Abstract
Isolated fractures of shaft of ulna are common. Plate fixation with anatomic reduction is thought to produce the best functional results in closed or open fractures. Surgery can be done under general and various types of regional anaesthesia. We report a case of fracture shaft of ulna treated by plating under a combination of WALANT (wide awake, local anaesthesia, no tourniquet) using tumescent anaesthesia and periosteal nerve block as a day care procedure.
Keywords: Plating of ulna, Periosteal block, WALANT
Introduction
Isolated fracture of ulnar shaft is notorious for prolonged healing time with average healing time of 10.5 weeks and non-union rate of 8% [1].The perception that ulnar shaft fractures treated by nonsurgical means frequently failed to unite prompted Watson-Jones to recommend internal fixation in preference to cast immobilization [2].
Local anaesthetic techniques (hematoma blocks, nerve blocks, intravenous regional anaesthesia, periosteal block) are well described for closed reduction of forearm fractures in children and adults.
WALANT (wide awake, local anaesthesia, no tourniquet) is affectively used in hand surgery as it offers less total blood loss and provide effective anaesthesia [3]. Tumescent anaesthesia involves subcutaneous infiltration of large volumes of tumescent fluid containing lidocaine (0.05% or 0.1%), saline, and epinephrine (1:1,000,000) to produce anaesthesia, swelling, and firmness of targeted areas [4].
We described open reduction and plating of isolated fracture ulnar shaft under a combination of WALANT and periosteal nerve block.
Case report
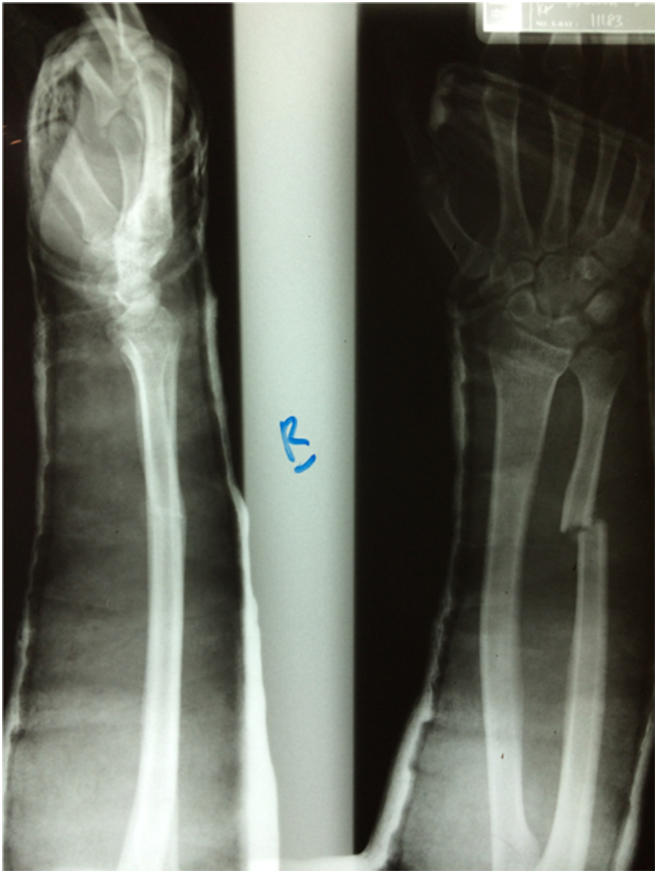
MR KZ is a 46 year old gentleman involved in a motor vehicle accident while he was riding his motorbike. His left forearm hit on the curb and he felt pain immediately after the fall. He also noticed swelling over his left forearm. He did not sustain any other major injury. The patient attended Accident and Emergency Department within 24 h of the injury. Primary and secondary surveys revealed a deformity over his left forearm which was tender on palpation (Fig. 1, Fig. 2). There was no neurovascular deficit over his left upper limb.
Fig. 1.
Plain radiograph revealed an isolated displaced fracture at the junction of distal and middle third shaft of left ulna.
Fig. 2.
Radiograph after 4 weeks did not show any callus formation.
He was then advised for open reduction and internal fixation of the fracture. Due to financial constraints, he refused admission and general anaesthesia. An option of doing the ulna plating under a combination of WALANT (wide awake, local anaesthesia, no tourniquet) and periosteal nerve block as a day care procedure was offered and he agreed.
The operation went smoothly without any difficulty in reducing or fixing the fracture and the most important thing was patient did not complain of any pain during the operation (Fig. 3). Patient was discharged home on the same day.
Fig. 3.
Per operative photograph showing the plate in situ after reduction whereby the patient is not in pain and actively flexing the elbow and extending his wrist.
Technique
We prepared the solution by mixing 50 ml of normal saline, 50 ml of lignocaine 2% & 1 mg adrenaline(1:1000).This will make the preparation of 100 ms of lignocaine 1% and 1:100,000 adrenaline.
Patient was brought into the day care ward in the morning of the operation. While in the ward, aside from the vital signs, his weight was taken and it was 65 kg. The widely quoted maximal dose of lignocaine with adrenaline is 7 mg/kg [5].
Once the solution was prepared, tumescent local anaesthesia and periosteal block was given at the site of the operation. Both are given 1 h prior to skin incision.We used 20 ml of the solution for the tumescent local anaesthesia.
Next, a periosteal block was given using 20 ml of the solution (Fig. 4, Fig. 5). We started by injecting proximally and subperiosteally along the whole length of posterior surface of ulna where the plate insertion was planned. The most important step not to be missed is to inject the local anaesthesia to cover the far cortex.
Fig. 4.
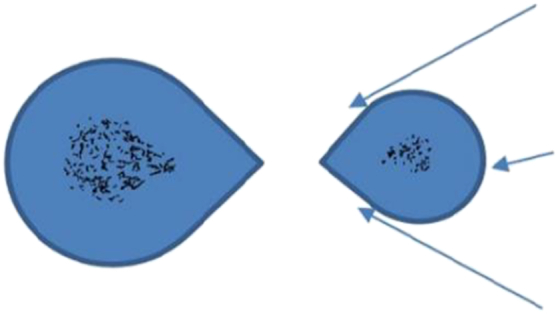
Diagram showing how we injected to get the periosteal block at ulna.
Fig. 5.
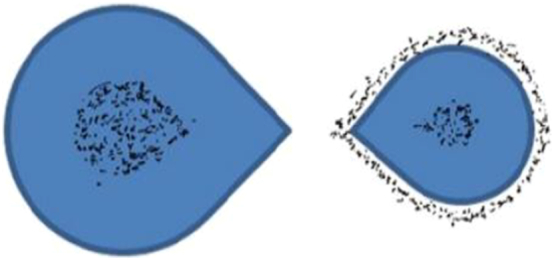
Diagram showing the local anaesthesia covering the whole circumference of the ulna.
We made sure we had at least 1 cm of visible or palpable subcutaneous local anaesthetic beyond the site where we plan to incise and where we were going to put the plate in.
Discussion
The optimal management for ulnar shaft fractures remains debatable with different authors recommending both surgical and non-surgical management.
Various regional anaesthetic techniques are commonly used including haematoma block, intravenous regional anaesthesia (Biers block), sedation and brachial plexus block; the first three of these techniques are frequently used in the emergency room setting.
Tumescent anaesthesia is a technique commonly used in cosmetic and dermatologic procedures. It involves subcutaneous infiltration of large volumes of tumescent fluid containing lidocaine (0.05% or 0.1%), saline, and epinephrine (1:1,000,000) to produce anaesthesia, swelling, and firmness of targeted areas.
There is still no agreement in Anatomy books on the sensory nerve pathway from the periosteum to the central nervous system but Tageldin ME showed the success of this method in 42 patients. From the periosteal pain receptors the sensory fibres course within the periosteum proximally through the muscular origin then join the muscular nerve supply to the central nervous system. The nerves that join the nutrient arteries are vaso-active for arteries and for bone cells to control osteoblastic and osteoclastic activities [6].
It is ideal to give the local anaesthetic 30 min or more to work. It takes an average 25 min for maximal cutaneous vasoconstriction to occur with 1:100,000 adrenaline [7].
Summary
WALANT allows us to perform the operation while the patient is awake. We use a combination of lignocaine and adrenaline, injected locally at the surgical site,which provide bloodless and anesthesized field for surgery.
Additional benefits include cost savings by performing plating as a day surgery.
No published studies on the use of the WALANT for plating of ulna was found in the literature.
Conflict of interest statement
We state that any financial and personal relationships with other people or organizations that could inappropriately influence our work is NONE.
References
- 1.Pollock F.H., Pankovich A.M., Prieto J.J., Lorenz M. The isolated fracture of the ulnar shaft. Treatment without immobilization. J. Bone Joint Surg. 1983;65(3):339–342. [PubMed] [Google Scholar]
- 2.Watson-Jones R. Adequate immobilization and non-union of fractures. Br. Med. J. 1934;1:936. doi: 10.1136/bmj.1.3829.936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ruxasagulwong S., Kraisarin J., Sananpanich K. Wide awake technique versus local anesthesia with tourniquet application for minor orthopedic hand surgery: a prospective clinical trial. J. Med. Assoc. Thail. 2015;98(1):106–110. [PubMed] [Google Scholar]
- 4.Klein J.A. Tumescent technique for local anesthesia. West J Med. 1996;164(6):517. [PMC free article] [PubMed] [Google Scholar]
- 5.Burk R.W., 3rd, Guzman-Stein G., Vasconez L.O. Lidocaine and epinephrine levels in tumescent technique liposuction. Plast. Reconstr. Surg. 1996;97(7):1379–1384. doi: 10.1097/00006534-199606000-00009. [DOI] [PubMed] [Google Scholar]
- 6.Tageldin M.E. Periosteal nerve blocks for distal radius and ulna fracture manipulation — the technique and early results. J. Orthop. Surg. Res. 2015;10:134. doi: 10.1186/s13018-015-0277-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McKee D.E., Lalonde D.H., Thoma A., Glennie D.L., Hayward J.E. Optimal time delay between epinephrine injection and incision to minimize bleeding. Plast. Reconstr. Surg. 2013;131(4):811–814. doi: 10.1097/PRS.0b013e3182818ced. [DOI] [PubMed] [Google Scholar]