Abstract
Objective
Rates of sexually transmitted infections (STIs) among adolescents are on the rise. The majority of adolescents who contract STIs do so through risky sexual behavior. Previous literature has identified multiple correlates of risky sexual behaviors among adolescents, including physical and sexual victimization, mental health concerns, and substance use. Few studies, however, have examined these relationships together in a comprehensive model. The primary purpose of this study was to examine whether relationship violence was related to risky sexual behavior, and whether mental health symptoms and substance use mediated this relationship.
Method
A cross-sectional design was used, and adolescent females (N=179), recruited from social service agencies, were 18.9 years old on average and were 37.2% White, 19.3% Black, 37.9% Multiracial and 5.6% other.
Results
Regression results revealed that females who were physically assaulted and sexually victimized by their intimate partners did engage in more sex without condoms. Mediational analyses indicated that PTSD symptoms significantly influenced the relationship between 1) physical assault and risky sexual behavior and 2) sexual victimization and risky sexual behavior.
Conclusion
Contrary to expectations, PTSD may act to reduce risk perhaps by reducing interest in sex. It is important to address victimization, PTSD and sexual risk in young women. More work is needed to understand these complex relationships using longitudinal designs.
Keywords: intimate violence, post-traumatic stress disorder, depression, substance use, risky sexual behaviors
There has been an increase in rates of sexually transmitted infections (STIs) among adolescents in the United States (Centers for Disease Control and Prevention [CDCP], 2012). Although young adults reflect one quarter of the sexually engaged population, virtually half of newly reported STI cases are found in young adults (CDCP, 2012). Among female high school students, 12.6% have had sexual intercourse in their life-time with four or more people and 15.1% did not use condoms or any form of birth control during their last sexual intercourse (CDCP, 2013). The majority of adolescents who contract HIV and STIs do so through risky sexual behavior (i.e., inconsistent condom use, multiple sexual partners, and poor sexual communication practices) (Alleyne-Green et al., 2012). Due to this, several studies have sought to examine the underlying pathways that lead to risky sexual behavior among adolescents. One pathway that has recently received attention is the role relationship violence plays in risky sexual behaviors among adolescents (Alleyne-Green et al., 2012; Allsworth et al., 2009). To date, this association remains poorly understood (Rizzo et al., 2012; Smith et al., 2006). ). From a stand point of risk, females who come from disadvantaged backgrounds may be more susceptible to physical and sexual abuse (Freeman & Temple, 2010), which may directly or indirectly lead to mental health problems, substance use, and risky sexual behaviors (Goodkind et al., 2006; Green et al., 2005; Silverman et al., 2001).
Adolescent girls involved in social settings (e.g., mental health agencies, juvenile justice settings, or residential social service agencies) represent a very vulnerable, high risk and underserved population (Brady & Caraway, 2002; Zelechosiki et al., 2013). A high number of adolescent females involved in social services have experienced physical and sexual trauma by an intimate partner (Briggs et al., 2012; Jaycox et al., 2004). Collin-Vézina and colleagues (2011) found among a sample of adolescents in a residential setting, females were more likely to have experienced physical and sexual abuse by an intimate partner (46%) compared to boys (18%). Additionally, a significant association has been found between traumatic experiences and risky sexual behavior among females involved in juvenile justice system (Biswas et al., 2011). Although research has examined relationship violence and risky sexual behavior among female adolescents involved in social service settings, less is known about the underlying mechanisms of this relationship. Examination of factors related to risky sexual behavior among female adolescents from disadvantaged backgrounds, who are at risk for mental health problems, substance use and violence, is critical for identifying and implementing intervention programs and addressing treatment needs.
Literature Review
Physical Assault and Sexual Victimization by an Intimate Partner
Prior literature has suggested that adolescent females involved in physically abusive relationships have a higher likelihood of engaging in unhealthy sexual behaviors (Silverman et al., 2001; Wingood et al., 2001). Physical assault by an intimate partner can be defined as any physical violence involving a steady partner including pushing, shoving, slapping, or kicking (Alleyne-Green et al., 2012). Studies have associated physical assault from an intimate partner with inconsistent condom use, non-monogamous sexual partners, and an increased risk of incident STIs (Allsworth et al., 2009; Wingood et al., 2001). Additionally, negotiating condom use has been significantly associated with a history of STIs among women who have been abused by their partners (Perrino et al., 2006).
A number of studies have also examined the relationship between sexual victimization and risky sexual behaviors (Gookind et al., 2006; Green et al., 2005). Sexual victimization by an intimate partner can be defined as sexual coercion involving a steady partner that can include insisting on having sex without a condom or using force (i.e., hitting, holding down, or using a weapon) to make a partner have sex (Gidycz et al., 2008; Straus et al., 1996). Among a sample of young women, it was found that those who were sexually abused by an intimate partner were more likely to engage in risky sexual behaviors and have multiple sexual partners in the last 6 months (Gookind et al., 2006). Additionally, there is evidence that forced sexual experiences with an intimate partner are associated with lower condom usage and higher frequency of sexually transmitted diseases (Molitor et al., 2000; Upchurch & Kusunoki, 2004). Individuals who experience sexual victimization by an intimate partner may often suffer mental and emotional disorders (Miller et al., 1995) or engage in substance use (Silverman et al., 2001) which might lead to risky sexual behavior (Brener et al., 1999).
Mental Health Concerns and Intimate Violence
Relationship violence, including physical assault and sexual victimization, may increase sexually risky behavior through its relationship with mental health such as post-traumatic stress disorder (PTSD) and depression (Cavanaugh et al., 2010; Smith et al., 2006). Research has indicated that relationship violence can lead to the development of psychopathology that may increase self-destructive behavior (e.g., multiple sexual partners) (Littleton et al., 2007). Women who have met criteria for PTSD specifically have been found to be more likely to engage in risky sexual behavior such as inconsistent condom use, early sexual intercourse, and having intercourse before knowing a partner’s sexual history (Lang et al., 2003). Although research has provided evidence that PTSD is related to relationship violence and risky sexual behavior, few studies have investigated whether PTSD mediates the relationship between relationship violence and risky sexual behaviors (Green et al., 2005; Smith et al., 2006).
Similarly to PTSD, depressive symptoms can also be viewed as another pathway between relationship violence and risky sexual behavior. There is evidence that depressive symptoms are associated with both physical assault and sexual victimization by an intimate partner among female adolescents (Seth et al., 2011). Victims of relationship violence may experience low self-esteem and locus of control (Littelton et al., 2007). Depressive symptoms have also been strongly related to engaging in risky sexual behavior (Seth et al., 2011). Findings indicate that high levels of depressive symptoms among adolescents are associated with inconsistent condom use, multiple sexual partners, incidence of STIs, poor sexual communication practices, and sex at first meeting (Seth et al., 2011). Although correlates of depressive symptoms have been linked to relationship violence and risky sexual behavior, less is known about whether depressive symptoms mediate the relationship between the two (Green et al., 2005; Seth et al., 2011).
Substance Use and Intimate Violence
Another way that interpersonal violence may increase sexually risky behavior is through alcohol use. Researchers have demonstrated that adolescents with a history of relationship violence are more likely to report higher rates of alcohol use (Goodkind et al., 2006; Shorey et al., 2011; Temple & Freeman, 2011). Survivors of sexual and physical abuse by an intimate partner may use alcohol as a coping mechanism from the psychological distress they experienced, which can potentially put them at even greater risk (Littleton et al., 2007). Studies have also identified a link between adolescent alcohol use, unprotected sex, and multiple sex partners (Guo et al., 2002). Because victims of relationship violence may be more prone to alcohol use, they may have a higher likelihood of engaging in alcohol use before sexual intercourse (Shorey et al., 2011; Temple & Freeman, 2011). Alcohol use has also been shown to impair ones cognitive ability to perform safer sexual practices (Temple & Freeman, 2011).
In addition to alcohol use, marijuana use can be seen as another pathway between relationship violence and risky sexual behavior. There is evidence that women who have suffered physical and sexual abuse by an intimate partner are more likely to engage in marijuana use (Temple & Freeman, 2011). Previous literature has found that adolescent victims dating violence were almost 3 times more likely to smoke marijuana (Temple & Freeman, 2011). Researchers have also shown that adolescents who smoke marijuana are more likely to engage in risky sexual behavior (Bryan et al., 2012). Bryan and colleagues (2012) explored the relationship between marijuana use and risky sexual behavior among a sample of female adolescents on probation and found that females were less likely to use condoms and more inclined to have sexual intercourse with strangers if marijuana was being used.
Current Study
The existing literature has identified multiple correlates of risky sexual behaviors among adolescents including relationship violence, mental health concerns, and substance use, but few studies have examined these associations together in a comprehensive model (Green et al., 2005; Rizzo et al., 2012). Furthermore, limited literature has investigated these factors among female adolescents involved in social service settings (i.e., community outpatient mental health agencies, juvenile justice settings, or residential social service agencies).
The specific aims of this study were to: 1) Test whether physical assault and sexual victimization by an intimate partner predict risky sexual behavior among females involved in social service settings. It was hypothesized that physical assault and sexual victimization by an intimate partner would be significantly related to risky sexual behavior. 2) Determine whether PTSD and depressive symptoms, which are often psychological reactions to abuse, and substance use, such as alcohol and marijuana use, mediate the association between relationship violence (i.e., physical assault and sexual victimization) and risky sexual behaviors among at-risk females. It was hypothesized that intimate partner violence (physical and sexual) would be significantly associated to mental health concerns (i.e., PTSD and depressive symptoms), and to substance use (i.e., alcohol and marijuana use), which in turn would be significantly related to risky sexual behaviors.
Methodology
Participants
The sample consisted of 179 sexually active adolescent females, who were not pregnant and who planned on engaging in coital sex within the next 6 months at the time of recruitment. Racial composition of the sample was 37.2% White, 19.3% Black, 37.9% Multiracial, and 5.6% other; ethnic makeup included 42.5% Hispanic girls; and the average age of girls was 18.7 years (SD= 1.88). Participants were recruited from four social service settings including juvenile justice, community outpatient mental health, alternative schools, and residential social services from the Northeast.
Measures
Physical assault and sexual victimization
Physical assault and sexual victimization were measured using the Conflict Tactics Scale (CTS2; Straus et al., 1996; Straus & Douglas, 2004). The CTS2 measures tactics used during relationship conflicts: Negotiation, physical assault and psychological aggression. In addition, it includes two supplemental scales: Injury from assault and sexual coercion. Respondents rate ten items regarding their own behavior during the last 3 months (e.g., “I insulted or swore or shouted or yelled at my partner”) and the same 10 items regarding partner behaviors (e.g., “My partner insulted or swore or shouted or yelled at me”) on the following scale: Once (coded as 1), Twice (2), 3 times (3), 4–6 times (5), 7–12 times (10), more than 12 times (coded as 15). In addition, the following are coded: The tactic was not used in the last 3 months, but occurred before that (7); and the tactic was never used (8). Items coded as 7 were recoded as 0 because only proximal events (last 3 months) were of interest. Items coded as 8 were also recoded as 0 for past 3 months. For purposes of this study, items reflecting severe physical assault on respondent and severe sexual coercion (i.e., sexual victimization) of respondent were utilized. Physical assault and sexual victimization were positively skewed, therefore these variables were transformed using a log transformation.
Post-traumatic stress disorder symptoms
PTSD symptoms were measured using the PTSD Checklist-6 (PCL-6; Lang & Stein, 2005; Lang, Wilkins, Roy-Byrne et al., 2012; Weathers, Litz, Herman, Huska & Keane, 1993). The PCL-6 is a brief screener that assesses whether a respondent has had any stressful experiences affecting them in the last month. All 6 items were rated on a 5-point Likert scale ranging from not at all (1) to extremely (5) and a single score is produced (α = .79; Lang et al., 2012). A score ≥ 14 indicates a positive screen (Lang & Stein, 2005).
Depressive symptoms
Depressive symptoms were assessed with the Center for Epidemiological Studies-Depression Scale (CES-D; Melchoir et al., 1993). The CES-D is designed to detect the presence and severity of depressive symptoms in the past week. All 10 items were rated on 4-point Likert scale ranging from rarely or none of the time (0) to most or all of the time (3), producing a single summary score (α = .88; Zhang et al., 2012). A cut off score of 10 indicates significant Depressive symptoms (Bradley et al., 2010).
Substance use
Alcohol and marijuana use was assessed using a demographics questionnaire. In addition to obtaining demographic information, this questionnaire gathers information on drug and alcohol history. Participants were asked the number of days in the last 12 months that they have used alcohol, and this inquiry is repeated for marijuana. Trained Research Assistants (RAs) helped participants to recall and estimate use patterns so that a final “days of use” could be provided. Although “days of use” over 12 months may not be entirely accurate, this metric can be an important indicator of risk for alcohol (NIAAA, 2011) and was extended for marijuana use. Number of days of alcohol use (and number of days of marijuana use) was used in the analyses. The responses were positively skewed, therefore the alcohol use variable was transformed using a log transformation and the marijuana use variable was transformed using a square root transformation.
Risky sexual behavior
Risky sexual behavior was measured using the Timeline Follow-back (TLFB; Carey et al., 2001; Sobell et al., 1992). The TLFB provides summary scores for total number of days of sexual intercourse without condoms and total number of days of sexual intercourse without birth control over the past 90 days. Preliminary analyses revealed that the total number of days of sexual intercourse without birth control was relatively low; therefore, the primary focus is on total number of days girls had sexual intercourse without a condom. The responses were positively skewed, therefore these variables were transformed using a square root transformation.
Procedures
The current study is a secondary data analysis of a randomized clinical trial (R01 HD065942; PI-Stein) testing the efficacy of behavioral intervention versus psycho-education in reducing STIs and pregnancy among female adolescents recruited from social service settings. Data for this study were obtained at baseline before intervention was provided. Female adolescents involved in social service settings were invited to participate in the study. Trained research assistants (RAs) approached females at recruitment sites to introduce the study. RAs explained the purpose of the study to interested females, the voluntary nature of participation, and confidentiality. All procedures were explained and written informed consent was utilized. Following the consent process, the baseline assessment was conducted using a computer program facilitated by an RA who provided clarification and administered the program. The program included all of the above described measures, and took approximately 90 minutes. Participants received $25 for the assessment.
Analytic Approach
Descriptive statistics and bivariate correlations were calculated for all predictor and outcome variables. Exploratory analyses were conducted to determine whether participants differed on demographic, predictor, mediator, or outcome variables across the various types of recruitment settings. A series of analyses of variance (ANOVAs) and chi-square analyses revealed that the only significant difference found across the various types of recruitment settings was age, F(3,139) = 4.04, p < .05. Therefore, age was set as a covariate for the following analyses and the data were collapsed across settings.
Multiple regression analyses were conducted in order to examine whether relationship violence (i.e., physical assault and sexual victimization) predicted risky sexual behavior (i.e., number of days had sexual intercourse without condoms), after controlling for age. Multiple mediation analyses (Hayes, 2013) were conducted in order to determine if the mental health (i.e., PTSD and depressive symptoms) and substance use variables (i.e., alcohol and marijuana) mediate the relationship between physical assault and number of days had sexual intercourse without condoms, after controlling for age. Multiple mediation analyses were also conducted in order to determine if the mental health concerns and substance use mediate the relationship between sexual victimization and number of days had sexual intercourse without condoms, after controlling for age.
Mediators can be seen as intervening variables that help completely or partially explain the relationship between a variable and an outcome (Shrout & Bolger, 2002). Multiple mediation analyses can reduce the likelihood of parameter bias and increase power (Preacher & Hayes, 2008). Additionally, mediation analyses can be used to test paths from predictor to mediator variables (i.e., the path denoted by a) and from mediator to outcome variables (i.e., the path denoted by b) (Preacher & Hayes, 2008). The direct effect of the predictor variable on the outcome variable is also calculated (i.e., the path denoted by c′), as is the total effect (c), and R2 for the model (Preacher & Hayes, 2008). Two multiple mediator statistical models were calculated, one with physical assault as the independent variable (IV) and one with sexual victimization as the IV. The total indirect effect (Σaibi) for each model was calculated, along with confidence intervals (CIs) using bootstrap methods. This was followed by tests of indirect effects (aibi) for each mediator in the context of the multiple mediator model, again using bootstrap CIs. Indirect effects with CIs not including zero indicate significant mediation effects (Zhao et al., 2010).
Hayes model number 6 was tested (Hayes, 2013), which included four mediators (PTSD, and depressive symptoms, and alcohol, and marijuana use), the IVs (physical assault or sexual victimization), and the dependent variable (DV, number of days girls had intercourse without condoms), while covarying for age. Data analyses were performed using the PROCESS procedure for SPSS 22.0 (2013) Release 2.13 (http://www.processmacro.org/index.html). Finally effect sizes are presented, as recommended by Preacher and Kelley (2011), in terms of the ratio of the total indirect effect to total effect (PM = Σaibi /[Σaibi + c′]) for the overall model, and in terms of the ratio of the indirect effect for specific mediators to the total effect for the model (aibi/[Σaibi + c′]), with .01, .09 and .25 representing small, medium and large effect sizes, respectively (Cohen, 1988). Although these effect size metrics can be limited under certain methodological conditions, they are presented for descriptive purposes as there are currently few other options, and they can be cautiously interpreted in context (Preacher & Kelley, 2011). Analyses conducted by Fritz and MacKinnon (2007) suggest that mediation models will have power of .80 with sample sizes of about 160 assuming modest indirect path effect sizes (about midway between small and medium) and assuming a medium effect size for the direct effect. These results hold across a variety of test approaches, including the joint significant test and the bias-corrected bootstrap procedure.
Results
Descriptives
Descriptive statistics for the predictor variables and outcome variables are shown in Table 1. Using untransformed data, the average physical assault score was 0.81 (SD = 2.69; Mdn = 0) and the average score of sexual victimization was 0.62 (SD = 2.16; Mdn = 0). There were 29 (16%) female adolescents who reported being physically assaulted by a steady sexual partner and 31 (17%) female adolescents who reported being sexually victimized by a steady sexual partner. Using untransformed data, the average number of days the participants reported drinking alcohol in the last 12 months was 24.04 days (SD = 45.39; Mdn = 4), indicating a moderate level of risk (NIAAA, 2011). The untransformed average number of days the participants reported smoking marijuana in the last 12 months was 76.58 days (SD = 118.35; Mdn = 10), indicating some risk for a substance use disorder (Levy et al., 2014). The average CES-D score was 12.67 (SD = 6.01), indicating moderate levels of depressive symptoms for the sample, such that more than half (69%) screened positive for depressive symptoms. Average PCL-6 score was 17.45 (SD = 6.58), again indicating moderate levels of PTSD symptoms (124 out of 179 screened positive for PTSD symptoms). There were 61 (34%) female adolescents who reported having sex without condoms. For the entire sample, the untransformed average number of days of no condom use was 13.32 (SD = 33.12, Mdn = 2).
Table 1.
Means, standard deviations, and correlations of predictor and outcome variables
| Variable | Mean | SD | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
|---|---|---|---|---|---|---|---|---|---|
| 1. Physical Assault | 0.11 | 0.27 | - | ||||||
| 2. Sexual Vic. | 0.10 | 0.24 | .46** | - | |||||
| 3. Dep. Symptoms | 12.67 | 6.01 | .20** | .18* | - | ||||
| 4. PTSD Symptoms | 17.45 | 6.58 | .16* | .15* | .48*** | - | |||
| 5. Alcohol Use | 0.81 | 0.72 | .08 | −.06 | .07 | .11 | - | ||
| 6. Marijuana Use | 5.85 | 6.53 | .14 | .09 | .11 | .16* | .49*** | - | |
| 7. Days No Condom Use | 2.32 | 2.82 | .35*** | .31*** | .08 | −.06 | .00 | .16* | - |
Note:
p<.05,
p<.01,
p<.001.
Means, standard deviations (SDs), and correlations were conducted with transformed variables. Vic. = Victimization, Dep. = Depressive, PTSD = Post Traumatic Stress Disorder. Depressive Symptoms derived from the CES-D and PTSD Symptoms derived from the PCL-6.
Correlations
Bivariate correlations for the predictor and outcome variables are shown in Table 1. Physical assault was positively correlated with sexual victimization, severity of PTSD and depressive symptoms, and the number of days girls had intercourse without a condom. Sexual victimization was positively associated with severity of PTSD and depressive symptoms and number of days girls had intercourse without a condom. Greater severity of depressive symptoms was related to greater severity of PTSD symptoms. Greater severity of PTSD symptoms was also associated with higher frequency of smoking marijuana. Higher frequency of drinking alcohol was correlated with higher frequency of smoking marijuana. Lastly, higher frequency of smoking marijuana was positively related to number of days girls had intercourse without a condom. Although significant relationships were found among variables, generally, the constructs do not evidence collinearity.
Main Analyses
A multiple regression was performed to evaluate whether physical assault and sexual victimization predicted number of days girls had intercourse without a condom, after controlling for age. The results of the regression indicated that the model explained 18.2% of the variance, R2 = .182, F(3,160) = 11.66, p < .01. It was found that both physical assault (β = .33, t(160) = 3.99, p < .001) and sexual victimization (β = .16, t(160) = 1.98, p < .05) predicted sexual intercourse without a condom.
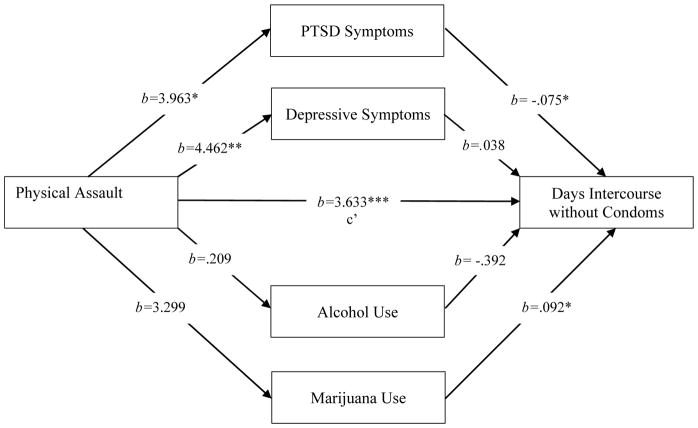
A multiple mediation analysis was conducted to determine whether mental health concerns and substance use mediated the relationship between physical assault by an intimate partner and number of days girls had intercourse without a condom (see Figure 1). The total indirect effect (Σaibi) was not significant, b = 0.094, [95% bias-corrected bootstrap confidence interval (BCa CI) = −0.429, .908; effect size (ES) = 0.025 (small ES)], indicating no mediation in the overall model. For the overall model, R2adj = 0.178, F(6, 163) = 5.874, p < 0.001, and for the total effect (c), b = 3.727, p < 0.001. Indirect effects were then calculated to determine the importance of individual mediators (aibi) within the context of the multiple mediator model. There was a significant indirect effect of physical assault on number of days of intercourse without a condom through PTSD symptoms, b = −0.295, [95% BCa CI = −.876, −.029; ES = 0.079 (small – medium ES)], indicating that PTSD symptoms significantly mediated the relationship between physical assault and number of days of intercourse without a condom. However, there was no significant indirect effect of physical assault on number of days of intercourse without a condom through other mediators and so ES not shown for those. In particular, for depressive symptoms, b = 0.169 [95% BCa = −0.090, .573], for alcohol use, b = −0.082 [95% BCa = −0.478, 0.027], and for marijuana use, b = 0.303 [95% BCa = −0.008, 1.073], indicating that depressive symptoms, alcohol use, and marijuana use did not mediate the relationship between physical assault and number of days of intercourse without a condom.
Figure 1. Direct effect of individual mediators and direct effect of physical assault.
Note: *p <.05, **p <.01, ***p <.001.The direct effect, c′, represents the relationship between physical aggression and days of intercourse without condoms after accounting for the effects of the mediators. Unstandardized paths, b, shown.
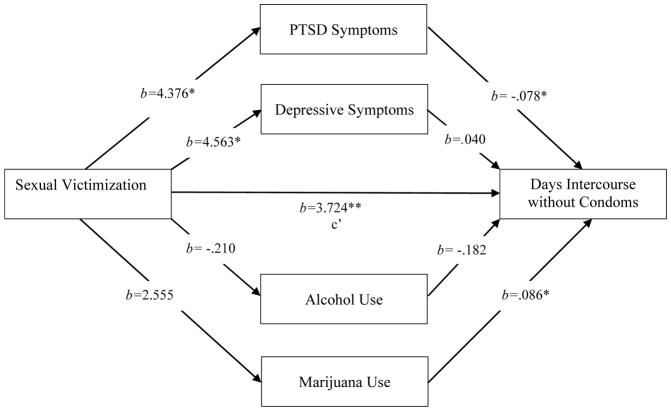
Another multiple mediation analysis was conducted to determine whether mental health concerns (i.e., PTSD and depressive symptoms) and substance use (i.e., alcohol and marijuana) mediated the relationship between sexual victimization and risky sexual behavior (i.e., sexual intercourse without a condom) (see Figure 2). The total indirect effect (Σaibi) was not significant, b = 0.097, [95% BCa CI = −0.467, .856; ES = 0.025 (small ES)], indicating no mediation in the overall model. For the overall model, R2adj = 0.148, F(6, 157) = 6.417, p < 0.001, and for the total effect (c), b = 3.821, p = 0.001. Indirect effects were then calculated to determine the importance of individual mediators (aibi) within the context of the multiple mediator model. There was a significant indirect effect of sexual victimization on number of days of intercourse without a condom through PTSD symptoms, b = −0.343, [95% BCa CI = −1.165, −.008; ES = 0.090 (medium ES)], indicating that PTSD symptoms significantly mediated the relationship between sexual victimization and number of days of intercourse without a condom. However, there was no significant indirect effect of sexual victimization on number of days of intercourse without a condom through other mediators and so ES not shown for those. In particular, for depressive symptoms, b = 0.183 [95% BCa = −0.101, .754], for alcohol use, b = 0.038 [95% BCa = −0.061, 0.313], and for marijuana use, b = 0.219 [95% BCa = −0.075, 1.048], indicating that depressive symptoms, alcohol use, and marijuana use did not mediate the relationship between sexual victimization and number of days of intercourse without a condom.
Figure 2. Direct effect of individual mediators and direct effect of sexual victimization.
Note: *p <.05, **p <.001.The direct effect, c′, represents the relationship between sexual victimization and days of intercourse without condoms after accounting for the effects of the mediators. Unstandardized paths, b, shown.
Discussion
The current study examined whether physical assault and sexual victimization predicted risky sexual behavior and whether mental health concerns and substance use mediated the relationship between relationship violence (i.e., physical assault and sexual victimization) and risky sexual behaviors (number of days girls had intercourse without condoms) among at-risk females. It was found that female adolescents who reported being physically assaulted by their intimate partner had a significantly higher risk of engaging in sex without a condom. The results of the current study confirm findings of previous literature reporting that women with a history of physical abuse from their intimate partner have a higher chance of engaging in unhealthy sexual behaviors (Silverman et al., 2001; Wingood et al., 2001). Additionally, the findings suggested that female adolescents who indicated being sexually victimized by their intimate partner had a significantly higher risk of engaging in sex without a condom. The results of the current study corroborate findings of prior research reporting that women who have experienced forced sexual activities with an intimate partner have a higher likelihood of engaging in risky sexual behaviors (Molitor et al., 2000; Upchurch & Kusunoki, 2004).
Two multiple mediator models were analyzed to predict days of intercourse without condoms, taking into account several mediators (PTSD and depressive symptoms, and days used alcohol and marijuana) and age as a covariate: First with intimate partner physical abuse as the predictor, then with sexual victimization by intimate partner as the predictor. Mediational analyses indicated that PTSD symptoms significantly influenced the relationship between physical assault and risky sexual behavior in addition to sexual victimization and risky sexual behavior. Contrary to expectations, PTSD was associated with a decrease in the number of days girls had intercourse without condoms. Prior research has looked at only portions of the model presented in the current study. For example, Cavanaugh and colleagues (2010) found that low-income women who had experienced PTSD related to intimate partner violence had increased chances of engaging in sexually risky behavior. Similarly, juvenile justice involved girls who had experienced life-time trauma, but not necessarily PTSD, were at greater risk to engage in risky sexual behaviors (Smith et al., 2006). The models tested here were comprehensive in inclusion of multiple mediators, and tested total mediating effects as well as effects of single mediators. Although it was unexpected for PTSD symptoms to reduce the number of days girls had intercourse without condoms, the results were consistent with findings that indicate that PTSD can reduce sexual desire and functioning which could lead to fewer sexual interactions (Yehuda et al., 2015). More specifically, symptoms of PTSD may impede various sexual behaviors (e.g., arousal, activity, satisfaction) and individuals who exhibit these symptoms may purposely avoid sexual activity in order to reduce experiences of physical arousal that could potentially trigger flashbacks or intrusive memories (Letourneau et al., 1996; Yehuda et al., 2015). Earlier childhood trauma can be considered an important factor that can impact victimization, sex risk, and mental health (Clum et al., 2012; Lacelle et al., 2012; Shin et al., 2010). However, the current study focused on relations among more proximal phenomena, as compared to more distal phenomena.
In this study, the presence of depressive symptoms and substance use (i.e., marijuana and alcohol use) did not mediate the relationship between relationship violence (i.e., physical assault and sexual victimization) and number of days girls had intercourse without condoms. The lack of significant mediation effects could be due to the fact that the measures used in the current study contained different lengths of time (i.e., relationship violence covered past 3 months, PTSD symptoms covered past month, depressive symptoms covered past week, substance use covered past 12 months, and intercourse without condoms covered past 3 months). Also, it cannot be confirmed whether PTSD symptoms resulted from physical assault, and some of the constructs (i.e., PTSD and depressive symptoms) were comprised of screeners, not diagnostic assessments. Further examination of additional relevant mediators could be beneficial for future research. Another potential limitation of the current study was the cross-sectional nature of the study, which precludes determination of the temporal and causal nature of relationships. Additionally, the general nature of self-report data particularly regarding sensitive experiences including violence, mental health symptoms, or substance use can be considered a limitation. However, the participants were assured that their reports were private and confidential. Literature suggests that youth respond generally accurately even on sensitive topics when they believe reports are confidential (Brener et al., 2003).
The literature reviewed here was based on samples drawn from a variety of settings such as community mental health centers, colleges, prisons, and included mostly adult samples with less racial and ethnic diversity than the current sample (Goodkind et al., 2006; Shorey et al., 2011; Wingwood et al., 2001). The current study focused on a high need sample from social service settings, comprised of participants who were young (44.6% were adolescents), Hispanic (42.5%), and non-White (62.8%). These differences in samples could in part account for unexpected results and can be considered in future recruitment strategies and model building. It may be found that mediators accounting for the relationship between relationship violence and risky sex differ by sample type.
In conclusion, intimate partner violence (both physical assault and sexual victimization) was associated with risky sex as hypothesized. Unexpected but informative results indicated that physical assault and sexual victimization by an intimate partner reduced sex risk, through PTSD symptoms. The complex multiple mediator models need refinement in future work to determine if results can be replicated, especially in longitudinal designs, and to identify mediators more completely. The current study is consistent with the idea that PTSD symptoms reduce interest in sex and thereby reduce opportunity for sex, however more work is needed in this area. This study has many strengths such as a diverse sample with respect to age, ethnicity, race and recruitment setting, which support the generalizability of the results. Methodological strengths include specific hypotheses, use of bootstrap CIs, multiple mediator modeling, examination of specific indirect effects for single mediators within complex models, and attention to effect size (Preacher & Hayes, 2008; Preacher & Kelly, 2011; Shrout & Bolger, 2002; Zhao et al., 2010). Additionally, the hypothesized mediational sequences were supported by current literature and provide the basis for more complex longitudinal studies that examine these relationships in more detail. Girls who have experienced relationship violence are at risk for unprotected sex. Although PTSD symptoms may decrease this risk according to current findings, it is important to reduce both PTSD symptoms and sex risk for individuals involved in violent relationships.
The current findings have significant implications for prevention and intervention efforts. The need to implement for prevention programs tailored for adolescent female relationship violence is vital. Prevention programs that increase awareness regarding healthy relationships and warning signs of relationship violence may be useful (Ball et al., 2009). Further understanding the psychological outcomes that can occur from relationship violence may better inform effective interventions as well. Medical and mental health care providers may play an important role in recognizing individuals who have experienced relationship violence (i.e., screening mechanisms) and providing support (i.e., appropriate referrals). The current findings suggest that female adolescents who experience dating violence are at greater risk for sexual health concerns, therefore expanding education on risky sex among adolescents may be beneficial. Treatment for girls who have experienced relationship violence should address methods to reduce risky sexual behaviors. When PTSD is associated with this violence, it is incumbent on health professionals to mitigate PTSD symptoms and also reduce increased risk for unprotected sex, especially as trauma symptoms abate.
Acknowledgments
This research was supported in part by a grant from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) (R01 HD065942) awarded to L.A.R. Stein, as principle investigator and a diversity supplement (R01 HD065942-03S1) provided training/mentee support for Danielle C. Hill.
References
- Alleyne-Green B, Coleman-Cowger VH, Henry DB. Dating violence perpetration and/or victimization and associated sexual risk behaviors among a sample of inner-city African American and Hispanic adolescent females. Journal of Interpersonal Violence. 2012;27(8):1457–1473. doi: 10.1177/0886260511425788. [DOI] [PubMed] [Google Scholar]
- Allsworth JE, Anand M, Reddding CA, Peipert JF. Physical and sexual violence and incident sexually transmitted infections. Journal of Women’s Health. 2009;18(4):529–534. doi: 10.1089/jwh.2007.0757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ball B, Kerig PK, Rosenbluth B. Like a Family but Better Because You Can Actually Trust Each Other”“ The Expect Respect Dating Violence Prevention Program for At-Risk Youth. Health Promotion Practice. 2009;10(1 suppl):45S–58S. doi: 10.1177/1524839908322115. [DOI] [PubMed] [Google Scholar]
- Bradley KL, Bagnell AL, Brannen CL. Factorial validity of the center of epidemiological studies depression 10 in adolescents. Issues of Mental Health in Nursing. 2010;31:408–412. doi: 10.3109/01612840903484105. [DOI] [PubMed] [Google Scholar]
- Brener ND, McMahon PM, Warren CW, Douglas KA. Forced sexual intercourse and associated health-risk behaviors among female college students in the United States. Journal of Consulting and Clinical Psychology. 1999;67(2):252–259. doi: 10.1037//0022-006x.67.2.252. [DOI] [PubMed] [Google Scholar]
- Bryan AD, Schmiege SJ, Magnan RE. Marijuana use and risky sexual behavior among high-risk adolescents: trajectories, risk factors, and event level relationships. Developmental Psychology. 2012;48(5):1429–42. doi: 10.1037/a0027547. [DOI] [PubMed] [Google Scholar]
- Carey MP, Carey KB, Maisto SA, Gordan CM, Weinhardt LS. Assessing sexual risk behaviors with the timeline followback (TLFB) approach: Continued development and psychometric evaluation with psychiatric outpatients. Int STD AIDS. 2001;12(6):365–375. doi: 10.1258/0956462011923309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cavanaugh CE, Hansen NB, Sullivan TP. HIV sexual risk behavior among low-income women experiencing intimate partner violence: The role of posttraumatic stress disorder. AIDS and Behavior. 2010;14:318–327. doi: 10.1007/s10461-009-9623-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Sexually Transmitted Disease Surveillance 2012. Atlanta: U.S. Department of Health and Human Services; 2013. [Google Scholar]
- Centers for Disease Control and Prevention. Youth Risk Behavior Surveillance — United States, 2011. MMWR. 2012;61(SS-4) [00-162] [Google Scholar]
- Clum GA, Chung SE, Ellen JM, Perez LV, Murphy DA, Harper GW, Hamvas L. Victimization and Sexual Risk Behavior in Young, HIV Positive Women: Exploration of Mediators. AIDS and Behavior. 2012;16(4):999–1010. doi: 10.1007/s10461-011-9931-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2. New York, NY: Academic Press; 1988. [Google Scholar]
- Dutton M, Green BL, Kaltman SI, Roesch DM, Zeffiro TA, Krause ED. Intimate partner violence, PTSD, and adverse health outcomes. Journal of Interpersonal Violence. 2006;21(7):955–968. doi: 10.1177/0886260506289178. [DOI] [PubMed] [Google Scholar]
- Freeman D, Temple JR. Social factors associated with history of sexual assault among ethnically diverse adolescents. Journal of Family Violence. 2010;25(3):349–356. doi: 10.1007/s10896-009-9296-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fritz MS, MacKinnon DP. Required sample size to detect the mediated effect. Psychological Science. 2007;18:233–239. doi: 10.1111/j.1467-9280.2007.01882.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gidycz CA, Orchowski LM, King CR, Rich CL. Sexual Victimization and Health-Risk Behaviors A Prospective Analysis of College Women. Journal of interpersonal violence. 2008;23(6):744–763. doi: 10.1177/0886260507313944. [DOI] [PubMed] [Google Scholar]
- Goodkind S, Ng I, Sarri RC. The impact of sexual abuse in the lives of young women involved in the juvenile justice system. Violence Against Women. 2006;12(5):456–77. doi: 10.1177/1077801206288142. [DOI] [PubMed] [Google Scholar]
- Green BL, Krupnick JL, Stockton P, Goodman L, Corcoran C, Petty R. Effects of adolescent trauma exposure on risky behavior in college women. Psychiatry: Interpersonal and Biological Processes. 2005;68(4):363–378. doi: 10.1521/psyc.2005.68.4.363. [DOI] [PubMed] [Google Scholar]
- Guo J, Chung IJ, Hill KG. Developmental relationships between adolescent substance use and risky sexual behavior in young adulthood. Journal of Adolescent Health. 2002;31:354–362. doi: 10.1016/s1054-139x(02)00402-0. [DOI] [PubMed] [Google Scholar]
- Hayes AF. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. New York, NY: The Guilford Press; 2013. [Google Scholar]
- IBM Corp. IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp; 2013. [Google Scholar]
- Lacelle C, Hébert M, Lavoie F, Vitaro F, Tremblay RE. Child sexual abuse and women’s sexual health: The contribution of CSA severity and exposure to multiple forms of childhood victimization. Journal of child sexual abuse. 2012;21(5):571–592. doi: 10.1080/10538712.2012.688932. [DOI] [PubMed] [Google Scholar]
- Lang AJ, Rodgers CS, Laffaye C, Statz LE, Dresselhaus TR, Stein MB. Sexual trauma, posttraumatic stress disorder, and health behavior. Behavioral Medicine. 2003;28(4):150–158. doi: 10.1080/08964280309596053. [DOI] [PubMed] [Google Scholar]
- Lang AJ, Wilkins K, Roy-Byrne PP. Abbreviated PTSD checklist (PCL) as a guide to clinical response. General Hospital Psychiatry. 2012;34(4):332–8. doi: 10.1016/j.genhosppsych.2012.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lang AJ, Stein MB. An abbreviated PTSD checklist for use as a screening instrument in primary care. Behaviour Research and Therapy. 2005;43:585–594. doi: 10.1016/j.brat.2004.04.005. [DOI] [PubMed] [Google Scholar]
- Letourneau EJ, Resnick HS, Kilpatrick DG, Saunders BE, Best CL. Comorbidity of sexual problems and posttraumatic stress disorder in female crime victims. Behavior Therapy. 1996;27(3):321–336. [Google Scholar]
- Levy S, Weiss R, Sheritt L, Ziemnik R, Spalding A, Van Hook S, Shrier LA. An Electronic Screen for Triaging Adolescent Substance Use by Risk Levels. JAMA Pediatrics. 2014;168(9):822–828. doi: 10.1001/jamapediatrics.2014.774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Livingston JA, Testa M, Van Zile-Tansen C. The reciprocal relationship between sexual victimization and sexual assertiveness. Violence Against Women. 2007;13(3):298–313. doi: 10.1177/1077801206297339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Littleton H, Breitkopf CR, Berenson A. Sexual and physical abuse history and adult sexual risk behaviors: Relationships among women and potential mediators. Child Abuse & Neglect. 2007;31(7):757–768. doi: 10.1016/j.chiabu.2006.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Krull JL, Lockwood CM. Equivalence of the mediation, confounding, and suppression effect. Prevention Science. 2000;1:173–181. doi: 10.1023/a:1026595011371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melchoir LA, Huba GJ, Brown VB, Reback CJ. A short depression index for women. Educational and Psychological Measurement. 1993;53(4):1117–1125. [Google Scholar]
- Miller BC, Monson BH, Norton MC. The effects of forced sexual intercourse on White female adolescents. Child Abuse and Neglect. 1995;19:1289–1301. doi: 10.1016/0145-2134(95)00081-i. [DOI] [PubMed] [Google Scholar]
- Molitor F, Ruiz JD, Klausner JD, McFarland W. History of forced sex in association with drug use and sexual HIV risk behaviors, infection with STD’s and diagnostic medical care. Journal of Interpersonal Violence. 2000;15:262–278. [Google Scholar]
- Morokoff PJ, Quina K, Harlow LL, Whitmire L, Grimley DM, Gibson PR, Burkholder GJ. Sexual Assertiveness Scale (SAS) for women: Development and validation. Journal of Personality and Social Psychology. 1997;73(4):790–804. doi: 10.1037//0022-3514.73.4.790. [DOI] [PubMed] [Google Scholar]
- Perrino T, Fernandez M, Bowen G, Arheart K. Low-income African American women’s attempts to convince their main partner to use condoms. Cultural Diversity and Ethnic Minority Psychology. 2006;12(1):70–83. doi: 10.1037/1099-9809.12.1.70. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Kelley K. Effect size measures for mediation models: quantitative strategies for communicating indirect effects. Psychological Methods. 2011;16(2):93–115. doi: 10.1037/a0022658. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and re-sampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods. 2008;40:879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- Rizzo CJ, Hunter HL, Lang DL, Oliveira C, Donenberg G, DiClemente RJ, Brown LK. Dating violence victimization and unprotected sex acts among adolescents in mental health treatment. Journal of Child and Family Studies. 2012;21(5):825–832. [Google Scholar]
- Sales JM, Spitalnick JS, Crittenden CP, DiClemente RJ. Depression and sexual risk-taking in adolescents. In: Columbus F, editor. Sexual Risk Behaviors. Hauppauge, NY: Nova Science Publishers Inc; 2009. [Google Scholar]
- Seth P, Patel SN, Sales JM, DiClemente RJ, Wingood GM, Rose ES. The impact of depressive symptomology on risky sexual behavior and sexual communication among African American female adolescents. Psychology, Health & Medicine. 2011;16(3):346–356. doi: 10.1080/13548506.2011.554562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shin SH, Hong HG, Hazen AL. Childhood sexual abuse and adolescent substance use: A latent class analysis. Drug and alcohol dependence. 2010;109(1):226–235. doi: 10.1016/j.drugalcdep.2010.01.013. [DOI] [PubMed] [Google Scholar]
- Shrout PE, Bolger N. Mediation in experimental and non-experimental studies: New procedures and recommendations. Psychological Methods. 2002;(7):422–445. [PubMed] [Google Scholar]
- Shorey RC, Rhatigan DL, Fite PJ, Stuart GL. Dating violence victimization and alcohol problems: An examination of the stress-buffering hypothesis for perceived support. Partner Abuse. 2011;2:31–45. [Google Scholar]
- Silverman JG, Raj A, Mucci LA, Hathaway JE. Dating violence against adolescent girls and associated substance use, unhealthy weight control, sexual risk behavior, pregnancy, and suicidality. Journal of the American Medical Association. 2001;2863(5):572–579. doi: 10.1001/jama.286.5.572. [DOI] [PubMed] [Google Scholar]
- Smith DK, Leve LD, Chamberlain P. Adolescent girls’ offending and health-risking sexual behavior: The predictive role of trauma. Child Maltreatment. 2006;11(4):346–353. doi: 10.1177/1077559506291950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Timeline Follow-Back: A technique for assessing self-reported alcohol consumption. In: Litten R, Allen J, editors. Measuring Alcohol Consumption: Psychosocial and biological methods. Totowa, N.J: Humana Press; 1992. pp. 41–72. [Google Scholar]
- Straus MA, Douglas EM. A short form of the revised Conflict Tactics Scales, and typologies for seventy and mutuality. Violence and Victims. 2004;19(5):507–520. doi: 10.1891/vivi.19.5.507.63686. [DOI] [PubMed] [Google Scholar]
- Straus MA, Hamby SL, Boney-McCoy S, Sugarman DB. The revised conflict tactics scales (CTS2): development and preliminary psychometric data. Journal of Family Issues. 1996;17(3):283–316. [Google Scholar]
- Temple JR, Freeman D. Dating violence and substance use among ethnically diverse adolescents. Journal of Interpersonal Violence. 2011;26(4):701–718. doi: 10.1177/0886260510365858. [DOI] [PubMed] [Google Scholar]
- Upchurch DM, Kusunoki Y. Associations between forced sex, sexual and protective practices, and sexually transmitted diseases among a national sample of adolescent girls. Women’s Health Issues. 2004;14(3):75–84. doi: 10.1016/j.whi.2004.03.006. [DOI] [PubMed] [Google Scholar]
- Weathers F, Litz B, Herman D, Huska J, Keane T. The PTSD Checklist (PCL): Reliability, Validity, and Diagnostic Utility. Paper presented at the Annual Convention of the International Society for Traumatic Stress Studies; San Antonio, TX. Oct, 1993. [Google Scholar]
- Wingood GM, DiClemente RJ. The effects of an abusive primary partner on the condom use and sexual negotiation practices of African-American women. American Journal of Public Health. 1997;87(6):1016–1018. doi: 10.2105/ajph.87.6.1016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wingood GM, DiClemente RJ, McCree DH, Harrington K, Davies SL. Dating violence and the sexual health of Black adolescent females. Pediatrics. 2001;107:E72–E75. doi: 10.1542/peds.107.5.e72. [DOI] [PubMed] [Google Scholar]
- Yehuda R, Lehrner A, Rosenbaum TY. PTSD and sexual dysfunction in men and women. Journal of Sexual Medicine. 2015;12:1107–1119. doi: 10.1111/jsm.12856. [DOI] [PubMed] [Google Scholar]
- Zelechosiki AD, Sharma R, Beserra K, Miguel JL, DeMarco M, Spinazzola J. Traumatized youth in residential treatment settings: Prevalence, clinical presentation, treatment, and policy implications. Journal of Family Violence. 2013;28(7):639–652. [Google Scholar]
- Zhang W, O’Brien N, Forrest JI, Salters KA, Patterson TL, Montaner JS, Hogg RS, Lima VD. Validating a shortened depression scale (10 item CES-D) among HIV-positive people in british columbia, canada. PLoS One. 2012;7(7):e40793. doi: 10.1371/journal.pone.0040793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao X, Lynch JG, Chen Q. Reconsidering Baron and Kenny: Myths and truths about mediation analysis. Journal of Consumer Research. 2010;37(2):197–206. [Google Scholar]