Abstract
Substantial investments have been made in clinical social franchising to improve quality of care of private facilities in low- and middle-income countries but concerns have emerged that the benefits fail to reach poorer groups. We assessed the distribution of franchise utilization and content of care by socio-economic status (SES) in three maternal healthcare social franchises in Uganda and India (Uttar Pradesh and Rajasthan). We surveyed 2179 women who had received antenatal care (ANC) and/or delivery services at franchise clinics (in Uttar Pradesh only ANC services were offered). Women were allocated to national (Uganda) or state (India) SES quintiles. Franchise users were concentrated in the higher SES quintiles in all settings. The percent in the top two quintiles was highest in Uganda (over 98% for both ANC and delivery), followed by Rajasthan (62.8% for ANC, 72.1% for delivery) and Uttar Pradesh (48.5% for ANC). The percent of clients in the lowest two quintiles was zero in Uganda, 7.1 and 3.1% for ANC and delivery, respectively, in Rajasthan and 16.3% in Uttar Pradesh. Differences in SES distribution across the programmes may reflect variation in user fees, the average SES of the national/state populations and the range of services covered. We found little variation in content of care by SES. Key factors limiting the ability of such maternal health social franchises to reach poorer groups may include the lack of suitable facilities in the poorest areas, the inability of the poorest women to afford any private sector fees and competition with free or even incentivized public sector services. Moreover, there are tensions between targeting poorer groups, and franchise objectives of improving quality and business performance and enhancing financial sustainability, meaning that middle income and poorer groups are unlikely to be reached in large numbers in the absence of additional subsidies.
Keywords: Private sector, private providers, maternal health, reproductive health, equity
Key Messages
Clinical social franchising has been a fast growing private sector intervention in recent years but concerns have emerged that the benefits are captured by the better off and fail to reach poorer groups.
We studied three maternal health social franchises in Uganda, Rajasthan and Uttar Pradesh and found that antenatal and delivery users were concentrated in higher wealth quintiles. However, the content of care received at social franchise visits did not vary by SES.
Although most social franchises acknowledge they will not reach the very poorest, the tension between targeting poorer groups and financial sustainability remains a challenge for this type of intervention.
Introduction
In many developing countries, private providers play a major role in healthcare provision, leading international agencies to support interventions to strengthen the care they provide, including training, social marketing, social franchising, targeted vouchers and accreditation (Montagu and Goodman, 2016). The private sector encompasses both for-profit and not-for-profit providers which are highly heterogeneous, ranging from sophisticated hospitals to small shops where staff have no qualifications, though a growing component of this sector is small and medium-sized private facilities. One concern often raised with initiatives that work with such private providers is that they may be inequitable, with their benefits obtained disproportionally by higher socio-economic status (SES) groups, who are able to afford private sector fees (Patouillard et al., 2007).
One of the fastest growing private sector interventions in recent years has been clinical social franchising, which aims to improve quality of care and increase utilization of quality services (Montagu et al., 2016). Eighty-three healthcare social franchising programmes were identified as being active in 2015 in low- and middle-income countries (LMIC), with 37 programmes emerging between 2007 and 2012 alone (Viswanathan et al., 2016). Social franchising applies commercial franchising business principles to support the provision of branded, quality-assured services of social importance, such as healthcare, via a network of private providers. The model has been applied to a wide range of services, mostly family planning, sexual and reproductive health services, safe motherhood, tuberculosis (TB), malaria, HIV/AIDS, abortion care and paediatric services. Other services such as dental and vision care are also present to a lesser extent. Although there is considerable variation across programmes, Viswanathan et al. identify a set of core characteristics that most have in common: (1) the presence of a third party administrator, typically an Non Governmental Organisation (NGO) which manages the brand and supervises the network providers through regular visits and audits, (2) the use of protocols and guidelines under which providers must operate, (3) a focus on the sale of healthcare services, in addition to healthcare commodities, (4) the aim of achieving self-sustainability both from the franchisor and franchisees’ perspectives and (5) the aim of providing quality-assured health services to the most under-served populations.
Although the social franchise model does not inherently include a focus on reaching poorer groups, the implementers of healthcare social franchises in LMIC generally have a stated goal of reaching vulnerable populations and providing care to the most in need, and the Clinical Social Franchising Compendium, compiled by the programmes themselves, considers equity as a key measure of performance (Viswanathan et al., 2016). Moreover, these programmes are nearly all heavily donor-supported, with the donors generally having a focus on reaching poorer groups and/or an interest in equity in distribution. As a result, equity has arisen as a policy concern around LMIC social franchises (Beyeler et al., 2013), though evidence on this topic remains patchy. Several published articles compare the SES of family planning social franchise clients with those visiting other provider types (Stephenson et al., 2004; Hennink and Clements, 2005; Montagu et al., 2005; Bishai, 2008; Shah et al., 2011). However, comparing franchise clients to those of other providers does not indicate how representative they are of the whole population, as e.g. it is possible that both facility types generally serve higher-income groups. Other studies have therefore compared franchise clients with the general population based on household surveys in the study area. In urban Kenya, franchise clients were broadly reflective of the communities where the providers practiced (Montagu et al., 2005), while in urban Pakistan two-thirds of franchise clients were in the top two SES quartiles and only 9% in the lowest quartile (Hennink and Clements, 2005). Other studies have compared franchise clients with the national SES distribution based on national household surveys, which gives a better indication of the overall equity impact. In Kenya, two-thirds of clients were in the top quintile nationally, and a fifth in the lowest quintile (Montagu et al., 2005). In contrast, a study of a TB franchise in Myanmar found the SES distribution of clients to be similar to the national distribution, and in urban areas franchise clinics served a higher proportion of poorer clients (Montagu et al., 2013). Similar data are reported in the Clinical Social Franchise Compendium for 15 of the 83 social franchises identified (Viswanathan et al., 2016); six of these programmes reported that over 90% of clients were in the top quintile nationally, with a further six over 75%. Only three programmes in India, Pakistan and Cambodia had over 40% of their clients in the bottom three quintiles.
So far, most studies have focused on family planning users, reflecting the predominance of these services in social franchise programmes. However, this approach is increasingly being used for a range of maternal healthcare services as well, with this now the second most represented service in social franchising (Viswanathan et al., 2016). This reflects women’s frequent use of private providers for maternal healthcare; of those seeking care, 16 and 55% use the private sector for antenatal care (ANC) in sub-Saharan Africa and Asia, respectively, and 22 and 56% for delivery care (Campbell et al., 2016). Less is known about the socio-economic profile of social franchise users for maternal health. No published articles were identified on this topic, and although some programmes included in the Compendium offered maternal healthcare in addition to other services, none reported results disaggregated by service type (Viswanathan et al., 2016). Furthermore, there is no information on whether client SES affects the content of care received at social franchised facilities, though it has been noted that in some health system contexts better off patients tend to receive better quality services (Gwatkin et al., 2004).
In light of these knowledge gaps, we assessed the socio-economic profile of clients of three maternal health social franchise: the ProFam network in Uganda, the Merrygold network in Rajasthan, India and the Sky network in Uttar Pradesh, India. These three programmes received funding from MSD for Mothers (www.msdformothers.com), and this study formed part of a larger evaluation of some MSD for Mothers initiative projects (www.met-lshtm.com). Using a common methodology, we situated the social franchise users within national or state representative wealth quintiles and so assessed their relative wealth compared with the general population. We also assessed whether women’s report of content of ANC and delivery care received at social franchise facilities differed across wealth quintiles.
The social franchise programmes
The characteristics of the three programmes are summarized in Table 1. Their goals were similar, focusing on improving access to and quality of maternal care provided through the private sector, and increasing utilization of quality healthcare services. All three worked with existing private facilities using a ‘fractional franchise’ model, meaning that the franchise covered only some of the services that facilities provided. All three franchises covered ANC and family planning, with Merrygold and ProFam also providing delivery care. ProFam also covered broader sexual and reproductive health services. At the time of data collection (2015–16), the ProFam network was the largest encompassing 134 health facilities across 43 of Uganda’s 111 districts, followed by Merrygold with 57 facilities across 19 of Rajasthan’s 33 districts. The 50 SkyHealth facilities were concentrated in three of Uttar Pradesh’s 75 districts (the Sky network also included smaller SkyCare Centres but these did not provide ANC). All facilities in the India programmes were private for-profit (PFP) but in Uganda some facilities enrolled were not-for-profit facilities, mainly faith based. All three programmes worked with community health workers to educate and inform women and generate demand for high quality services. Other common activities included technical training for providers and monitoring and supervision for quality assurance. In addition, SkyHealth facilities were equipped with telemedicine equipment to allow internet-based videoconferencing and diagnostic services during ANC visits. Although none of the programmes had specific targets for the SES groups reached, the Merrygold and Sky networks had a clear goal of targeting the poor and marginalized by providing affordable care [World Health Partners (WHP) proposal to MSD for Mothers; Hindustan Latex Family Planning Promotion Trust (HLFPPT) proposal to MSD for Mothers]. Although the ProFam network did not expressly target a specific population, it aimed to provide ‘affordable care’. The fee policies varied across networks, with SkyHealth providing free ANC services, Merrygold fixing a price for delivery services and ProFam not having standardized prices across facilities.
Table 1.
Description and main characteristics of the social franchising programmes, at the time of the data collectiona
| ProFam | Merrygold | Sky | |
|---|---|---|---|
| NGO | Programme for accessible health, communication and education | HLFPPT | WHP |
| Set up of franchise | Family planning program started in 2007 with addition of maternal services in 2012 | Started in 2014 in Rajasthan, following earlier implementation in Uttar Pradesh | Started in 2013 with maternal health in Uttar Pradesh, following earlier implementation in Bihar for childhood illnesses services |
| Geographical coverage | 42 of Uganda’s 111 districts, covering rural, peri-urban and urban areas | 19 of Rajasthan’s 33 districts, covering rural, peri-urban and urban areas | Facilities located in rural/peri-urban areas in the three districts of Kannauj, Kanpur Dehat and Kanpur Nagar |
| Services covered |
|
|
|
| Number of facilities enrolled at time of data collectiona | More than 140 facilities. Mix of PFP and PNFP facilities | 57 facilities of which:
|
50 SkyHealth clinics (the Sky network also included lower level SkyCare providers which did not provide ANC) |
| Community workers | 539 ‘Mama Ambassadors’:
|
1330 trained Merrytarang workers, acting as safe motherhood and referring agents | Accredited social health activists, acting as safe motherhood and referring agents for both public and SkyHealth facilities |
| Main activities |
|
|
|
| Prices for ANC and delivery | Prices not fixed by the social franchise. Variables charges, with only one PNFP facility free of charge | Variable charges for ANC | ANC provided free (though sometimes there were charges for commodities) |
| Normal delivery: 4000 rupees (∼60 USD) |
Mid 2015 in Uganda, early 2016 in India. STI: sexual transmitted infection.
Methods
In each setting, we undertook a cross-sectional survey of women who had attended a social franchise facility for ANC and/or delivery care and who had delivered at the time of the survey.
Sampling strategy
We aimed to survey a total of 760 women in each of the three study settings. The sample size was estimated to allow detection of a difference of 50% between two equally sized groups (e.g. wealthiest and poorest) for a proportion of 50%, with power of 80%, significance level of 5% and an estimated design effect of two to account for clustering at facility level. In each facility, we contacted more women than we targeted to interview to account for an estimated non-response rate of 20% and low utilization of some facilities.
In Uganda, we randomly selected 15 out of the 140 ProFam facilities. The sample was stratified by whether the facility provided C-sections or not (selecting 4 out of 16 C-section facilities and 11 out of 124 other facilities). Of the total sample of 15 facilities, eight were PFP and seven private not-for-profit (PNFP). Similarly, in Rajasthan, we randomly selected 15 out of 57 Merrygold facilities stratified by level (10 out of 19 urban facilities and 5 out of 38 rural/peri-urban facilities). In Uttar Pradesh, out of the 50 SkyHealth facilities we randomly selected 12.
For each program, women eligible for the survey were identified through available records, together with their contact details. Target numbers of women to recruit from each facility were set in proportion to estimated utilization, as reported by the implementing NGO. In Uganda, all facilities kept records using standard Health Management Information System (HMIS) books and it was possible to randomly select our sample from these records. In India, the data we could access from the facilities were limited: they varied by format, content and completeness. Sometimes they were even not available at all. As a result, in Rajasthan we obtained women’s details from the Merrygold registers maintained by Outreach District Coordinators, who are implementing agency staff based at the clinics. In Uttar Pradesh, we had to rely on a mix of data from facility records (4 facilities), implementing agency district coordinators (7 facilities) and community health workers (1 facility). In both Rajasthan and Uttar Pradesh, we requested the names of all clients who had delivered in the year prior to the survey but in both cases were only provided a sub-set of these, and it was not clear how this sub-set had been selected. For all facilities in Rajasthan and three in Uttar Pradesh, we aimed to interview all women from the lists provided since the numbers were close to our targets for these facilities. In the other Uttar Pradesh facilities, where the lists were larger than our target, we randomly selected from these lists.
Data collection
We contacted women by telephone to arrange appointments and community health workers often assisted the team in identifying their addresses. We requested informed written consent (or oral witnessed consent in the case of illiterate participants) from all women located, and if they agreed, we carried out an interview. Women were assured about the confidentiality of their answers. In Uganda, based on facility utilization and target numbers of women per facility, we interviewed women who had delivered in the last 4 months prior to the survey, giving a time lag of 6–10 months between the first ANC visit and the survey. In India, because of poor record keeping and low patient volumes in some facilities, we extended the recruitment period to 1 year prior to the survey, giving a time lag of 6–18 months from first ANC to survey. To aid women’s recall, in Uganda enumerators asked to see the women’s ANC cards where available, which contain detailed information about their pregnancy (such cards were not available in India). Data were collected from July to November 2015 in Uganda and from March to June 2016 in India. Response rates in Uganda, Rajasthan and Uttar Pradesh were 74.5, 76.2 and 71.7%, respectively, with the main reasons for non-response being that mobile numbers were either missing from the records or were wrong (incomplete number of digits) or nobody answered the call. In Uttar Pradesh, we managed to contact most women from the sampling lists from all but one facility, which had a particularly low response rate (3/56), which reflected a high number of inaccuracies in those records.
Data analysis
Data were double entered and analysis was conducted in Stata 14. The analysis was weighted to reflect variation in sampling probability across facilities and across women within facilities, thereby producing estimates that were representative of all women using the social franchise network. Each woman was given a specific weight relevant to (1) the stratum-specific probability of the facility she visited being sampled and (2) her probability of being selected within that facility. The second probability varied depending on whether the analysis concerned women attending for ANC, delivery or either service.
To assign the sampled women to SES groups, in each setting we derived asset weights and SES quintile cut-offs from an existing household survey that was representative of the whole country (Uganda) or State (India). In Uganda, we used the 2011 Ugandan Demographic Health Survey (DHS). The most recent Indian DHS was quite dated (2005–06) so we used the 2012 Indian Human Development Survey (IHDS) for Rajasthan State for Merrygold, and for Uttar Pradesh State for the Sky network. In each setting, our survey included all the questions on household characteristics and asset ownership in the DHS/IHDS, e.g. ownership of televisions and bicycles, materials used for housing construction and types of water access and sanitation. For Uganda, we used the asset weights provided on the DHS website (www.measuredhs.com), while asset weights for the IHDS were calculated using principal component analysis. These weights were applied to the assets of each woman’s household in our survey and summed to calculate the wealth score for each woman. Using the SES quintile cut-offs for the asset scores from the DHS/IHDS, we then allocated each woman to a national wealth quintile (Uganda) or state wealth quintile (India). The full list of assets used in each setting and their weights is presented in the Supplementary Appendix S1.
Given the construction of wealth quintiles as a relative measure of wealth using national/state populations as references, the meaning of belonging to a specific wealth category will differ according to the average wealth of the population of reference. For example, in 2015 Gross Domestic Product (GDP) per capita ranged from 1300 USD in Rajasthan to 770 USD in Uttar Pradesh and 609 USD in Uganda (Economic and Statistical Organization Government of Punjab, 2016; www.esopb.gov.in) (www.knoema.com), meaning that a household in Quintile 5 in Rajasthan will be substantially wealthier in absolute term than a household in the fifth quintile in Uganda. It should also be noted that in poorer countries even some of those in higher quintiles would still be considered as poor in absolute terms. For example, 34.6% of the Ugandan population lived on less than the standard poverty lines of 1.9 USD per day in 2012 and 69.4% on <3.1 USD per day (2011 Purchasing Power Parity (PPP)) (www.data.worldbank.org), meaning that even the fourth quintile will include people living under accepted poverty thresholds.
We also assessed the coverage and equity of the content of ANC and delivery care received. We included only care received at franchise facilities, though we recognize that women may have received some components of ANC at other public or private providers during the course of their pregnancy. For ANC, we assessed all components of care included in the DHS: weight measurement, blood pressure measurement, urine test, blood test, discussion about previous pregnancy complications, iron supplementation, malaria prophylaxis and deworming tablets (the latter two are only relevant for Uganda, as they were not included in government ANC guidelines in India). For delivery content, we selected the DHS indicators which we felt women could reasonably be expected to recall during a household survey: blood pressure taken upon arrival at the facility, presence of a person for support during labour, type of delivery, baby immediately dried and wrapped, baby weighed at birth. We also included two indicators on disrespect and abuse. Concentration indices were used to summarize the socio-economic distribution for each content of care indicator. The concentration index, ranging from −1.0 to +1.0, captures the extent to which a health variable is distributed among the economically worse off as compared with the better off. The convention is that the index takes a negative value when the health variable is disproportionately concentrated among the poor and a positive value when it is concentrated among the better off (O’Donnell and Van Doorslaer, 2008). We used the methods proposed by Erreygers (2009) to derive the concentration indexes.
Ethical clearance was obtained from the London School of Hygiene and Tropical Medicine (LSHTM) Makerere University and Gene Bandhu (NGO) Ethics Committees.
Results
Characteristics of women sampled
Table 2 describes the characteristics of surveyed women in the three settings. In Uganda, we interviewed 761 women, among which 59.6% came from 11 facilities providing normal deliveries only and 40.3% from four facilities providing C-sections. In Rajasthan, 768 women were interviewed, among which 37% were from five rural/peri-urban facilities and 63% from 10 urban facilities. In Uttar Pradesh, 659 women were interviewed from 12 SkyHealth facilities. In all settings, the majority of the women was concentrated in the 20–29 age group. Nearly all women in Rajasthan and Uttar Pradesh reported being married compared with 89.0% in Uganda. Differences in fees paid across the networks reflect to some degree the variation in their standard charges (Table 1). Women reported paying out-of-pocket for ANC visits for most Merrygold visits (83.3%) and approximately one-half of ProFam visits (49.1%) but less than a fifth of SkyHealth visits (19.4%). Most women reported incurring out-of-pocket payments for delivery in Merrygold and ProFam facilities. Merrygold ANC and delivery fees were the highest across the three networks, with a median cost of 13.5 USD for an ANC visit and 75 USD for a normal delivery.
Table 2.
Basic characteristics of surveyed women
| ProFam | Merrygold | SkyHealtha | |
|---|---|---|---|
| Number of women surveyed | 761 (100%) | 768 (100%) | 659 (100%) |
| Number of ANC users | 636 | 662 | 659 (100%) |
| Number of delivery users | 529 | 314 | NA |
| Number of users for both | 406 | 210 | NA |
| Education | N = 748 (95% CI) | N = 768 (95% CI) | N = 659 (95% CI) |
| Completed primary education | 76.2% (64.3–85.0) | 58.6% (52.0–64.9) | 59.2% (43.8–72.9) |
| Age | N = 750 (95% CI) | N = 768 (95% CI) | N = 659 (95% CI) |
| <20 years | 15.1% (10.0–22.2) | 5.0% (3.1–7.9) | 2.1% (8.2–5.3) |
| 20–29 years | 56.0% (48.4–63.3) | 81.4% (77.6–84.7) | 73.6% (71.0–76.1) |
| 30–39 years | 26.5% (24.0–29.1) | 13.4% (9.1–19.5) | 23.8% (21.1–26.7) |
| >40 years | 2.4% (1.5–3.8) | 0.2% (0–1.0) | 0.5% (0.2–1.3) |
| Mean age (years, 95% CI) | 25.3 (24.8–25.9) | 25.3 (25.0–25.6) | 26.1 (25.8–26.5) |
| Marital status | N = 759 (95% CI) | N = 768 (95% CI) | N = 659 (95% CI) |
| Currently married | 88.9% (81.3–93.6) | 99.7% (98.4–99.9) | 100% |
| Never married | 8.0% (3.4–17.8) | 0.0% | 0.0% |
| Separated/divorced | 2.9% (1.3–6.5) | 0.0% | 0.0% |
| Widowed | 0.2% (0–1.8) | 0.3% (0–1.6) | 0.0% |
| Mean number of household members (95% CI) | 5.8 (5.0–6.8) | 7.4 (7.1–7.7) | 6.9 (6.4–7.3) |
| Median number of ANC visits per woman | |||
| At the franchise facilities | 3 | 1 | 1 |
| In total | 4 | 5 | 4 |
| Percentage of all franchise ANC visits paid for out-of-pocket (%) | 49.1 | 83.3 | 19.4 |
| Median cost of visit of those who paid (in USD) | 0.74 | 13.5 | 1.5 |
| Percentage of normal deliveries paid for out-of-pocket (%) | 71.7 | 91.9 | NA |
| Median cost of delivery of those who paid (in USD) | 8.1 | 75 | NA |
| Percentage of C-sections paid for out-of-pocket (%) | 99.4 | 86.4 | NA |
| Median cost of delivery of those who paid (in USD) | 67.5 | 225 | NA |
The full sample for our survey in Uttar Pradesh included clients from delivery facilities that were not part of the Sky network but acted as possible referral sites for delivery; in this analysis, we present data for SkyHealth clients only and the sample is therefore <760. CI: confidence interval.
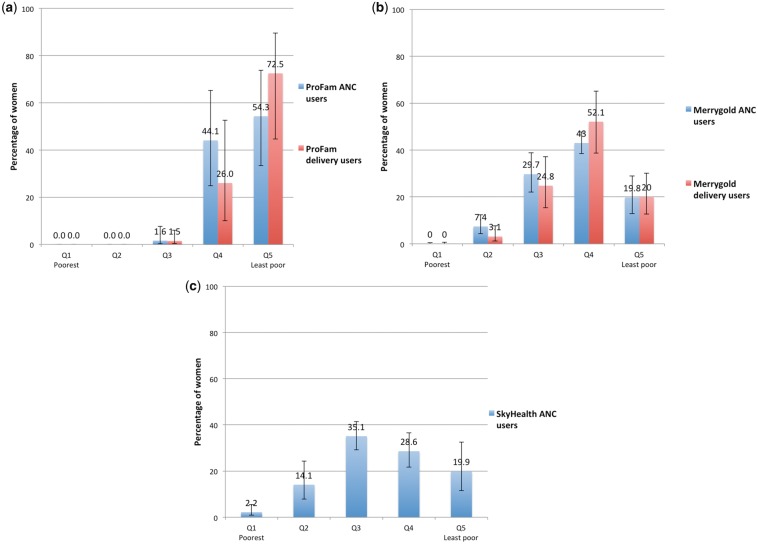
SES of social franchise clients
Figure 1 presents the wealth distribution of users of the three social franchises. Although the confidence intervals are broad, ProFam users were highly concentrated in the highest quintiles. Greater than 98% of ANC and delivery users came from Q4 to 5 combined. In Rajasthan, 72.1% of delivery users and 52.8% of ANC users came from Q4 to 5 combined. Although hardly any women came from the three lowest quintiles in Uganda, more than a quarter of women came from Q3 in Rajasthan. In these two settings, there was some indication that the distribution of delivery users was more skewed towards the top quintiles than for ANC users but the overlap of the confidence intervals did not allow for strong conclusions. The wealth distribution of SkyHealth ANC users was more spread across the quintiles, with the highest representation of women in Q3, though the overall distribution was also skewed towards the top three quintiles. The null hypothesis of an equal distribution across quintiles was rejected for ANC and delivery clients for ProFam (chi-square goodness of fit: P < 0.001) and Merrygold (P < 0.05) and for ANC for Sky Health (P < 0.01).
Figure 1.
Distribution of social franchise users by national/state wealth quintile (percentage, with 95% CI). (a) ProFam, Uganda, (b) Merrygold, Rajasthan and (c) Sky, Uttar Pradesh
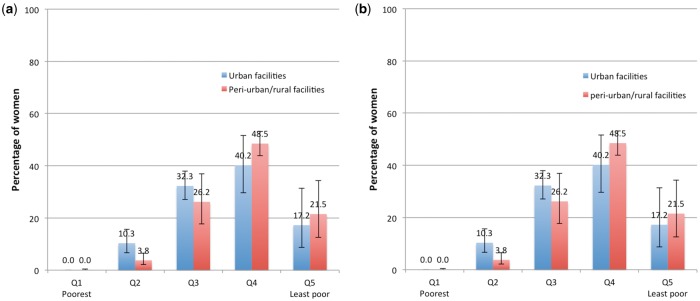
As the ProFam and Merrygold franchises involved a mix of facility types, we also explored whether the SES distribution of clients varied by facility type in these programmes, combining both ANC and delivery users (Figure 2). In Uganda, there was some indication that for-profit facilities served better off women than not-for-profit facilities, and in Rajasthan that Level 2 (sub-divisional) facilities served better off women than Level 1 (district level) but in both cases the width of the confidence intervals means that it is difficult to make strong conclusions.
Figure 2.
Distribution of social franchise users by national/state wealth quintile—by facility type (ANC and delivery users combined) (percentage, with 95% CI). (a) ProFam, Uganda—comparison of PFP and PNFP facilities (ANC and delivery users combined). (b) Merrygold, Rajasthan—comparison of urban and peri-urban/rural facilities (ANC and delivery users combined)
Content of care received by SES
Table 3 presents the percentage of women who reported receiving each component of ANC and delivery care at least once at the social franchise facility during their pregnancy, and the corresponding concentration indices. In the three settings, over 70% of women reported receiving each ANC component of care at least once at the franchise facilities, with the exception of urine test in ProFam facilities; weight, urine test, iron supplementation and discussion of pregnancy complications in Merrygold facilities and urine test, blood test and discussion of pregnancy complications in SkyHealth facilities. In Uganda and Rajasthan, over 70% of women reported receiving the included aspects of delivery care, with the exception of blood pressure on arrival in Uganda. Although over 93% of women reported being treated with respect and dignity in both settings, 9.6 and 2.6% reported being slapped, pinched or hit during delivery in ProFam and Merrygold facilities, respectively.
Table 3.
Content of ANC and delivery care received at social franchise facilities—women reporting having received each component and concentration index by component
| ANC indicators | ProFam, Uganda |
Merrygold, Rajasthan |
SkyHealth, Uttar Pradesh |
|||
|---|---|---|---|---|---|---|
| Women receiving component N = 636 | Conc. index | Women receiving component N = 662 | Conc. index | Women receiving component N = 659 | Conc. index | |
| Weight measured | 97.1% | −0.006 | 63.6% | 0.052 | 95.2% | 0.004 |
| Blood pressure taken | 92.6% | 0.015 | 80.8% | 0.008** | 91.2% | 0.014 |
| Urine test done | 46.9% | 0.098 | 55.2% | −0.006 | 25.3% | 0.109* |
| Blood test done | 93.5% | −0.004 | 75.9% | −0.008 | 60.9% | 0.037 |
| Discussed previous pregnancy complications | 71.9% | −0.026 | 46.1% | 0.024 | 69.1% | −0.012 |
| Iron supplementation | 81.2% | 0.013 | 36.5% | 0.04 | 72.0% | 0.027 |
| Malaria prophylaxis | 80.6% | −0.001 | NA | NA | NA | NA |
| Deworming tablets | 80.1% | −0.001 | NA | NA | NA | NA |
| Delivery indicators | Women receiving component N = 529 | Conc. index | Women receiving component N = 314 | Conc. index | ||
| Blood pressure taken upon arrival | 54.3% | 0.034 | 84.0% | 0.013 | NA | |
| Presence of person for support during labor | 80.8% | −0.038 | 77.5% | −0.080** | ||
| Baby immediately dried and wrapped | 95.7% | −0.002 | 99.4% | 0.002 | ||
| Baby weighed at birth | 95.6% | −0.002 | 97.7% | 0.012* | ||
| Felt they were treated with respect and dignity | 93.1% | 0.007 | 98.1% | −0.001 | ||
| Reported being slapped, pinched or hit during delivery | 9.6% | −0.138 | 2.6% | −0.447* | ||
P < 0.10;
P < 0.05
Results suggest that most content of care indicators did not generally vary by SES. The confidence interval for concentration indices did not straddle zero for only three indicators: blood pressure during ANC in Merrygold facilities and urine test during ANC in SkyHealth were both skewed towards women from higher quintiles, while the presence of a person for support during labour was more prevalent among poorer Merrygold clients. However, the magnitude of all these effects was relatively low.
Discussion
We assessed the SES of women using three maternal health franchises: the ProFam network in Uganda, the Merrygold network in Rajasthan and the Sky network in Uttar Pradesh. All three programmes had received funding from the same funder (MSD for Mothers), raising the question of the generalizability of these findings to other maternal healthcare social franchises. However, based on the programmes described in the Clinical Social Franchising Compendium, there are clearly common key features across most programmes regardless of the services offered: they typically operate on a fractional franchise model, therefore offering some sort of maternal health services as one of many other services; community health workers and marketing campaigns are frequently used to generate demand; and fee-for services is applied, although a small number of programmes include a voucher component. The geographical scope of these programmes is typically a mix of urban, peri-urban and rural areas, and the franchised facilities are usually run by a midwife or a nurse, although bigger clinics can be doctor run. Sale of commodities is also common across programmes.
A strength of our approach was the identification of a sampling frame of social franchise users from the records of participating facilities. By contrast, using community-based survey data to document client SES relies on women being able to report correctly the type of facility they visited and whether it was a franchise member, which may be difficult for respondents. However, reliance on facility records also led to challenges, particularly in India where the lists of women provided by staff of the franchising NGO (facility-based outreach coordinators in Rajasthan, and district coordinators in Uttar Pradesh) were incomplete and sometimes inaccurate. It seems unlikely that these lists would have represented a random sample of all clients. However, based on extensive discussions with the study team and NGO staff, there were no direct indications that any purposive selection of women had taken place. Rather, it was noted that the incomplete list mainly reflected poor record keeping both at the facilities and among the implementers of the social franchise (SF) programmes. A further limitation is that our data on components of ANC and delivery care received at franchise clinics is based on women’s recall, which may be inaccurate for specific services, especially if there is a substantial time lag between the visits and the survey or if women had multiple ANC visits during their pregnancy. However, the time lag between the first ANC visit and the survey in both Uganda and India was shorter than in the DHS, which covers the pregnancies of all children born in the last 5 years. Additionally, data on out-of-pocket payment for ANC and delivery services at the social franchises may be prone to inaccuracies given that other family members often paid for care. Finally, the reference surveys used to allocate women to wealth quintiles, the 2012 IHDS and 2011 Ugandan DHS, were conducted several years before our data collection, though they remained the most recent available source of information at the time of analysis.
Although all the programmes had a stated aim to serve poorer groups, or to provide affordable care, we found that franchise users were concentrated in the higher wealth quintiles of the national/state population distribution in all three programmes. The percentage of women in the top two quintiles was highest for the ProFam network (>98% for both services), followed by Merrygold (62.8% for ANC and 72.1% for delivery) and Sky (48.5% for ANC). The percent of clients in the lowest two quintiles was zero for ProFam, 7.1 and 3.1% for Merrygold ANC and delivery users, respectively, and 16.3% for Sky. Our findings are consistent with the results presented by the programmes themselves in the Clinical Social Franchise Compendium, although there are some differences in the package of services studied (Viswanathan et al., 2016). We found that ProFam maternal health users were even more concentrated in the top two quintiles than the family planning users reported in the Compendium (88% in top two quintiles) but that Merrygold users for maternal health services were poorer than all Merrygold users reported in the Compendium (88% in the top two quintiles though a relatively old 2006 DHS was used as a reference). Although we found little variation by SES in women’s report of content of ANC and delivery care at franchise facilities, the inequalities in utilization of franchised services are particularly concerning in the context of overall inequalities in coverage of maternal healthcare. Despite reports of recent increases in coverage of maternal and child health services among the poorest 40% of the population in LMIC, important inequalities persist (Victora et al., 2017).
The higher proportion of clients in lower quintiles for the Sky network compared with ProFam and Merrygold may partly have reflected the charging of fees for ANC and delivery in all but one facility in Uganda and in all facilities in Rajasthan, while there was no consultation fee for ANC at SkyHealth providers (though nearly 20% of patients paid for some commodities). Perhaps most importantly, it is possible that the more skewed distribution in Uganda compared with Rajasthan and Uttar Pradesh simply reflects the lower average SES of Uganda compared with the Indian states, meaning that fewer women in the bottom one-half of the SES distribution can even contemplate using private facilities in Uganda compared with India. It is important to note that the quintiles are calculated relative to the population in each setting, and therefore the absolute wealth level of a given quintile will vary across settings. To explore this, we compared the ownership of individual assets by women’s households belonging to Quintile 5 across the three sites (see Supplementary Appendix S2). We recognize that the SES significance of a given asset may vary across settings; e.g. the weight for bicycle was 0.066 in Rajasthan but in Uganda the weight was −0.008, meaning that owning a bicycle was associated with a lower wealth score. However, comparisons across sites do indicate some important differences between the populations in absolute terms, in particular highlighting the lower average SES in Uganda. Out of the eight assets that were common across the three sites, ownership in Q5 was over 20% points lower in Uganda than in Rajasthan and Uttar Pradesh for four assets (electricity, refrigerator, bicycle and motorcycle).
The inequalities in service coverage documented in this study are not unique to social franchises, with distributions favouring the better off also documented in the private sector in general and in some cases in the public sector. In sub-Saharan Africa, Campbell et al. found that, among women in need for services, the use of family planning and ANC services favoured women from the top quintiles in both public and private sectors; while in other regions utilization was pro-poor in the public sector and favoured wealthier women in the private sector. In all regions, the use of delivery services was higher in women from the highest quintiles in both public and private sectors (Campbell et al., 2016). In the specific case of Uganda, among women in need for services, the absolute difference in ANC coverage between lowest and highest quintiles was −20% (the negative value indicates higher use by women from highest quintiles) in the private sector, while the distribution was pro-poor in the public sector, with a difference of 12%. In India, the difference between the lowest and highest quintiles for ANC was important in the private sector (−55%) and again the distribution was pro-poor (10%) in the public sector. The level of inequity was even greater for both sectors when looking at delivery care. In Uganda, the difference between Q5 and 1 in private and public sectors reached −25 and −21%, respectively, and in India it was as high as −57% in the private sector and −15% in the public sector.
A key question in interpreting this analysis is whether such private facility orientated interventions should be expected to reach poorer groups. One could argue that it is not essential for social franchises to reach the poorest groups; rather better private sector services might lead wealthier women to shift to these private facilities, leaving more capacity in the public sector to serve poorer women and facilitating improvements in public sector quality. However, evidence remains scarce on this topic. We explored this in Uganda and did not find any increase in average patient volumes at franchise facilities post-entry to the franchise, indicating that such shifting was not occurring, at least within the first couple of years of franchise membership (Haemmerli et al., 2016). One could also argue that in low-income contexts such as Uganda, even women in Quintiles 4 and 5 may be considered poor in absolute terms: e.g. of households in Quintile 5 from the Ugandan DHS, only 58.4% of households had electricity, 48.1% a TV and 19.7% a refrigerator.
It is possible that the very nature of social franchising programmes may restrict their ability to serve the poorest groups. In some settings private facilities might not even be found in the poorest communities, or may be present, but fail to meet the enrolment criteria, particularly for delivery care. Interviews with implementers in Uganda revealed that this was the case in some rural areas where they struggled to find private facilities that met their minimum quality standards and which were not already involved with another social franchise programme. Even when franchised facilities are located in areas which include poorer women, most social franchise organizations acknowledge that they will not attract the very poorest who would be unlikely to use private facilities at all. However, they may also struggle to attract Q2 and 3 women, given competition with government facilities which provide free delivery care or in India give financial incentives for public sector delivery (https://www.nhp.gov.in/janani-suraksha-yojana-jsy-_pg). Finally, social franchising is a complex and multi-faceted intervention (Prata et al., 2005). All three programmes in this analysis included a wide range of objectives: establishing a recognized brand, recruiting providers to the network, generating demand, improving quality of care, developing the business of private facilities and targeting the poor. There may be tensions between these objectives—particularly between targeting the poor and improving quality or developing the business, especially over a relatively short timeframe. This is likely to be especially challenging for relatively complex services such as delivery care, where quality improvement is not straightforward, and fees are relatively high compared, e.g. with family planning.
There are mechanisms sometimes put in place to improve the equity of the distribution of social franchise users, such as insisting on fixed prices, linking patients to available insurance programmes and using community health workers to reach remote communities but implementation of these features can be challenging. In sum, for delivery in particular, it seems unlikely that social franchises will reach a representative number of women in Quintiles 2 and 3 unless some form of subsidy is applied, e.g. through targeted vouchers (Bellows et al., 2011; Brody et al., 2013). Voucher programmes are demand-side incentives where ‘vouchers are distributed for free or highly subsidized reproductive health services and providers are reimbursed for seeing voucher-bearing patients’ (Bellows et al., 2011). Bellows et al. found that among the seven reproductive health voucher programmes they evaluated, all indicated an increased utilization of services, though none of these took place in the context of a social franchise. Moreover, while adding demand-side financing might improve utilization among poorer groups, adding a further subsidy is challenging in a context where there is increasing pressure from funders on social franchise organizations to recover a higher percentage of their costs in the name of financial sustainability (UCSF Global Health Sciences, 2014).
Conclusion
Despite important variations between the three social franchise networks, we found that franchise users were concentrated in the higher SES quintiles in all settings. The majority of clients was in the top two SES quintiles in Uganda and Rajasthan, and almost one-half of the women came from these quintiles in Uttar Pradesh. Differences across the programmes may reflect variation in their user fees, in the average SES of the national/state populations and in the range of services covered. Although most social franchises acknowledge they will not reach the very poorest, the tension between targeting poorer groups and financial sustainability remains a challenge for this type of intervention, and it seems unlikely that middle income and poorer groups will be reached in large numbers in absence of additional targeted subsidies. Whatever strategies are adopted, it is essential that social franchise programmes be clear about who they are targeting in the socio-economic distribution, and report systematically on their equity results.
Supplementary Data
Supplementary data are available at Health Policy and Planning online.
Supplementary Material
Acknowledgements
We would like to thank the social franchising programmes for their cooperation and comments on earlier drafts, as well as the staff and clients of the study health facilities for their participation and insights during data collection.
Funding
The research in this publication was supported by funding from MSD, through its MSD for Mothers program. Funding was used for general financial support, including staff salaries, travel, and overhead. MSD had no role in the design, collection, analysis and interpretation of data, in writing of the manuscript, or in the decision to submit the manuscript for publication. The content of this publication is solely the responsibility of the authors and does not represent the official views of MSD. MSD for Mothers is known as Merck for Mothers in the United States and Canada.
Conflict of interest statement. None declared.
References
- Bellows NM, Bellows BW, Warren C.. 2011. Systematic review: the use of vouchers for reproductive health services in developing countries: systematic review. Tropical Medicine & International Health: TM & IH 16: 84–96. [DOI] [PubMed] [Google Scholar]
- Beyeler N, Briegleb C, Sieverding M.. 2014. Financial sustainability in social franchising: promising approaches and emerging questions. San Francisco: Global Health Group, Global Health Sciences, University of California, San Francisco. [Google Scholar]
- Beyeler N, York De La Cruz A, Montagu D, Bullen C.. 2013. The impact of clinical social franchising on health services in low- and middle-income countries: a systematic review. PLoS One 8: 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bishai DM. 2008. Social franchising to improve quality and access in private health care in developing countries. Harvard Health Policy Review 8: 12. [Google Scholar]
- Brody CM, Bellows N, Campbell M. et al. 2013. The impact of vouchers on the use and quality of health care in developing countries: a systematic review. Global Public Health 8: 363–88. [DOI] [PubMed] [Google Scholar]
- Campbell OMR, Benova L, MacLeod D. et al. 2016. Family planning, antenatal and delivery care: cross-sectional survey evidence on levels of coverage and inequalities by public and private sector in 57 low- and middle-income countries. Tropical Medicine and International Health 21: 486–503. [DOI] [PubMed] [Google Scholar]
- Economic and Statistical Organization Government of Punjab. 2016. State Wise Data www.esopb.gov.in.
- Erreygers G. 2009. Correcting the concentration index. Journal of Health Economics 28: 504–15. [DOI] [PubMed] [Google Scholar]
- Gwatkin DR, Bhuiya A, Victora CG.. 2004. Making health systems more equitable. Lancet 364: 1273–80. [DOI] [PubMed] [Google Scholar]
- Haemmerli M. 2016. How far can a social franchise cover its costs? An economic analysis of the PROFAM maternal health franchise in Uganda, paper presented to African Health Economics and Policy Association, Rabat, 26th of September 2016. [Google Scholar]
- Hennink M, Clements S.. 2005. The impact of franchised family planning clinics in poor urban areas of Pakistan. Studies in Family Planning 36: 33–44. [DOI] [PubMed] [Google Scholar]
- Montagu D, Sudhinaraset M, Lwin T. et al. 2013. Equity and the sun quality health private provider social franchise: comparative analysis of patient survey data and a nationally representative TB prevalence survey. International Journal for Equity in Health 12: 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montagu D. et al. 2005. Kenya: Reaching the Poor through the Private Sector-A Network Model for Expanding Access to Reproductive Health Service In: Gwatkin D. ed., Reaching the Poor with Health, Nutrition, and Population Services: What Works, What Doesn't, and Why, 1st edn. Washington DC: The World Bank, 81–96. [Google Scholar]
- Montagu D, Goodman C, Berman P. et al. 2016. Recent trends in working with the private sector to improve basic healthcare: a review of evidence and interventions. Health Policy and Planning 31: 1117–32. [DOI] [PubMed] [Google Scholar]
- Montagu D, Goodman C.. 2016. Prohibit, constrain, encourage, or purchase: how should we engage with the private health-care sector?. The Lancet 388: 613–21. [DOI] [PubMed] [Google Scholar]
- O’Donnell O, Van Doorslaer E.. 2008. Analyzing Health Equity Using Household Survey Data.
- Patouillard E, Goodman CA, Hanson KG. et al. 2007. Can working with the private for-profit sector improve utilization of quality health services by the poor? A systematic review of the literature. International Journal for Equity in Health 6: 17.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prata N, Montagu D, Jefferys E.. 2005. Private sector, human resources and health franchising in Africa. Bulletin of the World Health Organization 83: 74–9. [PMC free article] [PubMed] [Google Scholar]
- Shah NM, Wang W, Bishai DM.. 2011. Comparing private sector family planning services to government and NGO services in Ethiopia and Pakistan: how do social franchises compare across quality, equity and cost?. Health Policy and Planning 26: i63.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stephenson R, Tsui AO, Sulzbach S. et al. 2004. Franchising reproductive health services. Health Services Research 39: 2053–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The World Bank et al. 2008. Analyzing Health Equity Using Household Survey Data. Washington DC: The World Bank. [Google Scholar]
- UCSF Global Health Sciences. 2014. Financial Sustainability in Social Franchising: Promising Approaches and Emerging Questions.
- Victora CG. et al. 2017. The contribution of poor and rural populations to national trends in reproductive, maternal, newborn, and child health coverage: analyses of cross-sectional surveys from 64 countries. The Lancet Global Health 5: 402–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Viswanathan R, Behl R, Seefeld C.. 2016. Clinical Social Franchising Compendium: An Annual Survey of Programs: findings from 2015. San Francisco: The Global Health Group, Global Health Sciences, University of California, San Francisco. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.