Abstract
Background
Implementation of the first Danish helicopter emergency medical service (HEMS) was associated with reduced time from first medical contact to treatment at a specialized centre for patients with suspected ST elevation myocardial infarction (STEMI). We aimed to investigate effects of HEMS on mortality and labour market affiliation in patients admitted for primary percutaneous coronary intervention (PCI).
Methods
In this prospective observational study, we included patients with suspected STEMI within the region covered by the HEMS from January 1, 2010, to April 30, 2013, transported by either HEMS or ground emergency medical services (GEMS) to the regional PCI centre. The primary outcome was 30‐day mortality.
Results
Among the 384 HEMS and 1220 GEMS patients, time from diagnostic ECG to PCI centre arrival was lower with HEMS (median 71 min vs. 78 min with GEMS; P = 0.004). Thirty‐day mortality was 5.0% and 6.2%, respectively (adjusted OR = 0.82, 95% CI 0.44–1.51, P = 0.52. Involuntary early retirement rates were 0.62 (HEMS) and 0.94 (GEMS) per 100 PYR (adjusted IRR = 0.68, 0.15–3.23, P = 0.63). The proportion of patients on social transfer payments longer than half of the follow‐up time was 22.1% (HEMS) vs. 21.2% (adjusted OR = 1.10, 0.64–1.90, P = 0.73).
Conclusion
In an observational study of patients with suspected STEMI in eastern Denmark, no significant beneficial effect of helicopter transport could be detected on mortality, premature labour market exit or work ability. Only a study with random allocation to one system vs. another, along with a large sample size, will allow determination of superiority of helicopter transport.
Editorial comment.
In this observational assessment of long‐term outcomes for acute myocardial patients, based on the type of ambulance system which transported them to the tertiary care centre for their acute revascularization procedure, no differences could be identified in associations of outcome with helicopter or ground‐based ambulance system. Still, to understand if the prehospital system type can cause a better outcome, a randomized clinical trial would be needed.
Coronary heart disease is a leading cause of death and morbidity in Western countries, but a great reduction in mortality has been achieved throughout the last couple of decades1. New invasive techniques and medical treatments have improved the chance of surviving the acute phase of a myocardial infarction; consequently, awareness has increased regarding the importance of improving the long‐term outcome as well. Return to work can be a desirable goal of cardiac rehabilitation2, 3, 4, 5.
Since 2003, primary percutaneous coronary intervention (pPCI) for ST‐segment elevation myocardial infarction (STEMI) has been the preferred therapy in Denmark if performed within 120 min of symptom onset. Centralization of PCI at designated centres increases the volume and experience at each centre but may lead to increased average transport distance and time, which is associated with increased mortality after pPCI6. Transportation by helicopter is often quicker than ground transport7, 8 and thus may improve overall prognosis9 through reduced ischaemic injury and infarction size.
The first Danish helicopter emergency medical service (HEMS), implemented in eastern Denmark on May 1, 201010, significantly reduced the time from the electrocardiogram (ECG) diagnosis on‐scene to arrival at the cardiac catheterization laboratory, despite longer transport distances. In addition, 30‐day mortality in HEMS patients tended to be lower10.
The aim of the present study was to investigate the effect of HEMS on mortality and labour market affiliation for patients admitted for pPCI during the first 3 years after HEMS implementation. We hypothesized that HEMS‐transported patients admitted for pPCI would have lower 30‐day mortality compared to patients transported by ground emergency medical services (GEMS).
Methods
Study design and setting
This single‐centre, prospective, observational study had up to 5.5 years of follow‐up. The HEMS covered a catchment area of 8400 km2 in the eastern part of Denmark with a population of approximately 1.1 million. It operated during daylight only and was staffed with a consultant in anaesthesiology, a HEMS crew member (paramedic), and a pilot. Dispatches were for both pre‐hospital and in‐hospital (referral) patients with suspected STEMI if driving duration to the PCI centre at Rigshospitalet was expected to exceed 30 min, which was changed to 25 min shortly after the implementation of HEMS. Two designated maps (rush hour/non‐rush hour) with estimated time interval markings were available for the dispatchers with the purpose of correct dispatch of the HEMS. Furthermore, the dispatch centre had Geographical Information Systems to aid this process.
GEMS in eastern Denmark is organized as a partially 1‐tier or 2‐tier ground unit system. In case of critical illness, a primary unit (ground ambulance) staffed with two emergency medical services (EMS) personnel, either trained as basic life support providers or paramedics, is dispatched. All units are allowed to administer heparin and other anticoagulant medication after telephone contact with a cardiologist at the PCI centre. Depending on availability and determined by either the dispatch centre or assessed by the primary unit, a physician‐staffed mobile emergency care unit (MECU) can, on rare occasions, attend the scene. Both units operate 24 h a day 7 days a week. The MECU was discontinued in most of the Region Zealand in March 2011.
Ground ambulances are equipped for acquisition and transmission of ECG data for rapid interpretation by a triaging cardiologist. Patients can be transported directly to the designated PCI centre in Copenhagen for immediate coronary angiography, and pPCI can be performed if indicated. The PCI centre is situated at Rigshospitalet, an urban, highly specialized hospital in the Capital Region of Denmark. This centre was merged on June 1, 2011, with another PCI centre in the region, creating a “mega‐centre” serving about 2.5 million people and 10,000 km2, performing around 1000 pPCIs annually11.
Participant selection
We included all patients suspected of having STEMI in the geographical area covered by both the HEMS and GEMS and who were admitted to the PCI centre at Rigshospitalet. The geographical catchment area was defined as the area from where the HEMS transported patients in the first year of implementation. We included patients with first‐time admission to the PCI centre during the inclusion period from January 1, 2010, until April 30, 2013. This 40‐month period consisted of the initial 16‐month period from the first HEMS study10 plus an additional 24‐month data collection period. Patients were followed until May 1, 2015, or death, whichever came first. Patients without EMS data were excluded.
Exposure
We compared patients transported by HEMS in a 36‐month period (May 1, 2010–April 30, 2013) with patients transported by GEMS in a 40‐month period (January 1, 2010–April 30, 2013).
Data sources
PCI data
Data from existing databases at the PCI centre (Rigshospitalet) were analysed. These databases contain information on demographics, comorbidity, Killip class, time of symptom onset, diagnostic ECG, the pre‐hospital, in‐hospital, and procedure‐specific time intervals, and pre‐procedural clinical status. The Killip class (I–IV) stratifies patients with acute myocardial infarction according to severity of heart failure and is related to risk of death within 30 days12. Hospital records were used in case of missing data in the databases.
EMS data
Data on geographic location, demographics, transport mode, and specific transport time interval were extracted from either EMS databases at the pre‐hospital centres in Region Zealand (GEMS data) and the Capital Region of Denmark (HEMS data) or from hospital records.
Vital status
Information about death or migration was extracted via the Danish Civil Registration System (DCRS). DCRS uses the unique Civil Personal Registration number assigned to all citizens at birth or immigration.
Labour market data (the DREAM database)
Data on employment status in Denmark were obtained from the Danish Agency of Labour market and Recruitment's DREAM (Danish Register for Evaluation of Marginalization) database, which holds information on all social transfer payments such as sickness benefits, unemployment benefits, social assistance, and pensions (disability and old‐age pension). The DREAM database is updated weekly with a latency period of 3 months. Citizens who receive social transfer payments are registered on a weekly basis with a code corresponding to the person's current employment status.
Outcome measures
The primary outcome was 30‐day mortality after admission to the PCI unit. Secondary outcomes were 1‐year mortality, mortality rates over the follow‐up period, involuntary early retirement rates, the prevalence of reduced work ability, and the percentage of time on social transfer payments during the first 2 years after admission to the PCI unit.
Statistical analyses
Continuous variables are reported as medians and interquartile range (IQR) and were compared using the Mann–Whitney U test. Categorical data are reported as numbers (%). Group characteristics were compared by the Chi‐square or Fisher's exact test where appropriate. We considered P values < 0.05 as statistically significant. SAS 9.4 (SAS Institute Inc., Cary, NC, USA) was used for statistical analyses.
The 30‐day and 1‐year mortality values were compared between HEMS and GEMS patients by logistic regression, adjusting for gender, age, resuscitated cardiac arrest before hospital admission, inter‐hospital transfer, and acute cardiac failure defined as Killip class I/II or III/IV as dichotomous variable, assessed at hospital admission. Some analyses also included transport time (i.e. diagnostic ECG to arrival at the hospital), daytime vs. nighttime and use of vasopressors. Time to death was visualized by Kaplan–Meier curves. Event rates were compared using multivariable Cox proportional hazard regression models adjusted for gender, age, resuscitated cardiac arrest, inter‐hospital transfer, and Killip class III or IV prior to admission.
Reduced work ability 2 years after admission (yes/no) and time on social transfer payments (less than/equal vs. more than 50% of the time) during the first 2 years after admission were assessed by logistic regression models adjusted for the same explanatory variables as in the primary outcome analysis. Work ability 2 years after admission was divided into either full work ability or reduced work ability. In these analyses, we excluded patients not working full time 3 weeks prior to admission as well as patients with resuscitated cardiac arrest before hospital admission.
Each of these statistical analyses was performed on the following groups: (1) those aged 18–60 years, to ensure a sample at risk of only involuntary early retirement during the full follow‐up period (i.e., not eligible for voluntary early retirement); (2) those aged 18–67 years, because the public retirement scheme (old‐age pension plan) in Denmark is available for those aged 65 years (statutory retirement age at the time of the study) or older, but some patients may choose to postpone their retirement until age 67; thus, we include all patients still at risk of premature exit from the labour market; and (3) all ages, included to describe the total population.
Additional analyses
For sensitivity analyses, the 30‐day mortality analysis was performed only on directly referred (“field triaged”) patients who underwent acute PCI. Not all patients who undergo acute coronary angiography receive coronary intervention (balloon/stenting) because a coronary stenosis is not always detected. Furthermore, we performed an analysis of patients with the longest transport distances to see if a higher proportion of patients in the HEMS group had PCI done within a specific time limit. For the time interval between first medical contact and “balloon”, a 120 min limit has been used but in our analysis, we used the time interval between symptom onset to “balloon”. Based on a study of similar patients from Denmark, we added 30 min (estimated time from symptom onset to first medical contact) to the 120 min and used 150 min as the cut‐off in the analysis13.
Finally, we repeated the analyses of all outcomes with adjustment also for transport distance.
Sample size determination
In the previous study in patients bound for pPCI10, the investigators included 450 patients, of whom 114 were transported by HEMS and 336 by GEMS, for a ratio of 1 : 3. The 30‐day mortality was 2.6% in the HEMS group and 6.3% in the GEMS group. In the present study, we extended the inclusion period by 2 years and thus expected approximately 1350 patients. This number of patients would be adequate to detect a similar difference in 30‐day mortality with a power of 80% at the 5% significance level.
Ethics
The study was approved by the Danish Data Protection Agency (file number: 2013‐41‐1973 and 2013‐231‐0042) and by the National Board of Health (file number: 3‐3013‐352/1/HKR). Approval from the Ethics Committee was not required for this study.
Clinical Trial registration
The study was registered at ClinicalTrials.gov (NCT02512991) before data analysis.
Results
A total of 4165 patients were admitted to the PCI centre for acute angiography during the 40‐month inclusion period, and 1604 of them were eligible for inclusion in the study (Fig. 1). The 2547 patients who did not meet the inclusion criteria were patients outside the catchment area (n = 1416), and patients who had acute coronary angiography on other indications than primary PCI or acute PCI > 12 h (n = 1131). Median follow‐up time was 38 (IQR 29–47) months.
Figure 1.
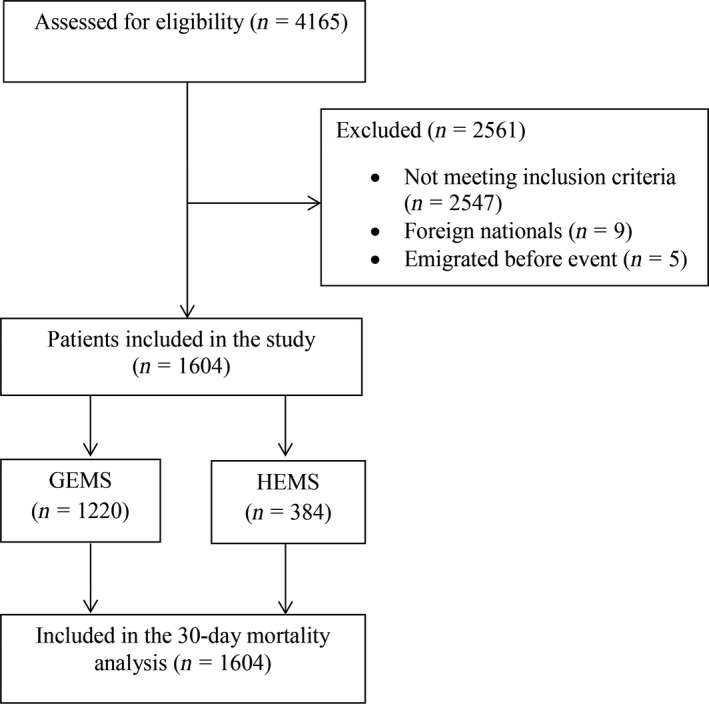
Flowchart of included patients admitted for primary percutaneous coronary intervention. GEMS, ground emergency medical services; HEMS, helicopter emergency medical services.
GEMS and HEMS patients were comparable in relation to gender, age, co‐morbidity, resuscitated cardiac arrest, acute cardiac failure, labour market affiliation, door‐to‐balloon time, and the proportion of patients who received acute PCI. A greater proportion of GEMS patients were referred from other hospitals; 35.4% vs.18.4% (P < 0.0001), and at full work ability at baseline (46.2% vs. 39.1%, P = 0.043) compared to HEMS patients. However, time (median) from diagnostic ECG to arrival at the PCI centre was significantly lower in the HEMS group; 71 min vs. 78 min in the GEMS group (P = 0.004), despite significantly longer transport distances (median); 110 km in the HEMS group vs. 77 km in the GEMS group (P < 0.0001; Table 1). The percentage of patients with time from diagnostic ECG to PCI < 90 min was 716/1114 (64.3%) (490 missing).
Table 1.
Characteristics for patients admitted for primary percutaneous coronary intervention
| GEMS (n = 1220) | HEMS (n = 384) | Total (n = 1604) | Missing | P value | |
|---|---|---|---|---|---|
| Gender, n (%) | 0 | 0.75 | |||
| Male | 889 (72.9) | 283 (73.7) | 1172 (73.1) | ||
| Age, median (IQR) | 64 (55–73) | 64 (55–71) | 64 (55–72) | 0 | 0.96 |
| Age, n (%) | 0 | 0.50 | |||
| 18–60 years | 514 (42.1) | 157 (40.9) | 671 (41.8) | ||
| 61–67 years | 267 (21.9) | 95 (24.7) | 362 (22.6) | ||
| ≥68 years | 439 (36.0) | 132 (34.4) | 571 (35.6) | ||
| Diabetes, n (%) | 63 | 0.08 | |||
| Yes | 150 (12.8) | 34 (9.3) | 184 (11.9) | ||
| Hypertensiona, n (%) | 99 | 0.32 | |||
| Yes | 464 (40.5) | 135 (37.5) | 599 (39.8) | ||
| Hyperlipidaemiaa, n (%) | 231 | 0.58 | |||
| Yes | 311 (29.6) | 90 (27.9) | 401 (29.2) | ||
| Active smokera, n (%) | 158 | 0.42 | |||
| Yes | 520 (47.1) | 170 (49.7) | 690 (47.7) | ||
| Previous myocardial infarction, n (%) | 108 | 0.35 | |||
| Yes | 102 (8.9) | 38 (10.7) | 140 (9.4) | ||
| Inter‐hospital transfer, n (%) | 22 | <0.0001 | |||
| Yes | 428 (35.4) | 69 (18.4) | 497 (31.4) | ||
| Resuscitated cardiac arrest, n (%) | 139 | 0.85 | |||
| Yes | 82 (7.4) | 25 (7.1) | 107 (7.3) | ||
| Acute cardiac failure, n (%) | 288 | 0.09 | |||
| Yes | 48 (4.8) | 8 (2.6) | 56 (4.3) | ||
| Fulltime work before event (37 h/week), n (%) | 0 | 0.06 | |||
| Yes | 508 (41.6) | 139 (36.2) | 647 (40.3) | ||
| Work ability, n (%) | 0 | 0.04 | |||
| Full work ability | 563 (46.2) | 150 (39.1) | 713 (44.5) | ||
| Reduced work ability | 46 (3.8) | 24 (6.3) | 70 (4.4) | ||
| Involuntary early retirement | 124 (10.2) | 41 (10.7) | 165 (10.3) | ||
| Retirement | 435 (35.7) | 146 (38.0) | 581 (36.2) | ||
| Voluntary early retirement | 52 (4.3) | 23 (6.0) | 75 (4.7) | ||
| Acute PCI performed, n (%) | 1 | 0.95 | |||
| Yes | 999 (81.89) | 315 (82.03) | 1314 (81.92) | ||
| Door‐to‐balloon time (min)b, median (IQR) | 32 (26–40) | 31 (25–40) | 32 (26–40) | 411 | 0.57 |
| Time from diagnostic ECG to arrival at the PCI centre (min), median (IQR) | 78 (56–107) | 71 (60–86) | 75 (57–100) | 490 | 0.0037 |
| Transport distance (km), median (IQR) | 77 (49–110) | 110 (98–133) | 94 (54–111) | 86 | <0.0001 |
| Use of vasopressor, n (%) | 139 | 0.20 | |||
| Yes | 46 (4.1) | 9 (2.5) | 55 (3.8) | ||
| Time of Diagnostic ECG, n (%) | 449 | <0.0001 | |||
| Night (20:01–07:59) | 355 (40.3) | 19 (6.9) | 374 (32.4) | ||
| Day (8:00–20:00) | 525 (59.7) | 256 (93.1) | 781 (67.6) | ||
GEMS, ground emergency medical services; HEMS, helicopter emergency medical services; IQR, interquartile range; PCI, percutaneous coronary intervention; ECG, electrocardiogram.
Defined by the treating physician.
Defined as the time from arrival at the PCI centre to time of inflation of the first balloon in the coronary artery lesion in the cardiac catheterization laboratory.
The result of the primary analysis of 30‐day mortality showed no significant difference between groups; 6.2% (GEMS) vs. 5.0% (HEMS), adjusted OR = 0.82 (CI 0.44–1.51, P = 0.52). Neither 1 year mortality nor mortality rates were significantly different either (Table 2 and Fig. 2). Our labour market analyses were limited to the 32% of patients aged 18–67 years who were working full time before the cardiac event and who did not suffer cardiac arrest before admission.
Table 2.
Outcome in patients admitted for primary percutaneous coronary intervention
| Number of persons under observation in each group (GEMS/HEMS) | GEMS n (%) | HEMS n (%) | Unadjusted OR (95%CI) | P value | Adjusteda OR (95%CI) | P value | Adjustedb OR (95%CI) | P value | Adjustedc OR (95%CI) | P value | Adjustedd OR (95%CI) | P value | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 30‐day mortality (n = 1604) | 1220/384 | – | – | 76 (6.2) | 19 (5.0) | 0.78 (0.47–1.31) | 0.35 | 0.82 (0.44–1.51) | 0.52 | 0.86 (0.37–1.97) | 0.72 | 0.99 (0.53–1.87) | 0.98 | 1.05 (0.39–2.85) | 0.91 |
| 30‐day mortality in directly referred patients who underwent PCI (n = 920) | 659/261 | – | – | 24 (3.6) | 10 (3.8) | 1.05 (0.50–2.24) | 0.89 | 1.20 (0.52–2.79) | 0.67 | ||||||
| 1‐year mortality (n = 1601) | 1218/383 | – | – | 111 (9.1) | 33 (8.6) | 0.94 (0.63–1.41) | 0.77 | 1.05 (0.66–1.67) | 0.85 | 1.22 0.67–2.21) | 0.80 | 1.04 (0.63–1.71) | 0.89 | 1.60 (0.81–3.12) | 0.17 |
| Reduced work ability 2 years after admission (n = 514) | 401/113 | – | – | 104 (25.9) | 26 (23.0) | 0.85 (0.52–1.40) | 0.53 | 0.91 (0.52–1.60) | 0.75 | 0.66 (0.30–1.46) | 0.30 | 0.90 (0.50–1.61) | 0.72 | 0.88 (0.42–1.85) | 0.74 |
| Over 50% of time on social transfer payments during the first 2 years after admission (n = 514) | 401/113 | – | – | 85 (21.2) | 25 (22.1) | 1.06 (0.64–1.75) | 0.83 | 1.10 (0.64–1.90) | 0.73 | 1.17 (0.61–2.25) | 0.64 | 1.26 (0.72–2.22) | 0.41 | 1.40 (0.66–2.97) | 0.38 |
| Number of persons under observation in each group (GEMS/HEMS) | Number of events | Total PYR | GEMS IR (per 100 PYR) | HEMS IR (per 100 PYR) | Unadjusted IRR (95%CI) | P value | Adjusteda IRR (95%CI) | P value | Adjustedb IIRR (95%CI) | P value | Adjustedc IRR (95%CI) | P value | Adjustedd IRR (95%CI) | P value | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Long‐term mortality ratee (n = 1604) | 1220/384 | 194/66 | 3750/1198 | 5.17 (4.45–5.90) | 5.51 (4.18–6.84) | 0.91 (0.69–1.21) | 0.52 | 1.20 (0.90–1.61) | 0.21 | 0.71 (0.49–1.04) | 0.08 | 0.83 (0.61–1.13) | 0.24 | 0.74 (0.50–1.09) | 0.13 |
| Involuntary early retirement or death (n = 510) | 398/112 | 27/9 | 1170/321 | 2.31 (1.44–3.18) | 2.80 (0.97–4.63) | 0.83 (0.39–1.76) | 0.62 | 1.35 (0.60–3.13) | 0.46 | 0.74 (0.26–2.14) | 0.58 | 0.68 (0.29–1.56) | 0.36 | 1.22 (0.38–3.92) | 0.74 |
| Involuntary early retirement (n = 510) | 398/112 | 11/2 | 1170/321 | 0.94 (0.38–1.50) | 0.62 (0.00–1.50) | 1.53 (0.34–6.92) | 0.58 | 0.68 (0.15–3.23) | 0.63 | 0.84 (0.16–4.37) | 0.84 | 1.10 (0.22–5.42) | 0.90 | 1.21 (0.23–6.38) | 0.83 |
HEMS, helicopter emergency medical services; GEMS, ground emergency medical services; PCI, percutaneous coronary intervention; OR, odds ratio; CI, confidence interval; IR, incidence rate; IRR, incidence rate ratio; PYR, person‐years at risk.
Adjusted for gender, age, resuscitated cardiac arrest, inter‐hospital transfer, acute cardiac failure.
Adjusted for gender, age, resuscitated cardiac arrest, inter‐hospital transfer, acute cardiac failure, transport time (squared).
Adjusted for gender, age, resuscitated cardiac arrest, inter‐hospital transfer, acute cardiac failure, vasopressor.
Adjusted for gender, age, resuscitated cardiac arrest, inter‐hospital transfer, acute cardiac failure, daytime.
Mortality rate over the full follow‐up period.
Figure 2.
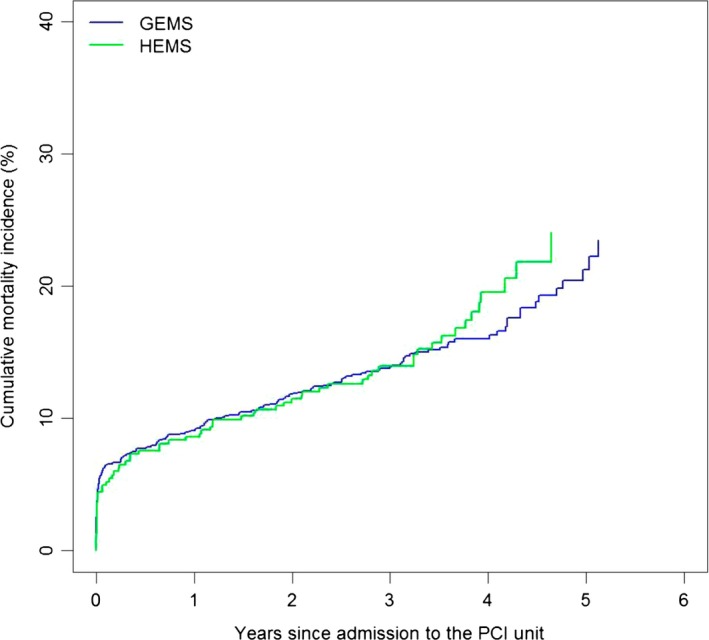
Cumulative mortality in patients admitted for primary percutaneous coronary intervention. HEMS, helicopter emergency medical services; GEMS, ground emergency medical services; PCI, percutaneous coronary intervention. [Colour figure can be viewed at http://wileyonlinelibrary.com]
Reduced work ability 2 years after admission was 25.9% (GEMS) vs. 23.0% (HEMS), adjusted OR = 0.91 (CI 0.52–1.60, P = 0.75), and the percentage of time on social transfer payments during the first 2 years after event was 21.2% (GEMS) vs. 22.1% (HEMS), adjusted OR = 1.10 (CI 0.64–1.90, P = 0.73; Table 2).
The IR of involuntary early retirement was 0.94 per 100 PYR vs. 0.62 per 100 PYR in GEMS and HEMS patients, respectively, adjusted IRR= 0.68 (CI 0.15–3.23, P = 0.63; Table 2).
We found no significant difference between groups in any analyses adjusted for transport distance, transport time, use of vasopressors, or time of day. However, we did find that significantly more HEMS‐patients had PCI within 150 min from estimated symptom onset in the group of patients with the longest transport distances; 37.2% vs. 24.1%, P = 0.03 (94–123 km) and 21.2% vs. 7.9%, P = 0.03 (> 123 km) (Fig. 3). For results adjusted for transport distance and results stratified by age, please refer to Tables S1 and S2.
Figure 3.
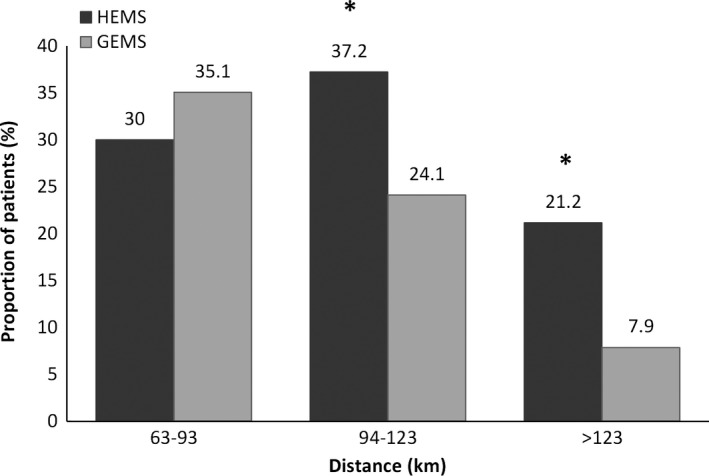
Proportion of directly referred patients having PCI within 150 min of estimated symptom onset. Distance: The transport distance on ground from the site of event (patient location) to the PCI centre. HEMS, helicopter emergency medical services; GEMS, ground emergency medical services. *P < 0.05.
Discussion
We found that transportation by helicopter did not seem to be associated with reduced mortality or with improved labour market affiliation for patients admitted for primary PCI with an expected ground transportation time of more than 25 min.
Among the main strengths of our study are the prospective study design, the well‐defined geographical catchment area, and the high completeness of the registries, providing high internal validity and reducing the risk of selection bias. No patients were lost to follow‐up in the primary outcome analysis, and our follow‐up period of up to 5.5 years allowed us to assess long‐term physical outcome and labour market status. Finally, because we included all patients and not only those who actually underwent acute PCI, our results are estimates of the effectiveness observed in the clinical situation where a decision should be made regarding optimal mode of transfer.
This study has some important limitations. First, the study took place in the eastern part of Denmark including the Region Zealand and some parts of the Capital Region of Denmark, with a population of approximately 1.1 million. Hence, data were collected in rural and more urban areas but clearly, the region is rather small and also densely populated compared with many other countries. In addition, the country is flat with very good opportunities for ground transport almost all the time. A major benefit of a helicopter is therefore difficult to detect as few patients came from more remote areas or from smaller islands.
The observational study design is prone to confounding by indication because we cannot know in detail how the dispatch centre decided to allocate either the HEMS or GEMS to the scene within the defined area. If the HEMS was allocated to those patients with the most severe disease, any gain from quicker transport might be offset by the worse clinical conditions. Indeed, more HEMS patients had myocardial infarction, thus indicating more severe disease in this group. On the other hand, fewer HEMS patients had acute cardiac failure, but because this variable was assessed at the time of arrival in the hospital, it might have been the result of the shorter transport time or treatment by the HEMS physician en route rather than a condition present at the time of transport mode allocation. Likewise, confounding by indication can be a concern in the dispatch of HEMS to the patients with the longest transport distances. However, we found no significant difference between groups in any analyses when also adjusting for transport distance. Moreover, adjusting for transport time (i.e. diagnostic ECG to arrival at the hospital), daytime vs. nighttime, or use of vasopressors did not change the odds ratios significantly.
A recent report found that inter‐hospital transfer was associated with prolonged reperfusion times regardless of transport mode14. In our study, a significantly higher proportion of GEMS patients were transferred from other hospitals instead of directly referred to the PCI centre. This difference may have led to the slightly longer transport time observed in the GEMS group. Furthermore, the variable “time from diagnostic ECG to arrival at the PCI centre” was missing in significantly more inter‐hospital transfer patients compared to directly referred patients, and because this variable was missing in one‐third of patients, this may have affected results in either direction. However, it did not translate into significantly higher mortality in this group, and there was also no difference in the analysis of field‐triaged patients only.
Transfer time improved for both HEMS and GEMS patients during the 2‐year span between the first HEMS study10 and the current study (HEMS: from 84 to 71 min; GEMS: from 104 to 78 min), leading to a reduction in median time difference between HEMS and GEMS from 20 to 7 min. This decrease may be the result of continuous organizational improvements (e.g., improved communication and better triage) over time, with the largest effect on the GEMS group. The dispatch procedure of the HEMS was optimized during the study period as ground ambulances were allowed to contact the HEMS directly without having to wait for the triaging cardiologist to accept to receive the patients. Moreover, because HEMS operated in increasingly more distant parts of the catchment area, this may have led to the observed improved transport time in the GEMS group.
Our sensitivity analysis on directly referred patients who had acute PCI revealed that a larger proportion of HEMS‐patients had the procedure performed within 150 min with increasing transport distances as compared to the GEMS patients. Thus, HEMS may be considered to facilitate equal and timely access to specialized treatment for people living in rural areas. However, it may be argued that a 7 min difference in transport time (diagnostic ECG to arrival at the hospital) comparing the entire study population (primary study population) may be too small a difference to translate into a clinically relevant improvement in favour of HEMS in terms of mortality and labour market affiliation.
Organizational changes markedly reducing the number of physician‐staffed mobile emergency care units in March 2011 may have increased mortality in the GEMS group. In contrast, survivorship bias inherent in our study design may have been introduced because patients who died before arrival at the PCI centre were not included in the PCI databases, thereby falsely lowering mortality in the GEMS group, which had the longest transport times. However, a large Danish study comparing coronary angioplasty with fibrinolytic therapy found that no patients died during transportation to the hospital15, hence we do not consider these two potential sources of bias to be strong enough to have an impact on the overall conclusions.
Around 60% of both HEMS and GEMS patients who were working full time before the cardiac event sustained full work ability 2 years after the event, suggesting that the majority of patients who survive the acute phase also seem to recover reasonably well independently of transport mode. This result is in line with another Scandinavian study on return to work after STEMI4. Still, the proportion of patients returning to work in our study was somewhat lower than in most studies. In a study by Laut et al., for example, up to 90% of patients had returned to work after 1 year16, and another study found that almost 80% of STEMI patients had resumed work after approximately 6 months17. These findings are consistent with those of a Swedish review in which it was estimated that as many as three of four patients return to work18.
Comparisons between geographical areas and countries like these should be interpreted with caution because differences in patient characteristics (age, line of work, etc.), follow‐up time, and legislative labour market policies affect outcome. We included patients up to 67 years of age in our labour market analyses; thus, our labour market population was substantially older and at a higher risk of leaving the labour market. Additionally, the fact that we assessed work ability after 2 years could be considered an advantage because patients had more time to recover but also could be seen as the opposite in that they had more time to retire. In a Danish cohort of 22,000 patients with acute coronary syndrome, only 45% of patients maintained an affiliation with the labour market2.
In conclusion, in our observational study of patients with suspected STEMI in eastern Denmark, no significant beneficial effect of helicopter transport could be detected on mortality, premature labour market exit, or work ability. Only a large study with random allocation to one system vs. another, will provide conclusive evidence regarding superiority of helicopter transport versus ground transport.
Supporting information
Table S1. Outcome stratified by age and adjusted for transport distance in patients admitted for primary percutaneous coronary intervention with 30‐day and 1‐year mortality, reduced work ability and time on social transfer payments 2 years after admission
Table S2. Outcome stratified by age and adjusted for transport distance in patients admitted for primary percutaneous coronary intervention with long‐term mortality and involuntary early retirement rate (combined endpoint) at follow‐up.
Acknowledgements
We thank The Danish Agency for Labour Market and Recruitment for providing data on labour market affiliation and social transfer payments, and The Emergency Medical Services Copenhagen for providing EMS data from The Capital Region of Denmark.
Funder KS, Rasmussen LS, Siersma V, Lohse N, Hesselfeldt R, Pedersen F, Hendriksen OM, Steinmetz J. Helicopter vs. ground transportation of patients bound for primary percutaneous coronary intervention. Acta Anaesthesiologica Scandinavica 2018.
Conflict of interest
None.
Funding
This work was supported by TrygFonden by an unrestricted grant [Grant number 7‐12‐0744].
References
- 1. Schmidt M, Jacobsen JB, Lash TL, Bøtker HE, Sørensen HT. 25 year trends in first time hospitalisation for acute myocardial infarction, subsequent short and long term mortality, and the prognostic impact of sex and comorbidity: a Danish nationwide cohort study. BMJ 2012; 344: e356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Osler M, Mårtensson S, Prescott E, Carlsen K. Impact of gender, co‐morbidity and social factors on labour market affiliation after first admission for acute coronary syndrome. A cohort study of Danish patients 2001‐2009. PLoS ONE 2014; 9: e86758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Mital A, Desai A, Mital A. Return to work after a coronary event. J Cardiopulm Rehabil 2004; 24: 365–73. [DOI] [PubMed] [Google Scholar]
- 4. Hämäläinen H, Mäki J, Virta L, Keskimäki I, Mähönen M, Moltchanov V, Salomaa V. Return to work after first myocardial infarction in 1991‐1996 in Finland. Eur J Public Health 2004; 14: 350–3. [DOI] [PubMed] [Google Scholar]
- 5. Isaaz K, Coudrot M, Sabry MH, Cerisier A, Lamaud M, Robin C, Richard L, Da Costa A, Kahmis H, Abd‐Alaziz A, Gerenton C. Return to work after acute ST‐segment elevation myocardial infarction in the modern era of reperfusion by direct percutaneous coronary intervention. Arch Cardiovasc Dis 2010; 103: 310–6. [DOI] [PubMed] [Google Scholar]
- 6. Terkelsen CJ, Sørensen JT, Maeng M, Jensen LO, Tilsted HH, Trautner S, Vach W, Johnsen SP, Thuesen L, Lassen JF. System delay and mortality among patients with STEMI treated with primary percutaneous coronary intervention. JAMA 2010; 304: 763. [DOI] [PubMed] [Google Scholar]
- 7. Diaz MA, Hendey GW, Bivins HG. When is the helicopter faster? A comparison of helicopter and ground ambulance transport times. J Trauma 2005; 58: 148–53. [DOI] [PubMed] [Google Scholar]
- 8. Knudsen L, Stengaard C, Hansen TM, Lassen JF, Terkelsen CJ. Earlier reperfusion in patients with ST‐elevation myocardial infarction by use of helicopter. Scand J Trauma Resusc Emerg Med 2012; 20: 70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Hata N, Kobayashi N, Imaizumi T, Yokoyama S, Shinada T, Tanabe J, Shiiba K, Suzuki K, Matsumoto H, Mashiko K. Use of an air ambulance system improves time to treatment of patients with acute myocardial infarction. Intern Med 2006; 45: 45–50. [DOI] [PubMed] [Google Scholar]
- 10. Hesselfeldt R, Pedersen F, Steinmetz J, Vestergaard L, Simonsen L, Jørgensen E, Clemmensen P, Rasmussen LS. Implementation of a physician‐staffed helicopter: impact on time to primary PCI. EuroIntervention 2013; 9: 477–83. [DOI] [PubMed] [Google Scholar]
- 11. Schoos MM, Pedersen F, Holmvang L, Engstrøm T, Saunamaki K, Helqvist S, Kastrup J, Mehran R, Dangas G, Jørgensen E, Kelbæk H, Clemmensen P. Optimal catchment area and primary PCI centre volume revisited: a single‐centre experience in transition from high‐volume centre to “mega centre” for patients with ST‐segment elevation myocardial infarction. EuroIntervention 2015; 11: 503–10. [DOI] [PubMed] [Google Scholar]
- 12. Lee KL, Woodlief LH, Topol EJ, Weaver WD, Betriu A, Col J, Simoons M, Aylward P, Van de Werf F, Califf RM. Predictors of 30‐day mortality in the era of reperfusion for acute myocardial infarction. Results from an international trial of 41,021 patients. GUSTO‐I Investigators.. Circulation 1995;91:1659–68. [DOI] [PubMed] [Google Scholar]
- 13. Rasmussen MB, Frost L, Stengaard C, Brorholt‐Petersen JU, Dodt KK, Søndergaard HM, Terkelsen CJ. Diagnostic performance and system delay using telemedicine for prehospital diagnosis in triaging and treatment of STEMI. Heart 2014; 100: 711–5. [DOI] [PubMed] [Google Scholar]
- 14. Nicholson BD, Dhindsa HS, Roe MT, Chen AY, Jollis JG, Kontos MC. Relationship of the distance between non‐PCI hospitals and primary PCI centers, mode of transport, and reperfusion time among ground and air interhospital transfers using NCDR's ACTION Registry‐GWTG: a report from the American Heart Association Mission: L. Circ Cardiovasc Interv 2014; 7: 797–805. [DOI] [PubMed] [Google Scholar]
- 15. Andersen HR, Nielsen TT, Rasmussen K, Thuesen L, Kelbaek H, Thayssen P, Abildgaard U, Pedersen F, Madsen JK, Grande P, Villadsen AB, Krusell LR, Haghfelt T, Lomholt P, Husted SE, Vigholt E, Kjaergard HK, Mortensen LS, for the DAMAMI‐2 investigators . A comparison of coronary angioplasty with fibrinolytic therapy in acute myocardial infarction. N Engl J Med 2003; 349: 733–42. [DOI] [PubMed] [Google Scholar]
- 16. Laut KG, Hjort J, Engstrøm T, Jensen LO, Tilsted Hansen H‐H, Jensen JS, Pedersen F, Jørgensen E, Holmvang L, Pedersen AB, Christensen EF, Lippert F, Lang‐Jensen T, Jans H, Hansen PA, Trautner S, Kristensen SD, Lassen JF, Lash TL, Clemmensen P, Terkelsen CJ. Impact of health care system delay in patients with ST‐elevation myocardial infarction on return to labor market and work retirement. Am J Cardiol 2014; 114: 1810–6. [DOI] [PubMed] [Google Scholar]
- 17. Abbas AE, Brodie B, Stone G, Cox D, Berman A, Brewington S, Dixon S, O′Neill WW, Grines CL. Frequency of returning to work one and six months following percutaneous coronary intervention for acute myocardial infarction. Am J Cardiol 2004; 94: 1403–5. [DOI] [PubMed] [Google Scholar]
- 18. Perk J, Alexanderson K. Swedish Council on Technology Assessment in Health Care (SBU). Chapter 8. Sick leave due to coronary artery disease or stroke.. Scand J Public Health Suppl 2004;63:181–206. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Outcome stratified by age and adjusted for transport distance in patients admitted for primary percutaneous coronary intervention with 30‐day and 1‐year mortality, reduced work ability and time on social transfer payments 2 years after admission
Table S2. Outcome stratified by age and adjusted for transport distance in patients admitted for primary percutaneous coronary intervention with long‐term mortality and involuntary early retirement rate (combined endpoint) at follow‐up.


