importance of addressing these structural drivers of HIV in women has been demonstrated through peer-reviewed literature and emphasized through donor investment priorities (Underwood 2011; Bandiera et al. 2012; Gibbs et al. 2012; Hargreaves 2013). PEPFAR’s DREAMS programme (Determined Resilient AIDS Free Mentored and Safe) was specifically designed to address not only the behavioural but also the social and structural determinants of HIV among adolescent girls and young women (AGYW) in Sub-Saharan Africa (PEPFAR, 2014; Fleischman and Peck, 2015). The development and inclusion of targets to track gender inequality in NSPs is necessary to monitor changes over time in these key social and structural influencers of HIV outcomes in women and girls.
The development of gender responsive NSPs is of particular importance in settings with high sex disparities in HIV disease burden. HIV/AIDS is the leading cause of death among AGYW in many low and middle income countries, including in Sub-Saharan Africa (Melaku et al. 2014). In Sub-Saharan African countries, 56% of new infections are in women, due to a combination of biological vulnerability and predisposing social risk factors including lack of education, education income inequality, and violence, and harmful norms (UNAIDS 2016a). This sex-disparity is even more pronounced among younger populations; in Southern Africa, 90% of new infections among 10- to 19-year-olds were in AGYW in 2015 (UNAIDS 2016b). In these settings, the inclusion of targets to track gender inequality, as well as the collection and inclusion of sex-disaggregated health data in HIV national planning, is vital to ensure that programmes make progress for all population groups and identify those being left behind.
Despite the importance of high-quality HIV targets and gender responsive NSPs, research and reviews to monitor government HIV targets has been limited. This may be in part because NSPs are country-specific, are not stored centrally, and do not follow standardized structures, making the extraction of information difficult and complicating country comparisons. However, the analysis of these documents is a valuable strategy to examine country priority-setting and identify gaps in both domestic and international HIV monitoring capacity. The primary objective of this analysis is to assess the extent to which sex-disaggregated and gender-equality HIV targets are included in the NSPs for HIV/AIDS of high burden countries in Sub-Saharan African.
Methods
Data collection
The most recent publicly available NSPs were downloaded directly from country Ministry of Health websites, or from the International Labor Organization’s website, in June, 2016. Countries in Sub-Saharan Africa with generalized HIV epidemics in youth, defined as HIV prevalence greater than one percent among young people (ages 15–24) were included: Botswana, Cameroon, Central African Republic, Republic of Congo, Guinea-Bissau, Kenya, Lesotho, Malawi, Mozambique, Namibia, Nigeria, Rwanda, South Africa, Swaziland, Tanzania, Uganda, Zambia and Zimbabwe (UNAIDS AIDSinfo http://aidsinfo.unaids.org/.). The authors reviewed the NSPs from each country and manually extracted each nation’s self-identified HIV targets and related indicators (n = 815). Formal submission to an ethical review board was not required for this study, which includes only secondary data analysis of publicly available content not involving human subjects. This review uses the World Health Organization’s (WHO) definition of gender-sensitive indicators, which define; (i) sex-specific indicators as those which pertain only to women or men, (ii) sex-disaggregated indicators as those which measure the difference between women and men in relation to a particular metric and (iii) gender-equality indicators as those that measure gender inequality directly or through proxies for gender inequality (i.e. violence against women) (WHO 2016).
Sex-disaggregated targets
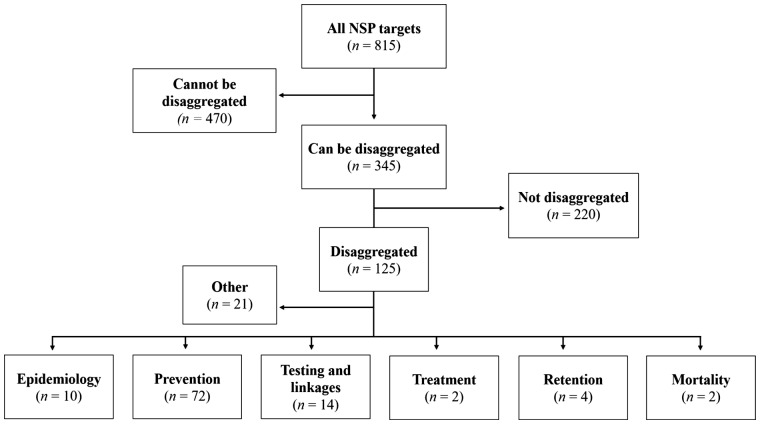
To measure the percent of country targets that are disaggregated by sex, the authors included only targets for topic areas where disaggregation was possible; for example, it is both possible and logical to track new infection rates and the proportion of people receiving treatment and retained in care, by sex (Figure 1). Targets that could not be disaggregated by sex were excluded (n = 470). These included targets related to policy, health system governance, and health facilities. Sex-specific (i.e. for women or men) targets were also excluded. These included targets related to reducing mother-to-child transmission, addressing HIV in men who have sex with men or female sex workers, increasing male circumcision, or reaching infants/children between 0 and 5 years. All targets were independently reviewed by two investigators and coded as sex-disaggregated if a numeric target was set for men and for women separately, or if any data related to the monitoring of the target (i.e. baseline or interim data) were reported for both men and women. Targets were coded as non-disaggregated if the target was set for ‘adults’ or ‘adolescents’ overall, without reporting any baseline or progress data separately by sex. All coder disagreements were discussed and targets were re-reviewed to yield agreement. In the cases of target ambiguity, for example, when a target referenced men and women but did not present data separately for each sex, targets were coded as non sex-disaggregated. The percent of targets disaggregated for each country was calculated as the number of sex-disaggregated targets divided by the total number of targets that could be disaggregated in each country.
Figure 1.
Flowchart for NSP target coding.
Each of the sex-disaggregated targets was grouped broadly into five categories: epidemiology, prevention, testing and linkage, provision of treatment, and retention in care. Epidemiological targets included measures for population trends, specific to reducing HIV incidence, prevalence, or mortality. The prevention category included targets for prevention activities, including: reducing high-risk sexual behaviours (concurrent partnerships, alcohol use), increasing condom use, safe injection drug use, school attendance and HIV education. The remaining categories (testing/linkage, treatment, and retention in care) were selected to reflect the stages of the HIV care continuum and are considered core indicators of clinical HIV care (Institute of Medicine 2012).
Targets for gender equality
All targets related to improving gender equality in health outcomes, defined as indicators to measure the social or structural drivers of HIV for AGYW (WHO 2016), were extracted (n = 43). All targets which the authors deemed to (i) meet the WHO criteria for a gender-equality target and, (ii) respond to current evidence in the field for social or structural drivers of HIV in AGYW, were thematically coded using an inductive approach. Initial codes were grouped into sub-themes and then categorized into five larger themes including: (i) integration of sexual and reproductive health (SRH) and HIV programming, (ii) improving pregnancy outcomes or increasing the use of modern contraception (methods other than fertility awareness and withdrawal), (iii) reducing gender-based or sexual violence, (iv) improving rights or access to resources for women and girls and (v) improving AGWY’s school attendance/access.
Previous research has demonstrated a link between these structural factors and women’s sexual health outcomes in many African settings. The integration of SRH services can improve a women’s uptake of both family planning and HIV services, as well as improve her satisfaction and continued engagement with care (Adamchak et al. 2010; Church and Mayhew 2009; Kennedy et al. 2010). There is substantial evidence that GBV and male relationship control can both directly and indirectly increase a women’s risk of HIV though non-protected forced sex, and through the downstream effects of violence such as future risky sex, less protective powers, and substance use (Maman et al. 2000; Dunkle et al. 2004; Jewkes et al. 2010). Adolescent girls’ economic opportunity and access to resources has also been shown to be associated with sexual health outcomes; for example providing young women loans, cash-transfers, or vocational training can decrease sexual risk taking, drug use, engagement in transactional sex, and increase condom use (Erulkar and Chong 2005; Ssewamala et al. 2010; Bandiera et al. 2012; Rotheram-Borus et al. 2012). Finally, research has also shown that interventions to improve girls’ school attendance through cash transfers, reduced fees and/or social support, have decreased the risk of HIV infection, reduced dropout rates, early pregnancy, and adolescent marriage rates (Duflo et al. 2006; Hallfors et al. 2011; Baird et al. 2012). Although there are certainly other relevant social and structural factors that influence AGYW’s HIV outcomes, only those factors that were found in the NSPs targets are represented in this paper. Categories are mutually exclusive, where all identified targets that met criteria are represented in only one category.
Results
Overall, the analysis found inconsistent incorporation of sex-disaggregated HIV targets within NSPs of Sub-Saharan African countries. For the eighteen countries included in this review, the proportion of general population targets that were sex-disaggregated ranged from 0% (Botswana, Cameroon and Mozambique) to 92% (Zambia), with an average of 31% across countries (Table 1). Only the NSPs from South Africa, Swaziland and Zambia disaggregated a majority (>50%) of their targets by sex. Sex-disaggregation was more common among targets related to the early phases of the HIV care continuum, with 83% (15/18) of countries including sex-disaggregated targets related to HIV prevention (i.e. condom use and reducing high-risk sexual behaviours). In contrast, sex-disaggregated targets are less common in the later phases of the care continuum—with 56% (10/18) of countries setting targets related to HIV testing and linkage to care, 22% (4/18) setting targets for improving ARV treatment coverage and 11% (2/18) disaggregating targets by sex aimed at increasing long-term access and retention in ARV treatment programmes. Sex-disaggregated national targets for reducing HIV prevalence, incidence or mortality were found in 33% (6/18) of countries. Only Zambia and South Africa set at least one sex-disaggregated target across all pillars of the HIV care continuum. Examples of commonly included targets (both sex-disaggregated and non-disaggregated) are presented in Table 2.
Table 1.
Sex-disaggregated targets and indicators in NSPs of African countries with generalized HIV epidemics in youth
| Country | Sex-disaggregated targets (%)a | Epidemiologyb | Preventionc | Testing and linkaged | Treatmente | Retentionf |
|---|---|---|---|---|---|---|
| Botswana | 0·0 | |||||
| Cameroon | 0·0 | |||||
| Central African Republic | 9·7 | √ | √ | |||
| Republic of Congo | 11·8 | √ | √ | |||
| Guinea-Bissau | 16·7 | √ | √ | |||
| Kenya | 22·2 | √ | ||||
| Lesotho | 36·8 | √ | √ | |||
| Malawi | 38·1 | √ | √ | √ | ||
| Mozambique | 0·0 | |||||
| Namibia | 30·4 | √ | √ | √ | ||
| Nigeria | 31·3 | √ | ||||
| Rwanda | 42·3 | √ | √ | √ | ||
| South Africa | 82·6 | √ | √ | √ | √ | √ |
| Swaziland | 52·9 | √ | √ | √ | ||
| Tanzania | 40·9 | √ | √ | √ | ||
| Uganda | 37·5 | √ | ||||
| Zambia | 92·3 | √ | √ | √ | √ | √ |
| Zimbabwe | 14·3 | √ |
Calculation includes only targets for the general population—excluding targets for: policy and health system governance, health facilities, PMTCT, key populations and children 0–5 years.
Includes sex-disaggregated targets for HIV incidence, prevalence or mortality.
Includes sex-disaggregated targets for condom use, reducing high-risk sexual behaviours (concurrent partnerships, alcohol use), safe injections and HIV education.
Includes sex-disaggregated targets for HIV testing and counselling, or initiation in a pre-ART programme.
Includes sex-disaggregated targets for increased ARV treatment coverage.
Includes sex-disaggregated targets for increasing long-term access and use of ARVs.
Table 2.
Common indicators/targets by category
| Sex-disaggregated | Non-sex disaggregated | |
|---|---|---|
| Epidemiology | HIV prevalence in the population aged 15–24 (disaggregated by sex and urban/rural)—(Rwanda NSP 2013–18) | HIV prevalence in youth ages 15-24—(Republic of Congo NSP 2009–13) |
| Prevention | Men and women aged 15-49 who had 2 or more sexual partners in the last 12 months who reported using a condom during the last sexual intercourse to increase from 52.3% for men and 37.5% for women in 2009 to 80% for men and 70% for women by 2015/16—(Lesotho NSP 2011–16) | Proportion of people aged 15-49 years who always use condoms with non-regular partners in the last 12 months—(Botswana NSP 2010–16) |
| Testing and Linkage | Percentage of women and men aged 15–49 who received an HIV test in the last 12 months and who know the results of the last test—(Malawi NSP 2011–16) | Percent of adults that are tested and know their serostatus—(Republique de Centraafricaine (CAR), Comite National de Lutte Contre le SIDA 2012–16) |
| Treatment | Percent of people per year becoming eligible who receive ART (reported for men and women)—(South Africa NSP, 2012–16) | Improved coverage of ARV treatment—(Zimbabwe NSP, 2015–18) |
| Retention | Percentage of people (reported as men and women separately) who initiated ART who are alive and on treatment at 12, 24, 36 and 60 months—(Zambia NSP 2014–16) | Increase retention to antiretroviral treatment after three years from 52% to 70% by 2019—(Mozambique NSP 2015–19) |
This analysis also found inconsistent inclusion of gender-equality targets to combat the social and structural drivers of HIV in women. In total, 15 of the 18 countries (83%) set at least one target to improve gender-equality; however, there are prominent gaps across countries. No gender-equality targets were found in the NSPs of Botswana, Guinea-Bissau or Mozambique. The most commonly incorporated category of gender-equality target in NSPs was to prevent or reduce GBV, present in 50% (9/18) of country’s NSPs (Table 3). Common GBV targets related to improving post-assault care for survivors of violence, reducing the proportion of women who experience intimate partner violence, and changing norms about acceptable behaviour within partnerships.
Proportion of ever-married or partnered women aged 15-49 who experienced physical or sexual violence from a male intimate partner in the past 12 months reduced to 20% by 2018 (from 40.7% in 2007/08) (GBV indicator, Tanzania) (United Republic of Tanzania 2013)
Table 3.
Gender-equality targets in NSPs of African countries with generalized HIV epidemics in youth
| Country | Integration of SRH and HIV | Improving pregnancy outcomes or contraception coverage | Gender-based or sexual violence | Improving rights or access to resources for women and girls | AGWY school attendance/access |
|---|---|---|---|---|---|
| Botswana | |||||
| Cameroon | √ | ||||
| Central African Republic | √ | √ | √ | ||
| Republic of Congo | √ | ||||
| Guinea-Bissau | |||||
| Kenya | √ | √ | |||
| Lesotho | √ | ||||
| Malawi | √ | √ | |||
| Mozambique | |||||
| Namibia | √ | √ | √ | √ | |
| Nigeria | √ | √ | √ | ||
| Rwanda | √ | √ | |||
| South Africa | √ | √ | |||
| Swaziland | √ | √ | |||
| Tanzania | √ | ||||
| Uganda | √ | √ | √ | ||
| Zambia | √ | ||||
| Zimbabwe | √ |
Six of the 18 countries (33%) set targets to improve the integration of family planning and HIV services, such as ‘Percent of health facilities offering family planning services for HIV-positive women’—SRH/HIV integration indicator, CAR (2012). Seven of the 18 (39%) set targets to improve pregnancy outcomes or contraception coverage. Commonly set targets related to increasing the availability of family planning services for women living with HIV:
Percent of women aged 15-59 living with HIV and accessing comprehensive family planning package to increase by 20% by 2012/13 and 50% by 2015/16 (Family Planning indicator, Namibia) (Republic of Namibia 2010)
Additionally, five countries (28%) set at least one target designed to improve the legal rights and access to economic resources for women and girls. Common themes in these targets included expanding poverty alleviation programmes, women’s access to land, and increasing decision making power for women within households.
Percentage of married women participate in all three decisions pertaining to their own health care, major household purchases, and visits to their family or relatives (Access to rights and resources indicator, Uganda) (Uganda 2015)
Two of the 18 countries (11%) included targets for improving school attendance for AGWY. Although many countries included targets to increase school attendance of adolescents overall, or for particularly at-risk children, such as orphans, only two countries included sex-specific indicators that would allow for monitoring of gender disparities in school attendance.
Discussion
The results of this study indicate a lack of consistent disaggregation by sex for national HIV targets in Sub-Saharan African countries with the highest HIV burden in youth. Aggregated outcome and progress data may mask significant inequalities in sub-populations. Indeed, countries that report only HIV data combined for men and women may suggest population-level achievements while masking significant sex-differences. The future development of NSPs must ensure that all general population targets are disaggregated by sex and age, where applicable. This analysis also reveals that sex-disaggregation is most often specified for targets in the area of HIV prevention but less so in the areas of treatment and retention in care. Since sex differences occur in the acquisition of HIV, its diagnosis, treatment initiation, and retention in care, it is crucial for national governments to include sex-disaggregated targets at all stages of the care continuum. International funders and technical partners, such as the Global Fund, that participate in NSP development should provide increased technical assistance around target setting to ensure that sex-disaggregated targets are set and that data are reported for any differences.
This analysis further showed gaps in the incorporation of gender-equality targets NSPs across countries, and therefore demonstrates a significant opportunity to improve the gender-responsiveness of plans through increased inclusion of gender-equality targets. Since NSP targets must be responsive to the local social drivers of HIV in women and girls, it cannot be asserted that every country should include every category of gender-equality target presented here. However, these broad social and structural factors have been shown to be key influencers of the HIV epidemic in AGYW across many Sub-Saharan African settings. NSPs that are highly gender-responsive will move beyond targets that track individual behaviour to also include a comprehensive set of targets to measure gender equality as a major structural driver of local epidemics.
Recent WHO guidance aimed at increasing gender-sensitive monitoring and evaluation in NSPs recommends measuring intimate partner violence as a priority outcome related to HIV and as a proxy for gender inequality (WHO 2016). This review shows that indicators for GBV are among the most commonly included targets related to gender-inequality, albeit only used as an indicator in half of countries in this study. Given the substantial link between violence and HIV acquisition (Jewkes et al. 2010), as well as the potential to use the prevalence of intimate partner violence as a proxy for gender inequality, incorporating GBV-related indicators in future NSPs is of upmost importance. Additionally, targets to improve school attendance among AGYW are currently only included in two of the 18 countries. Existing evidence points to the multiple health benefits of girls’ education, which include a reduction in HIV risk (Duflo et al. 2006; Hallfors et al. 2011; Baird et al. 2012). Efforts should be made to disaggregate school attendance targets by sex and age in order to make sex-specific monitoring possible in future national planning and evaluating efforts.
This article provides an analysis of sex-disaggregation in NSP targets, as well as an overview of which countries have included gender-equality targets across several categories of social and structural drivers of HIV. Although a formal analysis of the quality of these targets is outside the scope of this article, it is worth noting that some targets/indicators lacked the specificity and precision to be effective and measurable indicators. For example the target, ‘Reduced social exclusion for PLHIV, key populations, women, men, boys and girls’ (Kenya Ministry of Health 2014), does not include a specific target population or define the type of activities that are prescribed. It is unclear how this target will be measured or if it can be used to track changes in the inclusion of marginalized populations in Kenya. Governments could improve the gender-responsiveness of NSPs by setting targets for one relevant subpopulation or age group of women and by defining the specific intervention to be measured—taking into account what is feasible given available data. Successful targets may narrow in on one measurable outcome that can be used to track the success of a programme or indicate gender inequalities more broadly. For example the target ‘Increase the percent of women and men aged 60+ who have received an old age grant in the past 12 months to 70%’ (Republic of Namibia 2010) is focused on one measurable outcome. Improvements could still be made to ensure that these data were disaggregated by sex.
Despite the challenges of measuring the structural drivers of HIV, which is complicated by incomplete data and lack of standardized metrics, it is vital that countries include targets to address these issues in order to ensure that women’s health and rights are prominent on the national agenda. Improving the quality of HIV targets generally to ensure that they are specific and measurable will improve monitoring and evaluation efforts over time, as well as foster greater government accountability for identified objectives.
Limitations
This analysis is limited by accessibility of country NSPs. Although every effort was made to obtain the most recent NSP from each country, it is possible that there are other national documents containing HIV targets, which have not been made publicly available and were therefore not included in this review. However, this review does reflect those targets which have been published and for which national governments are responsible. Additionally, in the current analysis, targets that were ambiguous were coded as non-disaggregated, which may have resulted in an underestimation of the number of sex-disaggregated targets in NSPs. Indeed, targets may have been set for the general population and subsequently analysed for sex differences, but these would not be identified as sex-disaggregated. Such population aggregated targets are not guaranteed to result in sex-disaggregated data collection and reporting, and therefore this coding decision reflects the need for greater specificity in target formulation for both sexes.
Finally, this analysis cannot evaluate the extent to which NSP targets are driving country programming, resource allocation, or whether targets are actually being met. Future work must analyse specific country data and target setting over time to examine the potential impacts of gender-responsive NSPs, including if disaggregating data by sex results in concrete actions to address the HIV epidemic in women and improves results.
Conclusion
The quality of NSP targets matters for local, national, and international efforts to combat HIV. This analysis reveals an urgent need to set specific and separate targets for men and women in order to achieve an equitable and effective HIV response, as well as to align government planning with international priorities. Gender-equality targets are critical to addressing the structural and behavioural drivers of HIV, and should be incorporated into all NSPs in Sub-Saharan Africa. We note that it is possible to reach national and global HIV goals while failing to make progress for women and girls; indeed, the world achieved the Millennium Development Goal 6.A, by beginning to reverse the spread of HIV, yet during this same period, the HIV infection rate among young women in Sub-Saharan Africa doubled as compared with that of young men (UNAIDS 2015). Universal disaggregation of data by sex in national target setting and reporting across the entire HIV care continuum is needed to identify sex-specific gaps in HIV service delivery and ensure that the world is not declaring progress in fighting the HIV/AIDS pandemic while leaving many women behind.
Acknowledgements
We thank the dedicated staff of amfAR, the Foundation for AIDS Research, for providing the technical assistance and resources required to undertake this analysis; specifically Brian Honermann and Greg Millett.
Funding. The authors report no external funding source for this study
Conflict of interest statement. None declared.
References
- Adamchak S, Janowitz B, Liku J, Munyambanza E, Grey T, Keyes E. 2010. Study of Family Planning and HIV Integrated Services in Five Countries: Final Report. Research Triangle Park, NC: Family Health International.
- Baird SJ, Garfein RS, McIntosh CT, Özler B.. 2012. Effect of a cash transfer programme for schooling on prevalence of HIV and herpes simplex type 2 in Malawi: a cluster randomised trial. The Lancet 379:1320–9. [DOI] [PubMed] [Google Scholar]
- Bandiera O, Buehren N, Burgess R.. et al. 2012. Empowering Adolescent Girls: Evidence from a Randomized Control Trial in Uganda. Washington, DC: World Bank. [Google Scholar]
- Church K, Mayhew SH.. 2009. Integration of STI and HIV prevention, care, and treatment into family planning services: a review of the literature. Studies in Family Planning 40: 171–86. [DOI] [PubMed] [Google Scholar]
- Duflo E, Dupas P, Kremer M, Sinei S. 2006. Education and HIV/AIDS Prevention: Evidence from a Randomized Evaluation in Western Kenya. Policy Research Working Paper; No. 4024. World Bank, Washington, DC.
- Dunkle KL, Jewkes RK, Brown HC.. et al. 2004. Gender-based violence, relationship power, and risk of HIV infection in women attending antenatal clinics in South Africa. The Lancet 363:1415–21. [DOI] [PubMed] [Google Scholar]
- Erulkar A, Chong E.. 2005. Evaluation of a Savings and Micro-Credit Program for Vulnerable Young Women in Nairobi. New York, NY, Population Council. [Google Scholar]
- Fleischman J, Peck K.. 2015. Addressing HIV Risk in Adolescent Girls and Young Women Washington DC, Center for Strategic & International Studies. April 2015. https://csis-prod.s3.amazonaws.com/s3fspublic/legacy_files/files/publication/150410_Fleischman_HIVAdolescentGirls_Web.pdf, accessed 10 November 2016.
- Gibbs A, Willan S, Misselhorn A, Mangoma J.. 2012. Combined structural interventions for gender equality and livelihood security: a critical review of the evidence from southern and eastern Africa and the implications for young people. Journal of the International AIDS Society 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hallfors D, Cho H, Rusakaniko S. et al. 2011. Supporting adolescent orphan girls to stay in school as HIV risk prevention: evidence from a randomized controlled trial in Zimbabwe. American Journal of Public Health 101:1082–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hargreaves JR. 2013. Incorporating A Structural Approach Within Combination HIV Prevention: An Organising Framework. Structural Approaches to HIV Prevention Position Paper Series. Arlington, VA: USAID’s AIDS Support and Technical Assistance Resources, AIDSTAR-One, Task Order 1, and London: UKaid’s STRIVE research consortium.
- Institute of Medicine. 2012. Monitoring HIV Care in the United States: Indicators and Data Systems. Ford MA, Spicer CM, editors. 15 March 2012. nationalacademies.org/hmd/Reports/2012/Monitoring-HIV-Care-in-the-United-States.aspx, accessed 10 November 2016.
- Jewkes RK, Dunkle K, Nduna M, Shai N.. 2010. Intimate partner violence, relationship power inequity, and incidence of HIV infection in young women in South Africa: a cohort study. The Lancet 376: 41–8. [DOI] [PubMed] [Google Scholar]
- Kennedy CE, Spaulding AB, Brickley DB.. et al. 2010. Linking sexual and reproductive health and HIV interventions: a systematic review. Journal of the International AIDS Society 13: 26.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenya Ministry of Health. Kenya AIDS Strategic Framework, 2014/2015 – 2018/2019. National AIDS Control Council.
- Kingdom of Lesotho, National AIDS Commission. 2011. National HIV and AIDS Strategic Plan 2011/12 – 2015/16.
- Malawi National AIDS Commission. 2011. Malawi National HIV and AIDS Strategic Plan 2011-2016.
- Maman S, Campbell J, Sweat MD, Gielen AC.. 2000. The intersections of HIV and violence: directions for future research and interventions. Social Science and Medicine 50:459–78. [DOI] [PubMed] [Google Scholar]
- Melaku YA, Weldearegawi B, Aregay A.. et al. 2014. Causes of death among females-investigating beyond maternal causes: a community-based longitudinal study. BMC Research Notes 10: 629.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- PEPFAR. 2013. Updated Gender Strategy: FY2014 The President’s Emergency Plan for AIDS Relief. December, 2013. https://www.pepfar.gov/documents/organization/219117.pdf, accessed 17 October 2016.
- PEPFAR. 2014. DREAMS Core Package of Intervention Summary. The President’s Emergency Plan for AIDS Relief. 2014. https://www.pepfar.gov/documents/organization/269309.pdf, accessed 17 October 2016.
- Republic of Botswana National AIDS Coordinating Agency. 2009. The Second National Strategic Framework for HIV and AIDS: 2010-2016.
- Republic of Namibia, Ministry of Health and Social Services. 2010. National Strategic Framework for HIV and AIDS Response in Namibia, 2010/11 – 2015/16.
- Republic of Rwanda, Ministry of Health. 2013. Rwanda HIV and AIDS National Strategic Plan 2013-2018.
- Republic of Uganda, Uganda AIDS Commission. 2015. National HIV and AIDS Strategic Plan 2015/2016 – 2019/2020.
- Republic of Zambia National HIV/AIDS/STI/TB Council. 2014. National HIV AIDS Strategic Framework 2014-2016.
- Republica de Mocambique Conselho Nacional Decombate ao HIV/SIDA. 2015. Plano Estrategico Nacional de Resposta ao HIV e SIDA 2015-2019.
- Republique du Congo, Conseil National de Lutte Contre le SIDA. 2009. Cadre Strategique National de Lutte Contre le VIH/SIDA et les IST 2009-2013.
- Republique de Centraafricaine (CAR), Comite National de Lutte Contre le SIDA. 2012. Cadre Strategique National de Lutte Contre le VIH et le SIDA 2012-2016.
- Rotheram-Borus MJ, Lightfoot M, Kasirye R, Desmond K.. 2012. Vocational training with HIV prevention for Ugandan youth. AIDS and Behavior 16:1133–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- South African National AIDS Commission. 2011. National Strategic Plan on HIV, STIs and TB 2012-2016.
- Ssewamala FM, Han CK, Neilands TB, Ismayilova L, Sperber E.. 2010. Effect of economic assets on sexual risk-taking intentions among orphaned adolescents in Uganda. American Journal of Public Health 100:483–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Underwood C, Skinner J, Osman N, Schwandt H.. 2011. Structural determinants of adolescent girls’ vulnerability to HIV: views from community members in Botswana, Malawi, and Mozambique. Social Science and Medicine 73: 343–50. [DOI] [PubMed] [Google Scholar]
- UNAIDS. 2014. Fast-Track: Ending the AIDS Epidemic by 2030. The Joint United Nations Programme on HIV/AIDS. 18 November 2014. unaids.org/en/resources/documents/2014/JC2686_WAD2014report, accessed 2 September 2016.
- UNAIDS. 2015. How AIDS changed everything. Joint United Nations Programme on HIV/AIDS. http://www.unaids.org/sites/default/files/media_asset/MDG6Report_en.pdf, accessed 2 September 2016.
- UNAIDS. 2016a. Global AIDS Update 2016. Joint United Nations Programme on HIV/AIDS. unaids.org/sites/default/files/media_asset/global-AIDS-update-2016_en.pdf, accessed 2 September 2016.
- UNAIDS. 2016b. UNAIDS announces 18.2 million people on antiretroviral therapy, but warns that 15-24 years of age is a highly dangerous time for young women. 21 November 2016. Joint United Nations Programme on HIV/AIDS. unaids.org/en/resources/presscentre/pressreleaseandstatementarchive/2016/november/20161121_PR_get-on-the-fast-track, accessed 2 September 2016.
- United Nations 2016. Political declaration on HIV and AIDS: On the Fast-Track to Accelerate the Fight against HIV and to End the AIDS Epidemic by 2030. United Nations General Assembly. A/70/L.52 (7 June 2016), unaids.org/en/resources/documents/2016/2016-political-declaration-HIV-AIDS, accessed 10 November 2016.
- United Republic of Tanzania. 2013. Tanzania third national multi-sectoral strategic framework for HIV and AIDS (2013/14 – 2017/18). Prime Minister’s Office. Nov 2013.
- WHO. 2016. A tool for strengthening gender-sensitive national HIV and Sexual and Reproductive Health (SRH) monitoring and evaluation systems. World Health Organization. apps.who.int/iris/bitstream/10665/251903/1/9789241510370-eng.pdf?ua=1, accessed 2 September 2016.
- Zimbabwe National AIDS Council. 2015. Zimbabwe National HIV and AIDS Strategic Plan 2015-2018: Commitment Towards Fast Tracking 90.90.90 Targets by 2020 and Ending AIDS by 2030.