Abstract
Reducing avoidable emergency department (ED) visits is an important health system goal. This is a retrospective cohort study of the impact of a primary care intervention including an in-hospital, free, adult clinic for poor uninsured patients on ED visit rates and emergency severity at a nonprofit hospital. We studied adult ED visits during August 16, 2009-August 15, 2011 (preintervention) and August 16, 2011-August 15, 2014 (postintervention). We compared pre- versus post-mean annual visit rates and discharge emergency severity index (ESI; triage and resource use–based, calculated Agency for Healthcare Research and Quality categories) among high-users (≥3 ED visits in 12 months) and occasional users. Annual adult ED visit volumes were 16 372 preintervention (47.5% by high-users), versus 18 496 postintervention. High-users’ mean annual visit rates were 5.43 (top quartile) and 0.94 (bottom quartile) preintervention, versus 3.21 and 1.11, respectively, for returning high-users, postintervention (all P < .001). Postintervention, the visit rates of new high-users were lower (lowest and top quartile rates, 0.6 and 3.23) than preintervention high-users’ rates in the preintervention period. Visit rates of the top quartile of occasional users also declined. Subgroup analysis of medically uninsured high-users showed similar results. Upon classifying preintervention high-users by emergency severity, postintervention mean ESI increased 24.5% among the lowest ESI quartile, and decreased 12.2% among the top quartile. Pre- and post-intervention sample demographics and comorbidities were similar. The observed reductions in overall ED visit rates, particularly low-severity visits; highest reductions observed among high-users and the top quartile of occasional users; and the pattern of changes in emergency severity support a positive impact of the primary care intervention.
Keywords: emergency department, low-acuity emergency department visits, high-users of emergency departments, reducing avoidable ED visits, longitudinal study of emergency department patients, medically uninsured, retrospective study
Introduction
Emergency departments (EDs) are mission-critical for hospitals, and a key source of inpatient admissions, accounting for 50% of all inpatient admissions nationally in 2011. About 14.7% of ED visits end in inpatient admission.1-3 However, EDs also present financial and medical resource challenges, being mandated to provide care to all patients under the Emergency Medical Treatment and Active Labor Act. In 2011, uninsured patients accounted for 16% of 131 million ED visits, nationwide.3 ED crowding steadily increased since 1997 through 2007, partly due to ED closures exceeding new EDs opened by 23.7%, while ED visit volumes increased 30%.4,5 Since 2003, crowding has been aggravated by a new role served by EDs, as intermediate care zones (Observational Units) to preempt medically unnecessary inpatient admissions.2 These developments have led to the current ED capacity crisis, requiring evidence-based initiatives to reduce nonemergent ED visits.
The Society for Academic Emergency Medicine’s ED Crowding Task Force noted that ED crowding has resulted in several adverse impacts on patient outcomes related to patient safety, care timeliness, patient centeredness, efficiency, effectiveness, and equity.6-8 Suboptimal outcomes noted were delayed life-saving care (eg, pneumonia, myocardial infarction), increased mortality, and increased hospital-acquired infection rates.6,9 We used a before-after, observational cohort study design to examine the impact of free primary care access via an in-hospital primary care clinic on annual ED visit frequency and mean emergency severity of adult high-users.
Methods
Study Design
This is a retrospective, observational study of one nonprofit, religious missionary hospital’s attempt to reduce low-severity ED visits through a primary care intervention. The hospital is located in the inner-city neighborhood of Columbia, South Carolina, with pockets of minority- and poor-population concentration. In the hospital vicinity, there are 2 other functioning EDs—one about 3 miles away at a county nonprofit hospital that serves as a teaching hospital for the University of South Carolina School of Medicine, and another at a nonprofit secular hospital in an adjacent county about 8 miles away in a different direction. The teaching hospital ED is typically overcrowded, known for its long ED waiting time. We studied adult ED patients’ visit patterns at the study hospital before and after implementation of a primary care intervention at a nonprofit urban hospital in South Carolina. Preintervention period patients, classified into ED high-users and occasional users, were studied for their mean annual visit rates and emergency severity, before and after the clinic start date. We also compared preintervention high-users with new high-users of the postintervention period.
On August 16, 2011, the hospital established a primary care intervention that included an adult walk-in primary care clinic on-campus, which remains operational to date. The intervention consisted of 2 components, an adult primary care clinic on-campus, free of cost for uninsured patients under 200% of poverty. Another component of the intervention was to actively urge insured ED patients who were ED high-users or having a chronic disease/primary care–preventable condition, to either acquire a primary care physician (PCP) if they did not have one, or regularly visit their existing PCP. The hospital management sent the ED staff a directive to educate qualifying patients at discharge about the importance of primary care for their condition, and to (1) visit their own PCP regularly, (2) visit one of the hospital’s primary care practices (if insured but did not have a PCP), or (3) visit the clinic if uninsured. Uninsured patients below 200% of poverty income qualified for free clinic services. Patient education at discharge consisted of a one-time, short conversation by the ED staff nurse, reinforced, in some cases with a detailed work-up by the clinic social worker if she was available. ED staff compliance with the directive was not monitored, and the predischarge advice was subject to the prevailing urgencies in the ED environment.
The clinic is free for uninsured patients up to 200% of poverty income (self-reported by the patient with minimal supporting documentation), and it charges a modest, sliding-scale fee above this income. It is staffed by an internal medicine, osteopathy-trained physician; a nurse-practitioner; nurse; social worker (to assist chronically ill patients with sociomedical needs, and liaise with charity care sources for pharmacy, laboratory, and imaging); and medical assistants. Clinic hours are Monday to Wednesday 8 am to 4:30 pm, Thursday 10 am to 7 pm, and Friday 8 am to 12 pm, supplemented by phone access to on-call physicians (for registered clinic patients) during off-clinic hours and weekends. The clinic PCP and staff provide a primary care medical home environment, including education about primary care and self-management of chronic conditions. After-hours call service is shared by PCPs of the hospital’s 7 office-based practices including the clinic. The physician on call logs in remotely to access the electronic medical record (EMR) system, evaluates the patient’s medical history and resolves the call as appropriate (eg, verbal advice or reassurance, calling in repeat prescriptions, advice to attend the clinic the next day or the ED immediately).
Free clinical care is complemented by orchestrating patient access to a network of charity care options available in the region. The social worker provides navigation assistance for the paperwork needed to access prescriptions through Welvista, a statewide, charitable donation-supported, mail-order pharmacy that dispenses free medications donated by leading pharmaceutical manufacturers for uninsured patients. This source is reinforced by GoodRx, an Internet-based, discounted prescription drug program, and partnerships with low-cost generic drug offerings by large retailers (eg, Walmart). Together, these initiatives have resulted in almost full access for indigent patients to either free or negligible cost medications including most state-of-the-art prescription drugs. For essential laboratory services, the clinic has negotiated very low patient co-pays ($5 for basic lab work) with the leading corporate provider of lab services in the South Carolina Midlands. Specialized lab tests are provided as a charitable donation by the same firm on a case-by-case basis. Similar arrangements are in place for radiology services, supplemented by gratuitous service by the hospital-employed own radiologists/hematologists/other physicians and gratuitous use of the hospital’s diagnostic equipment when the out of pocket costs of external providers are beyond a patient’s financial reach. Limited specialist services are provided through a low-cost referral network maintained by a nearby rural county hospital, which includes this clinic in its network. These arrangements are supplemented by gratuitous consultations by the hospital’s specialists when needed. Most patients, however, are managed by the clinic internist and nurse. Specifically, ED high-users with high medical need are eligible for free hospital outpatient procedures including imaging, free of charge. In addition to active referral of qualifying ED patients to the clinic, potential future ED patients from the community are solicited from patients who register with the clinic. These patients are encouraged by the clinic staff to ask their medically needy, indigent friends and neighbors to use the clinic services. Word-of-mouth dissemination among social networks of clinic users was thought to be a cost-effective way to preempt avoidable ED use from the surrounding community. However, upon arrival at the clinic, the same income criteria were applied to walk-in patients to identify those who qualified for free services and sliding-scale fees.
Our primary measures of interest were overall hospital ED visit volumes contributed by high-users, patient-level annual visit rates, and mean emergency severity. These measures were compared pre- versus postintervention. High-users and occasional users of the preintervention period were tracked through the postintervention period. The secondary outcome of interest was postintervention convergence of mean annual visit rates and emergency severity between returning preintervention high-users and new (postintervention) high-users. We considered this an important outcome because the primary care intervention continues to date, and should preempt nonemergent ED visits by emerging new high-users from the community. The study was approved by the hospital Ethics Committee and the university’s Institutional Review Board.
Study Protocol
We extracted billing data on all ED visits of adults aged 18 years or older during 2 periods. The preintervention period was August 16, 2009-August 15, 2011, and the postintervention period, August 16, 2011-August 15, 2014. Data were organized to group visits by patient (based on name, social security number [SSN], date of birth [DOB]). To minimize exclusions due to missing/erroneous identifiers, we linked ED data to the ED patient registration and inpatient admission databases using the above as link variables, followed by manual review to rectify errors/missing data. This step reduced sample exclusions from 7.6% to 2.7% of visits. De-identified data were extracted into University of South Carolina computers for analysis. We excluded patients with a single ED visit during the 5-year study period if that visit ended in inpatient admission, implying a clearly appropriate use of the ED for a true, occasional emergency. The study intervention did not target such visits, nor was there a subsequent visit by these patients to study longitudinal ED use behavior. These visits constituted similar proportions of the total ED visit volume, pre- and postintervention, 19.7% versus 18.3%, respectively (Table 1), suggesting that the study results may be robust to their exclusion. We studied ED patients with all payer sources because significant proportions of insured patients in the preintervention period did not have a primary care provider (22% of Medicare patients, 60% of Medicaid, and 47% of privately insured patients), and because the intervention targeted the uninsured as well as insured patients without a PCP. All ED visits of study patients during the study period were included in the study.
Table 1.
Preintervention and Postintervention ED Patients: Demographic Characteristics, ED Use Frequency, and Medical Status.
| Preintervention (2 years) | Postintervention (3 years) | |
|---|---|---|
| Total ED visits | 40 763 | 67 954 |
| Visits by 1-time ED users ending in inpatient admissiona | 8020 | 12 465 |
| Study-eligible ED visitsa | 32 743 | 55 489 |
| Study-eligible ED patients | 20 153 | 30 754 (includes 3278 preperiod patients) |
| Gender | ||
| Female | 11 671 (57.9%) | 17 709 (57.6%) |
| Male | 8482 (42.1%) | 13 045 (42.4%) |
| Age (years) | ||
| 18-39 | 8278 (41.1%) | 12 413 (40.4%) |
| 40-64 | 7317 (36.3%) | 11 135 (36.2%) |
| ≥65 | 4558 (22.6%) | 7206 (23.4%) |
| Race | ||
| White | 8401 (41.7%) | 12 499 (40.6%) |
| Black | 11 398 (56.6%) | 17 591 (57.2%) |
| Other/unknown | 354 (1.8%) | 664 (2.2%) |
| Insurance (all visits insured vs otherwise) | ||
| Medicare, no visit uninsured | 4627 (23.0%) | 7084 (23.0%) |
| Medicaid, no visit uninsured | 671 (3.3%) | 801 (2.6%) |
| Private/other, no visit uninsured | 7968 (39.5%) | 12 119 (39.4%) |
| Uninsured at 1 or more visits | 6885 (34.1%) | 10 743 (34.9%) |
| Residence zip code | ||
| Hospital’s or adjacent zip codes | 8736 (43.4%) | 13 264 (43.1%) |
| Other zip codes | 11 407 (56.6%) | 17 481 (56.8%) |
| Comorbidity | ||
| Serious chronic comorbidity | 3833 (19.0%) | 5618 (18.3%) |
| Ambulatory care sensitive condition | 5473 (27.2%) | 8775 (28.5%) |
| None of the above | 10 747 (53.3%) | 16 284 (53.0%) |
| Missing | 100 (0.5%) | 77 (0.3%) |
| ESI score,* mean (SD) | 3.62 (0.94) | 3.73 (0.93) |
| Annual ED visit frequency,* mean (SD) | 1.91 (2.37) | 1.63 (1.58) |
| ED user type* | ||
| High-user patients (≥3 visits in 12 consecutive months) | 5124 (25.4%) | 6899 (22.4%) (includes 2398 preperiod high-users) |
| Occasional users | 15 029 (74.6%) | 23 855 (77.6%) (includes 880 preperiod patients) |
Note. ESI is a calculated discharge ESI in the billing database. The original AHRQ ESI score is the initial triaged status 1-5, higher score indicating lower severity. In this hospital, the ESI is revised to reflect true emergency and clinical severity by calculating it at discharge, based on final diagnosis, resources used to treat, and discharge disposition. The documented ESI is also reverse coded (relative to the AHRQ scale) to align with the billing convention, higher ESI = higher severity. ED = emergency department; ESI = emergency severity index; AHRQ = Agency for Healthcare Research and Quality.
These visits by 1-time users admitted as inpatients are excluded from the study, given that the intervention was designed to reduce avoidable ED visits that are remediable by primary care. These patients had no other ED visit in the study period, were not targeted by the intervention, and not amenable for study of subsequent behavior.
P < .01 for pre-post difference. Race and insurance were statistically significant, but not highlighted due to negligible magnitude of difference.
Due to distinct and independent patient registration systems at the clinic and hospital, there was no way to link clinic visits with specific ED patients except through matching name, SSN, and DOB. However, emergency service users are known to provide inaccurate SSN/DOB. One study reported a 66.6% discrepancy between SSNs documented by emergency medical service providers versus hospital-recorded SSNs among acute chest pain patients, compared with a discrepancy rate of 19.7% in the names and 18.3% in DOB for the same patients.10 Reluctance to provide accurate SSN is widely thought to be due to patient concerns about billing department follow-up for dues collection, especially among poor or uninsured patients. (Anecdotally, inaccurate SSN or refusal to provide an SSN was also a frequent experience at this clinic.) Triangulation of the clinic patient data with the hospital inpatient and ED billing databases to correct SSN/DOB errors (as done with ED billing data) could not be accomplished.
We defined high-users as patients with 3 or more ED visits in a continuous 12-month period. The state of South Carolina’s Department of Health and Human Services defines high-users as those making 3 or more visits in a year, asking hospitals to use this definition to monitor ED utilization in an effort to minimize the overall health system cost, part of which is reimbursed by the State through Disproportionate Share Hospital (DSH) payments. We found this definition to satisfy the recommendation of the research literature that high-users being targeted for interventions should account for at least 25% of total visits to produce a meaningful impact on ED volumes.11 In the preintervention period, our high-user definition attributed 47.5% of total ED visits to high-users. Other studies have also used this definition.12 We identified preintervention high-users as follows. For patients with an ED visit during the preintervention period, their visits during the year before the calendar start date of the preintervention period (August 16, 2008-August 15, 2009) and year after (August 16, 2011-August 15, 2012) were drawn into a temporary analytic dataset to flag high-users who would qualify as high-users based on their visits in the months adjacent to the calendar duration of the preintervention period. This preempts misclassification bias due to the calendar limits of the study period. Similarly, to flag new high-users of the postintervention period, we used visits during August 16, 2010-August 15, 2011 (1 year prior to the calendar postintervention period). However, after identifying high-users of the 2 periods, visits were used for analysis only if they occurred in the calendar period of study. Visits that occurred before the study period were excluded from analysis. Study period visits were assigned to the pre- or post-period as applicable. Patients other than high-users were defined as “occasional users.”
We chose to study 2 preintervention years to avoid biased results from a single, potentially outlier year (eg, preintervention year). We limited it to 2 years to minimize cohort maturation bias due to disease evolution among comorbid patients. We selected 3 years for the postintervention period to allow adequate time for the 2-year cohort of preintervention patients to visit the ED postintervention, potentially receive a primary care referral, and then manifest changes in their ED use behavior. Despite imbalanced pre- and postintervention periods, we ensure comparable measures by using the average annual patient visit rate in each period, and averaging the emergency severity across a patient’s visits in each period.
Measures
At the hospital level, we compared preintervention versus postintervention ED patient volumes, total, high-users, and occasional users. We define emergency severity as the patient’s discharge emergency severity index (ESI), a calculated measure that adjusts the nurse-triaged AHRQ ESI score with the resources used to treat (total charges), and their discharge disposition. The calculation is based on an internal hospital algorithm and uses the AHRQ categories of severity but reverse coded, so that increasing score represents higher severity to align with the hospital billing convention (5 = life-threatening, 4 = emergent, 3 = urgent, 2 = nonurgent, 1 = fast track).13 A calculated ESI approach (in contrast to initial nurse-triaged score) is consistent with the prevailing consensus that the initial triaged ESI has poor replicability and predictive validity for outcomes, largely because subsequent diagnostic assessments and treatments are highly variable relative to the initial, symptom-based triage.14
Patient-level mean annual visit rates and mean ESI scores were aggregated across the total ED population in each period, grouping patients as high-users and occasional users. We hypothesized that longitudinally tracked high-users’ annual visit rates would decline following the intervention, and mean ESI would increase due to fewer low-severity visits. For preintervention high-users, we compared these measures pre- versus postintervention, both overall, and classified into quartiles based on mean annual visit frequency. Preintervention high-users were also compared with preintervention occasional users. Returning high-users were compared with new high-users of the postintervention period. Finally, we classified preintervention high-users into severity quartiles based on their preintervention average severity, and compared each quartile’s pre- versus post-mean severity.
We assigned serious comorbidity to the patients if, at any preintervention visit, their primary or secondary diagnoses (up to 3) showed one of 10 serious conditions (HIV and the 9 Dartmouth conditions—serious malignant or metastatic cancer, chronic pulmonary disease, coronary artery disease, severe congestive heart failure, peripheral vascular disease, severe chronic liver disease, diabetes with end-organ damage, renal failure, dementia). The Dartmouth comorbidities are validated predictors of in-hospital mortality and inpatient care intensity.15 We also identified the presence of ambulatory care sensitive conditions (ACSCs; 24 conditions, see supplementary appendix). Because these are chronic conditions, a given patient was assigned the comorbidity/ACSC to all their visits. Analyses were performed using SAS version 9.4.
Results
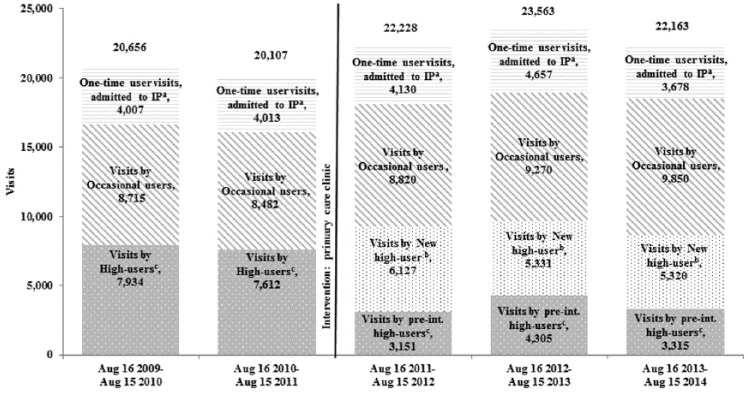
Of total 108 717 adult ED visits, 2898 (2.7%) were excluded due to missing patient identifying information. Figure 1 shows the distribution of 105 819 visits by year and user type. Overall ED volumes increased over the study period. After excluding 1-time ED patients whose visit ended in inpatient admission, the mean annual visit volume was 16 372 preintervention, and 18 496 postintervention. Annual visit volumes contributed by preintervention high-users declined in the postintervention period, by 53.8% (P < .001).
Figure 1.
Pre- and postintervention ED visit volumes, total visits, and distributed by user type.
Note. ED = emergency department; IP = inpatient; Int = intervention.
aOne-time use, IP admitted: These are patients who visited the ED only once during the entire 5-year period and were admitted as inpatients. Because they did not visit any other time, they are excluded from the subsequent analysis which focused on tracking patient use behavior over time.
bNew high-users are those who were not high-users in the preintervention period. They consist of occasional users of the preintervention period and new patients from the community.
Table 1 presents the distribution of preintervention and postintervention ED patients (the latter including returning preintervention patients). We present their demographics, average annual visit frequency, insurance status (uninsured at any visit in the study period/insured at all visits), residential proximity (based on zip code at first visit), serious comorbidity, ACSC, mean ESI, and user type (high-user/occasional user). Of preintervention patients, 77.4% were of working age, 56.6% Black, 34.1% were uninsured at 1 or more ED visits, and 25.4% were high-users who accounted for 47.5% of all preintervention visits. Prevalence of serious comorbidity was 19% and ACSC, 27.2%, total with comorbidity, 46.2%. About 43.4% lived in the hospital zip code or adjacent zip codes. Preintervention, the mean annual visit rate per patient was 1.91 (±2.37), and mean ESI score, 3.62 (±0.94). By comparison, fewer postintervention patients were high-users (22.4%), the mean annual visit rate was lower, and ESI score was higher (all P < .001). Serious comorbidity and ACSC rates were similar in the pre- and postintervention periods.
Table 2 presents the pre- versus postintervention, mean visit rates and mean ESI scores of preintervention high-users (Section A) and occasional users (Section B). Each group was classified into quartiles based on their preintervention mean annual visit rate. A large number of high-users had a visit rate equal to the quartile cutoff frequencies; we assigned all these patients to the quartile below the cutoff point (consistent with the definition of percentile values). The lowest and top quartile values, preintervention, were 0.94 and 5.43, respectively (highest value for an individual patient was 27.5). About 41.7% did not visit the ED in the postintervention period and are excluded from the denominators for postintervention visit rates and severity calculations. Across returning high-users, their mean annual visit rate was 7.3% lower than the mean visit rate of all high-users before the intervention (1.51 reduced to 1.40). Significant visit rate reductions postintervention were noted in every quartile (mean visit rates were 1.11-1.72; and the highest individual annual visit rate fell to 14.0). We noted a statistically significant postintervention increase in the overall mean ESI score (3.51-3.61), with significant increases noted within each of the lower 3 quartiles of high-users (P < .001, P = .009, P = .013, respectively).
Table 2.
Preintervention Patients Classified Into Quartiles by Preintervention Visit Frequency: Pre- Versus Postintervention Visit Characteristics.
| Preintervention period (August 16, 2009-August 15, 2011) |
Postintervention period (August 16, 2011-August 15, 2014) |
|||||||
|---|---|---|---|---|---|---|---|---|
| No. of preintervention patients | Total ED visits (2 years) | Mean annual visits per patienta (range) | Mean ESI, preintervention (range/SD) | Returning preintervention patients | Total visits (3 years) | Mean annual visits per patienta (range) | Mean ESI, postintervention (SD) (Range 1-5 for all groups) |
|
| Section A: Preintervention high-users | ||||||||
| Total* | 5124 | 15 546 | 1.51* (0.5-27.5) | 3.51* (1.0-5.0) | 2985 | 12 505 | 1.40* (0.3-16.0) | 3.61* (0.81) |
| Quartile 1 | 3757 | 7088 | 0.94* (0.5-1.5) | 3.53* (1.0-5.0) | 2063 | 6870 | 1.11* (0.3-10.0) | 3.62* (0.83) |
| Quartile 2 | 571 | 2284 | 2.00* (2.0-2.0) | 3.49* (1.7-5.0) | 354 | 1535 | 1.45* (0.3-10.7) | 3.61* (0.75) |
| Quartile 3 | 448 | 2398 | 2.68* (2.5-3.0) | 3.43* (1.2-5.0) | 305 | 1570 | 1.72* (0.3-14.0) | 3.56* (0.74) |
| Quartile 4 | 348 | 3776 | 5.43* (3.5-27.5) | 3.47 (2.0-4.9) | 263 | 2530 | 3.21* (0.3-16.0) | 3.53* (0.74) |
| Section B: Preintervention occasional usersb | ||||||||
| Total | 15 029 | 17 197 | 0.57* (0.5-1.5) | 3.66* (0.97) | 3367 | 6283 | 0.62* (0.3-10.0) | 3.72* (0.92) |
| Quartiles 1, 2, 3 | 12 933 | 12 933 | 0.50* (0.5-0.5) | 3.69* (1.00) | 2701 | 4939 | 0.61* (0.3-10.0) | 3.73* (0.93) |
| Quartile 4 | 2096 | 4264 | 1.02* (1.0-1.5) | 3.54* (0.82) | 666 | 1344 | 0.67* (0.3-5.0) | 3.66* (0.92) |
Note. Quartile cut-points are 1.5, 2.0, 3.0, and 27.5 visits annually for high-users. ESI = emergency severity index—adapted AHRQ ESI and reverse coded; higher ESI = higher severity; ED = emergency department; AHRQ = Agency for Healthcare Research and Quality.
Averaged per year for comparability of preintervention period (2 years) with postintervention period (3 years). Lowest quartile has a mean annual visit frequency of 0.94 due to visits outside the calendar years of the study period that were used to flag high-user status, ≥3 visits during any 12 consecutive months. Visits outside calendar period of study were excluded, causing the minimum annual visit rate of 0.5 per year for high-user patients. Cutoff point between Quartile 4 and the lower is 0.5 for occasional users, respectively. Quartiles 1 to 3 are pooled due to 12 933 patients having only 1 visit in the preintervention period, that is, annual visit rate = 0.5.
ESI range for occasional users is 1.0 to 5.0 for both groups.
P < .01 for pre-post difference.
Among occasional ED users, the annual visit rate of the top quartile nearly halved, from a preintervention rate of 1.02 to 0.67 postintervention, P < .001 (Table 2, Section B). Their mean ESI score increased from 3.54 to 3.66 (P < .001). The lower 3 quartiles of occasional users had to be pooled (all these patients had only 1 visit in the preintervention period). A smaller change in mean severity is observed in this group (3.69 and 3.73, respectively, P = .039) along with a slight increase in mean visit rate (0.5 vs 0.6). Overall, the top quartile and the lower quartiles of occasional users converged to one common profile in the postintervention period (0.67 vs 0.6).
Table 3 presents the postintervention period comparison of new high-users with returning high-users. For new high-users, the lowest quartile and top quartile values were 0.6 and 3.23 visits, respectively. These values are higher than the corresponding values for returning high-users (1.11 and 3.21, respectively), but lower than those of preintervention high-users in the preintervention period (0.94 and 5.43, respectively). In the postintervention period, visit rates of new high-users and returning high-users show similarity among the lower quartiles (0.60 for quartiles 1 and 2 combined vs 1.11 and 1.45 for the first and second quartiles of returning high-users). The latter’s corresponding rates in the preintervention period were 0.94 and 2.0, respectively. New high-users’ mean ESI scores in the top quartile and lowest quartile are 3.62 and 3.68, compared with 3.53 and 3.62, respectively, for returning high-users. Upon reviewing the preintervention period ESI of high-users (Table 2) against the postintervention mean ESI of returning high-users and new high-users (Table 3), all quartiles show higher ESI levels in the postintervention period.
Table 3.
Visit Frequency and Emergency Severity in the Postintervention Period: New High-Users Versus Returning Preintervention High-Users.
| New postintervention high-users |
Visits by returning preintervention high-users |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| Quartile based on visit frequencya | No. of patients | Total visits (3 years) | Mean annual visits per patienta (range) | Mean of patients’ ESI (range) | Preintervention quartile groupa | No. of patients | Total ED visits (3 years) | Mean annual visits per patient (range) | Mean of patients’ ESI (SD) (Range 1.0-5.0 all groups) |
| Total | 5011 | 14 968 | 1.00* (0.3-13.0) | 3.65* (1.0-5.0) | Total | 2985 | 12 505 | 1.40* (0.3-16.0) | 3.61* (0.81) |
| Quartiles 1 and 2 | 3454 | 6258 | 0.60* (0.3-1.0) | 3.68* (1.0-5.0) | Quartile 1 | 2063 | 6870 | 1.11* (0.3-10.0) | 3.62* (0.83) |
| — | — | — | — | — | Quartile 2 | 354 | 1535 | 1.45* (0.3-10.7) | 3.61 (0.75) |
| Quartile 3 | 1238 | 5621 | 1.51* (1.3-2.0) | 3.58 (1.0-5.0) | Quartile 3 | 305 | 1570 | 1.72* (0.3-14.0) | 3.56 (0.74) |
| Quartile 4 | 319 | 3089 | 3.23 (2.3,13.0) | 3.62 (2.1-5.0) | Quartile 4 | 263 | 2530 | 3.21 (0.3-16.0) | 3.53 (0.74) |
Note. Despite statistically significant difference between quartile mean values between the 2 patient groups, the numeric values show convergence of visit rates and severity of new high-users and preintervention high-users in the postintervention period. ESI = emergency severity index—adapted AHRQ ESI and reverse coded; higher ESI = higher severity; ED = emergency department; AHRQ = Agency for Healthcare Research and Quality.
Quartiles’ cut-points for mean annual visits: new high-users: Q1 and Q2 (median) 1.0; Q3: 2.0, Q4:13.0. Q1 and Q2 are pooled because 50% of the sample had a mean annual visit rate of 1.0.
P < .05 for new high-users versus preintervention high-users.
A subgroup analysis was performed of preintervention high-users of working age 18 to 64 years. They were classified by insurance status (insured, including private and government sources) and uninsured, and the results are shown in Supplemental Table 2 in the supplementary materials. Similar to the main analysis, uninsured high-users tracked into the postintervention period also showed substantial and statistically significant reductions in annual visit rates, concurrent with an increase in emergency severity. Insured working-age high-users showed an increase in emergency severity but no change in the visit rate. Postintervention, a convergence of mean visit rates of uninsured and insured high-user groups is also observed.
We also studied preintervention high-users classified into quartiles by their mean ESI score in the preintervention period (table presented in supplemental materials). The lowest severity quartile showed the highest postintervention increase in mean ESI, from 2.65 to 3.30, a 24.5% increase. The mean ESI decreased among the upper quartiles of severity. Mean ESI of the top quartile (4.66, which is close to the “life-threatening” score, 5.0) declined to 4.09. The mean ESI of the next quartile (3.93, almost at the “emergent” level of 4.0) also declined to 3.76. It is notable that the above changes occurred despite similar rates of serious comorbidity and ACSCs among the preintervention and postintervention ED patients (Table 1).
Discussion
Following the primary care access intervention, we observed a large reduction in ED visit rates of both high-users and higher end occasional users. The reductions were sustained even when the analysis was restricted to uninsured working-age patients, showing substantial changes in visit rates and severity among uninsured high-users tracked through the postintervention period, compared with the modest or no change observed among tracked insured high-users. The visit volume reductions of the uninsured occurred concurrent with increasing emergency severity of visits. The study intervention consisted of 2 components. First, an active offer of free primary care access, on-campus, to poor uninsured ED patients, prioritizing ED high-users and chronic disease patients, supplemented by 24/7 phone access to primary care doctors, was provided. For insured patients who were high-users or chronic disease patients, an educational conversation on the importance of regularly using a primary care doctor was provided at a “teachable moment,” when the patient has just survived a scary, possibly life-threatening episode. Given the broad scope of the intervention, this evaluation study included ED patients with all types of payers: Medicare, Medicaid, private insurance, and the uninsured. Medicare beneficiaries are documented to have a usual source of care (>95%).16 However, 26% to 35% of beneficiaries use a specialist as their usual source of care, and they are more likely to be the highest-cost beneficiaries, compared with PCP users.16 In this study, 22% of Medicare ED patients, 60% of Medicaid, and 47% of privately insured patients did not have a primary care provider as reported at their first ED visit.
While 41.7% of high-users did not return to the ED postintervention, among returning high-users, there were dramatic reductions in the annual visit frequency within every quartile (by 28%-68%). The 3-year duration of the postintervention period provided adequate time for the primary care intervention to be availed as and when a patient returned to the ED, and for patients to manifest a change in their ED use patterns. This may mitigate the likelihood of spurious findings due to chance. A definitive, intervention impact is supported by the concurrent increase in the discharge ESI, averaged over this large high-user cohort. Furthermore, the differentiation of severity changes between patient quartiles classified on severity is notable—a dramatic increase in ESI among the lowest severity patients, and clinically salient severity reductions among the emergent and life-threatening severity quartiles to lower severity levels (see supplemental materials). (The opposite directions of effect among the low- and high-severity quartiles explain the modest (0.10) increase in average severity across all high-users, shown in Table 2.) A note of caution, however, is appropriate. The ESI scale as computed by this hospital is not empirically validated for predictive accuracy. The original AHRQ ESI scale was designed to capture initial, nurse-triaged severity of a patient before diagnostic investigations are done to finalize the diagnoses and treatment needs, and is therefore, more a measure of symptomatic emergent severity rather than true disease state emergent severity. At this hospital, the concern regarding the severity validity of the original AHRQ ESI is mitigated because the ESI is calculated with an algorithm that uses initial triage, resources used to treat patient outcome. Intuitively, this method is superior to the AHRQ ESI scale, because it captures the true emergent status of the patient by differentiating symptom-driven emergencies versus life-threatening conditions. However, the hospital’s algorithm is proprietary (used across hospitals owned by the parent missionary group), not validated by empirical research.
A true primary care impact would be best verified by identifying ED patients who visited the free clinic and those who acquired an office-based PCP to study their ED use changes. The former proved logistically impossible due to unlinkable clinic IT and hospital EMR systems. No data are available to quantify the latter. The free clinic registered 5701 visits over 3 years, made by 741 patients, mostly uninsured patients.
The decline in preintervention high-users’ visit rates could be argued as a secular, natural regression from sporadic high ED use caused by transient medical exacerbations. With stabilization of their medical condition, these patients should regress to the mean pattern of the local population. Two findings mitigate this explanation. First, if the historic high-users’ visit reductions were due to this effect, new high-users should repeat the historic visit rates and severity levels of the preintervention period, which is not the case. On the contrary, their visit rates are much lower than the historic rates of preintervention high-users in the preintervention period. Notably in the postintervention period, new high-users and returning high-users show convergence of both visit rates and ESI levels among the lower quartiles of visit frequency. Serious comorbidity and ACSC prevalence rates were similar among the pre- and postintervention groups of ED patients (Table 1). Collectively, the findings suggest that more patients may have used primary care, resulting in less need for ED visits, and when they used the ED, it was more appropriate, for emergent needs. Also supporting an intervention effect is the similar direction of change, although of lower magnitude among higher-end occasional users. The top quartile of occasional users (containing a large number of patients who fell short of the 3-visits-in-12-months criterion) showed large postintervention changes (a 75% decrease in visit frequency), and an increase in mean ESI score to similar levels as those of the lower quartiles of returning high-users.
The pattern of visit rate declines among high-users is reinforced by the observed longitudinal changes in visit ESI among patients of different severity levels. When preintervention high-users were classified on emergency severity, the lowest severity quartile, accounting for the largest fraction of preintervention high-users (39.1%), showed a 25% ESI increase in their postintervention visits. Concurrently, the higher severity patients (with emergent and life-threatening range of ESI) showed ESI reductions toward less life-threatening levels. The combination of visit rates and ESI changes in these longitudinally tracked patients supports a primary care impact. Potentially, the observed increase in ESI could be argued as a manifestation of disease evolution of chronically comorbid patients. If such was the case, one would expect a concurrent increase in the visit rate. Advancing chronic disease should cause more ED visits (for various complications) and more severe visits. On the contrary, we find a much-reduced visit rate by the same high-users, postintervention, concurrent with increased severity among the lower ESI quartiles, and reduced severity among the highest ESI quartiles.
The postintervention increase of emergency severity among low-severity patients and a decrease among high-severity patients validate the normative expectations from this primary care intervention. Primary care is the first level of contact with the health care system. The study hospital’s intervention was carefully crafted and executed to ensure a primary care medical home environment, continuity of providers (who were full-time and salaried), collaborative chronic disease management activities, care coordination, almost free access to accessory care needs such as specialist care, diagnostic and imaging services, and prescription drugs. This approach would be expected to help patients to mitigate or eliminate acute exacerbations through proactive chronic disease management, and may have helped patients to substitute ED use with primary care office visits for some low-severity episodes. Among patients with emergent and life-threatening severity preintervention, primary care may have reduced the likelihood and severity of complications of their chronic disease, or provided a medical home for early treatment of exacerbations before the condition became emergent. The collective internal consistency of findings across multiple subgroups of this ED population mitigates some of the methodological limitations, which, however, cannot be ruled out as potential explanatory factors. One methodological limitation of the study is the group-level analysis. However, individual, subject-based analysis requires accounting for medical diagnoses, which in turn requires a consolidation schema to group disparate diagnoses into a usable medical status variable for statistical analysis. Such an effort is beyond the scope of this study. Second, we are unable to identify ED patients who used the clinic. Up to 67% of SSNs in emergency service system databases may be inaccurate.10 Anecdotal experiences at the study clinic confirm this issue.
Another major limitation is the absence of data on patient visits to other EDs in the area. The presence of 2 hospitals in the region (3 and 8 miles away, respectively) may give pause about offsetting visits to those hospital EDs that may partly account for the volume reduction at this ED. Both hospitals pose significant logistic deterrents to neighborhood patients. The teaching hospital ED had a community-wide reputation for very long waiting times for all but life-threatening and emergent patients. The second ED, located in an adjacent county, is quite distant from the study hospital’s patient source neighborhoods, a key factor in a city with limited public transportation, with no buses operating in the direction of the second hospital. Furthermore, the study hospital and its ED are focused on specialized services such as maternity and pediatrics, services that are not targeted by the study hospital. Countering the expected natural response of high-users to disperse their ED visits across hospitals, is the religious mission of the study hospital, which translated into management’s expectation that hospital staff adhere to the key creed, including an accepting attitude toward the indigent. The hospital’s hinterland is a low-income, minority-dominated neighborhood with poor transportation options. Therefore, it is likely that this study limitation is mitigated by the above factors.
The study overcomes several limitations of previous studies that showed disparate findings. Some cross-sectional studies and patient surveys showed that primary care access was associated with fewer ED visits, while others show the opposite. Supportive evidence largely consisted of cross-sectional, population-based survey data, comparing self-reported ED use by respondents with and without primary care access, or comparing the self-reported primary care access of persons reporting ED use versus nonuse.17-22 Other cross-sectional studies report higher ED use by persons having a primary care provider.23-26 Notably, these studies do not account for medically substantiated emergency severity. In the current study, our measure of discharge ESI (based on staff-triaged severity, resources used to treat, and final discharge disposition) represents medically robust severity and urgency representation, compared with patient-perceived need for ED care that is captured in cross-sectional surveys.
One cross-sectional study examined the likelihood of low-emergency visits to the ED by patients enrolled at one of 4 free-standing free clinics versus unenrolled ED patients at 4 hospitals in Virginia. The study reported reduced likelihood of a low-emergency visit by free clinic users, but no difference in the likelihood of an avoidable, primary care–amenable visit.20 Acknowledged study limitations were the cross-sectional nature of the study, lack of information on the composition of each free clinic’s services, nature and continuity of medical providers, processes (if any) for care continuity, care coordination and chronic disease self-management (the essential elements of primary care), and the presence of a primary care medical home environment. As acknowledged in the paper, most free clinics depend on an uncertain roster of volunteer physicians based on availability of spare time. As such, it is difficult to expect that avoidable ED visits (that are primary care–amenable and preventable) would be reduced by the typical free clinic. Possibly due to this issue, the study showed no association of free clinic enrollment with avoidable visits. Their study also did not examine associations with ED visit volumes of the study patients. ED visit volumes are a critical issue for hospitals. As such, the significance of findings for policy-making remains limited.
Our study addresses several limitations of the above study, notably, (1) offering a longitudinal study of the ED population; (2) tracking individual patients’ ED use patterns before and after implementation of the intervention to examine utilization changes by user type; (3) studying a hospital-funded, on-campus primary care clinic which ensured prompt patient acceptance into primary care; (4) a clinic with a systematic approach to care continuity and care coordination implemented by salaried medical and ancillary providers offering dependable provider availability; and (5) a systematized approach to facilitate real access to ancillary medical services (pharmaceuticals, laboratory, and imaging services) that are critical to make a primary care intervention meaningful for the goal of reducing avoidable medical care.
Longitudinal cohort studies are critical to study ED use changes within nested subgroups. Crude, before-after volume comparisons are deceptive, due to the complex and dynamic composition of the ED population. High-users of a given year may remain high-users, or become low-users/nonusers due to complex reasons: health status changes (eg, chronic disease deterioration, resolution of acute exacerbations, new complications, death), insurance changes, acquiring a PCP, and patient preferences (eg, convenience of a snap visit to the ED vs scheduling an office visit). These dynamics of returning high-users are constantly being churned by new high-users from the community who will cycle through these processes. Secondary data sources (eg, the Healthcare Cost and Utilization Project (HCUP) nation-wide hospital discharge database) cannot accommodate patient tracking beyond a calendar year. Moreover, missing or misreported SSN and DOB (reportedly more likely by high-users) result in significant patient exclusions in HCUP data–driven studies. Triangulation of claims data with internal hospital databases is critical; our sample exclusions were reduced from 7.6% to 2.7% by such triangulation.
Few longitudinal interventional studies are documented. A 42-hospital collaborative used process reengineering to reduce ED waiting times, but it did not target the medical care content.27 In another study, ED staff referred 965 consenting, nonemergent ED patients without a personal physician to the in-hospital primary care clinic. Of them, 50% visited the clinic versus 39% of control patients, with no subsequent difference in ED use.28 Indigent ED patients who were generically referred to local safety-net clinics showed no change in their ED visit rates.29 Reduced ED use was reported when uninsured patients were provided an insurance plan requiring adherence to one PCP.30 Patients of primary care practices transformed into primary care medical homes used the ED less than comparison practice patients.31 Overall, the evidence supports that a definitive assumption of primary care responsibility by an entity offering dependable clinic hours, and implementing key primary care principles may be the key to success.
In addition to the limitations noted earlier, other limitations include retrospective, single-hospital study, lack of data on after-hours teleconsultations, and not accounting for 2 issues: the 2008-2009 economic recession and disease maturation. Bias due to the economic recession is partly mitigated by similar time trends of the study hospital’s ED volumes to those of South Carolina and the neighboring states.32,33 One unmeasured source of bias remains: policy changes at the national, state, or local level.
Disease maturation and new comorbidities that arose postintervention may underestimate the primary care impact, because they would necessitate more, not less ED visits. We observe a significant decline in visit rates. Our study, therefore, potentially underestimates the visit rate reduction attributable to the primary care intervention. Generalizability to other hospitals may be a concern, although mitigated by the study hospital’s similarity to the typical, urban hospital on many indicators: ED patient-to-visit ratio of 1:1.6 (1:1.9 among nonteaching hospitals, and 1:1.6 at a teaching hospital20,34); 19% of adult ED visits ending in inpatient admission (14.7% nationally for adult and pediatric visits combined3); 34% uninsured (31.7% in another study35,36). Overall, the study findings support proactive, well-organized primary care interventions as a strategy to reduce avoidable ED visits.
Supplemental Material
Supplemental material, SupplTableAndAppendixRev3Jan25-2018 for Reducing High-Users’ Visits to the Emergency Department by a Primary Care Intervention for the Uninsured: A Retrospective Study by Meng-Han Tsai, Sudha Xirasagar, Scott Carroll, Charles S. Bryan, Pamela J. Gallagher, Kim Davis, and Edward C. Jauch in INQUIRY: The Journal of Health Care Organization, Provision, and Financing
Acknowledgments
The authors gratefully acknowledge Sisters of Charity Providence Hospitals, Columbia, South Carolina (now known as Providence Health) for financial support to carry out the study and providing the data. They are grateful to Lib Cumbee, Elizabeth Sears, Kenneth Beasley, Lindsey Kilgo, and Carmen Wilson of Providence Hospitals for data extraction assistance and informational input. They are particularly grateful to Scott Campbell, Chief Executive Officer of Providence Health, for his support and insightful comments to improve the study.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The study was partially supported by the Sisters of Charity Providence Hospitals, Columbia, South Carolina.
References
- 1. Greenwald PW, Estevez RM, Clark S, Stern ME, Rosen T, Flomenbaum N. The ED as the primary source of hospital admission for older (but not younger) adults. Am J Emerg Med. 2016;34:943-947. [DOI] [PubMed] [Google Scholar]
- 2. Morganti-Gonzalez K, Baufman S, Blanchard J, et al. The Evolving Role of Emergency Departments in the United States. RR 280-ACEP. RAND. http://www.rand.org/pubs/research_reports/RR280.html. Published 2013. Accessed April 12, 2016. [PMC free article] [PubMed]
- 3. Weiss AJ, Wier LM, Stocks C, et al. Overview of Emergency Department Visits in the United States, 2011. HCUP Statistical Brief #174. Rockville, MD: Agency for Healthcare Research and Quality; 2014. [PubMed] [Google Scholar]
- 4. Hsia RY, Kellermann AL, Shen YC. Factors associated with closures of emergency departments in the United States. JAMA. 2011;305:1978-1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Tang N, Stein J, Hsia RY, Maselli JH, Gonzales R. Trends and characteristics of US emergency department visits, 1997-2007. JAMA. 2010;304:664-670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Bernstein SL, Aronsky D, Duseja R, et al. The effect of emergency department crowding on clinically oriented outcomes. Acad Emerg Med. 2009;16:1-10. [DOI] [PubMed] [Google Scholar]
- 7. Pines JM, Hollander JE. Emergency department crowding is associated with poor care for patients with severe pain. Ann Emerg Med. 2008;51:1-5. [DOI] [PubMed] [Google Scholar]
- 8. Schull MJ, Vermeulen M, Slaughter G, Morrison L, Daly P. Emergency department crowding and thrombolysis delays in acute myocardial infarction. Ann Emerg Med. 2004;44:577-585. [DOI] [PubMed] [Google Scholar]
- 9. Ward MJ, Baker O, Schuur JD. Association of emergency department length of stay and crowding for patients with ST-elevation myocardial infarction. West J Emerg Med. 2015;16:1067-1072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Brice JH, Friend KD, Delbridge TR. Accuracy of EMS-recorded patient demographic data. Prehosp Emerg Care. 2008;12:187-191. [DOI] [PubMed] [Google Scholar]
- 11. Zuckerman S, Shen YC. Characteristics of occasional and frequent emergency department users: do insurance coverage and access to care matter? Med Care. 2004;42:176-182. [DOI] [PubMed] [Google Scholar]
- 12. Ronksley PE, Liu EY, McKay JA, et al. Variations in resource intensity and cost among high users of the emergency department. Acad Emerg Med. 2016;23:722-730. [DOI] [PubMed] [Google Scholar]
- 13. Agency for Healthcare Research and Quality (AHRQ). Emergency Severity Index (ESI): a triage tool for Emergency Department care; 2012. Available at https://www.ahrq.gov/professionals/systems/hospital/esi/index.html, accessed January 2017. [Google Scholar]
- 14. Misty B, de Ramirez SS, Kelen G, et al. Accuracy and reliability of emergency department triage using the Emergency Sever-ity Index: an international multicenter assessment [published online ahead of print November 23, 2017]. Ann Emerg Med. doi: 10.1016/j.annemergmed.2017.09.036. [DOI] [Google Scholar]
- 15. The Dartmouth Atlas Institute. List of ICD-9-CM codes by chronic disease category: nine chronic conditions used in the Dartmouth Atlas of Health Care 2008. http://www.dartmouthatlas.org/downloads/methods/chronic_disease_codes_2008.pdf. Published March 3, 2008. Accessed June 13, 2016.
- 16. Reschovsky JD, Hadley J, Saiontz-Martinez B, Boukus ER. Following the money: factors associated with the cost of treating high-cost Medicare beneficiaries. Health Serv Res. 2011;46:997-1021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Burns J, Sacchetti A. Enrollment with a primary care provider does not preclude ED visits for patients with woman’s health-related problems. Am J Emerg Med. 2016;34:266-268. [DOI] [PubMed] [Google Scholar]
- 18. Fung CS, Wong CK, Fong DY, Lee A, Lam CL. Having a family doctor was associated with lower utilization of hospital-based health services. BMC Health Serv Res. 2015;15:42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Grumbach K, Keane D, Bindman A. Primary care and public emergency department overcrowding. Am J Public Health. 1993;83:372-378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Hwang W, Liao K, Griffin L, Foley KL. Do free clinics reduce unnecessary emergency department visits? The Virginian experience. J Health Care Poor Underserved. 2012;23:1189-1204. [DOI] [PubMed] [Google Scholar]
- 21. Reid RJ, Johnson EA, Hsu C, et al. Spreading a medical home redesign: effects on emergency department use and hospital admissions. Ann Fam Med. 2013;11(suppl 1):S19-S26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Rust G, Baltrus P, Ye J, et al. Presence of a community health center and uninsured emergency department visit rates in rural counties. J Rural Health. 2009;25:8-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Hunt KA, Weber EJ, Showstack JA, Colby DC, Callaham ML. Characteristics of frequent users of emergency departments. Ann Emerg Med. 2006;48:1-8. [DOI] [PubMed] [Google Scholar]
- 24. Glover CM, Purim-Shem-Tov YA, Johnson TJ, Shah SC. Medicaid beneficiaries who continue to use the ED: a focus on the Illinois Medical Home Network. Am J Emerg Med. 2016;34:197-201. [DOI] [PubMed] [Google Scholar]
- 25. Palmer E, Leblanc-Duchin D, Murray J, Atkinson P. Emergency department use: is frequent use associated with a lack of primary care provider? Can Fam Physician. 2014;60:e223-e229. [PMC free article] [PubMed] [Google Scholar]
- 26. Scherer TM, Lewis LM. Follow-up to a federally qualified health center and subsequent emergency department utilization. Acad Emerg Med. 2010;17:55-62. [DOI] [PubMed] [Google Scholar]
- 27. Zocchi MS, McClelland MS, Pines JM. Increasing throughput: results from a 42-hospital collaborative to improve emergency department flow. Jt Comm J Qual Patient Saf. 2015;41:532-542. [DOI] [PubMed] [Google Scholar]
- 28. Doran KM, Colucci AC, Hessler RA, et al. An intervention connecting low-acuity emergency department patients with primary care: effect on future primary care linkage. Ann Emerg Med. 2013;61:312-321.e7. [DOI] [PubMed] [Google Scholar]
- 29. Kim TY, Mortensen K, Eldridge B. Linking uninsured patients treated in the emergency department to primary care shows some promise in Maryland. Health Aff (Millwood). 2015;34:796-804. [DOI] [PubMed] [Google Scholar]
- 30. Pourat N, Davis AC, Chen X, Vrungos S, Kominski GF. In California, primary care continuity was associated with reduced emergency department use and fewer hospitalizations. Health Aff (Millwood). 2015;34:1113-1120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Rosenthal MB, Alidina S, Friedberg MW, et al. A difference-in-difference analysis of changes in quality, utilization and cost following the Colorado multi-payer patient-centered medical home pilot. J Gen Intern Med. 2016;31:289-296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. The Henry J. Kaiser Family Foundation. Hospital emergency room visits per 1,000 population by ownership type. Date unknown. http://kff.org/other/state-indicator/emergency-room-visits-by-ownership/#. Accessed July 26, 2016.
- 33. US Census Bureau. Annual population estimates by state. https://www.census.gov/popest/data/state/totals/2015/index.html. Accessed May 5, 2016.
- 34. Mandelberg JH, Kuhn RE, Kohn MA. Epidemiologic analysis of an urban, public emergency department’s frequent users. Acad Emerg Med. 2000;7:637-646. [DOI] [PubMed] [Google Scholar]
- 35. Schumacher JR, Hall AG, Davis TC, et al. Potentially preventable use of emergency services: the role of low health literacy. Med Care. 2013;51:654-658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Hsia RY, Friedman AB, Niedzwiecki M. Urgent care needs among nonurgent visits to the emergency department. JAMA Intern Med. 2016;176:852-854. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, SupplTableAndAppendixRev3Jan25-2018 for Reducing High-Users’ Visits to the Emergency Department by a Primary Care Intervention for the Uninsured: A Retrospective Study by Meng-Han Tsai, Sudha Xirasagar, Scott Carroll, Charles S. Bryan, Pamela J. Gallagher, Kim Davis, and Edward C. Jauch in INQUIRY: The Journal of Health Care Organization, Provision, and Financing