Abstract
Background
Pediatrician and pediatric subspecialist density varies substantially among the various Canadian provinces, as well as among various states in the US. It is unknown whether this variability impacts health outcomes. To study this knowledge gap, we evaluated pediatric asthma admission rates within the 2 Canadian provinces of Manitoba and Saskatchewan, which have similarly sized pediatric populations and substantially different physician densities.
Methods
This was a retrospective cross-sectional cohort study. Health regions defined by the provincial governments, have, in turn, been classified into “peer groups” by Statistics Canada, on the basis of common socio-economic characteristics and socio-demographic determinants of health. To study the relationship between the distribution of the pediatric workforce and health outcomes in Canadian children, asthma admission rates within comparable peer group regions in both provinces were examined by combining multiple national and provincial health databases. We generated physician density maps for general practitioners, and general pediatricians practicing in Manitoba and Saskatchewan in 2011.
Results
At the provincial level, Manitoba had 48.6 pediatricians/100,000 child population, compared to 23.5/100,000 in Saskatchewan. There were 3.1 pediatric asthma specialists/100,000 child population in Manitoba and 1.4/100,000 in Saskatchewan. Among peer-group A, the differences were even more striking. A significantly higher number of patients were admitted in Saskatchewan (590.3/100,000 children) compared to Manitoba (309.3/100,000, p < 0.0001).
Conclusions
Saskatchewan, which has a lower pediatrician and pediatric asthma specialist supply, had a higher asthma admission rate than Manitoba. Our data suggest that there is an inverse relationship between asthma admissions and pediatrician and asthma specialist supply.
Keywords: Health manpower/trends, Physicians/supply and distribution, Pediatric, General practitioners
Background
There is substantial variability in the ratio of pediatric subspecialists to the population of children among the Canadian provinces, with higher ratios in provinces such as Alberta (AB) and Manitoba (MB), and lower ratios in provinces such as Saskatchewan (SK), British Columbia (BC) and Ontario (ON) [1]. In some provinces, the physician density in certain subspecialties can be up to four times greater than in others [1]. The cause of the uneven distribution of physicians is multifactorial, and an imbalanced physician distribution has been identified as one of the major challenges facing the healthcare workforce.
Regional variability of access to pediatricians and pediatric subspecialists results in prolonged wait times [2, 3]. Best practice-based patient management may greatly influence asthma hospitalization inpatient rates and emergency visits [4]. Expert-based asthma care may be more likely to follow consensus guideline recommendations [5]. A potential consequence of not having access to asthma specialists may be reduced patient and family access to asthma education and lack of such access has been shown to worsen childhood asthma outcomes [6].
There is evidence that expert-based outpatient asthma care improves asthma outcomes in adults, including hospitalization rates and the level of asthma control [5, 7]. Data from Manitoba (MB) suggest the reported prevalence of diagnostic label of asthma in adults is positively related to the number of referrals to specialists [8]. In the world of pediatric asthma, the effect that access to expert care has on health outcomes is unknown. We hypothesized that a paucity of pediatricians and pediatric asthma specialists (pediatric pulmonologists and allergists [9]) would lead to worse health outcomes. In this novel study, we elected to compare asthma health outcomes within comparable health regions in Saskatchewan (SK), the province with the lowest supply of pediatric asthma subspecialists, with MB, the province with one of the highest supplies of pediatric asthma subspecialists. These provinces were also selected due to their similarities in climate, population diversity, indigenous populations, housing conditions, and other variables (see Table 3). We hypothesized that the differing supply of pediatricians and pediatric asthma specialists would affect admission rates.
Table 3.
Key environment (2012) and housing parameters (2011 Census, 2011 Household Survey) that may affect asthma admission rates in the four peer-group A health regions in MB and SK
| Parameter | Winnipeg | Brandon | Regina | Saskatoon | t-testa | |
|---|---|---|---|---|---|---|
| Days above 0 °C | 175 | 171 | 168 | 170 | 0.11 | |
| Growing days (average temperature above 5 °C) | 181 | 182 | 182 | 177 | 0.26 | |
| Average persons per household | 2.4 | 2.3 | 2.4 | 2.4 | 0.21 | |
| Housing in need of major repair (%) | 9.30 | 6.70 | 9.40 | 6.20 | 0.47 | |
| Indigenous population (%) | 11.7 | 11.23 | 10.2 | 10.24 | 0.02 | |
| Immigrant population (%) | 21.88 | 12.86 | 11.16 | 11.93 | 0.16 | |
| Population density per square kilometer | 1430 | 599 | 1328 | 1060 | 0.36 | |
| Average income ($) | 38,159 | 38,544 | 45,698 | 43,497 | 0.02 | |
| Prevalence of low income in 2010 based on after-tax low-income measure (%)b | < 18 years | 22.8 | 20.9 | 18.6 | 18.5 | 0.04 |
| Prevalence of low income in 2010 based on after-tax low-income measure (%)b | < 6 years | 26.3 | 24.2 | 23.9 | 21.6 | 0.12 |
acomparing the two provinces; b2010 data.
Sources: Environmental data from Environment Canada database (http://climate.weather.gc.ca/, last accessed on 17-Dec-2013), Stats Canada 2011 Census (http://www12.statcan.gc.ca/census-recensement/2011/dp-pd/index-eng.cfm, last accessed 3-Apr-2018), and Stats Canada 2011 National Household Survey (http://www12.statcan.gc.ca/nhs-enm/index-eng.cfm, last accessed 18-Dec-2013)
Methods
Inter-regional comparisons of pediatric asthma hospitalizations should control for the multiple factors that may influence asthma prevalence and severity, including demographic, environmental, and socio-economic factors [7]. Unfortunately, a multivariate analysis could not be performed as CIHI privacy regulations prevent sharing of record-level information. Therefore, a multistep approach was used instead, to allow regional comparisons while attempting to control for other relevant factors, as follows:
-
i.
Within provinces, health regions have been defined by each provincial government, and are termed Regional Health Authorities (RHA). At the time of the analysis, there were 11 health regions in MB (2 of which are considered or include urban areas) and 13 in SK (2 of which are urban).
-
ii.
Health region peer groups have been defined by Statistics Canada based on 24 variables that are important determinants of health, including a variety of socioeconomic, social, and demographic factors. Using these defined peer groups, it is possible to compare regions with similar socio–economic characteristics. Statistics Canada performed a stepwise discriminant analysis and found that, of the 24 variables, 4 were found to play a key role in defining the health region peer groups: population density, proportion of indigenous population, proportion of immigrants, and employment rate [10].
-
iii.
Due to privacy considerations, rural peer groups could not be examined because the small number of children meeting study criteria in sparsely-populated peer groups (< 5 entries per peer group) would make these children potentially identifiable.
-
iv.
For our analysis, we therefore used patient data originating from peer group “A,” which includes 4 predominantly-urban health regions grouped together based on their similar social and economic health determinants (Saskatoon RHA and Regina Qu’Appelle RHA in SK, and Brandon RHA and Winnipeg RHA in MB). Peer Group A is distinguishable from the other Peer Groups because the values for each of the 4 defining variables fall within the 35th percentile to 65th percentile range (the medium range) [10].
-
v.
We compiled a geo-database of all family physicians with their postal code using the Canadian Institute of Health Information (CIHI) – Scott’s Medical Database. Each record was associated to a dissemination area using the postal code and Statistics Canada’s Postal Code Conversion File (PCCF) and then geo-coded. Pediatrician and pediatric subspecialty data were obtained from validated academic & provincial databases provided by the Pediatric Department Chairs in both MB and SK. Asthma experts were defined as pediatric allergists and pediatric pulmonologists [9]. The provincial physician workforce (general practitioners (GPs) and pediatricians) was then mapped for each province and health region, using maps generated by ArcGIS 10.1, a commercially available geomapping software program.
-
vi.
Since peer groups have similar characteristics, mapping the physician workforce in each health region allowed us to assess the impact of the workforce on patient outcomes for asthma. This assessment was relatively independent of the other parameters that could affect asthma morbidity and health outcomes [7].
-
vii.Using the Canadian Association of Pediatric Health Centers - Pediatric Decision Support Network (CAPHC-CPDSN) database, data extraction from the CIHI Portal [FY2009–2010 DAD]), the Case Mix Group (CMG) [11] comprising pediatric admissions to hospital for upper/lower respiratory was identified and data for CMG 147 (asthma) were extracted. The following parameters were collected:
- Total number of hospital admissions in the provinces of MB and SK,
- Length of stay (LOS) [12],
- Expected length of stay (ELOS) [12]. The calculation for ELOS as defined by Statistics Canada: (a) takes into account the reason for hospitalization, age, comorbidity, and complications; (b) uses case mix group methodology (statistically and clinically homogeneous groups based on the collection of clinical and administrative data); and (c) is calibrated for the given year [13]. ELOS and LOS were compared to determine whether the actual LOS was longer or shorter than predicted, based on disease severity.
- Case Mix Group Resource Intensity Weight. Case Mix Groups are defined by CIHI, and combine inpatients with similar resource-use characteristics. The Resource Intensity Weight describes total patient resource use, for a particular case mix group [12].
-
viii.
Provincial-level health outcomes were compared with physician manpower per 100,000 children.
-
ix.
Asthma admission rates are affected by a number of variables, including age [14], climate [15, 16], ethnicity [7, 17], sex [14, 18], housing [19], income [19], environmental tobacco smoke exposure [16], and many other factors. We analyzed these covariates within the peer-group comparison.
Statistical analysis
The data analysis was performed directly from the Excel spreadsheets provided by each centre. The actual admissions were provided through the CIHI portal. Population was based on the 2011 census, and data for 2010 and 2012 were estimated based on population growth. Statistical analysis was performed with simple statistical tests using Excel (Microsoft ® Excel for Mac version 12.1.0 (080409) and GraphPad Prism version 4.02 for Mac (GraphPad Software, San Diego, CA, U.S.A.). Continuous data were analyzed for normal distribution with the Shapiro Wilks test. Since data were normally distributed, they were reported as mean and standard deviation. Admission rates were compared using the Fisher’s exact test. Administrative data were compared using unpaired t-test. A p-value of < 0.05 was considered statistically significant.
Results
The populations of the two provinces were comparable (MB 1,208,268; SK 1,053,960). MB had 48.6 pediatricians and pediatric subspecialists per 100,000 children compared to 23.5 in SK. Figure 1 maps all general practitioners and pediatricians in both provinces, according to health regions, with health regions of the same peer group shaded identically. In MB, 3 cities: Winnipeg, Brandon and Thompson had pediatricians, whereas in SK pediatricians were located in 5 cities: Regina, Saskatoon, Prince Albert, Swift Current, Moose Jaw, Yorkton and North Battleford. Province-wide, there were 1.1 pediatric pulmonologists per 100,000 children in MB and 0.4 in SK respectively. Moreover, there were 2 pediatric allergists in MB per 100,000 children and 1 in SK. With regards to peer group comparison, there was a much higher pediatrician and pediatric subspecialist density in the peer group “A” cities of Winnipeg and Brandon, MB when compared to Regina and Saskatoon, SK (Fig. 1, Table 2).
Fig. 1.
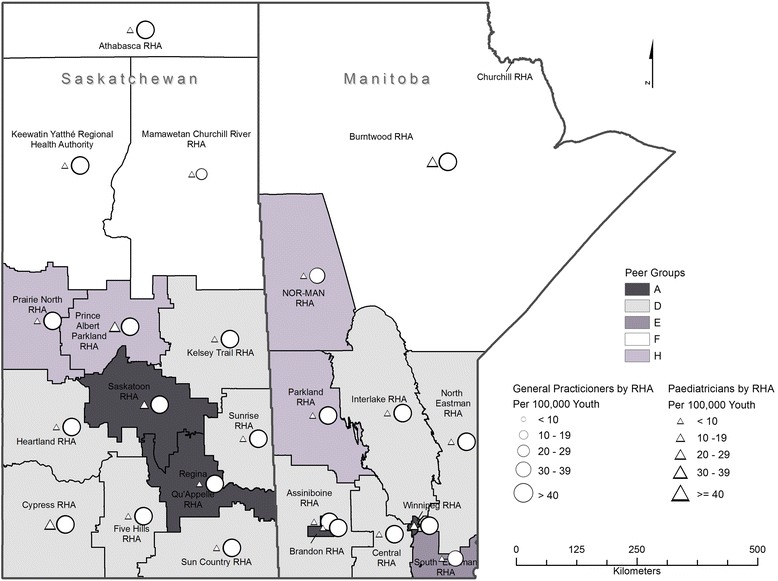
Density of paediatricians and general practitioners in the provinces of MB and SK based on health region. RHA: Regional Health Authority (Health Region). Statistics Canada defines a RHA as an administrative area defined by the provincial ministries of health. The figure was generated by JG, based on a shapefile provided by EB
Table 2.
Comparison of key administrative data as cases/100,000 child population in the four peer-group A health regions: Case mix group plus rate intensity weight using case mix group and rate intensity weight (CMG + RIW); expected length of stay (ELOS); and acute length of stay (LOS); not significant (n.s.). Actual cases were taken from the CIHI database. Population was extrapolated based on 2011 census data and the annual growth rates. Cases/100,000 child population were calculated from real numbers. The 3 right columns were provided from the CIHI portal. In the bottom of the table, the averages for the 3 years are provided
| Province | Peer Group A Regional Health Authority | Year | Cases | Population < 19 | Cases / 100,000 child population | CMG/RIW (Average) | ELOS Days (Average) | Acute LOS Days (Average) |
|---|---|---|---|---|---|---|---|---|
| Manitoba | Winnipeg | 2010 | 79 | 167,557 | 47.1 | 0.57 | 1.9 | 2.2 |
| Winnipeg | 2011 | 88 | 169,592 | 51.9 | 0.46 | 1.8 | 2.2 | |
| Winnipeg | 2012 | 113 | 171,627 | 65.8 | 0.50 | 1.9 | 2.3 | |
| Brandon | 2010 | 17 | 13,714 | 124.0 | 0.41 | 1.8 | 2.1 | |
| Brandon | 2011 | 26 | 13,881 | 187.3 | 0.45 | 1.7 | 1.7 | |
| Brandon | 2012 | 21 | 14,048 | 149.5 | 0.41 | 1.7 | 2.0 | |
| Saskatchewan | Regina Qu’Appelle | 2010 | 199 | 65,088 | 305.7 | 0.44 | 1.8 | 2.0 |
| Regina Qu’Appelle | 2011 | 130 | 66,484 | 195.5 | 0.45 | 1.8 | 2.0 | |
| Regina Qu’Appelle | 2012 | 98 | 67,880 | 144.4 | 0.43 | 1.7 | 1.8 | |
| Saskatoon | 2010 | 55 | 22,516 | 244.3 | 0.40 | 1.7 | 2.1 | |
| Saskatoon | 2011 | 44 | 22,999 | 191.3 | 0.47 | 1.7 | 2.0 | |
| Saskatoon | 2012 | 51 | 23,482 | 217.2 | 0.51 | 1.9 | 2.5 | |
| Average over 3 years | ||||||||
| Manitoba |
Combined Manitoba Peer Groups A
(Winnipeg RHA + Brandon RHA) |
2010–2012 | 115 | 183,473 | 62.4 | 0.47 | 1.8 | 2.08 |
| Saskatchewan |
Combined Saskatchewan Peer Groups A
(Regina Qu’Appelle RHA + Saskatoon RHA) |
2010–2012 | 192 | 89,483 | 215.8 | 0.45 | 1.77 | 2.07 |
| Comparison between provinces (unpaired Student t-test) | n.s | n.s | n.s. | |||||
| Comparison between provinces (Fisher’s Exact Test) | 0.012* | |||||||
At the provincial level, there were 967 admissions for asthma in MB and 1533 in SK (CMG 147) in the year 2011. The number of admissions /100,000 child population were 309.3 in MB and 590.3 in SK (p < 0.0001, Fisher’s exact test). Table 1 provides characteristics of patients in both provinces. The mean actual LOS was not significantly different: 2.7 versus 3.1 days (p > 0.5). The sum of the acute LOS was 3014 days in MB versus 4153 days in SK, a difference which was not statistically significant. The patients in MB tended to be sicker; their ELOS was 2.9 days in MB versus 2.4 days in SK, although the difference was not statistically significant. Similarly, Case Mix Group-based Resource Intensity Weight was very similar in both provinces.
Table 1.
Admissions for asthma in children and youth under 18 years of age in the two provinces. Data were based on the 2011 census and the 2011 calendar year. LOS = length of stay; ELOS = expected length of stay
| Parameter | MB | SK |
|---|---|---|
| Total population | 1,208,268 | 1,053,960 |
| Child population | 312,598 | 259,709 |
| General practitioners /100,000 child population | 386.4 | 383.1 |
| General paediatricians /100,000 child population | 19.2 | 10.0 |
| Specialized paediatricians (all subspecialties) /100,000 child population | 29.4 | 13.5 |
| Number of admissions | 967 | 1533* |
| Number of admissions /100,000 child population | 309.3 | 590.3* |
| Number of readmissions | 181 | 152 |
| Number of readmissions /100,000 child population | 57.9 | 58.5 |
| Total acute LOS | 3014 | 4153 |
| Average ELOS | 2.9 days | 2.4 days |
| Average LOS | 3.1 days | 2.7 days |
* p < 0.0001, Fisher’s exact test
Table 2 provides a comparison of the four health regions belonging to peer group A. Similar to findings by province in Table 1, the number of pediatric asthma cases /100,000 child population was significantly higher in peer group A regions in Saskatchewan (215.8/100,000) than in the same peer group in Manitoba (62.4/100,000) (p = 0.012) from 2010 to 2012.
With regards to covariates affecting asthma admission rates, the cities in the four peer groups appear to be similar (Table 3), with only the percentage indigenous population and household income being significantly different (p = 0.02, Table 3). While higher admission rates have been found to be associated with lower income and indigenous ethnicity [20], incomes were lower, and the proportion of the population that is indigenous was higher, in MB. Outdoor air quality, defined using annual mean respirable particles (PM10) was very similar in Winnipeg, Brandon, Regina, and Saskatoon (11, 24, 21, and 12 mcg/m3, respectively (2010 Data) [21]. While previous Canadian research has related mean aeroallergen levels to asthma hospitalizations [15], mean aeroallergen counts were not available for SK cities, so this factor could not be compared. Population rates of smoking in MB and SK are extremely similar: 18.7 and 19.2% (2011 data) [22]. As a proxy for climate, we compared days above 0 degrees Celsius and growing days (defined as average temperatures above 5 degrees Celsius), and found that both of these variables were also similar in MB and SK. As sex and age affect patient outcomes [14], we also compared the patient demographics in the four peer group A health regions. The male to female ratio was comparable in both provinces (p = 0.538). Age was also not significantly different. The percentage of young children aged 1–4 was 63.8% in MB and 61.6% in SK (p = 0.599). When only using data on pediatric patients from the peer group A health regions, there was a clear inverse relationship between the number of pediatricians and subspecialists, and specifically pediatric asthma specialists, and the admission rate.
Discussion
Our analysis demonstrated significant differences in the rate of asthma admissions between the provinces of MB and SK. Significantly more patients were admitted in SK, when compared with MB, and the patients in SK had a lower acuity but the same LOS. At the same time, there was a much lower density of pediatricians and pediatric subspecialists in SK when compared with MB. It appears that–similar to adults [7]–decreased access to pediatricians and pediatric asthma experts has a negative impact on admissions with asthma.
A variety of studies [17] have suggested that care by asthma experts improves asthma outcomes. Vollmer et al. evaluated 914 children and adults with asthma followed in an American health maintenance organization and found that patients managed by an allergist were more likely to take daily asthma medications and inhaled anti-inflammatory agents than patients followed by a generalist [5]. The allergists’ patients were also less likely to visit the emergency department and had higher quality of life scores [5]. Similarly, Wu et al. examined 1954 adults with asthma treated by a managed care company and found that patients treated by an asthma expert rather than a generalist were more knowledgeable about asthma, more likely to have received inhaled corticosteroids, less likely to have had emergency department visits or hospitalizations and had better asthma control [7]. Pediatric pulmonologists, pediatric allergists and pediatricians can provide expert asthma care [16]. Klomp et al. reported that suboptimal asthma control was common in SK and was associated with inadequate use of inhaled corticosteroids, including lack of use or inadequate doses [23]. As our findings suggest that disparities in access to pediatric asthma specialists were associated with an increased number of asthma hospitalizations in SK, we hypothesize that a significant number of admissions in SK may have been avoidable.
Our findings are particularly concerning given wide interprovincial variations in the national availability of adult and pediatric pulmonologists, as discussed by Cockcroft and Wensley in 2000 [24]. In fact, reported average wait times to see an adult pulmonologist in SK were 7–8 weeks for university-based consultants and 4–5 weeks for community-based consultants [24]. Given that the ratio of pulmonologists to the population was 1:86,000 for adults and 1:756,000 for pediatrics, it can be safely assumed that wait times are a great deal longer for pediatric patients. Given the disparity in the density of asthma experts in SK as compared to MB wait times can be assumed to be considerably longer in SK.
Our study is limited by demographic and environmental data, which can substantially affect asthma control, severity and admission rates. However, the four group A peer regions were remarkably similar and should thus have similar asthma incidence rates. Only indigenous population and average income differed slightly between the group A peer regions in both provinces. However, assuming the trends found in previous studies, the differences should have resulted in higher admission rates in MB. It should be emphasized that data required for a multivariate analysis could not be released due to privacy considerations, and fewer than 5 entries were omitted for the same reason. For this reason, we could only compare group A health regions with large populations.
The study is also limited by the assumption that non-subspecialists including pediatricians are not asthma “experts.” It is certain that many pediatricians and some family physicians have special expertise, experience, and interest in asthma care in children. Additionally, it is likely that some expert asthma care in SK and MB is provided by adult pulmonologists and allergists. Nevertheless, the number of these types of physicians is likely small and is therefore unlikely to have substantially impacted our findings. We base this on the low number of physicians with predominantly adult billings that billed for patients under 18. Asthma hospitalization rates and LOS are likely affected by numerous other factors, including age distributions, sex [14, 18], poverty [25], and ethnicity [26], including indigenous origin [20], but these parameters are similar in peer group A health regions and/or have been taken into account. Asthma misclassification is possible, although it has been shown that asthma classification in large Canadian databases is generally accurate [27]. Differences in access to expert physicians may have complex effects on asthma classification. In children, there is significant overlap between asthma and a variety of other conditions, including bronchiolitis, recurrent upper respiratory tract infections, and croup. Asthma experts may be more likely to diagnose asthma accurately. Conversely, asthma may be over-diagnosed by non-expert physicians, who may also be less reliant on objective testing in children 6 years and older, as recommended by current guidelines [28]. Our data are unable to determine whether SK has an increased number of shorter admissions as a result of unnecessarily early admission to hospital, or whether admission for children in MB is unduly delayed so children are sicker when they are admitted. Inaccuracy in the numbers of specialists and family doctors is always a possibility; however, we believe that the errors are negligible based on the fee codes used for mapping the physicians and the confirmation of the accuracy by the department chairs.
The question of the generalizability of our findings is important. The literature is scarce on the topic. We are only aware of one study from comparing the US states Georgia and North Carolina [29]. That study suggests similar evidence for the association between geographical variation in access to primary and asthma specialists and pediatric asthma outcomes [29]. Thus, the conclusions presented in this study are likely more broadly applicable beyond Canada.
In conclusion, this novel study demonstrated disparities in specialist and subspecialist availability likely have an adverse impact on asthma control in Canadian children and youth from the provinces studies. Efforts to ensure more uniform availability of pediatricians and pediatric subspecialists will likely improve health outcomes in asthma care.
To the best of our knowledge, this is the first study to find an association between access to specialized health care providers and health outcome parameters from administrative databases. Further research is required to establish this relationship between health outcomes and providers across the nation, which in turn will enable health care providers to rank admission rates in equivalent peer group health regions according to the supply of specialists and subspecialists. This may lead to a better understanding of the number of health care providers necessary per region to optimize pediatric health outcomes. To validate the findings of this pilot study and to assess whether the findings apply to other disease groups, we plan to conduct a Pan-Canadian study using the same geo-mapping and peer group methodology.
Conclusions
This pilot study demonstrates a link between specialist and subspecialist supply and health outcomes. It may be possible to perform health human resource planning by matching the number of specialists and subspecialists with the administrative data used to determine what the appropriate supply for a given population should be.
Acknowledgements
We acknowledge the data extraction for the environmental and housing parameters as well as the expert editing of Ms. Lana Rothfels, Research Assistant to Dr. Guido Filler. We would also like to acknowledge the contributions of Leah Boon, National Coordinator, CAPHC – Canadian Pediatric Decision Support Network.
Funding
The study was self-funded through discretionary research accounts of GF at Lawson Health Research Institute. The funding bodies had no role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Availability of data and materials
The data that support the findings of this study are available from CIHI but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Only the results of the analysis were made available to the authors as per CIHI policies.
Abbreviations
- AB
Alberta
- BC
British Columbia
- CAPHC-CPDSN
Pediatric Decision Support Network
- CIHI
Canadian Institute of Health Information
- CMG
Case Mix Group
- ELOS
Expected length of Stay
- GP
General Practitioner
- LOS
Length of Stay
- MB
Manitoba
- PCCF
Postal Code Conversion File
- RHA
Regional Health Authority
- SK
Saskatchewan
Authors’ contributions
GF conceived the study, led the research group, was primarily responsible for writing the manuscript, and was responsible for the study; TK acted as the asthma expert, significantly contributed to the analysis and presentation of data, and significantly contributed to the written manuscript by composing several versions of the paper; JG was the senior Health Geographer, was indispensable for all of the geographical analysis, significantly modified and contributed to the study approach, read all versions of the manuscript, and developed the geographical figure; EB was the scientist at CIHI who made it possible to obtain the study data, established the physician map and the geodata for each physician, and significantly contributed to all stages of the production of the manuscript; SJ as a department chair, was instrumental in developing the concept for the study, contributed to the analysis of the data, and critically revised the paper multiple times; MW in her role as the research coordinator of PCC, coordinated the collaborative research, critically revised different versions of the manuscript, supported several different aspects of the study through administrative assistance, and successfully coordinated such a diverse group of scientists; EO was primarily responsible for organizing the data retrieval from the CAPHC-CPDSN portal, revised multiple versions of the manuscript, and was instrumental in sorting through various approaches to determine the final method of presenting the data; CG as the Chair of the Department of Pediatrics in Winnipeg, her contribution to the project was critical in that she clearly identified all specialists and subspecialists in the province, and she critically revised multiple iterations of the paper; LG as the Chair of the Department of Pediatrics in Saskatoon, his contribution to the project was critical in that he clearly identified all specialists and subspecialists in Saskatchewan, and he critically revised multiple iterations of the paper; BP had the original idea that we need to consider GPs, specialists and subspecialists as care providers for children and that the knowledge gap concerning whether or not the substantial variability affects child outcomes must be addressed, and has always envisioned the use of this knowledge in national health human resource planning, to ensure that health outcomes of children are similar across the country. All authors read and approved the final manuscript
Ethics approval and consent to participate
The study was deemed ethics approval exempt by the Research Ethics Board at Laval University, Quebec City, Quebec, Canada. As the data were anonymized data and not at a single data entry level but rather in clusters of a minimum of 5, the study was deemed exempt from the need for individual consent. If within a health region there were less than 5 records, data were not provided. As a CIHI employee, EB had administrative permission to access and use the data using data queries. Data were not revealed at record level and remained anonymized. All authors assessing the CIHI data signed an agreement to use the portal after appropriate training and that no individual data is available.
Consent for publication
Not Applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Guido Filler, Phone: +1-519-685-8377, Email: guido.filler@lhsc.on.ca.
Tom Kovesi, Email: kovesi@cheo.on.ca.
Erik Bourdon, Email: ebourdon@cihi.ca.
Sarah Ann Jones, Email: sarah.jones@lhsc.on.ca.
Laurentiu Givelichian, Email: dr.givelichian@usask.ca.
Cheryl Rockman-Greenberg, Email: cgreenberg@exchange.hsc.mb.ca.
Jason Gilliland, Email: jgillila@uwo.ca.
Marion Williams, Email: mwilliams@paediatricchairs.ca.
Elaine Orrbine, Email: eorrbine@caphc.org.
Bruno Piedboeuf, Email: bruno.piedboeuf@fmed.ulaval.ca.
The Paediatric Chairs of Canada Mark Bernstein:
Robert Connelly, Denis Daneman, Ciarán Duffy, Marc-Andre Dugas, Allison Eddy, Guido Filler, Jean-Yves Frappier, Susan Gilmour, Laurentiu Givelichian, Cheryl Rockman-Greenberg, Lennox Huang, James D. Kellner, Michael Shevell, Cathy Vardy, and Hervé Walti
References
- 1.Filler G, Piedboeuf B. Paediatric chairs of C. Variability of the pediatric subspecialty workforce in Canada. J Pediatr. 2010;157(5):844–847. doi: 10.1016/j.jpeds.2010.05.015. [DOI] [PubMed] [Google Scholar]
- 2.Miller AR, Armstrong RW, Masse LC, Klassen AF, Shen J, O'Donnell ME. Waiting for child developmental and rehabilitation services: an overview of issues and needs. Dev Med Child Neurol. 2008;50(11):815–821. doi: 10.1111/j.1469-8749.2008.03113.x. [DOI] [PubMed] [Google Scholar]
- 3.Filler G, Sutandar M, Poulin D. Waiting times in a tertiary paediatric nephrology clinic. Paediatr Child Health. 2007;12(1):15–18. [PMC free article] [PubMed] [Google Scholar]
- 4.Lougheed MD, Garvey N, Chapman KR, et al. Variations and gaps in management of acute asthma in Ontario emergency departments. Chest. 2009;135(3):724–736. doi: 10.1378/chest.08-0371. [DOI] [PubMed] [Google Scholar]
- 5.Vollmer WM, O'Hollaren M, Ettinger KM, et al. Specialty differences in the management of asthma. A cross-sectional assessment of allergists' patients and generalists' patients in a large HMO. Arch Intern Med. 1997;157(11):1201–1208. doi: 10.1001/archinte.1997.00440320095009. [DOI] [PubMed] [Google Scholar]
- 6.Cicutto L, Murphy S, Coutts D, et al. Breaking the access barrier: evaluating an asthma center's efforts to provide education to children with asthma in schools. Chest. 2005;128(4):1928–1935. doi: 10.1378/chest.128.4.1928. [DOI] [PubMed] [Google Scholar]
- 7.Wu AW, Young Y, Skinner EA, et al. Quality of care and outcomes of adults with asthma treated by specialists and generalists in managed care. Arch Intern Med. 2001;161(21):2554–2560. doi: 10.1001/archinte.161.21.2554. [DOI] [PubMed] [Google Scholar]
- 8.Erzen D, Roos LL, Manfreda J, Anthonisen NR. Changes in asthma severity in Manitoba. Chest. 1995;108(1):16–23. doi: 10.1378/chest.108.1.16. [DOI] [PubMed] [Google Scholar]
- 9.Kovesi T, Giles BL, Pasterkamp H. Long-term management of asthma in first nations and Inuit children: a knowledge translation tool based on Canadian paediatric asthma guidelines, intended for use by front-line health care professionals working in isolated communities. Paediatr Child Health. 2012;17(7):e46–e64. [PMC free article] [PubMed] [Google Scholar]
- 10.Canada S. Health region peer groups – user guide. Health regions and peer groups. 2007;2007 http://www.statcan.gc.ca/pub/82-221-x/2012002/regions/hrpg2007-eng.htm. Accessed 10 Jan 2014
- 11.CMG+ (Case Mix Groups). Case Mix 2014; https://www.cihi.ca/en/cmg. Accessed 3 Apr 2018.
- 12.Resource Indicators: DAD Resource Intensity Weights and Expected Length of Stay. Standards: Case Mix 2014; https://www.cihi.ca/en/resource-indicators-dad-resource-intensity-weights-and-expected-length-of-stay. Accessed 3 Apr 2018.
- 13.Definitions and Data Sources. Health Indicators 2000; http://www.statcan.gc.ca/pub/82-221-x/4060874-eng.htm. Accessed 10 Jan 2014.
- 14.Strid JM, Gammelager H, Johansen MB, Tonnesen E, Christiansen CF. Hospitalization rate and 30-day mortality among patients with status asthmaticus in Denmark: a 16-year nationwide population-based cohort study. Clin epidemiol. 2013;5:345–355. doi: 10.2147/CLEP.S47679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dales RE, Cakmak S, Judek S, et al. Influence of outdoor aeroallergens on hospitalization for asthma in Canada. J Allergy Clin Immunol. 2004;113(2):303–306. doi: 10.1016/j.jaci.2003.11.016. [DOI] [PubMed] [Google Scholar]
- 16.Gaspar AP, Morais-Almeida MA, Pires GC, et al. Risk factors for asthma admissions in children. Allergy Asthma Proc. 2002;23(5):295–301. [PubMed] [Google Scholar]
- 17.Bartter T, Pratter MR. Asthma: better outcome at lower cost? The role of the expert in the care system. Chest. 1996;110(6):1589–1596. doi: 10.1378/chest.110.6.1589. [DOI] [PubMed] [Google Scholar]
- 18.Lougheed MD, Garvey N, Chapman KR, et al. The Ontario asthma regional variation study: emergency department visit rates and the relation to hospitalization rates. Chest. 2006;129(4):909–917. doi: 10.1378/chest.129.4.909. [DOI] [PubMed] [Google Scholar]
- 19.Kercsmar CM, Dearborn DG, Schluchter M, et al. Reduction in asthma morbidity in children as a result of home remediation aimed at moisture sources. Environ Health Perspect. 2006;114(10):1574–1580. doi: 10.1289/ehp.8742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sin DD, Wells H, Svenson LW, Man SF. Asthma and COPD among aboriginals in Alberta, Canada. Chest. 2002;121(6):1841–1846. doi: 10.1378/chest.121.6.1841. [DOI] [PubMed] [Google Scholar]
- 21.Database: outdoor air pollution in cities. Public Health and Environment (PHE) http://www.who.int/phe/health_topics/outdoorair/databases/en/. Accessed 6 Jan 2014.
- 22.Tobacco Use in Canada: Patterns and Trends. 2013; http://www.tobaccoreport.ca/2013/TobaccoUseinCanada_2013.pdf. Accessed 24 Dec 2014.
- 23.Klomp H, Lawson JA, Cockcroft DW, et al. Examining asthma quality of care using a population-based approach. CMAJ. 2008;178(8):1013–1021. doi: 10.1503/cmaj.070426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cockcroft DW, Wensley D. Respirology manpower in Canada--a report for the Canadian thoracic society education committee. Can Respir J. 2000;7(6):451–455. doi: 10.1155/2000/704369. [DOI] [PubMed] [Google Scholar]
- 25.Halm EA, Wisnivesky JP, Leventhal H. Quality and access to care among a cohort of inner-city adults with asthma: who gets guideline concordant care? Chest. 2005;128(4):1943–1950. doi: 10.1378/chest.128.4.1943. [DOI] [PubMed] [Google Scholar]
- 26.Flores G, Snowden-Bridon C, Torres S, et al. Urban minority children with asthma: substantial morbidity, compromised quality and access to specialists, and the importance of poverty and specialty care. J Asthma. 2009;46(4):392–398. doi: 10.1080/02770900802712971. [DOI] [PubMed] [Google Scholar]
- 27.Gershon AS, Wang C, Guan J, Vasilevska-Ristovska J, Cicutto L, To T Identifying patients with physician-diagnosed asthma in health administrative databases. Can Respir J. 2009;16(6):183–188. doi: 10.1155/2009/963098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Aaron SD, Vandemheen KL, FitzGerald JM, et al. Reevaluation of diagnosis in adults with physician-diagnosed asthma. JAMA. 2017;317(3):269–279. doi: 10.1001/jama.2016.19627. [DOI] [PubMed] [Google Scholar]
- 29.Garcia E, Serban N, Swann J, Fitzpatrick A. The effect of geographic access on severe health outcomes for pediatric asthma. J Allergy Clin Immunol. 2015;136(3):610–618. doi: 10.1016/j.jaci.2015.01.030. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from CIHI but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Only the results of the analysis were made available to the authors as per CIHI policies.


