Abstract
Perinatal route of transmission of human papillomavirus (HPV) has been demonstrated in several small studies. We designed a large prospective cohort study (HERITAGE) to better understand perinatal HPV. The objective of this article is to present the study design and preliminary data. In the first phase of the study, we recruited 167 women in Montreal, Canada, during the first trimester of pregnancy. An additional 850 are currently being recruited in the ongoing phase. Cervicovaginal samples were obtained from mothers in the first trimester and tested for HPV DNA from 36 mucosal genotypes (and repeated in the third trimester for HPV-positive mothers). Placental samples were also taken for HPV DNA testing. Conjunctival, oral, pharyngeal and genital samples were collected for HPV DNA testing in children of HPV-positive mothers at every 3–6 months from birth until 2 years of age. Blood samples were collected in mother and children for HPV serology testing. We found a high prevalence of HPV in pregnant women (45%[95%CI:37–53%]) and in placentas (14%[8–21%]). The proportion of HPV positivity (any site) among children at birth/3-months was 11%[5–22%]. HPV was detected in children in multiple sites including the conjunctiva (5%[10–14%]). The ongoing HERITAGE cohort will help provide a better understanding of perinatal HPV.
Keywords: Human papillomavirus (HPV), Perinatal transmission, Pregnancy, Placenta, Children, Persistence
1. Introduction
Human papillomaviruses (HPVs) are unequivocally recognised as the necessary cause of virtually all cervical cancers, of a substantial proportion of many other anogenital neoplasms (anal, vaginal, vulvar, and penile cancers), of a non-negligible portion of head and neck cancers (oral cavity, pharynx, and larynx) and are also suspected to play a role in other neoplasms as well, such as conjunctiva carcinoma [1], [2], [3], [4]. HPVs also cause benign lesions such as respiratory papillomatosis and anogenital condylomas [5], [6]. HPV infection is the most common sexually transmitted infection in the world. The prevalence of any cervical HPVs among cytologically normal women in the Americas has been estimated at 4.8% [7] and can reach 30–50% among young sexually active women of reproductive age [8], [9]. Most HPV infections are asymptomatic and only a small proportion of infected individuals will progress to persistent infection and even less to cancer, as most people will clear the infection within 12–24 months [10].
Evidence suggests that newborns are exposed to HPV in the perinatal period and can contract the infection. Vertical transmission of HPV (perinatal infection) was first reported in 1956 in a case of juvenile laryngeal papillomatosis [11]. Confirmation of the perinatal transmission in different mucosa (genital, oral) was subsequently supported in several studies, although the exact mode of transmission is not well understood. Previous small studies have reported widely varying rates of infection in newborns, with estimates ranging from 4% to 79% among day old infants born to mothers testing positive for HPV during pregnancy [12], [13], [14], [15], [16], [17], [18], [19], [20], [21], [22], [23], [24].
There is a need for a better understanding of the rate and determinants of perinatal transmission as well as the rate and determinants of HPV persistence in children in a prospective study with a large sample size and long term follow-up [25]. The incidence of HPV-associated diseases, such as squamous cell carcinomas, has increased in children in recent years which may be, in part, related to an increase in HPV prevalence in parents [26], [27]. The impact of HPV on pregnancy outcomes also needs to be elucidated. We undertook such a study on Human Papillomavirus perinatal transmission and risk of HPV persistence among children (HERITAGE study) to further our understanding of HPV perinatal transmission and natural history of HPV infection. The aim of this article is to present the study design and provide preliminary data from this large prospective cohort study on the perinatal transmission of HPV.
2. Methods
2.1. Design and participants
HERITAGE is a prospective cohort study of pregnant women recruited in academic hospitals and high volume obstetrical units in Montreal, Canada. Within each hospital, participants were recruited in outpatient obstetric clinics catering to the local community. Pregnant women were accrued in the first phase of the study from November 2010 to June 2012 at Sainte-Justine hospital centre, at the Centre Hospitalier de l′Université de Montréal (CHUM) and at St-Mary's Hospital. For the extended phase, the recruitment was from February 2015 to July 2016 in Sainte-Justine hospital centre and the CHUM (and affiliated clinics). The first phase of HERITAGE was undertaken as an ancillary study of the 3D-study (Design, Discover, Develop), a prospective birth cohort of the Integrated Research Network in Perinatology of Québec and Eastern Ontario (IRNPQEO) network through the main university hospitals affiliated with Québec's 4 medical faculties: Université de Montréal, McGill University, Université Laval and Université de Sherbrooke. Through a CIHR grant, the IRNPQEO network put in place a cohort of 2366 pregnant women (recruitment between 2010 and 2012) in Quebec to address specific disease mechanisms, while providing a comprehensive perspective of combined prenatal exposures on both birth outcomes and infant health until 2 year of age. Recruitment for HERITAGE was implemented in 3 teaching hospitals participating to IRNPQEO in Montreal (Sainte-Justine, CHUM and St-Mary's Hospital) as a subsample of the 3D-study.
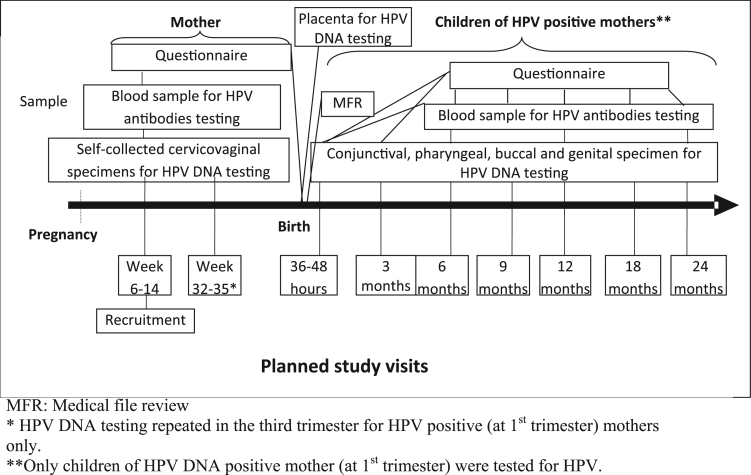
Pregnant women 18 years of age and older and between 6 and 14 weeks of gestation (restricted to 18–30 years old women and 8–14 weeks of gestation for the first phase) and planning to give birth in a participating hospital were eligible to be enroled in HERITAGE. Exclusion criteria were: unable to provide informed consent and HIV infection. The total number of women recruited in phase 1 was 167 and an additional 850 are expected to be recruited in the extended phase (phase 2). Pregnant women (recruited during the first trimester of pregnancy) provided samples for HPV DNA (cervociovaginal samples at first trimester and placenta samples at birth) and for HPV serology. HPV DNA testing was repeated in the third trimester for participants who tested positive in the 1st trimester. Children of participants who tested HPV DNA positive in first trimester were followed until 2 years of age, according to the timeline presented in Fig. 1. Additionally, children of phase 1 were followed until 5 years of age (at 3, 4 and 5 year old) for HPV DNA and HPV serology testing. Mothers signed an informed consent form. Nurses and research staff were trained for the collection of samples in adult and children participants and to disclose and explain HPV DNA test results. The study protocol was approved by the institutional ethical and research review boards of the participating institutions.
Fig. 1.
Design and timeline for information and specimen collection. MFR: Medical file review. *HPV DNA testing repeated in the third trimester for HPV positive (at 1st trimester) mothers only. **Only children of HPV DNA positive mother (at 1st trimester) were tested for HPV.
2.2. Specimen and data collections
2.2.1. Swabs in pregnant participants and children for HPV DNA testing
At the first visit (recruitment), a self-collected cervicovaginal specimen was obtained using a dry Dacron swab (Copan Italia S.p.A) from pregnant mothers for type-specific HPV DNA testing (Fig. 1). An additional self-collected cervicovaginal dry Dacron swab for type-specific HPV DNA testing was obtained at a second visit (at week 32–35) from mothers who were HPV positive in the first trimester. In children born from HPV-positive mother, specimens were collected by a research nurse at 36–48 h (delayed from birth to avoid contamination from the mother), and at 3, 6, 9, 12, 18 and 24 months. Scrapings for HPV DNA testing were collected from the: 1) labia or prepuce and scrotum and anal region (genital sample) (Dacron swab); 2) oral mucosa (buccal) (Dacron swab); 3) pharyngeal mucosa (Dacron swab) as well as 4) from the conjunctive using a soft swab (FLOQSwabs™, Copan Flock Technologies). For the conjunctiva, 2 samples were collected (one for left eye and one for right eye). For the visit planned at 36–48 h after birth, research nurses met mothers/children before they were discharged from the hospital. Postnatal visits were all done at Sainte-Justine Hospital. Mothers and children were asked to come to Saint-Justine Hospital for the postnatal follow-up visits but were also offered home-visits.
Swabs from women and children were rinsed individually in 1.5 ml of PreservCyt (Cytyc Corporation, Boxborough, MA) in a plastic vial, DNA was purified with the Master pure procedure [28], [29] and stored at −70° until testing.
2.2.2. Swabs and biopsies on placenta for HPV DNA testing
At delivery, placenta brush and biopsy specimens were collected for HPV DNA testing on both maternal and foetal side for every participant. The placenta was collected after birth, rinsed in tap water to remove excess blood and placed on the maternal side so the cord (foetal side) was facing upward. Two cytology brushes were used to collect cells from peripheral and central zones taking the implantation of the cord as landmark. For each zone, two biopsies (0.5 cm3) were then taken using scissors and clamps (individual for each biopsy to avoid contamination). For maternal side specimens, the placenta was turned over so the maternal side faced upwards. Brush samples and biopsies (peripheral and central) were taken according to the same procedure and care for contamination. Virox™ was used to clean scissors, clamps and all other tools after the procedure. Gloves were changed at each different step to avoid contamination: after the placenta was rinsed and for specimen collection on each side (maternal and foetal). In phase 2, two additional brush samples were collected from the foetal side. For both peripheral and central zone, we collected a brushing from the membrane and one after the foetal membrane was removed. Biopsies were collected after the membrane has been removed.
After specimen collection, swabs were placed directly into a plastic vial with a liquid preservative, processed and stored as described above. The biopsies were placed in cryogenic storage tubes, processed and stored as described above.
2.2.3. Blood in pregnant participants and children for HPV antibody testing
At the first visit, drops of blood on blotter were collected from the mother for HPV antibodies testing (serum from women was also collected in the first phase in order to validate antibody testing on blotter). A few drops of blood on blotter were also collected from children at birth, 6, 12 and 24 months for HPV antibodies testing. At birth, drops of blood were collected at the same time as the heel-prick Guthrie test.
Drops of blood were collected on blotting paper (Whatman 903™, GE healthcare Ltd.) using a Contact-Activated Lancet (BD Microtainer®) for both mother and children. After a minimum of 2–6 h at ambient air, the blotting paper was stored at −80° pending transfer to the Laboratoire de Santé Publique du Québec (LSPQ) for various HPV antibody testing. Serum collected from mother was placed in cryogenic storage tubes and stored at −80° until being transfer to the LSPQ.
2.2.4. Questionnaires and medical file review (MFR)
At entry, a questionnaire documented socio-demographic data and pre-birth indicators including: age, ethnic group, marital status, education, annual household income, gestational age at recruitment, number of previous pregnancies, number of children, age at first pregnancy, medical history (HPV vaccination, abnormal Pap test, history of colposcopy assessment, infertility, etc.), sexual activity (lifetime number of sexual partners, age at first intercourse, number of sexual partner during the last year, etc.) and smoking, alcohol and drugs consumption. During follow-up, questionnaires and/or medical file review (MFR) documented additional information on a range of variables during pregnancy (update on medical history, Pap testing, sexual activity, number of sexual relations per week, smoking, alcohol and drug consumption) and at delivery (method of delivery, rupture of membrane, labour length, cervix maturation method, induction method, episiotomy, vaginal lacerations, neonatal information for the baby, pregnancy outcome, preeclampsia, etc.). Questionnaires for post-partum and follow-up visits collected information on breastfeeding, child's height and weight, child's health, child's medication and environmental exposures such as mother's alcohol, smoking and drug consumption.
2.3. HPV DNA testing
The Linear Array HPV genotyping assay (LA-HP; Roche Molecular Systems) was used to detect 36 mucosal HPV genotypes including types 6, 11, 16, 18, 26, 31, 33, 34 (formerly known as type 64), 35, 39, 40, 42, 44 (formerly known as type 55), 45, 51, 52, 53, 54, 56, 58, 59, 61, 62, 66, 67, 68, 69, 70, 71, 72, 73, 81, 82, 83, 84, and 89. β-globin DNA was co-amplified to assess DNA integrity and to screen for the presence of inhibitors [28], [30], [31], [32]. Negative, weak positive and strong positive controls were included in each amplification run. Extensive safeguards to avoid contamination were used. Samples that were both β-globin and HPV-negative were considered inadequate. HPV-52 was detected in the LA with a probe that also cross-reacts with types 33, 35 and 58. Samples reactive in the LA with the cross-reactive probe for HPV52 were further tested with a validated HPV-52-specific real-time PCR assay [33]. HPV molecular variant analysis as well as measures of HPV viral load will also be conducted in future studies.
2.4. Antibodies to HPV capsids testing
Blood samples collected on blotter from mothers (during pregnancy) and children (at birth, and month 6, 12 and 24) were tested for HPV antibodies using HPV Virus-Like Particle (VLP)-Based Enzyme Immunoassay for seroreactivity to HPV types 6/11/16/18 capsids. Serum and blotter blood samples collected in mothers were compared to validate HPV serology testing on blotter. Testing was done at the LSPQ under the supervision of an expert in serodiagnosis.
2.5. Statistical analysis
Descriptive analysis was used to describe prevalence of type-specific HPV and groups of HPV (HR- and LR-types) among pregnant women, placenta and in children for phase 1. Mean, median, inter-quartile range (IQR) were computed for continuous variables and proportion (and 95% CI) was used for categorical variables.
Twelve genotypes are officially recognised as High-Oncogenic risk (HR-) HPV (HPV-16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59) according to their frequency of association with malignancy while 13 others are recognised as possibly HR-HPV according to the latest classification published by the World Health Organization's International Agency for Research on Cancer (IARC) [34]. Other classifications also categorised genotype, 66, 68, 73 and 82 as HR-HPV [35], [36]. In this study, for HPV groups, HPV-16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 66, 68, 73 and 82 were considered HR-HPV, and HPV types 6, 11, 26, 34, 40, 42, 44, 53, 54, 61, 62, 67, 69, 70, 71, 72, 81, 83, 84 and 89 were considered as low oncogenic risk (LR-HPVs) [34], [35], [36].
3. Results
Of the 207 women identified as eligible to participate in the phase 1 of the HERITAGE study, 167 accepted to participate (participation rate=81%). Table 1 describes the characteristics at baseline of the participants recruited in Phase 1. The mean and median age of participating women were 26.9 years (SD±2.4) and 27.5 years (Interquartile range (IQR)=25.8–28.6), respectively. Mean age was similar between HPV-positive and -negative women (27.1 versus 26.7 years of age, respectively), the majority identified as Caucasian (79%) and 94.0% were not vaccinated for HPV.
Table 1.
Characteristics at enrolment of the 167 participants recruited in phase 1 of HERITAGE.
| Variables | ||
|---|---|---|
| Age | Mean (SD): | 26.9 (±2.4) |
| Median (IQR): | 27.5 (25.8–28.6) | |
| Race; n (%) | White | 130 (78.8) |
| Other | 35 (21.2) | |
| Education; n (%) | Completed elementary | 11 (6.6) |
| Completed secondary | 23 (13.8) | |
| College | 47 (28.1) | |
| University | 75 (44.9) | |
| Other/missing | 11 (6.6) | |
| Marital status; n (%) | Married | 43 (25.9) |
| Common law/living with a partner | 105 (63.3) | |
| Single | 16 (9.6) | |
| Divorced | 2 (1.2) | |
| Annual household income; n (%) | Low (≤39,999$) | 42 (26.1) |
| Middle low (40,000–59,999$) | 38 (23.6) | |
| Middle high (60,000– 99,999$) | 53 (32.9) | |
| High (≥100,000$) | 28 (17.4) | |
| HPV vaccinated; n (%) | No | 156 (94.0) |
| Yes (all with Gardasil® (4 types)) | 10 (6.0) | |
| Lifetime smoking; n (%) | No | 105 (63.3) |
| Yes | 61 (36.8) | |
| Age first sexual intercourse | Mean (SD) | 16.9 (±2.8) |
| Median (IQR) | 17 (16–18) | |
| Number of lifetime sexual partners | Mean (SD) | 9.7 (±6.5) |
| Median (IQR) | 9.5 (3–16) | |
| Number of sexual partners in the last year | Mean (SD) | 1.1 (±0.8) |
| Median (IQR) | 1 (1–1) | |
| Type of deliverya; n (%) | Spontaneous | 109 (71.7) |
| Vaginal with vacuum | 3 (2.0) | |
| Vaginal with forceps | 9 (5.9) | |
| Caesarian-section | 31 (20.3) | |
| Gestational age | Mean | 39.5 (±2.0) |
Missing data excluded. n, number; SD, standard deviation; IQR, interquartile range.
Excluded miscarriage, stillbirth.
3.1. HPV DNA in pregnant women
The proportion of pregnant women who were HPV-positive at the time of recruitment (first trimester) was 45% [95% Confidence Intervals (CI): 37–53%] (75 out of 167). Of those, 80% [95% CI: 70–88%] were still infected during the third trimester (60 out of 75). From the 75 women infected at baseline, 56 (33.5% [95% CI: 26–41%]) were infected with HR-HPV. There were 14 women (out of the 75 infected at first trimester) who acquired a new HPV type at the second sampling (third trimester) (19% [95% CI: 11–29%]). Multiple types were frequently detected among HPV-infected women with 38 (out of 75) (51% [95% CI: 39–62%]) harbouring ≥2 genotypes (range=2–11). The mean number of genotypes detected was 1.2 (SD=1.8). Table 2 shows type-specific prevalence of HPV among women at first trimester.
Table 2.
Prevalence of genotype-specific HPV infection among pregnant women at first trimester.
| HPV genotype | n | % (n type+/n) | 95% LCI | 95% HCI |
|---|---|---|---|---|
| 6 | 1 | 0.6 | 0.0 | 3.3 |
| 11 | 0 | 0.0a | 0.0 | 2.2 |
| 16 | 10 | 6.0 | 2.9 | 10.7 |
| 18 | 7 | 4.2 | 1.7 | 8.4 |
| 26 | 0 | 0.0a | 0.0 | 2.2 |
| 31 | 12 | 7.2 | 3.8 | 12.2 |
| 33 | 3 | 1.8 | 0.4 | 5.2 |
| 34 | 1 | 0.6 | 0.0 | 3.3 |
| 35 | 3 | 1.8 | 0.4 | 5.2 |
| 39 | 11 | 6.6 | 3.3 | 11.5 |
| 40 | 3 | 1.8 | 0.4 | 5.2 |
| 42 | 8 | 4.8 | 2.1 | 9.2 |
| 44 | 5 | 3.0 | 1.0 | 6.8 |
| 45 | 2 | 1.2 | 0.1 | 4.3 |
| 51 | 7 | 4.2 | 1.7 | 8.4 |
| 52 | 8 | 4.8 | 2.1 | 9.2 |
| 53 | 10 | 6.0 | 2.9 | 10.7 |
| 54 | 7 | 4.2 | 1.7 | 8.4 |
| 56 | 3 | 1.8 | 0.4 | 5.2 |
| 58 | 6 | 3.6 | 1.3 | 7.7 |
| 59 | 9 | 5.4 | 2.5 | 10.0 |
| 61 | 5 | 3.0 | 1.0 | 6.8 |
| 62 | 11 | 6.6 | 3.3 | 11.5 |
| 66 | 4 | 2.4 | 0.7 | 6.0 |
| 67 | 3 | 1.8 | 0.4 | 5.2 |
| 68 | 2 | 1.2 | 0.1 | 4.3 |
| 69 | 0 | 0.0a | 0.0 | 2.2 |
| 70 | 2 | 1.2 | 0.1 | 4.3 |
| 71 | 2 | 1.2 | 0.1 | 4.3 |
| 72 | 0 | 0.0a | 0.0 | 2.2 |
| 73 | 6 | 3.6 | 1.3 | 7.7 |
| 81 | 1 | 0.6 | 0.0 | 3.3 |
| 82 | 3 | 1.8 | 0.4 | 5.2 |
| 83 | 4 | 2.4 | 0.7 | 6.0 |
| 84 | 5 | 3.0 | 1.0 | 6.8 |
| 89 | 14 | 8.4 | 4.7 | 13.7 |
| HPV groups | ||||
| Any HPV | 75 | 44.9 | 37.2 | 52.8 |
| HR-HPV | 56 | 33.5 | 26.4 | 41.2 |
| LR HPV only | 19 | 11.4 | 7.0 | 17.2 |
| ß-globin negative | 0 | 0 | ||
n, number; LCI, low confidence interval; HCI, high confidence interval; HR-, high-oncogenic risk; LR-, low-oncogenic risk.
One-sided, 97.5% confidence interval.
3.2. HPV DNA in placenta
The overall prevalence of HPV in placental brush samples was 14% [95% CI: 8–21%] (Table 3). The prevalence of HPV in placental brush samples for women who tested positive for HPV DNA during the first trimester was 27% [95% CI: 16–40%] whereas it was only 3% [95% CI: 0.3–10%] for those who tested negative during the first trimester.
Table 3.
Prevalence of any HPV in placenta.
| HPV in placenta |
Total |
HPV DNA positive women at 1st trimester |
HPV negative women at 1st trimester |
|||
|---|---|---|---|---|---|---|
| n | % (95% CI) | n | % (95% CI) | n | % (95% CI) | |
| BRUSH | ||||||
| HPV positive | 18 | 14% (8–21) | 16 | 27% (16–40) | 2 | 3% (0.3–10) |
| HPV negative | 112 | 86% (79–92) | 44 | 73% (60–84) | 68 | 97% (90–99) |
| ß-globin neg | 0 | – | 0 | – | 0 | – |
| Total tested | 130 | 60 | 70 | |||
| Missinga | 37 | |||||
| BIOPSY | ||||||
| HPV positive | 6 | 5% (2–10) | 5 | 8% (3–18) | 1 | 2% (1–7) |
| HPV negative | 124 | 95% (90–98) | 55 | 92% (82–97) | 69 | 98% (93–99) |
| Total tested | 130 | 60 | 70 | |||
n=Number.
Missing results included pregnancy interruption, withdrawn, women who gave birth to another hospital and missing HPV DNA testing on placenta at birth.
The proportion of HPV-positive placental biopsies was lower than placental brushes with an overall HPV prevalence of 5% [95% CI: 2–10%]. A prevalence of 8% [95% CI: 3–18%] and 2% [95% CI: 1–7%] was estimated among HPV-positive and -negative women in the first trimester, respectively (Table 3). Table 4 describes longitudinal type-specific infections (during pregnancy, in placental samples (brush and biopsy) and in children at birth and/or 3 months) for women who were HPV-positive on placental samples or who had an HPV positive child. In our study, we detected HPV on both sides of the placenta (foetal and maternal) and when placental infection was detected, it was often with genotypes detected in the cervicovaginal sample during pregnancy (14 out of 18 HPV positive placenta were infected with genotype(s) detected in women during pregnancy).
Table 4.
HPV genotypes detected in women with placental infection or who delivered a children who was HPV positive.
| During pregnancy |
Placenta |
Children (at birth and/or 3 month of age) |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| 1st trimester |
3rd trimester |
Swabs |
Biopsies |
Conjunctival |
Oral |
Pharyngeal |
Genital |
||
| Maternal sidea | Foetal sidea | Maternal sidea | Foetal sidea | ||||||
| 52, 62 | 52, 62, 89 | 89 | 89 | – | – | – | – | – | – |
| 59 | 59 | – | 59 | – | – | – | – | – | – |
| 16, 73 | 16 | 16, 39 | – | – | – | – | – | – | – |
| 66, 70, 89 | 66 | 66 | – | – | – | – | – | – | – |
| 16, 59 | 16, 59 | 16 | 16, 59 | – | – | – | – | – | – |
| 31, 35, 42, 51, 53, 58 | 31, 35, 42, 51, 53, 58, 84 | 51 | 42, 51 | – | – | – | 39, 42 | 42 | 42 |
| 31, 34, 59 | Missing samples | 31, 68 | 31, 68 | – | 34, 68 | 31 | 31 | – | 31 |
| 39 | 39 | 39 | – | 39 | – | – | – | – | – |
| – | Missing samples | 16 | – | 16 | – | – | – | – | – |
| 16 | 16 | 16 | – | – | 16 | – | – | – | – |
| – | Missing samples | 16 | – | – | – | – | – | – | – |
| 53 | 53 | 53 | – | – | – | – | – | – | – |
| 66 | 16, 66 | – | 44 | – | – | – | – | – | – |
| 51, 52, 53, 59, 67, 73, 82 | 51, 52, 53, 54, 59 | 51, 52, 53, 54 | 52, 53, 54 | 51, 52, 53 | 52, 53 | – | – | – | – |
| 53 | – | – | 53 | – | – | – | – | – | – |
| 18, 31, 84 | 18, 31, 84 | 39 | – | – | – | – | – | – | – |
| 51 | 51 | 51 | 51 | – | 51 | 51 (both eyes) | – | – | 51 |
| 33, 56, 73 | 33, 56 | – | 33, 56 | – | – | – | – | – | – |
| 53 | 59 | – | – | – | – | – | 89 | – | – |
| 89 | 89 | – | – | – | – | – | 89 | – | – |
| 18 | 18 | – | – | – | – | – | 18 | ||
| 40, 42, 71, 83 | 40, 62, 71, 73, | – | – | – | – | 62 | – | – | – |
–=HPV negative.
Included infection detected in peripheric and/or central zone.
3.3. Children
Overall, 67 children were tested for HPV at birth (from the 75 HPV-positive participating mother (89%)). The reason for missing HPV results among offspring included miscarriage, stillbirth, withdrawals and missing HPV DNA testing on the child at birth. Table 5 shows the prevalence of HPV among children at birth and/or 3 months of age. Interestingly, 4.8%, 8.1%, 1.6% and 4.8% of samples were positive for HPV for conjunctival, oral, pharyngeal and genital sites, respectively. Globally, seven (11.2% [95% CI: 4.7–21.9]) children were HPV-positive in at least one site, some of them testing positive at multiples sites (mouth, pharynx, genital surface). One of the most novel findings of our study is the detection of HPV in conjunctival samples of 3 children. One of them was infected with the same genotype in both eyes (Table 4) and was born to a mother who tested persistently positive during pregnancy (and placenta) for the same HPV genotype.
Table 5.
Number (and %) of children HPV positive (any of the 36 genotypes) at birth/3-month visits.
| Totala |
HPV positive |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Conjunctive (left and/or right eye) | Oral (mouth) | Pharynx (throat) | Genital (surface) | All sites combined | ||||||
| N | % (95% CI) | N | % (95% CI) | N | % (95% CI) | N | % (95% CI) | N | % (95% CI) | |
| 67 | 3 | 4.8% (10.1–13.5) | 5 | 8.1% (2.7–17.8) | 1 | 1.6% (0.4–8.6) | 3 | 4.8% (10.1–13.5) | 7 | 11.2% (4.7–21.9) |
Number of children tested for HPV from the 75 women who tested HPV positive during pregnancy. Missing HPV results included miscarriage, stillborn, withdraw and missing HPV DNA testing on child at birth.
4. Discussion
We found a high prevalence (44.9%) of HPV at prenatal testing in young pregnant women.
Furthermore, HPV was frequently detected in placenta samples (14%). There was a non-negligible global prevalence (11.2%) of HPV in newborns (at birth and/or at 3 months of age) from HPV-positive mother. This is also the first study to report transmission of HPV in children's conjunctiva. This interesting data lead to the continuation of the study with an extended phase (phase 2) to increase sample size. The data also seems to be in accordance with recent small studies that report that perinatal transmission (oral and/or genital) is between 4–22% [17], [20], [21], [23], [24]. In their meta-analysis published in 2005, Medeiros et al., estimated the perinatal transmission of HPV at 20% [37].
There are many reasons to explain the high prevalence of HPV found in our cohort of pregnant women. First, cervicovaginal samples were collected for which prevalence is expected to be higher than in cervical samples. The “wide area” sampling of the lower genital track detects HPV in multiple foci in the cervical and vaginal areas. Also, these are young women (18–30 years) who are more likely to be infected than older women and they obviously all had sexual activity (the most important risk factor for HPV) in a near past as they are pregnant. Furthermore, a low proportion of women were vaccinated against HPV and herd immunity is very unlikely as the school-based vaccination programme in Quebec started in 2008, a few years only before our study.
Perinatal transmission in different mucosa seems possible although the exact mode of transmission is not well understood. Most cases of vertical transmission may occur at delivery through direct contact of the foetus with maternal infected cells during vaginal delivery or at caesarean section following early membrane rupture [25], [38]. Transmission in utero is also possible through ascending infection from mother's genital tract or HPV infected semen present in the vagina following sexual intercourse [25], [26]. Peri-conceptional transmission from male sexual partner is possible since HPV DNA has been detected in 8–64% of the seminal fluid and spermatozoa [25], [26], [27], [28], [29], [30], [31], [32], [33], [34], [35], [36], [37], [38], [39]. Moreover, HPV DNA has been detected in the endometrium and ovaries. However, HPV transmission to the embryos just after fertilisation remains theoretical [25]. Transplacental transmission has also been supported as HPV DNA was detected in amniotic fluid with detection rates varying between 15–65% [40], [41], [42]. HPV DNA has also been found in placental cells and in cord blood. The detection rate of HPV DNA in trophoblastic cells varies from 0% to 60% [42], [43], [44], [45], [46] and from 0% to13% in cord blood cells [23], [44], [46], [47], [48]. Recently, HPV DNA has been detected in breast milk with a rate varying between 2–8% [49], [50], [51] suggesting that HPV could be transmitted vertically to neonates through breastfeeding. Finally, horizontal transmission just after delivery can occur via digital contacts [26].
Risk factors for perinatal transmission are not well characterised. The following factors have been associated with transmission: viral load [52], lesions in maternal genital tract [53] and maternal HPV infection with multiple genotypes [21], [24]. Several authors also reported a higher risk of transmission following a vaginal delivery [17], [21], [24], [41] but these results are controversial [54]. Finally, very little is known about the effect of HPV on pregnancy outcomes. In vitro experiments suggest that the presence of HPV in trophoblastic cells could induce changes in placental viability and adhesion [55]. Interestingly, some observational studies found that HPV was associated with spontaneous abortion [43], [56], [57]; others did not find that association [58]. Other studies linked the infection to prematurity [54] and spontaneous preterm delivery [54], [59], [60]. Further studies on the consequences of HPV infection in pregnancy outcomes are needed. For example, to date, no clinical guidelines are in place to test sperm donor for HPV. A better understanding of mechanisms of transmission to the mother and her foetus could highlight the need for such guidelines. Furthermore, a better understanding of the development and persistence of HPV antibodies acquired during childhood will improve the overall comprehension of the natural history of HPV. Passively acquired immunity from maternal antibodies could also modulate acquisition and persistence of infection in the infant.
The first phase of our study is underpowered for an analysis of risk factors or statistical associations. With a larger sample size and a longer term follow-up, phase 2 of the HERITAGE study will allow analysis of the rate and determinants of perinatal transmission as well as the rate and determinants of persistent infection in children. With the completion of phase 2, we also expect to have adequate power to verify associations such as association between HPV infection and pregnancy outcomes as well as between mode of delivery and HPV transmission. The recruitment for the extended phase will end in September 2016. Accounting for pregnancy duration and at least 2-years follow-up of children, HERITAGE will provide final data in 2019.
Funding
HERITAGE study was supported by a Grant from the Canadian Institutes of Health Research (CIHR) (Grant MOP-93564 and MOP-136833) to HT. The IRNPQEO (3D study) was supported by the Canadian Institutes of Health Research [CRI 88413]. HT holds a salary award (chercheur-boursier) from the Fonds de la recherche du Québec en santé (FRQ-S) and from CIHR (New investigator salary award). MHM holds a salary award (chercheur-boursier clinicien) from the FRQ-S. Funding for quality control of HPV testing was provided in part by the Réseau FRQS SIDA-MI. PM is supported by the Research Institute of the McGill University Health Centre (Start-up funds).
Authors' contribution
All authors of this research paper have directly contributed to the conception and design (HT, MHM, FC, PM, WF, AMC), or acquisition of data (LL, JN, PB, IG, MJB, JL, FA), or analysis and interpretation (HT, MHM, FC, PB, AMC) of the study. HT, MHM and FC wrote the first draft of the manuscript. All authors have subsequently read, revised, and approved the version that is being submitted.
Competing interests
HT has received occasional lecture or consultation fees from GlaxoSmithKline Biologicals and Merck. MHM was a site PI for a Merck clinical trial on HPV vaccination. FC has received grants through his institution from Merck and Roche, as well as honoraria from Merck and Roche for lectures on HPV. All other co-authors have no conflict of interests.
Portions of the data presented in conferences
Portions of this manuscript were presented in an oral presentation form at the International HPV Conference (IPV) in Seattle in August 2014 [Niyibizi et al., Human papillomavirus (HPV) perinatal transmission and risk of HPV persistence among children: a cohort study. 29th International Papillomavirus (IPV) conference & Clinical Workshop. Seattle, USA. August 21–25, 2014] as well as in Porto Rico, in December 2012 [Trottier et al., Human papillomavirus (HPV) perinatal transmission and risk of HPV persistence among children: A cohort study. 28th IPV conference & Clinical Workshop, Porto Rico, December 2012] and in Montebello in Canada [Niyibizi et al., Human papillomavirus (HPV) perinatal transmission and risk of HPV persistence among children: a cohort study. Canadian National Perinatal Research Meeting. Montebello, Canada. February 2015].
Acknowledgement
The authors are grateful to Susanne Anderson, Hasna Meddour, Myra Geoffrion, Kathleen Auclair, Nicole Hurtubise, Véronique Prévost, Sophie Perreault, Lise-Angela Ouellet, Maryse Thibeault, Bouziane Azedine (Sainte-Justine Hospital), to Sylvie Daigle, Mélanie Robinson, Sophie Leblanc (CHUM Hospital) and to all other contributing research staffs for managing patients and specimens from all sites. Authors are also grateful to Josée Poirier, Audrey Janelle-Montcalm, Nicole Lupien, Martine Fournier, Isabelle Krauss and Cindy Rousseau for coordinating HERITAGE phase 1 study within the IRNPQEO and to Dr. Louise DuPerron, Dr Line Leduc and Dr. François Beaudoin for their help with the recruitment of patients. Authors are also grateful to Julie Guenoun,Émilie Comète and Pierre Forêt for DNA extraction and HPV testing.
References
- 1.Muñoz N., Castellsagué X., de González A.B., Gissmann L. Chapter 1: HPV in the etiology of human cancer. Vaccine. 2006;24(Suppl 3):S3/1–S10. doi: 10.1016/j.vaccine.2006.05.115. [DOI] [PubMed] [Google Scholar]
- 2.Parkin D.M., Bray F. Chapter 2: The burden of HPV-related cancers. Vaccine. 2006;24(Suppl 3):S3/11–S25. doi: 10.1016/j.vaccine.2006.05.111. [DOI] [PubMed] [Google Scholar]
- 3.Trottier H., Burchell A.N. Epidemiology of mucosal human papillomavirus infection and associated diseases. Public Health Genom. 2009;12(5–6):291–307. doi: 10.1159/000214920. [DOI] [PubMed] [Google Scholar]
- 4.Trottier H., Franco E.L. Part III: 8. Infectious diseases and cancer: HPV. In: Kramer A., Kretzschmar M., Krickeberg. K., editors. Modern Infectious Disease Epidemiology. Concept, Methods, Mathematical Models, Public Health. Springer; New York: 2010. p. 443. [Google Scholar]
- 5.Stanley M. Pathology and epidemiology of HPV infection in females. Gynecol. Oncol. 2010;117(Suppl 2):S5–S10. doi: 10.1016/j.ygyno.2010.01.024. [DOI] [PubMed] [Google Scholar]
- 6.Lacey C.J., Lowndes C.M., Shah K.V. Chapter 4: Burden and management of non-cancerous HPV-related conditions: HPV-6/11 disease. Vaccine. 2006;24(Suppl 3):S3/35–S41. doi: 10.1016/j.vaccine.2006.06.015. [DOI] [PubMed] [Google Scholar]
- 7.Bruni L., Diaz M., Castellsagué X., Ferrer E., Bosch F.X., de Sanjosé S. Cervical human papillomavirus prevalence in 5 continents: meta-analysis of 1 million women with normal cytological findings. J. Infect. Dis. 2010;202(12):1789–1799. doi: 10.1086/657321. [DOI] [PubMed] [Google Scholar]
- 8.Muñoz N., Méndez F., Posso H., Molano M., van den Brule A.J., Ronderos M., Meijer C., Muñoz A., Instituto Nacional de Cancerologia HPV Study Group Incidence, duration, and determinants of cervical human papillomavirus infection in a cohort of Colombian women with normal cytological results. J. Infect. Dis. 2004;190(12):2077–2087. doi: 10.1086/425907. [DOI] [PubMed] [Google Scholar]
- 9.Trottier H., Franco E.L. The epidemiology of genital human papillomavirus infection. Vaccine. 2006;24(Suppl 1):S1–S15. doi: 10.1016/j.vaccine.2005.09.054. [DOI] [PubMed] [Google Scholar]
- 10.Schiffman M., Castle P.E. Human papillomavirus: epidemiology and public health. Arch. Pathol. Lab. Med. 2003;127:930–934. doi: 10.5858/2003-127-930-HPEAPH. [DOI] [PubMed] [Google Scholar]
- 11.Hajek E.F. Contribution to the etiology of laryngeal papilloma in children. J. Laryngol. Otol. 1956;70(3):166–168. doi: 10.1017/s0022215100052798. [DOI] [PubMed] [Google Scholar]
- 12.Pakarian F., Kaye J., Cason J., Kell B., Jewers R., Derias N.W., Raju K.S., Best J.M. Cancer associated human papillomaviruses: perinatal transmission and persistence. Br. J. Obstet. Gynaecol. 1994;101(6):514–517. doi: 10.1111/j.1471-0528.1994.tb13153.x. [DOI] [PubMed] [Google Scholar]
- 13.Cason J., Kaye J., Pakarian F., Raju K.S., Best J.M. HPV-16 transmission. Lancet. 1995;345:197–198. doi: 10.1016/s0140-6736(95)90204-x. [DOI] [PubMed] [Google Scholar]
- 14.Tenti P., Zappatore R., Migliora P., Spinillo A., Belloni C., Carnevali L. Perinatal transmission of human papillomavirus from gravidas with latent infections. Obstet. Gynecol. 1999;93(4):475–479. doi: 10.1016/s0029-7844(98)00459-1. [DOI] [PubMed] [Google Scholar]
- 15.Watts D.H., Koutsky L.A., Holmes K.K., Goldman D., Kuypers J., Kiviat N.B., Galloway D.A. Low risk of perinatal transmission of human papillomavirus: results from a prospective cohort study. Am. J. Obstet. Gynecol. 1998;178(2):365–373. doi: 10.1016/s0002-9378(98)80027-6. [DOI] [PubMed] [Google Scholar]
- 16.Bandyopadhyay S., Sen S., Majumdar L., Chatterjee R. Human papillomavirus infection among Indian mothers and their infants. Asian Pac. J. Cancer Prev. 2003;4(3):179–184. [PubMed] [Google Scholar]
- 17.Smith E.M., Ritchie J.M., Yankowitz J., Wang D., Turek L.P., Haugen T.H. HPV prevalence and concordance in the cervix and oral cavity of pregnant women. Infect. Dis. Obstet. Gynecol. 2004;12(2):45–56. doi: 10.1080/10647440400009896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rintala M.A., Grénman S.E., Järvenkylä M.E., Syrjänen K.J., Syrjänen S.M. High-risk types of human papillomavirus (HPV) DNA in oral and genital mucosa of infants during their first 3 years of life: experience from the Finnish HPV family study. Clin. Infect. Dis. 2005;41(12):1728–1733. doi: 10.1086/498114. [DOI] [PubMed] [Google Scholar]
- 19.Rombaldi R.L., Serafini E.P., Mandelli J., Zimmermann E., Losquiavo K.P. Transplacental transmission of human papillomavirus. Virol. J. 2008;5:106. doi: 10.1186/1743-422X-5-106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Castellsagué X., Drudis T., Cañadas M.P., Goncé A., Ros R., Pérez J.M., Quintana M.J., Muñoz J., Albero G., de Sanjosé S., Bosch F.X. Human papillomavirus (HPV) infection in pregnant women and mother-to-child transmission of genital HPV genotypes: a prospective study in Spain. BMC Infect. Dis. 2009;9:74. doi: 10.1186/1471-2334-9-74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Park H., Lee S.W., Lee I.H., Ryu H.M., Cho A.R., Kang Y.S., Hong S.R., Kim S.S., Seong S.J., Shin S.M., Kim T.J. Rate of vertical transmission of human papillomavirus from mothers to infants: relationship between infection rate and mode of delivery. Virol. J. 2012;9:80. doi: 10.1186/1743-422X-9-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Koskimaa H.M., Waterboer T., Pawlita M., Grénman S., Syrjänen K., Syrjänen S. Human papillomavirus genotypes present in the oral mucosa of newborns and their concordance with maternal cervical human papillomavirus genotypes. J. Pediatr. 2012;160(5):837–843. doi: 10.1016/j.jpeds.2011.10.027. [DOI] [PubMed] [Google Scholar]
- 23.Lee S.M., Park J.S., Norwitz E.R., Koo J.N., Oh I.H., Park J.W., Kim S.M., Kim Y.H., Park C.W., Song Y.S. Risk of vertical transmission of human papillomavirus throughout pregnancy: a prospective study. PLoS One. 2013;8(6):e66368. doi: 10.1371/journal.pone.0066368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hahn H.S., Kee M.K., Kim H.J., Kim M.Y., Kang Y.S., Park J.S., Kim T.J. Distribution of maternal and infant human papillomavirus: risk factors associated with vertical transmission. Eur. J. Obstet. Gynecol. Reprod. Biol. 2013;169(2):202–206. doi: 10.1016/j.ejogrb.2013.02.024. [DOI] [PubMed] [Google Scholar]
- 25.Syrjänen S. Current concepts on human papillomavirus infections in children. APMIS. 2010;118(6–7):494–509. doi: 10.1111/j.1600-0463.2010.02620.x. [DOI] [PubMed] [Google Scholar]
- 26.Syrjänen S., Puranen M. Human papillomavirus infections in children: the potential role of maternal transmission. Crit. Rev. Oral Biol. Med. 2000;11(2):259–274. doi: 10.1177/10454411000110020801. [DOI] [PubMed] [Google Scholar]
- 27.Chow C.W., Tabrizi S.N., Tiedemann K., Waters K.D. Squamous cell carcinomas in children and young adults: a new wave of a very rare tumor? J. Pediatr. Surg. 2007;42(12):2035–2039. doi: 10.1016/j.jpedsurg.2007.08.025. [DOI] [PubMed] [Google Scholar]
- 28.Coutlee F., Rouleau D., Petignat P. Enhanced detection and typing of human papillomavirus DNA in anogenital samples with PGMY primers and the linear aRRAY HPV genotyping test. J. Clin. Microbiol. 2006;44:1998–2006. doi: 10.1128/JCM.00104-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Koushik A., Ghosh A., Duarte-Franco E. The p53 codon 72 polymorphism and risk of high-grade cervical intraepithelial neoplasia. Cancer Detect. Prev. 2005;29:307–316. doi: 10.1016/j.cdp.2005.06.007. [DOI] [PubMed] [Google Scholar]
- 30.Castle P.E., Sadorra M., Garcia F., Holladay E.B., Kornegay J. Pilot study of a commercialized human papillomavirus (HPV) genotyping assay: comparison of HPV risk group to cytology and histology. J. Clin. Microbiol. 2006;44:3915–3917. doi: 10.1128/JCM.01305-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Castle P.E., Gravitt P.E., Solomon D., Wheeler C.M., Schiffman M. Comparison of linear array and line blot assay for detection of human papillomavirus and diagnosis of cervical precancer and cancer in the atypical squamous cell of undetermined significance and low-grade squamous intraepithelial lesion triage study. J. Clin. Microbiol. 2008;46:109–117. doi: 10.1128/JCM.01667-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gravitt P.E., Schiffman M., Solomon D. A comparison of linear array and hybrid capture 2 for detection of carcinogenic human papillomavirus and cervical precancer in ASCUS-LSIL triage study human papillomavirus genotype specificity of hybrid capture 2. Cancer Epidemiol. Biomark. Prev. 2008;17:1248–1254. doi: 10.1158/1055-9965.EPI-07-2904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Coutlee F., Rouleau D., Ghattas G. Confirmatory real-time PCR assay for human papillomavirus (HPV) type 52 infection in anogenital specimens screened for HPV infection with the linear array HPV genotyping test. J. Clin. Microbiol. 2007;45:3821–3823. doi: 10.1128/JCM.01145-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bouvard V., Baan R., Straif K., Grosse Y., Secretan B., El Ghissassi F., Benbrahim-Tallaa L., Guha N., Freeman C., Galichet L., Cogliano V., WHO International Agency for Research on Cancer Monograph Working Group A review of human carcinogens--Part B: biological agents. Lancet Oncol. 2009;10(4):321–322. doi: 10.1016/s1470-2045(09)70096-8. [DOI] [PubMed] [Google Scholar]
- 35.International Agency for Research on Cancer (IARC), Monographs on the evaluation of carcinogenic risks to humans, Human Papillomaviruses, vol. 100B, Lyon, France, 2009.
- 36.Muñoz N., Bosch F.X., de Sanjose S. Epidemiologic classification of human papillomavirus types associated with cervical cancer. N. Engl. J. Med. 2003;348:518–527. doi: 10.1056/NEJMoa021641. [DOI] [PubMed] [Google Scholar]
- 37.Medeiros L.R., Ethur A.B., Hilgert J.B., Zanini R.R., Berwanger O., Bozzetti M.Cl. Vertical transmission of the human papillomavirus: a systematic quantitative review. Cad. Sau´de Pu´blica. 2005;21:1006–1015. doi: 10.1590/s0102-311x2005000400003. [DOI] [PubMed] [Google Scholar]
- 38.Lacour D.E., Trimble C. Human papillomavirus in infants: transmission, prevalence, and persistence. J. Pediatr. Adolesc. Gynecol. 2012;25(2):93–97. doi: 10.1016/j.jpag.2011.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Laprise C., Trottier H., Monnier P., Coutlée F., Mayrand M.H. Prevalence of human papillomaviruses in semen: a systematic review and meta-analysis. Hum. Reprod. 2014;29(4):640–651. doi: 10.1093/humrep/det453. [DOI] [PubMed] [Google Scholar]
- 40.Armbruster-Moraes E., Ioshimoto L.M., Leao E., Zugaib M. Detection of human papillomavirus deoxyribonucleic acid sequences in amniotic fluid during different periods of pregnancy. Am. J. Obstet. Gynecol. 1993;169(4):1074. doi: 10.1016/0002-9378(93)90060-v. [DOI] [PubMed] [Google Scholar]
- 41.Xu S., Liu L., Lu S., Ren S. Clinical observation on vertical transmission of human papillomavirus. Chin. Med. Sci. J. 1998;13(1):29–31. [PubMed] [Google Scholar]
- 42.Favre M., Majewski S., De Jesus N., Malejczyk M., Orth G., Jablonska S. A possible vertical transmission of human papillomavirus genotypes associated with epidermodysplasia verruciformis. J. Investig. Dermatol. 1998;111(2):333–336. doi: 10.1046/j.1523-1747.1998.00312.x. [DOI] [PubMed] [Google Scholar]
- 43.Hermonat P.L., Kechelava S., Lowery C.L., Korourian S. Trophoblasts are the preferential target for human papilloma virus infection in spontaneously aborted products of conception. Hum. Pathol. 1998;29(2):170–174. doi: 10.1016/s0046-8177(98)90228-3. [DOI] [PubMed] [Google Scholar]
- 44.Sarkola M.E., Grénman S.E., Rintala M.A., Syrjänen K.J., Syrjänen S.M. Human papillomavirus in the placenta and umbilical cord blood. Acta Obstet. Gynecol. Scand. 2008;87(11):1181–1188. doi: 10.1080/00016340802468308. [DOI] [PubMed] [Google Scholar]
- 45.Weyn C., Thomas D., Jani J., Guizani M., Donner C., Van Rysselberge M., Hans C., Bossens M., Englert Y., Fontaine V. Evidence of human papillomavirus in the placenta. J. Infect. Dis. 2011;203(3):341–343. doi: 10.1093/infdis/jiq056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Worda C., Huber A., Hudelist G., Schatten C., Leipold H., Czerwenka K., Eppel W. Prevalence of cervical and intrauterine human papillomavirus infection in the third trimester in asymptomatic women. J. Soc. Gynecol. Investig. 2005;12(6):440–444. doi: 10.1016/j.jsgi.2005.03.003. [DOI] [PubMed] [Google Scholar]
- 47.Pao C.C., Lin S.S., Lin C.Y., Maa J.S., Lai C.H., Hsieh T.T. Identification of human papillomavirus DNA sequences in peripheral blood mononuclear cells. Am. J. Clin. Pathol. 1991;95(4):540–546. doi: 10.1093/ajcp/95.4.540. [DOI] [PubMed] [Google Scholar]
- 48.Skoczyński M., Goździcka-Józefiak A., Kwaśniewska A. Risk factors of the vertical transmission of human papilloma virus in newborns from singleton pregnancy – preliminary report. J. Matern. Fetal Neonatal Med. 2014;27(3):239–242. doi: 10.3109/14767058.2013.807238. [DOI] [PubMed] [Google Scholar]
- 49.Cazzaniga M., Gheit T., Casadio C., Khan N., Macis D., Valenti F., Miller M.J., Sylla B.S., Akiba S., Bonanni B., Decensi A., Veronesi U., Tommasino M. Analysis of the presence of cutaneous and mucosal papillomavirus types in ductal lavage fluid, milk and colostrum to evaluate its role in breast carcinogenesis. Breast Cancer Res. Treat. 2009;114(3):599–605. doi: 10.1007/s10549-008-0040-3. [DOI] [PubMed] [Google Scholar]
- 50.Sarkola M., Rintala M., Grénman S., Syrjänen S. Human papillomavirus DNA detected in breast milk. Pediatr. Infect. Dis. J. 2008;27(6):557–558. doi: 10.1097/INF.0b013e318169ef47. [DOI] [PubMed] [Google Scholar]
- 51.Yoshida K., Furumoto H., Abe A., Kato T., Nishimura M., Kuwahara A., Maeda K., Matsuzaki T., Irahara M. The possibility of vertical transmission of human papillomavirus through maternal milk. J. Obstet. Gynaecol. 2011;31(6):503–506. doi: 10.3109/01443615.2011.570814. [DOI] [PubMed] [Google Scholar]
- 52.Kaye J.N., Cason J., Pakarian F.B., Jewers R.J., Kell B., Bible J., Raju K.S., Best J.M. Viral load as a determinant for transmission of human papillomavirus type 16 from mother to child. J. Med. Virol. 1994;44(4):415–421. doi: 10.1002/jmv.1890440419. [DOI] [PubMed] [Google Scholar]
- 53.Rodier C., Lapointe A., Coutlée F., Mayrand M.H., Dal Soglio D., Roger M., Trottier H. Juvenile respiratory papillomatosis: risk factors for severity. J. Med. Virol. 2013;85(8):1447–1458. doi: 10.1002/jmv.23615. [DOI] [PubMed] [Google Scholar]
- 54.He Y., Wu Y.M., Wang T., Song F., Wang Y., Zhu L. Perinatal outcomes of pregnant women with cervical intraepithelial neoplasia. Arch. Gynecol. Obstet. 2013;288(6):1237–1242. doi: 10.1007/s00404-013-2889-6. [DOI] [PubMed] [Google Scholar]
- 55.Boulenouar S., Weyn C., Van Noppen M., Moussa Ali M., Favre M., Delvenne P.O., Bex F., Noël A., Englert Y., Fontaine V. Effects of HPV-16 E5, E6 and E7 proteins on survival, adhesion, migration and invasion of trophoblastic cells. Carcinogenesis. 2010;31(3):473–480. doi: 10.1093/carcin/bgp281. [DOI] [PubMed] [Google Scholar]
- 56.Hermonat P.L., Han L., Wendel P.J., Quirk J.G., Stern S., Lowery C.L., Rechtin T.M. Human papillomavirus is more prevalent in first trimester spontaneously aborted products of conception compared to elective specimens. Virus Genes. 1997;14(1):13–17. doi: 10.1023/a:1007975005433. [DOI] [PubMed] [Google Scholar]
- 57.Srinivas S.K., Ma Y., Sammel M.D., Chou D., McGrath C., Parry S., Elovitz M.A. Placental inflammation and viral infection are implicated in second trimester pregnancy loss. Am. J. Obstet. Gynecol. 2006;195(3):797–802. doi: 10.1016/j.ajog.2006.05.049. [DOI] [PubMed] [Google Scholar]
- 58.Skoczyński M., Goździcka-Józefiak A., Kwaśniewska A. Prevalence of human papillomavirus in spontaneously aborted products of conception. Acta Obstet. Gynecol. Scand. 2011;90(12):1402–1405. doi: 10.1111/j.1600-0412.2011.01189.x. [DOI] [PubMed] [Google Scholar]
- 59.Gomez L.M., Ma Y., Ho C., Mcgrath C.M., Nelson D.B., Parry S. Placental infection with human papillomavirus is associated with spontaneous preterm delivery. Hum. Reprod. 2008;23(3):709–715. doi: 10.1093/humrep/dem404. [DOI] [PubMed] [Google Scholar]
- 60.Zuo Z., Goel S., Carter J.E. Association of cervical cytology and HPV DNA status during pregnancy with placental abnormalities and preterm birth. Am. J. Clin. Pathol. 2011;136(2):260–265. doi: 10.1309/AJCP93JMIUEKRPIW. [DOI] [PubMed] [Google Scholar]