Abstract
The lack of human resources is a key challenge in scaling up of HIV services in Africa’s health care system. Integrating HIV services could potentially increase their effectiveness and optimize the use of limited resources and clinical staff time. We examined the impact of integration of provider initiated HIV counselling and testing (PITC) and family planning (FP counselling and FP provision) services on duration of consultation to assess the impact of PITC and FP integration on staff workload. This study was conducted in 24 health facilities in Kenya under the Integra Initiative, a non-randomized, pre/post intervention trial to evaluate the impact of integrated HIV and sexual and reproductive health services on health and service outcomes. We compared the time spent providing PITC-only services, FP-only services and integrated PITC/FP services. We used log-linear regression to assess the impact of plausible determinants on the duration of clients’ consultation times. Median consultation duration times were highest for PITC-only services (30 min), followed by integrated services (10 min) and FP-only services (8 min). Times for PITC-only and FP-only services were 69.7% higher (95% Confidence Intervals (CIs) 35.8–112.0) and 43.9% lower (95% CIs −55.4 to − 29.6) than times spent on these services when delivered as an integrated service, respectively. The reduction in consultation times with integration suggests a potential reduction in workload. The higher consultation time for PITC-only could be because more pre- and post-counselling is provided at these stand-alone services. In integrated PITC/FP services, the duration of the visit fell below that required by HIV testing guidelines, and service mix between counselling and testing substantially changed. Integration of HIV with FP services may compromise the quality of services delivered and care must be taken to clearly specify and monitor appropriate consultation duration times and procedures during the process of integrating HIV and FP services.
Keywords: Integration, health systems, family planning, human resources, HIV
Key Messages
Integrating HIV services, particularly in resource-limited settings, could potentially increase their effectiveness and optimise the use of limited resources and clinical staff time.
In Kenya, integration is increasingly being rolled out and significant resources have gone, and are going, into provider initiated HIV counselling and testing (PITC) into FP services at different levels of the health systems. However, the evidence of the impact of integration on staff workloads, and specifically on consultation duration times, remains unclear.
Integration may improve consultation times for some but not for all services, but most importantly this may mean a reduction in quality for some services.
Introduction
Global policy recommendations support the integration of HIV and sexual and reproductive health (SRH) (Kennedy et al. 2010; Johnson et al. 2012). Integration in this context commonly refers to ‘the delivery of different sets of HIV and SRH services within the same setting, during the same hours, and, preferably, under the same roof, or as part of a facilitated referral within the same facility or to off-site facilities’ (Liambila et al. 2013). The emerging evidence to support the health benefits of integration has identified increased acceptability from both patients and providers; and some potential technical efficiency (‘providing services or producing outputs at the lowest cost’) and allocative efficiency (‘achieving health outcomes at a low cost’) improvements (Askew and Berer 2003; Sweeney et al. 2012, 2014; Obure et al. 2015). Specifically, as integration is occurring in the context of a shortage of human resources for health; it is argued that integrating HIV and SRH services can improve the use of limited staff time (World Health Organization and UNAIDS 2006; Callaghan et al. 2010; Howard and El-Sadr 2010; Sweeney et al. 2014; Siapka et al. 2014), and reduce workload (Sweeney et al. 2012).
HIV and SRH service integration is therefore increasingly being rolled out in many countries as a mechanism for both increasing demand (through exposure), meeting dual FP and HIV/STI needs and improving efficiency. In Kenya, family planning (FP) and HIV counselling and testing (HCT) services have traditionally been provided separately. The Integra Initiative conduced a household survey among men and women aged 18–49 that was conducted in 2009 (Mak et al. 2013). In the two study Provinces (Central and Eastern), the survey showed that, at the population level, 53% women and 67% men had not been tested for HIV or have not received their results in the past year. Furthermore, the survey found there were substantial unmet needs among men and women for both FP and HIV/STI services and that there were significant missed opportunities to provide integrated services to men and women who already attended services but did not receive services that addressed both their FP and HIV/STI prevention and care needs (Mak et al. 2013).
While the substantial investment in integration has demonstrated improvements in the uptake of PITC services in Kenya (Kimani et al. 2015), there is less known about the impact of these increased demand on human resources. Human resources for health remain scarce in Kenya and elsewhere, but the evidence of the impact of integration on staff workloads remains unclear. Theoretically, integration could reduce the time taken to deliver services, as certain tasks do not need to be repeated. However, integration may also increase providers’ workload, as clients seek and receive more comprehensive services (Baumgartner et al. 2014). Where there is excess capacity, an increase in workload may not be problematic, but where staff are already overworked, this could place a strain on scarce resources (Sweeney et al. 2014). In this article, we present detailed evidence on the impact of integration of provider initiated HCT (PITC) and FP (FP counselling and FP provision) services on consultation duration times in Kenya, in order to explore how integration may impact overall workload and service quality.
Methods
We measured and compared consultation duration times for integrated and non-integrated services for a range of different providers. FP consultations were carried out by FP-trained nurses of different cadres; PITC consultations were usually carried out by general nurses, but in some facilities pharmacists or trained HIV counsellors also did this; integrated PITC/FP consultations were carried out by the FP nurses. Currently, there is no guidance on consultation length for integrated services in Kenya and we did not have an a priori hypothesis about the difference in consultation times between integrated PITC/FP services and PITC services and FP services. We therefore compared consultation duration times with one another and to the World Health Organisation (WHO) norms to provide an HIV test at a sufficient quality in terms of providing an accurate results and offering counselling, which is 15 min (World Health Organization 2005). We also analysed the determinants of consultation times using a multivariate analysis, to understand the extent to which integration influenced consultation duration when considering other determinants of consultation time and staff workload.
Study design and study setting
The study was conducted as part of the Integra Initiative. The study originally sought a controlled, non-randomized intervention design to evaluate the impact of different models of delivering integrated HIV and SRH services on a range of health and service outcomes (Warren et al. 2012). As the study took an implementation science approach and was embedded with Ministry of Health activities, however, this design was rendered unreliable over time, as SRH/HIV integration was adopted nationally in Kenya. The Integra Initiative therefore developed a measure of the extent integration to allow for robust assessment of its impact (see Supplementary Annex and Mayhew et al. 2016 for rationale, details and measures) on a range of outcomes. Specifically, the Integra Initiative sought to add to the limited evidence base on the benefits of integrating HIV and SRH services, examining service outcomes, quality and costs.
The Integra study sites were purposefully chosen from six priority districts based on previous operational research relationships with the Ministries of Health in Kenya. Integra study sites varied by setting, facility type, ownership and clinical model of integration. In Kenya, the Integra sites included 24 public facilities and 6 non-government organisations (NGO) affiliated SRH clinics. This study uses data collected from the 24 public facilities. The public facilities were selected from two provinces (Central and Eastern) and 6 districts (Nyeri, Nyandarua, Thika, Muranga, Kitui and Makueni) and included a provincial general hospital, 5 district hospitals, 5 sub district hospitals and 13 health centres. The intervention included strengthening integrated delivery within FP and post-natal services as well as broad support for integration to the facility (see Warren et al. 2012 and the Supplementary Annex for details). Further details are provided in Supplementary Table S1.
Study procedure
Consultation duration times
Data on consultation duration times were measured through client flow assessments (CFAs) (Warren et al. 2012). The CFAs were designed using the Patient Flow Analysis, which is a method developed by the Centres for Disease Control to monitor patients’ movements through a clinic over 1 day (Lynam et al. 1994; Centers for Disease Control and Prevention 2015). In the Integra evaluation, CFAs were used to measure the duration of consultations and service utilisation patterns among client seeking maternal and child health (MCH) services. CFAs were carried out in all sites over three time points in quarter 3 in 2009, quarter 3 in 2010 and quarter 1 in 2011 covering a period of 5 days (Monday through Friday). A client flow form was provided to all clients accessing MCH services by teams of trained local researchers or service providers. Throughout their visit, each service provider completed the form during the consultation by indicating the session’s start and end times, the service(s) received by the client and any referrals to other providers (Warren et al. 2012; Birdthistle et al. 2014). Up to five consultations could be recorded. Detailed methods on the client flow component are provided elsewhere, with descriptive analysis of client-receipt of integrated services (Birdthistle et al. 2014).
Integration indicator
Services were grouped into PITC-only, FP-only, integrated PITC/FP and all other services. PITC-only services were the provision of HIV counselling and/or testing services but no FP-related service on the day of the survey; FP-only services were the provision of FP-related services (including counselling, method-provision or method-check); Integrated PITC/FP services were defined as a client receiving both an FP-related service AND an HIV counselling and/or testing service during one of their (up to five) consultations on the day they were surveyed.
The unit of analysis for the client-level dataset was individual clients (who could have multiple consultations in one visit). An integration indicator was constructed for each client, and was described as ‘integrated FP/PITC’, when a combination of FP and PITC services were provided in a single consultation (joined) or when a combination of FP and PITC services were provided in different consultations during the same visit (separate). Together these give an indication of ‘facility level’ (as opposed to provider level) integration. Clients were classified as ‘FP-only’ when at least one of the five consultations was FP and none of the other consultations was PITC. Clients were classified as ‘PITC-only’ when at least one of the five consultations was PITC and none of the other consultations were FP. We estimated a consultation duration time that excluded times for non PITC and FP services. If a person had more than one consultation of the same type the consultation duration times were added to one another to come to a composite consultation duration time.
As a sensitivity analysis we also constructed a provider-level dataset (see Supplementary Material). In this case, the unit of analysis was individual consultations, and a consultation was described as ‘integrated FP/PITC’ when FP and PITC services were provided in the same consultation.
Determinants of consultation times and staff workload
We examined a range of determinants that were a priori considered plausible to impact on consultation duration times. These included client characteristics of client’s age, sex and type (‘Adult’ indicates an individual going to the consultation alone and ‘adult with child’ indicates an individual going to the consultation with a child); integration characteristics, such as the consultation–integration indicator (described above) and total number of services provided per facility; facility characteristics such as location (urban and rural) and inpatient/outpatient facilities; other geographical/study design characteristics such as province (Central Province and Eastern Province) and the original allocation of the site into intervention or comparison; facility size characteristics, including human resources, such as number of MCH visits per facility at baseline (to estimate size of the facility), total outpatient visits per year per facility, total staff FTE across all services per facility and proportion of clinical staff out of total staff per facility; and workload characteristics, such as facility workload, time of arrival at facility and waiting time.
For some of these metrics we had a choice of methods. Specifically, facility workload was measured as the ratio of the actual staffing levels to the estimated staffing requirements, using an adaptation of basic methods from the WHO’s Workload Indicators of Staffing Needs (WISN). We estimated the time required to deliver services at the facility level through a mixed methods approach to staff time observation; this is an improvement on the typical WISN methodology, which uses expert opinion on timing of health services and may not reflect real practice (Sweeney et al. 2014). Time observations were combined with detailed service statistics to estimate the total staff FTE required to deliver services in each facility. Our estimates conservatively assume 220 working days per year accounting for national holidays and leave time, and assume 33% of this time to be taken by administrative duties, trainings and so on—leaving 70 752 annual minutes per clinical staff FTE for direct patient care. For some services, including HCT and HIV care and treatment, we also considered the time of technical staff such as lab technicians and lay counsellors (Shipp 1998; Ozcan and Hornby 1999; World Health Organization 2010; Sweeney et al. 2014). A workload ratio greater than 1 (or 100%) indicates some down times for staff members. A ratio of 1 (or 100%) indicates that the estimated time to deliver services is equal to the staff time available for patient visits within a facility. A ratio of < 1 (or 100%) indicates that staff are likely overworked (Sweeney et al. 2014). Supplementary Table S1 provides a description of these variables with calculations made, where applicable.
Sample size
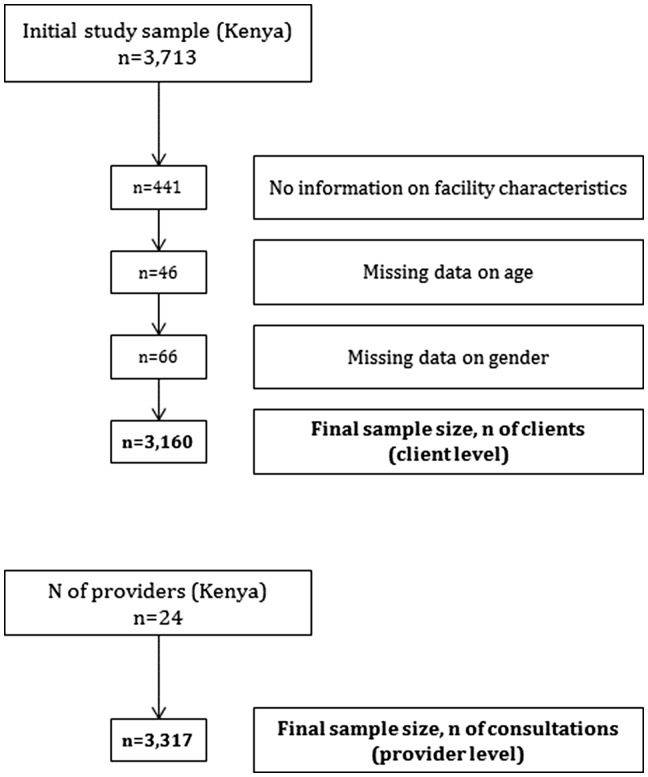
Of the 13 552 individual clients, 3713 clients had FP-only, PITC-only or PITC/FP consultations and therefore retained for the analysis. Of those, 553 were removed due to lack of information on facility characteristics (n = 441), and missing data on age (n = 46) and sex (n = 66). Final sample sizes were 3160 clients for client-level data and 3317 consultations for provider-level data (Figure 1).
Figure 1.
Study sample—flow chart
Data analysis
Descriptive analysis was first conducted for the basic demographic and study characteristics of clients and facilities. When reporting consultation duration times we use medians, interquartiles and range as data were highly skewed. We analysed the differences between consultation duration times for PITC-only, FP-only and integrated services, taking into account other plausible determinants of consultation time, using ordinary least square (OLS) regression analysis with a log transformation for the consultation duration times. We examined differences, or any emerging patterns, in consultation duration times for clients (i.e. client-level data) and individual consultations (provider-level data). We did not have a specific a priori hypothesis about whether and to what extent differences between the two exist. Examining the times for clients, allows us to understand whether this service is more beneficial from a client perspective (in terms of the opportunity cost of time spent receiving a service). Comparing times across consultations is more important from a health provider performance perspective. We run sensitivity analysis on both the client-level and provider-level data to examine the impact of possible measurement bias in consultation duration times by selecting 3 min as the minimum time for any consultation given. All our analyses adjusted for clustering effects at the facility level. For ease of interpretation, regression coefficients were converted into per cent change in consultation duration times using the formula [exp(β) − 1]×100. Proportions were transformed into natural logarithmic form, implying that the coefficients of the independent variables can be interested as elasticities (Gerdtham et al. 1992). All analyses were carried out in Stata 14.1.
Results
Facilities substantially varied in terms of overall number of MCH visits (interquartile range 6329–21 686), total outpatient visits (interquartile range 8545–21 804), size of facility (interquartile range 513.8–4189.4 m2), staff (interquartile range 21.6–48.6 total FTE) and facility workload (interquartile range 13.1–30.8%) (Table 1).
Table 1.
Summary statistics for facility characteristics (n = 24)
| Mean | SD | Median | Q1; Q3 | Range | |
|---|---|---|---|---|---|
| Integration characteristics | |||||
| Total number of services provided per facility | 39.7 | 16.7 | 41.2 | 24.9; 51.3 | 14.2; 79.7 |
| Facility size characteristics | |||||
| Total number of mother and child health visits per facility (at baseline in 2009) | 14 191 | 11 974.8 | 9010 | 6329; 21 686 | 2354; 44 840 |
| Total outpatient visits per year per facility | 19 064 | 14 312.0 | 15 310 | 8545; 21 804 | 3805; 52 642 |
| Size of facility (total square meters of consultation rooms) | 3409.8 | 5233.2 | 894.5 | 513.8; 4189.4 | 181.8; 19 542.8 |
| Total staff FTE across all services per facility | 33.9 | 14.9 | 31.6 | 21.6; 48.6 | 6.2; 55.9 |
| Proportion of clinical staff out of total stuff per facility (%) | 48.8% | 4.3% | 49.5% | 46.6%; 51.6% | 38.6%; 56.8% |
| Workload characteristics | |||||
| Facility workload (at baseline in 2009) (%) | 24.9% | 17.9% | 21.9% | 13.1%; 30.8% | 3.6%; 84.8% |
Table 2 presents summary statistics on clients’ consultation duration times by client and facility characteristics. Mean age of clients was 28 years. Clients’ had a waiting time of 77 min and almost all clients were female (99.6%) (Supplementary Table S2). Median consultation duration times were higher: in the intervention compared to the comparison arm (15 vs 7 min); for PITC-only compared with FP-only consultations (30 vs 8 min) and integrated services PITC/FP (10 min); in the Central Region compared to Eastern Region (15 vs 7 min); and in adults only and adult and child (10 min) compared with unknown coded (8 min) (Table 2). Similar patterns were observed in the provider-level dataset (Supplementary Table S4).
Table 2.
Summary statistics on clients’ consultation duration times (n = 3160)
| Variable | Median | Q1; Q3 | Range |
|---|---|---|---|
| Integration characteristics | |||
| PITC only | 30 | 15; 53 | 1; 291 |
| FP only | 8 | 4; 16 | 1; 268 |
| Integrated PITC & FP a | 10 | 5; 21 | 1; 183 |
| Integrated PITC & FP (Joined) | 9 | 5; 18 | 1; 183 |
| Integrated PITC & FP (Separate) | 32 | 23; 44 | 6; 146 |
| Client characteristics | |||
| Client typeb | |||
| Adult | 10 | 5; 26 | 1; 291 |
| Adult + child | 10 | 5; 21 | 1; 268 |
| Unknown | 8 | 5; 15 | 3; 103 |
| Inpatient/facility characteristics | |||
| Inpatient/outpatient | |||
| Inpatient | 10 | 5; 20 | 1; 291 |
| Outpatient | 13 | 6; 27 | 1; 159 |
| Location | |||
| Rural | 10 | 5; 22 | 1; 268 |
| Urban | 11 | 5; 26 | 1; 291 |
| Study selection characteristics | |||
| Intervention/arm | |||
| Comparison | 7 | 4; 15 | 1; 225 |
| Intervention | 15 | 6; 30 | 1; 291 |
| FP/PNC model | |||
| FP model | 15 | 7; 29 | 1; 256 |
| PNC model | 7 | 4; 15 | 1; 291 |
| Workload characteristics | |||
| Pooled consultation duration times (min)c | 10 | 5; 24 | 1; 291 |
FP, Family planning; PITC, Provider-initiated HIV counselling and testing; PNC, Postnatal Care; SD, Standard deviation
Classified as integrated services when a combination of FP and PITC services were provided in a single consultation (joined) or when a combination of FP and PITC services were used in different consultations (separate). Classified as FP when at least one of the consultations was FP and none of the other consultation were PITC. Classified as PITC when at least one of the consultations was PITC and none of the other consultations were FP
‘Adult’ indicates an individual going to the consultation alone, and ‘adult with child’ indicates an individual going to the consultation with a child
Pooled consultation duration times data of up to five consultations excluding any services not classified as FP, PITC or integrated PITC & FP
Table 3 presents summary statistics by type of service (PITC-only, FP-only and integrated PITC/FP) and facility and patient characteristics. In general, patterns were consistent with median consultation duration times in integrated services being lower when compared with PITC-only but higher when compared with FP-only services irrespective of stratification made by population and facility characteristics. The only exception was when looking at times by client type. Adults with a child had a lower median consultation duration time in integrated services when compared to PITC-only and FP-only (7 vs 20 vs 10 min). Supplementary Table S7 shows the types of services provided in each type of consultation, whether HIV test only, HIV counsel and test and HIV counselling only. PITC only consultations had substantial higher levels of HIV testing (83.2%) and lower levels of counselling (82.4%) than FP/PITC consultations (35.6 and 95.2%, respectively).
Table 3.
Summary statistics on clients’ consultation duration timesa by type of service (n = 3160)
| PITC only (n = 541) |
FP only (n = 1897) |
Integrated PITC and FPb(n = 722) |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Median | Q1; Q3 | Range | Median | Q1; Q3 | Range | Median | Q1; Q3 | Range | |
| Client characteristics | |||||||||
| Client typec | |||||||||
| Adult | 34 | 18; 61 | 2; 291 | 6 | 4; 14 | 1; 219 | 15 | 7; 26 | 1; 168 |
| Adult + child | 20 | 9; 32 | 1; 159 | 10 | 5; 20 | 1; 268 | 7 | 5; 17 | 1; 183 |
| Unknown | 15 | . | 15; 15 | 6 | 4; 9 | 3; 103 | 21 | 10; 32 | 10; 32 |
| Inpatient/facility characteristics | |||||||||
| Inpatient/Outpatient | |||||||||
| Inpatient | 27 | 11; 48 | 1; 291 | 8 | 4; 16 | 1; 268 | 7 | 5; 15 | 1; 183 |
| Outpatient | 31 | 17; 57 | 4; 159 | 8 | 4; 17 | 1; 132 | 18 | 11; 36 | 1; 147 |
| Location | |||||||||
| Rural | 28 | 15; 55 | 1; 169 | 8 | 4; 16 | 1; 268 | 7 | 5; 16 | 1; 183 |
| Urban | 30 | 15; 51 | 2; 291 | 9 | 4; 16 | 1; 256 | 16 | 8.5 – 30 | 2; 137 |
| Study selection characteristics | |||||||||
| Intervention/Arm | |||||||||
| Comparison | 19 | 10; 34 | 1; 225 | 6 | 4; 13 | 1; 162 | 6 | 5; 13 | 1; 183 |
| Intervention | 37 | 22; 60.5 | 3; 291 | 10 | 5; 20 | 1; 268 | 20.5 | 12; 35 | 1; 147 |
| FP/PNC model | |||||||||
| FP model | 27 | 14; 46 | 2; 180 | 11 | 5; 22 | 1; 256 | 18 | 10; 30 | 1; 146 |
| PNC model | 33 | 15; 68 | 1; 291 | 5 | 4; 10 | 1; 268 | 6 | 4; 12 | 1; 183 |
FP, Family planning; PITC, Provider-initiated HIV counselling and testing; PNC, Postnatal Care; SD, Standard deviation.
Pooled consultation duration times data of up to five consultations excluding any services not classified as FP, PITC or integrated PITC & FP
Classified as integrated services when a combination of FP and PITC services were provided in a single consultation or, only in the case of individual-level data, when a combination of FP and PITC services were used in different consultations. Classified as FP when at least one of the consultations was FP and none of the other consultation were PITC. Classified as PITC when at least one of the consultations was PITC and none of the other consultations were FP
‘Adult’ indicates an individual going to the consultation alone, and ‘adult with child’ indicates an individual going to the consultation with a child
Table 4 presents the results of the OLS regression for log transformed consultation duration times. Our model could explain ∼30% of the variation in consultation duration times, reflecting that there are other potential determinants of consultation times that we had no data on. PITC-only services were significantly related to a 69.7% increase (95% confidence intervals (CIs) 35.8–112.0) in consultation duration times, whereas FP-only services were significantly related to a 43.9% decrease (95% CIs: −55.4 to −29.6) in consultation duration times when compared with integrated services. Total number of services provided per facility (decrease of 0.8% per one added service, 95% CIs −1.5 to −0.1), patient’s age (decrease of 0.6% per one year increase in client’s age, 95% CIs −1.1 to −0.03), intervention arm (increase of 42.8% compared with comparison arm, 95% CIs 11.1–83.5), Eastern Region (decrease of 38.1% compared with Central Region, 95% CIs −55.3 to −14.1), time of arrival (decrease of 0.1% per 1 min increase, 95% CIs −0.12 to −0.02) and proportion of clinical staff (decrease of 1.3% per 1% increase in clinical staff, 95% CIs −2.5 to −0.1) were statistically significantly related to consultation duration times. In sensitivity analysis, the impact of integration on consultation duration times was reduced but remained statistically significant. PITC-only services were significantly related to a 58.5% increase (95% CIs 26.7–98.2) in consultation duration times, whereas FP-only services were significantly related to a 40.5% decrease (95% CIs −51.3 to −27.2) in consultation duration times when compared with integrated services. Direction of effect and size of association remained the same for all plausible determinants, except age (Supplementary Table S9). Similar patterns with less pronounced effects were observed in the provider-level dataset (Supplementary Table S10).
Table 4.
Impact of plausible determinants on log transformed minutes of clients’ consultation duration times
| Model 1 (n = 3160) |
Model 2 (n = 2929) |
Model 3 (n = 2491) |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Beta | % changea | 95% CIsa | Beta | % changea | 95% CIsa | Beta | % changea | 95% CIsa | |
| Integration characteristics | |||||||||
| Integrated PITC and FP (reference) | |||||||||
| PITC only | 0.558*** | 74.72 | 39.70; 118.40 | 0.485*** | 62.47 | 30.09; 102.90 | 0.018 | 1.84 | −20.98; 31.24 |
| FP only | −0.566*** | −43.22 | −54.34; −29.36 | −0.509*** | −39.87 | −50.42; −27.08 | −1.106*** | −66.90 | −75.81; −54.70 |
| Total number of services provided per facility | −0.007 | −0.70 | −1.48; 0.01 | −0.009* | −0.91 | −1.58; −0.24 | −0.003 | −0.32 | −1.06; 0.42 |
| Client characteristics | |||||||||
| Age (years) | −0.006* | −0.60 | −1.09; −0.09 | −0.004 | −0.41 | −0.93; 0.10 | −0.007* | −0.68 | −1.23; −0.12 |
| Client typeb(Adult—reference) | |||||||||
| Adult + child | 0.042 | 4.29 | −9.99; 20.77 | 0.029 | 2.97 | −9.52; 17.18 | 0.066 | 6.87 | −7.28; 23.19 |
| Unknown | −0.241 | −21.41 | −51.04; 26.01 | −0.355 | −29.90 | −56.70; 13.49 | −0.350 | −29.56 | −59.05; 21.18 |
| Inpatient/facility characteristics | |||||||||
| Inpatient (reference) | |||||||||
| Outpatient | 0.129 | 13.77 | −17.98; 57.82 | 0.093 | 9.70 | −17.51; 45.88 | 0.112 | 11.81 | −19.58; 55.45 |
| Location (Rural – reference) | |||||||||
| Urban | 0.535* | 70.74 | 1.93; 186.04 | 0.369 | 44.70 | −5.13; 120.70 | 0.385 | 46.93 | −16.17; 157.53 |
| Facility size characteristics | |||||||||
| Total number of mother and child health (MCH) visits per facility (at baseline in 2009) c | 0.000 | 0.00 | −0.01; 0.00 | 0.000 | 0.00 | −0.01; 0.00 | 0.000 | 0.00 | −0.01; 0.00 |
| Total outpatient visits per year per facility d | 0.000 | 0.00 | 0.00; 0.00 | 0.000 | 0.00 | 0.00; 0.00 | 0.000 | 0.00 | 0.00; 0.00 |
| Size of facility (total square meters of consultation rooms) e | 0.000 | 0.00 | 0.00; 0.01 | 0.000 | 0.00 | 0.00; 0.01 | 0.000 | 0.00 | 0.00; 0.01 |
| Total staff FTE across all services per facility | −0.007 | −0.70 | −1.97; 0.51 | −0.007 | −0.72 | −1.81; 0.39 | −0.005 | −0.54 | −1.97; 0.92 |
| Proportion of clinical staff out of total stuff per facility | −3.920** | −98.02 | −99.80; −80.23 | −3.548** | −97.12 | −99.63; −77.62 | −3.828** | −97.83 | −99.80; −76.18 |
| Study selection characteristics | |||||||||
| Intervention/Arm (Comparison – reference) | |||||||||
| Intervention | 0.396** | 48.59 | 18.56; 86.31 | 0.353** | 42.37 | 16.07; 74.62 | 0.315* | 36.99 | 7.15; 75.14 |
| FP/PNC (FP model – reference) | |||||||||
| PNC model | −0.367* | −30.72 | −51.65; −0.82 | −0.283 | −24.63 | −43.74; 0.96 | −0.331 | −28.15 | −51.70; 6.88 |
| Workload characteristics | |||||||||
| Facility Workload (at baseline in 2009) | 1.189 | 228.38 | −4.21; 1026.47 | 0.992* | 169.53 | 3.28; 603.43 | 1.132 | 210.14 | −7.10; 935.44 |
| Time of arrival at facility | −0.001** | −0.10 | −0.12; −0.02 | −0.001*** | −0.08 | −0.12; −0.04 | −0.001* | −0.07 | −0.13; −0.01 |
| Waiting timef,g | 0.000 | 0.00 | −0.09; 0.09 | −0.000 | −0.01 | −0.09; 0.06 | 0.000 | 0.03 | −0.07; 0.13 |
| R2 | 0.309 | 0.311 | 0.307 | ||||||
| AIC | 8208 | 6999 | 6603 | ||||||
| BIC | 8323 | 7113 | 6714 | ||||||
AIC, Akaike Information Criterion; BIC, Bayesian Information Criterion; CIs, Confidence Intervals; FP, Family planning; HR, Human resources; OLS, Ordinary Least Squares; PITC, Provider-initiated HIV counselling and testing; PNC, Postnatal Care
Model 1 using full range of consultation duration times, Model 2 restricted to consultation duration times of over 3 min; Model 3 restricted to separate consultations only
Regression coefficients were converted into per cent change in consultation duration times using the formula [exp(β)−1]×100
‘Adult’ indicates an individual going to the consultation alone, and ‘adult with child’ indicates an individual going to the consultation with a child
Beta = −0.0000317, % change = −0.003%, 95% CIs = −0.0068% to 0.0005% in Model 1. Beta = −0.0000263, % change = −0.003%, 95% CIs = −0.0055% to 0.0002% in Model 2
Beta = −0.0000072, % change = −0.001%, 95% CIs = −0.003% to 0.001% in Model 1. Beta = −0.00000631, % change = −0.001%, 95% CIs = −0.002% to 0.001% in Model 2
Beta = 0.0000373, % change = 0.004%, 95% CIs = −0.001% to 0.009% in Model 1. Beta = 0.0000333, % change = 0.003%, 95% CIs = −0.001% to 0.007% in Model 2
Beta = 0.0000065, % change = 0.001% in Model 1. Beta = −0.0001351, % change = −0.001%, 95% CIs = −0.004% to 0.001% in Model 2
Between arrival and first consultation (and subsequent consultations when there was more than one consultation)
P < 0.05, **P < 0.01, ***P < 0.001
Discussion
The aim of this article was to examine the impact of integration of PITC/FP services on consultation duration times and workload. Using OLS regression with co-variates that were considered to be driving consultation duration times, we found that PITC-only services had higher consultation duration times than for integrated PITC/FP services, and that integrated service consultation duration times were higher than those for FP-only services. The findings around PITC contrast with other studies which have suggested that consultation times of integrated services may be higher when compared with stand-alone services as patients receive a more comprehensive service (Topp et al. 2010; Leon et al. 2013; Baumgartner et al. 2014). In this Journal Supplement, another article examines whether quality of FP care is compromised as a result of integration but finds that it is not (Mutemwa et al. 2017)—despite the finding here that integration of FP and PITC does not substantially increase consultation times compared with FP-only consultations. This suggests that the quality of HIV care may be a point of concern. The median consultation times for PITC/FP integrated services in the provider-level analysis were substantially lower (7 min) (at the client level they were slightly higher, 10 min) than times required for accurate HIV-rest results reading (15 min, followed by counselling) (World Health Organization 2005). However, integrated care resulted in higher levels of counselling, but a lower proportion of HIV testing compared with PITC only.
There are several possible explanations for the observed differences in consultation durations for integrated vs non-integrated PITC consultations. The primary explanation is likely to be the different service mix between counselling and testing. While some of this may be due to the differing needs of receiving integrated services—possibly those receiving FP had more recent HIV tests—given the similarities in the demographical profile of those accessing integrated and non-integrated care, it may also be due to provider behaviour in respect of recommending testing. In addition, the higher consultation time for PITC-only compared with integrated PITC/FP services could be due to the fact that more pre-and post-counselling is provided for a PITC-only service compared with the integrated PITC set up within an FP service (Obure et al. 2015) (for those clients that receive counselling). Given the association between the proportion of clinical staff at the facility and consultation times, the observed differences in integrated and non-integrated PITC consultation times may also be due to the provision of different services by clinician and non-clinician staff (Hontelez et al. 2012), although we were unable to determine that from our data, as we did not have individual level data on the cadre of provider.
Decreases in consultation times may be in part a consequence of a lack of training and support for staff during integration(Johnson et al. 2012). Delivering integrated services is likely to require additional and more specialized training than single service provision (Sweeney et al. 2014). It should be noted that in this study, clients are receiving both separate and integrated services at the same facility. Johnson et al. (2012) reported that health workers may receive training to deliver either HIV or FP services but may not provide either of these services at every consultation. Health workers may also have limited time to provide comprehensive care in all consultations, especially if a daily quota needs to be achieved (Mutemwa et al. 2013; Uebel et al. 2013). Having said this, it should be noted that integrated care resulted in higher levels of counselling, with fewer tests being provided without counselling. A lack of infrastructure and resources to support integration in some facilities has also been reported, which may impede the full delivery of services(Mutemwa et al. 2013; Phiri et al. 2016). Other explanations for the lower times for integrated services, include the willingness of health workers to engage in integrated HIV services and provision of care (Uebel et al. 2013), in this case carrying out fewer HIV tests. There is also some evidence that the integration of services may increase job satisfaction through improvements in work-based skills and client satisfaction, but at the same time increase workload and stress and reduce the quality of time with clients (Mutemwa et al. 2013). These provider-level tensions are further explored in another Integra paper in this Supplement (Mayhew et al. 2017).
In applying our findings to policy, these should be considered alongside the research that suggests integration may bring a range of benefits (Johnson et al. 2012). In relation to cost-effectiveness, Shade et al. (2013) have reported that integration of FP and HIV services can be inexpensive, cost-efficient and cost-effective. Specifically, they found that integration was associated with a marginal cost of $65 for each additional use of more effective FP and $1368 for each pregnancy averted. Reductions in consultation duration times through integration may allow clinics to receive more patients; and without an increase in staff this could lead to reduced client waiting and treatment times overall (Farrell 2007; Mutemwa et al. 2013). Obure et al. (2015) also reported that better use of human and capital resources can reduce costs of integrated SRH and HIV services.
Some limitations to our analysis should be acknowledged. There may be a risk of information bias in terms of mis-reporting consultation duration times (Sweeney et al. 2014). Measurement error cannot be ruled out, as some of the consultation duration times were as low as 1 min and we examined how effect estimates might change using a minimum of 3 min. It might be possible that some of the clients had a pre-test counselling but then referred to do a test elsewhere. In addition, we did not have data on other potentially important determinants of consultation time, such as information on first or a follow-up consultation or contraceptive method used or the type of provider. Client flow data were collected over 1 week, and not on the same week for all sites, which may not be representative of a typical month or annual client flow (Birdthistle et al. 2016). Our analysis was undertaken from the provider perspective and we are unable to comment on how duration consultation times may affect quality of care or how patients may value different consultation times (Sweeney et al. 2014). Service integration is not unique to HIV and FP services, and future studies should examine how duration times are affected when different services are integrated. In addition, provider time and capacity should be among the many factors that need to be taken into account when selecting an integrated model (Baumgartner et al. 2014).
Conclusion
Integrating HIV services with SRH services like FP has important financial, management and policy implications, particularly in resource-limited settings. Integration may reduce consultation times for some services, but this will depend on the service mix provided. Our findings suggest that the time spent on PITC in an integrated consultation is much lower than in a PITC-only consultation. These findings should also be seen in the context of the additional financial costs and time needed to implement a strategy to integrate services. Future studies should examine the cost-effectiveness of reductions in consultation times for such services, considering the consequences of integration on cost, service mix, quality and service outcomes simultaneously. Going forward, it is important for those implementing integration to have sound systems in place to monitor workload, levels of testing and the quality of care being provided.
Supplementary Data
Supplementary data are available at HEAPOL online.
Funding
The study was funded by the Bill & Melinda Gates Foundation through the International Planned Parenthood Federation (Grant 48733). The research team is completely independent from the funders. The funders had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript.
Conflict of interest statement. None declared.
Supplementary Material
Acknowledgements
The Integra Initiative team members are: At the London School of Hygiene & Tropical Medicine: Susannah Mayhew (PI), Anna Vassall (co-PI), Isolde Birdthistle, Kathryn Church, Manuela Colombini, Martine Collumbien, Natalie Friend-DuPreez, Natasha Howard, Joelle Mak, Richard Mutemwa, Dayo Obure, Sedona Sweeney, Charlotte Watts. At the Population Council: Charlotte Warren (PI), Timothy Abuya, Ian Askew, Joshua Kikuvi, James Kimani, Jackline Kivunaga, Brian Mdawida, Charity Ndwiga, Erick Oweya. At the International Planned Parenthood Federation: Jonathan Hopkins (PI), Lawrence Oteba, Lucy Stackpool-Moore, Ale Trossero; at FLAS: Zelda Nhlabatsi, Dudu Simelane; at FHOK: Esther Muketo; at FPAM: Mathias Chatuluka. We would also like to thank the fieldwork teams; the research participants who gave their time to be interviewed; the managers of the clinics who facilitated data collection; and the Ministries of Health in Kenya and Swaziland who supported the research and are key partners in the Integra Initiative. Finally, we would like to thank other colleagues who gave feedback on aspects of research design and/or analysis and Jon Hopkins for comments on the final draft of this article.
References
- Askew I, Berer M.. 2003. The contribution of sexual and reproductive health services to the fight against HIV/AIDS: a review. Reproductive Health Matters 11: 51–73. [DOI] [PubMed] [Google Scholar]
- Baumgartner JN. et al. 2014. Integrating family planning services into HIV care and treatment clinics in Tanzania: evaluation of a facilitated referral model. Health Policy and Planning 29: 570–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birdthistle IJ. et al. 2014. Integration of HIV and maternal healthcare in a high HIV-prevalence setting: analysis of client flow data over time in Swaziland. BMJ Open 4: e003715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birdthistle IJ. et al. 2016. Integration of HIV and reproductive health services in public sector facilities: analysis of client flow data over time in Kenya. [Under review]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Callaghan M, Ford N, Schneider H.. 2010. A systematic review of task- shifting for HIV treatment and care in Africa. Human Resources for Health 8: 8.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Patient Flow Analysis for Windows 2015. http://www.cdc.gov/reproductivehealth/ProductsPubs/PFA_support/, accessed 28 February 2016.
- Farrell BL. 2007. Family Planning-Integrated HIV Services: A Framework for Integrating Family Planning and Antiretroviral Therapy Services. New York: EngenderHealth/The ACQUIRE Project. [Google Scholar]
- Gerdtham UG. et al. 1992. An econometric analysis of health care expenditure: a cross-section study of the OECD countries. Journal of Health Economics 11: 63–84. [DOI] [PubMed] [Google Scholar]
- Hontelez JA. et al. 2012. Human resources needs for universal access to antiretroviral therapy in South Africa: a time and motion study. Human Resources for Health 10: 39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howard AA, El-Sadr WM.. 2010. Integration of tuberculosis and HIV services in sub-Saharan Africa: lessons learned. Clinical Infectious Diseases 50: S238–44. [DOI] [PubMed] [Google Scholar]
- Johnson K, Varallyay I, Ametepi P. 2012. Integration of HIV and Family Planning Health Services in Sub-Saharan Africa: A Review of the Literature, Current Recommendations, and Evidence from the Service Provision Assessment Health Facility Surveys. Calverton, MD: ICF International. [Google Scholar]
- Kennedy CE. et al. 2010. Linking sexual and reproductive health and HIV interventions: a systematic review. Journal of the International AIDS Society 13: 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimani J. et al. 2015. Use of HIV counseling and testing and family planning services among postpartum women in Kenya: a multicentre, non-randomised trial. BMC Women's Health 15: 104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leon N, Lewin S, Mathews C.. 2013. Implementing a provider-initiated testing and counselling (PITC) intervention in Cape Town, South Africa: a process evaluation using the normalisation process model. Implementation Science 8: 97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liambila W. et al. 2013. Acceptability and effectiveness of linking HIV-positive family planning clients to treatment and care services among health care providers in Kenya. Journal of AIDS and Clinical Research 4: 232. [Google Scholar]
- Lynam PF, Smith T, Dwyer J.. 1994. Client flow analysis: a practical management technique for outpatient clinic settings. International Journal for Quality in Health Care 6: 179–86. [DOI] [PubMed] [Google Scholar]
- Mak J. et al. 2013. Need, demand and missed opportunities for integrated reproductive health-HIV care in Kenya and Swaziland: evidence from household surveys. AIDS 27: S55–63. [DOI] [PubMed] [Google Scholar]
- Mayhew SH. et al. 2016. Innovation in evaluating the impact of integrated service-delivery: the Integra Indexes of HIV and reproductive health integration. PLoS One 11: e0146694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayhew SH. et al. 2017. Numbers, systems, people: how interactions influence integration. Insights from case studies of HIV and reproductive health services delivery in Kenya. Health Policy and Planning 32: iv67–iv81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mutemwa R. et al. 2013. Experiences of health care providers with integrated HIV and reproductive health services in Kenya: a qualitative study. BMC Health Services Research 13: 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mutemwa R. et al. 2017. Does service integration improve technical quality of care in low-resource settings? An evaluation of a model integrating HIV care into family planning services in Kenya. Health Policy and Planning 32: iv91–iv101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Obure CD. et al. 2015. The costs of delivering integrated HIV and sexual reproductive health services in limited resource settings. PLoS One 10: e0124476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ozcan S, Hornby P.. 1999. Determining hospital workforce requirements: a case study. Human Resources for Health Development Journal 3: 210–20. [Google Scholar]
- Phiri S. et al. 2016. Integrating reproductive health services into HIV care: strategies for successful implementation in a low-resource HIV clinic in Lilongwe, Malawi. J Fam Plann Reprod Health Care 42: 17–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shade SB. et al. 2013. Cost, cost-efficiency and cost-effectiveness of integrated family planning and HIV services. AIDS 27: S87–92. [DOI] [PubMed] [Google Scholar]
- Shipp PJ. Workload Indicators of Staffing Need (WISN): A Manual for Implementation 1998. http://www.who.int/hrh/documents/en/workload_indicators.pdf., accessed 15 April 2016.
- Siapka M. et al. 2014. Is there scope for cost savings and efficiency gains in HIV services? A systematic review of the evidence from low- and middle-income countries. Bulletin of the World Health Organization 92: 499–511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sweeney S. et al. 2012. Costs and efficiency of integrating HIV/AIDS services with other health services: a systematic review of evidence and experience. Sexually Transmitted Infections 88: 85–99. [DOI] [PubMed] [Google Scholar]
- Sweeney S. et al. 2014. The impact of HIV/SRH service integration on workload: analysis from the Integra Initiative in two African settings. Human Resources for Health 12: 42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Topp SM. et al. 2010. Strengthening health systems at facility-level: feasibility of integrating antiretroviral therapy into primary health care services in Lusaka, Zambia. PLoS One 5: e11522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uebel K. et al. 2013. Integrating HIV care into nurse-led primary health care services in South Africa: a synthesis of three linked qualitative studies. BMC Health Services Research 13: 171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warren CE. et al. 2012. Study protocol for the Integra Initiative to assess the benefits and costs of integrating sexual and reproductive health and HIV services in Kenya and Swaziland. BMC Public Health 12: 973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization and UNAIDS 2006. Progress on global access to HIV antiretroviral therapy. A report on 3 by 5 and beyond. Geneva: World Health Organization. [Google Scholar]
- World Health Organization. Determine HIV Rapid Test. 2005. http://www.who.int/diagnostics_laboratory/documents/guidance/determine.pdf, accessed 1 May 2016
- World Health Organization. Workload Indicators of Staffing Need: User’s Manual 2010. http://www.who.int/hrh/resources/wisn_user_manual/en/, accessed 15 April 2016.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.