Abstract
Introduction:
Integrated care programmes are increasingly being put in place to provide care to older people who live at home. Knowledge of how to further develop integrated care and how to transfer successful initiatives to other contexts is still limited. Therefore, a cross-European research project, called Sustainable Tailored Integrated Care for Older People in Europe (SUSTAIN), has been initiated with a twofold objective: 1. to collaborate with local stakeholders to support and monitor improvements to established integrated care initiatives for older people with multiple health and social care needs. Improvements focus on person-centredness, prevention orientation, safety and efficiency; 2. to make these improvements applicable and adaptable to other health and social care systems, and regions in Europe. This paper presents the overall structure and approach of the SUSTAIN project.
Methods:
SUSTAIN uses a multiple embedded case study design. In three phases, SUSTAIN partners: (i) conduct interviews and workshops with stakeholders from fourteen established integrated care initiatives to understand where they would prefer improvements to existing ways of working; (ii) collaborate with local stakeholders to support the design and implementation of improvement plans, evaluate implementation progress and outcomes per initiative, and carry out overarching analyses to compare the different initiatives, and; (iii) translate knowledge and experience to an online roadmap.
Discussion:
SUSTAIN aims to generate evidence on how to improve integrated care, and apply and transfer the knowledge gained to other health and social care systems, and regions. Lessons learned will be brought together in practical tools to inform and support policy-makers and decision-makers, as well as other stakeholders involved in integrated care, to manage and improve care for older people living at home.
Keywords: older people, integrated care, long-term care, implementation science, mixed methods, knowledge translation, European research
Introduction
Health and social care systems face the challenge of offering care and support to an increasing number of older people living at home [1]. This increase is partly due to an ageing population, but also governments in and outside Europe are pursuing agendas that seek to enable older people to participate in society and to live at home for as long as possible [2,3,4]. While a large proportion of older people are able to stay in their own homes, the prevalence of frailty, multimorbidity and disability increases with age, leading to a growing number of older people living in the community with multiple health and social care needs. These multiple needs may restrict social participation, and lead to reduced self-reliance and increased care dependence, which in turn may result in a higher utilisation of long-term care and support services [5,6,7,8].
Sustainable health and social care systems will need to be able to optimally support older people by addressing both their health and social care needs, while at the same time minimise service utilisation and expenditure. Integrated care is widely acknowledged to be a promising approach for meeting such challenges [9,10,11,12,13,14,15]. There are several definitions for the term ‘integrated care’ in place [16,17,18]. In this study, integrated care is defined as those initiatives that proactively seek to structure and coordinate care for older people in their own home environments, centred around their needs [12,13,14,19,20,21,22].
Numerous integrated care initiatives have been rolled out, in a wide range of settings and contexts, in and outside Europe [23,24,25,26], offering a rich and varied field of practical examples. Evaluations of these initiatives have established potential benefits of greater levels of service integration, but they have also highlighted limitations. For instance, evidence for the effectiveness of integrated care programmes for older people living at home remains inconsistent [14,27]. Also, knowledge of how to successfully implement and improve integrated care is still limited, as is knowledge of how to transfer these experiences to other contexts [28]. Furthermore, improvements to the current way of working in existing initiatives are considered necessary, to make them more person-centred, prevention-oriented, safe and efficient [24,27,29,30,31]. In addition, more insight into how to measure and evaluate (improvements in) integrated care programmes is needed to be able to capture outcomes and processes adequately and consistently across different programmes and evaluation studies.
The SUSTAIN research project
To take a step forward in the development of integrated care, the cross-European research project called ‘SUSTAIN’ has been initiated, which stands for ‘Sustainable Tailored Integrated Care for Older People in Europe’ (http://www.sustain-eu.org). The project is funded under Horizon 2020 – the Framework Programme for Research and Innovation (2014–2020) from the European Commission (EC). SUSTAIN’s objectives are twofold: 1. to support and monitor improvements to established integrated care initiatives for older people living at home with multiple health and social care needs, and in so doing move towards more person-centred, prevention-oriented, safe and efficient care; and 2. to contribute to the adoption and application of these improvements to other health and social care systems, and regions in Europe. SUSTAIN is a four-year research project (2015–2019) carried out by thirteen partners from nine European countries: Austria (n = 1 partner), Belgium (n = 1 partner), Estonia (n = 1 partner), Germany (n = 1 partner), Ireland (n = 1 partner), Norway (n = 1 partner), Spain (n = 1 partner), the Netherlands (n = 4 partners) and the United Kingdom (n = 2 partners). The project team consists of dissemination partners focusing on knowledge translation and dissemination, and research partners who focus on supporting and evaluating improvements to the integrated care initiatives. The dissemination partners are from Belgium, Ireland, the Netherlands and the United Kingdom, and the research partners are from Austria, Estonia, Germany, Norway, Spain, the Netherlands and the United Kingdom. The aim of this paper is to describe SUSTAIN’s overall structure and intended approach and activities to generate evidence on improving integrated care and to transfer obtained knowledge to other health and social care systems, and regions.
Methods
Design and setting
Using a multiple embedded case study design [32,33], data are being collected from fourteen established integrated care initiatives for older people in seven European countries; Austria, Estonia, Germany, Norway, Spain, the Netherlands and the United Kingdom. The initiatives were already operating within their local health and social care systems. Each initiative, also referred to as ‘site’, is treated as one case study in the research. The project focuses on older people because complexity of needs and, consequently, care delivery tend to increase with age with the result that a more coordinated approach to service delivery, as pursued in the project, is required. Prior to the start of the project, SUSTAIN research partners invited integrated care initiatives in their networks within their countries, that were motivated to improve their current practice, to participate in the SUSTAIN project. Most sites already had a longstanding partnership with one of the SUSTAIN research partners. Criteria for including them in the study were defined by SUSTAIN research partners and drawn from the principles of the Chronic Care Model and related models [12,14,20,22,28,34]. Accordingly, initiatives should:
Be willing and committed to improve their current practice by working towards more person-centred, prevention-oriented, safe and efficient care, which, in line with the EC’s stipulations, are SUSTAIN’s four key domains (see Table 1 for definitions);
Focus on people aged 65 years and older, who live in their own homes and who have multiple health and social care needs;
Support people to stay in their own homes (or local environments) for as long as possible;
Address older people’s multiple needs, in other words, they should not be single disease oriented;
Involve professionals from multiple health and social care disciplines working in multidisciplinary teams (e.g. nurses, social workers, pharmacists, dieticians, general practitioners);
Be established, i.e. preferably operational for at least two years;
Cover one geographical area or local site;
Be mandated by one organisation that represents the initiative and that facilitates collaboration with SUSTAIN research partners.
Table 1.
Definitions of SUSTAIN’s key domains.
| Person-centredness | Involve older people and their informal carers in decision-making and planning their care process in order to tailor the delivery of care and support as much as possible to individual needs, preferences and capabilities, taking into account socio-demographic factors, cultural backgrounds and gender [35,36]. |
| Prevention orientation | Preserve and promote the health and wellbeing of older people with multiple needs by preventing deterioration in existing conditions, and providing active support to help them to maintain and regain as much autonomy, independence and resilience as possible, and to make optimal use of individual resources [37]. |
| Safety | Prevent adverse outcomes of care (e.g. drug related problems, unnecessary hospitalisations and admissions in long-term care institutions), decrease preventable decline in health status (e.g. falls) and address treatment adherence [38]. |
| Efficiency | Affordability of interventions and effective use of infrastructure, resources for sustainability (e.g. hours of service and labour allocated to recipients) and equipment and technology (e.g. IT), and the extent to which interventions may be able to shift activity from acute services to primary care services, improve alignment between the care professionals involved and reduce waste in healthcare spending (e.g. unnecessary readmissions within 30 days) [39,40]. |
The fourteen initiatives selected according to these criteria show great diversity in the type of care services provided (see Table 2). Their focus ranges from proactive primary care for frail older people and care for older people being discharged from hospital, to nursing care for frail older people, care for people with dementia, and palliative care. More detailed information about the initiatives can be found in an EU report that we wrote about the fourteen initiatives [41].
Table 2.
Characteristics of fourteen integrated care initiatives participating in the SUSTAIN project.
| Country | Region | Integrated care initiative | Type of care services |
|---|---|---|---|
| Austria | Vienna | Gerontopsychiatric Centre | Dementia care |
| Styria | Coordinated Palliative Care | Palliative care | |
| Estonia | Ida-Viru | Alutaguse Care Centre | Home nursing and rehabilitative care |
| Tallinn | Medendi | Home nursing | |
| Germany | Uckermark | KV RegioMed Zentrum Templin | Rehabilitative care |
| Berlin Marzahn-Hellersdorf | Careworks Berlin | Home nursing and rehabilitative care | |
| Norway | Surnadal | Surnadal Holistic Patient Care at Home | Home nursing and rehabilitative care |
| Søndre Nordstrand in Oslo | Søndre Nordstrand Everyday Mastery Team | Rehabilitative care and mastery of activities of daily living | |
| Spain | Osona | Severe Chronic Patients/Advanced chronic disease/Geriatrics Osona | Proactive primary and intermediate care |
| Sabadell | Social and health care integration Sabadell | Proactive primary care | |
| The Netherlands | West-Friesland | Geriatric Care Model | Proactive primary care |
| Walcheren | Walcheren Integrated Care Model | Proactive primary care | |
| United Kingdom | Kent | Over 75 Service | Proactive primary care |
| Kent | Swale Home First | Hospital discharge planning | |
Procedures and measures
The project is divided into three interrelated phases, namely: the preparation phase (phase 1), the implementation and evaluation phase (phase 2), and the knowledge translation phase (phase 3) (see Figure 1). At the time of writing, the project is in phase 2.
Figure 1.
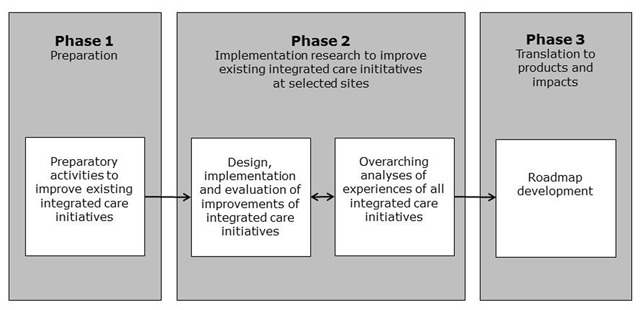
Three interrelated project phases of the SUSTAIN project.
Phase 1: Preparation phase
Between autumn 2015 and winter 2016, SUSTAIN research partners established working relationships with the fourteen participating initiatives, and identified relevant local stakeholders related to the initiative (i.e. managers, health and social care professionals, representatives of older people and informal carers, local policy officers). Furthermore, they carried out baseline assessments of each initiative’s principal characteristics and also worked with local stakeholders to identify areas of current practice in the initiative, which might be subject to improvement (e.g. collaboration between formal and informal care providers, involvement of older people in care processes). For the purpose of the baseline assessments, interviews were conducted using a semi-structured interview guide, covering the context and characteristics of the site, stakeholders’ interpretation of SUSTAIN’s four key domains (i.e. person-centredness, prevention-orientation, safety and efficiency) and each site’s performance in relation to them, facilitators and barriers to integration, and potential areas for improvement. At each site, interviews were conducted with the following four study participants: one older person receiving care services from the initiative (user), one informal caregiver, one health or social care professional involved in the initiative and one manager of the initiative. All SUSTAIN research partners used the same interview schedules for their interviews. The interviews were audiotaped with interviewees’ permission.
Interview transcripts from each site were thematically analysed using a uniform, structured template of analysis, generated by structured discussion among research partners. Interview findings were used as inputs for workshops with key stakeholders related to the initiative (i.e. managers, health and social care professionals, representatives of older people and informal carers, local policy officers) at each site. The purpose of the workshops was to discuss outcomes of the baseline assessments and enable sites to determine local improvement priorities.
Phase 2: Implementation research to improve existing integrated care initiatives at selected sites
Based on the outcomes of phase 1, local steering groups were set up in spring 2016. Steering groups consists of stakeholders who participated in the workshops together with additional local stakeholders considered relevant to the initiative. These steering groups have been designated to design and implement improvement plans, that is, sets of improvements that apply to local, site-specific priorities and address SUSTAIN’s key domains (e.g. offering training to staff to promote older people’s involvement in care planning and decision-making). Each steering group has agreed to implement their plans over the 18-month period from autumn 2016 to spring 2018.
The implementation of improvement plans and the evaluation of implementation progress and outcomes per initiative are guided by the Evidence Integration Triangle model (see Figure 2) [42]. The Evidence Integration Triangle model, which has its origins in implementation science, supports the effective implementation of theoretical models and scientific evidence in daily practice by tailoring evidence to the multi-level context (i.e. the historical, political, economic, social, environmental, and cultural settings in which a service/programme is being implemented) in which local stakeholders (e.g. managers, health and social care professionals, representatives of older people and informal carers, local policy officers) operate. The Evidence Integration Triangle model thus corresponds well with the objectives of the SUSTAIN project. There are three main components to the Evidence Integration Triangle model:
Figure 2.

The Evidence Integration Triangle model (adapted) [42].
The intervention, which in this case are the improvement plans of the different sites to work towards more person-centred, prevention-oriented, safe and efficient care. The plans include specific areas for improvement (e.g. information exchange between health and social care professionals, assessment of older people’s needs, involvement of older people in the care process) together with actions required to realise such improvements (e.g. creating a shared platform for data sharing, designing a common multidimensional needs assessment tool, training of staff to empower older people). Each site designs and implements its own improvement plan and, consequently, interventions differ across sites;
The participatory implementation process, which is the collaboration of SUSTAIN research partners with local stakeholders. Regular meetings between SUSTAIN research partners and steering groups of local stakeholders will take place to design and implement the improvement plans. The research partners will also continue to provide support to the local steering groups by contributing improvement support from theoretical models, scientific evidence and best practices. Following the principles of the Evidence Integration Triangle model, SUSTAIN research partners will further conduct mid-course site-specific analyses so as to share emerging interim site-specific feedback to the steering group about outcomes and progress during the implementation process. In addition, overarching analyses will be undertaken, first, around month 12 of the improvement plans’ implementation. And second, shortly after the end of the 18-month implementation period to compare outcomes and progress at each site and communicate emerging themes to all of them. This will support local stakeholders to further refine their improvement projects and, thereby, foster rapid learning cycles at and between sites [42];
Practical measures, a set of qualitative and quantitative data collection tools (see Table 3), for evaluating how the sets of improvements for each of the fourteen initiatives have impacted on SUSTAIN’s key domains. The tools will further allow us to evaluate the implementation progress by focussing on perceptions and experiences of professionals, managers and the steering group of the fourteen initiatives, and on progress in implementing the different components of the improvement plans, including factors that were perceived to facilitate and impede progress. Data will be collected at agreed and specified times during the 18-month implementation period, using the same procedures and tools for all initiatives. In addition to a core set of data collection tools applied in all initiatives, sites are being encouraged to select site-specific tools tailored to their site-specific context and improvement priorities. All data collection tools developed by SUSTAIN research partners are prepared in English and are then translated into the sites’ national languages. Regular meetings and teleconferences take place between research partners to standardise methods of data collection in each country.
Table 3.
Practical measures for monitoring outcomes and progress of the implementation of the improvement plans.
| Item | Data collection tool | Short description |
|---|---|---|
|
DEMOGRAPHIC INFORMATION | ||
| Socio-demographics of older people (users) | Demographic data sheet – older people, administered to older people | Survey developed by SUSTAIN researchers requesting information on age, gender, education, marital status, living situation and self-reported medical conditions |
| Socio-demographics of informal carers | Demographic data sheet – carers, administered to informal carers | Survey developed by SUSTAIN researchers requesting information on age, gender, education, marital status, relationship and distance to older person (user), paid work and caregiving activities |
| Socio-demographics of professionals | Demographic data sheet – professionals, administered to professionals | Survey developed by SUSTAIN researchers requesting information on age, gender, nationality and occupation |
| Socio-demographics of managers | Demographic data sheet – managers, administered to managers | Survey developed by SUSTAIN researchers requesting information on age, gender, nationality and occupation |
|
OUTCOMES | ||
| Person-centredness | ||
| Patient perceptions of quality and coordination of care and support | The Person Centred Coordinated Care Experience Questionnaire (P3CEQ) [43], administered to older people | Survey measuring older people’s experience and understanding of the care and support they have received from health and social care services |
| Proportion of older people with a needs assessment | Care plan template (in case sites do not work with care plans, information will be retrieved from clinical notes or other documentation) | Template developed by SUSTAIN researchers for predetermined content analysis of care plans of older people |
| Proportion of care plans actioned (i.e. defined activities in care plan actually implemented) | ||
| Proportion of care plans shared across different professionals and/or organisations | ||
| Proportion of informal carers with a needs assessment and/or care plan | ||
| Perception and experiences of older people, informal carers, professionals and managers with person-centredness | Semi-structured interviews and focus group interviews with older people, informal carers, professionals and managers | Interview and focus group schedules developed by SUSTAIN researchers including interview items on perception and experiences with receiving person-centred care |
| Prevention orientation | ||
| Perceived control in care and support of older people | Perceived Control in Health Care (PCHC) [37], administered to older people | Survey addressing older people’s perceived own abilities to organise professional care and to take care of themselves in their own homes, and perceived support from the social network |
| Proportion of older people receiving a medication review | Care plan template (in case sites do not work with care plans, information will be retrieved from clinical notes or other documentation) | Template developed by SUSTAIN researchers for predetermined content analysis of care plans of older people |
| Proportion of older people receiving advice on medication adherence | ||
| Proportion of older people receiving advice on self-management and maintaining independence | ||
| Perception and experiences of older people, informal carers, professionals and managers with prevention | Semi-structured interviews and focus group interviews with older people, informal carers, professionals and managers | Interview and focus group schedules developed by SUSTAIN researchers including interview items on perception and experiences with receiving prevention-oriented care |
| Safety | ||
| Proportion of older people receiving safety advice | Care plan template (in case sites do not work with care plans, information will be retrieved from clinical notes or other documentation) | Template developed by SUSTAIN researchers for predetermined content analysis of care plans of older people |
| Proportion of older people with falls recorded in the care plan | ||
| Perception of older people, informal carers, professionals and managers with safety | Semi-structured interviews and focus group interviews with older people, informal carers, professionals and managers | Interview and focus group schedules developed by SUSTAIN researchers including interview items on perception and experiences with receiving safe care, and safety consciousness |
| Efficiency | ||
| Number of emergency hospital admissions of older people | Care plan template (in case sites do not work with care plans, information will be retrieved from clinical notes or other documentation); template to register staff hours and costs | Template developed by SUSTAIN researchers for predetermined content analysis of care plans of older people; template developed by SUSTAIN researchers to collect data on costs and the number of staff hours from local services, organisations or registries |
| Length of stay per emergency admission of older people | ||
| Number of hospital readmissions of older people | ||
| Number of staff hours dedicated to improvement project | ||
| Costs related to equipment and technology for improvement project | ||
| Perception of older people, informal carers, professionals and managers with efficiency | Semi-structured interviews and focus group interviews with older people, informal carers, professionals and managers | Interview and focus group schedules developed by SUSTAIN researchers including interview items on perception and experiences with receiving efficient care, and finances |
|
IMPLEMENTATION PROGRESS | ||
| Team coherence of improvement team (professionals) | Team Climate Inventory – short version (TCI-14) [44,45], administered to professionals | Survey measuring vision, participative safety, task orientation and experienced support for innovation of the improvement team |
| Perception and experiences of professionals | Focus group interviews with professionals and minutes from steering group meetings | Focus group schedule developed by SUSTAIN researchers including interview items on experienced factors facilitating and impeding outcomes and implementation progress |
| Minutes cover progress, issues and contextual issues impacting on outcomes and implementation progress | ||
| Perception and experiences of managers | Semi-structured interviews with managers and minutes from steering group meetings | Interview schedule developed by SUSTAIN researchers including interview items on experienced factors facilitating and impeding outcomes and implementation progress |
| Minutes cover progress, issues and contextual issues impacting on outcomes and implementation progress | ||
More detailed information about how the Evidence Integration Triangle model is applied in the SUSTAIN project will be described elsewhere [paper in preparation].
Data analysis: Data are centrally managed in a secure online database, which is accessible to SUSTAIN research partners. Strict guidelines for data entry have been developed and are shared across research partners. For each site, quantitative and qualitative data analyses will take place to monitor outcomes and progress at the different integrated care sites. Qualitative data will be analysed thematically, quantitative data will be analysed using statistical methods. The coupling of qualitative with quantitative elements is the approach of choice for evaluating complex community-based interventions which are context bound and noted for their differences in application and implementation [14,46,47]. Uniform templates for analysis of each data source are generated through a discussion among research partners. As per the Evidence Integration Triangle model, research partners will conduct site-specific analyses during (month 12; autumn 2017) and at the end (month 18; spring 2018) of the 18-month implementation period to give the local steering groups insight into their progress, and provide them with starting-points for follow up action. In addition, overarching analyses will be undertaken around month 12 and shortly after the end of the 18-month implementation period, in which data from the different sites will be compared and integrated to identify recurring patterns in the implementation of the tailored sets of improvements. In order to enable comparison, uniform procedures for data analysis are being developed. In the overarching analyses, we will follow the principles of the case study design [32]. There will be three steps in our analyses: 1. all data sources will be analysed separately; 2. data will be reduced to a series of thematic statements for each data source; and 3. these site analyses will then undergo a process of pattern-matching across the data from all sites using the identified actions in the improvement plans and SUSTAIN’s propositions (research questions) that have been formulated a priori: I. which actions in the improvement plans are able to improve person-centredness, prevention-orientation, safety and efficiency of care?; II. which actions work for whom, in what context?; III. what are possible explanations for (not) succeeding in improving integrated care?; and IV. what is necessary to guarantee transferability and applicability of actions across the EU for improvement? By comparing outcomes, barriers, facilitators, and experiences, as well as taking into account the characteristics of the study participants and initiatives, we hope to be able to explore how outcomes and implementation progress at the different sites relate to their particular contextual factors and characteristics. In addition to the results of the site-specific analyses, those of the overarching analyses will also be communicated to the different sites so that they can learn from the experiences at the other sites and, where potentially relevant, apply lessons learned to their own context. Comparing and integrating data from the different sites will also support us to ascertain what works for whom, in what context and with what outcomes. As such, we intend to generate EU evidence on improvements to integrated care and their adoption and application to other European health and social care systems, and regions.
Phase 3: Translation to products and impacts
SUSTAIN dissemination partners will merge and translate all knowledge and experiences obtained in SUSTAIN to different products for policy-makers and decision-makers from different types of organisations tasked with designing, establishing and maintaining systems of integrated care that focus on older people with complex needs (e.g. national or regional governments, care delivery organisations, and representative organisations of older people and informal carers), during and after the end of the implementation period (spring 2018). This will include the development of an online roadmap, which is a set of instructions, guidelines and proposed actions that provides a step-by-step guide for improving integrated care. In addition, a toolbox will be developed which will be embedded within the roadmap, consisting of a collection of tools (e.g. tool to evaluate person-centredness, tool to evaluate experiences of professionals and managers), lessons learned (e.g. potential solutions for certain implementation issues), scientific evidence and good practices (e.g. actions that will enhance person-centredness), to support the process of improving integrated care. The rationale for developing a roadmap and toolbox is to support the flow of theory, evidence and experiences obtained and observed during the SUSTAIN project into practice. As such, the roadmap and toolbox aim to facilitate the implementation of the tailored sets of improvements at the fourteen sites during the SUSTAIN project, and to facilitate improvements to the way of working for other integrated care sites in Europe after the SUSTAIN project.
Ethics statement
Ethical approval has been granted by the ethical review committees of Estonia, Spain and the United Kingdom. In Austria, Germany, Norway and the Netherlands, research activities were exempt from the need for ethics committee review as allowed under national standards and regulations. Prior to data collection, informed consent will be obtained for all study participants.
Discussion
This paper has outlined the overall structure and approach of the SUSTAIN project; a European project designed to improve the current ways of working in fourteen existing integrated care initiatives for older people living at home with multiple health and social care needs.
Many integrated care initiatives for older people with multiple health and social care needs have been introduced in European health systems in a diversity of contexts. These initiatives offer a rich and varied field of practical examples, as described for example in European-wide initiatives including INTERLINKS, the ICARE4EU project and the European Innovation Partnership on Active and Healthy Ageing (EIP-AHA) [48,49,50]. However, there is still discussion on how to measure and evaluate integrated care. This leads to practices being evaluated in different ways, which in turn complicates international comparisons. In SUSTAIN we are not evaluating integrated care programmes as a whole as previous studies have done. Rather we focus on how to identify and implement specific practical improvements to established initiatives based on previous evidence and their experiences with implementation of integrated care to date. We believe SUSTAIN can make important contributions to the research field, especially by contributing to European-wide sharing of evidence and improvement methods by employing uniform procedures for data collection and analysis. As such, we will be able to compare different initiatives across different settings through overarching analyses, thereby encouraging an understanding of generic and contextual factors affecting outcomes and progress of implementation.
In addition to responding to methodological challenges in the area of evaluating integrated care, SUSTAIN further aims to respond to challenges related to knowledge transfer. The translation of project findings and their application into daily practice is fraught with conceptual and operational difficulties. Firstly, scientific evidence is usually developed in isolation from daily practice. As a result, it often fits uncomfortably in the settings and populations where it is intended to be applied, and as such sustainable implementation is scarce. The SUSTAIN project aims to respond to this challenge by taking an action-oriented approach based on the Evidence Integration Triangle model [42], in which local stakeholders and research partners co-design and implement transformative changes. By so doing, the changes implemented are expected to be better tailored to the stakeholders’ context, which in turn may reinforce their motivation to improve current practice and establish sustainable change. Secondly, the rolling-out of the research findings to other health and social care systems, and regions is often limited due to difficulties in translating context-specific knowledge and experience to more generalisable recommendations. As a methodological framework, the Evidence Integration Triangle model provides a consistent approach that, when applied across multiple contexts, may be able to produce generalisable results to make improvements applicable and adaptable to other health and social care systems, and regions.
Besides the opportunities offered by the SUSTAIN project, it should also be noted that our approach poses a challenge to SUSTAIN research partners. Indeed, they will have a dual role during the design and implementation of the tailored sets of improvements in the integrated care initiatives. On the one hand, they are scientific researchers monitoring and evaluating outcomes and progress at the sites. On the other hand, they are facilitators collaborating with local stakeholders by organising meetings, bringing local stakeholders together, and supporting the design and implementation of plans to improve current services. It will be important for SUSTAIN research partners to clearly adjust to these roles and to avoid inappropriately influencing decisions taken by local stakeholders. Firstly because the improvement projects should reflect the preferences of local stakeholders at the sites to encourage the success and sustainability of the improvement projects; and secondly, because lessons learned should be applicable for other contexts not involved in the SUSTAIN project.
A number of other projects aside from SUSTAIN aim to provide guidance to a broader implementation and scaling up of good practices in integrated care across European regions, including SELFIE, ACT@Scale and JA-CHRODIS [51,52,53]. Although each project has its own unique approach, perspective and/or target group, it will be important for these projects to look for opportunities in achieving synergy. Combining each research project’s strengths and perspectives may result in for instance a more comprehensive evidence base or greater consensus on how to evaluate integrated care, upon which we will be able to provide meaningful recommendations to policy-makers and decision-makers and share what can be learned from these European-wide projects.
In conclusion, the SUSTAIN project intends to generate valuable evidence on improving integrated care for older people, and to transfer this knowledge within the SUSTAIN programme and to other regions and health and social care systems in Europe and beyond. By translating lessons learned to products targeted at policy-makers and decision-makers from different types of organisations, we aim to inform and support those managing and improving care for older people with multiple health and care needs.
Acknowledgements
The SUSTAIN project is funded under Horizon 2020 – the Framework Programme for Research and Innovation (2014–2020) from the European Commission under grant agreement No. 634144. The content of this article reflects only the SUSTAIN consortium members’ views. The European Union is not liable for any use that may be made of the information contained herein.
Reviewers
Fenna RM Leijten, MSc, PhD, Erasmus School of Health Policy & Management, Erasmus University Rotterdam, The Netherlands.
René Melis, Assistant professor geriatric epidemiology, Radboud university medical center, Nijmegen, The Netherlands.
Verena Struckmann, Researcher, Department of Health Care Management, WHO Collaborating Centre for Health Systems Research and Management, TECHNISCHE UNIVERSITÄT BERLIN, Germany.
One anonymous reviewers.
Competing Interests
One of the authors of this article, Viktoria Stein, is working for the International Foundation for Integrated Care, which supports the journal publishing this paper.
Author Information
This paper was published on behalf of the SUSTAIN consortium. People that are or were member of the SUSTAIN consortium when this manuscript was written, are:
Research partners: Maria Marta Arcas Ferre, Eliva Atieno Ambugo, Caroline Baan, Jenny Billings, Gabriela Barbaglia, Simone de Bruin, Carme Carrion, Laia Domingo, Reelika Ermel, Mireia Espallargues Carreras, Erica Gadsby, Christina Häusler, Terje Hagen, Henrik Hoffmann, Kathrine Hofgaard Vaage, Daniëlle Jansen, Kai Leichsenring, Manon Lette, Julie MacInnes, Lina Masana, Eneli Mikko, Mirella Minkman, Peter Müller, Henk Nies, Ulla-Karin Nurm, Giel Nijpels, Konrad Obermann, Gerli Paat-Ahi, Jillian Reynolds, Mari Rull, Georg Ruppe, Sophia Schlette, Riina Sikkut, Monique Spierenburg, Annerieke Stoop, Esther de Weger, Paulina Wosko and Nick Zonneveld.
Knowledge brokering and transfer partners: Borja Arrue, Jeni Bremner, Michele Calabro’, Marie Curran, Sandra Degelsegger, Nick Goodwin, Anne Hendry, Mudi Kadu, Usman Khan, Maggie Langins, Henriikka Laurola, Maude Luherne, Fiona Lyne, Federica Margheri, Nhu Tram, David Smith, Viktoria Stein and Gerald Wistow.
References
- 1.National Institutes of Health/World Health Organization. Global health and aging. NIH publication no 11-7737. 2011. [cited 2016 October 7]. Available from: http://www.who.int/ageing/publications/global_health.pdf.
- 2.Commission of the European Communities. Regions 2020: An assessment of future challenges for EU regions. 2008. [cited 2016 October 7]. Available from: http://ec.europa.eu/regional_policy/sources/docoffic/working/regions2020/pdf/regions2020_en.pdf.
- 3.Ricciardi, W, Specchia, ML and Marino, M. Health of the elderlies and healthy ageing: Challenge for Europe. Studies in Health Technology and Informatics, 2014; 203: 1–9. DOI: 10.3233/978-1-61499-425-1-1 [DOI] [PubMed] [Google Scholar]
- 4.OECD. Health reform: Meeting the challenge of ageing and multiple morbidities. 2011. [cited 2016 October 7]. Available from: http://www.oecd-ilibrary.org/docserver/download/8111171e.pdf?expires=1493716006&id=id&accname=ocid49027884&checksum=255577E73173C96A9607DFAA81932937.
- 5.Fried, LP, Tangen, CM, Walston, J, Newman, AB, Hirsch, C, Gottdiener, J, Seeman, T, Tracy, R, Kop, WJ, Burke, G and McBurnie, MA. Frailty in older adults evidence for a phenotype. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences, 2001; 56(3): M146–M157. DOI: 10.1093/gerona/56.3.M146 [DOI] [PubMed] [Google Scholar]
- 6.Markle-Reid, M and Browne, G. Conceptualizations of frailty in relation to older adults. Journal of advanced nursing, 2003; 44(1): 58–68. DOI: 10.1046/j.1365-2648.2003.02767.x [DOI] [PubMed] [Google Scholar]
- 7.Fried, LP, Ferrucci, L, Darer, J, Williamson, JD and Anderson, G. Untangling the concepts of disability, frailty, and comorbidity: Implications for improved targeting and care. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences, 2004; 59(3): M255–M263. DOI: 10.1093/gerona/59.3.M255 [DOI] [PubMed] [Google Scholar]
- 8.Metzelthin, SF, van Rossum, E, de Witte, LP, Ambergen, AW, Hobma, SO, Sipers, W and Kempen, GIJM. Effectiveness of interdisciplinary primary care approach to reduce disability in community dwelling frail older people: Cluster randomised controlled trial. British Medical Journal, 2013; 347: f5264 DOI: 10.1136/bmj.f5264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Berwick, DM, Nolan, TW and Whittington, J. The Triple Aim: Care, Health, And Cost. Health Affairs 2008; 27(3): 759–769. DOI: 10.1377/hlthaff.27.3.759 [DOI] [PubMed] [Google Scholar]
- 10.Gress, S, Baan, CA, Calnan, M, Dedeu, T, Groenewegen, P, Howson, H, Maroy, L, Nolte, E, Redaelli, M, Saarelma, O, Schmacke, N, Schumacher, K, van Lente, EJ and Vrijhoef, B. Co-ordination and management of chronic conditions in Europe: The role of primary care – position paper of the European Forum for Primary Care. Quality in Primary Care, 2009; 17(1): 75–86. [PubMed] [Google Scholar]
- 11.Mattke, S, Seid, M and Ma, S. Evidence for the effect of disease management: Is $1 billion a year a good investment? American Journal of Managed Care, 2007; 13(12): 670–676. [PubMed] [Google Scholar]
- 12.Wagner, EH, Bennett, SM, Austin, BT, Greene, SM, Schaefer, JK and Vonkorff, M. Finding common ground: Patient-centeredness and evidence-based chronic illness care. Journal of Alternative and Complementary Medicine, 2005; 11 Suppl 1: S7–15. DOI: 10.1089/acm.2005.11.s-7 [DOI] [PubMed] [Google Scholar]
- 13.Boult, C, Green, AF, Boult, LB, Pacala, JT, Snyder, C and Leff, B. Successful models of comprehensive care for older adults with chronic conditions: Evidence for the Institute of Medicine’s “retooling for an aging America” report. Journal of the American Geriatrics Society, 2009; 57(12): 2328–2337. DOI: 10.1111/j.1532-5415.2009.02571.x [DOI] [PubMed] [Google Scholar]
- 14.De Bruin, SR, Versnel, N, Lemmens, LC, Molema, CCM, Schellevis, FG, Nijpels, G and Baan, CA. Comprehensive care programs for patients with multiple chronic conditions: A systematic literature review. Health Policy, 2012; 107(2–3): 108–145. DOI: 10.1016/j.healthpol.2012.06.006 [DOI] [PubMed] [Google Scholar]
- 15.Hopman, P, de Bruin, SR, Forjaz, MJ, Rodriguez-Blazquez, C, Tonnara, G, Lemmens, LC, Onder, G, Baan, CA and Rijken, M. Effectiveness of comprehensive care programs for patients with multiple chronic conditions or frailty: A systematic literature review. Health Policy, 2016; 120(7): 818–832. DOI: 10.1016/j.healthpol.2016.04.002 [DOI] [PubMed] [Google Scholar]
- 16.van Raak, A, Mur-Veeman, I, Hardy, B, Steenbergen, M and Paulus, A (eds.). Integrated care in Europe: Description and comparison of integrated care in six EU countries Maarssen: Elsevier; 2003. [Google Scholar]
- 17.Goodwin, N, Stein, V and Amelung, V. What Is Integrated Care? In: Amelung V, Stein V, Goodwin N, Balicer R, Nolte E and Suter E, (eds.) Handbook Integrated Care. Cham: Springer International Publishing; 2017. p. 3–23. DOI: 10.1007/978-3-319-56103-5_1 [DOI] [Google Scholar]
- 18.World Health Organization, Health Services Delivery Programme and Division of Health Systems and Public Health. Roadmap. Strengthening people-centred health systems in the WHO European region: A framework for action towards coordinated integrated health services delivery (CIHSD). 2013. [Google Scholar]
- 19.Barr, VJ, Robinson, S, Marin-Link, B, Underhill, L, Dotts, A, Ravensdale, D and Salivaras, S. The expanded Chronic Care Model: An integration of concepts and strategies from population health promotion and the Chronic Care Model. Hospital Quarterly, 2003; 7(1): 73–82. DOI: 10.12927/hcq.2003.16763 [DOI] [PubMed] [Google Scholar]
- 20.Epping-Jordan, JE, Pruitt, SD, Bengoa, R and Wagner, EH. Improving the quality of health care for chronic conditions. Quality and Safety in Health Care, 2004; 13(4): 299–305. DOI: 10.1136/qshc.2004.010744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Raleigh, V, Bardsley, M, Smith, P, Wistow, G, Wittenberg, R, Erens, B and Mays, N. Integrated care and support pioneers: Indicators for measuring the quality of integrated care 2014, Policy Innovation Research Unit (PIRU). [Google Scholar]
- 22.Minkman, MMN. Developing integrated care: Towards a development model for integrated care 2012, Kluwer. [Google Scholar]
- 23.Van der Heide, I, Snoeijs, S, Melchiorre, MG, Quattrini, S, Boerma, W, Schellevis, F and Rijken, M. Innovating care for people with multiple chronic conditions in Europe: An overview 2015, Nivel: Utrecht. [Google Scholar]
- 24.Noordman, J, Van der Heide, I, Hopman, P, Schellevis, F and Rijken, M. Innovative health care approaches for patients with multi-morbidity in Europe. 2015. [Google Scholar]
- 25.Kodner, DL and Kyriacou, CK. Fully integrated care for frail elderly: Two American models. International Journal of Integrated Care 2000; 1: e08 DOI: 10.5334/ijic.11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hébert, R, Durand, PJ, Dubuc, N and Tourigny, A. PRISMA: A new model of integrated service delivery for the frail older people in Canada. International journal of integrated care, 2003; 3: e08 DOI: 10.5334/ijic.73 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hoogendijk, EO. How effective is integrated care for community-dwelling frail older people? The case of the Netherlands. Age and Ageing, 2016; 45: 587–590. DOI: 10.1093/ageing/afw081 [DOI] [PubMed] [Google Scholar]
- 28.Leichsenring, K, Billings, J and Nies, H (eds). Long-term care in Europe – improving policy and practice Basingstoke: Palgrave Macmillan; 2013. DOI: 10.1057/9781137032348 [DOI] [Google Scholar]
- 29.Onder, G, Palmer, K, Navickas, R, Jurevičiene, E, Mammarella, F, Strandzheva, M, Mannucci, P, Pecorelli, S and Marengoni, A. Time to face the challenge of multimorbidity. A European perspective from the joint action on chronic diseases and promoting healthy ageing across the life cycle (JA-CHRODIS). European Journal of Internal Medicine, 2015; 26(3): 157–159. DOI: 10.1016/j.ejim.2015.02.020 [DOI] [PubMed] [Google Scholar]
- 30.Banerjee, S. Multimorbidity – older adults need health care that can count past one. The Lancet; 385(9968): 587–589. DOI: 10.1016/S0140-6736(14)61596-8 [DOI] [PubMed] [Google Scholar]
- 31.Blom, J, Den Elzen, W, Vn Houwelingen, AH, Heijmans, M, Stijnen, T, Van den Hout, W and Gussekloo, J. Effectiveness and cost-effectiveness of a proactive, goal-oriented, integrated care model in general practice for older people. A cluster randomised controlled trial: Integrated Systematic Care for older People—the ISCOPE study. Age and Ageing, 2016; 45(1): 30–41. DOI: 10.1093/ageing/afv174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yin, RK. Case study research: Design and methods Sage Publications Inc; 2013. [Google Scholar]
- 33.Van der Eerden, M, Csikos, A, Busa, C, Hughes, S, Radbruch, L, Menten, J, Hasselaar, J and Groot, M. Experiences of patients, family and professional caregivers with Integrated Palliative Care in Europe: Protocol for an international, multicenter, prospective, mixed method study. BMC Palliative Care, 2014; 13(1): 52 DOI: 10.1186/1472-684X-13-52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Billings, JR and Leichsenring, K (eds.). Integrating health and social services for older persons: Evidence from nine European countries Public Policy and Social Welfare Aldershot: Ashgate; 2005. [Google Scholar]
- 35.Coulter, A, Roberts, S and Dixon, A. Delivering better services for people with long-term conditions: Building the house of care. 2013. [Google Scholar]
- 36.Lloyd, J and Wait, S. Integrated care: A guide for policymakers 2006, Alliance for Health & the Future. [Google Scholar]
- 37.Claassens, L, Terwee, CB, Deeg, DJH, Broese van Groenou, MI, Widdershoven, GAM and Huisman, M. Development and validation of a questionnaire assessing the perceived control in health care among older adults with care needs in the Netherlands. Quality of Life Research, 2016; 25(4): 859–870. DOI: 10.1007/s11136-015-1124-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lau, DT, Scandrett, KG, Jarzebowski, M, Holman, K and Emanuel, L. Health-related safety: A framework to address barriers to aging in place. The Gerontologist, 2007; 47(6): 830–837. DOI: 10.1093/geront/47.6.830 [DOI] [PubMed] [Google Scholar]
- 39.Suter, E, Oelke, ND, Adair, CE and Armitage, GD. Ten key principles for successful health systems integration. Healthcare Quarterly, 2009; 13(Spec No): 16–23. DOI: 10.12927/hcq.2009.21092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Shaw, S, Rosen, R and Rumbold, B. What is integrated care: An overview of integrated care in the NHS 2011, The Nuffield Trust: London. [Google Scholar]
- 41.Arrue, B, Ambugo, EA, Baan, C, Barbaglia, G, Billings, J, de Bruin, S, de Weger, E, Espallargues Carrera, M, Hagen, T, Leichsenring, K, Lette, M, Minkman, M, Nies, H, Nijpels, G, Paat-Ahi, G, Ruppe, G, Schlette, S, Stoop, A, Tram, N, Vaage, SK, Wistow, G, Wosko, P and Zonneveld, N. Integrated care for older people living at home: Current situation and ambition of sites participating in the SUSTAIN project, In: Wosko, P and Ruppe, G (ed.). Vienna: Austrian Interdisciplinary Platform on Ageing/OEPIA; 2016. Available from: http://www.sustain-eu.org/products/eu-baseline-report/. [Google Scholar]
- 42.Glasgow, RE, Green, LW, Taylor, MV and Stange, KC. An evidence integration triangle for aligning science with policy and practice. American Journal of Preventive Medicine, 2012; 42(6): 646–654. DOI: 10.1016/j.amepre.2012.02.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sugavanam, T, Byng, R, Horrell, J, Fosh, B, Close, J, Lloyd, H. Co-designing a Generic Measure to Probe Person Centred Coordinated Care from the Perspective of the Patient: The Development of the P3CEQ. Journal of patient experience (under review). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Anderson, N and West, MA. Team Climate Inventory: Manual and user’s guide Windsor, UK: NFER-Nelson; 1994. [Google Scholar]
- 45.Kivimaki, M and Elovainio, M. A short version of the Team Climate Inventory: Development and psychometric properties. Journal of occupational and organizational psychology, 1999; 72(2): 241–246. DOI: 10.1348/096317999166644 [DOI] [Google Scholar]
- 46.Craig, P, Dieppe, P, Macintyre, S, Michie, S, Nazareth, I and Petticrew, M. Developing and evaluating complex interventions: The new Medical Research Council guidance. British Medical Journal, 2008; 337 DOI: 10.1136/bmj.a1655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Billings, J. The INTERLINKS framework for long-term care of older people in Europe. Journal of Integrated Care, 2013; 21(3): 126–138. DOI: 10.1108/JICA-02-2013-0007 [DOI] [Google Scholar]
- 48.Billings, J and Leichsenring, K. Methodological development of the interactive INTERLINKS Framework for Long-term Care. International journal of integrated care, 2014; 14: e021 DOI: 10.5334/ijic.1173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Rijken, M, Struckmann, V, Dyakova, M, Melchiorre, MG, Rissanen, S and Van Ginneken, E. ICARE4EU: Improving care for people with multiple chronic conditions in Europe. Eurohealth, 2013; 19(3): 29–31. [Google Scholar]
- 50.European Innovation Partnership on Active and Healthy Ageing. [webpage on the internet]. [cited 2017 January 6]. Available from: http://ec.europa.eu/research/innovation-union/index_en.cfm?section=active-healthy-ageing.
- 51.SELFIE. 2020 (Sustainable integrated care models for multi-morbidity: Delivery, financing and performance) [webpage on the internet]. [cited 2017 January 9]. Available from: http://www.selfie2020.eu/.
- 52.ACT@Scale [webpage on the internet]. [cited 2017 January 9]. Available from: https://www.act-at-scale.eu/.
- 53.JA-CHRODIS. (EU Joint Action on Chronic Diseases and promoting healthy ageing across the life-cycle) [webpage on the internet]. [cited 2017 January 9]. Available from: http://chrodis.eu/.


