Abstract
Background:
Several methods have been used in wound closure for traumatic wounds, but it is not clear that which of these methods has more safety and efficacy. This study aimed to compare scar width due to standard and current treatments in wound repair by suturing and method of wound restoration using wound tape in patients with traumatic ulcers.
Materials and Methods:
This randomized clinical trial was done in ninety patients with wounds in the facial area. They were divided randomly into two groups of 45. The wounds in the first group were sutured, and wound tapes were used to wound closure in the second group. After 2 months, length and width of scar and results of life-size photography were recorded in a list, especially prepared for this purpose.
Results:
The mean age of the patients was 22.7 ± 12.9 years with 46 males (56.1%) and 36 females (43.9%). After 2 months, scars width in suture wound group was 2.9 mm and in wound tape group was 2.5 mm, with no statistically significant difference (P = 0.07). In patients with wound length of >20 mm, scars width was similar between groups and no significant differences was noted (P = 0.27), but in patients with wound length of <20 mm, scars width in wound tape group was significantly less than suture wound group (1.7 vs. 2.5 mm, respectively, P = 0.01). Wound complications were not significantly different between the two groups.
Conclusion:
Findings revealed that scar formation in wounds lower than 20 mm treated using wound tape was lower than suture, but for wounds between 20 and 50 mm were similar between wound tape and suture.
Keywords: Scar, suture, traumatic wound, wound tape
Introduction
Human are exposured to different types of skin injuries and complications that cause so much effort to be made by specialists to accelerate wound healing, prevent its complications, and remove scars.
The method of wound suturing has been one of the techniques that is time-consuming and is dependent on the person performing the technique although there is a risk of needle-stick injury in this method.[1,2]
Over the past years, researchers have found out that wound healing with suture in patients with cuts and injuries is faster and also the remaining scars is less in these people. Therefore, extensive research to discover mechanisms related to wound healing without scarring is ongoing and each year a new product is offered to the medical community based on this aim.
Wound closure using wound tape benefits from more advantages than closing the wound with suture, such as avoiding puncture in healthy skin and subsequent scar, also eliminating the risk of infection in point of entering and leaving the stitch needle and in dipping anesthetic syringe needle into the wound and separation of wound edges.[3]
Wound tape is even a simple and efficient way to stabilize the skin graft which has the capability of implementing in the emergency operating room and particularly in children.[4]
The main indication of use for these tapes is superficial wounds with low tension in the forehead, cheek, chin, chest, and other nonarticular parts of organs, especially in children.[5]
Wound tape is typically used in clinics, first-aid stations, emergency departments, and operation theaters. Benefits include ease of use, reducing the need for local anesthesia, equal distribution of wound tension, the lack of remaining stitches symptoms, minimal skin reaction, no need to remove the stitches, advantage over some grafts and flaps, and suitability for using in plaster mold. A major advantage of wound tape to standard suture is its more resistance to infection.[6,7]
A comprehensive study was done on several types of wound tapes, namely, Cicagraf, Curi-strip, Nichi-Strip, Suture Strip, and Steri-Strip to compare their elasticity bearing, adhesion strength, and wounds ventilation.
The highest ratings of performance belonged to the type of Steri-Strip (adhesive tape sample in this study).[8]
In experimental, ulcers inoculated with Staphylococcus aureus, closing the wound with Band-Aid has had better resistance to wound closure with suture by nylon thread.[9]
Healing ulcers with suture method in the anterior region of the leg in the elderly due to tissue atrophy is difficult, and using wound tape is an alternative method. In case of high tension in restored wound edges by suture, even after restoring wound and removing sutures, stitch tape can be used to reduce tension on the wound and subsequent scar alleviation.[10,11]
However, some researchers believe that wound healing results in better esthetic or cosmetic outcome using wound tape.[12]
Given, the importance of accelerating wound healing and its scar reduction, we decided to study the effect of implementing wound tape in ulcer closure and if its effectiveness is proved in wound healing and scar reduction, it can be used for dermal wound healing and prevention of scar emergence.
This study compares scar width due to standard and current treatments in wound healing by suturing and method of wound restoration using wound tape in patients with traumatic ulcers who are admitted to the Emergency Department of Al-Zahra and Kashani Hospitals in Isfahan.
Materials and Methods
This randomized clinical trial was done in the Emergency Department of Al-Zahra and Ayatollah Kashani Hospitals after obtaining permission from the Ethics Committee of Isfahan University of Medical Sciences. The statistical population included patients with traumatic wounds who were admitted to these medical and educational centers from June 2015 to June 2016. Inclusion criteria were defined as follows: simple traumatic wound, lesion length of <5 cm and depth of <0.5 cm without muscle involvement, do not require debridement, and <24 h from the time of their emergence. In addition, exclusion criteria were impossibility of patient follow-up at 4 weeks, underlying diseases such as diabetes and the ones related to the heart and kidney, known immune deficiency, severe malnutrition, atrophic wounds and scars caused by burns, multiple trauma, and wounds with high tension, irregular edges, and ones which are around the eyelids. Written informed consent was obtained from all studied patients.
In this study, ninety patients with traumatic facial wound area, whose information was concluded in the list and has been confirmed by the research council, were collected and then in a simple random method, they were placed in one of the two groups of wound tapes and suture. During sampling, patients were matched in both groups in terms of gender, the depth of the wound, the cause of lesion, and age were considered, and consent was provided for each of the test units to respect the moral context of plan. Patients were distributed into two groups of 45.
In suture group, the wounds were sutured after washing with normal saline solution under sterile conditions with 0.6 cut nylon stitches which have been manufactured in Supa Co, at a distance of 5 mm from each other, and 0.5 cm distance between entering and leaving of needle from the edges on both sides of the wound. Then, the wound was dressed, and sutures were removed after 5 days. Required training for wound care with an emphasis on lack of exposure to sunlight and using protection was recommended. Returning for visit 4 weeks after treatment was also suggested.
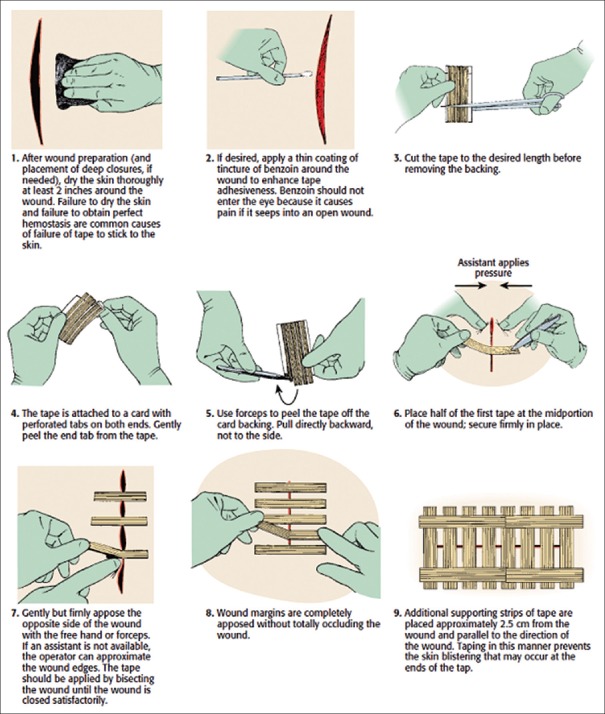
In wounds tapes group, at first, the wound with normal saline solution was washed and after ensuring the lack of deep tissue involvement and bleeding control, wound around a radius of at least 2 inches (5 cm) was perfectly cleaned and dried with sterile gauze. Then, a thin coating of benzoin tincture around the wound is created by swab in such a way that benzene does not enter the wound. After that, the right size of tape was measured before removing the protective layer and then was cut with scissors. The protective layer of tape was removed from one side briefly. Then, the tape was removed completely from the protective layer by forceps while an individual closed two side edges of the wound up of and the tape was adhered tightly to the middle of wound vertically.
Taping was continued to the required extent gently and firmly in a periodic and divergent way from the middle of wound. While taping, the edges of the wound were closed together perfectly. For the more adhesive strength, another wound tape was fixed which was perpendicular to the ulcer at a distance of 2.5 cm, parallel with the two sides of the wound (if we were worried about tampering wound tapes by children, the whole restored area could be dressed with sterile gauze). After 5 days, tape was removed from the wound and required training for wound care with an emphasis on the lack of exposure to sunlight and using the protection and referring after 4 weeks of treatment was recommended.
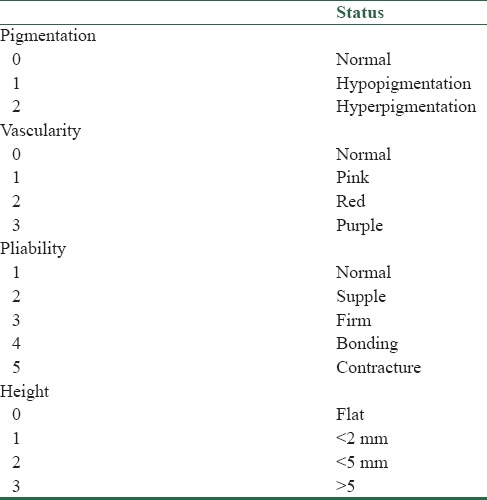
After intervention, all wounds in both groups were placed under 16 MP camera photography from a distance of approximately 10 cm. Wound condition, healing, and scar were compared by using those photographs. Examined scar in this research was hypertrophic one, and condition investigation of wound was done by Vancouver criteria. Other information such as age, sex, cause of ulcers, ulcer size, depth, and location of wound in the two groups was also specified and recorded in the questionnaire.
Possible complications included the opening wound tape that in case of occurrence, another tape was provided for the patient [Table 1]. Furthermore, in case of local infection for patients, antibiotic therapy and required measures follow-ups were done to them.
Table 1.
The measuring outcomes
The sample size was calculated using the comparison of means formula with the two-sided log-rank test, α = 0.05, and 80% power. The required information including demographic information, the wound-related data as well as length and width of scar and results of life-size photography were recorded in a list especially prepared for this purpose. In the end, the mentioned outcomes were compared and analyzed by using SPSS version 23 (Chicago, IL, USA) software and implementing tests containing Student's t-test, Chi-square, and Mann–Whitney's U-test [Figure 1].
Figure 1.
Wound tape application
Results
Of 108 screened patients for eligibility, 18 patients were not eligible or refused informed consent and did not enter to the study. Ninety eligible patients randomly assigned into two intervention groups of wound tape or suture wound. During 1-month follow-up period five patients in suture wound group and three patients in wound tape group were lost (six patients did not return, and two patients did not desire to continue). Finally, 82 patients completed the study and analyzed (40 patients in suture wound group and 42 in wound tape group) [Figure 2]. The mean of age in studied patients was 22.7 ± 12.9 years. Forty-six patients (56.1%) were male, and 36 patients (43.9%) were female. Table 2 shows baseline characteristics of studied patients calculated by independent sample t-test or Chi-square test. Age, sex, wounds’ site and size were similar between groups, and no statistical significance was noted (P > 0.05).
Figure 2.
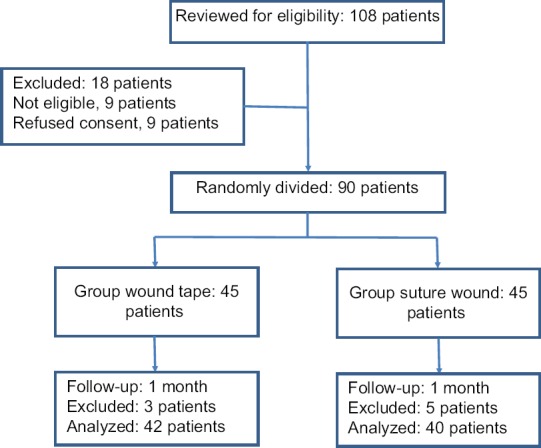
Flowchart of the study, patients who entered to the study, divided into the study groups and analyzed
Table 2.
Baseline characteristics between studied groups
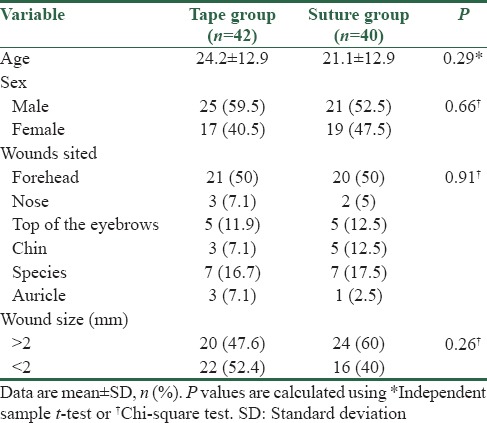
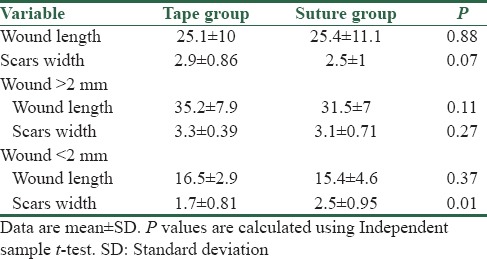
Table 3 shows comparison of wound length at baseline and scars width after 2 months between intervention groups using independent sample t-test. Wound length at baseline was similar between groups, and no significant differences were noted (25.1 mm in suture wound group versus 25.4 mm in wound tape group, P = 0.88). After 2 months scars width in suture wound group was 2.9 mm and in wound, tape group was 2.5 mm. The differences between groups were not statistically significant (P = 0.07). In patients whose wound length was more than 20 mm, scars width was similar between groups, and no significant differences were noted (P = 0.27); however in patients with wound length lower than 20 mm, scars width in wound tape group was significantly less than suture wound group (1.7 vs. 2.5 mm, respectively, P = 0.01).
Table 3.
Comparison of wound length and scars width between groups
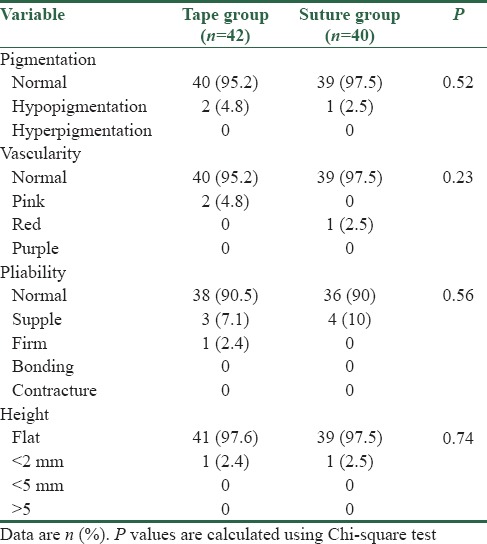
Wound complications were not significantly different between the two groups [Table 4]. Wound infection was not occurred in studied patients. Pigmentation in most of the patients was normal, and only two patients in wound tape group and one patient in suture group had hypopigmentation. Vascularity in most of the patients was normal, in two patients of wound tape group was pink, and in one patient of suture group was red. Pliability in wound tape group in 38 patients was normal, in three patients was supple, and in one patient was firm, whereas in suture group in 36 patients was normal, and in four patients was supple. Height on wound in two patients in both groups was lower than 2 mm, and in other patients was flat.
Table 4.
Comparison of wound complications between groups
Discussion
In Iran, most of the governmental hospitals are faced with crowding in the emergency department. Patients and medical personnel in the emergency department are suffering from crowding, and their satisfactions would be decreased due to long waiting times, increased pain-exposure time for patients, increased potential for violence against medical personnel, and increased burnout of medical personnel. Hence, strategies that can be used for reducing emergency department crowding are notable for hospital managers.
The main common medical care seeks by the people that emergency medicine providers are faced with its traumatic wounds.[1] To treat the traumatic wound, physicians and patients influence the decisions on wound closure techniques.[2] Beside the cost-effective, time-efficient and easy to perform of a wound closure method, this should be the optimal cosmetic result. Cosmetic results are naturally important to most patients, and all patients should be counseled on this aspect of wound healing.[3] All wounds will contract and form scar tissue, and scars are represented an abnormal and exaggerated healing response after skin injury.[4] In the present study, two methods of wound closures included suturing and wound tape, were assessed in regard to scar formation. In this study, wounds lower than 50 mm of length were selected, and our finding shows that after 2 months, scars width was not significantly different between the two methods. When scars width was assessed among patients who their wound length was lower than 20 mm, wound tape was more effective than suture.
The correct choice of wound closure technique is important. For all traumatic wound, there is no perfect wound closure technique that would be suitable. The closure of any traumatic wound should take into account the site and the tissues involved.[12,13] The result of the present study beside to the similar findings can be useful as a strategy to manage some cause of the emergency department crowding. Because, by the use of wound tape in traumatic wound <50 mm in emergency department instead of suture, satisfaction would be increased in patients and medical personnel. Some of these advantages that have positive effects on patients and medical personnel satisfaction and reduction of the emergency department crowding are easy to perform, decrease in length of stay in emergency department, less use of medical facilities, and lower costs to patients and systems.
The previous studies show different result in comparing the different methods of wounds closure. In a randomized controlled trial, cosmetic results were similar with reduced cost using adhesive tape closure than with tissue glue in facial lacerations in children.[5] In another study, similar cosmetic results were reported in octylcyanoacrylate method in comparison to suture closure.[6] In Wang et al. study, the results of cosmetic demonstrated that skin tape reduced scar formation as well as silicone gel in the rabbit model.[7] Some other studies show that the early cosmetic outcome of wound closed by adhesive tapes is significantly better than sutured wounds, whereas three studies support this and reported that patients who treated with adhesive tape were more satisfied with the results in comparison to sutured wounds.[8,9,10] Many studies showed that initial cosmetic outcome in adhesive tapes was better, but delayed scar widening was not significantly different between sutured wounds and adhesive tapes.[6,11,14,15] Findings of the present study show that wound tape in comparison to suture in wounds <20 mm was more effective in scar formation, but in wound <50 mm was similar to suture. Hence, these show that wound tape can be used as a suitable wound closure technique in wounds <20 mm. In addition, despite the fact that in wound <50 mm no differences was noted between wound tape and suture in this study, cost-effective, time-efficient, and easy to perform suggests that wound tapes can be used as an alternative to suture for traumatic wound <50 mm by emergency physicians. As shown in the previous studies, data about the comparison of scar formation in traumatic wounds between wound tape and suture in facial wounds lower than 50 mm have been reported with different results. Some studies were comparable with our study, and some other studies were dissimilar, although differences in the methods of wound closure, studied populations, kind of wounds, and wounds areas and locations can be noted as possible causes of differences in results of reported studies.
The present study has some limitations. First, our study was limited to traumatic wounds on the face, so our findings are limited to generalize to other wounds and other body areas and locations. Second, the mean length of wounds short and was limited to wounds lower than 50 mm so generalize the results to longer wounds is difficult. Third, blinding was not possible, and patients such as the providers who closed the wounds were not masked to the closure technique.
Conclusion
This study evaluated wound outcomes of traumatic wounds closed with a wounds tape or suture, and our findings show that wound tape was more effective than suture in scar formation when it used for wound lower than 20 mm but was similar to suture when it used for wound between 20 and 50 mm. Hence, because of many advantages of wound tapes such as simple to use, time-efficient, and cost-effective, this can be good choice for traumatic wounds to decrease scar formation. However, further randomized trials are required to validate these findings and compare wound tape and suturing of traumatic wounds with regard to scar formation.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Singer AJ, Thode HC, Jr, Hollander JE. National trends in ED lacerations between 1992 and 2002. Am J Emerg Med. 2006;24:183–8. doi: 10.1016/j.ajem.2005.08.021. [DOI] [PubMed] [Google Scholar]
- 2.Flynn D, Knoedler MA, Hess EP, Murad MH, Erwin PJ, Montori VM, et al. Engaging patients in health care decisions in the emergency department through shared decision-making: A systematic review. Acad Emerg Med. 2012;19:959–67. doi: 10.1111/j.1553-2712.2012.01414.x. [DOI] [PubMed] [Google Scholar]
- 3.Quinn JV, Polevoi SK, Kohn MA. Traumatic lacerations: What are the risks for infection and has the ‘golden period’ of laceration care disappeared? Emerg Med J. 2014;31:96–100. doi: 10.1136/emermed-2012-202143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Singer AJ, Hollander JE, Valentine SM, Turque TW, McCuskey CF, Quinn JV. Prospective, randomized, controlled trial of tissue adhesive (2-octylcyanoacrylate) vs standard wound closure techniques for laceration repair. Stony Brook Octylcyanoacrylate Study Group. Acad Emerg Med. 1998;5:94–9. doi: 10.1111/j.1553-2712.1998.tb02590.x. [DOI] [PubMed] [Google Scholar]
- 5.Zempsky WT, Parrotti D, Grem C, Nichols J. Randomized controlled comparison of cosmetic outcomes of simple facial lacerations closed with Steri Strip Skin Closures or Dermabond tissue adhesive. Pediatr Emerg Care. 2004;20:519–24. doi: 10.1097/01.pec.0000136068.45198.ae. [DOI] [PubMed] [Google Scholar]
- 6.Toriumi DM, O’Grady K, Desai D, Bagal A. Use of octyl-2-cyanoacrylate for skin closure in facial plastic surgery. Plast Reconstr Surg. 1998;102:2209–19. doi: 10.1097/00006534-199811000-00062. [DOI] [PubMed] [Google Scholar]
- 7.Wang CC, Cherng JH, Chen SG, Huang TW, Lin LC, Pan RY, et al. A comparative study evaluating the clinical efficacy of skin tapes versus silicone gel for the treatment of posttrauma scar in the rabbit model. J Med Sci. 2014;34:195. [Google Scholar]
- 8.Lazar HL, McCann J, Fitzgerald CA, Cabral HJ. Adhesive strips versus subcuticular suture for mediansternotomy wound closure. J Card Surg. 2011;26:344–7. doi: 10.1111/j.1540-8191.2011.01257.x. [DOI] [PubMed] [Google Scholar]
- 9.Gkegkes ID, Mavros MN, Alexiou VG, Peppas G, Athanasiou S, Falagas ME. Adhesive strips for the closure of surgical incisional sites: A systematic review and meta-analysis. Surg Innov. 2012;19:145–55. doi: 10.1177/1553350611418989. [DOI] [PubMed] [Google Scholar]
- 10.Kuo F, Lee D, Rogers GS. Prospective, randomized, blinded study of a new wound closure film versus cutaneous suture for surgical wound closure. Dermatol Surg. 2006;32:676–81. doi: 10.1111/j.1524-4725.2006.32140.x. [DOI] [PubMed] [Google Scholar]
- 11.Rothnie NG, Taylor GW. Sutureless skin closure. A clinical trial. Br Med J. 1963;2:1027–30. doi: 10.1136/bmj.2.5364.1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Al-Mubarak L, Al-Haddab M. Cutaneous wound closure materials: An overview and update. J Cutan Aesthet Surg. 2013;6:178–88. doi: 10.4103/0974-2077.123395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ghazizadeh Hashemi SA, Barati B, Mohammadi H, Saeidi M, Bahreini A, Kiani MA. Effect of topical estrogen in the mangement of traumatic facial wounds. Iran J Otorhinolaryngol. 2016;28:45–9. [PMC free article] [PubMed] [Google Scholar]
- 14.Kochar MP, Singh SP. Incised surgical wound closure with sutures and staples: A controlled experimental study. Int Surg J. 2015;2:369–72. [Google Scholar]
- 15.Abdus-Salam RA, Bello FA, Olayemi O. A randomized study comparing skin staples with subcuticular sutures for wound closure at caesarean section in black-skinned women. Int Sch Res Notices. 2014;2014:807937. doi: 10.1155/2014/807937. [DOI] [PMC free article] [PubMed] [Google Scholar]