Abstract
Background
Non-fatal firearm injuries constitute approximately 70% of all firearm trauma injuries in the United States. Patterns of severity of these injuries are poorly understood. We analyzed the overall, age-, sex- and intent-specific temporal trends in the injury severity of firearm hospitalizations from 1993 to 2014.
Methods
We assessed temporal trends in the severity of patients hospitalized for firearm using Nationwide Inpatient Sample (NIS) data over a 22 year period. Firearm hospitalization was identified using assault (E965x), unintentional (E922x), intentional self-harm (E955x), legal (E970) and undetermined (E985x) International Classification of Diseases, Ninth Revision, Clinical Modification (ICD9) codes. Injury severity was measured using the computed New Injury Severity Score (NISS). We used survey weighted means, SD and annual percent change (APC), and joinpoint regression to analyze temporal trends.
Results
A weighted total of 648 662 inpatient admissions for firearm injury were analyzed. Firearm injury severity demonstrated a significant annual increase of 1.4% (95% CI=1.3 to 1.6), and was driven by annual increases among young adults (APC=1.4%, 95% CI=1.3 to 1.5), older adults (APC=1.5%, 95% CI=1.3 to 1.6), female (APC=1.5%, 95% CI=1.3 to 1.6) and male (APC=1.4%, 95% CI=1.3 to 1.6) hospitalizations. The annual increase among assault/legal injuries was 1.4% (95% CI=1.3 to 1.5), similar to unintentional (APC=1.4%, 95% CI=1.3 to 1.6), intentional self-harm (APC=1.5%, 95% CI=1.4 to 1.6) and undetermined (APC=1.4%, 95% CI=1.3 to 1.6).
Conclusions
The severity of hospitalized firearm injuries increased significantly from 1993 to 2014. This annual increase reflects a move towards hospitalization of more serious injuries, and outpatient management of less serious injuries across the board, suggesting a mounting burden on the US healthcare system.
Level of evidence
Level IV.
Keywords: injury severity, injury, time trends
Background
The majority of injuries related to traumatic injuries caused by firearms in the US result in non-fatal firearm hospitalizations.1 2 Roughly 30% of these people will die after being shot, about 30% are treated and discharged from hospital emergency departments, and the roughly 40% who remain sustain more severe injuries and are hospitalized for further treatment.3 4 Injury severity is often greater among firearm hospitalizations as compared with other traumatic injury hospitalizations.5 6
National data that have accumulated for over two decades may now permit new analyses and a new understanding of previously unreported, long-term trends and changes in firearm hospitalization.7 8 We broadly know that national firearm hospitalizations rates per 100 000 hospitalizations declined after the year 2000 and there has been little change in assault-related firearm hospitalizations in that same time period.8 9 We also know that there are substantial age-, gender- and intent-specific differences in firearm hospitalizations.3 8 10 Most firearm hospitalizations victims are male and most firearm hospitalizations are due to assault. Younger adults between the age of 16 and 45 years hospitalized for firearm injury were more likely to be injured by assault7 11 as compared with older adults who are hospitalized for self-inflicted injuries.12Older youth between 16–19 years of age had firearm injury profile similar to that of adults,13 particularly with respect to firearm homicide rates.
However, very little is known regarding the patterns of injury severity in firearm hospitalizations over time, and by age, sex and intent of injury subgroups. Therefore, the aim of this study was to analyze temporal trends in injury severity of firearm injury hospitalization over a multi-decade period. We also assessed the magnitude of firearm hospitalizations and compared the differences in temporal trends of injury severity across age, sex, and intent of injury subgroups.
Methods
Data source
We used inpatient hospitalization dataset, the Nationwide Inpatient Sample (NIS), Healthcare Cost and Utilization Project (HCUP), Agency for Healthcare Research and Quality from 1993 to 2014.14 The NIS data are nationally representative claims based data and contains information on hospital stays in 1000 hospitals sampled to represent a 20% stratified sample of US community hospitals from 47 states. Survey weights are provided to estimate weighted counts and estimates. Trend weights are provided for calculation of trends. We used trend weights for the analysis. Each year of the NIS provides information on approximately 9 million inpatients records.
Study design
This study used a subset of all firearm hospitalizations from NIS from 1993 to 2014 and we used a repeated cross-sectional study design to assess temporal trends of injury severity of firearm hospitalizations during this time period. Boston University School of Medicine Institutional Review Board approved the study.
Study cohort
The flow chart of data inclusion and exclusion is represented in online supplementary figure 1. There was a total of 789 782 871 weighted hospitalizations from 1993 to 2014. First, we excluded 524 270 hospitalizations, that were missing information on age, leading to remaining 789,258,601 hospitalizations. Second, we restricted in each year of NIS, those hospitalizations that had a secondary diagnosis International Classification of Diseases, Ninth Revision, Clinical Modification codes (ICD-9 CM) of assault (E9650, E9651, E9652, E9653, E9654), unintentional (E9220, E9221, E9222, E9223, E9224, E9228, E9229), intentional self-harm (E9550, E9551, E9552, E9553, E9554, E9556, E9559), legal (E970), war (E991) and undetermined (E9850, E9851, E9852, E9853, E9854, E9856) traumatic injuries. All injuries are captured as secondary diagnosis codes. For analytical purposes, we included legal under the assault category. Therefore, we excluded 788 535 952 non-firearm hospitalizations resulting in 722 649 firearm hospitalizations. We restricted the firearm hospitalizations to those admitted from ER, in attempt to use only those hospitalizations that are new events rather than a re-hospitalization due to a prior firearm injury. After excluding those hospitalizations admitted without a prior ER visit (n=73 987), the final weighted count of firearm hospitalizations was 648 662. Each record refers to a single hospitalization; as a result, a person may have multiple hospitalizations, and unique patient records may not be identified.
tsaco-2017-000139supp001.docx (147.2KB, docx)
Variables
We used Computed New Injury Severity Score (NISS) as a measure of overall injury severity on a continuous scale.15–17 NISS is a continuous variable measuring the firearm injury severity ranging from 0 to 75.16 Age groups used in the analysis were 0–15 (pediatric), 16–45 (young adult) and 46 and older (older adults) and sex into two groups of male and female. Intent of injury was categorized into assault (includes legal intervention), intentional self-harm, unintentional and undetermined.
The other patient variables we used were race/ethnicity, defined in NIS data as white (non-Hispanic white), black, Hispanic, other (includes Asian or Pacific Islander, Native American and others), and unknown (which have missing race/ethnicity data), type of insurance (private insurance/Medicare, self-pay, and Medicaid/no charge/other), median neighborhood income quartiles ($1–$24,999, $25,000–$34,999, $35,000–$44,999, $45 000 and above) and co-morbidities. Elixhauser comorbidity score was calculated from 29 co-morbidities identified based on ICD-9 CM codes.18 The hospital-level characteristics were location (rural and urban), teaching status (teaching and non-teaching), size of the hospital (small, medium and large) and US census regions (Northeast, Midwest, South and West).
Statistical analysis
First we used package ICDPIC Version 3.0 to calculate the new injury severity scores, NISS, for each firearm hospitalizations in each NIS data from 1993 to 2014.19 We used the primary scores of NISS for further analyses. Second, we used survey weighted multilevel mixed-effects generalized linear model (Gaussian family) with NISS as a linear dependent variable, year as a factor term and stratum as the random coefficient. We then obtained Bayesian shrinkage estimates as a way to decrease classification error of stratum, by shrinking the estimates towards the average estimated effect in each stratum.20 Third, we assessed the breakpoints and temporal changes in injury severity of firearm hospitalizations from 1993 to 2014 using Joinpoint Regression Programme version 4.5.0.1.21 Joinpoint regression is used to assess temporal trends by using an algorithm to test whether a segmented line is significantly better than a straight line. The regression is performed on a log scale and the points where the segments joint is called joinpoints or breakpoints. We used the predicted shrinkage Bayes estimates to calculate the annual mean, the log of the annual mean and the SE for Joinpoint analysis. For the Joinpoint analysis, the minimum number of observations from a joinpoint to either end of the data (excluding first or last joinpoint if it falls on an observation) was set 2. The number of points to place between adjacent observed x values in the grid search was set at 0. The number of joinpoints were set ranging from 0 to 4. The model selection method was based on permutation test, where the overall significance level was set at 0.05, and the number of randomly permuted data sets was 4499. Fourth, annual percent change (APC) was obtained for each segment along with 95% confidence intervals (95% CI). All P values were two-sided and significance level was <0.05. STATA MP 14.2 (StataCorp LP, College Station, Texas; 2009) was used for data analyses.
Results
Descriptive characteristics
Between 1993 and 2014, there were a weighted total of 648 662 inpatient admissions of firearm injury. The majority were of assaultive intent (389 506, 60.1%), followed by unintentional (n=157 225, 24.2%), intentional self-harm (55 601, 8.6%) and undetermined (46 330, 7.1%). Table 1 presents the overall demographic characteristics of firearm hospitalizations and by 4 year time periods. firearm hospitalizations were more likely to be between 16–45 years of age, black, men, reported to have either private or Medicare as private insurance, from low income neighborhoods. The characteristics of the hospitals where firearm injuries were treated were more likely to be urban, teaching, large and located in the south of the country. Each comorbidity by the same time periods are presented in online supplementary table 1.
Table 1.
Demographic and hospital characteristics of firearm injury hospitalizations, NIS 1993–2014
| n | Total | 1993–1996 | 1997–2002 | 2003–2007 | 2008–2014 | P |
| 648 662 | 152 442 | 167 900 | 144 942 | 183 378 | ||
| Demographic | ||||||
| Age | <0.0001 | |||||
| 0–15 | 36 032 (5.6) | 11 123 (7.3) | 10 188 (6.1) | 7432 (5.1) | 7289 (4.0) | |
| 16–45 | 534 140 (82.3) | 127 595 (83.7) | 139 609 (83.2) | 119 477 (82.4) | 147 458 (80.4) | |
| 46+ | 78 491 (12.1) | 13 724 (9.0) | 18 103 (10.8) | 18 033 (12.4) | 28 631 (15.6) | |
| Race | <0.0001 | |||||
| White | 146 805 (22.6) | 33 754 (22.1) | 35 163 (20.9) | 28 428 (19.6) | 49 461 (27.0) | |
| Black | 260 478 (40.2) | 67 292 (44.1) | 59 955 (35.7) | 51 193 (35.3) | 82 038 (44.7) | |
| Hispanic | 94 519 (14.6) | 23 800 (15.6) | 21 100 (12.6) | 22 625 (15.6) | 26 994 (14.7) | |
| Other | 26 379 (4.1) | 5434 (3.6) | 6406 (3.8) | 5827 (4.0) | 8712 (4.8) | |
| Unknown | 120 481 (18.6) | 22 162 (14.5) | 45 277 (27.0) | 36 869 (25.4) | 16 173 (8.8) | |
| Sex | 0.38 | |||||
| Male | 575 604 (89.0) | 134 820 (88.5) | 149 548 (89.1) | 128 306 (89.3) | 162 931 (89.1) | |
| Female | 71 161 (11.0) | 17 598 (11.6) | 18 310 (10.9) | 15 402 (10.7) | 19 851 (10.9) | |
| Insurance | 0.13 | |||||
| Private/Medicare | 178 774 (27.8) | 38 604 (25.5) | 51 107 (30.9) | 39 326 (27.6) | 49 737 (27.3) | |
| Self-pay | 202 409 (31.5) | 50 089 (33.0) | 54 395 (32.9) | 45 312 (31.8) | 52 614 (28.9) | |
| Medicaid/No charge/Other | 260 902 (40.6) | 62 969 (41.5) | 60 068 (36.3) | 57 945 (40.6) | 79 920 (43.9) | |
| Neighborhood income quartiles | <0.0001 | |||||
| ≤$24 999 | 275 761 (45.2) | 75 036 (55.9) | 41 096 (25.7) | 71 332 (51.2) | 88 297 (50.1) | |
| $25,000–$34 999 | 172 802 (28.3) | 39 604 (29.5) | 54 244 (34.0) | 34 727 (24.9) | 44 228 (25.1) | |
| $35,000–$44 999 | 104 320 (17.1) | 14 542 (10.8) | 38 080 (23.8) | 22 393 (16.1) | 29 305 (16.6) | |
| ≥$45 000 | 56 906 (9.3) | 5076 (3.8) | 26 332 (16.5) | 10 986 (7.9) | 14 512 (8.2) | |
| Hospital | ||||||
| Location | 0.015 | |||||
| Rural | 29 983 (4.8) | 9902 (6.5) | 9650 (5.8) | 5749 (4.0) | 4683 (3.0) | |
| Urban | 589 822 (95.2) | 142 021 (93.5) | 157 960 (94.2) | 139 180 (96.0) | 150 661 (97.0) | |
| Teaching hospital | 0.002 | |||||
| Non-teaching | 156 828 (25.4) | 56 146 (37.0) | 41 550 (24.8) | 32 467 (22.4) | 26 665 (17.3) | |
| Teaching | 461 547 (74.6) | 95 777 (63.0) | 126 060 (75.2) | 112 460 (77.6) | 127 249 (82.7) | |
| Size | 0.097 | |||||
| Small | 32 846 (5.1) | 11 604 (7.6) | 8399 (5.0) | 6150 (4.2) | 6693 (3.7) | |
| Medium | 157 507 (24.4) | 42 122 (27.7) | 48 080 (28.7) | 30 085 (20.8) | 37 220 (20.7) | |
| Large | 454 296 (70.5) | 98 197 (64.6) | 111 131 (66.3) | 108 693 (75.0) | 136 275 (75.6) | |
| Region | 0.31 | |||||
| Northeast | 111 872 (17.3) | 30 327 (19.9) | 25 994 (15.5) | 20 618 (14.2) | 34 933 (19.1) | |
| Midwest | 123 618 (19.1) | 21 243 (13.9) | 39 404 (38.6) | 29 449 (20.3) | 33 522 (18.3) | |
| South | 264 577 (40.8) | 56 585 (37.1) | 64 875 (38.6) | 64 210 (44.3) | 78 907 (43.0) | |
| West | 148 596 (22.9) | 44 287 (29.1) | 37 627 (22.4) | 30 666 (21.2) | 36 017 (19.6) | |
| Intent of injury | 0.025 | |||||
| Assault/Legal | 389 506 (60.1) | 89 183 (58.5) | 98 547 (58.7) | 89 545 (61.8) | 1 12 231 (61.2) | |
| Unintentional | 157 225 (24.2) | 38 738 (25.4) | 42 348 (25.2) | 32 733 (22.6) | 43 406 (23.7) | |
| Intentional self-harm | 55 601 (8.6) | 11 270 (7.4) | 13 628 (8.1) | 12 263 (8.5) | 18 440 (10.1) | |
| Undetermined | 46 330 (7.1) | 13 251 (8.7) | 13 378 (8.0) | 10 401 (7.2) | 9301 (5.1) | |
| Location of injury | <0.0001 | |||||
| Head or neck | 75 594 (11.9) | 15 403 (10.5) | 19 234 (11.9) | 17 086 (12.2) | 22 769 (13.0) | |
| Face | 24 626 (3.9) | 5090 (3.5) | 6099 (3.8) | 5402 (3.9) | 7455 (4.2) | |
| Chest | 81 039 (12.7) | 17 442 (11.9) | 20 635 (12.8) | 18 428 (13.2) | 23 092 (13.2) | |
| Abdominal/pelvic contents | 152 231 (23.9) | 33 981 (23.2) | 39 470 (24.4) | 34 841 (24.9) | 42 187 (24.0) | |
| Extremities/pelvic girdle | 195 070 (30.6) | 43 096 (29.5) | 46 912 (29.0) | 42 601 (30.5) | 58 583 (33.4) | |
| External | 109 298 (17.1) | 31 178 (21.3) | 29 540 (18.3) | 21 523 (15.4) | 21 532 (12.3) |
All values are weighted frequencies (n) and weighted percentages (%) using survey weighted analysis except Elixhauser comorbidity score presented as mean and SD. From 1993 to 1997, median household income fell into four categories: (1) $1–$25 000, (2) $25 001–$30 000, (3) $30 001–$35,000, (4) $35 001 and above. From 1998 to 2002, median household income fell into four categories: (1) $1– $24 999, (2) $25 000–$34 999, (3) $35 000– $44 999, (4) $45 000 and above. From 2003 onwards, median household income was present in the data as national quartiles for patient’s ZIP Code.
Distribution of firearm hospitalizations
Of the 648 662 firearm hospitalizations, 5.6% were among children, 82.3% among young adults and 12.1% among older adults. Across the years the proportion of those 0–15 year-old firearm hospitalizations ranged from 7.7% in 1993 to 3.7% in 2014, among 16–45 year-old firearm hospitalizations ranged from 84.6% to 78.7% and among >=46 year-old firearm hospitalizations ranged from 7.7% to 17.5%. The weighted stacked proportions of firearm hospitalizations across the years by age group are presented in online supplementary figure 2. The proportion of firearm hospitalizations that were male ranged from 88.6% in 1993 to 88.1% in 2014 and that were female ranged from 11.4% to 11.9% in the respective years. The weighted stacked proportions of firearm hospitalizations across the years by sex are presented in online supplementary figure 3. The weighted stacked proportions of firearm hospitalizations across the years by intent of injury are presented in online supplementary figure 4. Assault/legal firearm hospitalizations ranged from 55.6% to 58.9%, unintentional firearm hospitalizations from 30.6% to 26.0%, intentional self-harm firearm hospitalizations from 4.6% to 10.4% and undetermined from 9.1% to 4.6% in 1993 and 2014 respectively.
Computed New Injury Severity Score
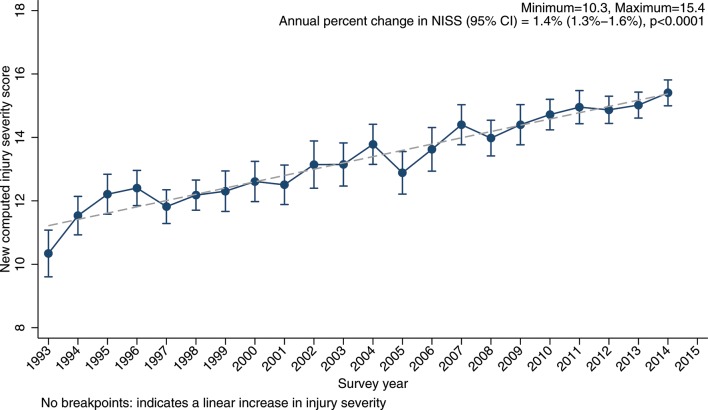
Online supplementary table 2 presents the annual mean and SE of overall NISS. The mean and SE in 1993 was 10.3 (0.4), increased to 15.4 (0.2) in 2014. Online supplementary table 3 presents the results of the Joinpoint analysis of overall NISS and by age group, sex, and by intent of injury. Figure 1 presents the temporal trends in predicted mean of overall NISS. There were no breakpoints, indicating a single segment from 1993 to 2014 with an increase (APC=1.4%, 95% CI=1.3% to 1.6%).
Figure 1.
Temporal trends in predicted mean computed new injury severity score, NIS 1993–2014. Solid marker denotes the observed mean NISS with 95% CI. The dotted line is the predicted Bayes’ shrinked estimates using multilevel generalized linear model with Gaussian distribution.
Figure 2 presents the temporal trends in predicted mean of NISS by three age groups. Among children, there were two breakpoints at 1995 and 1998 and three segments: 1993–1995 (APC=9.2%, 95% CI=3.5% to 15.3%), 1995–1998 (APC=−0.9%, 95% CI=−6.0% to 4.5%) and 1998–2014 (APC=1.5%, 95% CI=1.4% to 1.7%). There were no breakpoints in young and older adults and each group demonstrated temporal increase in injury severity.
Figure 2.
Temporal trends in predicted computed new injury severity score by age categories, NIS 1993–2014. Solid marker denotes the observed mean NISS with 95% CI. The dotted line is the predicted Bayes’ shrinked estimates using multilevel generalized linear model with Gaussian distribution.
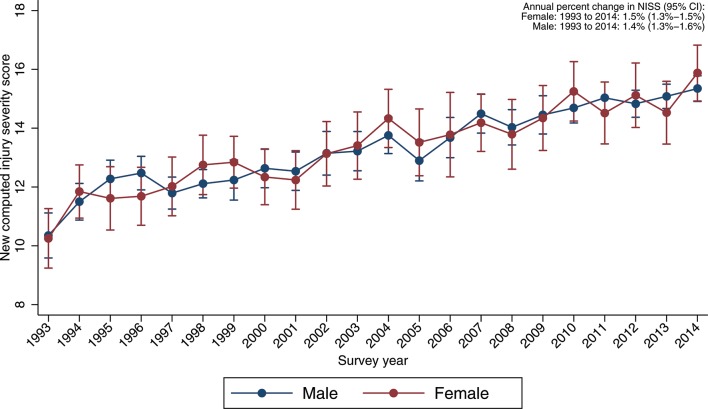
Figure 3 presents the temporal trends in predicted mean of NISS by sex. There were no breakpoints among females or males, with a single segment from 1993 to 2014 and an increase in each group of 1.5% (95% CI=1.3% to 1.6%) and 1.4% (95% CI=1.3% to 1.6%) respectively.
Figure 3.
Temporal trends in predicted computed new injury severity score by sex, NIS 1993–2014. Solid marker denotes the observed mean NISS with 95% CI. The dotted line is the predicted Bayes’ shrinked estimates using multilevel generalized linear model with Gaussian distribution.
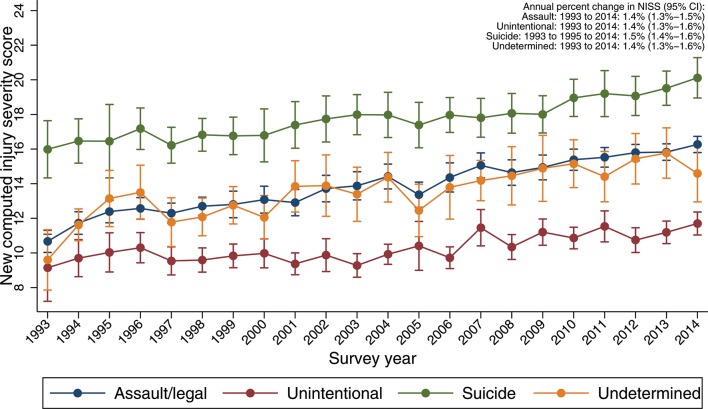
Figure 4 presents the temporal trends in predicted mean of NISS by intent of injury. There were no breakpoints in the four intent groups, with a single segment from 1993 to 2014. An increasing trend was observed in assault/legal (APC=1.4%, 95% CI=1.3% to 1.5%), unintentional (APC=1.4%, 95% CI=1.3% to 1.6%), intentional self-harm (APC=1.5%, 95% CI=1.4% to 1.6%) and undetermined (APC=1.4%, 95% CI=1.3% to 1.6%) firearm hospitalizations.
Figure 4.
Temporal trends in predicted computed new injury severity score by intent, NIS 1993–2014. Solid marker denotes the observed mean NISS with 95% CI. The dotted line is the predicted Bayes’ shrinked estimates using multilevel generalized linear model with Gaussian distribution.
Discussion
Using nationally representative hospitalization data from 1993 to 2014 we found an overall increase in injury severity in firearm hospitalizations over time. There were two additional findings. First, both males and females and all types of intents of firearm injury demonstrated a comparable significant increase in national trends in firearm hospitalizations injury severity. Second, although the magnitude of injury severity was lower in children than adults, there were increasing temporal trends in injury severity from 1998 to 2014 among children as compared with a consistent increase among adults.
Our main finding of increasing severity of injury among firearm hospitalizations across years was concordant with a smaller study that assessed fatalities and severity of firearm injuries at one city trauma center from 2000 to 20134 and other studies that showed increasing injury severity among other forms of injury related hospitalizations over time.22–24 Another trauma center study reported a similar uptrend of severity in an urban pediatric population.25 The increase in firearm injury severity observed in our study is in concordance with an increase in length of stay reported using the same nationally representative hospitalization data in another study.26 Increasing lethality of civilian firearms, such as increase in the caliber of pistols may be another explanation in the observed increase in severity of firearm injuries.27 This finding is consequential in the context of an increasing national non-fatal firearm injury rate.2 Increasing severity of firearm injuries, potentially reflects both changes in firearm injury and in hospitalization patterns, may result in long term morbidity and disability, thereby increasing overall healthcare costs.
Our study also demonstrated comparable increasing trends among both men and women and in all intents of injury. However, we also found that the proportion of these subgroup firearm hospitalizations differed greatly. About 88% of firearm hospitalizations were male, which is similar to majority of studies that reported a similar proportion to be males.2 28 We found that majority of firearm hospitalizations were of assault and unintentional intent. Our finding of increasing injury severity during this study time period being driven by the increasing trends of injury severity among assault firearm hospitalizations is similar to a finding about firearm hospitalization attributed to assaultive firearm injuries in a study using national hospitalization data.8 Our findings are also in concordance with the overall increasing severity related to firearm injury and may be due both to better medical care that saves more lives, resulting in increasing severity of injuries in firearm hospitalizations,29 30 and injuries being better treated and discharged in the emergency room and trauma centers without being hospitalized.28 31 Intentional self-harm firearm hospitalizations have a slightly greater injury severity and may be explained by the results of a study that used data over 5 year period of gunshot to the brain that found an increasing survival rate from 10% to 46% with aggressive management,31 which is also indicative of the potential long-term physical and health consequences in the context of very severe injuries.
We report changes in temporal trends only among children with a large annual increase between 1993 and 1995, which then plateaued briefly between 1995 and 1998 and followed by a more steady but smaller annual increase from 1998 to 2014. The large increase may be indicative of acute care improvements in trauma centers.31 Our results are concordant with a retrospective review of assault in children admitted to trauma centers found that the risk of mortality was high among children, suggestive of an increased injury severity among children.32 Additionally, an analysis of emergency room visits found that firearm injuries increased 31.7% between 2006 and 2012,33 corroborating our results of increasing injury severity on subsequent hospitalization. The increase in such injuries in our study among young adults indicates the potential for prolonged disability and loss of productivity in young people.
Additionally, our investigation indicates that more than half of the firearm hospitalizations are assaultive firearm injuries corroborating other reports using hospitalization data and overall non-fatal data.2 8 Recent reports have reported that the increase in assault related non-fatal firearm injuries are an artifact of the Centers for Disease Control and Prevention’s (CDC) publicly available non-fatal data due to systematic error in misclassification of 40% of assault injuries as undetermined injuries from just two hospitals.34 35 Our results using firearm hospitalizations indicate the reverse, demonstrating an increasing proportion of assault-related firearm hospitalizations from 55.6% to 58.9% of all firearm hospitalizations along with a decline in undetermined injuries from 9.1% to 4.6% from 1993 to 2014. Therefore, our results remain in concordance with the reports using the publicly available CDC data.
Our results should be interpreted with caution due to some limitations. The central limitation is the lack of patient specific identifiers to identify index versus re-hospitalizations that is inherent in the design of such nationally representative claims based surveys that are exclusively based on hospitalizations alone. Firearm injury has a high risk of re-hospitalizations especially in patients with greater severity, which increases their likelihood of rehospitalizations.36 A second limitation is the lack of detailed integrated information regarding emergency department visits, where they were treated and released without hospitalization. Of all the non-fatal firearm injuries, about 40% are treated and released in the emergency department, while the rest are hospitalized. Improvement of trauma care and policies may have contributed to changes in hospitalization from emergency room treatment across the years. A third limitation is the missing race/ethnicity information that ranges between 31.2% to 5.2% from 1993 to 2014. That limits further exploration by race/ethnicity. The fourth limitation is that the enrolment of states was not similar across years; there were fewer states in earlier years. A final limitation is that the NISS, and the older injury severity score from which it evolved, have also potentially changed in usage and application over time, as has potentially the recording of anatomic injury information that is used to calculate these scores.37 Although the findings here may represent temporal trends in enhanced medical recorder skills, it is unlikely that this played a large role in what we found given the long-standing standardization of and education around the recording of injury and ICD data.
In conclusion, our data show growing injury severity among firearm hospitalizations over time. The increase in severity of firearm injury hospitalizations from 1993 to 2014 suggests an increasing healthcare burden related to firearm violence survivorship. This increasing challenge is primarily driven by assaultive intent particularly among young adults. It seems likely that these shifts reflect a move towards hospitalization of more serious injuries,22–25 and outpatient management of less serious injuries across the board.
Footnotes
BK and YZ contributed equally.
Contributors: BK, YZ and SG conceived and supervised the study. YZ and BK completed the analyses. BK, YZ, ZX, MBS, JF, CB and SG led the writing and revisions of the manuscript. YZ assisted with obtaining data and performed data management.
Competing interests: None declared.
Ethics approval: Boston University IRB.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Centers for Disease Control and Prevention, National Centers for Injury Prevention and Control. Web-based Injury Statistics Query and Reporting System) (WISQARS) [online]. http://www.cdc.gov/ncipc/wisqars (accessed 2 Jun 2017).
- 2. Kalesan B, Adhikarla C, Pressley JC, Fagan JA, Xuan Z, Siegel MB, Galea S. The hidden epidemic of firearm injury: increasing firearm injury rates during 2001–2013. Am J Epidemiol 2017;185:1–8. [DOI] [PubMed] [Google Scholar]
- 3. Leventhal JM, Gaither JR, Sege R. Hospitalizations due to firearm injuries in children and adolescents. Pediatrics 2014;133:219–25. doi:10.1542/peds.2013-1809 [DOI] [PubMed] [Google Scholar]
- 4. Sauaia A, Miller JI, Moore EE, Partrick D. Firearm injuries of children and adolescents in 2 Colorado trauma centers: 2000-2008. JAMA 2013;309:1683–5. doi:10.1001/jama.2013.3354 [DOI] [PubMed] [Google Scholar]
- 5. Sauaia A, Gonzalez E, Moore HB, Bol K, Moore EE. Fatality and severity of firearm injuries in a denver trauma center, 2000-2013. JAMA 2016;315:2465–7. doi:10.1001/jama.2016.5978 [DOI] [PubMed] [Google Scholar]
- 6. Cheong KX, Lo HY, Teo LT, Raphael CA, Go KT, Appasamy V, Chiu MT. A 10-year profile of trauma admissions caused by interpersonal violence: a major trauma centres experience. Ann Acad Med Singapore 2014;43:170–6. [PubMed] [Google Scholar]
- 7. Cherry D, Annest JL, Mercy JA, Kresnow M, Pollock DA. Trends in nonfatal and fatal firearm-related injury rates in the United States, 1985-1995. Ann Emerg Med 1998;32:51–9. [DOI] [PubMed] [Google Scholar]
- 8. Kalesan B, French C, Fagan JA, Fowler DL, Galea S. Firearm-related hospitalizations and in-hospital mortality in the United States, 2000-2010. Am J Epidemiol 2014;179:303–12. doi:10.1093/aje/kwt255 [DOI] [PubMed] [Google Scholar]
- 9. David-Ferdon C, Dahlberg LL, Kegler SR. Centers for Disease Control and Prevention (CDC). Homicide rates among persons aged 10-24 years - United States, 1981-2010. MMWR Morb Mortal Wkly Rep 2013;62:545–8. [PMC free article] [PubMed] [Google Scholar]
- 10. Kalesan B, Dabic S, Vasan S, Stylianos S, Galea S. Racial/ethnic specific trends in pediatric firearm-related hospitalizations in the United States, 1998-2011. Matern Child Health J 2016;20:1082-90 doi:10.1007/s10995-015-1894-8 [DOI] [PubMed] [Google Scholar]
- 11. Tholpady SS, DeMoss P, Murage KP, Havlik RJ, Flores RL. Epidemiology, demographics, and outcomes of craniomaxillofacial gunshot wounds in a level I trauma center. J Craniomaxillofac Surg 2014;42:403–11. doi:10.1016/j.jcms.2013.06.004 [DOI] [PubMed] [Google Scholar]
- 12. Curtin SC, Warner M, Hedegaard H. Increase in Suicide in the United States, 1999-2014. NCHS Data Brief 2016;241:1–8. [PubMed] [Google Scholar]
- 13. Hendry PL, Suen A, Kalynych CJ, Lott M, Paul J, Smotherman C. A 6-year retrospective review of pediatric firearm injuries: do patients < 14 years of age differ from those 15-18 years of age? J Trauma Acute Care Surg 2014;77(3 Suppl 1):S41–5. doi:10.1097/TA.0000000000000384 [DOI] [PubMed] [Google Scholar]
- 14. Agency for Healthcare Research and Quality. HCUP Nationwide Inpatient Sample (NIS) : Healthcare Cost and Utilization Project (HCUP). Rockville, MD, 1988-2012. [Google Scholar]
- 15. Cook A, Weddle J, Baker S, Hosmer D, Glance L, Friedman L, Osler T. A comparison of the injury severity score and the trauma mortality prediction model. J Trauma Acute Care Surg 2014;76:47–53. doi:10.1097/TA.0b013e3182ab0d5d [DOI] [PubMed] [Google Scholar]
- 16. Lavoie A, Moore L, LeSage N, Liberman M, Sampalis JS. The New Injury Severity Score: a more accurate predictor of in-hospital mortality than the Injury Severity Score. J Trauma 2004;56:1312–20. [DOI] [PubMed] [Google Scholar]
- 17. Osler T, Baker SP, Long W. A modification of the injury severity score that both improves accuracy and simplifies scoring. J Trauma 1997;43:922–6. doi:10.1097/00005373-199712000-00009 [DOI] [PubMed] [Google Scholar]
- 18. Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care 1998;36:8–27. doi:10.1097/00005650-199801000-00004 [DOI] [PubMed] [Google Scholar]
- 19. Clark DE, Osler TM, Hahn DR. ICDPIC: Stata module to provide methods for translating International Classification of Diseases (Ninth Revision) diagnosis codes into standard injury categories and/or scores. 2009. https://ideas.repec.org/c/boc/bocode/s457028.html Version S457028.
- 20. Greenland S, Robins JM. Empirical-Bayes adjustments for multiple comparisons are sometimes useful. Epidemiology 1991;2:244–51. [DOI] [PubMed] [Google Scholar]
- 21. Joinpoint Regression Program. Statistical Methodology and Applications Branch SRP. Version 4.5.0.1 Rockville, Maryland: National Cancer Institute; ed2017. [Google Scholar]
- 22. Farst K, Ambadwar PB, King AJ, Bird TM, Robbins JM. Trends in hospitalization rates and severity of injuries from abuse in young children, 1997-2009. Pediatrics 2013;131:e1796–802. doi:10.1542/peds.2012-1464 [DOI] [PubMed] [Google Scholar]
- 23. Missikpode C, Peek-Asa C, Young T, Swanton A, Leinenkugel K, Torner J. Trends in non-fatal agricultural injuries requiring trauma care. Inj Epidemiol 2015;2:30 doi:10.1186/s40621-015-0062-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. de Guise E, LeBlanc J, Dagher J, Tinawi S, Lamoureux J, Marcoux J, Maleki M, Feyz M. Trends in hospitalization associated with TBI in an urban level 1 trauma centre. Can J Neurol Sci 2014;41:466–75. doi:10.1017/S0317167100018503 [DOI] [PubMed] [Google Scholar]
- 25. Davis JS, Castilla DM, Schulman CI, Perez EA, Neville HL, Sola JE. Twenty years of pediatric gunshot wounds: an urban trauma center’ s experience. J Surg Res 2013;184:556–60. doi:10.1016/j.jss.2012.12.047 [DOI] [PubMed] [Google Scholar]
- 26. Agarwal S. Trends and burden of firearm-related hospitalizations in the United States across 2001-2011. Am J Med 2015;128:484–92. doi:10.1016/j.amjmed.2014.12.008 [DOI] [PubMed] [Google Scholar]
- 27. Smith VM, Siegel M, Xuan Z, Ross CS, Galea S, Kalesan B, Fleegler E, Goss KA. Broadening the perspective on gun violence: an examination of the firearms industry, 1990-2015. Am J Prev Med 2017;53:584–91. doi:10.1016/j.amepre.2017.05.002 [DOI] [PubMed] [Google Scholar]
- 28. Livingston DH, Lavery RF, Lopreiato MC, Lavery DF, Passannante MR. Unrelenting violence: an analysis of 6,322 gunshot wound patients at a Level I trauma center. J Trauma Acute Care Surg 2014;76:2–9. doi:10.1097/TA.0b013e3182ab19e7 [DOI] [PubMed] [Google Scholar]
- 29. Rubano JA, Paccione MF, Rutigliano DN, Vosswinkel JA, McCormack JE, Huang EC, Yang J, Shapiro MJ, Jawa RS, Shaprio YJ. Outcomes following prolonged mechanical ventilation: analysis of a countywide trauma registry. J Trauma Acute Care Surg 2015;78:289–94. doi:10.1097/TA.0000000000000515 [DOI] [PubMed] [Google Scholar]
- 30. Sise RG, Calvo RY, Spain DA, Weiser TG, Staudenmayer KL. The epidemiology of trauma-related mortality in the United States from 2002 to 2010. J Trauma Acute Care Surg 2014;76:913–9. doi:10.1097/TA.0000000000000169 [DOI] [PubMed] [Google Scholar]
- 31. Joseph B, Aziz H, Pandit V, Kulvatunyou N, O’Keeffe T, Wynne J, Tang A, Friese RS, Rhee P. Improving survival rates after civilian gunshot wounds to the brain. J Am Coll Surg 2014;218:58–65. doi:10.1016/j.jamcollsurg.2013.08.018 [DOI] [PubMed] [Google Scholar]
- 32. Barmparas G, Dhillon NK, Smith EJT, Tatum JM, Chung R, Melo N, Ley EJ, Margulies DR. Assault in children admitted to trauma centers: injury patterns and outcomes from a 5-year review of the national trauma data bank. Int J Surg 2017;43:137–44. doi:10.1016/j.ijsu.2017.05.068 [DOI] [PubMed] [Google Scholar]
- 33. DiMaggio CJ, Avraham JB, Lee DC, Frangos SG, Wall SP. The epidemiology of emergency department trauma discharges in the United States. Acad Emerg Med 2017;24:1244–56. doi:10.1111/acem.13223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Cook PJ, Rivera-Aguirre AE, Cerdá M, Wintemute G. Constant lethality of gunshot injuries from firearm assault: United States, 2003-2012. Am J Public Health 2017;107:1324–8. doi:10.2105/AJPH.2017.303837 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Cook PJ, Rivera-Aguirre AE, Cerda M, Wintemute G. The "hidden epidemic of firearms injury" is an artifact of problems with the data. Am J Epidemiol. In Press 2017. [DOI] [PubMed] [Google Scholar]
- 36. Richardson JD, Davidson D, Miller FB. After the shooting stops: follow-up on victims of an assault rifle attack. J Trauma 1996;41:789–93. [DOI] [PubMed] [Google Scholar]
- 37. Barell V, Aharonson-Daniel L, Fingerhut LA, Mackenzie EJ, Ziv A, Boyko V, Abargel A, Avitzour M, Heruti R. An introduction to the Barell body region by nature of injury diagnosis matrix. Inj Prev 2002;8:91–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
tsaco-2017-000139supp001.docx (147.2KB, docx)