Abstract
We report a case of nephrogenic syndrome of inappropriate antidiuresis caused by carbamazepine (CBZ). CBZ, an antiepileptic drug, is known to cause hyponatremia. The mechanism is generally considered to be inappropriate secretion of antidiuretic hormone, whereas an experimental study suggests a direct effect of CBZ on the kidney by stimulating vasopressin receptor. An 18-year-old male with atypical autism and epilepsy has been treated with CBZ and clobazam since age 9 and 10 years, respectively. At age 11, he was found to have asymptomatic hyponatremia. He had the habit of drinking tea approximately 3 L/day. The low plasma osmolality and high urine osmolality and sodium concentration in the presence of normal thyroid and adrenal function were compatible with syndrome of inappropriate excretion of antidiuretic hormone. His plasma vasopressin level, however, was undetectable. Urine cyclic AMP level was higher than expected from urine osmolality despite the suppressed plasma arginine vasopressin. With fluid restriction, hyponatremia improved. CBZ tapering begun later in the course maintained normal serum sodium concentrations with less strict water intake. This case demonstrates the direct effect of CBZ stimulating vasopressin receptor in the kidney leading to nephrogenic syndrome of inappropriate diuresis.
Keywords: Hyponatremia, Carbamazepine, Nephrogenic syndrome of inappropriate antidiuresis, Syndrome of inappropriate antidiuretic hormone secretion, Cyclic AMP
Introduction
Carbamazepine (CBZ) is an antiepileptic drug widely used. Hyponatremia is a well-known side effect of CBZ. The cause of hyponatremia is considered to be the stimulation of arginine vasopressin (AVP) from pituitary gland and subsequent water retention. We report a patient with hyponatremia who has been prescribed CBZ. He fulfilled the diagnostic criteria of syndrome of inappropriate antidiuretic hormone secretion (SIADH). His plasma AVP levels, however, were undetectable, and his urine cyclic AMP (cAMP) was higher than expected from urine osmolality suggesting that his hyponatremia was due to the stimulatory effect of CBZ on AVP receptor.
Case report
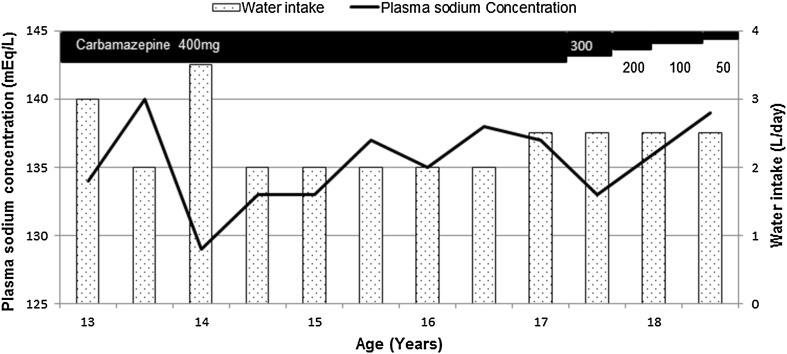
An 18-year-old male with epilepsy and speech delay has been prescribed CBZ and clobazam since age 9 and 10 years, respectively. He has been well until age 8, when he had an afebrile seizure, which recurred several times thereafter. He subsequently was diagnosed with atypical autism. At age 10 years, he had status epilepticus associated with influenza type A infection. At that time he developed epidural hematoma, which disappeared after 2 weeks. He has no neurological sequelae except for mild atrophy of frontal lobe. His seizure was controlled with CBZ 400 mg and clobazam 10 mg per day. At age 11 years, he was found to have hyponatremia (131 mEq/L) at a regular check-up. He had no symptoms or abnormal physical findings; blood pressure was normal, and edema or signs of dehydration was absent. His mother reported that he drank tea approximately 3 L/day. With fluid restriction serum sodium was increased to 138 mEq/L. At age 14 years, laboratory findings again showed hyponatremia of 133 mEq/L. His blood pressure was 99/63 mmHg. There was no edema or signs of dehydration. Plasma osmolality was 273 mOsm/kg, urine osmolality 458 mOsm/kg, urine sodium 110 mEq/L, blood urea nitrogen 9.0 mg/dL, serum creatinine 0.6 mg/dL, and serum uric acid 3.9 mg/dL. Thyroid function and serum cortisol were normal. Plasma renin activity, aldosterone, atrial natriuretic peptide, and brain natriuretic peptide were within normal limits. Mild atrophy of frontal lobe was found on magnetic resonance imaging of the brain with no change since age 10. These findings were compatible with SIADH. Plasma AVP levels, measured by double-antibody radioimmunoassay, were undetectable in the presence of hyponatremia on two occasions. His urine cAMP, measured by radioimmunoassay dextran coated charcoal method, was 1.0 µmol/L with urine osmolality 204 mOsm/kg, which was higher than expected value of approximately 0.5 µmol/L [1]. Urine cAMP/osmolality of 4.9 µmol/Osm was also higher than 3.0 ± 0.4 µmol/Osm of normal controls after water load as previously reported [1]. There is no family history of hyponatremia. We restricted his fluid intake to 2 L/day and his plasma sodium increased to within the normal range (Fig. 1). While he was on CBZ 400 mg/day, serum CBZ concentration remained within therapeutic range (4–12 µg/ml). At age 17, we started to taper CBZ since he had no seizure for 6 years, in parallel with less strict fluid restriction (2.5 L/day). When his serum CBZ concentration was 2.6 µg/ml, plasma sodium was 138 mEq/L and plasma AVP was detectable (0.5 pg/mL).
Fig. 1.
Plasma sodium concentration and water intake. Reciprocal changes in plasma sodium and water intake were observed during the course
Discussion
We report a case of hyponatremia in a patient prescribed CBZ. Low plasma osmolality, high urine osmolality and sodium, in the presence of undetectable plasma AVP were compatible with the diagnosis of nephrogenic syndrome of inappropriate antidiuresis (NSIAD).
It has been reported that hyponatremia is detected in 4.8–40% of patients receiving carbamazepine [2]. In addition, CBZ was reported to decrease the ability to excrete oral water load, with higher urine/plasma osmolality ratio and lower free water clearance [3]. Thus, CBZ has been even used for the treatment of diabetes insipidus in the past [4, 5]. Regarding CBZ-induced hyponatremia, several mechanisms have been suggested. Plasma AVP levels are generally elevated, indicating that CBZ stimulates the release of AVP from the pituitary gland. On the other hand, there were a few papers reporting low plasma AVP levels, suggesting that antidiuretic effect of CBZ is a direct one on renal tubules [4]. Tormey proposed that the mechanisms of CBZ-induced antidiuresis include an AVP-like action or an increase in the sensitivity of the AVP receptor based on reported data [6].
In 2005, Feldman reported two infants with chronic hyponatremia compatible with SIADH and with undetectable plasma AVP levels [7]. Gain-of-function mutation of vasopressin V2 receptor gene (AVPR2) was identified, and the disease was named NSIAD. The pathophysiology is constitutive activation of AVPR2 independent of ligand. Thirty-four cases of NSIAD with AVPR2 have been reported as of September 2017 [8]. The CBZ-induced hyponatremia in our case may also be explained by the activation of AVPR2.
The effect of CBZ on the kidney was investigated by Ana et al. in lithium-induced diabetes insipidus in rats [9]. In vivo studies showed that CBZ decreased urine volume and increased urine osmolality. In in vitro studies, CBZ increased water permeability and, therefore, water absorption in inner collecting ducts isolated from normal rats. Furthermore, the effect of CBZ was blocked by AVP receptor antagonist as well as by an inhibitor of cAMP-dependent protein kinase indicating the effect of CBZ was mediated by AVP2R-associated cAMP production. In normal subjects, a strong correlation has been reported to exist between urine osmolality and cAMP concentrations [1]. In addition, urine cAMP/osmolality was reported to be 3.0 ± 0.4 µmol/Osm by after water loading. In our patient, urine cAMP in relation to urine osmolality and cAMP/osmolality were higher than the reported values. Thus, the pathophysiology is the same as NSIAD with gain-of-function mutations of AVP2R. Urine cAMP has not previously examined in patients with CBZ-induced SIADH with suppressed AVP levels. This case, therefore, demonstrates for the first time the direct effect of CBZ on tubules via AVP2R-cAMP in clinical setting.
A subset of patients with SIADH of the so-called “type D” SIADH are known to exist. Type D is rare and characterized by minimal level of serum ADH with highly concentrated urine. NSIAD due to AVPR2 mutation and CBZ are thought to constitute type D SIADH. Other causes of NSIAD or “type D” SIADH may be uncovered if the pathophysiology of this condition becomes more recognized.
Polydipsia is thought to have contributed to the development of hyponatremia in our case. From around age 11, the patient had the habit of drinking tea 3 L/day. Fluid restriction improved hyponatremia even with continued administration of CBZ. As described above, patients on CBZ have a decreased ability to excrete water load and, therefore, at a risk of developing hyponatremia when given a large amount of water.
Risk factors other than polydipsia for CBZ-induced hyponatremia include old age [10], high serum CBZ levels [11], and concomitant medications affecting electrolyte balance such as hydrochlorothiazide [12] and levomepromazine [13]. In our case, serum CBZ level was within therapeutic rage, and clobazam, used along with CBZ, has not been associated with hyponatremia. Initially only water restriction was implemented which improved hyponatremia (Fig. 1). CBZ tapering was begun towards the end of follow-up period, which transiently decreased serum sodium concentration with water intake of 2.5 L/day. Further tapering of CBZ increased serum sodium to 138 mEq/L with the same water intake. Therefore, water restriction as well as CBZ tapering was thought to have contributed for the improvement of hyponatremia.
In conclusion, we reported a patient who developed hyponatremia due to CBZ administration in association with polydipsia. Suppressed plasma AVP level and high urine cAMP/osmolality demonstrated the cAMP-dependent action of CBZ via AVP2R on collecting ducts.
Compliance with ethical standards
Conflict of interest
The authors have declared that no conflict of interest exists.
Human and animal participants right
This article does not contain any studies with animals performed by any authors.
Informed consent
Informed consent was obtained from the patient and his parents in this case report.
References
- 1.Barash I, Ponda MP, Goldfarb DS, Skolnik EY. A pilot clinical study to evaluate changes in urine osmolality and urine cAMP in response to acute and chronic water loading in autosomal dominant polycystic kidney disease. Clin J Am Soc Nephrol. 2010;5:693–697. doi: 10.2215/CJN.04180609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Van Amelsvoort T, Bakshi R, Devaux CB, Schwabe S. Hyponatremia associated with carbamazepine and oxcarbazepine therapy: a review. Epilepisia. 1994;35:181–188. doi: 10.1111/j.1528-1157.1994.tb02930.x. [DOI] [PubMed] [Google Scholar]
- 3.Stephens WP, Coe JY, Baylis PH. Plasma arginine vasopressin concentrations and antidiuretic action of carbamazepine. Br Med J. 1978;1:1445–1447. doi: 10.1136/bmj.1.6125.1445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Meinders AE, Cejka V, Robertson GL. The antidiuretic action of carbamazepine in man. Clin Sci Mol Med. 1974;4:289–299. doi: 10.1042/cs0470289. [DOI] [PubMed] [Google Scholar]
- 5.Wales JK. Treatment of diabetes insipidus with carbamazepine. Lancet. 1975;306:948–951. doi: 10.1016/S0140-6736(75)90361-X. [DOI] [PubMed] [Google Scholar]
- 6.Tormey WP. Mechanisms of carbamazepine-induced antidiuresis. J Neuro Neurosurg Psychiatry. 1993;56:567. doi: 10.1136/jnnp.56.5.567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Feldman BJ, Rosenthal SM, Vargas GA, Fenwick RG, Huang EA, Matsuda-Abedini M, Lustig RH, Mathias RS, Portale AA, Miller WL, Gitelman SE. Nephrogenic syndrome of inappropriate antidiuresis. New Engl J Med. 2005;352:1884–1890. doi: 10.1056/NEJMoa042743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vandergheynst F, Brachet C, Heinrichs C, Decaux G. Long-term treatment of hyponatremic patients with nephrogenic syndrome of inappropriate antidiuresis: personal experience and review of published case reports. Nephron Clin Pract. 2012;120:c168–c172. doi: 10.1159/000338539. [DOI] [PubMed] [Google Scholar]
- 9.de Bragança AC, Moyses ZP, Magaldi AJ. Carbamazepine can induce kidney water absorption by increasing aquaporin 2 expression. Nephrol Dial Transpl. 2010;25:3840–3845. doi: 10.1093/ndt/gfq317. [DOI] [PubMed] [Google Scholar]
- 10.Kalff R, Houtkooper MA, Meyer JW, Goedhart DM, Augusteijn R, Meinardi H. Carbamazepine and serum sodium levels. Epilepsia. 1984;25:390–397. doi: 10.1111/j.1528-1157.1984.tb04205.x. [DOI] [PubMed] [Google Scholar]
- 11.Henry DA, Lawson DH, Reavey P, Renfrew S. Hyponatraemia during carbamazepine treatment. Br Med J. 1977;1:83–84. doi: 10.1136/bmj.1.6053.83-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ranta A, Wooten GF. Hyponatremia due to an additive effect of carbamazepine and thiazide diuretics. Epilepsia. 2004;45:879. doi: 10.1111/j.0013-9580.2004.00604.x. [DOI] [PubMed] [Google Scholar]
- 13.Matsumura M, Yamaguchi M, Sato T. Severe hyponatremia in a patient treated with levomepromazine and carbamazepine. Intern Med. 2001;40:459. doi: 10.2169/internalmedicine.40.459. [DOI] [PubMed] [Google Scholar]