Abstract
This study investigates how clay art therapy affects Parkinson’s disease patients’ overall mental and physical condition as well as future treatment potentiality. The research was nonequivalent control groups pre and post study. A total of 54 patients with Parkinson’s disease (control = 28, experimental = 26) were recruited from 3 setting locations in South Korea. Test measures were completed before and after the 16 sessions. The experimental group received two 80-minute evaluations per week for 8 weeks. Demographic information: hand dexterity, self-expression, mood depression, and quality of life measurements. There were significant differences in hand dexterity (t = 4.96, P < .001), self-expression (t = 3.74, P < .001), mood depression (t = −11.85, P < .001), and quality of life (t = 8.07, P < .001) between the 2 groups. Further research and development of clay art therapy can advocate the benefits, highlight practicality and demonstrate the possibility for its usage as a treatment methodology.
Keywords: clay, art therapy, Parkinson
Parkinson’s disease (PD) is a neurodegenerative disorder that commonly affects seniors. The number of PD patients is rapidly rising proportionately compared with a growing senior population. Currently, PD is diagnosed in 428 cases per 100 000 individuals between the ages of 60 and 70 years and 2990 cases per 10 000 in those aged 70 years and older.1 As of 2014, PD patients are estimated at 7.5 million people worldwide and projected to double by 2030.2
PD is a chronic muscular condition that leads to progressive muscle deterioration, induces dementia and decreases mortality.3 Common physical symptoms include hand tremors, stiffness, and difficulty walking.4 In addition, PD patients can appear cold, unfeeling, and angry, which can lead to restriction of activities and interaction with others.4 Lyons et al5 reported that due to physical impairments, individuals with PD tend to have a more negative personality, decreased quality of life, and limited interaction with their environment. An individual’s psychological responses to these physical limitations can include loss of independence, depression, obsessive compulsive thinking, phobia, and stress.4,5
PD is a noncurable condition that requires constant patient support and treatment. There are complementary therapies such as speech, occupational, physical, and creative art to relieve PD symptoms. Each therapy offers distinct advantages and resources for patients to alleviate their symptoms; however the other therapies do not combine the imaginative and stimulating elements of art. This study concentrates on clay art versus other therapies because the art making process is creative, interactive, and allows patients to cope with physical or mental limitations.
Clay is a frequently used art material because of its accessibility and adaptability. It is a very supple material for PD patients to work with. Clay is neutral, and through tactile manipulation, the hands move and perceive the textures and qualities of the clay.6 This process can stimulate all of the body senses and is known to hold regressive qualities.7(pp127-142) Clay art making process is interactive between the patient, materials, and their environment.6,7 More specifically, clay art provides a perceptible vehicle by which something is created with imagination and skill, enabling expression of important ideas or feelings.6,7
The physical activity is the key facilitator. Through interaction with clay, kinesthetic experiences of physical actions and movements release energy and sensory focuses on the experiences of both external and internal sensations.6 PD patients can establish a sensory dialogue between themselves and their surroundings with clay art therapy.
Free clay manipulation is an effective sensorimotor solution in rehabilitation,8 and can reduce physical symptoms of tremors and stiffness in PD patients.9 To support this point, clay art therapy is an alternative treatment that promotes the enhancement of various aspects of mental and physical health in long-term care.10
In short, this study suggests that patients are having a “dialogue” with the clay, which can create a bridge between themselves and their surroundings. This connection allows individuals to reflect back positive aspects of their “core self” despite the adversity of their condition. The study will examine the data compiled from the 2 groups and attempt to establish evidence for clay art therapy as a clinical treatment for PD patients.
Methods
Design
This observational study used a nonequivalent group pre-post design for 8 weeks. The experimental group received two 80-minute clay art therapy sessions per week. The experimental group was introduced to clay art plus usual rehabilitation exercises whereas the control group only maintained routine rehabilitation programs, such as physical activities, game playing, oral-motor exercises, and solving logic/arithmetic puzzles. Test assessment was done before the therapy started and after the 16 sessions. The pre- and pos-test occurred at baseline and 8 weeks. Primary and secondary outcome measures were collected throughout the process.
Sample
From July 16, 2015 to September 15, 2015, this clay art therapy study was announced to the long-term health care boards of hospitals, clinics, and senior rehabilitation facilities in Busan, South Korea, via email and phone calls.
The selected participants were permanent residents of 3 long-term care centers in Busan, South Korea. The 3 senior care facilities averaged between 100 and 150 beds, and provided 24-hour supervision of skilled nursing care, rehabilitation services, meals, and help with daily living. There were no other art therapy programs before this study at the chosen locations.
The inclusion criteria consisted of currently diagnosed PD patients, stages 1 to 4 on the Hoehn and Yahr Staging Scale (H-Y stage ranges from 1 to 5, a higher score indicates more severe impairment and disability), stable on anti-Parkinsonian medication, no previous clay art therapy testing, medication histories (if allowed), and Mini-Mental State Examination (MMSE) scores of 23 or greater denoting good cognitive status. The exclusion criteria as follows: prior art therapy studies, history of brain injury or trauma, and preexisting psychiatric problems.
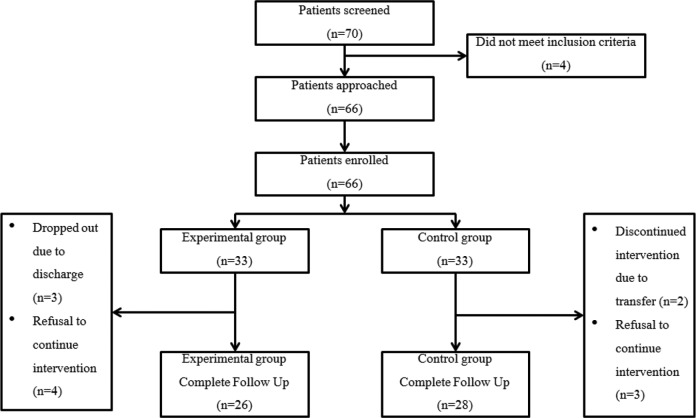
To determine the sample size, a significance level of .05, power of .80, and an effect size of .75 were set. The effect size was based on Cohen.11 The net sample size was 27 PD patients for each group. Thus, 33 PD patients were selected for both the experimental and control groups with a predetermined dropout margin. During the baseline demographic process, 7 PD patients from the experimental group and 5 PD patients from the control group, were eliminated by facility patient discharge or refusal to continue intervention. The final sample of 54 PD patients divided into 2 groups, 26 experimental and 28 control (Figure 1).
Figure 1.
Patient flowchart.
Ethical Consideration
The research protocol, including the questionnaires and clay art therapy layout, were approved by the Institutional Review Board of Pusan National University (PUN IRB/2015-34HR). This program provided each participant a preface that clearly explained the purpose, nature and voluntary rights of this study. All participants were informed and provided written consent forms prior to study inclusion.
Clay Art Program Procedure
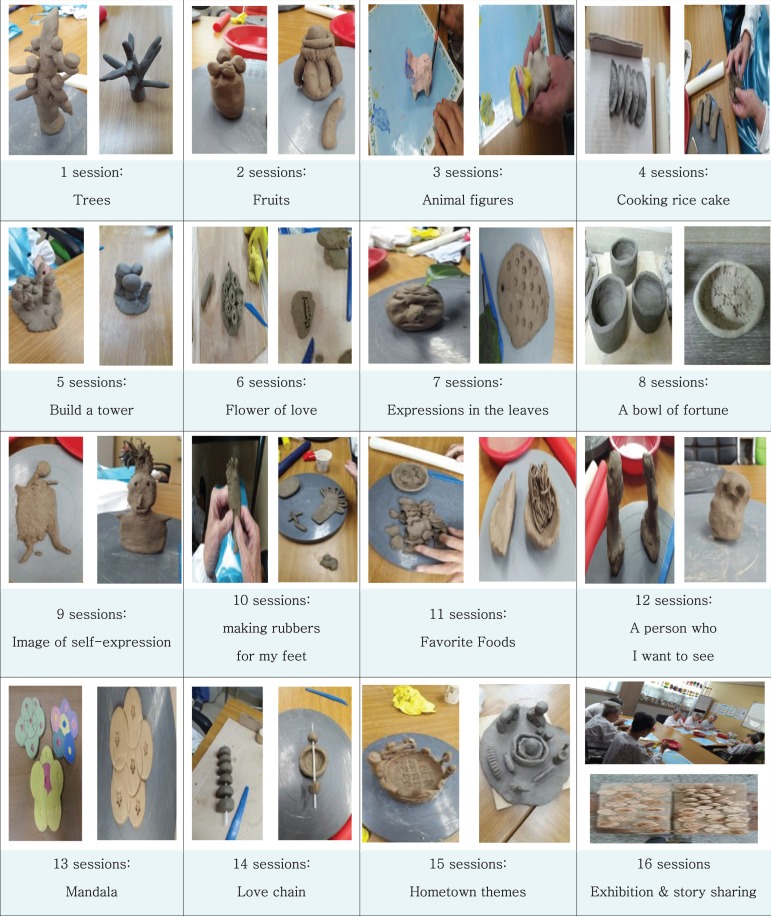
Clay art therapy was performed 2 times a week, 80 minutes per session for 8 weeks, from July 16, 2015 to September 15, 2015. These sessions were co-facilitated by an art therapist and licensed psychologist. Each session consisted of clay art manipulation focused on 16 alternating themes.
Topics covered with modeling were as follows: week 1 (session 1, trees; session 2, fruits), week 2 (session 3, animal figures; session 4, cooking rice cakes), week 3 (session 5, build a tower; session 6, flower of love), week 4 (session 7, expressions in the leaves; session 8, a bowl of fortune), week 5 (session 9, image of self-expression; session 10, making rubbers for my feet), week 6 (session 11, favorite foods; session 12, a person who I want to see), week 7 (session 13, Mandala; session 14, love chain), week 8 (session 15, hometown themes; session 16, exhibition and story sharing) (Figure 2).
Figure 2.
Clay art therapy program.
The clay art therapy process combined person centered theory by Rogers12(pp135-156) and the process-experiential approach by Rice and Greenberg.13,14 Each session used ADDIE (analysis, design, development, implementation, evaluation) to measure and record results.
Each analysis step per topic was corrected with constant reviews and formative evaluations via literature and group interviews with complied individual responses. The literature reviews were performed by a program operator related to Parkinson’s patients, steps, sessions, themes, contents, and attitudes.
From the procedure above, the themes, designs and contents of the entire 16 program sessions were corrected and verified by specialists in a peer evaluation process by calculating the program’s content validity index (CVI). All sessions consisted of the following phases: introduction, activity, and closing. A typical test session would introduce each patient to clay, ask them to mold their interpretations of the session’s theme, collect data on their feelings, expressions, creations, and collate the results.
This program also incorporated 5 stages of change designed by Rice and Greenberg13,14 as listed: Stage 1 (1-4 sessions): The beginning stage fostered: self-perception and self-exploration (themes: trees, fruits, animal figures, and cooking rice cakes). Stage 2 (5-8 sessions): The middle stage focused on the internal desires of exploration & self-discovery (themes: build a tower, flower of love, expressions in the leaves, a bowl of fortune). Stage 3 (9-12 sessions): This stage concentrated on the process change approach to experiential reminiscences (themes: image of self-expression, making rubbers for my feet, favorite foods, and a person who I want to see). Stage 4 (13-14 sessions): Stage 4 aimed at fostering self-understanding and self-acceptance (themes: Mandala, love chain). Stage 5 (15-16 sessions): The last stage centered on self-integration and self-balance (theme: hometown themes, exhibition and story sharing) (Figure 2).
Each clay art therapy session’s contents were based on the image works of Silverstone.15 To have “dialogue” with clay art, PD patients can make bridges between the image and their inner self. Dialogue procedure consisted of: imaging, creating the images in clay art-form, defining the image, recording the emerging feelings, thoughts and physical mannerisms. The following dialogue of a patient session illustrates the constructive benefits of clay art therapy applied to geriatric groups:
Close your eyes. [pause] Please relax and breathe slowly and regularly [pause], clear your mind totally. [pause] Picture an empty room with a door and many windows [lengthy pause], you can see a vibrant and beautiful fruit orchard outside [pause], Imagine yourself opening this door and going for a walk in the orchard. [pause] As you slowly approach the fruits, you see clusters of delicious, ripe and inviting citrus fruit. [pause] As you enter the grove, look very closely and carefully focus on the fresh fruit. [long pause]. What type of fruit do you see and what do you experience. [pause] Collect your thoughts, ideas, dreams or memories of this wonderful moment like a basket of fruit. [pause] Now, picture yourself going home to enjoy, reflect on and express this little journey in a clay art form, in whatever way is right for you. [pause] Slowly open your eyes, maintain your relaxed state of mind and concentrate on how your clay will show your perceptions of this exercise. [pause].
PD patients created subjective, self-made extensions of beliefs, thoughts, feelings and creativity, visible in a symbolic art form.
Measures
We collected demographic and medical variables such as gender, age, marriage status, education, and H-Y stages, duration of disease and treatment, and PD medications. Outcome measures were assessed at baseline and at 8 weeks, after completion of the program: The Box and Block Test (BBT),16,17 scale for self-expression,18 Geriatric Depression Scale Short Form-Korean Version (GDSSF-K),19 Parkinson’s Disease Quality Of Life (PDQOL).20
Hand Dexterity
To measure hand dexterity, we used the BBT. The standard BBT is a functional outcome measure that is commonly used across multiple clinical populations. It is a useful measure because of its ease and speed of implementation, reliable and objective measurement, and repetition of motion.16,17 The BBT counts the number of blocks (2.5 × 2.5 × 2.5) that can be transported one place to another place within 1 minute using both hands.17
Assertive Behavior Assessment Scale for Self-Expression
For self-expression assessment, we used a self-administered version of the Assertive Behavior Assessment Scale (ABAS) form–Korean version developed by Byeun and Kim.18 This scale consists of 20 items divided into 3 domains: content, phonetics, and nonverbal. Each item was rated on a 5-point Likert-type scale (from 5 = never to 1 = always). Higher scores indicated greater self-expression. The internal consistency reliability (Cronbach’s alpha) for this scale was .80.
Geriatric Depression Scale Short Form–Korean Version
For measuring depression, we used a self-administered GDSSF-K version developed by Kee.19 The scale had 2 questions about their depression with a “yes” or “no” response (yes = 1, no = 0). A GDSSF-K included 15 items score ≥5 was used to characterize participants as having clinically significant depression. The internal consistency reliability (Cronbach’s alpha) for this scale was .88.
Parkinson’s Disease Quality of Life
To measure Parkinson’s disease quality of life, we used PDQOL-37 scale developed by Hong.20 PDQOL was a self-administered test with 37 line items in 4 domains: 14 for Parkinson’s symptoms, 7 for general symptoms, 9 for emotional functions, 7 for social functions. Each item was rated on a 5-point Likert-type scale with labels at each scale (from 5 = never to 1 = always). Higher scores are reflected in quality of life. The internal consistency reliability (Cronbach’s alpha) for this scale was .87.
Statistical Analysis
The data were analyzed using SPSS version 22.0 (IBM Corp, Armonk, NY). Descriptive statistics were used to summarize the participants’ demographic and clinical characteristics. In order to determine the homogeneity of the experimental and control group, Chi-square tests and t test were used. To examine the differences between the group variables, t test, analyses of variance, and Scheffé tests were performed. Before and after administering clay art to both subject groups, independent t tests/paired t tests were conducted to measure the values of homogeneity of hand dexterity, self-expression, depression and PDQOL. A P value of <.05 was considered significant.
Results
Demographic and Medical Variables
Table 1 shows the results of demographic and medical variables. The participants were 54 PD patients divided into experimental group (n = 26) and control group (n = 28). For the experimental group 34.5% were male, 65.4% were female, mean age of 80.27 years, 51.7% displayed bereavement, 57.7% were married, 57.6% completed elementary school, and 61.5% reported 2 to 2.5 H-Y stages. Periods of disease/treatment duration were 7.76 and 7.78 years were disease/treatment duration periods, additionally 57.6% took Levodopa.
Table 1.
Homogeneity Test of General Characteristics Between Experimental and Control Groups (N = 54).
| Characteristics | Variables | Experimental (n = 26); n (%) or Mean ± SD | Control (n = 28); n (%) or Mean ± SD | χ2 or t | P |
|---|---|---|---|---|---|
| Gender | Male | 9 (34.5) | 13 (46.4) | 0.77 | .377 |
| Female | 17 (65.4) | 15 (53.6) | |||
| Age (years) | 80.27 ± 8.42 | 82.07 ± 6.46 | −0.88 | .380 | |
| Marital status | Single | 1 (3.8) | 0 (0.0) | 3.36 | .086 |
| Married | 15 (57.7) | 11 (39.3) | |||
| Bereavement | 10 (38.5) | 17 (60.7) | |||
| Education level | Elementary | 15 (57.6) | 16 (57.1) | 9.18 | .057 |
| Middle | 5 (19.2) | 4 (14.3) | |||
| High | 4 (15.4) | 6 (21.4) | |||
| ≥College | 2 (7.7) | 2 (7.1) | |||
| Hoehn and Yahr Stagea | 1-1.5 | 6 (23.0) | 6 (21.4) | 0.39 | .538 |
| 2-2.5 | 16 (61.5) | 16 (57.2) | |||
| 3 | 4 (15.4) | 6 (21.4) | |||
| Duration of disease (years) | 7.76 ± 4.80 | 9.71 ± 5.06 | −1.44 | .154 | |
| Duration of treatment (years) | 7.78 ± 4.80 | 9.53 ± 4.57 | −1.37 | .157 | |
| Anti-Parkinsonian medication | Levodopa | 15 (57.7) | 10 (35.7) | −0.947 | .735 |
| Pramipexole IR | 4 (15.4) | 9 (32.1) | |||
| Cabergoline | 3 (11.5) | 3 (10.7) | |||
| Ropinirole | 4 (15.4) | 6 (21.4) |
aScheffé tests
For the control group, 46.4% were male, 53.6% were female, mean age was 82.07 years, 60.7% show bereavement, 57.1% finished elementary school, 57.2% reported 2 to 2.5 H-Y stages. Also, 9.71 and 9.53 years were disease/treatment duration periods, additionally 35.7% took Levodopa.
Statistically, there were no significant differences between the 2 groups in gender (χ2 = 0.77, P = .377), age (t = −0.88, P = .380), marriage status (χ2 = 3.36, P = .086), education (χ2 = 9.18, P = .057), H-Y stages (χ2 = 0.39, P = .538), duration of disease (t = −1.44, P = .154), duration of treatment (t = −1.37, P = .157), and anti-Parkinsonian medication (t = −0.947, P = .735).
Table 2 shows homogeneity of hand dexterity, self-expression, depression, and quality of life, prior to the 2 groups’ participation in the study regimen. There were marginal differences between the 2 groups in hand dexterity (t = −0.11, P = .907), self-expression (t = −1.51, P = .137), depression (t = −0.55, P = .954), and quality of life (t = −1.22, P = .227).
Table 2.
Homogeneity Test of Dependent Variables Between Experimental and Control Groups (N = 54).
| Variables | Experimental (n = 26); Mean ± SD | Control (n = 28); Mean ± SD | t | P |
|---|---|---|---|---|
| Hand dexterity | 35.88 ± 5.61 | 36.07 ± 5.99 | −0.11 | .907 |
| Self-expression | 63.11 ± 12.92 | 63.35 ± 16.95 | −1.51 | .137 |
| Depression | 10.34 ± 2.71 | 11.60 ± 3.35 | −0.55 | .954 |
| Quality of life | 92.26 ± 32.97 | 105.03 ± 43.27 | −1.22 | .227 |
Table 3 shows the pre- and posttest results of clay art therapy on hand dexterity, self-expression, depression, and quality of life between the 2 groups. The post-pretest scores highlighted statistically significant variances in hand dexterity (t = 4.96, P < .001), self-expression (t = 3.74, P < .001), improved mood (t = −11.85, P < .001), and quality of life (t = 8.07, P < .001).
Table 3.
Comparison of the Effects in Hand Dexterity, Self-Expression, Depression, and Quality of Life Before and After the Clay Art Therapy Between Groups (N = 54).
| Characteristic | Variables | Experimental (n = 26); Mean ± SD | Control (n = 28); Mean ± SD | t | P |
|---|---|---|---|---|---|
| Hand dexterity | Pre | 35.88 ± 5.61 | 36.07 ± 5.99 | ||
| Post | 37.57 ± 5.20 | 34.07 ± 6.29 | |||
| Post-pre | 1.69 ± 2.13 | −2.00 ± 3.18 | 4.96 | <.001 | |
| Self-Expression | Pre | 63.11 ± 2.92 | 63.35 ± 16.95 | ||
| Post | 69.69 ± 0.63 | 64.32 ± 15.63 | |||
| Post-pre | 6.57 ± 4.58 | 0.96 ± 6.37 | 3.74 | <.001 | |
| Depression | Pre | 10.34 ± 2.71 | 11.60 ± 3.35 | ||
| Post | 5.73 ± 2.12 | 11.89 ± 3.18 | |||
| Post-pre | −4.61 ± 1.83 | 0.28 ± 1.15 | −11.85 | <.001 | |
| Quality of life | Pre | 92.26 ± 32.97 | 105.03 ± 43.27 | ||
| Post | 110.80 ± 25.94 | 100.71 ± 41.67 | |||
| Post-pre | 18.53 ± 8.05 | −4.32 ± 12.16 | 8.07 | <.001 |
Discussion
Study results indicate that clay art is a viable platform of therapy for PD patients. The study findings revealed statistically significant: improved hand dexterity, better mood, elevated self-expression, and enhanced quality of life. Creating art can help distract PD patients from thoughts of the disease, and stimulating a relaxed, peaceful state of mind.10
Clay manipulation involves tactile sensations, which stimulates and coordinates physical sensorimotor hand usages along with ocular movements. With hand manipulation and direct contact with clay, “skin sense” is instantly reflected back, as a sensory perception to an individual’s mind. Clay art therapy creates, both a psychological and physiological environment, for PD patients to experience and cultivate a better quality of life.
In a study by Elkis-Abuhoff et al,21 a PD group engaging in the clay medium had a greater decrease of emotional stress and somatic symptoms than a non-PD group. Goldblatt et al22 has also reported that using clay art therapy reduced negative ruminating thoughts in 22 PD patients. All of the above referenced participants, showed significantly lower measures of depression, obsessive-compulsive symptoms, and phobic anxiety as a result of the manipulation of modeling clay. This research shows how PD patients can engage in creative expression to value individuality, bolster creativity, promote memories, maintain motor skills, and expand their overall aesthetic experience while in treatment.
The aforementioned research,21,22 coincides with the results of this study, to reveal similar statistics that support the use of clay manipulation for PD patients. This study’s experimental group using clay art therapy produced significant beneficial effects in scores of depression compared with the control group. This result found that clay art should be further pursued as a complementary therapy to discharge negative emotionality, subjectivity and physicality in PD patients.
In 2013, Abramowitz23 reported that 4 females, ranging in age from 86 to 93 years, participated in a clay art therapy course for 15 months, and conducted posttherapy interviews about their experiences. Their feedback indicated that each individual experienced higher levels of self-expression through “tactile applications of clay” versus other forms of art like dancing, painting, or singing.
This study showed significant improvement in PD patients’ self-expression after 8 weeks of molding clay. The evidence suggests that clay art work allows people to connect their internal and external worlds. PD patients can release emotions, by applying control over their feelings through their hands. In effect, they can experience relaxation, pleasure and fulfillment because working with the clay simultaneously creates something for personal satisfaction as well as reveals inner emotions to themselves and others.
In addition, based on this study, the pre-post test scores highlighted statistically significant in hand dexterity. The findings revealed that the clay medium lends itself best to manipulation with both hands. Each patient can squeeze, roll, and form clay to experience a form of self-expression that overcomes their physical limitations.
Previous studies6,21,24 have reported that clay art work allows kinesthetic motor impulses to emerge and introduces sensory body awareness through the sense of touch. Consistent with our findings, clay manipulation stimulates hand dexterity. Patients can squeeze, roll, and form clay to experience a form of self-expression that helps alleviate psychological, physical, neurological, and cognitive impairments.
In summary, clay art is an empowering tool for PD patients to strengthen their inherent abilities through a creative process. The process is impulsive and imaginative. With clay art therapy, PD patients can gain perspective, value, and reality to their inner self. With this study, we suggest continued research with clay art to develop strategic methods that will improve hand dexterity, enhance patient interaction, refine testing/data collection systems, and introduce it as a potential component of standard rehabilitation.
Limitations
There are several limitations in this study. First, to strengthen this evidence-based study, the PDQ-39 scale versus PDQOL-37 scale Korean version could have been used. Second, research on the effects of clay art therapy with PD patients has been limited because previous studies23,25,26 also included physical exercise or training as test measures. Third, patient diversity in the study sample was limited by geography, all participants came from the same city, Busan, despite attempts to recruit candidates from different cities. Fourth, the effects of anti-Parkinson’s medication were not considered. Dosage evaluations would have affected results. Fifth, this study did not factor in minimal clinically important difference values. Minimal clinically important differences would have analyzed the impact of clay art therapy on PD patient’s functional abilities.
Conclusions
This study’s results indicate that clay art therapy can affect PD patients overall mental and physical condition in long-term care centers. Clay art therapy can even allow PD patients to experience and possibly develop new interpersonal or social relationships with in a group setting.
Social interaction or activities can boost self-confidence, increase emotional stability, and enhance the quality of life for PD patients. Clay modeling also helps alleviate the physical symptoms of PD such as muscle rigidity, tremors, fatigue, impaired speech, and sleep disorders.
These findings have important implications for clay art as a nonpharmacological form of therapy. Therefore, this study suggests that clay work’s potentiality for implementation as a clinical model should be explored and advanced for PD patients.
Acknowledgments
The authors wish to thank all staff, PD patients, and volunteers participating in this research study conducted at Sungshim, Inchang, and Joeunaein long-term care centers.
Footnotes
Author Contributions: Y-SB was involved with understanding the original research articles, writing of the reviews, and editing. D-HK was involved with discussion, reference editing, and collection of original articles.
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
Ethical Approval: The research was approved by the Institutional Review Board of Pusan National University (PUN IRB/2015-34HR).
References
- 1. Pringsheim T, Jette N, Frolkis A, Steeves TD. The prevalence of Parkinson’s disease: a systematic review and meta-analysis. Mov Disord. 2014;29:1583–1590. [DOI] [PubMed] [Google Scholar]
- 2. Dorsey ER, Constantinescu R, Thompson JP, et al. Projected number of people with Parkinson disease in the populous nations, 2005 through 2030. Neurology. 2007;68:384–386. [DOI] [PubMed] [Google Scholar]
- 3. Simpson J, Haines K, Lekwuwa G, Wardle J, Crawford T. Social support and psychological outcome in people with Parkinson’s disease: evidence for a specific pattern of associations. Br J Clin Psychol. 2006;45:585–590. doi:10.1348/014466506X96490. [DOI] [PubMed] [Google Scholar]
- 4. Lyons KD, Tickle-Degnen L, Henry A, Cohn ES. Behavioral cues of personality in Parkinson’s disease. Disabil Rehabil. 2004;26:463–470. [DOI] [PubMed] [Google Scholar]
- 5. Pereira DDC, Siqueira SA, Alvisl TC, Vasconcelos LAP. Group physical therapy program for patients with Parkinson’s disease: alternative rehabilitation. Fisioterapia em Movimento. 2009:22;229–237. [Google Scholar]
- 6. Elbrecht C, Antcliff LR. Being touched through touch, Trauma treatment through haptic perception at the clay field: a sensorimotor art therapy. Int J Art Ther. 2014;19:19–30. [Google Scholar]
- 7. Henley D. Clayworks in Art Therapy: Plying the Sacred Circle. London, England: Jessica Kingsley; 2002. [Google Scholar]
- 8. Symons J, Clark H, Williams K, Hansen E, Orpin P. Visual art in physical rehabilitation: experiences of people with neurological conditions. Br J Occup Ther. 2011:74;44–52. [Google Scholar]
- 9. Park S. Goal setting in occupational therapy: a client-centred perspective In: Duncan EAS, ed. Skills for Practice in Occupational Therapy. 4th ed Edinburgh, Scotland: Churchill Livingstone/Elsevier; 2009:105–122. [Google Scholar]
- 10. Nan JKM, Ho RTH. Effects of clay art therapy on adult’s outpatients with major depressive disorder: a randomized controlled trial. J Affect Disord. 2017;217:237–245. doi:10.1016/j.jad.2017.04.013. [DOI] [PubMed] [Google Scholar]
- 11. Cohen H. Statistical Power Analysis for the Behavioral Sciences. Rev ed Hillsdale, NJ: Lawrence Erlbaum; 1987:179–209. [Google Scholar]
- 12. Rogers CR. The Carl Rogers Reader Kirschenbaum H, Henderson VL, Translators. Boston, MA: Houghton Mifflin; 1989. [Google Scholar]
- 13. Rice LN, Greenberg LS. Two affective change events in client-centered therapy In: Safran JD, Greenberg LS, eds. Emotion, Psychotherapy, and Change. New York, NY: Guilford Press; 1991:197–210. [Google Scholar]
- 14. Rice LN, Greenberg LS. Fundamental dimensions in experiential therapy: new directions in research In: Lietaer G, Rombauts J, Van Balen R, eds. Client-Centered and Experiential Psychotherapy in the Nineties. Leuven, Belgium: Leuven University Press; 1990:397–414. [Google Scholar]
- 15. Silverstone L. Art therapy Exercises: Inspirational and Practical Ideas to Stimulate the Imagination (Foreword by Thorne B.). Philadelphia, PA: Jessica Kingsley; 2009. [Google Scholar]
- 16. Kontson K, Marcus I, Myklebust B, Civillico E. Targeted box and blocks test: normative data and comparison to standard tests. PLoS One. 2017;12:e0177965 doi:10.1371/journal.pone.0177965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Marthiowetz V, Volland G, Kashman N, Weber K. Adult norms for the Box and Block Test of manual dexterity. Am J Occup Ther. 1985;39:386–391. [DOI] [PubMed] [Google Scholar]
- 18. Byun CJ, Kim SH. Assertiveness training program. Stud Guiding Res. 1980;13:51–85. [Google Scholar]
- 19. Kee BS. A preliminary study for the standardization of geriatric depression scale short form-Korea version. J Korean Neuropsychiatr Assoc. 1996;35:298–307. [Google Scholar]
- 20. Hong SK. Quality of Life in Patients With Parkinson’s Disease [dissertation] Busan, South Korea: Dong-A University; 2001. [Google Scholar]
- 21. Elkis-Abuhoff DL, Goldblatt RB, Gaydos M, Corrato S. Effects of clay manipulation on somatic dysfunction and emotional distress in patients with Parkinson’s disease. J Am Art Ther Assoc. 2008;25:122–128. [Google Scholar]
- 22. Goldblatt R, Elkis-Abuhoff D, Gaydos M, Napoli A. Understanding clinical benefits of modeling clay exploration with patients diagnosed with Parkinson’s disease. Arts Health. 2010;2:140–148. doi:10.1080/17533010903495405. [Google Scholar]
- 23. Abramowitz K. The unstructured use of clay in art therapy with older adults. J Can Art Ther Assoc. 2013;26:74–79. [Google Scholar]
- 24. Hass-Cohen N, Carr R. Art Therapy and Clinical Neuroscience. London, England: Jessica Kingsley; 2008:45–50. [Google Scholar]
- 25. Harro CC, Shoemaker MJ, Frey O, et al. The effects of speed-dependent treadmill training and rhythmic auditory-cued overground walking on balance function, fall incidence, and quality of life in individuals with idiopathic Parkinson’s disease: a randomized controlled trial. NeuroRehabilitation. 2014;34:541–556. doi:10.3233/NRE-141048. [DOI] [PubMed] [Google Scholar]
- 26. Paker N, Bugdayci D, Goksenoglu G, Sen A, Kesiktas N. Effects of robotic treadmill training on functional mobility, walking capacity, motor symptoms and quality of life in ambulatory patients with Parkinson’s disease: a preliminary prospective longitudinal study. NeuroRehabilitation. 2013;33:323–328. doi:10.3233/NRE-130962. [DOI] [PubMed] [Google Scholar]