Abstract
Aim
Many countries require individuals with diabetes to adhere to standards regarding blood glucose testing in order to be granted or retain a driving licence. Currently, interstitial glucose results may not be used. The aim of this study was to determine whether interstitial glucose measurements using flash glucose‐sensing technology can provide additional information to augment safe driving.
Methods
Sensor data from two European studies (NCT02232698 and NCT02082184) of the FreeStyle Libre Glucose Monitoring System™ in insulin‐treated Type 1 and Type 2 diabetes, 241 and 224 participants respectively, were used to determine the frequency of a low interstitial sensor glucose result (< 3.9 mmol/l) up to 4 h subsequent to a daytime (07:00–21:00 h) capillary blood glucose result ≥ 5 mmol/l.
Results
Within 4 h of a capillary blood glucose result ≥ 5 mmol/l a sensor glucose result of < 3.9 mmol/l occurred on 22.0% of occasions (2573 of 11 706 blood glucose readings) for those with Type 1 diabetes, and 8.4% of occasions (699/8352) for those with Type 2 diabetes; 13.8% (1610/11 628) and 4.4% (365/8203) within 2 h, and 10.0% (1160/11 601) and 3.1% (254/8152) within 1.5 h. Analysis of sensor glucose results 5–7 mmol/l demonstrated the glucose trend arrow descending on 14.7% (1163/7894, Type 1 diabetes) and 9.4% (305/3233, Type 2 diabetes) of occasions.
Conclusions
Sensor‐based glucose information with directional arrows has the potential to support assessment of safe glucose levels associated with driving and offers distinct advantages over blood glucose testing for individuals with Type 1 and Type 2 diabetes to concord with driving safety standards.
What's new?
This study shows new information on the potential risk of developing hypoglycaemia while driving at a ‘safe’ glucose level despite complying with blood glucose testing requirements associated with driving.
Analysis of masked daytime flash sensor‐based glucose data and capillary blood glucose results for individuals with insulin‐treated Type 1 or Type 2 diabetes suggests that there is a significant risk of hypoglycaemia within the 4 h driving ‘window’ of blood glucose testing 2 h before/after starting to drive.
Risk may be higher for individuals with Type 1 diabetes than those with Type 2 diabetes treated with multiple daily injection therapy.
What's new?
This study shows new information on the potential risk of developing hypoglycaemia while driving at a ‘safe’ glucose level despite complying with blood glucose testing requirements associated with driving.
Analysis of masked daytime flash sensor‐based glucose data and capillary blood glucose results for individuals with insulin‐treated Type 1 or Type 2 diabetes suggests that there is a significant risk of hypoglycaemia within the 4 h driving ‘window’ of blood glucose testing 2 h before/after starting to drive.
Risk may be higher for individuals with Type 1 diabetes than those with Type 2 diabetes treated with multiple daily injection therapy.
Introduction
In the UK, the Driver and Vehicle Licensing Agency (DVLA) issues driving licences to comply with both European Union and UK legislation. Drivers with diabetes are subject to restrictions on their licences and for many individuals with diabetes there are additional standards to be met in order to obtain or retain their licence including: demonstrating safe glucose management, awareness of hypoglycaemia, no more than one severe hypoglycaemic event per year, and blood glucose testing relevant to driving 1. The relatively recent European legislative requirement to report severe hypoglycaemia has prompted much discussion 2, 3, 4, whereas the obligation to test glucose levels prior to/during driving, which has been present in some countries for more than a decade, has received scant attention 5, 6. Diabetes specialists generally recommend glucose levels of ≥ 5 mmol/l as a ‘safe’ glucose threshold for driving 7. Blood glucose testing is both a legal requirement 1 and considered crucial for safe driving with diabetes 8, particularly in those treated with insulin 4. UK drivers with insulin‐treated diabetes should test their blood glucose level within 2 h of the start of their journey and at least every 2 h into their journey 1. Thus, according to this regulation up to 4 h could elapse after blood glucose testing before another test is required to continue driving. Our aim was to evaluate data from participants performing capillary blood glucose testing and sensor‐based flash glucose monitoring to determine the likelihood of hypoglycaemia occurring within this time period and whether interstitial sensor glucose results could provide additional information to inform driving decisions.
Methods
The FreeStyle Libre™ Glucose Monitoring System is described in detail elsewhere 9. Briefly, after sensor scanning, the reader displays 8 h of historic glucose data and current sensor glucose result with a glucose trend arrow indicating the direction and rate of change.
Arrows are defined as: ↑, increasing > 0.1 mmol/l/min; ↗ , increasing 0.06–0.1 mmol/l/min; →, changing < 0.06 mmol/l/min; ↘ , decreasing 0.06–0.1 mmol/l/min; and ↓, decreasing > 0.1 mmol/l/min.
We retrospectively analysed blood glucose results and interstitial sensor readings from two European randomized controlled trials (NCT02232698 and NCT02082184) to determine the frequency with which a low sensor glucose result (< 3.9 mmol/l) occurred after a capillary blood glucose result ≥ 5 mmol/l, the level considered safe for driving. In both studies the analysis was confined to waking hours (07:00–21:00 h) for a 14‐day masked sensor wear (sensor glucose results were not visible to participants). Study one was in 241 adults with well‐controlled Type 1 diabetes (HbA1c < 58 mmol/mol; < 7.5%) 10 and study two in 224 adults with Type 2 diabetes treated with intensive insulin therapy (HbA1c 58–108 mmol/mol; 7.5–12%) 11. Analysis of 15‐min historic interstiti glucose sensor results was performed for the 4‐h period subsequent to a capillary blood glucose results of ≥ 5 mmol/l. The frequency of each of the downward direction arrows was calculated for all current interstitial glucose sensor results obtained in 07:00–21:00 h between 5 and 7 mmol/l. The frequency with which a low sensor glucose result (< 3.9 mmol/l) occurred after a sensor glucose result 5‐7 mmol/l, separately for downward or upward trend arrows, was calculated. For individuals with Type 1 diabetes responses to the hypoglycaemia status questionnaire were compared to the control group using the Wilcoxon Rank Sum Test.
Results
The analysis showed that subsequent to a finger stick blood glucose result ≥ 5 mmol/l, a sensor glucose result < 3.9 mmol/l occurred within 1.5 h on 10.0% of occasions for adults with Type 1 diabetes (1160 of 11 601 blood glucose readings ≥ 5 mmol/l) and 3.1% of occasions for adults with Type 2 diabetes (254 of 8152), increasing to 13.8% (1610 of 11628) and 4.4% (365 of 8203), respectively, after 2 hours and to 22% (2573 of 11 706) and 8.4% (699 of 8352), respectively, after 4 h. A sensor glucose result of < 3.0 mmol/l occurred on 3.1%, 5.0% and 9.2% of occasions within 1.5, 2 and 4 h respectively for Type 1 diabetes, and on 1.0%, 1.5% and 3.1% of occasions for Type 2 diabetes.
Analysis of the same masked sensor wear period of sensor results between 5 and 7 mmol/l showed the trend arrow descending (↘ decreasing 0.06–0.1 mmol/l/min or ↓ decreasing > 0.1 mmol/l/min) on 14.7% of occasions for participants with Type 1 diabetes (1163 of 7894 sensor glucose readings) and 9.4% of occasions for those with Type 2 diabetes (305 of 3233). Analysis of a higher glucose range (8–12 mmol/l) showed the trend arrow descending on 13.4% and 9.6% of occasions, respectively. Further analysis of sensor glucose results 5–7 mmol/l showed that, for individuals with Type 1 diabetes, a sensor glucose level < 3.9 mmol/l occurred within 2 h on 38.8% of occasions with a downward glucose trend arrow and on 10.3% of occasions with an upward arrow, demonstrating the predictive value of the trend arrow.
Prior to randomization, participants in study one (in Type 1 diabetes) completed a hypoglycaemia status questionnaire which included asking: ‘Do you check your blood glucose before driving?’ The optional answers were: yes always, yes sometimes, or no. By the end of the study, the likelihood of sensor glucose being checked before driving was significantly increased for intervention participants using FreeStyle Libre compared with controls using blood glucose testing (P = 0.0262) 10.
Discussion
Driving performance and safety are undoubtedly affected by hypoglycaemia, which is recognized as a cause for road traffic accidents 4. Modern glucose monitoring technology is a significant component of diabetes care; to date, the DVLA does not recognize the use of interstitial glucose measurements when assessing ability to drive with diabetes. An isolated blood glucose result > 5 mmol/l is perceived as an acceptable level for driving and, theoretically, following the ‘5 to drive’ principle and DVLA guidance, there could be 4 h between the blood glucose test performed prior to a journey and a blood glucose test taken after 2 h spent driving. Our analysis of masked daytime sensor data for individuals with insulin‐treated Type 1 or Type 2 diabetes suggests that there is a significant risk of hypoglycaemia within the 4‐h driving ‘window’ even when blood glucose testing is concordant with DVLA requirements. Any additional information to support thorough assessment of the current, prospective or retrospective risk of hypoglycaemia would be advantageous and is generally unavailable with finger stick blood glucose testing. Furthermore, our findings highlight that an elevated blood glucose level is not necessarily protective against falling glucose levels within a few hours.
Recent population‐based data indicate that day‐to‐day blood glucose testing frequency is low, with a mean number of test strips dispensed per day of 1.5 for insulin‐treated Type 2 diabetes and 2.6 for Type 1 diabetes, with around one‐third of individuals with Type 1 diabetes probably not testing at all 12. These results support findings that up to 60% of drivers with diabetes never test their glucose level before driving and this low testing frequency has changed little in the last decade 5, 6, 13, 14. Reasons for not regularly performing blood glucose testing before driving include inconvenience and not having access to a blood glucose meter or strips 13. As recently as 2010, a UK study reported only 65% of insulin using drivers would ‘consider’ blood glucose testing before driving and the mean length of time they would drive before re‐checking their glucose level was 2.8 h 15. Adequate hypoglycaemic awareness is a pre‐requisite for driving and the expected response on experiencing hypoglycaemic symptoms is to stop, however, many drivers continue to drive 4. Use of continuous monitoring with alarms may be advantageous for those with reduced, but not absent awareness of hypoglycaemic symptoms.
Despite the increased focus on hypoglycaemia reporting for licence holders, little else seems to have changed and many drivers continue to neglect the requirement for blood glucose testing associated with driving. With flash glucose technology, a quick sensor scan may be performed as often as every minute to display the current glucose level with a glucose trend arrow, in addition to a graph of 8 h of historic data (Fig. 1). The questionnaire responses indicate that scanning may be performed more regularly than blood glucose testing and there were no significant differences in treatment effects between age groups. Consistent, frequent use of FreeStyle Libre sensor glucose results exceeding self‐reported daily rates for blood glucose testing by up to five times in adults of all ages with insulin‐treated diabetes has been reported, indicating good acceptance of and confidence in this technology. Furthermore, flash technology is associated with significant, clinically meaningful reductions in both daytime and nocturnal hypoglycaemia 10, 11. Speculatively, if licence holders were able to utilize flash technology they are likely to access their glucose levels more frequently than has been reported for blood glucose testing, potentially enhancing general awareness of their sensor glucose level and trend before driving. It may also enable prospective hypoglycaemia avoidance management for driving.
Figure 1.
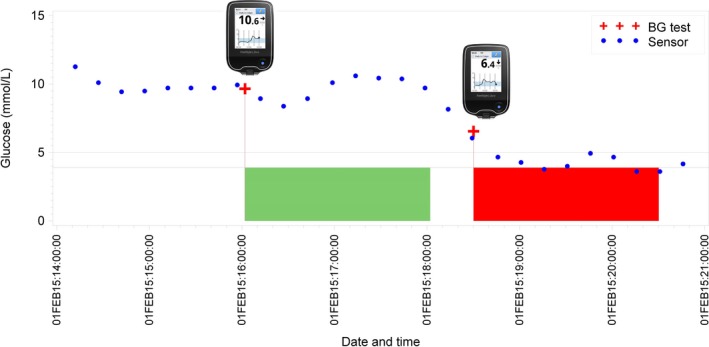
Example of daytime masked sensor glucose data and blood glucose (BG) results. Green shading signifies no sensor glucose results < 3.9 mmol/l in the 2 h after the BG reading ≥ 5 mmol/l. Red shading signifies at least one sensor glucose result < 3.9 mmol/l in the 2 h after the BG reading ≥ 5 mmol/l.
Because the sensor glucose data were masked, participants were unable to respond to them. On‐going glucose management was based solely on finger stick blood glucose levels, which may have triggered behaviour modifications such as increased food intake. This is one limitation of our analysis; furthermore, the glucose trend arrow findings in particular, should be interpreted with caution because of this. As we did not set out to evaluate glucose levels associated with driving, further limitations of the analysis are that the licence status of the participants and any periods of driving undertaken during the 14‐day wear are unknown. However, this is also potentially an advantage as participants and investigators in both the studies were unaware of this analysis and were not prompted to discuss or review blood glucose testing and driving requirements. Therefore, bias or influence is limited, enabling our results to be more reflective of real world conditions.
In conclusion, we believe that use of FreeStyle Libre sensor glucose results has the potential to offer licence holders with diabetes treated with insulin or at risk of hypoglycaemia distinct advantages over isolated blood glucose tests. This comprehensive glucose information could be invaluable to support decisions regarding safe glucose levels and ability to drive, hypoglycaemic risk assessment prior to driving to reduce the likelihood of an event whilst driving, and when to re‐test on longer journeys. Finally, although we did not set out to directly assess the impact of unmasked Freestyle Libre use on hypoglycaemia during driving, given that daytime hypoglycaemia was reduced in both Type 1 and Type 2 diabetes study groups in the two European randomized controlled trials described, it would be reasonable to expect that this would also be associated with a reduced frequency of hypoglycaemia during driving.
Funding sources
This retrospective study used data from two randomized controlled trials (NCT02232698 and NCT02082184). For both studies, Abbott Diabetes Care, in collaboration with the principal investigator for each country, designed the study protocol and provided all materials for the study. Abbott Diabetes Care was involved in the process for data collection, result reporting and funded medical writing services for these studies. For this submission, Abbott Diabetes Care was involved in the process for data collection and result reporting. Abbott Diabetes Care was not involved in the authors’ interpretation of the findings. The corresponding author had full access to the all the data in the study and, together with the authors, had final responsibility for the decision to submit for publication.
Competing interests
GR reports personal fees from Abbott Diabetes Care outside the submitted work. JK reports personal fees from Abbott Diabetes Care during the conduct of the study, personal fees from Abbott Diabetes Care, Lilly, Novo Nordisk, Berlin Chemie Medtronic, Sanofi MSD and AstraZeneca outside the submitted work. JB has received honoraria for consulting or lecture fees from Abbott Diabetes Care, AstraZeneca, Insulet Corporation, Integrity Applications, Novo Nordisk, and Sanofi‐Aventis.
Acknowledgements
We thank all the individuals who contributed to the original data collection at the sites for both studies. We also thank Zoë Welsh (Abbott Diabetes Care) for statistical support).
Diabet. Med. 35, 491–494 (2018)
[Correction: The Creative Commons license for this article was changed on 8 November 2017 after original online publication.]
References
- 1. Driver and Vehicle Licensing Agency (DVLA) . Assessing fitness to drive – a guide for medical professionals 2017. Available at https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/596959/assessing-fitness-to-drive-a-guide-for-medical-professionals.pdf Last accessed 5 April 2017.
- 2. Min T, Dixon AN. Driving and insulin‐treated diabetes. J Diabetes Nurs 2015; 19: 255–259. [Google Scholar]
- 3. Pedersen‐Bjergaard U, Faerch L, Allingbjerg ML, Agesen R, Thorsteinsson B. The influence of New European Union driver's license legislation on reporting of severe hypoglycaemia by patients with Type 1 diabetes. Diabetes Care 2015; 38: 29–33. [DOI] [PubMed] [Google Scholar]
- 4. Graveling AJ, Frier BM. Driving and diabetes: problems, licensing restrictions and recommendations for safe driving. Clin Diabetes Endocrinol 2015; 1–8. Available at https://clindiabetesendo.biomedcentral.com/articles/10.1186/s40842-015-0007-3 Last accessed 23 June 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Watson WA, Currie T, Lemon JS, Gold AE. Driving and insulin treated diabetes: who knows the rules and recommendations? Pract Diabetes 2007; 24: 201–206. [Google Scholar]
- 6. Graveling AJ, Warren RE, Frier BM. Hypoglycaemia and driving in people with insulin treated diabetes: adherence to recommendations for avoidance. Diabet Med 2004; 21: 1014–1019. [DOI] [PubMed] [Google Scholar]
- 7. Gallen I, Amiel S, Robinson T. McKnight J, on behalf of the ABCD Committee. Driving and hypoglycaemia: questions and answers. Pract Diabetes 2012; 29: 13–14. [Google Scholar]
- 8. Diabetes and Driving in Europe: A report of the second European working group on diabetes and driving, an advisory board to the Driving Licence Committee of the European Union , 2006. Available at http://ec.europa.eu/transport/road_safety/pdf/behavior/diabetes_and_driving_in_europe_final_1_en.pdf Last accessed 5 April 2017.
- 9. Bailey T, Bode BW, Christiansen MP, Klaff LJ, Alva S. The performance and usability of a factory‐calibrated flash glucose monitoring system. Diabetes Technol Ther 2015; 17: 787–794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bolinder J, Antuna R, Geelhoed P, Kroeger J, Weitgasser R. Using novel flash glucose‐sensing technology reduces hypoglycemia in individuals with Type 1 diabetes. Lancet 2016; 388: 2254–2263. [DOI] [PubMed] [Google Scholar]
- 11. Haak T, Hanaire H, Ajjan RA, Hermanns N, Riveline J‐P, Rayman G. Flash glucose‐sensing technology as a replacement for blood glucose monitoring for the management of insulin‐treated type 2 diabetes: a multicenter, open‐label randomized controlled trial. Diabetes Ther 2017; 8: 55–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Cameron D, Harris FM, Evans JMM. Patterns of self‐monitoring of blood glucose (SMBG) in insulin treated diabetes: analysis of a Scottish population over time. Diabetes Obes Metab 2016; 18: 729–731. [DOI] [PubMed] [Google Scholar]
- 13. Inkster B, Pooley D, De Saxe H, Ahraf M, Frier B. Blood glucose testing by drivers with diabetes: a survey of glucose meter users. Br J Diabetes, Vasc Dis 2015; 15: 20–23. [Google Scholar]
- 14. Bell D, Huddart A, Krebs J. Driving and insulin treated diabetes: comparing practices in Scotland and New Zealand. Diabet Med 2010; 27: 1093–1095. [DOI] [PubMed] [Google Scholar]
- 15. Jackson‐Koku G, Morrison G, Morrison CL, Weston PJ. Insulin‐treated diabetes and driving: what is the patient's knowledge of current regulations? Br J Diabetes Vasc Dis 2010; 10: 31–34. [Google Scholar]


