Abstract
Aims
To test the efficacy of a web‐based alcohol intervention with and without guidance.
Design
Three parallel groups with primary end‐point after 6 weeks.
Setting
Open recruitment in the German working population.
Participants
Adults (178 males/256 females, mean age 47 years) consuming at least 21/14 weekly standard units of alcohol (SUA) and scoring ≥ 8/6 on the Alcohol Use Disorders Identification Test.
Intervention
Five web‐based modules including personalized normative feedback, motivational interviewing, goal setting, problem‐solving and emotion regulation during 5 weeks. One intervention group received an unguided self‐help version (n=146) and the second received additional adherence‐focused guidance by eCoaches (n=144). Controls were on a waiting list with full access to usual care (n=144).
Measurements
Primary outcome was weekly consumed SUA after 6 weeks. SUA after 6 months was examined as secondary outcome, next to numbers of participants drinking within the low‐risk range, and general and work‐specific mental health measures.
Findings
All groups showed reductions of mean weekly SUA after 6 weeks (unguided: −8.0; guided: −8.5; control: −3.2). There was no significant difference between the unguided and guided intervention (P=0.324). Participants in the combined intervention group reported significantly fewer SUA than controls [B=−4.85, 95% confidence interval (CI)=−7.02 to −2.68, P < 0.001]. The intervention groups also showed significant reductions in SUA consumption after 6 months (B=−5.72, 95% CI=−7.71 to −3.73, P < 0.001) and improvements regarding general and work‐related mental health outcomes after 6 weeks and 6 months.
Conclusions
A web‐based alcohol intervention, administered with or without personal guidance, significantly reduced mean weekly alcohol consumption and improved mental health and work‐related outcomes in the German working population.
Keywords: Alcohol, drinking, employee, internet, mental health, occupational health, training, treatment
Introduction
Alcohol consumption is an important risk factor for conditions like cancer, cardiovascular disease, and mental and behavioral disorders 1, 2, 3. It is also associated with considerable economic costs, which include sick leave and impaired productivity at work 4.
Among a multitude of risk factors, several studies have highlighted associations between specific work‐related factors — like job strain 5, long work hours 6, and effort‐reward imbalance 7, 8 — and alcohol consumption. Concurrently, workplaces provide opportunities to deliver alcohol‐related interventions (e.g., via health promotion programs, alcohol policies, or screening and brief interventions) 9. While some studies have revealed small effects on alcohol consumption 10, 11, 12, others failed to demonstrate any beneficial effects among subjects offered such interventions relative to controls 13. In Germany, health insurance companies have been legally obligated to offer and reimburse for preventative measures to reduce alcohol consumption since the late eighties. As a result, a variety of public and occupational services have been established during the past decades. Still, a general problem with such services are low utilization rates 14, 15, 16. This is a common issue for both public 17 and occupational 18 alcohol‐related health services. Reasons for this include preferences for self‐help attempts 17 and fears of stigmatization 18, 19. It therefore would be of great value to investigate the use of lower‐threshold and less‐stigmatizing approaches. Web‐based interventions are a potentially promising solution, by which evidence‐based measures designed to prevent alcohol‐related problems in employees can be delivered less intrusively and conspicuously 9, 20.
Several web‐based alcohol interventions have been evaluated in the general population, producing small effects in terms of alcohol reduction, relative to controls 21, 22, 23. However, research on interventions targeting working populations is scarce and largely restricted to very specific sub‐populations. For example, in young employees, Doumas and Hannah tested a website that provided personalized normative feedback (PNF) 24. In turn, other studies focusing either on screening 25 or very brief interventions 26 have shown such measures not to be effective. All interventions have focused upon a single problem area (i.e., alcohol consumption). However, alcohol‐related problems are associated with other mental health problem domains, like depression and anxiety 27. It therefore seems worthwhile to explore whether or not web‐based alcohol interventions can exert any positive effect on co‐occurring mental problems 28. In particular, recent findings indicate an impact of work‐related rumination on alcohol use after work 29. People may use alcohol as a coping strategy to reduce work‐related rumination on the one hand, while on the other hand there also is evidence that workers facing high‐level work stress, in terms of effort‐reward imbalance, consume more alcohol than those with low‐work stress 7, 8, 30, 31. However, to our knowledge, there have been neither studies investigating the effects of web‐based alcohol interventions on work‐related outcomes, nor studies that have considered work‐stress as a factor that predicts drinking.
There also is a lack of evidence regarding the optimal form of personal support in web‐based alcohol interventions. Findings on meta‐analysis suggest that, on average, guided interventions may be better than pure self‐help interventions 21. To the best of our knowledge, however, only one study explored a web‐based alcohol intervention with different guidance formats 32, demonstrating greater effects for the intervention plus intensive accompanying chat therapy (d = 0.59) than for the self‐help intervention (d = 0.35), when compared against controls. Nonetheless, there was no significant difference in efficacy between both interventions.
The purpose of the present study was to test the efficacy of a web‐based alcohol intervention named ‘GET.ON Clever weniger trinken’ (CWT; be smart – drink less) in employees with a problematic drinking pattern 33. We tested two versions of the intervention: unguided/purely self‐help and guided, including additional support from eCoaches.
Methods
Study design
This study was conducted in compliance with the study protocol 33 and the Declaration of Helsinki. Within the context of a three‐arm randomized controlled trial (RCT), 434 participants were randomly assigned (at a ratio of 1:1:1 and block size of three) to either (1) the unguided web‐based self‐help intervention (unguided CWT, n = 146); (2) to CWT with additional adherence‐focused guidance (guided CWT, n = 144); or to a waiting list control group (WLC, n = 144) that was offered delayed access to unguided CWT. All groups otherwise had full access to usual care. Online outcome assessments took place before subjects were allocated to a study group (T1), six weeks later (T2), and at six months of follow‐up (T3).
Procedures
Individuals 18 years old or older were included if they were currently employed or self‐employed, if they reported drinking at least 14/21 (women/men) SUA per week, and if they had a score of ≥ 8/6 for men/women on the Alcohol Use Disorders Identification Test (AUDIT) 34. They were excluded if they had been diagnosed with any past psychosis or drug dependence (self‐disclosed); exhibited a notable suicidal risk, as indicated by a score greater than 1 on item 9 (‘I feel I would be better off dead’) of the Beck Depression Inventory 35; or if they had received any other kind of treatment for alcohol‐related problems or work‐related stress prior to the baseline assessment.
Subjects were recruited nationwide from the German‐speaking working population between October 2014 and February 2016. The recruitment process was supported by several health insurance companies (BARMER, KKH) and by the German company health insurance fund (BKK) via announcements in print membership magazines and on their websites. Participation was not limited to the insurants of these companies. Additionally, the intervention was announced in print newspaper articles. Potential participants signed up by providing an email address and name or pseudonym on an open‐access website (http://www.geton-training.de). After registration, applicants received an email with detailed information about the study procedures and were asked to complete an online screening questionnaire to assess their eligibility. Applicants who fulfilled all inclusion but no exclusion criteria, provided informed consent, and completed the baseline assessment (T1) were assigned to one of the three study groups. Randomization took place at an individual level and was performed by an independent researcher not otherwise involved in the study, using an automated, computer‐based, random integer generator (randomisation.eu). Prior to any subject recruitment, all procedures involved in the study had been approved by the University of Lueneburg (Germany) ethics committee (No. Boss201404_OT) and registered in the German clinical trials register (No. DRKS00006105).
Interventions
The web‐based intervention (CWT) consisted of five modules and participants were advised to complete one module per week. Each module contained general information, illustrative examples, interactive exercises, quizzes, audio and video files, and downloadable work sheets. Exercises in the intervention were adapted from evidence‐based treatment elements for alcohol use disorders 36, 37, such as motivational interviewing and tools to control drinking behaviors. The exercises included personalized normative feedback, pros and cons of drinking, goal setting, monitoring of drinking by an online‐diary, action and coping planning to control drinking behavior, and relapse prevention. In addition, we integrated emotional regulation techniques 38, that have not been tested in web‐based alcohol interventions so far. The study protocol contains a detailed description of the intervention's content and theoretical background 33.
All participants in either one of the two active intervention groups received the same web‐based CWT. The unguided intervention group could contact the study team via email only if technical problems arose. In the guided intervention group, each participant was assigned an eCoach, a trained psychologist who gave feedback following a semi‐structured manual. In this study, guidance primarily aimed at encouraging participants to adhere to their training schedule (i.e., adherence‐focused guidance) 39, 40. At the beginning of training, the eCoaches sent a message to each participant clarifying their supportive role in the program. Coaching guidance had two elements: a) adherence monitoring and b) feedback on demand. Adherence monitoring included regular monitoring of whether participants had completed the intervention modules on time. If subjects did not complete a module within seven days, the eCoaches sent reminders written in an encouraging and motivational style. Feedback on demand referred to the opportunity to contact the eCoaches for any question via the internal messaging system provided in the training platform. Individual feedback was provided within 48 hours. Participants in the waiting list group were informed that monitoring and reflecting on their drinking behaviors, by completing the online‐assessments, could be their first step towards developing healthier drinking habits. Furthermore, they were informed that they would ultimately receive access to the unguided training program after their six‐month follow‐up assessment.
Primary outcome
The primary outcome was the average self‐reported quantity of alcohol consumption in standard units of alcohol (SUA) over seven days prior to T2, using the Timeline Followback (TLFB) method 41. One SUA contains 10–12 grams of pure alcohol. The TLFB has been shown to be a valid and reliable procedure to document recent drinking histories, with average retest‐reliability of .90 42, 43.
Secondary outcomes and predictors
Secondary drinking outcomes included alcohol consumption in terms of SUA weekly prior to T3 and the number of responders who complied with the low‐risk guideline for problematic drinking at T2 and T3. Responders were defined as having consumed no more than 14 (for women) or 21 (for men) SUA weekly. The Depression Anxiety Stress Scale (DASS‐21) 44 was used to assess symptoms of depression, anxiety, and stress at T2 and T3, via seven items and subscores that ranged from 0 to 21 each. We used the Irritation Scale (IS) 45 with its subdomains cognitive irritation (3 items; range 3–21) and emotional irritation (5 items; range 5–35) to assess rumination in the context of the working environment at T2 and T3. The Effort Reward Imbalance Questionnaire – Short Form (ERI‐SF) 46 was also used, with the subdomains effort (3 items; range 3–12) and reward (7 items, range 7–28) that covers aspects of the working context as possible baseline predictors of the intervention effects. Further measures used in this trial 33 will be considered in subsequent publications.
Statistical analyses
All analyses are reported in accordance with the Consolidated Standards of Reporting Trials (CONSORT) 47 following intention‐to‐treat (ITT) procedures. For the main analyses, we used multiple imputations (MI) to deal with missing data. MI techniques are recommended as they provide the best estimate for missing data 48. We employed a Markov Chain Monte Carlo multivariate imputation algorithm, using the missing data module in SPSS v. 23, with 100 estimations per missing value. These estimations were aggregated to a single value that was included for all further analyses. In addition, we conducted sensitivity analyses with replacing missing values by the baseline score, assuming that study dropouts did not change their drinking behavior. All statistics were conducted using IBM SPSS (SPSS Inc, Chicago, IL, USA). For all statistical analyses, the significance level was set at P < 0.05 for two‐sided tests. Based on a power of 80%, we aimed to recruit 528 participants to detect an intervention effect of d = 0.30 relative to the control condition at T2 33. Eventually, recruitment was slower than anticipated, so we closed the trial with 434 participants. Considering this sample size, the trial had 80% power to detect an intervention effect of d = 0.33.
To test the effects of the intervention, we conducted hierarchical multiple regression analyses. We included the study condition and the baseline score of the relevant outcome in the regression model, as well as the following baseline predictors: gender, age, education (high vs. low and mid‐level), depression, irritation and effort and reward at work. The analysis plan followed a two‐stage procedure. First, we compared unguided CWT with guided CWT. Second, if these groups did not significantly differ, both groups were combined into a single intervention group that was compared with the control group then. For all continuous analyses, Cohen's d 49 was calculated based on imputed data by subtracting the average post‐assessment score of one study group from the other and then dividing this value by the pooled standard deviations of the post scores. To analyze interventional effects at an individual level, we tested for group differences in the number of responders using Pearson chi‐square analysis and calculated the odds ratio (OR) with 95% confidence intervals (CI).
Results
Participants
A total of 434 participants (178 males/256 females) were randomly allocated to the three study arms (Fig. 1). This was lower than the initially intended sample size 33. Recruitment in this trial was difficult compared to earlier studies on web‐based health interventions conducted by our research group, since this phase took substantially longer than expected. Due to a limited funding period, we had to stop recruitment after 17 months. In the guided intervention group, two participants withdrew from study participation and called for deletion of their datasets, which was a necessary option requested from the ethics committee. Thus, the final study sample consisted of 432 participants with an average age of 47 (Table 1). The majority of participants were employed full time, with an average working experience of 23 years.
Figure 1.

Study flow
Table 1.
Baseline characteristics.
| Characteristics | Control (n = 144) | Unguided CWT (n = 146) | Guided CWT (n = 142) |
|---|---|---|---|
| Socio‐demographic | |||
| Age, mean (SD) | 47.3 (10.3) | 47.6 (9.3) | 47.5 (9.8) |
| Women, n (%) | 89 (61.8) | 84 (57.5) | 83 (58.5) |
| Married or in a partnership, n (%) | 85 (59.0) | 100 (68.5) | 81 (57.1) |
| Educational level | |||
| Low, n (%) | 5 (3.5) | 11 (7.5) | 7 (4.9) |
| Middle, n (%) | 41 (28.5) | 47 (32.2) | 38 (26.8) |
| High, n (%) | 98 (68.1) | 88 (66.3) | 97 (68.3) |
| Work characteristics | |||
| Full‐time employed, n (%) | 102 (70.8) | 97 (66.4) | 102 (71.8) |
| Part‐time employed, n (%) | 34 (23.6) | 38 (26.0) | 33 (23.2) |
| On sick leave, n (%) | 3 (2.1) | ‐ | ‐ |
| Seeking work, n (%) | 4 (2.8) | 10 (6.8) | 5 (3.5) |
| Not gainfully employed, n (%) | 1 (0.7) | 1 (0.7) | 2 (1.4) |
| Work experience in years, mean (SD) | 23.5 (11.1) | 23.0 (11.1) | 23.2 (11.6) |
| Efforts spent at work,a mean (SD) | 8.30 (2.2) | 8.7 (2.3) | 8.5 (2.4) |
| Rewards received from work,a mean (SD) | 18.9 (4.0) | 18.0 (3.8) | 18.0 (4.0) |
| Effort–reward imbalance,b mean (%) | 76 (52.8) | 92 (63.0) | 87 (60.4) |
| Work sectors | |||
| Service, n (%) | 33 (22.9) | 34 (23.3) | 36 (25.4) |
| Economy, n (%) | 25 (17.4) | 21 (14.4) | 16 (11.3) |
| Health, n (%) | 16 (11.1) | 20 (13.7) | 23 (16.2) |
| Social, n (%) | 13 (9.0) | 26 (17.8) | 17 (12.0) |
| Information technologies, n (%) | 9 (6.3) | 7 (4.8) | 9 (6.3) |
| Others, n (%) | 48 (33.3) | 38 (26.0) | 41 (28.9) |
| Income in Euros, per month | |||
| < 1000, n (%) | 13 (9.1) | 10 (6.8) | 4 (2.8) |
| 1000–2000, n (%) | 29 (20.3) | 29 (19.9) | 31 (21.8) |
| 2000–3000, n (%) | 25 (17.5) | 26 (17.8) | 30 (21.1) |
| 3000–4000, n (%) | 19 (13.3) | 29 (19.9) | 22 (15.5) |
| 4000–5000, n (%) | 16 (11.2) | 14 (9.6) | 14 (9.9) |
| > 5000, n (%) | 23 (16.1) | 20 (13.7) | 22 (15.5) |
| Prefer not to say, n (%) | 6 (4.2) | 3 (2.1) | 7 (4.9) |
| No paid employment, n (%) | 13 (9.1) | 15 (10.3) | 12 (8.5) |
| Previous use of health services | |||
| Previous health training, n (%) | 12 (8.3) | 17 (11.6) | 22 (15.5) |
| Previous psychotherapy, n (%) | 64 (44.4) | 55 (37.7) | 60 (42.3) |
| Current psychotherapy, n (%) | 1 (0.7) | 3 (2.1) | 2 (1.4) |
SD = standard deviation; CWT = ‘clever weniger trinken’ (be smart—drink less).
Subdomains of the effort–reward imbalance (ERI) questionnaire;
according to Siegrist et al. (2004) 50 ERI ratio values > 1 indicate high work stress.
Missing data
Data on sociodemographic and outcome variables were available for the entire sample at T1. In total, 339 participants (78.4%) attended the post‐assessment (T2), while 270 (62.5%) came to the six‐month follow‐up (T3) (Fig. 1). The three groups differed with regard to missing data on primary and secondary outcomes at T2 (P = 0.032), but not at T3 (P = 0.092). Missing of outcome data appeared only in terms of wave non‐response and Little's overall test of randomness indicated that missing occurred completely at random (P = 0.817); as such, multiple imputations of the missing data could be conducted 48.
Intervention usage
On average, participants in the unguided CWT group completed 2.5 training modules, while participants in the guided CWT group completed 3.0 training modules (Fig. 2). Adherence — defined as completing a minimum of the first three intervention modules — was significantly greater in the guided CWT group (t277 = 2.86, P = 0.005). There were two major forms of interaction between participants and eCoaches in the guided CWT group (n = 142). First, 47 participants (33.1%) engaged in conversation with an eCoach as a response to reminder messages that were sent by eCoaches when participants had not completed a training module in time. Typically, participants used these conversations to state when they were going to finish the outstanding training session. Second, some requested feedback on specific topics or exercises of the intervention; however this only amounted to 15 participants (10.6%). In the waiting list control group, eight participants (5.6%) indicated that they had received other help within the study period (e.g., visits to their general practitioner, psychotherapy, addiction services, online‐forums, health training other than the CWT), versus seven participants (4.8%, P = 0.927) in the unguided CWT group and six (4.2%, P = 0.770) in the guided CWT group.
Figure 2.
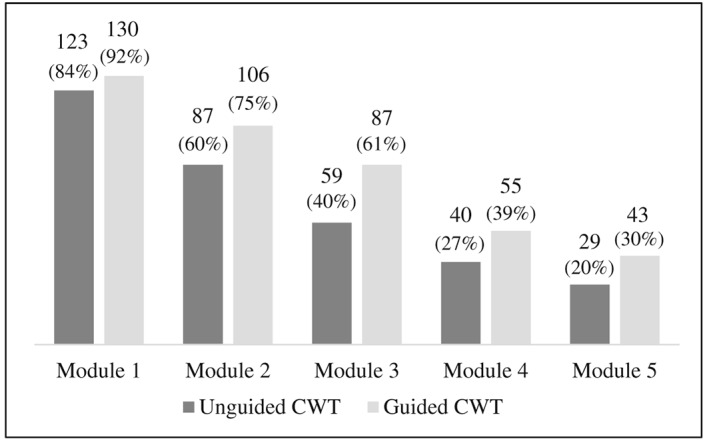
Participants who completed the intervention modules (based on log‐data). CWT = ‘clever weniger trinken’ (be smart ‐ drink less)
Primary outcome analysis
All study groups showed a reduction of mean weekly SUA from T1 to T2 (control: −3.2; unguided CWT: −8.0; guided: −8.5; Table 2). There was no significant difference between unguided and guided CWT in the unadjusted model (P = 0.324) or in any other model including possible baseline confounders (Table 3). Accordingly, we combined both active intervention groups and compared it with the control group. The fully adjusted regression model revealed a significant group effect (B = −4.85, 95% CI: ‐7.02 to −2.68, P < 0.001; Table 3). Participants who received any type of CWT reduced their weekly drinking by 4.9 SUA on average, relative to controls.
Table 2.
Means, standard deviations, and effect sizes on weekly standard units of alcohol.
| Baseline | 6 weeks after baselinea | 6 months after baselinea | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | d b | 95% CI | Mean | SD | d b | 95% CI | |||
| Control (n = 144) | 28.99 | 13.38 | 25.79 | 12.33 | 24.04 | 13.18 | ||||||
| Unguided CWT (n = 146) | 30.26 | 16.11 | 22.31 | 14.66 | 0.25 | 0.02 | 0.48 | 17.89 | 12.16 | 0.45 | 0.22 | 0.68 |
| Guided CWT (n = 142) | 29.44 | 17.68 | 20.96 | 14.39 | 0.38 | 0.14 | 0.61 | 19.63 | 11.70 | 0.38 | 0.14 | 0.61 |
| Combined CWT (n = 288) | 29.87 | 16.89 | 21.59 | 14.47 | 0.30 | 0.10 | 0.51 | 18.79 | 12.12 | 0.42 | 0.22 | 0.62 |
Missing data handled by multiple imputation;
effect size Cohen's d based on differences between the intervention and the control group. CI = confidence interval; SD = standard deviation; CWT = ‘clever weniger trinken’ (be smart—drink less).
Table 3.
Results of the primary outcome regression analyses.
| Guided versus unguided CWT after 6 weeks | Combined CWT versus control after 6 weeks | |||||||
|---|---|---|---|---|---|---|---|---|
| B | 95% CI | P | B | 95% CI | P | |||
| Model 1 (R 2 = 0.020)a | ||||||||
| Condition | −1.70 | −5.08 | 1.68 | 0.324 | −4.19 | −6.97 | −1.41 | 0.003 |
| Model 2 (ΔR 2 = 0.386, P < 0.001)a | ||||||||
| Condition | −1.23 | −3.90 | 1.45 | 0.367 | −4.66 | −6.82 | −2.49 | < 0.001 |
| SUA | 0.53 | 0.45 | 0.60 | < 0.001 | 0.55 | 0.48 | 0.61 | < 0.001 |
| Model 3 (ΔR 2 = 0.016, P = 0.010)a | ||||||||
| Condition | −1.29 | −3.92 | 1.35 | 0.338 | −4.71 | −6.85 | −2.56 | < 0.001 |
| SUA | 0.48 | 0.39 | 0.56 | < 0.001 | 0.51 | 0.44 | 0.58 | < 0.001 |
| Gender | −4.99 | −7.86 | −2.11 | 0.001 | −3.53 | −5.76 | −1.31 | 0.002 |
| Age | −0.08 | −0.22 | 0.06 | 0.238 | −0.03 | −0.14 | 0.07 | 0.519 |
| Education | 1.03 | −1.74 | 3.80 | 0.463 | 1.09 | −1.08 | 3.25 | 0.324 |
| Model 4 (ΔR 2 = 0.000, P = 0.762)a | ||||||||
| Condition | −1.29 | −3.93 | 1.35 | 0.336 | −4.72 | −6.87 | −2.57 | < 0.001 |
| SUA | 0.48 | 0.39 | 0.56 | < 0.001 | 0.51 | 0.44 | 0.58 | < 0.001 |
| Gender | −4.97 | −7.86 | −2.09 | 0.001 | −3.56 | −5.79 | −1.33 | 0.002 |
| Age | −0.08 | −0.22 | 0.06 | 0.239 | −0.03 | −0.14 | 0.07 | 0.529 |
| Education | 1.04 | −1.74 | 3.81 | 0.462 | 1.08 | −1.09 | 3.25 | 0.329 |
| Depression | −0.03 | −0.32 | 0.25 | 0.816 | 0.03 | −0.19 | 0.26 | 0.762 |
| Model 5 (ΔR 2 = 0.006, P = 0.376)a | ||||||||
| Condition | −1.32 | −3.97 | 1.33 | 0.326 | −4.85 | −7.02 | −2.68 | < 0.001 |
| SUA | 0.48 | 0.39 | 0.56 | < 0.001 | 0.51 | 0.44 | 0.58 | < 0.001 |
| Gender | −5.26 | −8.18 | −2.35 | < 0.001 | −3.69 | −5.93 | −1.44 | 0.001 |
| Age | −0.08 | −0.23 | 0.06 | 0.241 | −0.03 | −0.13 | 0.08 | 0.639 |
| Education | 0.77 | −2.06 | 3.59 | 0.594 | 0.98 | −1.23 | 3.19 | 0.384 |
| Depression | −0.11 | −0.43 | 0.22 | 0.519 | −0.03 | −0.28 | 0.23 | 0.834 |
| Emotional irritation | −0.04 | −0.29 | 0.21 | 0.770 | 0.01 | −0.18 | 0.20 | 0.919 |
| Cognitive irritation | 0.26 | −0.06 | 0.57 | 0.107 | 0.11 | −0.13 | 0.35 | 0.356 |
| Efforts | 0.20 | −0.43 | 0.83 | 0.537 | 0.30 | −0.20 | 0.79 | 0.240 |
| Rewards | −0.03 | −0.40 | 0.33 | 0.856 | 0.00 | −0.28 | 0.28 | 0.992 |
SUA = standard units of alcohol at baseline; CI = confidence interval; CWT = ‘clever weniger trinken’ (be smart—drink less).
R 2, ΔR 2 and P‐values refer to the comparison of combined CWT versus control; a negative score on the beta weight for condition indicates a lower consumption level in the guided and the combined intervention group compared to the control group. A negative score on the beta weight for gender indicates that females drink less than males. A positive score on the beta weight for education indicates that higher‐educated participants drink more than lower‐educated participants.
Secondary outcome analyses
The regression analysis showed that the combined intervention group was also significantly effective after 6 months, indicated by an adjusted lower mean SUA score of 5.7, compared to controls (95%‐CI = −7.71 to −3.73, P < 0.001). Analyzing the intervention effects at an individual level, we found that in the unguided and guided CWT group, n = 52 (36%) and n = 62 (43%) of the participants fell below the low‐risk threshold at T2, respectively. The difference between both intervention groups was not significant (χ2 = 1.948, P = 0.185). The combined intervention group yielded higher rates of response to the low‐risk threshold at T2 (χ2 = 14.00, P < 0.001; OR = 2.39, 95%‐CI: 1.51–3.77) and at T3 (χ2 = 21.63, P < 0.001; OR = 2.83, 1.82–4.38) than the control group (Fig. 3).
Figure 3.
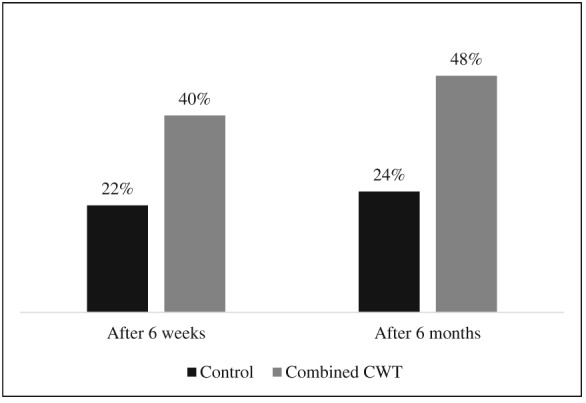
Participants complying with the low‐risk guideline (< 21/14 standard units/week for men/women) after 6 weeks and 6 months. CWT = ‘clever weniger trinken’ (be smart ‐ drink less)
The intervention also reduced symptoms of depression, stress, and anxiety with small effect sizes in terms of Cohen's d (Table 4), indicated by significant group differences between combined CWT and the controls (Table 5). Significant effects were also found on emotional and cognitive irritation.
Table 4.
Means, SDs and effect sizes on secondary outcomes.
| Outcome | Baseline | 6 weeks after baselinea | 6 months after baselinea | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | d b | 95% CI | Mean | SD | d b | 95% CI | |||
| Control (n = 144) | ||||||||||||
| DASS‐S | 6.72 | 4.81 | 6.46 | 4.50 | 6.10 | 4.43 | ||||||
| DASS‐D | 4.60 | 4.50 | 4.69 | 4.43 | 4.60 | 4.27 | ||||||
| DASS‐A | 2.31 | 2.71 | 2.22 | 2.64 | 2.51 | 2.87 | ||||||
| IS‐E | 14.24 | 7.22 | 13.47 | 6.57 | 13.35 | 6.74 | ||||||
| IS‐C | 11.64 | 5.38 | 10.72 | 4.91 | 10.52 | 4.61 | ||||||
| Unguided CWT (n = 146) | ||||||||||||
| DASS‐S | 7.33 | 4.67 | 5.10 | 3.73 | 0.33 | 0.10 | 0.56 | 5.00 | 4.00 | 0.26 | 0.03 | 0.49 |
| DASS‐D | 5.17 | 4.71 | 3.77 | 4.12 | 0.22 | −0.02 | 0.45 | 4.04 | 3.76 | 0.14 | −0.09 | 0.37 |
| DASS‐A | 2.42 | 2.97 | 1.63 | 2.28 | 0.24 | 0.01 | 0.47 | 2.04 | 2.53 | 0.18 | −0.05 | 0.41 |
| IS‐E | 15.66 | 6.89 | 12.26 | 5.67 | 0.20 | −0.03 | 0.43 | 12.03 | 5.95 | 0.21 | −0.02 | 0.44 |
| IS‐C | 11.93 | 5.50 | 10.22 | 4.65 | 0.11 | −0.12 | 0.34 | 9.53 | 4.64 | 0.21 | −0.02 | 0.45 |
| Guided CWT (n = 142) | ||||||||||||
| DASS‐S | 6.64 | 4.80 | 5.13 | 3.40 | 0.33 | 0.10 | 0.57 | 4.39 | 2.92 | 0.46 | 0.22 | 0.69 |
| DASS‐D | 4.96 | 4.73 | 3.30 | 3.10 | 0.36 | 0.13 | 0.60 | 3.43 | 3.30 | 0.31 | 0.08 | 0.54 |
| DASS‐A | 1.90 | 2.42 | 1.20 | 1.73 | 0.46 | 0.22 | 0.69 | 1.51 | 1.60 | 0.43 | 0.20 | 0.67 |
| IS‐E | 14.66 | 7.03 | 12.61 | 5.73 | 0.14 | −0.09 | 0.37 | 11.58 | 5.39 | 0.29 | 0.06 | 0.52 |
| IS‐C | 12.01 | 5.05 | 10.36 | 4.91 | 0.07 | −0.16 | 0.30 | 9.00 | 4.17 | 0.35 | 0.11 | 0.58 |
| Combined CWT (n = 288) | ||||||||||||
| DASS‐S | 6.98 | 4.74 | 5.11 | 3.56 | 0.34 | 0.14 | 0.55 | 4.69 | 3.51 | 0.37 | 0.16 | 0.57 |
| DASS‐D | 5.07 | 4.71 | 3.54 | 3.65 | 0.29 | 0.09 | 0.49 | 3.74 | 3.53 | 0.23 | 0.03 | 0.43 |
| DASS‐A | 2.16 | 2.72 | 1.41 | 2.03 | 0.36 | 0.16 | 0.56 | 1.77 | 2.13 | 0.31 | 0.11 | 0.51 |
| IS‐E | 15.16 | 6.96 | 12.43 | 5.69 | 0.17 | −0.03 | 0.37 | 11.81 | 5.67 | 0.26 | 0.05 | 0.46 |
| IS‐C | 12.00 | 5.28 | 10.29 | 4.77 | 0.09 | −0.11 | 0.29 | 9.27 | 4.41 | 0.28 | 0.08 | 0.48 |
Depression Anxiety Stress Scale (DASS)‐S = stress; DASS‐D = depression; DASS‐A = anxiety; IS‐E = emotional irritation; IS‐C = cognitive irritation. CI = confidence interval; SD = standard deviation; CWT = ‘clever weniger trinken’ (be smart—drink less).
Missing data handled by multiple imputation;
effect size Cohen's d based on differences between the intervention and the control group.
Table 5.
Summarized results of secondary outcomes regression analyses for the combined intervention groups compared to the control group.
| Combined CWT versus control after 6 weeks | Combined CWT versus control after 6 months | |||||||
|---|---|---|---|---|---|---|---|---|
| Ba | 95% CI | P | B | 95% CI | P | |||
| DASS‐S | −1.48 | −2.07 | −0.90 | <0.001 | −1.54 | −2.12 | −0.97 | < 0.001 |
| DASS‐D | −1.40 | −2.01 | −0.78 | <0.001 | −1.11 | −1.68 | −0.54 | < 0.001 |
| DASS‐A | −0.74 | −1.11 | −0.36 | <0.001 | −0.65 | −0.99 | −0.31 | < 0.001 |
| IS‐E | −1.57 | −2.45 | −0.70 | <0.001 | −2.15 | −2.93 | −1.37 | < 0.001 |
| IS‐C | −0.67 | −1.33 | −0.02 | 0.045 | −1.48 | −2.07 | −0.89 | < 0.001 |
Depression Anxiety Stress Scale (DASS)‐S = stress; DASS‐D = depression; DASS‐A = anxiety; IS‐E = emotional irritation; IS‐C = cognitive irritation; CI = confidence interval; CWT = ‘clever weniger trinken’ (be smart—drink less).
Group effect based on multiple regression model including condition and baseline score of the outcome as predictors.
Sensitivity analyses
An analysis using baseline observation carried forward for missing data showed similar results like the main‐analyses of the multiple imputed dataset. This was indicated by a significant small effect of combined CWT on the primary outcome (B = −3.99, 95% CI: −6.31 to −1.68, P = 0.001, d = 0.20), compared to controls. Detailed results of the sensitivity analyses for all continuous outcomes may be found online in the supporting information tab for this article (Tables S1–S4).
Discussion
In this study, we tested whether the web‐based intervention ‘GET.ON Clever weniger trinken’ is effective at reducing weekly standard units of alcohol in employees with problematic drinking. The study was designed around the concept that tailoring interventions to the needs of certain target groups — like employees — could enhance both their beneficial effects and reach. The intervention was effective, whether offered with or without guidance, at reducing weekly alcohol consumption. We detected a small effect of the intervention in terms of an average reduction of 4.9 SUA per week (d = 0.30), relative to usual care, after six weeks. This effect was slightly higher than the average effect found in the latest published meta‐analysis (g = 0.20) 21. Contrary to the results of recent meta‐analyses, which failed to uncover any significant effects in the long‐term 21 or at the most minimal significant effects (about 1 SUA/week) 23, 51, our findings showed that the effects were sustained over time, indicated by a mean difference of 5.7 SUA/week, relative to care as usual at six months.
The direct comparison of the guided and unguided groups failed to reveal any significant differences in the quantity of self‐reported SUA. This result corresponds to Blankers et al. 32, who detected similar advantages over standard care with an unguided intervention and the intervention plus chat therapy in a general population sample, without significant differences in effects between both interventions. Despite this, several points must be considered when interpreting our results. First, the intensity of guidance offered in this trial was relatively low 40, as it focused mainly on adherence promotion using standardized messages and only optional support in terms of feedback from eCoaches. Second, although the guided intervention group showed better adherence than the unguided group, which is consistent with previous reports 52, very few participants actually made use of this option and asked for feedback from their eCoaches. Concerns regarding fears of stigmatization and of giving up self‐disclosure when asking for help might have caused this result, especially as these concerns may be significant barriers against the use of alcohol interventions 17, 53. An alternative explanation might be that the addition of guidance to a web‐based alcohol intervention exerts no beneficial effect on drinking. Such an assumption is supported by recent meta‐analytic findings that found web‐based interventions with guidance not to be superior than unguided interventions for depression 54 and for anxiety disorders 55.
As alcohol‐related problems are often closely associated with stress and depressive symptoms, the intervention included therapeutic techniques like problem solving and emotion regulation. These techniques are commonly employed in stress management or depression interventions. We identified small‐size effects for the intervention, relative to usual care, on depression, stress, and anxiety at both follow‐up appointments. Accordingly, it seems worthwhile to conduct further studies testing the incremental effect of transdiagnostic interventions compared to pure alcohol interventions 28.
The workplace is considered a good setting in which to deliver alcohol‐related interventions 9, and work‐related stress is associated with drinking behaviors 5, 7, 8, 29. Therefore, it was assumed that a tailored, low‐threshold intervention might be an attractive approach to supplement established health care services and increase the overall reach of alcohol‐related interventions. That assumption was supported by the observation that the vast majority of employees in this study had never partaken in any occupational health services for alcohol‐related problems before. However, it also must be noted that more than half of our subjects had received psychotherapy for some psychological disorder in the past. This rate is much higher than the public health service utilization rates usually found among people with alcohol‐related problems 15, 16.
However, effects on work‐related outcomes were mixed. The intervention might help employees to find ways other than drinking to detach mentally from work‐related problems, indicated by small effects on emotional irritation at both follow‐ups. Hierarchical regression models analyzed in this study did not indicate that work‐related mental health variables in terms of irritation or effort and rewards had meaningful predictive effects on weekly alcohol consumption. Thus, longitudinal studies are needed to have a closer look at moderators of alcohol intervention success in the working context.
Limitations
This study had several limitations. First, the actual sample size was smaller than the intended sample size. For pragmatic reasons, we recruited via announcements in print membership magazines of health insurance companies and on their websites. As a result of being one of the first web‐based alcohol interventions in Germany, perhaps many lacked sufficient knowledge about the nature of such interventions. Low participation rates have been reported for other alcohol reduction approaches in various contexts 14, indicating that recruiting subjects can be challenging. However, it would have been beneficial to extend our impersonal recruiting strategy involving newspapers and the Internet, by collaborating closer with occupational health practitioners and other existing services. Health practitioners might be perceived as particularly trustworthy and, as such, their recommendations regarding study participation could have had a significantly positive effect on subject numbers. Second, the study was not intended nor powered to directly compare the effects between the guided and unguided groups. Therefore, any conclusions drawn about the two approaches' comparative efficacy should be made cautiously. Nonetheless, as this was one of the first studies to compare different intervention formats directly, our results should provide future investigators with invaluable information for power calculations and the design of appropriate studies like non‐inferiority trials 56. Third, because so few people actually made use of the guidance offered in this study, the generalizability of our findings regarding guidance is limited. One explanation for the low rate of guidance utilization could be the guidance format that we selected for this study, which was of very low intensity. Another explanation relates to fears regarding stigmatization 19 that might surface when participants think about interacting with eCoaches. One potential solution could be a more intensive, content‐focused guidance format 40 combined with introduction videos about guidance and the role of eCoaches in the intervention to increase acceptance 57. Anyhow, the results of the intervention should only be generalized to situations where comparable recruiting strategies were employed and participants actively searched for help by their own. Lastly, due to feasibility and ethical reasons, participants in the control group were offered access to the intervention after a waiting time of six months. Such waiting conditions have been discussed as being potentially associated with a nocebo effect. Participants might be discouraged to initiate behavioral changes or seek otherwise help because they expect to get help after the waiting time. Hence, delayed treatment access control conditions might overestimate intervention effects 58.
Conclusions
In this study, we found the intervention ‘GET.ON Clever weniger trinken’ to be effective at reducing weekly alcohol consumption, whether offered with or without additional guidance and support from eCoaches. Furthermore, the intervention led to significant reductions in subjects' depression, anxiety, general stress, and work‐related irritation. The present sample seemed to be more willing to accept psychological help and to make use of the web‐based intervention than traditional alcohol‐related health services. These findings indicate that the intervention could be a promising approach to enhance established services for alcohol‐related problems among employees. However, recruitment difficulties and the low use of guidance in this study highlight the need for innovative and effective strategies to increase the rate of intervention usage.
Randomized trial registration
This trial was registered at the German Register of Clinical Studies (DRKS): DRKS00006105, date of registration: 2014–07‐07. All procedures involved in the study were consistent with the generally‐accepted standards of ethical practice approved by the University of Lueneburg (Germany) ethics committee (No. Boss201404_OT).
Declaration of interests
Leuphana University, Lueneburg, has full exploitation rights for the intervention. The authors will have no share in any possible license revenues from Leuphana University Lueneburg. However, D.E., D.L. and M.B. report holding shares of the Institute for Online Health Training, which aims to transfer scientific knowledge related to the present research into routine mental health care in Germany. This institute licenses the intervention under study at Leuphana University, Lueneburg, to provide the intervention within routine preventative services of health insurance companies in Germany. Having the foundation of such an institute to disseminate the findings and products from the research project was the primary aim of the European Union for funding the presented research. M.B. reports receiving research grants from the German Ministry of Research and the German Research Association and receiving personal fees from various institutions providing ongoing training for psychotherapists. D.E. reports receiving funds from the European Union, German Ministry of Education and Research, as well as fees as scientific adviser from several companies such as Minddistrict Holding, Lantern Inc., BARMER, Techniker Krankenkasse.
Supporting information
Table S1 Means, standard deviations and effect sizes of all study groups on weekly standard units alcohol [imputation by baseline observation carried forward (BOCF)].
Table S2 Means, standard deviations and effect sizes of all study groups on secondary outcomes [imputation by baseline observation carried forward (BOCF)].
Table S3 Results of the primary outcome regression analyses [imputation by baseline observation carried forward (BOCF)].
Table S4 Summarized results of secondary outcomes regression analyses for the combined intervention groups compared to the control group [imputation by baseline observation carried forward (BOCF)].
Acknowledgements
The associated project of all the authors was funded by the European Union (project EFRE: CCI 2007DE161PR001).
Boß, L. , Lehr, D. , Schaub, M. P. , Paz Castro, R. , Riper, H. , Berking, M. , and Ebert, D. D. (2018) Efficacy of a web‐based intervention with and without guidance for employees with risky drinking: results of a three‐arm randomized controlled trial. Addiction, 113: 635–646. doi: 10.1111/add.14085.
References
- 1. Lim S. S., Vos T., Flaxman A. D., Danaei G., Shibuya K., Adair‐Rohani H. et al A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the global burden of disease study 2010. Lancet 2012; 380: 2224–2226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Rehm J., Anderson P., Barry J., Dimitrov P., Elekes Z., Feijão F. et al Prevalence of and potential influencing factors for alcohol dependence in Europe. Eur Addict Res 2015; 21: 6–18. [DOI] [PubMed] [Google Scholar]
- 3. Shield K., Parry C., Rehm J. Chronic diseases and conditions related to alcohol use. Alcohol Res Curr Rev 2013; 35: 155–171. [PMC free article] [PubMed] [Google Scholar]
- 4. Rehm J., Mathers C., Popova S., Thavorncharoensap M., Teerawattananon Y., Patra J. Global burden of disease and injury and economic cost attributable to alcohol use and alcohol‐use disorders. Lancet 2009; 373: 2223–2233. [DOI] [PubMed] [Google Scholar]
- 5. Heikkilä K., Nyberg S. T., Fransson E. I., Alfredsson L., de Bacquer D., Bjorner J. B. et al Job strain and alcohol intake: a collaborative meta‐analysis of individual‐participant data from 140 000 men and women. PLOS ONE 2012; 7: 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Virtanen M., Jokela M., Nyberg S. T., Madsen I. E. H., Lallukka T., Ahola K. et al Long working hours and alcohol use: systematic review and meta‐analysis of published studies and unpublished individual participant data. BMJ 2015; 350: g7772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Head J., Stansfeld S. A., Siegrist J. The psychosocial work environment and alcohol dependence: a prospective study. Occup Environ Med 2004; 61: 219–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Bobak M., Pikhart H., Kubinova R., Malyutina S., Pajak A., Sebakova H. et al The association between psychosocial characteristics at work and problem drinking: a cross‐sectional study of men in three eastern European urban populations. Occup Environ Med 2005; 62: 546–550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ames G. M., Bennett J. B. Prevention interventions of alcohol problems in the workplace. Alcohol Res Health 2011; 34: 175–187. [PMC free article] [PubMed] [Google Scholar]
- 10. Araki I., Hashimoto H., Kono K., Matsuki H., Yano E. Controlled trial of worksite health education through face‐to‐face counseling vs. e‐mail on drinking behavior modification. J Occup Health 2006; 48: 239–245. [DOI] [PubMed] [Google Scholar]
- 11. Hagger M. S., Lonsdale A., Chatzisarantis N. L. D. Effectiveness of a brief intervention using mental simulations in reducing alcohol consumption in corporate employees. Psychol Health Med 2011; 16: 375–392. [DOI] [PubMed] [Google Scholar]
- 12. Ito C., Yuzuriha T., Noda T., Ojima T., Hiro H., Higuchi S. Brief intervention in the workplace for heavy drinkers: a randomized clinical trial in Japan. Alcohol Alcohol 2015; 50: 157–163. [DOI] [PubMed] [Google Scholar]
- 13. Hermansson U., Helander A., Brandt L., Huss A., Ronnberg S. Screening and brief intervention for risky alcohol consumption in the workplace: results of a 1‐year randomized controlled study. Alcohol Alcohol 2010; 45: 252–257. [DOI] [PubMed] [Google Scholar]
- 14. Schulte B., O'Donnell A. J., Kastner S., Schmidt C. S., Schäfer I., Reimer J. Alcohol screening and brief intervention in workplace settings and social services: a comparison of literature. Front Psychiatry 2014; 5: 131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. de Matos E. G., Kraus L., Pabst A. Problembewusstsein und Inanspruchnahme von Hilfe bei substanzbezogenen Problemen [Awareness and help‐seeking behaviour in individuals with substance‐related problems]. SUCHT 2013; 59: 355–366. [Google Scholar]
- 16. Cunningham J. A., Breslin F. C. Only one in three people with alcohol abuse or dependence ever seek treatment. Addict Behav 2004; 29: 221–223. [DOI] [PubMed] [Google Scholar]
- 17. Saunders S. M., Zygowicz K. M., D'Angelo B. R. Person‐related and treatment‐related barriers to alcohol treatment. J Subst Abuse Treat 2006; 30: 261–270. [DOI] [PubMed] [Google Scholar]
- 18. Cook R., Schlenger W. Prevention of substance abuse in the workplace: review of research on the delivery of services. J Prim Prev 2002; 23: 115–142. [Google Scholar]
- 19. Reynolds G. S., Lehman W. E. K., Bennett J. B. Psychosocial correlates of the perceived stigma of problem drinking in the workplace. J Prim Prev 2008; 29: 341–356. [DOI] [PubMed] [Google Scholar]
- 20. Lehr D., Geraedts A., Asplund R., Khadjesari Z., Heber E., de Bloom J. et al Occupational e‐Mental Health—current approaches and promising perspectives for promoting mental health in workers In: Wiencke M., Fischer S., Cacace M., editors. Healthy at Work—Interdisciplinary Perspectives. Cham: Springer International Publishing; 2016, pp. 257–281. [Google Scholar]
- 21. Riper H., Blankers M., Hadiwijaya H., Cunningham J., Clarke S., Wiers R. et al Effectiveness of guided and unguided low‐intensity internet interventions for adult alcohol misuse: a meta‐analysis. PLOS ONE 2014; 9: e99912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. White A., Kavanagh D., Stallman H., Klein B., Kay‐Lambkin F., Proudfoot J. et al Online alcohol interventions: a systematic review. J Med Internet Res 2010; 12: e62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Donoghue K., Patton R., Phillips T., Deluca P., Drummond C. The effectiveness of electronic screening and brief intervention for reducing levels of alcohol consumption: a systematic review and meta‐analysis. J Med Internet Res 2014; 16: e142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Doumas D. M., Hannah E. Preventing high‐risk drinking in youth in the workplace: a web‐based normative feedback program. J Subst Abuse Treat 2008; 34: 263–271. [DOI] [PubMed] [Google Scholar]
- 25. Khadjesari Z., Newbury‐Birch D., Murray E., Shenker D., Marston L., Kaner E. Online health check for reducing alcohol intake among employees: a feasibility study in six workplaces across England. PLOS ONE 2015; 10: e0121174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Khadjesari Z., Freemantle N., Linke S., Hunter R., Murray E. Health on the web: randomised controlled trial of online screening and brief alcohol intervention delivered in a workplace setting. PLOS ONE 2014; 9: e112553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Grant B. F., Stinson F. S., Dawson D. A., Chou S. P., Dufour M. C., Compton W. et al Prevalence and co‐occurrence of substance use disorders and independent mood and anxiety disorders: results from the National Epidemiologic Survey on alcohol and related conditions. Arch Gen Psychiatry 2004; 61: 807–816. [DOI] [PubMed] [Google Scholar]
- 28. Schaub M. P., Blankers M., Lehr D., Boss L., Riper H., Dekker J. et al Efficacy of an internet‐based self‐help intervention to reduce co‐occurring alcohol misuse and depression symptoms in adults: study protocol of a three‐arm randomised controlled trial. BMJ Open 2016; 6; e011457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Frone M. R. Relations of negative and positive work experiences to employee alcohol use: testing the intervening role of negative and positive work rumination. J Occup Health Psychol 2015; 20: 148–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Ansoleaga E., Montaño R., Vézina M. Psychosocial risk at work and hazardous alcohol consumption among Chile's working adults. Can J Public Health 2013; 104: e502–e508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Puls W., Morkramer M. F., Wienold H. Arbeitsbedingungen, Persönlichkeitsmerkmale und Alkoholkonsum: Eine Befragung in zwei Betrieben der Metallindustrie [Working conditions, personality characteristics, and the consumption of alcohol: a survey carried out in two metal‐working companies]. Z Arb Organ 2005; 49: 69–84. [Google Scholar]
- 32. Blankers M., Koeter M. W. J., Schippers G. M. Internet therapy versus internet self‐help versus no treatment for problematic alcohol use: a randomized controlled trial. J Consult Clin Psychol 2011; 79: 330–341. [DOI] [PubMed] [Google Scholar]
- 33. Boß L., Lehr D., Berking M., Riper H., Schaub M., Ebert D. Evaluating the (cost‐)effectiveness of guided and unguided internet‐based self‐help for problematic alcohol use in employees ‐ a three arm randomized controlled trial. BMC Public Health 2015; 15: 1043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Babor T. F., Higgins‐Biddle J. C., Saunders J. B., Monteiro M. G. AUDIT: The Alcohol Use Disorders Identification Test: Guidelines for Use in Primary Care, 2nd edn. Geneva: World Health Organization; 2001. [Google Scholar]
- 35. Beck A. T., Steer A., Brown G. K. BDI‐II: Beck Depression Inventory Manual, 2nd edn. San Antonio: Psychological Corporation; 1996. [Google Scholar]
- 36. Hester R. K., Miller W. Handbook of Alcoholism Treatment Approaches: Effective Alternatives, 3rd edn. Boston: Allyn and Bacon; 2003. [Google Scholar]
- 37. Miller W. R., Muñoz R. F. Controlling Your Drinking: Tools to Make Moderation Work for You, 2nd edn. New York: Guilford Press; 2013. [Google Scholar]
- 38. Berking M., Ebert D., Cuijpers P., Hofmann S. G. Emotion regulation skills training enhances the efficacy of inpatient cognitive behavioral therapy for major depressive disorder: a randomized controlled trial. Psychother Psychosom 2013; 82: 234–245. [DOI] [PubMed] [Google Scholar]
- 39. Mohr D. C., Cuijpers P., Lehman K. Supportive accountability: a model for providing human support to enhance adherence to eHealth interventions. J Med Internet Res 2011; 13: e30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Zarski A.‐C., Lehr D., Berking M., Riper H., Cuijpers P., Ebert D. D. Adherence to internet‐based mobile‐supported stress management: a pooled analysis of individual participant data from three randomized controlled trials. J Med Internet Res 2016; 18: e146 https://doi.org/10.2196/jmir.4493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Sobell L. C., Agrawal S., Annis H., Ayala‐Velazquez H., Echeverria L., Leo G. I. et al Cross‐cultural evaluation of two drinking assessment instruments: alcohol timeline followback and inventory of drinking situations. Subst Use Misuse 2001; 36: 313–331. [DOI] [PubMed] [Google Scholar]
- 42. Toll B. A., Cooney N. L., McKee S. A., O'Malley S. S. Short communication correspondence between interactive voice response (IVR) and timeline Followback (TLFB) reports of drinking behavior. Addict Behav 2006; 31: 726–731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Rueger S. Y., Trela C. J., Palmeri M., King A. C. Self‐administered web‐based timeline followback procedure for drinking and smoking behaviors in young adults. J Stud Alcohol Drugs 2012; 73: 829–833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Lovibond P. F., Lovibond S. The structure of negative emotional states: comparison of the depression anxiety stress scales (DASS) with the Beck Depression and Anxiety Inventories. Behav Res Ther 1995; 33: 335–343. [DOI] [PubMed] [Google Scholar]
- 45. Mohr G., Müller A., Rigotti T., Aycan Z., Tschan F. The assessment of psychological strain in work contexts: concerning the structural equivalency of nine language adaptations of the irritation scale. Eur J Psychol Assess 2006; 22: 198–206. [Google Scholar]
- 46. Siegrist J., Wege N., Pühlhofer F., Wahrendorf M. A short generic measure of work stress in the era of globalization: effort‐reward imbalance. Int Arch Occup Environ Health 2009; 82: 1005–1013. [DOI] [PubMed] [Google Scholar]
- 47. Altman D. G. Better reporting of randomised controlled trials: the CONSORT statement. BMJ 1996; 313: 570–571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Schafer J. L., Graham J. W. Missing data: our view of the state of the art. Psychol Methods 2002; 7: 147–177. [PubMed] [Google Scholar]
- 49. Cohen J. Statistical Power Analysis for the Behavioral Sciences. Hillsdale, NJ: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- 50. Siegrist J., Starke D., Chandola T., Godin I., Marmot M., Niedhammer I. et al The measurement of effort–reward imbalance at work: European comparisons. Soc Sci Med 2004; 58: 1483–1499. [DOI] [PubMed] [Google Scholar]
- 51. Dedert E. A., McDuffie J. R., Stein R., McNiel J. M., Kosinski A. S., Freiermuth C. E. et al Electronic interventions for alcohol misuse and alcohol use disorders. Ann Intern Med 2015; 163: 205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Titov N., Dear B. F., Johnston L., Lorian C., Zou J., Wootton B. et al Improving adherence and clinical outcomes in self‐guided internet treatment for anxiety and depression: randomised controlled trial. PLOS ONE 2013; 8; e62873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Matano R., Koopman C., Wanat S. F., Winzelberg A. J., Whitsell S. D., Westrup D. et al A pilot study of an interactive web site in the workplace for reducing alcohol consumption. J Subst Abuse Treat 2007; 32: 71–80. [DOI] [PubMed] [Google Scholar]
- 54. Königbauer J., Letsch J., Doebler P., Ebert D., Baumeister H. Internet‐ and mobile‐based depression interventions for people with diagnosed depression: a systematic review and meta‐analysis. J Affect Disord 2017; 223: 28–40. [DOI] [PubMed] [Google Scholar]
- 55. Olthuis J. V., Watt M. C., Bailey K., Hayden J. A., Stewart S. H. Therapist‐supported internet cognitive behavioural therapy for anxiety disorders in adults. Cochrane Database Syst Rev 2015; 3; CD011565. [DOI] [PubMed] [Google Scholar]
- 56. Piaggio G., Elbourne D. R., Pocock S. J., Evans S. J. W., Altman D. G. Reporting of noninferiority and equivalence randomized trials. JAMA 2012; 308: 2594. [DOI] [PubMed] [Google Scholar]
- 57. Ebert D. D., Berking M., Cuijpers P., Lehr D., Pörtner M., Baumeister H. Increasing the acceptance of internet‐based mental health interventions in primary care patients with depressive symptoms. A randomized controlled trial. J Affect Disord 2015; 176: 9–17. [DOI] [PubMed] [Google Scholar]
- 58. Mohr D. C., Ho J., Hart T. L., Baron K. G., Berendsen M., Beckner V. et al Control condition design and implementation features in controlled trials: a meta‐analysis of trials evaluating psychotherapy for depression. Transl Behav Med 2014; 4: 407–423. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1 Means, standard deviations and effect sizes of all study groups on weekly standard units alcohol [imputation by baseline observation carried forward (BOCF)].
Table S2 Means, standard deviations and effect sizes of all study groups on secondary outcomes [imputation by baseline observation carried forward (BOCF)].
Table S3 Results of the primary outcome regression analyses [imputation by baseline observation carried forward (BOCF)].
Table S4 Summarized results of secondary outcomes regression analyses for the combined intervention groups compared to the control group [imputation by baseline observation carried forward (BOCF)].


