Abstract
Purpose
Research in the area of cultural response pattern on questionnaires in the oncological setting and direct cross-cultural comparisons are lacking. This study examined response pattern in the reporting of depressive symptoms in Chinese and US women with breast cancer. We hypothesized that Chinese women are less likely to endorse positive affect items compared to their US counterparts. Additionally, we explored cultural differences in the association between positive affect and QOL.
Methods
Secondary analyses of baseline assessments of two mind-body intervention studies for women with breast cancer undergoing radiotherapy in the USA (N = 62) and China (N = 97) are presented. All participants completed measures of depressive symptoms (CES-D) and cancer-specific QOL (FACT-B). We examined cultural differences on positive and negative affect items on the CES-D.
Results
Controlling for demographic factors, ANCOVA revealed a significant cultural difference in positive (F = 7.99, p = 0.005) but not negative affect (p = 0.82) with Chinese women reporting lower positive affect compared to US women (Chinese = 6.97 vs. US = 8.31). There was also a significant cultural difference (F = 3.94, p = 0.03) in the association between positive affect and QOL so that lower positive affect was more strongly associated with worse emotional well-being in Chinese (beta = 0.57, p < 0.0001) than US women (beta = 0.35, p < 0.01).
Conclusions
Chinese women reported lower positive affect compared to US women and lower levels of positive affect were more strongly associated with worse QOL. Special attention is needed when examining mental health in different cultures to ascertain effective delivery of clinical services to those in need.
Keywords: Depressive symptoms, Response pattern, Breast cancer, Chinese-US cross-cultural comparison, Quality of life
Introduction
Cancer is one of the leading causes of morbidity and mortality worldwide [1]. Traditionally, rates of breast cancer have been higher in western developed countries, but incidence is increasing in the developing world [1]. Whereas US breast cancer incidence has been declining since 2000, China has experienced a substantial increase [2, 3]. Nevertheless, methods of cancer prevention and control have improved in China so that many Chinese women are living longer after a diagnosis of breast cancer. With this increase in survival, psychosocial concerns including depression and quality of life (QOL) has gained increasing attention in China [4, 5]. Studies on breast cancer patients have found depressive symptoms ranging from 26 to 36% in Chinese samples and around 30% in US samples compared to 4.5 to 9.3% for women in the general US population [6–9]. General population depression statistics for Chinese women are less known, but depression symptomology in China appears to be similar to US rates and somewhat higher [10, 11].
The Center for Epidemiologic Studies Depression Scale (CES-D), a 20-question self-report depression scale, has been shown to be the most versatile tool in cancer populations [12]. The measure has been validated in both US and Chinese community samples [10, 13]. The scale consists of 4 positive affect items (e.g., “I was happy”) that are reverse scored, and 16 negative affect items (e.g., “I felt depressed”). In non-clinical samples, cross-cultural comparisons of CES-D scores from Asian countries (Japan and Korea) and the US have found that, although both populations report similar values for the negative affect items, Asian participants’ scores on positive affect items are lower. Thus, based on assumptions of universal content validity and psychometrics of the CES-D, one would conclude that Asians will score higher on depressive symptoms compared to US participants. Alternatively, some authors have argued that these studies may reveal a culturally sensitive response pattern to items assessing positive affect [14–20]. This idea is supported by data pointing to the association between level of acculturation and cultural differences in positive affect scores. For example, in one study, Korean American immigrants were less likely to endorse positive affect items than US Caucasians but more likely than Koreans who had not immigrated [17]. The study also revealed that immigrants’ degree of acculturation moderated the endorsement of positive affect. Specifically, when the CES-D was administered in Korean, immigrants who scored higher on acculturation were more likely to endorse positive affect items than immigrants who scored lower suggesting that culture as opposed to language or language translation is associated with the difference in positive affect endorsement [17].
Whether these findings are due to a difference in response pattern to positive affect items or if the actual experience of positive affect differs between cultures is not clear; however, a difference in the endorsement of positive affect appears to be consistent across Asian cultures, languages, and types of mood assessments. For instance, in one study, a difference in positive affect response pattern has also been shown on the State Trait Anxiety Inventory (STAI) questionnaire used to measure anxiety symptoms [14]. When responses on this questionnaire were compared between university students in Japan and in the USA, Japanese students were less likely to endorse positive feelings (I feel secure, self-confident, content, etc.), which resulted in higher anxiety scores compared to the US students. Scores on anxious feelings (e.g., I am tense, I feel nervous, I feel confused, etc.) were no different between groups. The literature refers to the term “positive affect suppression” to describe responses to positive affect relative to negative affect items [20].
Because previous studies focused entirely on healthy, community samples, the current study seeks to examine if the noted positive affect response pattern (or potential affect suppression) generalizes to women with breast cancer, who are more vulnerable to depressive symptoms than the general population [6, 7, 12]. It is important to identify potential cross-cultural influences that may impact responses on questionnaires to more appropriately assess depressive symptoms in diverse populations [21–23]. International clinical trials are increasingly assessing patient reported outcomes and thus, cultural differences in the expression of depressive symptoms become increasingly relevant. We hypothesize that Chinese women with breast cancer are less likely to endorse positive affect items compared to US counterparts. Additionally, we sought to extend previous findings and explored cultural differences in the association between positive affect and cancer-related QOL. Understanding cultural differences in depressive symptomology and its association with cancer-related QOL may inform culturally sensitive psychosocial interventions targeting mood management in cancer patients.
Methods
Participants
A total of 159 breast cancer patients (97 Chinese and 62 American) who participated in two comparable intervention studies conducted in Shanghai, China and Houston, USA were examined. Detailed information on the study methods and intervention outcomes has been published previously [24, 25]. The research nurse and oncologists identified eligible Chinese patients in the breast cancer clinic. Eligible US patients were identified through an electronic database. Both Chinese and US patients were recruited prior to beginning radiotherapy. Inclusion criteria for both studies were (1) women 18 years or older; (2) able to read, write, and speak Mandarin for Chinese participants or English for US participants; (3) diagnosed with stage 0-III breast cancer; and (4) completed breast surgery and/or chemotherapy and had not started radiotherapy. Patients were excluded if they were diagnosed with a major psychiatric illness.
Procedures
Informed consent was obtained prior to all data collection procedures. One hundred twenty-three Chinese participants were asked to participate in a Qigong intervention study and 100 consented. One hundred thirty-seven US participants were asked to participate in a Yoga intervention study and 81 consented. Before randomization to the control or intervention group and within 1 week of the start of radiotherapy, all participants completed self-reports about their depressive symptoms, QOL, and demographic information (Chinese and US response rates were 97 and 70.4%, respectively). Approval for the Yoga and Qigong intervention studies was obtained through the MD Anderson Institutional Review Board. The Qigong study was also approved by the Fudan University Shanghai Cancer Center Institutional Review Board.
Measures
Depressive symptoms were measured with the CES-D [19, 26]. Positive affect items were reverse scored so that higher scores represent more depressive symptomology. A score of 16 or greater is widely used as the cut-off to consider further evaluation for mood disorders [26–28]. For the purpose of this study, the conventional total score as well as positive and negative affect subscales are presented. Reliability coefficient Cronbach’s alphas (α) for CES-D negative affect items (Chinese, α = 0.82, US, α = 0.84) and positive affect items (Chinese, α = 0.87, US, α = 0.78) were acceptable in both samples.
Quality of life was measured with the Functional Assessment for Cancer Therapy breast cancer scale Version 4 (FACT-B); that is also validated for Chinese breast cancer patients [29–31]. The FACT-B consists of the original four subscales of the Functional Assessment for Cancer therapy general scale (FACT-G): physical well-being (PWB), functional well-being (FWB), emotional well-being (EWB), and social/family well-being (SWB). The FACT-B also contains a category of additional concerns, which addresses breast cancer specific issues (BCS). Because one of the items in the SWB dimension asked about sexual satisfaction and was largely omitted by Chinese women, the item was excluded from the analyses. To avoid measurement confounds with the CES-D, we removed the “I feel sad” item from the EWB subscale for all analyses.
Patients completed questions pertaining to basic demographics, and medical data was extracted from patient charts.
Data analyses
Data analysis was carried out in SPSS 23. Basic descriptive statistics were first computed within each of the cultural samples. Chi square and t test analyses were used to compare samples on demographic and cancer-related characteristics, age, income, education, stage, chemotherapy, mastectomy, and significant depressive symptoms (CES-D score ≥ 16). Factors on which a significant cultural difference was revealed at p < 0.05 were controlled for as covariates in the main analyses. To further characterize the samples, we examined within cultural bivariate correlations for study variables. We examined the associations between medical and demographic factors and study variables (CES-D negative and positive items subscales as well as Fact-B) with analysis of variance (ANOVA) to identify potential confounding variables. Factors that were significant as p < 0.05 were included as covariates in our primary analyses. We used analysis of covariance (ANCOVA) to test the hypothesis that Chinese women are less likely to endorse positive affect items compared to US women. To explore cultural differences in the association between positive affect and QOL, we examined the interactions between culture (i.e., Chinese vs. American) and positive affect controlling for main effects and appropriate covariates as described above.
Results
Descriptive findings
Comparisons between the Chinese and US sample on demographic factors and breast cancer factors are shown in Table 1. Based on t test and chi-square analyses, Chinese women tended to be younger (p < 0.001), less affluent (p < 0.001), less educated (p < 0.001), and were more likely to be given chemotherapy (p < 0.001) than their US counterparts. Regarding CES-D caseness, 39.2% of Chinese and 33.3% of American women scored 16 or above (p = 0.49). Level of income was significantly associated with the positive and negative affect subscales in both samples (p < 0.01) so that women with less income reported more negative and less positive affect. No other demographic or medical factor was significantly associated with CES-D subscales at p < 0.05.
Table 1.
Demographic and cancer-related characteristics
| Total N = 159 N (%) |
Chinese N = 97 N (%) |
US N = 62 N (%) |
F/X2 | Df | p value | |
|---|---|---|---|---|---|---|
| Age | M = 46.4, SD = 8.4 | M = 52.8, SD = 9.0 | 11.57 | 1 | 0.001 | |
| 25–45 years | 54 (34.0) | 38 (39.2) | 16 (25.8) | 15.53 | 2 | <0.001 |
| 46–55 years | 61 (38.4) | 43 (44.3) | 18 (29.0) | |||
| 56–68 years | 44 (27.7) | 16 (16.5) | 28 (45.2) | |||
| Annual personal income | 16.66 | 2 | <0.001 | |||
| Below average | 9 (5.7) | 6 (6.2) | 3 (4.8) | |||
| Average | 50 (31.4) | 43(44.3) | 7 (11.3) | |||
| Above average | 65 (40.9) | 33 (34.0) | 32 (51.7) | |||
| Missing | 35 (22.0) | 15 (15.5) | 20 (32.3) | |||
| Educational attainment | 35.11 | 2 | <0.001 | |||
| High school or lower | 51 (32.1) | 44 (45.4) | 7 (11.3) | |||
| College | 80 (50.3) | 47(48.4) | 33(51.3) | |||
| Graduate degree | 25 (15.7) | 4 (4.1) | 21 (33.9) | |||
| Missing | 3 (1.9) | 2 (2.1) | 1 (1.6) | |||
| Disease stage | 0.17 | 2 | 0.92 | |||
| 0-I | 47 (29.5) | 28 (28.9) | 19 (30.7) | |||
| II | 62 (39.0) | 35(36.1) | 27 (43.5) | |||
| III | 40 (25.2) | 24 (24.7) | 16(25.8) | |||
| Missing | 10 (6.3) | 10 (10.3) | 0 (0) | |||
| Mastectomy | 2.16 | 1 | 0.14 | |||
| Yes | 79 (49.7) | 53 (54.6) | 26 (41.9) | |||
| No | 79 (49.7) | 44 (45.4) | 35 (56.5) | |||
| Missing | 1 (.6) | 0 (0) | 1 (1.6) | |||
| Chemo | 15.73 | 1 | <0.001 | |||
| Yes | 137 (86.2) | 92 (94.8) | 45 (72.6) | |||
| No | 22 (13.8) | 5 (5.2) | 17 (27.4) | |||
| Caseness | 0.47 | 1 | 0.49 | |||
| Yes | 57 (35.8) | 38 (39.2) | 19 (30.6) | |||
| No | 97 (61.0) | 59 (60.8) | 38 (61.3) | |||
| Missing | 5 (3.1) | 0 (0) | 5 (8.1) |
The cut-off points of average and low income are retrieved from government report for each cultural sample, which are $8000 and $1500 (currency rate 6.34 Yuan = $1 USD) in the Chinese sample, and are $50,000 and $20,000 in the US sample. Caseness CES-D score of ≤16
Regarding QOL, Chinese women reported statistically and clinically significantly lower QOL on the FACT-B total score as well as statistically significantly lower QOL on all sub-scales compared to US women (Table 2; details on these comparisons have been previously reported elsewhere [32]). In both samples, lower level of income was significantly associated with lower QOL (p < 0.05). In the Chinese sample, chemotherapy and higher stage were significantly associated with lower QOL (p < 0.05). Correlations for depressive symptoms and QOL for each sample are also presented in Table 2.
Table 2.
Raw means, standard deviations and correlation coefficients of study variables by sample
| Variable | Chinese (N = 97) | US (N = 62) |
F | 1 | 2 | 3 | 5 | 6 | 7 | 8 | 9 | 10 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean (SD) | ||||||||||||
| 1. CES-D total score | 12.79 (9.09) | 11.16 (7.96) | 1.27 | 0.47*** | 0.15 | −0.42*** | −0.33** | −0.17 | −0.48*** | −0.27* | −0.33** | |
| 2. CES-D neg. score | 7.96 (6.49) | 7.90 (5.97) | 0.004 | 0.51*** | 0.51*** | −0.77*** | −0.55*** | −0.46*** | −0.50*** | −0.72*** | −0.48*** | |
| 3. CES-D pos. score | 4.84 (3.81) | 3.23 (2.97) | 7.84** | 0.27** | 0.53*** | −0.51*** | −0.33** | −0.26* | −0.28* | −0.51*** | −0.42*** | |
| 5. FACT-B | 91.90 (18.20) | 104.12 (14.77) | 19.62*** | −0.27** | −0.71*** | −0.63*** | 0.74**** | 0.62**** | 0.58*** | 0.84*** | 0.74*** | |
| 6. PWB | 19.70 (5.33) | 22.47 (4.17) | 12.01** | −0.24** | −0.68*** | −0.47*** | 0.88*** | 0.27* | 0.22 | 0.64** | 0.42*** | |
| 7. SWB | 19.29 (4.06) | 21.23 (3.58) | 9.41** | −0.19 | −0.30*** | −0.43*** | 0.63*** | 0.41 | 0.32* | 0.44**** | 0.25 | |
| 8. EWB | 14.87 (3.87) | 16.76 (2.74) | 11.20*** | −0.31** | −0.64*** | −0.60*** | 0.80*** | 0.67**** | 0.36 | 0.32** | 0.48*** | |
| 9. FWB | 15.75 (5.19) | 19.53 (5.27) | 19.84*** | −0.14 | −0.54*** | −0.48*** | 0.79*** | 0.60**** | 0.41 | 0.58*** | 0.44*** | |
| 10. BCS | 22.30 (4.88) | 24.13 (4.67) | 5.51* | −0.19 | −0.56*** | −0.51*** | 0.77*** | 0.66**** | 0.35 | 0.5*** | 0.40 |
CES-D neg. score negative items subscale of CES-D; CES-D pos. score positive items subscale of CES-D, reverse scored; PWB physical well-being subscale of FACT-B; SWB social well-being subscale of FACT-B; EWB emotional well-being subscale of FACT-B; FWB functional well-being subscale of FACT-B; BCS breast cancer symptom subscale of FACT-B; Question 14 “I am satisfied with my sex life” was removed from the social well-being subscale and question number 15 “I feel sad” was removed from emotional well-being subscale. Correlation coefficients below the diagonal present values from the Chinese sample and coefficients above the diagonal from the US sample
p < 0.05,
p < 0.01,
p < 0.001,
p < 0.0001
Hypothesis: response pattern on CES-D scores
Consistent with the hypothesis, controlling for level of income, age, education, and chemotherapy, Chinese and US women did not significantly differ on negative affect scores (p = 0.82) or the total score (p = 0.35) of the CES-D. As hypothesized, Chinese women reported significantly lower scores (higher reverse coded scores) on positive affect items (F = 7.99, p = 0.005) (Table 2). Figure 1 portrays least squared means (LSM) for both samples.
Fig. 1.
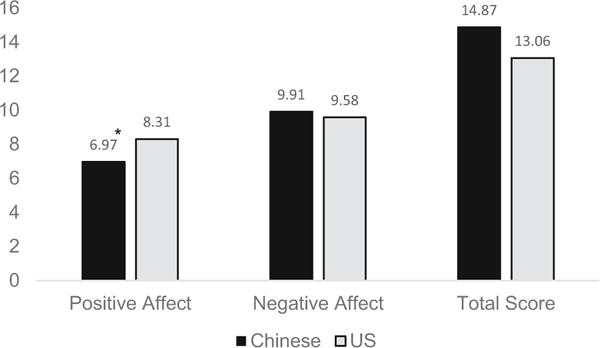
Least square means (controlling for income, age, education, and chemotherapy) for CES-D positive affect, negative affect, and total score for Chinese (n = 97) and US (n = 62) women. Note: The positive affect item subscale is not reversed scored here for the purpose of visual representation. Asterisk significant cultural difference at p < 0.05
Exploratory analysis: positive affect and QOL
Controlling for income, age, education, disease stage and chemotherapy, the interaction between positive affect and culture for FACT-B total scores was not significant (p = 0.79). Total FACT-B scores were significantly associated with the main effects of positive affect scores (F = 56.87, p < 0.0001) and culture (F = 12.01, p < 0.001; LSM, Chinese: 90.98, US mean: 101.90). Regarding FACT-B subscales, there was a significant interaction between positive affect x culture for EWB (F = 3.94, p < 0.05) so that lower positive affect was more strongly associated with worse emotional well-being in Chinese (beta = 0.57, p < 0.0001) than US women (beta = 0.35, p < 0.01). No other interactions for subscales were significant. Thus, for the remaining subscales, we reduced the models to examine the main effects of positive affect and culture controlling for income, age, education, disease stage, and chemotherapy. These multivariate analyses revealed that positive affect was uniquely associated with: SWB (F = 9.81, beta = −0.33, p = 0.002), FWB (F = 62.11, beta = −0.47; p < 0.0001), PWB (F = 21.77, beta = −0.40 p < 0.0001), and BCS (F = 30.49, beta = −0.49; p < 0.0001) so that women with lower positive affect scores reported worse well-being and more breast cancer symptoms. Culture was uniquely associated with SWB (F = 10.59, LSM, Chinese: 19.02, US mean: 21.72; p < 0.01), PWB (F = 4.30, LSM, Chinese: 19.80, US mean: 21.97; p < 0.05), and FWB (F = 10.18, LSM, Chinese: 14.74, US mean: 18.28; p < 0.01) but not BCS (p = 0.41) so that Chinese women reported significantly lower well-being compared to US women even when controlling for relevant covariates.
Discussion
This study examined response pattern on CES-D scores as a function of culture and the association between positive affect and QOL in two similar populations of women in China and the USA before starting breast cancer radiation treatment. Consistent with our hypothesis, this study revealed that, even though there were no significant differences between Chinese and US women in regard to CES-D total scores and the negative affect subscale, there was a significant cultural difference in the positive affect subscale. This difference remained after controlling for level of income, age, education, and previous chemotherapy. These results are consistent with other cross-cultural comparisons of CES-D scores from healthy community Asian populations including South Koreans, Japanese, and Chinese, which have reported that scores on positive affect components are lower, and can lead to higher depressive symptom scores [14, 16–18, 20].
Even though Chinese compared to US women were less likely to endorse positive affect items, this difference did not significantly change the prevalence of depression caseness (CES-D ≥ 16) or CES-D total scores. However, a larger sample size or an instrument that included more positive affect items may have resulted in statistical significant cultural differences. Nevertheless, our findings pertaining to cultural difference in positive affect scores are noteworthy. For one, these findings support the notion that affect is bi-dimensional and should be assessed as such [33]. Some authors have suggested removing positive affect items from depressive symptoms assessment tools or changing positive questions to negative ones (i.e., “I felt hopeful” to “I felt hopeless”) to remove potential measurement confounds [10, 13, 34]. However, our finding revealing cultural differences in the association between positive affect and emotional well-being does not support a unidimensional structure of depressive symptoms as positive affect may have unique predictability. Importantly, the EWB subscale of the FACT-B includes only one positive item (“I am satisfied with how I cope with my illness”) and five negative items (“I feel nervous”, “I worry about dying”, “I worry about my condition getting worse”, “I am losing hope against cancer”, and “I am sad” (sadness item omitted here)) so that the association between EWB and positive affect is not explained by a mere measurement confound due to positively worded items in both scales.
It has been argued that, rather than an index of depression, the positive affect response pattern may be indicative of cultural norms. For instance, Chinese and Japanese ethnicities value low-level positive affect states (e.g., calm) compared to European Americans who value high-level positive affect states (e.g., excited), which could contribute to lower reporting of positive affect in Asian populations [35]. However, the cultural difference in the association between positive affect and EWB may contradict the argument that low positive affect scores in Asian samples is mainly related to reporting patterns as opposed to an actual cultural difference in the manifestation or structure of depressive symptoms. In fact, positive affect was significantly associated with all aspects of QOL as measured by the FACT-B in Chinese women with effect sizes at least as high as or higher than in the US sample. Additionally, the Chinese sample demonstrated variability on positive affect reporting using the entire range of the scale. Thus, dismissing this cultural difference simply as a cultural norm or response pattern does not appear to represent these findings. Nevertheless, further research is needed, and clinical interviews are necessary to separate potential measurement bias and cultural norms from indicators of depression.
Clinical significance
This study revealed cultural differences in the assessment and potentially manifestation of depressive symptoms. Although clinical recommendations are premature at this point, our findings suggest that it may be important for clinicians to consider cultural differences when assessing depression in Chinese women and be aware of response patterns relevant to positive versus negatively worded items when interpreting scores on questionnaires like the CES-D. In addition to psychometrics, delineating the manifestation of depressive symptoms from response patterns may have important implications for psychosocial treatments. Although depressive symptom caseness for both groups was similar, and similar to the findings in other studies [6–9], 39% of the Chinese women and 30% of the US women met the clinically screening criteria suggesting that further assessment is warranted. As cultural differences appear to be found primarily in the area of reduced positive affect in the Chinese patients, interventions that target positive affect may be particularly beneficial to improve QOL in Chinese women. In fact, Eastern-based mind-body practices such as meditation, yoga, and tai chi often fall under the umbrella of “positive psychology” in the West as they tend to focus on fostering positive rather than reducing negative emotions. A substantial body of literature exists examining Eastern-based interventions in US women with breast cancer to enhance QOL. As psychosocial concerns are increasingly considered in Chinese studies, it will be interesting to examine cultural differences in the uptake and efficacy of such interventions.
Limitations
Several caveats of the current study are worth mentioning. The study used convenience samples of self-reported depressive symptoms in Chinese and US women undergoing breast cancer treatment. Both studies had a relatively small sample size limiting our statistical power to detect cultural differences. In addition, the sample size was not large enough to use factor analysis to analyze the likelihood of response on a particular question. Although the Chinese women were on average significantly younger than the US women, age was not linked with the outcomes and we controlled for age in the analyses. This study focused on women with breast cancer and limited the generalizability to men and other cancer patients and may not be representative of the larger cultural population. It is unclear if clinical interviews were used instead of self-reports would have resulted in different findings.
In conclusion, research in the area of cultural response patterns on questionnaires in the oncology setting and the direct comparability across cultural groups has been lacking. This study identified that Chinese women were less likely to endorse positive affect items compared to their US counterparts and that positive affect was more strongly associated with emotional well-being in Chinese compared to US women. Further research is needed with larger sample sizes and more definitive statistical methods to determine the influence of response pattern and depression manifestation in these cultures to better understand the unique ways in which Asian women are impacted by a breast cancer diagnosis and treatment.
Acknowledgments
Support was provided in part by the United States National Cancer Institute (NCI) grants CA108084 and CA121503 (principal investigator, Lorenzo Cohen). Partial support for Lorenzo Cohen was provided by the Richard E. Haynes Distinguished Professorship in Clinical Cancer Prevention and a career development award NIH/NCCIH K01 AT007559 awarded to Kathrin Milbury. Jennifer McQuade is supported by an ASCO Young Investigator Award and T32 Institutional Training Grant.
Footnotes
Compliance with ethical standards
Conflict of interest The authors declare that they have no conflict of interest.
References
- 1.Fitzmaurice C, et al. The global burden of cancer 2013. JAMA Oncol. 2015;1(4):505–527. doi: 10.1001/jamaoncol.2015.0735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Parkin DM, et al. Global cancer statistics, 2002. CA Cancer J Clin. 2005;55(2):74–108. doi: 10.3322/canjclin.55.2.74. [DOI] [PubMed] [Google Scholar]
- 3.Kohler BA, et al. Annual report to the nation on the status of cancer, 1975–2011 featuring incidence of breast cancer subtypes by race/ethnicity, poverty, and state. J Natl Cancer Inst. 2015;107(6):djv048. doi: 10.1093/jnci/djv048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yang YL, et al. The effects of psychological interventions on depression and anxiety among Chinese adults with cancer: a meta-analysis of randomized controlled studies. BMC Cancer. 2014;14:956. doi: 10.1186/1471-2407-14-956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cui Y, et al. The long-term impact of medical and sociodemographic factors on the quality of life of breast cancer survivors among Chinese women. Breast Cancer Res Treat. 2004;87(2):135–147. doi: 10.1023/B:BREA.0000041620.76871.97. [DOI] [PubMed] [Google Scholar]
- 6.So WK, et al. The symptom cluster of fatigue, pain, anxiety, and depression and the effect on the quality of life of women receiving treatment for breast cancer: a multicenter study. Oncol Nurs Forum. 2009;36(4):E205–E214. doi: 10.1188/09.ONF.E205-E214. [DOI] [PubMed] [Google Scholar]
- 7.Zainal NZ, et al. Prevalence of depression in breast cancer survivors: a systematic review of observational studies. Asian Pac J Cancer Prev. 2013;14(4):2649–2656. doi: 10.7314/apjcp.2013.14.4.2649. [DOI] [PubMed] [Google Scholar]
- 8.Zabora J, et al. The prevalence of psychological distress by cancer site. Psychooncology. 2001;10(1):19–28. doi: 10.1002/1099-1611(200101/02)10:1<19::aid-pon501>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 9.Shim RS, et al. Prevalence, treatment, and control of depressive symptoms in the United States: results from the National Health and Nutrition Examination Survey (NHANES), 2005–2008. J Am Board Fam Med. 2011;24(1):33–38. doi: 10.3122/jabfm.2011.01.100121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lin N. Measuring depressive symptomatology in China. J Nerv Ment Dis. 1989;177(3):121–131. doi: 10.1097/00005053-198903000-00001. [DOI] [PubMed] [Google Scholar]
- 11.Hou F, et al. Depression, social support and associated factors among women living in rural China: a cross-sectional study. BMC Womens Health. 2015;15:28. doi: 10.1186/s12905-015-0180-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vodermaier A, Linden W, Siu C. Screening for emotional distress in cancer patients: a systematic review of assessment instruments. J Natl Cancer Inst. 2009;101(21):1464–1488. doi: 10.1093/jnci/djp336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cheung CK, Bagley C. Validating an American scale in Hong Kong: the Center for Epidemiological Studies Depression Scale (CES-D) J Psychol. 1998;132(2):169–186. doi: 10.1080/00223989809599157. [DOI] [PubMed] [Google Scholar]
- 14.Iwata N, Higuchi HR. Responses of Japanese and American university students to the STAI items that assess the presence or absence of anxiety. J Pers Assess. 2000;74(1):48–62. doi: 10.1207/S15327752JPA740104. [DOI] [PubMed] [Google Scholar]
- 15.Jang S, et al. Smoking and quality of life among female survivors of breast, colorectal and endometrial cancers in a prospective cohort study. J Cancer Surviv. 2011;5(2):115–122. doi: 10.1007/s11764-010-0147-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jang Y, Kim G, Chiriboga D. Acculturation and manifestation of depressive symptoms among Korean-American older adults. Aging Ment Health. 2005;9(6):500–507. doi: 10.1080/13607860500193021. [DOI] [PubMed] [Google Scholar]
- 17.Jang Y, Kwag KH, Chiriboga DA. Not saying I am happy does not mean I am not: cultural influences on responses to positive affect items in the CES-D. J Gerontol B Psychol Sci Soc Sci. 2010;65(6):684–690. doi: 10.1093/geronb/gbq052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kanazawa A, White PM, Hampson SE. Ethnic variation in depressive symptoms in a community sample in Hawaii. Cultur Divers Ethnic Minor Psychol. 2007;13(1):35–44. doi: 10.1037/1099-9809.13.1.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Li Z, Hicks MH. The CES-D in Chinese American women: construct validity, diagnostic validity for major depression, and cultural response bias. Psychiatry Res. 2010;175(3):227–232. doi: 10.1016/j.psychres.2009.03.007. [DOI] [PubMed] [Google Scholar]
- 20.Iwata N, Buka S. Race/ethnicity and depressive symptoms: a cross-cultural/ethnic comparison among university students in East Asia, North and South America. Soc Sci Med. 2002;55(12):2243–2252. doi: 10.1016/s0277-9536(02)00003-5. [DOI] [PubMed] [Google Scholar]
- 21.Montazeri A. Quality of life data as prognostic indicators of survival in cancer patients: an overview of the literature from 1982 to 2008. Health Qual Life Outcomes. 2009;7:102. doi: 10.1186/1477-7525-7-102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lam WW, et al. Distress trajectories at the first year diagnosis of breast cancer in relation to 6 years survivorship. Psychooncology. 2012;21(1):90–99. doi: 10.1002/pon.1876. [DOI] [PubMed] [Google Scholar]
- 23.Giese-Davis J, et al. Decrease in depression symptoms is associated with longer survival in patients with metastatic breast cancer: a secondary analysis. J Clin Oncol. 2011;29(4):413–420. doi: 10.1200/JCO.2010.28.4455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chen Z, et al. Qigong improves quality of life in women undergoing radiotherapy for breast cancer: Results of a randomized controlled trial. Cancer. 2013 doi: 10.1002/cncr.27904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chandwani KD, et al. Yoga improves quality of life and benefit finding in women undergoing radiotherapy for breast cancer. J Soc Integr Oncol. 2010;8(2):43–55. [PubMed] [Google Scholar]
- 26.Radloff L. The CES-D scale: A self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1(3):385–401. [Google Scholar]
- 27.Roberts RE, Vernon SW. The Center for Epidemiologic Studies Depression Scale: its use in a community sample. Am J Psychiatry. 1983;140(1):41–46. doi: 10.1176/ajp.140.1.41. [DOI] [PubMed] [Google Scholar]
- 28.Schulberg HC, et al. Assessing depression in primary medical and psychiatric practices. Arch Gen Psychiatry. 1985;42(12):1164–1170. doi: 10.1001/archpsyc.1985.01790350038008. [DOI] [PubMed] [Google Scholar]
- 29.Cella DF, et al. The Functional Assessment of Cancer Therapy scale: development and validation of the general measure. J Clin Oncol. 1993;11(3):570–579. doi: 10.1200/JCO.1993.11.3.570. [DOI] [PubMed] [Google Scholar]
- 30.Brady MJ, et al. Reliability and validity of the Functional Assessment of Cancer Therapy-Breast quality-of-life instrument. J Clin Oncol. 1997;15(3):974–986. doi: 10.1200/JCO.1997.15.3.974. [DOI] [PubMed] [Google Scholar]
- 31.Wan C, et al. Validation of the simplified Chinese version of the FACT-B for measuring quality of life for patients with breast cancer. Breast Cancer Res Treat. 2007;106(3):413–418. doi: 10.1007/s10549-007-9511-1. [DOI] [PubMed] [Google Scholar]
- 32.Lu Q, et al. Differences in quality of life between American and Chinese breast cancer survivors. Support Care Cancer. 2016;24(9):3775–3782. doi: 10.1007/s00520-016-3195-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: the PANAS scales. J Pers Soc Psychol. 1988;54(6):1063–1070. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- 34.Iwata N. In: Cultural distinctiveness in response bias, in psychological factors at work in the Asia Pacific. Dollard MF, Shimazu A, Bin Nordin R, Brough P, Tuckey MR, editors. Springer; New York: 2014. pp. 77–78. [Google Scholar]
- 35.Tsai JL, Knutson B, Fung HH. Cultural variation in affect valuation. J Pers Soc Psychol. 2006;90(2):288–307. doi: 10.1037/0022-3514.90.2.288. [DOI] [PubMed] [Google Scholar]


