Highlights
-
•
A framework which integration national Electronic Healthcare Record datasets from England, Scotland and Wales is proposed.
-
•
Variable similarity is used to develop a schema which allows for variables to be linked and combined across the nations.
-
•
Evaluation of integration shows that it is possibly to perform data linkage across the nations.
Abbreviations: A&E, accident and emergency; APC, admitted patient care; CHI, community health index; DOB, date of birth; EHRs, electronic healthcare records; HES, health episode statistics; ISD, information services division; ICD-10, international classification of diseases, 10th revision; KCMHR, King’s College Centre for Military Health Research; NHS, National Health Service; OPCS-4, OPCS classification of interventions and procedures version 4; SAIL, secure anonymised information linkage; UK, United Kingdom
Keywords: Hospital episode statistics, Electronic health records, Hospital admission, Secondary care, Big data, Data linkage
Abstract
Background
Electronic Healthcare Records (EHRs) are created to capture summaries of care and contact made to healthcare services. EHRs offer a means to analyse admissions to hospitals for epidemiological research. In the United Kingdom (UK), England, Scotland and Wales maintain separate data stores, which are administered and managed exclusively by devolved Government. This independence results in harmonisation challenges, not least lack of uniformity, making it difficult to evaluate care, diagnoses and treatment across the UK. To overcome this lack of uniformity, it is important to develop methods to integrate EHRs to provide a multi-nation dataset of health.
Objective
To develop and describe a method which integrates the EHRs of Armed Forces personnel in England, Scotland and Wales based on variable commonality to produce a multi-nation dataset of secondary health care.
Methods
An Armed Forces cohort was used to extract and integrate three EHR datasets, using commonality as the linkage point. This was achieved by evaluating and combining variables which shared the same characteristics. EHRs representing Accident and Emergency (A&E), Admitted Patient Care (APC) and Outpatient care were combined to create a patient-level history spanning three nations. Patient-level EHRs were examined to ascertain admission differences, common diagnoses and record completeness.
Results
A total of 6,336 Armed Forces personnel were matched, of which 5,460 personnel had 7,510 A&E visits, 9,316 APC episodes and 45,005 Outpatient appointments. We observed full completeness for diagnoses in APC, whereas Outpatient admissions were sparsely coded; with 88% of diagnoses coded as “Unknown/unspecified cause of morbidity”. In addition, A&E records were sporadically coded; we found five coding systems for identifying reason for admission.
Conclusion
At present, EHRs are designed to monitor the cost of treatment, enable administrative oversight, and are not currently suited to epidemiological research. However, only small changes may be needed to take advantage of what should be a highly cost-effective means of delivering important research for the benefit of the NHS.
1. Background
Routinely collected Elxectronic Healthcare Records (EHRs) can be used to evaluate disease prevalence, tendencies, and to perform epidemiological analyses [1]; investigate quality of care and to improve clinical decision-making, which can influence patient outcome and care [[2], [3]]. In recent years, there has been a growth in the use of EHRs in the field of Big Data analytics, which is the analysis and evaluation of large datasets, to answer specific research questions [[4], [5]]. The term “Big Data” [6] has been used in a number of health settings, it is synonymous with the meaningful analyses of EHRs to identify health movements and associations [7]. Further, Schneeweiss et al. [8] summarises the potential applications into two key areas: generation of knowledge to improve the effectiveness of treatment; and to predict the outcome of treatment and diagnoses.
Globally, the development and use of EHRs is increasing, alongside Big Data innovation in a number of fields [[8], [9], [10]]. Standardised EHR systems are difficult to implement in larger countries, those which have complex political structures or multiple private entities [11], such as the United States. In the United Kingdom (UK), health and social care is devolved to national Government and local agencies using propriety systems which are not interconnected or able to identify patients who relocate from a nations [[11], [12], [13]]. In the UK, it is estimated that 53,000 individuals migrate from England and Wales to Northern Ireland and Scotland; with 46,800 individuals migrating from Northern Ireland and Scotland to England and Wales each year [14]. At present, migration statistics are not reported separately, making it difficult to determine cross-border migration. EHRs which represent the same patient across the three nations show great promise and could be used to identify risk, inform healthcare policy, service provision and improve health and social outcomes [[13], [15], [16]]. Using a cross-border cohort might provide the foundation of creating such a system. While several studies have sought to create national datasets of health and social care [[4], [17]], to our knowledge, no studies exist which integrate EHRs from multiple nations into a single repository for research.
There are multiple challenges in integrating EHRs in the UK. Firstly, there is no system or framework which uniquely identifies a person (e.g. unique ID number for each citizen) across public services such as welfare, housing, education and health [18]. Those registered with the National Health Service (NHS) of England and Wales are assigned a unique 10-digit number, which is used as the sole identifier in healthcare [19]. Similarly, in Scotland a person is assigned a Community Health Index (CHI) number which is used in the same manner. Second, EHRs provided by England [20], Wales [[4], [17]] and Scotland [21] are distinctive in structure, collection and management. Third, EHR data from each of these data sources include various data types, from structured information such as drug prescriptions, diagnoses and treatment, to unstructured data such as clinical notes and patient self-reported illness [11]. Finally, there is a dearth of literature which describes how to undertake EHR data linkage from multiple data sources [22].
Current research efforts have been directed towards modelling and predicting single conditions (e.g. depression, diabetes and epilepsy) and outcomes [[3], [16], [23], [24]]. In this work, we study a UK Armed Forces cohort [[25], [26]] (which includes individuals from England, Scotland and Wales) that has been linked separately to three sources of national secondary healthcare data. These data have then been integrated to form a patient-level dataset across 3 nations which include A&E, Outpatient Care and Admitted Patient Care (APC). The subsequent dataset is unique, population-based longitudinal dataset that contains a wide range of physical and mental health indicators of serving and ex-serving UK Armed Forces personnel. The objectives of this work are; 1) to develop and describe a methodology which integrates EHRs of Armed Forces personnel in England, Scotland and Wales 2) examine healthcare utilisation within these data and 3) evaluate characteristics of admission, record completion and diagnoses.
2. Methods
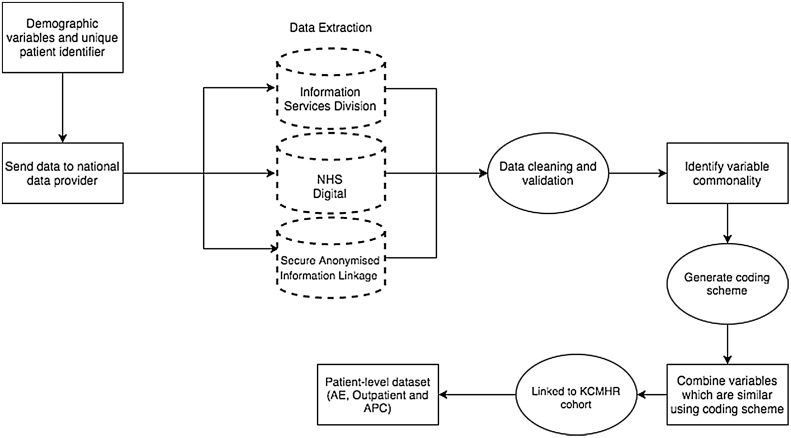
The proposed framework is illustrated in Fig. 1, and is represented by the following stages:
-
1.
Demographic identifiers of Armed Forces personnel are sent to each data provider;
-
2.
EHRs are extracted and sent to the research team by data providers;
-
3.
EHRs are cleaned and validated;
-
4.
Variables are linked using commonality;
-
5.
EHRs for each patient are integrated to generate a patient-level dataset.
Fig. 1.
Overview of the data linkage process and formation of patient-level dataset.
2.1. King’s centre for military health research (KCMHR) cohort
UK Armed Forces personnel receive all secondary care from the NHS while in service in the UK and after they have left service from the NHS. This study uses the example of an Armed Forces population to integrate data from England, Scotland and Wales. The reasons for this are 1) they frequently move/relocate, so it is important to capture EHRs from across the nations and 2) they may have different health needs due to being exposed to a high level of physical and mental strain. This study used the KCMHR cohort, which is a longitudinal cohort of the UK Armed Forces (full details of the methods and sample description were previously reported in [[25], [26]]), to develop methodologies to integrate EHR data. Briefly, data was collected in 2004–2006 from a sample of personnel deployed to the Iraq war during 2003 and from a sample of personnel serving in the UK Armed Forces but who did not deploy at that time (phase 1). Phase 1 participants were then followed up in 2007–2009, where two new samples were introduced to represent the demographics of the Armed Forces at that time point (phase 2). Individuals who took part in phase 1 only were not included in the study as they had not been asked for consent to access their medical records. Participants were only included in the study if they provided content for us to access their medical records, but the authors also sought and obtained a section 251 of the National Health Service Act 2006 [27] approval to allow transfer of confidential participant information to data providers for processing (to facilitate data linkage). In total, 86.11% of phase 2 respondents provided informed consent to access their healthcare records, resulting in a final cohort of 8,602. The consenting cohort available for data extraction and integration comprised 7,661 (89.06%) males and 941 (10.94%) females, which is in line with the demographics of the UK Armed Forces.
2.2. Data providers
EHRs are managed by NHS Digital in England [20], Secure Anonymised Information Linkage (SAIL) in Wales [[4], [17]] and Information Service Division (ISD) in Scotland [21]. Table 1 illustrates the datasets, periods of interest and requested number of variables. Variables that were comparable (e.g. similar in content and type) between data providers were requested. Where available, data was requested for the financial years 2003/04 to 2013/14 or closest available.
Table 1.
Defines the terminology used by data providers, data periods of interest and number of variables requested.
| Terminology | NHS Digital | Secure Anonymised Information Linkage (SAIL) | Information Services Division (ISD) | |
|---|---|---|---|---|
| Accident and Emergency (A&E) | Year range | 2007/08–2013/14 | 2009/10–2013/14 | 2003/04–2013/14 |
| Dataset | Accident and Emergency | Emergency Department Data Set | Accident and Emergency | |
| Variable Count | 142 | 69 | 42 | |
| Admitted Patient Care (APC) | Year range | 2003/04–2013/14 | 2003/04–2013/14 | 2003/04–2013/14 |
| Dataset | Admitted Patient Care | Patient Episode Database for Wales | Scottish Morbidity Records 01 | |
| Variable Count | 265 | 115 | 36 | |
| Outpatient | Year Range | 2003/04–2013/14 | 2004/05–2013/14 | 2003/04–2013/14 |
| Dataset | Outpatient | Outpatient | Outpatient | |
| Variable Count | 96 | 46 | 32 | |
2.3. Extracting electronic healthcare records
Data extraction was performed independently of the authors through the data providers to preserve privacy. Providers were supplied a set of demographic variables; 10-digit NHS number (where available), first name, middle name, surname, gender and date of birth (DOB). When providing extracted data, providers removed all demographic identifiers (e.g. first name, last name); to enable identification the authors supplied a unique identifier to represent each participant. For clarity, the extraction process is described hereafter, data extraction had no impact on the creation of the framework or integrated datasets.
NHS Digital required a valid NHS number to identify any individual and extract Health Episode Statistics (HES) EHR data. Valid NHS numbers were mapped with an internal identifier, the HES ID. EHRs were extracted if any of the following conditions were met: (1) match on NHS number, gender and DOB; (2) match on NHS number, partial match for gender or DOB; (3) match on NHS number only.
SAIL operated a two-stage extraction process to preserve privacy. First, demographic variables were supplied by the Data Provider to NHS Wales Informatics Service [28] where they were cross-referenced using a fuzzy matching procedure to create the Anonymised Linkage Field (a unique SAIL databank identifier). Second, NHS Wales Informatics Service supplied the Anonymised Linkage Field to the SAIL databank to join with record details provided to SAIL to produce an anonymised version of each dataset, linkable at the individual level to EHR datasets within SAIL.
ISD did not require a NHS/CHI number for matching. Participant demographics were cross-matched using probabilistic linking to identify a) valid NHS/CHI number; b) to confirm the NHS/CHI number is valid. EHRs which belonged to a valid CHI number were identified and extracted.
Data from each provider was supplied in financial year using a comma separate file format.
2.4. Developing the integrated dataset using variable commonality
The datasets contain many variables (Table 1); however, it is not practical to directly link, integrate, or combine variables which may be named or categorised differently. To overcome this, we assessed variable commonality; defined as those variables which represent similar data mediums but categorised in a different manner. The framework solely categorised variables based on the data they hold. For example, each dataset contained a variable which identified speciality; however, the coding schemes were different, therefore a new coding scheme was developed to be usable across all data providers. Table 2 defines the variable categories of interest. Variables which did not match the definition, or were only available for one data source were not selected unless they contributed and provided valuable insight (e.g. method of admission). Discussions were held within the research team to discuss variable categorisation, matching and development of coding schemes.
Table 2.
Stipulates the definition used for associating variables to a commonality category.
| Category | Criteria |
|---|---|
| Admittance/Discharge | Variables that provide information on the admission and discharge of a patient. This includes admission and discharge date, episode information, time of admission, source of admission and destination of patient upon discharge. |
| Diagnosis/Classification | Variables that provide information on the diagnosis of the patient, including ICD-10 coding and date of diagnosis, A&E coding or local diagnoses coding system. |
| Treatment/Procedure/Investigation | Variables that provide information on the treatment/procedures undertaken, including OPCS Classification of Interventions and Procedures version 4 coding, or local diagnoses coding system. |
| Care Provider | Variables that provide information on the provider of care, including geographical location and provider type. |
| Care Speciality | Variables that provide information on the speciality of care, including consultant association, department of care and clinical staff role. |
| Costing/Resources | Variables that provide information on the cost of care, including cost of treatment, staffing costs and direct costs incurred by the care provider. |
NHS Digital (HES datasets), the largest data provider of EHRs in the UK, was selected as the anchor for comparison to other datasets.
Variable commonality was undertaken in three stages. First, individually for each data provider; A&E, APC and Outpatient variables were grouped using the categories defined in Table 2. Second, variables that matched across the datasets were identified (e.g. admission date, discharge date, diagnoses and treatment). Finally, variables that were similar in nature were identified and a common coding scheme was developed to reflect coding schemes used by data providers (e.g. source of admission, source of discharge and source of injury) with the objective of having a single coding scheme. Supplement 1 outlines variables linked for each dataset and data provider.
Admitted Patient Care EHRs across the data providers, include details of the patient, when they were treated, where they were treated and what they were treated for. As illustrated in Table 1, APC records contain the largest number of variables compared to other departments. Variables identified include admission/discharge date, care provider, speciality and costing codes. For variables such as consultant speciality and admission/discharge source a national coding scheme was used. We developed a common coding scheme which was inclusive and representative of national coding schemes. Codes which were ambiguous or not an identical match to other nations were retained. Primarily, diagnoses were coded using the International Classification of Diseases, 10th revision (ICD-10) and interventions and procedures are coded using OPCS Classification of Interventions and Procedures version 3 or 4 (OPCS-4).
Outpatient appointments were recorded across the data providers, including appointment date, appointment treatment, care provider and outcomes. Variables differed widely across the data providers due to service provision and method of recording the visit. Variables identified for joining included appointment date, status of appointment attendance, diagnosis and speciality. For variables such as attendance type and appointment source, a common coding scheme was developed bringing together individual nation coding schemes. Codes which were ambiguous (without a suitable definition) or not an identical match were retained separately. Diagnoses, interventions and procedures were coded using ICD-10 and OPCS across the data providers.
Accident and Emergency attendance was recorded differently across the data providers, and for NHS Digital HES data were different between hospital trusts. Variables such as admission date, treatment time, conclusion time and discharge time/location were linked based on commonality. Major differences were observed when coding the reason for the visit to A&E; unlike APC, which utilises the ICD-10 coding system across the combined dataset, A&E does not use a national standard. For example, within England, care providers utilise a local coding system, ICD-10 coding or a NHS England coding standard [[29], [30]].
2.5. Integrated patient record and data cleaning
A patient-level EHR dataset was constructed using a five-stage integration process. First, Continuous Inpatient spells were computed for APC in HES, ISD and SAIL separately. A Continuous Inpatient spell is considered as a continuous period of care within the NHS, regardless of any transfers between care providers that may take place [31]; it can comprise one or more providers but starts when a decision has been made to admit the patient (admission date), and ends when the patient dies or is discharged from hospital (discharge date). APC records are treated differently to other EHRs (e.g. A&E, Outpatient) as a patient can have multiple episodes of care relating to a single admission into hospital. Second, admission and discharge date (A&E, Outpatient and APC) were checked to ensure consistency and that a valid date was present. Third, duplicate records (A&E, Outpatient and APC) relating to the same period of care or admission were identified and excluded. Fourth, EHR (A&E, Outpatient and APC) for the same individual were brought together within HES, SAIL and ISD to create a personal admission history for England, Wales and Scotland respectively using the unique identifier. Finally, admission history across the nations was merged to the KCMHR Armed Forces cohort to create a patient-level history for A&E, APC and Outpatient care.
2.6. Data analysis
This work compared the matched sample (n = 6,336) with the non-matched sample (n = 2,266) to assess differences on a range of demographic factors. Analyses including median and frequencies were computed in Stata 12 [32]. In addition, the following descriptive analyses were performed:
-
•
Linkage rate overall and by nation were computed using record matching information supplied by national data providers. The analyses were undertaken using those who gave consent for their medical records to be accessed (n = 8,602). Results were presented as frequency and percentage values. Students’ t-test was performed to identify significance in the matching.
-
•
Departmental utilisation was calculated based on the number of visits a patient made to the department. Gender frequencies and percentages were computed to provide a breakdown of departmental admissions.
-
•
Common conditions were calculated by summing the number of events for each 3-digit ICD-10 code and represented as a frequency. Gender frequencies and percentages were computed for each common condition.
-
•
The total numbers of hospital visits were calculated by summing the number of events per participant matched for each department. The frequency, median and inter-quartile range (IQR) were computed at the patient-level as the data was not normally distributed.
-
•
Variable completeness was calculated as the number of valid variable entries compared to missing or null entries (where 0 is treated as a valid entry). Valid variable entries were represented by records which have a value which is not null or missing. Results were presented as percentages.
It should be noted that the unit of analysis is the patient, rather than hospital, geographical region or nation.
3. Results
3.1. Overview of the data linkage
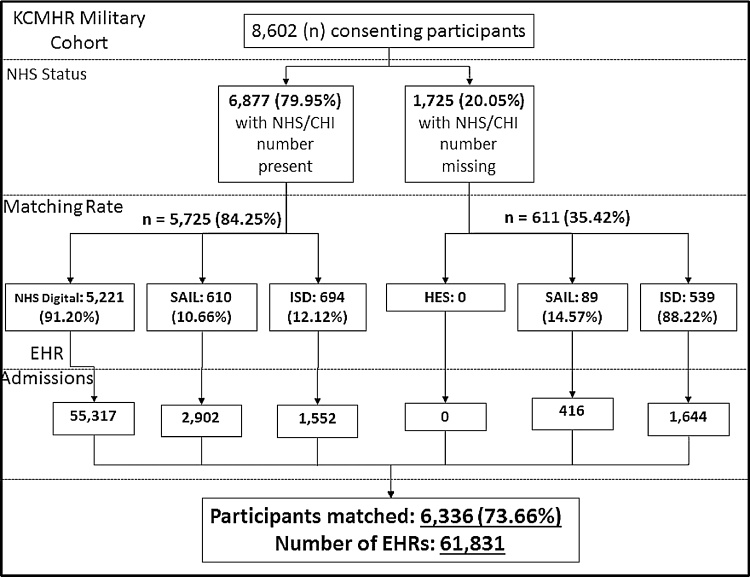
The completeness of demographic variables, which may impact data extraction, contained within the KCMHR Armed Forces cohort is presented in Table 3. The number of participants matched was 6,336 (74%) as illustrated in Fig. 2. The proportion matched was greater in those with a NHS/CHI number compared to those without, with the latter restricted to matching in Wales and Scotland. This was due to the NHS Digital in England requiring a valid NHS number for matching (blocking variable). Of individuals matched, 4,460 were matched in England only (71%), 257 were matched in Wales only (4%), 826 in Scotland only (13%) and 793 were matched in more than one nation (12%). 5,460 participants had a hospital contact during the period of interest.
Table 3.
Completeness of KCMHR demographics (n = 8,602). 1NHS/CHI number is complete if length is greater than 8. CHI number serves the same purpose as NHS number for Scotland. 2Valid if length 1 or greater. 3Valid if date of birth is present e.g. DD/MM/YY or DD/MM/YYYY.% represents row percentages.
| NHS Number/CHI Number1 | Initial | Forename2 | Surname2 | Gender | Date of Birth3 | |
|---|---|---|---|---|---|---|
| Variable Completeness | 6877 (79.95%) | 8179 (95.08%) | 8413 (97.8%) | 8602 (100%) | 8602 (100%) | 8597 (99.94%) |
| Missing Values | 1725 (20.05%) | 423 (4.92%) | 189 (2.2%) | 0 | 0 | 5 (0.06%) |
Fig. 2.
Data extraction, number of participants matched and the total number of EHR for each data source divided by those with and without an NHS/CHI number. Note: A participant can appear in multiple nation data providers. Percentage figures are cascading, where the percentage is out of the preceding value.
3.2. Overview of healthcare utilisation
The highest proportion of hospital visits recorded for England was 5,221 participants compared to Scotland with 1,233 participants or Wales with 699 participants (Fig. 2). The overall number of hospital episodes for each nation and department is presented in Table 4. In summary, A&E had a median of 2 (interquartile range [IQR] 2) admissions per participant, APC had a median of 2 (IQR: 2) episodes per participant and Outpatient had a median of 5 (IQR: 8) appointments per participant.
Table 4.
Represents the number of episodes and participant numbers for each department and nation. Percent values represent the percentage of the matched sample (n = 6336).
| Department | NHS Digital | Secure Anonymised Information Linkage | Information Services Division | |
|---|---|---|---|---|
| Accident and Emergency | Episodes | 6775 | 392 | 343 |
| Participant | 2873 (45.44%) | 163 (2.77%) | 206 (3.25%) | |
| Admitted Patient Care | Episodes | 7516 | 444 | 577 |
| Participant | 2970 (46.77%) | 176 (19.3%) | 251 (3.96%) | |
| Outpatient | Episodes | 41,026 | 1703 | 2276 |
| Participant | 4300 (67.87%) | 240 (3.79%) | 435 (6.87%) | |
3.3. Healthcare utilisation and diagnoses in accident and emergency
A total of 3,192 participants had 7,510 admissions to A&E (2,813 (88.13%) males and 379 (11.87%) females). 253 variables were available for linkage, we derived 102 common variables. Out of the admissions to A&E, 90.32% were discharged or transferred to a ward on the day of admission, with 9.62% spending at least 24 h within A&E. There were five methods identified for recording reason for an admission; for England: ICD-10, local coding and regional coding schemes, Wales: ICD-10 and regional coding schemes, finally Scotland: ICD-10 and free-text input. The most common mode of attendance was self-presentation (75.50%) followed-by road ambulance (7.49%) and then hospital transfer (6.52%).
Variable completeness of the original data providers (Table 1), measured as a valid value being present was 47.12% (Table 5). This reflects a code presence of less than 60% for A&E admissions with Reason for Admission, Treatment and Investigation. It is important to note that Reason for Admission relates to the presenting complaint(s) of the patient upon admission, in England up to 12 can be recorded. As illustrated in Table 5, completeness for Reason for Admission was 56.43%, meaning that almost half of all admissions did not have any presenting complaint or assigned diagnoses. Conversely, variables related to the patient admission, care provider and cost were consistently coded (>90%).
Table 5.
Variable completeness for a sample of common variables formed in England, Scotland and Wales.
| Data Source | Common Variable (national assigned variable name) | NHS Digital | Information Services Division | Secure Anonymised Information Linkage |
|---|---|---|---|---|
| Accident & Emergency | Reason for Admission1 | 42.44% | 67.93% | 58.93% |
| Attendance Category (attendance_cat) | 100% | 100% | 100% | |
| Admission Time (time_arrival) | 87.13% | 93.76% | 90.51% | |
| Arrival Mode (arrival_mode) | 100% | 97.96% | 100% | |
| Provider Code (provider_code) | 100% | 100% | 100% | |
| Admitted Patient Care | Primary (1st) Diagnosis (diag_01) | 100% | 100% | 100% |
| Admission Source (admin_source) | 98.59% | 100% | 100% | |
| Main Speciality (main_speciality) | 100% | 97.13% | 98.08 | |
| Operation (oper_01) | 100% | 72.62% | 68.52% | |
| Discharge Method (dist_meth) | 100% | 77.34% | 79.09% | |
| Outpatient | Attend (attended) | 100% | 77.07% | 80.28% |
| Attended Type (attend_type) | 100% | 100% | 100% | |
| Main Speciality (main_ speciality) | 100% | 100% | 100% | |
| Referral Source (ref_source) | 100% | 78.60% | 100% | |
| Diagnosis (diag_01)2 | 97.98% | 100% | 100% |
Represents a group of variables which describe the anatomical area, side body and presenting diagnosis.
“Unknown and unspecified causes of morbidity” assigned to 87.57% of all appointments.
3.4. Healthcare utilisation and diagnoses in admitted patient care
A total of 3,324 participants had 9,316 episodes, 2,842 were male (85.50%) and 482 were female (14.50%); 416 variables were present from the nations, with 89 common variables identified to represent a single episode. Overall, variable completeness across the derived dataset, in terms of a value being present was 78.06% (Table 5). All episodes were recorded with at least one diagnosis using ICD-10 coding scheme with full completeness across all three nations. There was high variable completeness amongst Admittance, Diagnosis/Classification and Care Speciality variable groups (>85%). Conversely, variables related to the patient discharge, episode order and cost were more likely to be missing data (<80%).
Unlike A&E or Outpatient EHR, each record was accompanied by a diagnosis; completeness was 100%. In this population, 17,541 individual ICD-10 diagnoses, representing 963 ICD-10 (3-digit) disease groups including primary and secondary diagnoses were recorded. Aggregating the ICD-10 code Z51 representing “Other medical care” was the most common (Table 6). Predominately, males across all codes are more likely to be admitted than females (except in the event of “Outcome of Delivery” which relates to child birth); this is not unexpected, as the cohort is largely male. The most common source of an admission was the residential home of the patient (90.07%) and other NHS hospitals was the second most common source (8.08%). Five participants died during a hospital episode.
Table 6.
Most common ICD-10 codes assigned during Admitted Patient Care visit with gender comparison.
| ICD-10 Code | Description | Occurrence (n = participants) | Male (n = 874) | Female (n = 109) | |
|---|---|---|---|---|---|
| 1 | Z51 | Other medical care | 490 (n = 116) | 99 (85.34%) | 17 (14.66%) |
| 2 | Z86 | Personal history of certain other diseases | 336 (n = 190) | 159 (83.68%) | 31 (16.32%) |
| 3 | I10 | Essential (primary) hypertension | 295 (n = 151) | 140 (92.72%) | 11 (7.28%) |
| 4 | Z37 | Outcome of delivery | 281 (n = 198) | 0 | 198 (100%) |
| 5 | Z30 | Contraceptive management | 272 (n = 262) | 247 (94.27%) | 15 (5.73%) |
| 6 | R10 | Abdominal and pelvic pain | 266 (n = 221) | 155 (70.14%) | 66 (29.86%) |
| 7 | M23 | Internal derangement of knee | 265 (n = 217) | 208 (95.85%) | 9 (4.15%) |
| 8 | F17 | Mental and behavioural disorders due to use of tobacco | 259 (n = 190) | 168 (88.42%) | 22 (11.58%) |
| 9 | Z72 | Problems related to lifestyle | 253 (n = 197) | 183 (92.89%) | 14 (7.11%) |
| 10 | M54 | Dorsalgia | 222 (n = 123) | 102 (82.93%) | 21 (17.07%) |
3.5. Healthcare utilisation and diagnoses in outpatient services
A total of 4,810 participants had 45,005 appointments, with 4,178 (86.86%) male and 632 (13.14%) female. Multiple coding systems were employed to encode diagnoses of an outpatient visit, including ICD-10 and free text. The most common ICD-10 code is R69, defined as “Unknown and unspecified causes of morbidity” assigned to 87.57% of all appointments. Only 5.16% of appointments were not coded with any type of diagnosis. England had the largest number of visits with a proportion of 91.34% compared to Scotland 4.72% and Wales 3.94%.
In total, 174 variables, which represent all three nations, were grouped resulting in 46 common variables being defined. Overall completeness of the derived variables, in terms of a value being present was an average of 57.11% (Table 5). Appointments were coded with an appointment date, with the reason for attendance fully coded. Conversely, there was poor coding for appointment waiting time, priority status, diagnoses and speciality (<70%).
4. Discussion
Our work introduces a framework to integrate data from national providers to produce a combined dataset of secondary health for serving and ex-serving Armed Forces personnel. This work can also be applied to other settings and populations. We have shown that a linked dataset containing national EHRs can be created and used to evaluate healthcare utilisation across England, Scotland and Wales. However, it is important to acknowledge that we do not know how many persons with an admission were not detected due to the matching and extraction methodology employed by data providers. Using linked EHRs, clinicians and researchers can monitor and improve admissions, quality of care, improve clinical decision making, and to influence patient outcomes and care. We have been able to use the data to show the frequency of APC, Outpatient and A&E visits, diagnosis and arrival mode for Armed Forces personnel. Conversely, we have identified disparities between data providers and their methods of recording, validating and storing of data which has been shown to impact data quality and reliability. Similarly, data completeness and accuracy in assigning presentation or diagnoses code values are of concern in A&E and Outpatient data across the nations. For Outpatient EHRs, diagnoses and main procedure variables were not a mandatory requirement, however recording is increasing over time [33]. Nevertheless, APC has been shown to consist of valid data points including diagnoses, treatments and operations, and admission/discharge dates. To our knowledge, this is the first to both link secondary care datasets across England, Scotland and Wales and to analyse Armed Forces personnel EHR data.
The ability to obtain EHR from multiple national providers and integrate to an existing cohort allows greater insight into patient admission patterns and history [[2], [34], [35]]. However, EHRs alone do not provide sufficient context to enable detailed evaluation of the data and therefore additional data providers and cohorts (e.g. National Joint Registry [36], Cancer Registry [37]) are used to provide personal identifiers. The Hertfordshire Cohort Study [3] linked hospital admissions to an existing cohort, the study was limited to a single English county (Hertfordshire county). The authors had difficulty obtaining EHRs for the cohort, similar to our own difficulties with national data providers performing data linkage using different algorithms. In Scotland, the Scottish Health Surveys Cohort [5] is an example of a data linkage between a cohort and health and social care in secondary care. The study linked Outpatient, APC, Mental Health and Outpatient records at the patient-level to provide detailed healthcare patterns.
4.1. Limitations and challenges for sustainability
For our methodology to be a functional resource it is important to be aware of the limits of health data and integration. Personal identifiers were obtained via the KCMHR cohort study, with permission from participants, and included participants’ first name, last name, date of birth gender, and National Health Number which can be difficult to obtain and record correctly. NHS number was not available for 20.05% of participants. The matching process undertaken by NHS Digital set NHS number as a mandatory variable, resulting in a lower success rate. However, ISD in Scotland and SAIL in Wales did not place this same requirement. We did not request data from Northern Ireland. This was because of the complex structures surrounding EHRs in Northern Ireland. No central organisation is responsible, instead it is delegated to the local trust. In addition, there are security concerns surrounding former Armed Forces personnel.
There are several problems with using national EHR datasets such as HES, ISD or SAIL when integrating these datasets. The complexity of gathering data at data centres and the large number of organisations and institutions which can provide submissions can give rise to reduced accuracy of the EHR including diagnoses, outcomes and patient management [[38], [39]]. Further, completeness of records is poor, particularly in Outpatient and A&E EHRs, giving rise to difficulty in linking variables and making any statistical analyses troublesome [[3], [5], [24]].
We were limited to the variables requested and provided by national data providers, to enable linkage. We undertook a pragmatic approach to matching variables based on commonality using variable definitions provided by the data providers. This is a time-consuming exercise, and might prove an obstacle in even larger datasets. Further, national coding schemes, may have been interpreted differently by hospital trust and coder leading to additional confusion and coding bias. It is important to be aware that though EHRs are widely used in research, offering a broad range of information about treatment, diagnoses and care, there are issues relating to determining data quality, completeness of data and drawing conclusions from the data [[40], [41], [42]].
4.2. Unanswered questions and future developments
Our initial examination of the dataset has proved useful in identifying the most common diagnoses, types of A&E admissions and number of Outpatient appointments for Armed Forces personnel. Further analysis of the dataset is required to evaluate clinical practices, common diagnoses stratified by patient characteristics and variable coding accuracy to improve dataset recording and retention. This could include assessing A&E trends in admission, prevalence of A&E admissions resulting in an APC episode and waiting times. Alternately, further data linkage to primary healthcare records might make it possible to identify pre and post follow-up health of individuals who have had a contact with secondary care. This could improve the quality of analysis and enable refinement of queries used on the dataset to improve the quality of the dataset.
In the future, there is potential to develop a more responsive, real-time and useful linked dataset based on the framework and methodologies presented in this work. This would require more regular and frequent updates from data providers, including more efficient data linkage of cohort users.
5. Conclusions
It was possible to integrate secondary health records to create a combined dataset of attendances to NHS hospitals in England, Scotland and Wales. This is the first to combine and present analyses of EHRs from Armed Forces personnel in the UK (excluding Northern Ireland). The dataset was developed using variable commonality and included both serving and ex-serving Armed Forces personnel, enabling evaluation of healthcare utilisation. The NHS of England, Scotland and Wales obtain, store and process EHRs using different methodologies. Scotland and Wales utilise participant demographics without the need of a NHS number whereas matching in England requires an NHS number. Future work should seek to harmonise the protocols for national linkage and seek a uniform UK-wide policy on EHRs for research. The increasing shift towards the use of EHR by health trusts presents an opportunity to monitor admissions, diagnoses and outcomes to inform public health policy and service provision.
Ethical approval and consent to participate
Ethical approval was obtained from the London-Dulwich NHS Research Ethics Committee in November 2014 (REC no: 07/Q0703/36). Further, a Section 251 of the National Health Service Act 2006 (Ref no: 15/CAG/0136) was obtained.
Consent for publication
None required.
Availability of data and materials
Coding schemes and syntax used to perform data linkage are available upon request from the corresponding author.
Fundings
This work is funded by the Economic and Social Research Council (grant number ES/L014521/1), DL and ZC were funded by the grant. Over the course of this work RDH was funded by a Medical Research Council Population Health Scientist Fellowship (grant number MR/J01219X/1). RDH and SL have received salary support from the National Institute for Health Research Mental Health Biomedical Research Centre at South London and Maudsley NHS Foundation Trust and King’s College London. The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health.
Conflict of interest
RDH has received research funding from Roche, Pfizer, Janssen, Lundbeck and In-Silico-Bioscience. SW is advisor to the British Army in psychiatry and a trustee of Combat Stress. This work was undertaken prior to NTF’s appointment to the Independent Group Advising on the Release of Data. NTF is a trustee of The Warrior Programme. DL, ZC, SL, PM, MJ and LG declare that they have no competing interests.
Author contributions
DL conducted the data linkage, data analysis and wrote all drafts of the manuscript. ZC provided advice on the data linkage, commented on drafts of the paper. MJ has provided guidance during the work and commented on drafts of the paper. SL, PM, RDH, SW and NTF participated in design of the work and commented on drafts of the paper. LG designed the work, sought and obtained funding, oversaw data collection, analysis, linkage and commented on all drafts of the paper. All authors have read and approved the final manuscript.
Summary table.
What was already known?
-
•
Electronic Healthcare Records are used to capture summaries of care and contact to healthcare services; in the United Kingdom they are intended to financially reimburse hospital trusts for care provided.
-
•
In the United Kingdom; England, Scotland and Wales maintain separate data stores for Electronic Healthcare Records with responsibility being devolved to National Governments. This has introduced a lack of uniformity, making it difficult to evaluate care, diagnosis and treatment across the entire United Kingdom.
-
•
Propriety systems are used by England, Scotland and Wales National Health Services which makes it challenging to perform analyses across England, Scotland and Wales.
What has this study added to the body of knowledge?
-
•
This paper presents the first framework to integrate national Electronic Health Records. It has been developed with collaboration from health professional and could be rolled out nationally to assist in United Kingdom wide research.
-
•
This paper found that variable completeness across the nations was varied, with Outpatient care being sparsely coded making it challenging for use in epidemiological research.
-
•
This paper highlights the types of analyses which can be performed when undertaking United Kingdom wide linkage, with the potential of combing additional data modalities.
Acknowledgments
We are grateful to NHS Digital, Information Service Division and Secure Anonymised Information Linkage for supplying the datasets and supporting this work.
Footnotes
Supplementary data associated with this article can be found, in the online version, at https://doi.org/10.1016/j.ijmedinf.2018.02.012.
Contributor Information
Daniel Leightley, Email: daniel.leightley@kcl.ac.uk.
Zoe Chui, Email: zoe.e.chui@kcl.ac.uk.
Margaret Jones, Email: margaret.jones@kcl.ac.uk.
Sabine Landau, Email: sabine.landau@kcl.ac.uk.
Paul McCrone, Email: paul.mccrone@kcl.ac.uk.
Richard D. Hayes, Email: richard.hayes@kcl.ac.uk.
Simon Wessely, Email: simon.wessely@kcl.ac.uk.
Nicola T. Fear, Email: nicola.t.fear@kcl.ac.uk.
Laura Goodwin, Email: laura.goodwin@liverpool.ac.uk.
Appendix A. Supplementary data
The following is Supplementary data to this article:
References
- 1.Perera G., Broadbent M., Callard F., Chang C.-K., Downs J., Dutta R., Fernandes A., Hayes R.D., Henderson M., Jackson R., Jewell A., Kadra G., Little R., Pritchard M., Shetty H., Tulloch A., Stewart R. Cohort profile of the south London and maudsley NHS foundation trust biomedical research centre (SLaM BRC) case register: current status and recent enhancement of an electronic mental health record-derived data resource. BMJ Open. 2016;6(3) doi: 10.1136/bmjopen-2015-008721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Payne R.A., Abel G.A., Guthrie B., Mercer S.W. The effect of physical multimorbidity, mental health conditions and socioeconomic deprivation on unplanned admissions to hospital: a retrospective cohort study. Can. Med. Assoc. J. 2013;185(5):E221–E228. doi: 10.1503/cmaj.121349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Simmonds S.J., Syddall H.E., Walsh B., Evandrou M., Dennison E.M., Cooper C., Aihie Sayer A. Understanding NHS hospital admissions in england: linkage of hospital episode statistics to the hertfordshire cohort study. Age Ageing. 2014;43(September (5)):653–660. doi: 10.1093/ageing/afu020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ford D.V., Jones K.H., Verplancke J.-P., Lyons R.A., John G., Brown G., Brooks C.J., Thompson S., Bodger O., Couch T., Leake K. The SAIL Databank: building a national architecture for e-health research and evaluation. BMC Health Serv. Res. 2009;9(December (1)):157. doi: 10.1186/1472-6963-9-157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gray L., Batty G.D., Craig P., Stewart C., Whyte B., Finlayson A., Leyland A.H. Cohort Profile: the Scottish Health Surveys Cohort: linkage of study participants to routinely collected records for mortality, hospital discharge, cancer and offspring birth characteristics in three nationwide studies. Int. J. Epidemiol. 2010;39(2):345–350. doi: 10.1093/ije/dyp155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mayer-Schnberger V. In: Big Data A Revolution That Will Transform How We Live, Work and Think. Mayer-Schnberger Viktor, Cukier Kenneth., editors. John Murray Publishers; UK: 2013. [Google Scholar]
- 7.Andreu-Perez J., Poon C.C.Y., Merrifield R.D., Wong S.T.C., Yang G.-Z. Big data for health. IEEE J. Biomed. Heal. Inform. 2015;19(July (4)):1193–1208. doi: 10.1109/JBHI.2015.2450362. [DOI] [PubMed] [Google Scholar]
- 8.Schneeweiss S. Learning from big health care data. N. Engl. J. Med. 2014;370(23):2161–2163. doi: 10.1056/NEJMp1401111. [DOI] [PubMed] [Google Scholar]
- 9.Raghupathi W., Raghupathi V. Big data analytics in healthcare: promise and potential. Heal. Inf. Sci. Syst. 2014;2(December (1)):3. doi: 10.1186/2047-2501-2-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Leightley D., McPhee J.S., Yap M.H. Automated analysis and quantification of human mobility using a depth sensor. IEEE J. Biomed. Heal. Inform. 2017;21(July (4)):939–948. doi: 10.1109/JBHI.2016.2558540. [DOI] [PubMed] [Google Scholar]
- 11.Jensen P.B., Jensen L.J., Brunak S. Mining electronic health records: towards better research applications and clinical care. Nat. Rev. Genet. 2012;13(6):395–405. doi: 10.1038/nrg3208. [DOI] [PubMed] [Google Scholar]
- 12.Bevan G. 2014. The Impacts of Asymmetric Devolution on Health Care in the Four Countries of the UK. [Google Scholar]
- 13.Coorevits P., Sundgren M., Klein G.O., Bahr A., Claerhout B., Daniel C., Dugas M., Dupont D., Schmidt A., Singleton P., De Moor G., Kalra D. Electronic health records: new opportunities for clinical research. J. Intern. Med. 2013;274(6):547–560. doi: 10.1111/joim.12119. [DOI] [PubMed] [Google Scholar]
- 14.Andrew Nash, Internal Migration, England and Wales – Office for National Statistics, Online, 2014. [Online]. Available: https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/migrationwithintheuk/bulletins/internalmigrationbylocalauthoritiesinenglandandwales/2014-06-26. (Accessed 11 September 2017).
- 15.Vayena E., Salathé M., Madoff L.C., Brownstein J.S. Ethical challenges of big data in public health. PLOS Comput. Biol. 2015;11(2) doi: 10.1371/journal.pcbi.1003904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wing K., Bhaskaran K., Smeeth L., van Staa T.P., Klungel O.H., Reynolds R.F., Douglas I. Optimising case detection within UK electronic health records: use of multiple linked databases for detecting liver injury. BMJ Open. 2016;6(9) doi: 10.1136/bmjopen-2016-012102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lyons R.A., Jones K.H., John G., Brooks C.J., Verplancke J.-P., Ford D.V., Brown G., Leake K. The SAIL databank: linking multiple health and social care datasets. BMC Med. Inform. Decis. Mak. 2009;9(1):3. doi: 10.1186/1472-6947-9-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bohensky M.A., Jolley D., Sundararajan V., Evans S., Pilcher D.V., Scott I., Brand C.A. Data Linkage: a powerful research tool with potential problems. BMC Health Serv. Res. 2010;10(1):346. doi: 10.1186/1472-6963-10-346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.NHS Direct, Your health and care records, 2015. [Online]. Available: http://www.nhs.uk/NHSEngland/thenhs/records/nhs-number/Pages/what-is-the-nhs-number.aspx.
- 20.NHS. Information Centre for Health and Social Care, Hospital episode statistics (HES). NHS Information Centre, 2010.
- 21.NHS. Information Services Division, Scottish Morbidity Records (SMRs). NHS Information Services Division. [Online]. Available: http://www.isdscotland.org.
- 22.Hagger-Johnson G., Harron K., Fleming T., Gilbert R., Goldstein H., Landy R., Parslow R.C. Data linkage errors in hospital administrative data when applying a pseudonymisation algorithm to paediatric intensive care records. BMJ Open. 2015;5(8) doi: 10.1136/bmjopen-2015-008118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Polling C., Tulloch A., Banerjee S., Cross S., Dutta R., Wood D.M., Dargan P.I., Hotopf M. Using routine clinical and administrative data to produce a dataset of attendances at Emergency Departments following self-harm. BMC Emerg. Med. 2015;15(1):15. doi: 10.1186/s12873-015-0041-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Samad L., Cortina-Borja M., Sutcliffe A.G., Marven S., Cameron J.C., El Bashir H., Lynn R., Taylor B. National hospital data for intussusception: data linkage and retrospective analysis to assess quality and use in vaccine safety surveillance. Vaccine. 2016;34(January (3)):373–379. doi: 10.1016/j.vaccine.2015.11.041. [DOI] [PubMed] [Google Scholar]
- 25.Hotopf M., Hull L., Fear N.T., Browne T., Horn O., Iversen A., Jones M., Murphy D., Bland D., Earnshaw M., Greenberg N., Hacker Hughes J., Tate A.R., Dandeker C., Rona R., Wessely S. The health of UK military personnel who deployed to the 2003 Iraq war: a cohort study. Lancet. 2006;367(May (9524)):1731–1741. doi: 10.1016/S0140-6736(06)68662-5. [DOI] [PubMed] [Google Scholar]
- 26.Fear N.T., Jones M., Murphy D., Hull L., Iversen A.C., Coker B., Machell L., Sundin J., Woodhead C., Jones N., Greenberg N., Landau S., Dandeker C., Rona R.J., Hotopf M., Wessely S. What are the consequences of deployment to Iraq and Afghanistan on the mental health of the UK armed forces? A cohort study. Lancet. 2010;375(May (9728)):1783–1797. doi: 10.1016/S0140-6736(10)60672-1. [DOI] [PubMed] [Google Scholar]
- 27.National Health Service Act 2006. Great Britain, 2006.
- 28.N.W.I. Service, NHS Wales Informatics Service – An Official NHS Wales website.
- 29.Greenhalgh T., Morris L., Wyatt J.C., Thomas G., Gunning K. Introducing a nationally shared electronic patient record: case study comparison of Scotland, England, Wales and Northern Ireland. Int. J. Med. Inform. 2013;82(May (5)):e125–e138. doi: 10.1016/j.ijmedinf.2013.01.002. [DOI] [PubMed] [Google Scholar]
- 30.Bridgman S.A., Clement D., Downing A., Walley G., Phair I., Maffulli N. Population based epidemiology of ankle sprains attending accident and emergency units in the West Midlands of England, and a survey of UK practice for severe ankle sprains. Emerg. Med. J. 2003;20(6):508–510. doi: 10.1136/emj.20.6.508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Health and Social Care Information Centre, Methodology to create provider and CIP spells from HES APC Data. 2014.
- 32.StataCorp, Stata: Release 12. Statistical Software, 2011.
- 33.Hospital Outpatient Activity, 2016.
- 34.Canavan C., West J., Card T. Calculating total health service utilisation and costs from routinely collected electronic health records using the example of patients with irritable bowel syndrome before and after their first gastroenterology appointment. Pharmacoeconomics. 2016;34(February (2)):181–194. doi: 10.1007/s40273-015-0339-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.John A., Dennis M., Kosnes L., Gunnell D., Scourfield J., Ford D.V., Lloyd K. Suicide Information Database-Cymru: a protocol for a population-based, routinely collected data linkage study to explore risks and patterns of healthcare contact prior to suicide to identify opportunities for intervention. BMJ Open. 2014;4(11):e006780. doi: 10.1136/bmjopen-2014-006780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Liddle A.D., Pandit H., Judge A., Murray D.W. Effect of surgical caseload on revision rate following total and unicompartmental knee replacement. J. Bone Jt. Surg. 2016;98(1):1–8. doi: 10.2106/JBJS.N.00487. [DOI] [PubMed] [Google Scholar]
- 37.Brewster D.H., Stockton D.L., Reekie A., Ashcroft G.P., Howie C.R., Porter D.E., Black R.J. Risk of cancer following primary total hip replacement or primary resurfacing arthroplasty of the hip: a retrospective cohort study in Scotland. Br. J. Cancer. 2013;108(May (9)):1883–1890. doi: 10.1038/bjc.2013.129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sinha S., Peach G., Poloniecki J.D., Thompson M.M., Holt P.J. Studies using English administrative data (Hospital Episode Statistics) to assess health-care outcomes—systematic review and recommendations for reporting. Eur. J. Public Health. 2013;23(February (1)):86–92. doi: 10.1093/eurpub/cks046. [DOI] [PubMed] [Google Scholar]
- 39.Burns E.M., Rigby E., Mamidanna R., Bottle A., Aylin P., Ziprin P., Faiz O.D. Systematic review of discharge coding accuracy. J. Public Health (Bangkok) 2012;34(1):138–148. doi: 10.1093/pubmed/fdr054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Majeed A., Car J., Sheikh A. Accuracy and completeness of electronic patient records in primary care. Fam. Pract. 2008;25(August (4)):213–214. doi: 10.1093/fampra/cmn047. [DOI] [PubMed] [Google Scholar]
- 41.Thiru K. Systematic review of scope and quality of electronic patient record data in primary care. BMJ. 2003;326(May (7398)):1070. doi: 10.1136/bmj.326.7398.1070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hersh W.R., Weiner M.G., Embi P.J., Logan J.R., Payne P.R.O., Bernstam E.V., Lehmann H.P., Hripcsak G., Hartzog T.H., Cimino J.J., Saltz J.H. Caveats for the use of operational electronic health record data in comparative effectiveness research. Med. Care. 2013;51(August (8)):S30–S37. doi: 10.1097/MLR.0b013e31829b1dbd. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Coding schemes and syntax used to perform data linkage are available upon request from the corresponding author.