Abstract
Background:
Several studies have reported that mindfulness meditation has a potential effect in controlling headaches, such as migraine and tension-type headache; however, its role remains controversial. This review assessed the evidence regarding the effects of mindfulness meditation for primary headache pain.
Methods:
Only English databases (PubMed, Cochrane Central Register of Controlled Trials [the Cochrane Library], PsycINFO, Psychology and behavioral science collection, PsyArticles, Web of Science, and Scopus) were searched from their inception to November 2016 with the keywords (“meditation” or “mindfulness” or “vipassana” or “dzogchen” or “zen” or “integrative body-mind training” or “IBMT” or “mindfulness-based stress reduction” or “MBSR” or “mindfulness-based cognitive therapy” or “MBCT” and “Headache” or “Head pain” or “Cephalodynia” or “Cephalalgia” or “Hemicrania” or “Migraine”). Titles, abstracts, and full-text articles were screened against study inclusion criteria: controlled trials of structured meditation programs for adult patients with primary headache pain. The quality of studies included in the meta-analysis was assessed with the Yates Quality Rating Scale. The meta-analysis was conducted with Revman 5.3.
Results:
Ten randomized controlled trials and one controlled clinical trial with a combined study population of 315 patients were included in the study. When compared to control group data, mindfulness meditation induced significant improvement in pain intensity (standardized mean difference, −0.89; 95% confidence interval, −1.63 to −0.15; P = 0.02) and headache frequency (−0.67; −1.24 to −0.10; P = 0.02). In a subgroup analysis of different meditation forms, mindfulness-based stress reduction displayed a significant positive influence on pain intensity (P < 0.000). Moreover, 8-week intervention had a significant positive effect (P < 0.000).
Conclusions:
Mindfulness meditation may reduce pain intensity and is a promising treatment option for patients. Clinicians may consider mindfulness meditation as a viable complementary and alternative medical option for primary headache.
Keywords: Headache Pain, Meta-Analysis, Mindfulness Meditation
摘要
背景:
已有文献报道正念冥想对诸如偏头痛、紧张性头痛等原发性头痛有潜在治疗作用,但是其确切效果仍有争议。因此本文主要为正念冥想治疗原发性头痛提供循证医学依据。
方法:
本文检索2016年11月之前的英文数据库(PubMed, Cochrane Central Register of Controlled Trials [the Cochrane Library], PsycINFO, Psychology and behavioral science collection, PsyArticles, Web of Science, Scopus),关键词是”meditation”或”mindfulness”或”vipassana”或”dzogchen”或”zen”或”integrative body-mind training”或”IBMT”或”mindfulness-based stress reduction”或”MBSR”或”mindfulness-based cognitive therapy”或”MBCT”与”Headache”或”Head pain”或”Cephalodynia”或”Cephalalgia”或”Hemicrania”或”Migraine”。然后依据纳入标准(对原发性头痛的成年患者行结构化冥想程序的对照试验研究)对标题、摘要和全文进行筛选。接着采用Yates质量评估量表评价文献质量,并运用Revman 5.3软件进行Meta分析。
结果:
一共纳入10篇随机控制试验、1篇临床对照试验和315名患者。与对照组比较发现,正念冥想可以显著减弱头痛的强度[SMD =-0.89, 95% CI (-1.63, -0.15), P = 0.02]和频率[SMD =-0.67, 95% CI (-1.24, -0.1), P = 0.02]。对不同正念形式进行亚组分析发现,正念减压(MBSR)和为期8周的干预对头痛强度有积极的改善(P < 0.000)。
结论:
正念冥想可以减弱原发性头痛强度,是一个有前景的治疗选择。临床医生可以考虑将正念冥想作为治疗原发性头痛的一个补充替代医学选择。
INTRODUCTION
Headache is one of the most common disorders of the nervous system and several subtypes such as tension-type headache (TTH) and migraine remain underrecognized and undertreated.[1] Since 1990, headache has ranked among the top three diseases among the several hundred contributors to the global burden of disease.[2] In the Asia-Pacific region, the median 1-year prevalence of primary headache such as migraine and TTH were 9.1% and 16.2%, respectively.[3] In Europe, the prevalence of TTH and migraine were 60% and 15%, respectively.[4] Prolonged use of medication (such as caffeine, aminopyrine, phenacetin, and phenobarbital) may lead to medication-overuse headache and other side effects.[5,6] Besides biofeedback treatment,[7,8,9] biopsychosocial interventions such as mindfulness meditation have been used to treat headache due to their high cost-effectiveness and fewer side effects.[10,11,12,13]
Meditation is defined as a form of mental training that aims to improve an individual's core psychological capacities, such as attentional and emotional self-regulation. There are three core components of meditation practice as follows: attention control, emotion regulation, and self-awareness.[14] Meditative techniques include transcendental meditation, mindfulness-based stress reduction (MBSR), and mindfulness-based cognitive therapy (MBCT).[15] Transcendental meditation emphasizes the use of a mantra by which one is transcended to an effortless state in which focused attention is absent.[16] MBSR focuses on the training in awareness or mindfulness that focuses on the present.[16] MBCT has been used to prevent relapse of major depression.[15] Although several studies have investigated the use of meditative techniques for treatment of headache, the intensity, frequency, and duration of headache in the respective study populations have tended to vary.[17,18,19,20]
Therefore, the purpose of this meta-analysis was to assess evidence regarding the effectiveness of meditation programs in dealing with primary headache and associated clinical outcomes and to determine whether meditation programs are a viable complementary and alternative medical therapeutic option for primary headaches.
METHODS
Database and literature search strategy
We searched the literature in the following databases: PubMed, Cochrane Central Register of Controlled Trials (the Cochrane Library), PsycINFO, Psychology and behavioral science collection, PsyArticles, Web of Science, and Scopus from inception to November 2016. Key words used for the search were “meditation” or “mindfulness” or “vipassana” or “dzogchen” or “zen” or “integrative body-mind training” or “IBMT” or “mindfulness-based stress reduction” or “MBSR” or “mindfulness-based cognitive therapy” or “MBCT” in combination with “Headache” or “Head pain” or “Cephalodynia” or “Cephalalgia” or “Hemicrania” or “Migraine.” These searches were limited to English publications. All potentially relevant studies, articles (including undocumented data and meta-analyses), and international guidelines were searched manually. The eligibility of identified citations was independently reviewed by two reviewers. An example of search strategy was shown as Supplementary File 1 (1.2MB, tif) .
Example of search strategy
Selection procedure and eligibility criteria
Inclusion criteria were as follows: (1) age 18 or older with primary headache (mainly, migraine or TTH) according to the diagnostic criteria of the International Headache Classification Subcommittee; (2) randomized controlled trials or controlled clinical trials for whom full text were available; (3) intervention of interest: structured meditation programs (any systematic or protocol meditation programs that follow predetermined curricula) including mindfulness-based programs (i.e., MBSR, MBCT, vipassana, Zen, and other mindfulness meditation), mantra-based programs (i.e., transcendental meditation, other mantra meditation), and other meditation programs; (4) comparison: relaxation, education, usual pharmacotherapy, delayed treatment, or wait-list. Exclusion criteria were as follows: additional diseases that might interfere with the primary headache such as human immunodeficiency virus-related pain, cancer pain, seizures, facial neuralgia, significant cognitive impairment, schizophrenia, bipolar affective disorder, and current substance abuse. No limitations of race, religion, or gender of the study population were imposed. Studies were independently screened by two investigators. All analyses were based on previously published studies, thus no ethical approval and patient consent were required. This study conforms to all preferred reporting items for systematic reviews and meta-analyses guidelines and reports the required information accordingly.
Data extraction and quality assessment
The following data were obtained: study characteristics (e.g., author, year, and country); patient characteristics (e.g., age and sample size); description of interventions and duration, and outcomes measured. Primary outcomes were headache intensity, frequency, and duration. Headache intensity reflected self-assessed headache severity according to numeric rating scales. Headache frequency and duration were defined as the days of headache attacks per unit of time and the duration of the attack, respectively. Quality of life, self-efficacy, pain tolerance, and perceived stress were secondary outcomes. Two reviewers independently extracted these data using predefined criteria. Primary authors of the selected publications were contacted when the relevant information was not reported. The Yates Quality Rating Scale (YQRS) was used to assess the quality of psychological trials for chronic pain.[21] The Yates Scale of 35 scores is composed of 26 items including specific psychological interventions such as the assessment of therapist training and treatment expectation. This scale is deemed to have good construct validity and reliability. A percentage was calculated from the final score so that trials could be compared. A Cochrane review used the midpoint (score of 18) as the divider between a “high-quality” and “low-quality” study.[22] Therefore, in this meta-analysis, a score ≥50% was deemed to have low risk of bias and a score ≤49% was deemed to have high risk of bias. Studies of low quality were also displayed in the results. Data from each included article were extracted independently by two investigators. In cases where a consensus could not be reached, the opinion of a third independent investigator was sought.
Statistical analysis
All variables were analyzed using the standardized mean difference (SMD) and 95% confidence interval (CI). SMD was calculated with Hedge's g formula. Heterogeneity was assessed by Cochrane's Q statistic (P < 0.10 was considered to be statistically significant) and was quantified by the I2 index (I2 >30%, >50%, and >75% indicate moderate, substantial, and considerable heterogeneity, respectively). Then, we undertook a conservative random-effect meta-analysis. To explore sources of heterogeneity, subgroup analysis was performed according to different meditation forms (standard and nonstandard MBSR), training durations, headache types, and different control groups. Control groups such as pharmacotherapy, wait-list, and delayed treatment were combined to one comparator as these were all passive controls. In contrast, the relaxation and education groups were deemed as active controls. Publication bias was not assessed due to the limited number of studies. A value of P < 0.05 was considered as statistically significant. All statistical analyses were performed using Revman 5.3 (Cochrane Collaboration).
RESULTS
Included studies
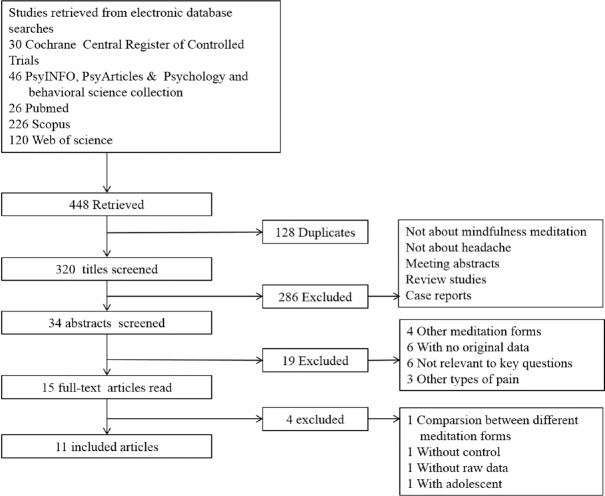
As shown in Figure 1, 448 articles were identified from five databases. Of these, 128 were duplicates. From the remainder, 286 articles were excluded through title screening, and 19 articles were excluded by abstract screening. After the review of 15 full-text articles, 11 studies met the eligibility criteria for this study.
Figure 1.
Flow diagram of study selection.
The characteristics of the included studies are summarized in Table 1. Of the 11 eligible studies, four studies were conducted in the United States,[11,12,17,23] three in Australia,[13,20,24] three in Iran[10,25,26] and one in India.[27] In 10 studies, the mean age of patients ranged from 30 to 45 years; in one study, the mean age of patients was 19.1 years.[11] The studied subtypes of headache included migraine (1 study),[17] TTH (7 studies),[10,13,20,23,24,25,27] and migraine mixed with TTH (three studies, of which one focused on migraine).[11,12,26] Control groups included the usual pharmacotherapy (three studies),[10,25,26] wait-list (five studies),[13,17,20,24,27] delayed treatment (1 study),[12] relaxation (one study),[11] and education (one study) groups.[23] The usual groups were on standard pharmacotherapy. The wait-list group as well as the delayed treatment group received the treatment after the active treatment group was treated. The relaxation group received progressive muscle relaxation. The educational group received education from a neurologist who specialized in headache and pain management. Interventional methods included standard MBSR,[10,17,20,24,25,26] MBCT,[12] brief mindfulness-based therapy,[13] mindfulness meditation,[23,27] and different meditations within subgroups,[11] most of which were combined with additional homework [Table 1]. An interventional form of transcendental meditation was not found on literature search. Sample size was calculated only in five studies, of which four were adequately powered to detect an effect [Table 2]. The other six studies were feasibility or pilot studies.
Table 1.
Characteristics of included studies
| Sources | Design | Pain | Yate Quality Score (range 0–35) | Mean age (SD), years | Male (%) | Sample size | Attrition rate (%) | Intervention group | Control group | Outcome measures |
|---|---|---|---|---|---|---|---|---|---|---|
| Omidi 2014, Iran | RCT | TTH | 20/35 (57%) | I: 34.5 (2.4) C: 32 (3.2) | 20 | 60 | I: 9.1 C: 9.1 | MBSR, 8 weekly sessions, each 2 h | Medication and clinical management | Headache severity Mindfulness awareness |
| Omidi 2015, Iran | RCT | TTH | 21/35 (60%) | I: 34.5 (2.4) C: 32 (3.2) | 20 | 60 | I: 9.1 C: 9.1 | MBSR, 8 weekly sessions, each 2 h | Medication and clinical management | Psychological symptom Perceived stress |
| Wachholtz 2008, United States | RCT | Migraine and TTH | 22/35 (62%) | 19.1 (1.1) | 9.6 | 83 | I: 10 C: 9.1 | Spiritual or internal secular or external secular meditation, 20 min/day for 30 days | Relaxation | Headache frequency and severity Pain tolerance Affect, anxiety, depression Quality of life Self-efficacy Spirituality |
| Rosdahl 2003, United States | RCT | TTH | 26/35 (74%) | 36.4 (13) | 21.8 | 64 | Not mention | Mindfulness meditation, 8 weekly sessions, each 2 h and 10–15 min a day at home | Education class | Perceived stress Time pressure Headache intensity and duration Spirituality sIgA in saliva |
| Day 2014, United States | RCT | Migraine (86.1%), TTH (11.1%), new daily persistent headache (2.8%) | 23/35 (65%) | 41.7 (12.0) | 11.1 | 24 | I: 52.6 C: 11.7 | MBCT, 8 weekly sessions, 2 h each and homework 45 min, 6 days per week | DT | Headache frequency, duration and intensity Pain severity and pain interference Pain catastrophizing Mindfulness Pain acceptance Self-efficacy Self-efficacy |
| Bakhshani 2015, Iran | RCT | Primary migraine, TTH | 16/35 (45%) | I: 30.6 (9.1) C: 31.5 (9.5) | 32.5 | 37 | I: 15 C: 0 | MBSR, 8 weekly sessions, each 1.5–2 h | Usual pharmacotherapy | Pain intensity, frequency, and duration A short-form 36 questionnaire |
| Wells 2014, United States | RCT | Migraine | 25/35 (71%) | I: 45.9 (17) C: 45.2 (12) | 11 | 19 | I: 0 C: 0 | MBSR, 8 weekly sessions, each 2 h plus 1 mindfulness retreat day (6 h) and daily practice for 45 min, at least 5 additional days per week | Wait-list | Headache frequency, duration and intensity Headache-related disability Migraine disability assessment Quality of life Depression, anxiety Perceived stress Mindfulness Self-efficacy |
| Cathcart 2014, Australia | RCT | Chronic TTH | 22/35 (62%) | I: 45.7 (13.1) C: 45.2 (14.1) | I: 43 C: 31.5 | 42 | I: 20.6 C: 34.4 | Mindfulness based therapy, 6 sessions, 3 weeks, | Wait-list | Headache frequency, duration, and intensity Depression, anxiety, stress |
| twice a week, each 2 h and homework 30 min per day | ||||||||||
| Cathcart 2013 (a, b), Australia | RCT | Chronic TTH | 16/35 (45%) | 45.5 (13.8) | 37 | 43 | Not mention | MBSR, six 1-h group class, twice per week, for 3 weeks, 30 min daily home practice | Wait-list | (a) Muscle tenderness Pressure pain detection threshold Cold pressor test Conditioned pain modulation (b) Inflammatory cytokines |
| Kiran 2014, India | CCT | Chronic TTH | 17/35 (48.5%) | 32.06 (9.43) | 22 | 50 | I: 14.2 C: 42.8 | Rajyoga meditation, 45 min per lesson, 8 lessons, twice a week, for 4 weeks | Wait-list | Headache frequency, duration, and intensity |
RCT: Randomized controlled trial; CCT: Controlled clinical trial; TTH: Tension-type headache; MBSR: Mindfulness-based stress reduction; MBCT: Mindfulness-based cognitive therapy; DT: Delayed treatment.
Table 2.
Yates quality rating of enrolled studies
| Items | Omidi 2014 | Omidi 2015 | Wachholtz 2008 | Rosdahl 2003 | Day 2013 | Bakhshni 2015 | Wells 2014 | Cathcart 2014 | Cathcart 2013 (a, b) | Kiran 2014 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Treatment quality | |||||||||||
| Treatment content and setting | 0, 1, 2 | 2 | 2 | 2 | 2 | 1 | 1 | 2 | 2 | 2 | 2 |
| Treatment duration | 0, 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Manualization | 0, 1, 2 | 0 | 0 | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 0 |
| Adherence to manual | 0, 1 | 0 | 0 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 0 |
| Therapist training | 0, 1, 2 | 0 | 0 | 1 | 2 | 2 | 0 | 2 | 1 | 1 | 1 |
| Patient engagement | 0, 1 | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 0 | 1 |
| Quality of study design and methods | |||||||||||
| Sample criteria | 0, 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Evidence criteria met | 0, 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Attrition | 0, 1, 2 | 1 | 2 | 2 | 1 | 1 | 1 | 0 | 1 | 0 | 1 |
| Rates of attrition | 0, 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Sample characteristics | 0, 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 0 |
| Group equivalence | 0, 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 |
| Randomization | 0, 1, 2 | 2 | 2 | 2 | 2 | 2 | 1 | 1 | 1 | 1 | 0 |
| Allocation bias | 0, 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 1 | 1 | 0 |
| Measurement bias | 0, 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 |
| Treatment expectations | 0, 1 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 |
| Justification of outcomes | 0, 1, 2 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 2 | 1 | 1 |
| Validity of outcomes for context | 0, 1, 2 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Reliability and sensitivity to change | 0, 1, 2 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Follow-up | 0, 1 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 |
| Power calculation | 0, 1 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 0 | 0 | 0 |
| Sufficient sample size | 0, 1 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 |
| Planned data analysis | 0, 1 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 0 | 1 |
| Statistics reporting | 0, 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Intention-to-treat analysis | 0, 1 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 |
| Control group | 0, 1, 2 | 2 | 2 | 1 | 2 | 2 | 1 | 2 | 1 | 1 | 1 |
| Total score/35 | 20 | 21 | 22 | 26 | 23 | 16 | 25 | 22 | 16 | 17 | |
Based on the clinical or psychosocial characteristics, the outcomes were divided into clinical and humanistic outcomes. The clinical outcomes reported in these studies were headache intensity (seven studies), headache frequency (five studies), headache duration (four studies), and pain tolerance (two studies). Humanistic outcomes measured in the studies included mindful awareness in four studies, perceived stress in three studies, quality of life in two studies, and self-efficacy in two studies [Supplementary Files 2 (434.2KB, tif) -4].
Supplementary File 4.
Outcomes measured within included studies
| Omidi 2014 | Omidi 2015 | Wachholtz 2008 | Rosdahl 2003 | Day 2013 | Bakhshani 2015 | Wells 2014 | Cathcart 2014 | Cathcart 2013 (a, b) | Kiran 2014 | |
|---|---|---|---|---|---|---|---|---|---|---|
| Clinical outcomes associated with pain | ||||||||||
| Pain intensity | √ | √ | √ | √ | √ | √ | √ | |||
| Headache frequency | √ | √ | √ | √ | √ | √ | ||||
| Headache duration | √ | √ | √ | √ | √ | √ | ||||
| Pain tolerance | √ | √ | ||||||||
| Muscle tenderness | √ | |||||||||
| Pressure pain detection threshold | √ | |||||||||
| Conditioned pain modulation | √ | |||||||||
| sIgA in saliva | √ | |||||||||
| Inflammatory cytokines | √ | |||||||||
| Outcomes associated with psychiatric symptoms | ||||||||||
| Pain interference | √ | |||||||||
| Headache-related disability | √ | |||||||||
| Psychological symptoms | √ | |||||||||
| Affect | √ | |||||||||
| Anxiety | √ | √ | ||||||||
| Depression | √ | √ | ||||||||
| Humanistic outcomes | ||||||||||
| Mindful awareness | √ | √ | √ | √ | ||||||
| Perceived stress | √ | √ | √ | |||||||
| Quality of life | √ | √ | √ | |||||||
| Self-efficacy | √ | √ | √ | |||||||
| Religious intensity | √ | |||||||||
| Spiritual well-being | √ | |||||||||
| Spiritual experiences | √ | √ | ||||||||
| Time pressure | √ | |||||||||
| Pain catastrophizing | √ | |||||||||
| Pain acceptance | √ | |||||||||
The tick means that the parameter was tested.
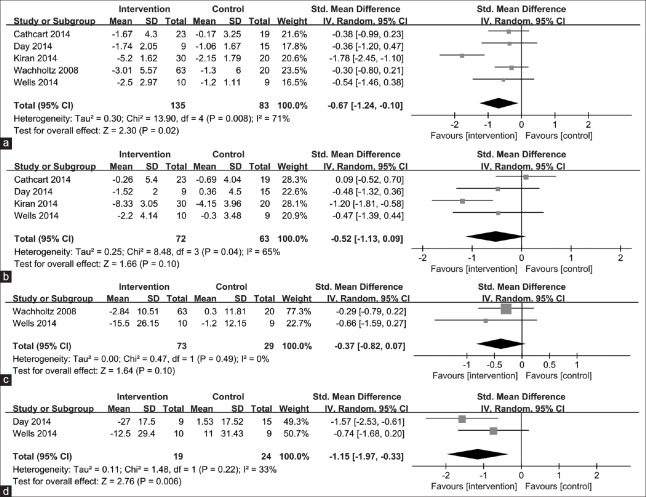
Forest plots of meta-analysis data for pain tolerance (a) and perceived stress (b). Effect sizes overlapped with zero reflect no significant difference between mindfulness meditation and control groups. Summary statistics were computed via random effects meta-analysis.
Subgroup analysis of pain intensity according to different items: (a) different types of headaches, (b) different ages and (c) different control groups.
Study quality and risk of bias
The YQRS score of inclusive studies varied from 16 to 26 points. Seven out of the eleven publications were graded as being at low risk of bias (57–74%), and the remainders were ranked as being at high risk of bias (45% and 48.5%). Quality criteria that these studies did not meet included measurement bias (eight studies), treatment expectations (nine studies), follow-up (eight studies), intention-to-treat analysis (10 studies), and sufficient sample size (seven studies). The quality rating for each study is displayed in Table 2.
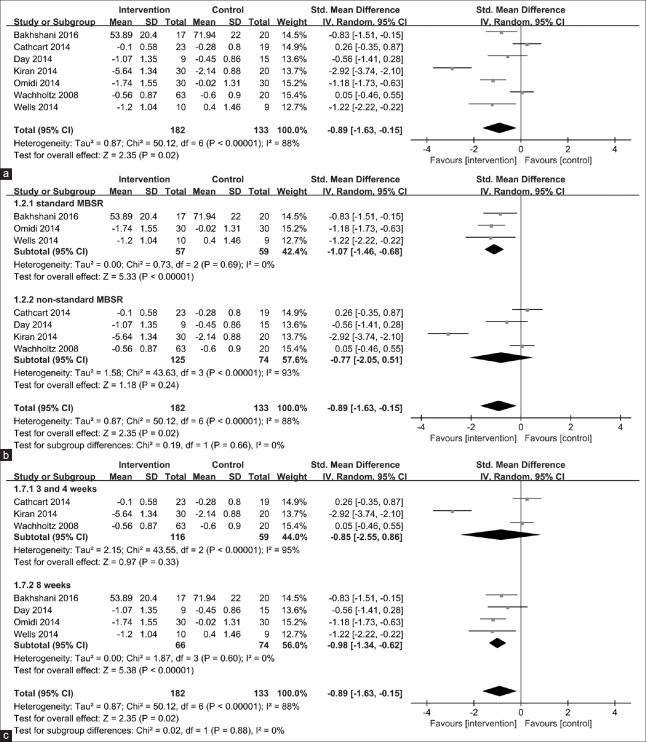
Heterogeneity was substantial for pain intensity (I2 = 88%, P < 0.000) [Figure 2a]. We found that heterogeneity was resolved (I2 = 0%, P = 0.69) [Figure 2b] when only studies that used standard MBSR meditation forms were included in the analysis. Moreover, we found that heterogeneity was resolved (I2 = 0%, P = 0.6) [Figure 2c] when the intervention duration lasted for 8 weeks. For self-efficacy, heterogeneity was moderate (I2 = 33%, P = 0.22) with a small sample size [Figure 3d].
Figure 2.
Forest plots of meta-analysis data for headache intensity. (a) Forest plot of headache intensity in headache patients and controls; (b) subgroup analysis for headache intensity according to standard and non-standard MBSR; (c) subgroup analysis headache intensity with different types of headache. Effect sizes to the left of zero reflect greater mindfulness meditation-induced headache relief. Confidence intervals that do not include zero reflect significant differences. Summary statistics were computed via random effects meta-analysis.
Figure 3.
Forest plots of meta-analysis data for headache frequency (a), duration (b), quality of life (c), and self-efficacy (d). Effect sizes to the left of zero reflect greater mindfulness meditation-induced headache relief. Confidence intervals that do not include zero reflect significant differences. Summary statistics were computed via random effects meta-analysis.
Mindfulness meditation for pain intensity
The results of meta-analysis for outcomes reported by more than one study for the mindfulness group were compared with control group and are displayed in Figures 2, 3 and Supplementary Files 2 (434.2KB, tif) , 3 (1.6MB, tif) . Pain intensity was the reported outcome in seven studies. The combined pain intensity response was −0.89 (95% CI, −1.63 to −0.15; P = 0.02) with heterogeneity (I2 = 88%) [Figure 2a]. Further, we conducted a sensitivity analysis according to the quality of these studies. The combined pain intensity response from the five studies at low risk of bias was −0.49 (95% CI, −1.12–0.14; P = 0.13) with heterogeneity (I2 = 78%). Figure 2b and 2c, respectively, show subgroup analysis of pain intensity according to different meditation forms and different therapy durations. In the subgroup analysis of different meditation forms, MBSR intervention displayed a positive influence on pain intensity with SMD [−1.07, 95% CI, −1.46 to −0.66; P < 0.000; I2 = 0%; Figure 2b]. In the subgroup analysis of different therapy durations, the 8-week intervention showed a significant effect [P < 0.000, I2 = 0%; Figure 2c]. In the subgroup analysis of different types of headache, intervention for migraine had a positive effect (P = 0.01; I2 = 0%) with small sample size [Supplementary File 3a (1.6MB, tif) ]. In the subgroup analysis of age, the intervention showed a positive influence on older participants [P = 0.01; I2 = 87%; Supplementary File 3b (1.6MB, tif) ]. A subgroup analysis of different control groups revealed a significant effect with meditation as compared to passive controls (P = 0.01; I2 = 87%), but when compared to active controls a meaningful result was not achieved because only one study remained [Supplementary File 3c (1.6MB, tif) ].
Mindfulness meditation for other indices
Meditation program reduced headache frequency [P = 0.02; I2 = 71%; Figure 3a], but had no significant effect on the duration [P = 0.1; I2 = 65%; Figure 3b]. Quality of life assessment was carried out for two studies, and the combined response was −0.37 [95% CI, −0.82–0.07; P = 0.1; I2 = 0%; Figure 3c]. There was a significant change in the combined effect size of self-efficacy [−1.15, 95% CI, −1.97 to −0.33; P = 0.006; I2 = 33%; Figure 3d].
DISCUSSION
Although the meta-analysis found limited evidence for the effectiveness of mindfulness-based interventions in treating primary headache, it revealed that mindfulness-based intervention might have a positive impact on headache intensity. However, a sensitivity analysis to the studies at low risk of bias may suggest a possible overestimation of pain intensity improvement in all studies. Based on the analysis of different subgroups, it was found that the heterogeneity of pain intensity might be derived from other meditation forms such as MBCT and brief MBSR and from other types of headache such as TTH. MBSR was developed by Kabat-Zinn and Hanh[28] and MBCT was proposed by Segal et al.,[29] and both were developed as secular clinical interventions. MBCT does not require the adoption of any specific spiritual orientation or belief system. A further source for MBCT is cognitive-behavioral therapy (CBT) – a psychotherapy based on the assumption that the way we perceive events largely determines how we feel about them and, in turn, how we behave.[15] This specific spiritual orientation or belief system of MBSR may help reduce pain intensity. After subgroup analysis of different types of headache, heterogeneity was resolved in the subgroup of migraine with a small sample size. However, regarding long-term effect with mindfulness meditation, more practice helps gain more in terms of benefits. In the future, we may conduct a study focusing on the difference between MBSR and MBCT.
The aim of CBT is to help patients learn how to think and behave in more adaptive ways. In the context of chronic pain, CBT components typically include cognitive restructuring of maladaptive pain-related beliefs, coping skills training, problem-solving training, and psychoeducation of pain and their particular syndromes. CBT often includes several behavioral strategies such as relaxation training, strategies for behavioral activation, pacing, activity scheduling, and motivating physical activity.[30] Although CBT has become a first-line psychosocial treatment for individuals with chronic pain,[31] mindfulness meditation has shown the same effect as CBT when treating adult patients with low back pain.[32] Furthermore, mindfulness meditation could reduce the anxiety and stress levels as the biofeedback.[33,34]
A subgroup analysis of passive and active groups showed meditation had a significant effect in the passive groups including usual medication, wait-list, and delayed treatment, as compared to the active group. A pooled-effect was derived from six passive controls and one active control. This is not paradoxical with regard to Davidson's conclusion,[35,36,37] which suggested MBSR does not differ with the active control group (Health Enhancement Program; a structurally equivalent, active control condition). Although the pain rating was tested, all subjects were without headache in Davidson's research.
Mindfulness-based intervention may influence headache frequency, but there was no significant change in the duration of headache. Pain tolerance and perceived stress did not change. The intervention had a positive effect on self-efficacy within small sample sizes. The methodological quality of the included studies was variable. We could not conduct quantitative tests to detect potential publication bias because only seven studies were available for the primary outcome. We reviewed unpublished trials related to our study in the clinicaltrials.gov registration database and found two trials that appeared to have not been completed before November 2016. As only 2 outcomes were excluded from the analysis, the findings of our meta-analysis are less likely to be affected by publication bias.
In clinical application, mindfulness meditation may reduce the intensity and frequency of primary headache with no associated side effects. Moreover, it helps improve self-efficacy as proposed by Bandura.[38] Self-efficacy is the extent or strength of one's belief in one's own ability to complete tasks and reach goals. When self-efficacy is elevated, patients may have a better quality of life. More humanistic outcomes should be measured as the process of pain essentially includes psychosocial information.[39] As a complementary and alternative medicine, mindfulness-based intervention has higher cost-efficiency, is convenient to practice at home, and does not require any special facilities. Despite the limitations of this analysis, the evidence suggests that mindfulness meditation may help control headache. Thus, physicians should suggest to their patients that they learn mindfulness meditation in addition to standard medical care for headache.
As the review analyzed pooled effects from a small number of studies, this limited our ability to draw definitive conclusions. In addition, some studies had limitations as they were underpowered.[12,17,26] Inclusion of studies that are analyzed by the person completing the program may result in bias in favor of treatment. Although some studies[12,13,17,20,23] referred to the home practice of the meditation form, the extent of completion of the intervention at home was not assessed. Three studies[10,25,26] did not specify therapist training which may have affected the quality of the intervention. Intention-to-treat analysis was performed only in one study.[12] There were three problems in the included studies as follows: lack of blinding to outcome assessment, lack of allocation concealment, and lack of intention-to-treat analysis.
Almost all of the included studies measured pain intensity with the Likert scale, which is relatively subjective. Only two studies[11,20] tested pain sensitivity in a cold-water task, which could be relatively objective. However, it was interesting that the cold-water task tested the cold sensitivity of the skin over the hand rather than that over the head, or the skin around the trigger point. Only a few studies[10,17,25] investigated the effects of mindfulness meditation on headache during follow-up. However, for chronic headache, more attention should be paid to long-term training effect of mindfulness meditation practice.
In conclusion, based on a small number of studies that limited our ability to draw a definitive conclusion, mindfulness meditation may be a promising treatment option for the amelioration of primary headache. Headache intensity was reduced by mindfulness meditation in the form of MBSR and when compared with passive controls. The attenuation of headache intensity may be due to the reduction of headache frequency and improvement of self-efficacy. In the future research, headache sensitivity should be tested objectively. Further, larger sample size and high-quality experimental designs are required to conclusively determine the role of mindfulness meditation in headache.
Supplementary information is linked to the online version of the paper on the Chinese Medical Journal website.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
The authors extend their sincere thanks to Dr. Rui-Li Wei for his assistance with manuscript writing.
Footnotes
Edited by: Yuan-Yuan Ji
REFERENCES
- 1.Stovner LJ, Hagen K, Jensen R, Katsarava Z, Lipton R, Scher A, et al. The global burden of headache: A documentation of headache prevalence and disability worldwide. Cephalalgia. 2007;27:193–210. doi: 10.1111/j.1468-2982.2007.01288.x. doi:10.1111/j.1468-2982.2007.01288.x. [DOI] [PubMed] [Google Scholar]
- 2.Steiner TJ, Birbeck GL, Jensen RH, Katsarava Z, Stovner LJ, Martelletti P, et al. Headache disorders are third cause of disability worldwide. J Headache Pain. 2015;16:58. doi: 10.1186/s10194-015-0544-2. doi:10.1186/s10194-015-0544-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Peng KP, Wang SJ. Epidemiology of headache disorders in the Asia-Pacific region. Headache. 2014;54:610–8. doi: 10.1111/head.12328. doi:10.1111/head.12328. [DOI] [PubMed] [Google Scholar]
- 4.Stovner LJ, Andree C. Prevalence of headache in Europe: A review for the Eurolight project. J Headache Pain. 2010;11:289–99. doi: 10.1007/s10194-010-0217-0. doi:10.1007/s10194-010-0217-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Srikiatkhachorn A, le Grand SM, Supornsilpchai W, Storer RJ. Pathophysiology of medication overuse headache – An update. Headache. 2014;54:204–10. doi: 10.1111/head.12224. doi:10.1111/head.12224. [DOI] [PubMed] [Google Scholar]
- 6.Dong Z, Chen X, Steiner TJ, Hou L, Di H, He M, et al. Medication-overuse headache in China: Clinical profile, and an evaluation of the ICHD-3 beta diagnostic criteria. Cephalalgia. 2015;35:644–51. doi: 10.1177/0333102414552533. doi:10.1177/0333102414552533. [DOI] [PubMed] [Google Scholar]
- 7.Stubberud A, Varkey E, McCrory DC, Pedersen SA, Linde M. Biofeedback as prophylaxis for pediatric migraine: A meta-analysis. Pediatrics. 2016;138:pii: e20160675. doi: 10.1542/peds.2016-0675. doi: 10.1542/peds.2016.0675. [DOI] [PubMed] [Google Scholar]
- 8.Rausa M, Palomba D, Cevoli S, Lazzerini L, Sancisi E, Cortelli P, et al. Biofeedback in the prophylactic treatment of medication overuse headache: A pilot randomized controlled trial. J Headache Pain. 2016;17:87. doi: 10.1186/s10194-016-0679-9. doi:10.1186/s10194-016-0679-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Arena JG, Bruno GM, Hannah SL, Meador KJ. A comparison of frontal electromyographic biofeedback training, trapezius electromyographic biofeedback training, and progressive muscle relaxation therapy in the treatment of tension headache. Headache. 1995;35:411–9. doi: 10.1111/j.1526-4610.1995.hed3507411.x. [DOI] [PubMed] [Google Scholar]
- 10.Omidi A, Zargar F. Effect of mindfulness-based stress reduction on pain severity and mindful awareness in patients with tension headache: A randomized controlled clinical trial. Nurs Midwifery Stud. 2014;3:e21136. doi: 10.17795/nmsjournal21136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wachholtz AB, Pargament KI. Migraines and meditation: Does spirituality matter? J Behav Med. 2008;31:351–66. doi: 10.1007/s10865-008-9159-2. doi:10.1007/s10865-008-9159-2. [DOI] [PubMed] [Google Scholar]
- 12.Day MA, Thorn BE, Ward LC, Rubin N, Hickman SD, Scogin F, et al. Mindfulness-based cognitive therapy for the treatment of headache pain: A pilot study. Clin J Pain. 2014;30:152–61. doi: 10.1097/AJP.0b013e318287a1dc. doi:10.1097/AJP.0b013e318287a1dc. [DOI] [PubMed] [Google Scholar]
- 13.Cathcart S, Galatis N, Immink M, Proeve M, Petkov J. Brief mindfulness-based therapy for chronic tension-type headache: A randomized controlled pilot study. Behav Cogn Psychother. 2014;42:1–5. doi: 10.1017/S1352465813000234. doi:10.1017/s1352465813000234. [DOI] [PubMed] [Google Scholar]
- 14.Tang YY, Hölzel BK, Posner MI. The neuroscience of mindfulness meditation. Nat Rev Neurosci. 2015;16:213–25. doi: 10.1038/nrn3916. doi:10.1038/nrn3916. [DOI] [PubMed] [Google Scholar]
- 15.Chiesa A, Malinowski P. Mindfulness-based approaches: Are they all the same? J Clin Psychol. 2011;67:404–24. doi: 10.1002/jclp.20776. doi:10.1002/jclp.20776. [DOI] [PubMed] [Google Scholar]
- 16.Goyal M, Singh S, Sibinga EM, Gould NF, Rowland-Seymour A, Sharma R, et al. Meditation programs for psychological stress and well-being: A systematic review and meta-analysis. JAMA Intern Med. 2014;174:357–68. doi: 10.1001/jamainternmed.2013.13018. doi:10.1001/jamainternmed.2013.13018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wells RE, Burch R, Paulsen RH, Wayne PM, Houle TT, Loder E, et al. Meditation for migraines: A pilot randomized controlled trial. Headache. 2014;54:1484–95. doi: 10.1111/head.12420. doi:10.1111/head.12420. [DOI] [PubMed] [Google Scholar]
- 18.Wachholtz AB, Malone CD, Pargament KI. Effect of different meditation types on migraine headache medication use. Behav Med. 2017;43:1–8. doi: 10.1080/08964289.2015.1024601. doi:10.1080/08964289.2015.1024601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rosenzweig S, Greeson JM, Reibel DK, Green JS, Jasser SA, Beasley D, et al. Mindfulness-based stress reduction for chronic pain conditions: Variation in treatment outcomes and role of home meditation practice. J Psychosom Res. 2010;68:29–36. doi: 10.1016/j.jpsychores.2009.03.010. doi:10.1016/j.jpsychores.2009.03.010. [DOI] [PubMed] [Google Scholar]
- 20.Cathcart S, Barone V, Immink M, Proeve M. Mindfulness training does not reduce generalized hyperalgesia in chronic tension-type headache. J Pain Manage. 2013;6:217–21. [Google Scholar]
- 21.Yates SL, Morley S, Eccleston C, de C Williams AC. A scale for rating the quality of psychological trials for pain. Pain. 2005;117:314–25. doi: 10.1016/j.pain.2005.06.018. doi:10.1016/j.pain.2005.06.018. [DOI] [PubMed] [Google Scholar]
- 22.Eccleston C, Fisher E, Law E, Bartlett J, Palermo TM. Psychological interventions for parents of children and adolescents with chronic illness. Cochrane Database Syst Rev. 2015;8:CD009660. doi: 10.1002/14651858.CD009660.pub3. doi:10.1002/14651858.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rosdahl DRL. The effect of mindfulness meditation on tension headaches and secretory immunoglobulin A in saliva. ProQuest Dissertations and Theses 399 (The University of Arizona, 2003) [Google Scholar]
- 24.Cathcart S, Barone V, Immink M, Proeve M, Hayball J. Mindfulness training does not reduce inflammatory cytokine levels in chronic tension-type headache. J Pain Manage. 2013;6:235–8. [Google Scholar]
- 25.Omidi A, Zargar F. Effects of mindfulness-based stress reduction on perceived stress and psychological health in patients with tension headache. J Res Med Sci. 2015;20:1058–63. doi: 10.4103/1735-1995.172816. doi:10.4103/1735-1995.172816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bakhshani NM, Amirani A, Amirifard H, Shahrakipoor M. The effectiveness of mindfulness-based stress reduction on perceived pain intensity and quality of life in patients with chronic headache. Glob J Health Sci. 2015;8:142–51. doi: 10.5539/gjhs.v8n4p142. doi:10.5539/gjhs.v8n4p142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kiran, Girgla KK, Chalana H, Singh H. Effect of rajyoga meditation on chronic tension headache. Indian J Physiol Pharmacol. 2014;58:157–61. [PubMed] [Google Scholar]
- 28.Kabat-Zinn J, Hanh TN. Massachusetts: Delta; 2009. Full Catastrophe Living: Using the Wisdom of Your Body and Mind to Face Stress, Pain, and Illness. [Google Scholar]
- 29.Segal ZV, Williams JM, Teasdale JD. Mindfulness-Based Cognitive Therapy for Depression. New York: Guilford Press; 2012. [Google Scholar]
- 30.Hatchard T, Lepage C, Hutton B, Skidmore B, Poulin PA. Comparative evaluation of group-based mindfulness-based stress reduction and cognitive behavioral therapy for the treatment and management of chronic pain disorders: Protocol for a systematic review and meta-analysis with indirect comparisons. Syst Rev. 2014;3:134. doi: 10.1186/2046-4053-3-134. doi:10.1186/2046-4053-3- [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ehde DM, Dillworth TM, Turner JA. Cognitive-behavioral therapy for individuals with chronic pain: Efficacy, innovations, and directions for research. Am Psychol. 2014;69:153–66. doi: 10.1037/a0035747. doi: 10.1037/a0035747. [DOI] [PubMed] [Google Scholar]
- 32.Cherkin DC, Sherman KJ, Balderson BH, Cook AJ, Anderson ML, Hawkes RJ, et al. Effect of mindfulness-based stress reduction vs. cognitive behavioral therapy or usual care on back pain and functional limitations in adults with chronic low back pain: A randomized clinical trial. JAMA. 2016;315:1240–9. doi: 10.1001/jama.2016.2323. doi: 10.1001/jama.2016.2323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ratanasiripong P, Park JF, Ratanasiripong N, Kathalae D. Stress and anxiety management in nursing students: Biofeedback and mindfulness meditation. J Nurs Educ. 2015;54:520–4. doi: 10.3928/01484834-20150814-07. doi:10.3928/01484834-20150814-07. [DOI] [PubMed] [Google Scholar]
- 34.van der Zwan JE, de Vente W, Huizink AC, Bögels SM, de Bruin EI. Physical activity, mindfulness meditation, or heart rate variability biofeedback for stress reduction: A randomized controlled trial. Appl Psychophysiol Biofeedback. 2015;40:257–68. doi: 10.1007/s10484-015-9293-x. doi:10.1007/s10484-015-9293-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.MacCoon DG, Imel ZE, Rosenkranz MA, Sheftel JG, Weng HY, Sullivan JC, et al. The validation of an active control intervention for Mindfulness Based Stress Reduction (MBSR) Behav Res Ther. 2012;50:3–12. doi: 10.1016/j.brat.2011.10.011. doi:10.1016/j.brat.2011.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.MacCoon DG, MacLean KA, Davidson RJ, Saron CD, Lutz A. No sustained attention differences in a longitudinal randomized trial comparing mindfulness based stress reduction versus active control. PLoS One. 2014;9:e97551. doi: 10.1371/journal.pone.0097551. doi:10.1371/journal.pone.0097551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rosenkranz MA, Davidson RJ, Maccoon DG, Sheridan JF, Kalin NH, Lutz A, et al. A comparison of mindfulness-based stress reduction and an active control in modulation of neurogenic inflammation. Brain Behav Immun. 2013;27:174–84. doi: 10.1016/j.bbi.2012.10.013. doi:10.1016/j.bbi.2012.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bandura A. Self-efficacy: Toward a unifying theory of behavioral change. Psychol Rev. 1977;84:191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- 39.Edwards RR, Dworkin RH, Sullivan MD, Turk DC, Wasan AD. The role of psychosocial processes in the development and maintenance of chronic pain. J Pain. 2016;17:T70–92. doi: 10.1016/j.jpain.2016.01.001. doi:10.1016/j.jpain.2016.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Example of search strategy
Forest plots of meta-analysis data for pain tolerance (a) and perceived stress (b). Effect sizes overlapped with zero reflect no significant difference between mindfulness meditation and control groups. Summary statistics were computed via random effects meta-analysis.
Subgroup analysis of pain intensity according to different items: (a) different types of headaches, (b) different ages and (c) different control groups.