Abstract
It is well-established that hospitals recognized for good nursing care – Magnet hospitals – are associated with better patient outcomes. Less is known about how Magnet hospitals compare to non-Magnets on quality measures linked to Medicare reimbursement. The purpose of this study was to determine how Magnet hospitals perform compared to matched non-Magnet hospitals on Hospital Value Based Purchasing (VBP) measures. A cross-sectional analysis of three linked data sources was performed. The sample included 3,021 non-federal acute care hospitals participating in the VBP program (323 Magnets; 2,698 non-Magnets). Propensity score matching was used to match Magnet and non-Magnet hospitals with similar hospital characteristics. After matching, linear and logistic regression models were used to examine the relationship between Magnet status and VBP performance. After matching and adjusting for hospital characteristics, Magnet recognition predicted higher scores on Total Performance (Regression Coefficient [RC] = 1.66, p < 0.05), Clinical Processes (RC = 3.85; p < 0.01), and Patient Experience (RC = 6.33; p < 0.001). The relationships between Magnet recognition and the Outcome and Efficiency domains were not statistically significant. Magnet hospitals known for nursing excellence perform better on Hospital VBP measures. As healthcare systems adapt to evolving incentives that reward value, attention to nurses at the front lines may be central to ensuring high-value care for patients.
Keywords: magnet hospitals, value-based care, medicare
The U.S. health care system is rapidly adopting incentive programs that reward high-value rather than high-volume services. Central to this transition is the Centers for Medicare and Medicaid Services (CMS) Hospital Value Based Purchasing (VBP) program—a reward and penalty program incentivizing hospitals to provide high-value care to Medicare patients (Centers for Medicare & Medicaid Services, 2015a). In 2015, 1.5% of Medicare payments under the Inpatient Prospective Payment System were redistributed through the VBP program from poor-performing hospitals to better-performing hospitals. In later years, this percentage will increase to 2% (Centers for Medicare & Medicaid Services, 2015a). With $1.4 billion of Medicare payments at stake (Centers for Medicare & Medicaid Services, 2015b), hospitals are interested in ensuring high-quality care to avoid financial losses; yet, little attention has been paid to the role of nurses in affecting VBP performance.
Hospitals known for good nursing care are more likely to perform better on a broad array of patient outcomes (Aiken, Smith, & Lake, 1994; Barnes, Rearden, & McHugh, 2016; Evans et al., 2014; Friese, Xia, Ghaferi, Birkmeyer, & Banerjee, 2015; Kutney-Lee et al., 2015; McHugh et al., 2013; Smith, 2014; Stimpfel, Sloane, McHugh, & Aiken, 2015); yet, it is unknown how these hospitals perform with respect to VBP measures. The purpose of this article is to test whether Magnet hospitals— those designated for excellence in nursing—are predictive of higher performance on VBP measures than similar non-Magnet hospitals. This article provides a background of Magnet hospitals and the VBP program, a detailed methods section, a description of the study results, a discussion of the key findings, as well as implications for nursing practice, research, and policy.
Background
Magnet Hospitals
The Magnet concept emerged in the 1980s during a national nursing shortage (McClure, Poulin, Sovie, & Wandelt, 1983). Researchers noted that certain hospitals were better able to recruit and retain nurses and were therefore described as having “magnet-like” qualities (McClure et al., 1983). In 1994, the American Nurses Credentialing Center (ANCC) established the Magnet Recognition Program to formally recognize hospitals excelling in nursing care and patient outcomes. As of February 2017, nearly 450 U.S. hospitals had Magnet recognition, including four countries other than the United States (ANCC, 2017).
Magnet recognition signals hospitals that excel in fostering a culture that prioritizes the clinical and administrative contributions of nurses with the mission of improving care for patients (ANCC, 2017). This voluntary recognition involves an application process that requires hospitals to demonstrate high achievement on the five Magnet model components, which includes (a) transformational leadership, (b) structural empowerment, (c) exemplary professional practice, (d) new knowledge, innovations, and improvements, and (e) empirical outcomes (ANCC, 2017). Underlying each of the components is an organizational structure and culture facilitating how nurses deliver care to impact patient outcomes. Nurses working in environments characterized by a visible and influential chief nursing officer, nurse participation in clinical and administrative decision-making, interdisciplinary collaboration, and innovative evidence-based care practices are well situated to influence patient outcomes. Mounting evidence supports the association between Magnet recognition and patient outcomes, including lower mortality (Aiken et al., 1994; Evans et al., 2014; Friese et al., 2015; Kutney-Lee et al., 2015; McHugh et al., 2013), lower rates of failure-to-rescue (Kutney-Lee et al., 2015; McHugh et al., 2013), fewer patient falls (Lake, Shang, Klaus, & Dunton, 2010), better nurse-reported quality of care (Kutney-Lee et al., 2015), fewer infections (Barnes et al., 2016), and greater patient satisfaction (Chen, Koren, Munroe, & Yao, 2014; Smith, 2014; Stimpfel et al., 2015).
Value-Based Purchasing
The CMS is an agency of the U.S. Department of Health and Human Services. CMS is responsible for many of the federal health-care programs that provide health insurance (e.g., Medicare) and improve health-care quality. As part of CMS's health-care quality mission, the VBP program was established in October 2012. VBP encourages hospitals to provide high-value care to Medicare patients through a financial incentives program (Centers for Medicare & Medicaid Services, 2015a). Medicare reimbursement to hospitals is modified based on hospital performance on the VBP Total Performance Score.
In 2015, the Total Performance Score represented the overall performance comprises four domains (Clinical Processes, Patient Experience, Outcome, and Efficiency). To calculate the Total Performance Score in 2015, each domain was weighted as follows: Clinical Processes (20%), Patient Experience (30%), Outcome (30%), and Efficiency (20%; Centers for Medicare & Medicaid Services, 2015a).
The Patient Experience domain comprises the Hospital Consumer Assessment of Health care Providers and Systems survey measures, which includes items related to care providers'ability to listen and explain things, the hospital environment (i.e., cleanliness of room, and noise level), patient experiences (i.e., adequate pain management, timely toileting assistance, and medication safety), and overall rating of the hospital. The Clinical Processes domain includes a broad array of patient care tasks, many of which are a primary responsibility of nursing. In 2015, items in the Clinical Process domain included whether a patient with a heart attack received fibrinolytic therapy within 30 min of hospital arrival and primary percutaneous intervention within 90 min. It also included whether discharge instructions were given to patients with congestive heart failure and blood cultures were collected prior to starting antibiotics in patients with pneumonia. The Efficiency domain, defined as Medicare spending per beneficiary, represents price-standardized risk-adjusted Medicare Part A and Part B payments for an episode of care beginning 3 days prior to admission through 30 days following discharge (QualityNet, 2016). Risk-adjustment allows for more valid comparisons across providers who care for patients of varying clinical complexity. Accounting for such variations in patient clinical complexity enhances a fair comparison of outcomes and spending measures across providers (Centers for Medicare & Medicaid Services, 2015c). Finally, the Outcome domain comprises measures related to 30-day mortality rates for acute myocardial infarction, heart failure, and pneumonia; patient safety for selected indicators (PSI-90; a composite measure of indicators related to patient safety, in-hospital complications, and adverse events during surgeries and procedures); and central line-associated bloodstream infections (Centers for Medicare & Medicaid Services, 2015a).
Methods
Data Sources and Sample
We conducted a secondary analysis of hospitals using cross-sectional data from three sources. We acquired available information on hospitals'VBP performance during federal fiscal year 2015 (i.e., October 1, 2014 to September 30, 2015) from Hospital Compare, the publicly available database where CMS reports all VBP outcomes (Hospital Compare, 2017). We identified hospitals with known Magnet recognition in 2014 using the ANCC Magnet database.
The 2014 American Hospital Association Annual Survey provided data on hospital structural and organizational characteristics. American Hospital Association data are collected annually from over 6,400 U.S. hospitals (American Hospital Association, 2017). The final study sample of 3,021 hospitals (323 Magnets; 2,698 non-Magnets) is nationally representative of nonfederal acute care hospitals participating in the VBP program.
Measures
Our explanatory variable was hospital Magnet recognition. We considered hospitals to be Magnet if they held recognition in 2014. Our outcome of interest was hospital-level VBP performance. We considered the Total Performance Score as the main indicator of VBP performance as it is the VBP measure linked to financial rewards and penalties. To assess for variation in the relationship between Magnet status and hospital VBP performance, we also treated each of the four domains individually as outcomes of interest. This approach allowed us to identify whether certain domains were driving the relationship between overall performance on the Total Performance Score and Magnet status.
For our analysis, we constructed the Total Performance Score and three of the domains (Clinical Processes, Patient Experience, and Outcome) as continuous variables ranging between 0 and 100. We constructed the Efficiency domain as a binary variable because the hospital distribution was highly skewed toward 0. We assigned hospitals with an Efficiency score at or above the national mean a value of “1”; and we assigned those below the mean a value of “0”.
We included hospital characteristics in the matching approach and the regression analyses, consistent with prior work in this area (Barnes et al., 2016; Friese et al., 2015; Kahn et al., 2015; Kutney-Lee et al., 2015; McHugh et al., 2013; Stimpfel et al., 2015). Continuous variables included the following: hospital size (number of beds), Herfindahl-Hirschman index (a measure of market competition calculated as the sum of the squares of the market share of each hospital competing in the market; Henke, Maeda, Marder, Friedman, & Wong, 2013; Werner, Kolstad, Stuart, & Polsky, 2011), and case-mix index (CMI; Park, Blegen, Spetz, Chapman, & De Groot, 2012). CMI is a measure of patient acuity based on the average annual cost of a diagnosis-related group for a hospital's Medicare patients. Dichotomous and ordinal variables included (a) teaching status (presence and extent of medical fellows and residents), (b) technology status (ability to perform organ transplantation or open-heart surgery), (c) ownership (profit, non-profit), and (d) core-based statistical area (a measure of population density).
Analysis
Critics of the Magnet Recognition Program often suggest that Magnet status represents a recognition for excellent (i.e., better resourced) hospitals, rather than an intervention for improving outcomes (Aiken et al., 1994). Magnet hospitals tend to differ from non-Magnets, particularly with regard to certain characteristics including larger size, private ownership, major teaching status, healthier financial status, and greater technologic capability (Aiken et al., 1994). Thus, evidence demonstrating an outcome advantage for Magnet compared with non-Magnet hospitals is open to criticism that outcomes differences are not due to Magnet, but rather are due to marked differences in hospital characteristics. Our study addressed this criticism by employing a matching approach that paired similar Magnet and non-Magnet hospitals on observable characteristics, thus reducing concern about selection bias. We examined the link between Magnet recognition and VBP performance to inform whether investing in a process aimed at supporting frontline nurses would influence hospital-level outcomes linked to Medicare reimbursement.
First, we descriptively analyzed the sample to examine differences in VBP performance and hospital characteristics among Magnet and non-Magnet hospitals. Next, we used linear and logistic regression models to test the effect of Magnet recognition on VBP performance, before and after controlling for hospital characteristics.
Hospitals with certain characteristics are more likely to pursue and achieve Magnet recognition (Aiken et al., 1994). The same hospital characteristics that increase a hospital's propensity to be Magnet, such as larger size and greater technology capacity, may also be correlated with care quality in those hospitals. To account for this selection bias, we employed propensity score matching to create a sample of hospitals that were balanced on all observable characteristics, except with respect to Magnet recognition. Propensity score matching allows the creation of an “apples to apples” comparison among two groups by matching a set of hospitals on specific characteristics but allowing them to differ with respect to Magnet status (Austin, 2011).
We examined multiple matching approaches, including nearest neighbor with and without replacement, optimal matching, and genetic matching, in order to determine which approach would yield the best match in terms of balance among the covariates. By comparing the sum of the absolute values of the standardized differences, genetic matching yielded the most balanced match on the covariates of interest. Genetic matching uses an evolutionary search algorithm to determine the weight given to each of the observed covariates. This evolutionary approach maximizes the balance on observed covariates by assigning each covariate a given weight according to its relative importance for achieving the best overall balance (Diamond & Sekhon, 2012). Our genetic matching approach matched 323 Magnet hospitals with 253 non-Magnet hospitals.
In the postmatch analysis, we used linear and logistic regression to examine the effect of Magnet recognition on VBP performance, before and after controlling for hospital characteristics. We excluded CMI from the matching analysis of the Outcomes domain because this measure is already risk-adjusted by CMS (Centers for Medicare & Medicaid Services, 2015a). We used the R 3.3.1 for Windows statistical program (R Core Team, 2016) for the matching analysis and STATA® Version 14 (StataCorp, 2015) for the postmatching analysis.
Results
The study hospitals (n = 3,021) included the full set of non-Magnet hospitals (n = 2,698), Magnet hospitals (n = 323), and the subset of matched non-Magnet hospitals (n = 253; see Table 1). Before the propensity score matching was done, the most pronounced differences between Magnet and non-Magnet hospitals were that Magnet hospitals were larger on average (441 vs. 197 beds, p < .001) and more likely to be high-technology (76% vs. 30%, p < .001), major teaching facilities (20% vs. 6%, p < .001), located in metropolitan areas (96% vs. 73%, p < .001), and with a higher mean CMI (1.72 vs. 1.40, p < .05).
Table 1.
Characteristics of Hospitals, Before and After Matching (2014–2015).
| All hospitals (N = 3,021) | All non-Magnet hospitals (n=2,698) | Magnet hospitals (n = 323) | p-value | Matched non-Magnet hospitals (n =253) | Standardized differences | ||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Prematch | Postmatch | ||||||
| Hospital characteristics | |||||||
| Bed size, mean (SD) | 223 (212) | 197 (183) | 441 (299) | <.001 | 385 (274) | 0.8129 | 0.0162 |
| Mean Case Mix Index (CMI), mean (SD) | 1.52 (0.31) | 1.50 (0.30) | 1.72 (0.27) | <.05 | 1.672 (0.24) | 0.82 | 0.0293 |
| Mean HHI (HRR), mean (SD) | 1239 (1021) | 1242 (1011) | 1220 (1101) | .7249 | 1184 (941) | −0.0192 | 0.0334 |
| Profit status (% for-profit) | 23 | 26 | 4 | <.001 | 5 | −1.1061 | 0.0157 |
| Technology status (% High Tech) | 35 | 30 | 76 | <.001 | 70 | 1.0683 | 0.0144 |
| Teaching status | |||||||
| Minor teaching (%) | 32 | 32 | 36 | .139 | 36 | 0.0848 | 0.0129 |
| Major teaching (%) | 8 | 6 | 20 | <.001 | 16 | 0.3481 | 0.0153 |
| Location | |||||||
| Metropolitan location (%) | 75 | 73 | 96 | <.001 | 95 | 1.1178 | 0 |
| Micropolitan location (%) | 17 | 18 | 4 | <.001 | 4 | −0.7332 | 0 |
| Rural location (%) | 8 | 9 | 0.31 | <.001a | 0.4 | −1.5031 | 0 |
Note. Minor teaching is defined by ≤ 1:4 medical residents or fellows to beds; Major teaching is defined by > 1:4 medical residents or fellows to beds; Micropolitan is defined by > 10,000 & ≤ 50,000 residents.
Uses fisher exact test because cell size < 5.
After propensity score matching, the standardized differences between Magnet and non-Magnet hospitals markedly decreased. The standardized differences for each of the postmatch hospital characteristics were less than 0.05, indicating a strong match (Silber et al., 2001).
Matching diagnostics for the sample before and after matching are shown in Figures 1 and 2. The histograms show the distribution of propensity scores before and after matching (Figure 1). Prior to matching, the distributions are dissimilar; however, the distributions after matching are comparable. Likewise, the standardized bias plot demonstrates a marked decrease in the standardized difference in means after matching, suggesting a well-matched sample (Figure 2). Before matching, the propensity for being a Magnet hospital given the hospital characteristics was dissimilar for Magnet (0.27) and non-Magnet (0.09). After matching, the propensity scores became more similar (0.27 for Magnet; 0.26 for non-Magnet).
Figure 1.
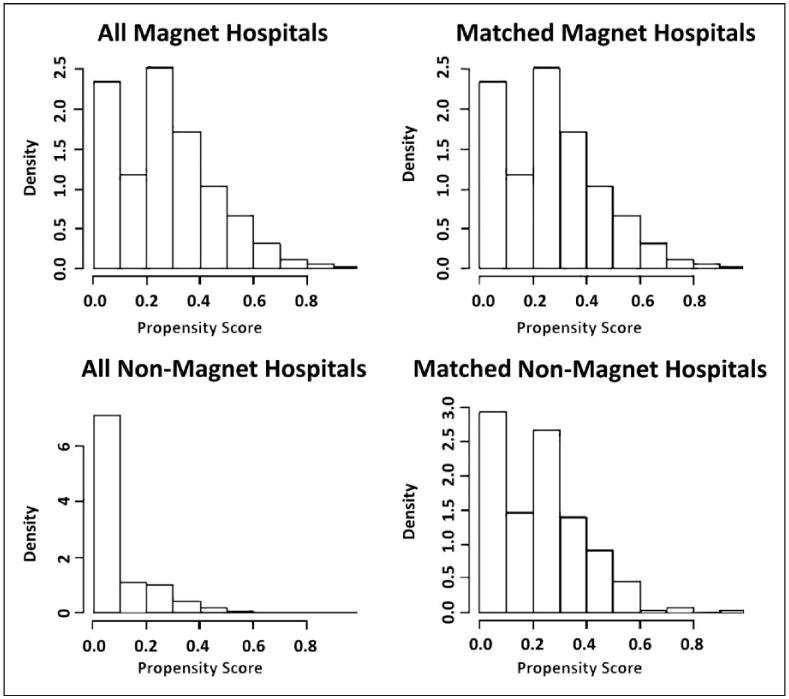
Distribution of propensity scores among Magnet and Non-Magnet hospitals, before and after matching. The histograms of the propensity scores of Magnet and non-Magnet hospitals show that prior to matching the distribution of the two groups'propensity scores were dissimilar; however, after matching, the distributions of the propensity scores were comparable.
Figure 2.
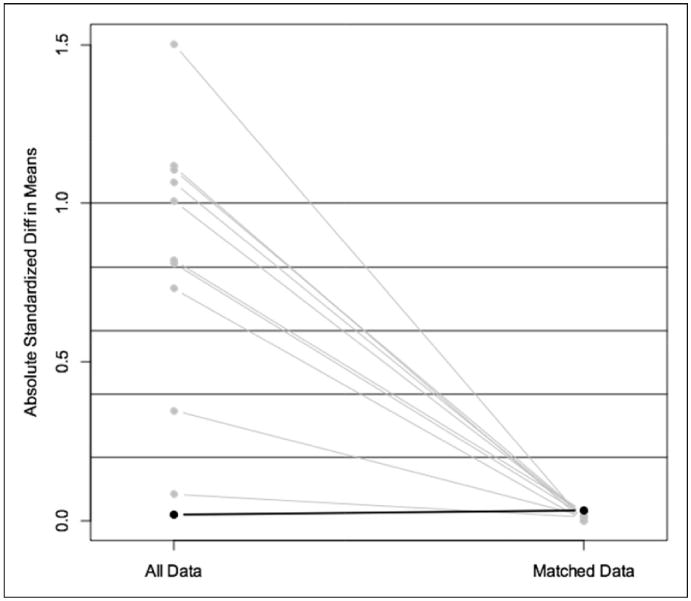
Absolute standardized differences in means, before and after matching. Note. The plot of the absolute standardized differences in means shows the improvement in balance between Magnet and non-Magnet hospitals, before and after matching. After matching, the individual hospital characteristics each had an absolute standardized difference in means below 0.2, suggesting a good match.
Comparisons of VBP performance between Magnet and non-Magnet hospitals, before and after propensity score matching, are presented in Table 2. Prior to matching, the Total Performance Score was not significantly different between Magnet and non-Magnet hospitals. After matching, the difference in means was significant (p < .05). In the postmatch sample, Magnet hospitals performed significantly better on Total Performance, Clinical Processes, and Patient Experience than non-Magnet hospitals.
Table 2.
Hospital Performance on VBP Performance Domains by Magnet Recognition, in Pre- and Postmatched Sample.
| Magnet | Non-Magnet | Matched non-Magnet | Prematch | Postmatch | ||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|
||||||
| Mean (SD) | Mean (SD) | p-value | Mean (SD) | Difference in means | p value | Difference in means | p value | |
| Total performance score (N = 3,021) | 40.6 (9.1) | 41.7 (12.8) | .1236 | 39.0 (9.7) | 1.1 | .1236 | 1.6 | <.05 |
| Domain scores | ||||||||
| Clinical process (N=2,906) | 58.5 (16.2) | 55.1 (20.7) | <.05 | 55.5 (17.3) | 3.4 | <.05 | 3 | <.05 |
| Patient experience (N=2,990) | 42.6 (15.5) | 41.6 (21.0) | .4399 | 36.6 (15.6) | 1 | 0.4399 | 6 | <.001 |
| Outcome (N=2,720) | 46.6 (17.3) | 44.9 (18.6) | .1291 | 46.1 (17.6) | 1.7 | .1291 | 0.5 | .7786 |
| N (%) | N (%) | N (%) | % Difference | % Difference | ||||
| Efficiencya (N=3,012) | 49 (15.2) | 933 (34.7) | <.001 | 55 (21.7) | 19.5 | <.001 | 6.5 | <.05 |
Percent of hospitals performing better than the national average on the Efficiency domain.
The associations between Magnet recognition and VBP performance, before and after matching, are displayed in Table 3. The unmatched analysis adjusting for hospital characteristics show that Magnet hospitals were associated with higher scores on Total Performance (Regression Coefficient [RC]=2.73; p < .001), Clinical Processes (RC = 3.61; p < .01), and Patient Experience (RC = 7.11; p < .001). Magnet hospitals were associated with lower scores on Efficiency (RC=−0.32); however, this association was not statistically significant. After matching and adjusting for hospital characteristics, Magnet recognition predicted higher scores on Total Performance (RC=1.66, p < .05), Clinical Processes (RC = 3.85; p < .01), and Patient Experience (RC = 6.33; p < .001). In the postmatched analysis, the relationships between Magnet recognition, Outcome, and Efficiency were not statistically significant.
Table 3.
Effect of Magnet Recognition on VBP Outcomes, Before and After Matching.
| Before matching | After matching | ||||
|---|---|---|---|---|---|
|
|
|
||||
| VBP outcomes | Unadjusted Coefficient (95% CI) | Adjusted for hospital characteristics Coefficient (95% CI) | VBP outcomes | Unadjusted Coefficient (95% CI) | Adjusted for hospital characteristics Coefficient (95% CI) |
| Total performance score (N=3,021) | −1.13 (−2.57, 0.31) | 2.73*** (1.27, 4.18) | Total performance score (N=576) | 1.60* (0.05, 3.14) | 1.66* (0.17, 3.16) |
| Domain scores | Domain scores | ||||
| Clinical process (N=2,906) | 3.37** (1.03, 5.72) | 3.61** (1.10, 6.11) | Clinical process (N=575) | 3.53* (0.78, 6.28) | 3.85** (1.10, 6.61) |
| Patient experience (N=2,990) | 0.93 (−1.43, 3.29) | 7.11*** (4.86, 9.36) | Patient experience (N=573) | 6.03*** (3.44, 8.61) | 6.33*** (3.86, 8.80) |
| Outcomea (N=2,720) | 1.66 (−0.49, 3.81) | 1.66 (−0.66, 3.98) | Outcomea (N=572) | 0.08 (−2.86, 3.01) | −0.05 (−3.01, 2.90) |
| Efficiencyb (N=3,012) | −1 09*** (−1.40, -0.77) | −0.32 (−0.66, 0.03) | Efficiencyb (N=575) | −0.45* (−0.87, −0.02) | −0.38 (−0.83, 0.07) |
Note. Adjusted for hospital size, profit status, technology status, teaching status, CBSA type, CMI: case-mix index; HHI: Herfindahl-Hirschman index.
Outcome domain excludes adjustment for CMI.
Percent of hospitals performing better than the national average on the Efficiency Domain.
p <.05.
p <.01.
p <.001.
Discussion
Our analysis is the first to explore whether hospitals known for excellence in nursing—Magnet hospitals— demonstrate higher performance on VBP measures than non-Magnet hospitals. We find that Magnet recognition predicts better performance on Total Performance, as well as two of the VBP domains: Clinical Processes and Patient Experience. Magnet hospitals in our study performed comparably to non-Magnets on the Outcomes and Efficiency domain.
Our finding that Magnet hospitals are most likely to perform better on the Patient Experience domain, which comprises the Hospital Consumer Assessment of Health care Providers and Systems survey measures, is consistent with prior findings (Stimpfel et al., 2015). Stimpfel et al. (2015) found that compared with patients in non-Magnet hospitals, patients in Magnet hospitals reported higher overall ratings, were more likely to recommend the hospital, and had a better experience with nurse communication (Stimpfel et al., 2015). Better patient experiences of care may reflect how the cultural and structural organization of Magnet hospitals afford nurses the support and resources to deliver thorough and thoughtful care. Nurses working in supportive environments are most likely to have requisite time and resources to complete necessary care tasks, critically assess patient plans of care, and educate patients and families (Brooks Carthon, Lasater, Sloane, & Kutney-Lee, 2015), which has been associated with greater patient satisfaction (Lake, Germack, & Viscardi, 2015).
In our study, Magnet hospitals performed significantly better on the Clinical Processes domain than their matched non-Magnet controls. Completing clinical care tasks in a timely fashion requires collaboration and communication among nurses and physicians. This inter-professional collaboration reflects a central tenet of Magnet's model component, exemplary professional practice. Indeed, nurses working in Magnet hospitals report delivering higher-quality care compared with nurses working in otherwise similar non-Magnet hospitals (Stimpfel, Rosen, & McHugh, 2014), suggesting in part that nurses in these supported environments are able to provide complete and timely patient care.
We found Magnet hospitals performed no differently than matched non-Magnets on the Efficiency domain, which is the measure of Medicare spending per beneficiary. This finding is unsurprising in light of prior research demonstrating a weak association between quality and costs of care (Fisher et al., 2003a; Fisher et al., 2003b; Hussey, Wertheimer, & Mehrotra, 2013; Jha, Orav, Dobson, Book, & Epstein, 2009; Yasaitis, Fisher, Skinner, & Chandra, 2009). Moreover, an analysis of quality and spending demonstrated that the Efficiency domain rewards low-spending hospitals even when those hospitals are also low quality (Das et al., 2016), suggesting the Efficiency domain may be a poor discriminator of high-value performance. In another study, researchers used a matching approach similar to ours and found Magnet hospitals and those with above average nurse staffing levels perform better on surgical mortality at similar costs, suggesting better value care in Magnet settings (Silber, Rosenbaum, et al., 2016). We assessed hospital spending using the Efficiency domain; however, measuring spending relative to outcomes may be a better metric than the current Efficiency domain measure. A measure of spending relative to outcomes would be more consistent with the aim of the VBP program, which is to reward hospitals demonstrating high-value care.
In our study, Magnet recognition was not significantly associated with performance on the Outcome domain. Prior research suggests Magnet hospitals are associated with lower mortality rates among adult medical-surgical patients than non-Magnet hospitals (Aiken et al., 1994; Kutney-Lee et al., 2015; McHugh et al., 2013). Researchers in these studies, however, used patient-level data which allowed for more precise risk-adjustment than was possible with VBP's hospital-level measure of patient outcomes. Our finding that Magnet hospitals may perform no better than non-Magnet hospitals on clinical outcomes may be related to inadequate risk-adjustment among hospital-level patient outcomes. Another study found little evidence that the VBP program led to lower mortality (Figueroa, Tsugawa, Zheng, Orav, & Jha, 2016). A different team of researchers criticized hospital-level outcome prediction modeling, suggesting it could be substantially improved by accounting for hospital characteristics (Silber, Satopaa, et al., 2016). In 2017, the VBP domains will be revised, resulting in the removal of the Outcome domain and the creation of a Safety domain. Measures that previously comprised the Outcome domain will be divided among the Clinical Processes domain and a newly created Safety domain (Centers for Medicare & Medicaid Services, 2015a). Future studies are warranted to assess whether our findings are influenced by the revised design of the VBP program.
This study was not without limitations. Our conclusions are limited to associations and cannot suggest causal relationships due to the cross-sectional design. However, we improve the validity of our findings by employing a sophisticated matching approach to account for possible selection bias into Magnet. Nonetheless, our matching approach could not account for unobserved factors, for example, whether particular hospitals implemented quality improvement interventions.
Implications for Nursing Practice, Research, and Policy
The results from this study have implications for nursing practice. Principally, the findings lend support for hospital investment in Magnet recognition. Being a Magnet hospital is associated with greater performance on VBP measures—notably, Total Performance Score, which is linked to Medicare reimbursements. Despite the initial and ongoing expense of Magnet recognition, the Magnet investment may be offset, at least in part, by better performance on VBP measures.
Future research in this area should explore how the relationship between Magnet status and VBP performance changes as the VBP program design continues to evolve over time. For example, in 2017, the Safety domain will be introduced and the Outcomes domain will be removed. In addition to redesigning the domains, CMS continues to modify the measures that comprise each domain by removing measures that hospitals consistently achieve and testing alternative measures. As the VBP program evolves and the financial incentives continue to grow as a proportion of Medicare reimbursement, follow-up studies of the relationship between Magnet recognition and VBP performance will be increasingly important.
With respect to policy implications, our findings point to nursing quality as one mechanism through which some hospitals perform better on quality metrics than others. Future policy initiatives to improve high-value health care should focus on nurses—particularly with respect to the quality of the working environments in which nurses care for patients. Currently, Magnet recognition is most often achieved by larger, for-profit hospitals, with significant financial resources. However, efforts to make Magnet recognition more accessible to a broader segment of the hospital sector could enhance access to high-value health care.
Conclusion
Our findings demonstrate that hospitals known for nursing excellence perform better on many VBP measures. Notably, Magnet hospitals perform better than similar non-Magnets on Total Performance Score, which is the VBP metric linked to financial rewards and penalties. These findings are of particular interest to hospital administrators as they adapt to the evolving health-care system that continues to reward high-value care.
Despite the high cost of investing in resources needed for initial and ongoing Magnet recognition, evidence suggests the expense may be offset within a 2-year period through higher net inpatient income (Jayawardhana, Welton, & Lindrooth, 2014). Our findings lend credence to the existing business case for Magnet, demonstrating that Magnet hospitals perform better on measures linked to Medicare reimbursement.
Acknowledgments
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This publication was made possible by funding support from the following grants: National Institute of Nursing Research T32-NR0714 (PI: Aiken), and the Leonard Davis Institute of Health Economics (Co-PIs: Lasater, Germack).
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Aiken LH, Smith HL, Lake ET. Lower Medicare mortality among a set of hospitals known for good nursing care. Medical Care. 1994;32:771–787. doi: 10.1097/00005650-199408000-00002. [DOI] [PubMed] [Google Scholar]
- American Hospital Association. AHA data: Data collection methods. 2017 Retrieved from https://www.ahadata-viewer.com/about/data/
- American Nurses Credentialing Center (ANCC) ANCC magnet recognition program. 2017 Retrieved from http://www.nursecredentialing.org/Magnet/
- Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behavioral Research. 2011;46:399–424. doi: 10.1080/00273171.2011.568786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnes H, Rearden J, McHugh MD. Magnet® hospital recognition linked to lower central line-associated bloodstream infection rates. Research in Nursing and Health. 2016;39:96–104. doi: 10.1002/nur.21709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks Carthon JM, Lasater KB, Sloane DM, Kutney-Lee A. The quality of hospital work environments and missed nursing care are linked to heart failure readmissions: A cross sectional study of U.S. hospitals. British Medical Journal Quality and Safety. 2015;24:255–263. doi: 10.1136/bmjqs-2014-003346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Medicare & Medicaid Services. Hospital value-based purchasing program. 2015a Retrieved from https://www.cms.gov/Medicare/Quality-initiatives-patient-assessment-instruments/hospital-value-based-purchasing/index.html.
- Centers for Medicare & Medicaid Services. Fiscal ysear 2015 results for the CMS hospital-acquired condition reduction program and hospital value-based purchasing program. 2015b Retrieved from https://www.cms.gov/Newsroom/MediaReleaseDatabase/Fact-sheets-items/2014-12-18-2.html.
- Centers for Medicare & Medicaid Services. Fact sheet: Risk adjustment. 2015c Retrieved from https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/PhysicianFeedbackProgram/Downloads/Risk-Adjustment-Fact-Sheet.pdf.
- Chen J, Koren ME, Munroe DJ, Yao P. Is the hospital's magnet status linked to HCAHPS scores? Journal of Nursing Care Quality. 2014;29:327–335. doi: 10.1097/NCQ.0000000000000062. [DOI] [PubMed] [Google Scholar]
- Das A, Norton EC, Miller DC, Ryan AM, Birkmeyer JD, Chen LM. Adding a spending metric to Medicare's Value-Based Purchasing Program rewarded low-quality hospitals. Health Affairs. 2016;35:898–906. doi: 10.1377/hlthaff.2015.1190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diamond A, Sekhon JS. Genetic matching for estimating causal effects: A general multivariate matching method for achieving balance in observational studies. Review of Economics and Statistics. 2012;95:932–945. doi: 10.1162/REST_a_00318. [DOI] [Google Scholar]
- Evans T, Rittenhouse K, Horst M, Osler T, Rogers A, Miller JA, et al. Rogers FB. Magnet hospitals are a magnet for higher survival rates at adult trauma centers. Journal of Trauma and Acute Care Surgery. 2014;77:89–94. doi: 10.1097/TA.0000000000000262. [DOI] [PubMed] [Google Scholar]
- Figueroa JF, Tsugawa Y, Zheng J, Orav EJ, Jha AK. Association between the value-based purchasing pay for performance program and patient mortality in US hospitals: Observational study. British Medical Journal. 2016;353:i2214. doi: 10.1136/bmj.i2214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher ES, Wennberg DE, Stukel TA, Gottlieb DJ, Lucas FL, Pinder EL. The implications of regional variations in Medicare spending. Part 1: the content, quality, and accessibility of care. Annals of Internal Medicine. 2003a;138:273–287. doi: 10.7326/0003-4819-138-4-200302180-00006. [DOI] [PubMed] [Google Scholar]
- Fisher ES, Wennberg DE, Stukel TA, Gottlieb DJ, Lucas FL, Pinder EL. The implications of regional variations in Medicare spending. Part 2: Health outcomes and satisfaction with care. Annals of Internal Medicine. 2003b;138:288–298. doi: 10.7326/0003-4819-138-4-200302180-00007. [DOI] [PubMed] [Google Scholar]
- Friese CR, Xia R, Ghaferi A, Birkmeyer JD, Banerjee M. Hospitals in ‘magnet’ program show better patient outcomes on mortality measures compared to non-‘magnet’ hospitals. Health Affairs. 2015;34:986–992. doi: 10.1377/hlthaff.2014.0793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henke RM, Maeda JL, Marder WD, Friedman BS, Wong HS. Medicare and commercial inpatient resource use: impact of hospital competition. American Journal of Managed Care. 2013;19:e238–248. [PubMed] [Google Scholar]
- Hospital Compare. Hospital compare. 2017 Retrieved from https://www.medicare.gov/hospitalcompare/search.html?
- Hussey PS, Wertheimer S, Mehrotra A. The association between health care quality and cost: A systematic review. Annals of Internal Medicine. 2013;158:27–34. doi: 10.7326/0003-4819-158-1-201301010-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jayawardhana J, Welton JM, Lindrooth RC. Is there a business case for magnet hospitals? Estimates of the cost and revenue implications of becoming a magnet. Medical Care. 2014;52:400–406. doi: 10.1097/MLR.0000000000000092. [DOI] [PubMed] [Google Scholar]
- Jha AK, Orav EJ, Dobson A, Book RA, Epstein AM. Measuring efficiency: The association of hospital costs and quality of care. Health Affairs. 2009;28:897–906. doi: 10.1377/hlthaff.28.3.897. [DOI] [PubMed] [Google Scholar]
- Kahn CN, Ault T, Potetz L, Walke T, Chambers JH, Burch S. Assessing Medicare's hospital pay-for-performance programs and whether they are achieving their goals. Health Affairs. 2015;34:1281–1288. doi: 10.1377/hlthaff.2015.0158. [DOI] [PubMed] [Google Scholar]
- Kutney-Lee A, Stimpfel AW, Sloane DM, Cimiotti JP, Quinn LW, Aiken LH. Changes in patient and nurse outcomes associated with Magnet hospital recognition. Medical Care. 2015;53:550–557. doi: 10.1097/MLR.0000000000000355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lake ET, Germack HD, Viscardi MK. Missed nursing care is linked to patient satisfaction: A cross-sectional study of US hospitals. British Medical Journal Quality and Safety. 2015;25:535–543. doi: 10.1136/bmjqs-2015-003961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lake ET, Shang J, Klaus S, Dunton NE. Patient falls: Association with hospital Magnet status and nursing unit staffing. Research in Nursing and Health. 2010;33:413–425. doi: 10.1002/nur.20399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McClure M, Poulin M, Sovie M, Wandelt MA. Magnet hospitals: Attraction and retention of professional nurses. Kansas City, MO: American Nurses Association; 1983. [Google Scholar]
- McHugh MD, Kelly LA, Smith HL, Wu ES, Vanak JM, Aiken LH. Lower mortality in magnet hospitals. Medical Care. 2013;51:382–388. doi: 10.1097/MLR.0b013e3182726cc5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park SH, Blegen MA, Spetz J, Chapman SA, De Groot HA. Comparison of nurse staffing measurements in staffing-outcomes research. Medical Care. 2012;53:e1–e8. doi: 10.1097/MLR.0b013e318277eb50. [DOI] [PubMed] [Google Scholar]
- QualityNet. Measure methodology reports: Medicare spending per beneficiary (MSPB) measure. 2016 Retrieved from http://www.qualitynet.org/dcs/ContentServer?c=Pageamp;pagename=4;QnetPublic%2FPage%2FQnetTier3&cid=1228772053996.
- R Core Team. R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2016. [Google Scholar]
- Silber JH, Rosenbaum PR, McHugh MD, Ludwig JM, Smith HL, Niknam BA, Aiken LH. Comparison of the value of nursing work environments in hospitals across different levels of patient risk. Journal of the American Medical Association Surgery. 2016;151:527–536. doi: 10.1001/jamasurg.2015.4908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silber JH, Rosenbaum PR, Trudeau ME, Even-Shoshan O, Chen W, Zhang X, Mosher RE. Multivariate matching and bias reduction in the surgical outcomes study. Medical Care. 2001;39:1048–1064. doi: 10.1097/00005650-200110000-00003. [DOI] [PubMed] [Google Scholar]
- Silber JH, Satopaa VS, Mukherjee N, Rockova V, Wang W, Hill AS, et al. George EL. Improving Medicare's hospital compare mortality model. Health Services Research. 2016;51:1229–1247. doi: 10.1111/1475-6773.12478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith SA. Magnet hospitals: Higher rates of patient satisfaction. Policy, Politics, and Nursing Practice. 2014;15:30–41. doi: 10.1177/1527154414538102. [DOI] [PubMed] [Google Scholar]
- StataCorp. Stata statistical software: Release 14. College Station; TX: StataCorp LP: 2015. [Google Scholar]
- Stimpfel AW, Rosen JE, McHugh MD. Understanding the role of the professional practice environment on quality of care in Magnet and non-Magnet hospitals. Journal of Nursing Administration. 2014;44:10–16. doi: 10.1097/NNA.0000000000000015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stimpfel AW, Sloane DM, McHugh MD, Aiken LH. Hospitals known for nursing excellence associated with better hospital experience for patients. Health Services Research. 2015;51:1120–1134. doi: 10.1111/1475-6773.12357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Werner RM, Kolstad JT, Stuart EA, Polsky D. The effect of pay-for-performance in hospitals: Lessons for quality improvement. Health Affairs. 2011;30:690–698. doi: 10.1377/hlthaff.2010.1277. [DOI] [PubMed] [Google Scholar]
- Yasaitis L, Fisher ES, Skinner JS, Chandra A. Hospital quality and intensity of spending: Is there an association? Health Affairs. 2009;28:w566–w572. doi: 10.1377/hlthaff.28.4.w566. [DOI] [PMC free article] [PubMed] [Google Scholar]


