Abstract
We present a case of a 61 year-old woman who suffered a bilateral posterior fracture-dislocation of the shoulder after an isolated episode of epileptic seizure. The patient was diagnosed at our Emergency department with x-rays and CT scans after being found unconscious. An indication for bilateral shoulder hemiprosthesis implant was initially given. However, given the peculiar pattern of the fracture, the hemiprosthesis was implanted on one side only, while the other side was treated with ORIF with four cannulated screws. After the one year, the patient had resumed her previous activities and had no complaints. We performed a review of similar cases in literature and provided a rationale for our choice of treatment and the reasons for its success.
Keywords: Shoulder, Posterior, Fracture, Dislocation, Bilateral, Seizure
Background
Bilateral posterior glenohumeral fracture-dislocation is an extremely rare clinical entity, accounting for a small minority of shoulder dislocations. Proposed etiologic mechanisms of injury include epileptic seizure, electrocution, or extreme trauma. Diagnosis of posterior gleno-humeral dislocation and fracture-dislocation is often challenging and thus frequently missed in the emergency setting [1], [2]. In light of the above, prompt diagnosis and adequate treatment are needed in order to best restore shoulder function.
We present a case of bilateral posterior fracture-dislocation of the shoulder after an episode of epileptic seizure, after which the patients was immediately transported to our Emergency Department. Diagnostic work-up, treatment plan, outcome and a final discussion are also presented.
Case presentation
A 61-year-old overweight female of Ukranian descent was admitted to the Emergency Department of the Umberto I hospital in Rome, Italy, after an isolated episode of tonic-clonic seizure while working as a cleaner. Past medical history was relevant for hypertension, cholecystectomy and appendectomy. No previous episodes of seizure were reported by the patient or the patient's family members. Upon arrival, the patient appears unresponsive, but is breathing spontaneously and displays biting marks on her tongue (Fig. 1). No focal neurological deficits are noted. Further workup includes Complete Blood Count (within normal limits), myoglobin (557 ng/mL), creatinine phosphokinase (2258 UI/L), Lactate Dehydrogenase (296 UI/L), creatinine kinase MB isoenzyme (7.6 ng/mL). Chest and brain CT scans, EEG, EKG and ABG are also requested and no abnormalities are noted by the attending neurologist. A traumatology assessment and workup reveals a right humeral head fracture (Fig. 2), for which a surgical indication is proposed. Further work up incudes CT scans of both shoulders (Figs. 3 and 4), highlighting the presence of a bilateral posterior fracture-dislocation: the left humeral head appears to have “collapsed” in an inward fashion, probably as a result of the muscle spasm and the simultaneous impact against the glenoid cavity, while the contralateral one appears to have a longitudinal cleft along the humeral head. The patient is then put in a Gilchrist immobilizer bilaterally and, once general conditions allow, transferred to the Traumatology department. During her stay, a new neurological consultation is performed and suggests the nature of the patient's fractures being due to the generalized muscular spasm experienced during the seizure. In light of the above, plain and Gd-enhanced brain MRIs and a polygraphic EEG are requested to further study the patient's conditions from the neurological standpoint: while the latter shows no abnormality, the former highlights several zones of high intensity signals in the white matter of the periventricular area and semioval centres, which is deemed compatible with chronic multi-infarct leukoencephalopathy, therefore ASA is added to her treatment regimen. The presence of an already known left parasagittal calcification is confirmed as well. A cardiology consultation also follows, with a request for Holter 24-hour test, which shows no abnormalities, and a sonographic examination of the heart and epiaortic vessels, which only displays a minimal quantity of pericardial fluid. These tests lead to the final neurologic diagnosis of isolated episode of epileptic seizure.
Fig. 1.
Clinical picture upon arrival. Note the biting marks on the patient's tongue and the absence of signs of direct trauma to either shoulder.
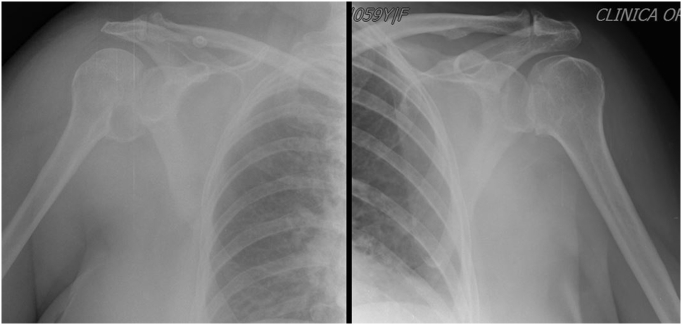
Fig. 2.
Emergency department X-ray in AP view.
Fig. 3.
Emergency department CT scan.
Fig. 4.
CT scan 3D reconstruction.
Once the patient is clear for surgery she is taken to the operating room, with the possibility of a bilateral one-stage hemiprosthesis implant: the decision-making criteria we used were medial hinge disruption, quality of humeral and glenoid bone stock, degree of involvement of articular surface cartilage caused by trauma and/or pre-existing conditions (i.e. osteoarthritis), fracture pattern and number of fragments. Intraoperative findings of the right humeral head showed two fracture lines, one involving the bicipital groove and the other being the reverse Hill-Sachs lesion. No significant articular cartilage or subchondral bone loss was noted. Also, although the fracture line partially involved the medial hinge, there appeared to be no significant displacement of such fracture. Conversely, the left humeral head showed medial hinge disruption, comminution of the humeral head fracture and loss of more than 50% of the articular surface. No significant bony lesions involving the glenoid cavity were noted on either side. Therefore, while a shoulder hemiprosthesis is implanted on the left side (Biomet Comprehensive Shoulder System® humeral stem and Versa-Dial humeral head), the decision is made intraoperatively to attempt an osteosynthesis on the right side: here the humeral head fracture is first reduced with the aid of Kirschner wires and the fixation is satisfactorily achieved with four cannulated screws (three 40 mm and one 42 mm, all 4 mm in diameter) (Fig. 5). The patient is then transferred to the physical medicine and rehabilitation department following surgery: early rehabilitation protocol consists of cautious Codman's passive ROM exercises under strict supervision and active ROM and muscle strengthening once conditions allow. Once adequate bilateral limb movement is achieved, parenteral anticoagulants are discontinued. She is ultimately discharged after a three-month inpatient treatment (including surgery, post-operative care and rehabilitation) after bilateral follow-up X-rays appear satisfactory (Fig. 6). A recommendation is given to strictly adhere to her physiotherapy protocol after discharge. No contraindication to a return to previous working activities (i.e. cleaner) is issued. At 24-months follow-up the patient has resumed her previous level of activity without significant discomfort (Fig. 7). Her Constant Score is 94 on the right side and 86 on the left side and her mobility restored to a satisfactory degree (Table 1).
Fig. 5.
Post-operative X-ray.
Fig. 6.
Two-year follow-up X-ray.
Fig. 7.
Two-year follow-up visit.
Table 1.
Comparison of ROM at 3 and 24 months post-operative.
| Shoulder ROM progression | 3 months post-operative | 24 months post-operative |
|---|---|---|
| Right side (ORIF) | Flexion: 110° Abduction: 90° External rotation: 30° Internal rotation: 45° |
Flexion: 180° Abduction: 160° External rotation: 80° Internal rotation: 45° |
| Left side (hemiprosthesis) | Flexion: 105° Abduction: 90° External rotation: 20° Internal rotation: 50° |
Flexion: 135° Abduction: 90° External rotation: 45° Internal rotation: 50° |
ROM: Range of Motion; ORIF: Open Reduction Internal Fixation.
Discussion
Bilateral posterior gleno-humeral fracture-dislocation is an extremely rare injury. The earliest report of the posterior pattern of this injury should be attributed to Mynter's description at the beginning of the 20th century [7]. Neer later identified fourteen cases of posterior shoulder fracture-dislocations out 1500 dislocations overall (0.9%) [8], [9]. Shaw [12] later reported the mechanism of injury in of posterior fracture dislocation as a partial adaptation of the previous description of posterior dislocation by McLaughlin [6]. Most Authors attribute the genesis of the fracture to generalized muscular spasm, especially when bilateral in nature [1], [3], [6], [12]. A high index of suspicion, along with adequate imaging techniques (x-rays with AP, scapular “Y” lateral and axillary views, and CT scans), are key in establishing a correct diagnosis [5], [10]. There appears to be no strict consensus and a variety of attempts to classify what constitutes a “fracture” of the humeral head after an episode of posterior shoulder dislocation: according to Robinson's proposed classification [11], in this case both fractures are to be considered as “complex” as an additional proximal humerus fracture line is present bilaterally besides a reverse Hill-Sachs lesion.
Various treatments have been proposed for the management of this injury. Predictors of humeral head ischemia are the main drivers in the treatment choice and have been described by Hertel, with metaphyseal head extension, medial hinge disruption and basic fracture pattern being the most reliable factors [4]. In general, hemiarthroplasty is indicated when the fracture involves more than 50% of the humeral head or when a Neer three- or four-part fracture is complicated by the presence of dislocation and/or porotic bone [3], [8], [9]. The patient described in this case was relatively young and appeared to have a bone stock of good quality. Furthermore, the medial hinge of the right shoulder was preserved. In fact, while the fracture pattern in the humeral head was rather unique, no comminution was present, which allowed for a satisfactory reduction and fixation of the fracture of the articular surface.
Conclusions
In conclusion, we believe the case we presented shows how Hertel criteria can be successfully used in case of a rare subtype of shoulder fracture. The presence of preserved vascularity, adequate fixation technique and joint surface congruence after fixation can lead to satisfactory results. Also, the presence of such lesions appears to be uniquely due to intense muscular spasm experienced during the epileptic seizure episode. In these cases, diagnosis based on etiology is important to better plan treatment both from the orthopaedic and neurological standpoint.
Disclaimer
None.
References
- 1.Brackstone M., Patterson S., Kertesz A. Triple “E” syndrome: bilateral locked posterior fracture dislocation of the shoulders. Neurology. 2001;56(10):1403–1404. doi: 10.1212/wnl.56.10.1403. [DOI] [PubMed] [Google Scholar]
- 2.Din K.M., Meggitt B.F. Bilateral four-part fractures with posterior dislocation of the shoulder: a case report. J. Bone Joint Surg. (Br.) 1983;65:176–178. doi: 10.1302/0301-620X.65B2.6826625. [DOI] [PubMed] [Google Scholar]
- 3.Hawkins R.J., Neer C.S., Pianta R.M., Mendoza F.X. Locked posterior dislocation of the shoulder. J. Bone Joint Surg. Am. 1987;69:9–18. [PubMed] [Google Scholar]
- 4.Hertel R., Hempfing A., Stiehler M., Leunig M. Predictors of humeral head ischemia after intracapsular fracture of the proximal humerus. J. Shoulder Elb. Surg. 2004;13(4):427–433. doi: 10.1016/j.jse.2004.01.034. [DOI] [PubMed] [Google Scholar]
- 5.Kokkalis Z.T., Iliopoulos I.D., Antoniou G., Antoniadou T., Mavrogenis A.F., Panagiotopoulos E. Posterior shoulder fracture–dislocation: an update with treatment algorithm. Eur. J. Orthop. Surg. Traumatol. 2016:1–10. doi: 10.1007/s00590-016-1840-5. [DOI] [PubMed] [Google Scholar]
- 6.McLaughlin H.L. Posterior dislocation of the shoulder. J. Bone Joint Surg. Am. 1952;24:584–590. [PubMed] [Google Scholar]
- 7.Mynter H. Subacromial dislocation from the muscular spasm. Ann. Surg. 1902;36:117. doi: 10.1097/00000658-190207000-00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Neer C.S., II Displaced proximal humeral fractures. I. Classification and evaluation. J. Bone Joint Surg. Am. 1970;52(6):1077–1089. [PubMed] [Google Scholar]
- 9.Neer C.S., II Displaced proximal humeral fractures. II. Treatment of three-part and four-part displacement. J. Bone Joint Surg. Am. 1970;52(6):1090–1103. [PubMed] [Google Scholar]
- 10.Paul J., Buchmann S., Beitzel K., Solovyova O., Imhoff A. Posterior shoulder dislocation: systematic review and treatment algorithm. Arthroscopy. 2011;27(11):1562–1572. doi: 10.1016/j.arthro.2011.06.015. [DOI] [PubMed] [Google Scholar]
- 11.Robinson C.M., Akhtar A., Mitchell M., Beavis C. Complex posterior fracture-dislocation of the shoulder. Epidemiology, injury patterns, and results of operative treatment. J. Bone Joint Surg. Am. 2007;89(7):1454–1466. doi: 10.2106/JBJS.F.01214. [DOI] [PubMed] [Google Scholar]
- 12.Shaw J.L. Bilateral posterior fracture-dislocation of the shoulder and other trauma caused by convulsive seizures. J. Bone Joint Surg. 1971;53A:1437–1440. [PubMed] [Google Scholar]