Abstract
Background
People living with HIV (PLWH) have higher levels of tobacco use compared to the general population, increasing their risk for morbidity and mortality. PLWH also face potential chronic stressors related to the stigma and discrimination associated with HIV and other characteristics (e.g., race, sexual orientation). These experiences may be associated with harmful health behaviors, such as tobacco use. The purpose of the current study is to explore the psychosocial context of tobacco use in PLWH, examining avoidance coping as a mediator in the relationship between multiple forms of discrimination and tobacco use.
Setting
Participants included 202 PLWH recruited from an HIV primary care clinic in Birmingham, AL between 2013 and 2015.
Methods
Participants responded to parallel items assessing experiences of discrimination related to HIV status, race, and sexual orientation as well as items assessing avoidance coping. Data on current tobacco use were obtained from participants’ clinic records. Mediation models for each form of discrimination (HIV, race, sexual orientation) adjusting for demographic variables and the other forms of discrimination were evaluated.
Results
The indirect effect of HIV-related discrimination on likelihood of tobacco use through avoidance coping was significant, suggesting that avoidance coping mediates the association between HIV-related discrimination and tobacco use. On the other hand, the indirect effects for the other forms of discrimination were not significant.
Conclusions
Given the disparity in tobacco use in PLWH, behavioral scientists and interventionists should consider including content specific to coping with experiences of discrimination in tobacco prevention and cessation programs for PLWH.
Keywords: HIV, discrimination, tobacco use, coping, intersectional stigma
INTRODUCTION
Prevalence of tobacco use among people living with HIV (PLWH) is double that of the general population, with an estimated 42% of PLWH reporting current tobacco use versus 20% of United States (US) adults.1 Recent research also suggests that poly-tobacco use (using multiple tobacco products concurrently) is elevated in PLWH, particularly among PLWH who already smoke cigarettes.2,3 While tools for primary and secondary prevention of HIV (i.e., Pre-Exposure Prophylaxis, Treatment as Prevention) gain increasing traction in public health efforts, our attention must also focus on preventing morbidity and mortality and improving quality of life among PLWH. Tobacco use puts PLWH at increased risk for opportunistic infections, chronic obstructive pulmonary disease (COPD), community-acquired pneumonia (CAP), periodontal diseases, cardiovascular diseases, and lung cancer.4,5 Other correlates of tobacco use experienced disproportionately by PLWH include greater HIV-related symptoms, greater use of other substances, lower social support, and lower health related quality of life.6,7 Due to factors that create health disparities in both HIV and tobacco use (e.g., lower socioeconomic status, lower education attainment, access to healthcare), PLWH are both at higher risk for tobacco uptake and face unique barriers to accessing tobacco cessation resources.8 Consequently, it is important to uncover the dynamics leading to tobacco use among PLWH to enhance accessible prevention and cessation programs.
Many PLWH face the stress of living with a stigmatized health condition. Stigma - the social devaluation and rejection of people with a certain attribute - is a chronic stressor that interferes with health and well-being.9,10 Stigma can be enacted or experienced as discrimination, and those experiences can have particularly negative consequences for health.10,11 Many PLWH also face discrimination related to other characteristics including their racial and ethnic identity, or sexual orientation.11,12 Literature on intersectional stigma and discrimination - the degree to which stigmas and forms of discrimination interact with each other within individuals who are stigmatized - suggests that multiple stigmas and discrimination have negative implications for health.11,13,14 It is possible these overlapping forms of discrimination explain disparities in tobacco use. Numerous studies have documented links between experiences of discrimination among people of color and higher tobacco use prevalence.15–17 Similarly, higher rates of smoking are observed among sexual minority individuals facing structural stigma and discrimination.18–20 Intersectional discrimination likely contributes to tobacco use disparities observed in PLWH and warrants further investigation. However, little empirical data have specifically linked experiences of HIV-related discrimination to smoking.
Individuals who experience discrimination in their communities make efforts to cope with those experiences. Coping includes any efforts to deal with stressors that overwhelm one’s perceived resources.21 In the HIV literature, avoidance coping responses are consistently associated with poorer outcomes including negative affect, maladaptive health behaviors, and poorer physical health.22 Avoidance coping (also termed passive or disengagement coping) typically refers to situation specific coping responses that do not address the cause of stress (e.g., behavioral disengagement, social isolation).22,23 The uncontrollable nature of discrimination may make avoidance coping strategies a frequently used coping tool. Avoidance coping can include strategies that result in negative health behaviors like smoking,18,23 especially when other coping strategies are perceived to be out of reach or ineffective.24 In a qualitative investigation, PLWH identified smoking as a coping tool to handle stress, and they may underestimate the negative health effects of tobacco use given immediate perceived benefits.25,26 Thus, the interrelationships between discrimination, coping, and smoking are dynamic and complex.
The literature on discrimination and HIV-related health has largely focused on HIV-specific outcomes such as medication adherence and viral suppression. This investigation is novel in its examination of the relationship between experienced discrimination and tobacco use for PLWH. Furthermore, this study examines the impact of multiple forms of discrimination (HIV, race, and sexual orientation) in relation to tobacco use behavior in a clinic-based sample of PLWH in the southeastern US. The US Deep South region leads the nation in HIV diagnoses and mortality.27,28 The co-occurring epidemic of HIV stigma, in addition to other stigmas and forms of discrimination that marginalize people at risk for HIV, may in part explain these HIV disparities.27,29,30 Concurrently, the prevalence of tobacco use is higher in the south, with approximately 15 out of 100 adults reporting current tobacco use.31 That estimate increases to approximately 22 out of 100 adults in the state of Alabama.31 Finally, this study explores avoidance coping as a potential mediating mechanism in the relationship between discrimination and tobacco use. Given that discrimination has been associated with negative health outcomes, we anticipate that more frequent experiences of discrimination will be associated with greater likelihood of tobacco use, and that avoidance coping will explain the association between discrimination and tobacco use.
METHODS
Participants and Procedure
Participants included 202 patients recruited from an outpatient HIV care clinic in Birmingham, Alabama between March 2013 and January 2015. Participants were recruited for a larger study on daily experiences of living with HIV, and they were included if they were currently on an antiretroviral treatment (ART) regimen and denied current substance use (not including tobacco) at the time of recruitment.32 At scheduled study-related visits, participants provided informed consent and completed measures via computer based survey. Data on participants’ current tobacco use was abstracted from clinic records dated closest to their survey completion date. The study was approved by the Institutional Review Board at the authors’ institution.
Measures
Demographics and Health Information
Participants self-reported their age, gender, race, sexual orientation, and level of education. Demographic information was cross-checked with chart data. Participants’ most recent viral load and CD4 cell count was abstracted from their medical records. For the purpose of this study, viral load was dichotomized as undetectable (<200 copies/mL) and detectable (≥200 copies/mL).
Experiences of Discrimination
Experiences of discrimination were assessed using the Everyday Discrimination Scale.33 Participants were asked each of the 9 items on the scale (e.g., “You are treated with less respect than other people are.”), and responded how often each item happened related to their HIV status, their race, and their sexual orientation. Participants responded to each item on a scale from 1: “Never” to 6: “Almost every day.” Composite scores were calculated by taking the mean of items for each form of discrimination. Internal consistency was very good across forms of discrimination (HIV: α=.94; race: α=.90; sexual orientation: α=.93).
Avoidance Coping
The avoidance subscale of the Ways of Coping List34 was used. This subscale includes 10 items (e.g.,” I try to forget the whole thing.”), that participants responded to on a scale from 1: “I don’t do this at all.” to 5: “I do this a lot.” Participants were asked to rate each coping statement in response to thinking about the stress of having HIV. Composite scores were calculated by taking the mean of item responses. Reliability across items was acceptable in the present sample (α=.75).
Tobacco Use
History of and current tobacco use were abstracted from participant medical records based on clinic-based paperwork they completed at their medical visit closest to their survey date. Current tobacco use was dichotomized for data analyses (0 = non-user, 1 = user).
Data Analyses
Descriptive analyses were used to assess sample demographic and health characteristics. These characteristics were compared between groups based on current tobacco use documented in participant medical records. Chi-square difference tests were used to examine differences in categorical variables and one-way ANOVAs were used to test differences in continuous variables. Bivariate analyses followed to assess relationships between study variables. Next, regression analyses were used to assess the relationships between discrimination, coping, and tobacco use with Hayes’ regression-based Process macro for SPSS.35 Three mediation models were conducted (single mediator models with covariates included in the models). Each of the models assessed each of the three forms of discrimination (HIV, race, and sexual orientation) as the predictor, while controlling for the other two forms of discrimination. Relevant demographic covariates were also included in each model: age, sex, race, sexual orientation, and education. Current tobacco use was entered as a dichotomous outcome. Unstandardized beta coefficients are reported to promote interpretation of findings based on the metrics used in the study. In all statistical models, a cutoff p-value of 0.05 and confidence intervals of 95% were used to assess significant results.
RESULTS
Sample Description
Demographic and clinical characteristics of the entire sample (N=202), and by current tobacco use (n=55 users and n=147 non-users) are presented in Table 1. Participants ranged in age from 24 to 71 (M: 44.7, SD: 11.1). The majority of the sample identified as male (63%), and 65% were black or African American. A total of 52% identified as gay, lesbian, or bisexual. Only 6% reported less than a high school degree, most (40%) reported completing some college, and 9% reported completing an advanced degree. Participants had been on ART for an average of 8 years (SD: 5), mean CD4 cell counts were in a healthy range, and the vast majority 93% had suppressed viral loads. The only demographic variable that differed significantly between current tobacco users versus non-users was education attainment.
Table 1.
Description of demographic and health information for all participants recruited from HIV care clinic in Birmingham, AL, as well as differences between current tobacco users and non-users.
| Demographic and Health Characteristics | All Participants N=202 |
Tobacco Users n=55 |
Non-users n=147 |
Chi-square or ANOVA |
|---|---|---|---|---|
|
| ||||
| n (%) or M ± SD, range | n (%) or M ± SD, range | n (%) or M ± SD, range | p-value | |
| Age (M ± SD, range) | 44.7 ± 11.1, 24–71 | 45.0 ± 10.6, 24–68 | 44.6 ± 11.3, 24–71 | .828 |
| Sex | .605 | |||
| Male | 127 (63%) | 33 (60%) | 94 (64%) | |
| Female | 75 (37%) | 22 (40%) | 53 (36%) | |
| Race | .581 | |||
| African American/Black | 131 (65%) | 34 (62%) | 97 (66%) | |
| White | 71 (35%) | 21 (38%) | 50 (34%) | |
| Sexual Orientation | .694 | |||
| Gay/Lesbian/Bisexual | 105 (51%) | 31 (56%) | 74 (50%) | |
| Heterosexual/Straight | 89 (44%) | 24 (44%) | 65 (44%) | |
| Education Level | .017 | |||
| Less than HS degree | 13 (6%) | 9 (16%) | 4 (3%) | |
| HS degree or equivalent | 32 (15%) | 10 (18%) | 22 (15%) | |
| Some college | 83 (40%) | 17 (31%) | 64 (44%) | |
| Bachelor’s Degree | 43 (21%) | 11 (20%) | 33 (22%) | |
| Graduate Degree | 19 (9%) | 5 (9%) | 14 (10%) | |
| Years since starting ART | 8 ± 5, 1–20 | 10 ± 7, 1–25 | 9 ± 6, 1–26 | .230 |
| CD4 cell count | 673.0 ± 333.6, 18–1890 | 724.6 ± 374.4, 18–1611 | 653.8 ± 316.2, 69–1890 | .180 |
| Viral Load | .248 | |||
| <200 c/mL (Undetectable) | 187 (93%) | 49 (89%) | 138 (92%) | |
| ≥200 c/mL (Detectable) Use | 15 (7%) | 6 (11%) | 9 (6%) | |
| History of Tobacco | 104 (51%) | 55 (100%) | 49 (33%) | <.001 |
|
| ||||
| Study Variables | n (%) or M ± SD, range | |||
|
| ||||
| HIV Discrimination | 1.5 ± 0.7, 1–5 | 1.7 ± 0.9, 1–5 | 1.5 ± 0.7, 1–5 | .067 |
| Race Discrimination | 1.8 ± 1.0, 1–5.4 | 1.6 ± 0.9, 1–5.4 | 1.8 ± 1.1, 1–5.4 | .216 |
| Sexual Orientation Discrimination | 1.5 ± 0.9, 1–5.4 | 1.6 ± 1.0, 1–5.4 | 1.5 ± 0.8, 1–5.3 | .417 |
| Avoidance Coping | 2.1 ± 0.7, 1–4.2 | 2.4 ± 0.8, 1–4.2 | 2.0 ± 0.6, 1–4.1 | <.001 |
Note: Chi-square difference tests computed for categorical values and one-way ANOVAs computed for continuous variables.
Discrimination was endorsed with relatively low frequency, occurring fewer than one time per year on average for HIV-related discrimination (M: 1.5, SD: 0.7), race discrimination (M: 1.8, SD: 1.0), and sexual orientation discrimination (M: 1.5, SD: 0.9). In terms of coping with the stress of living with HIV, participants tended to endorse use of avoidance strategies “a little” (M: 2.1, SD: 0.7) on average. Tobacco users reported significantly greater avoidance coping compared to non-users. In bivariate analyses (Table 2), all 3 forms of stigma were positively associated with each other. All three forms of stigma were also positively associated with avoidance coping.
Table 2.
Pearson and point-biserial correlations between study variables (N=202).
| HIV Discrimination | Race Discrimination | Sexual Orientation Discrimination | Avoidance Coping | |
|---|---|---|---|---|
| Race Discrimination | .37** | --- | --- | --- |
| Sexual Orientation Discrimination | .47** | .26** | --- | --- |
| Avoidance Coping | .48** | .24* | .29** | --- |
| Tobacco Use (0=Non-user) | .13† | −.09 | .06 | .25** |
Note:
p<.001;
p<.05;
p<.10
Mediation Analyses
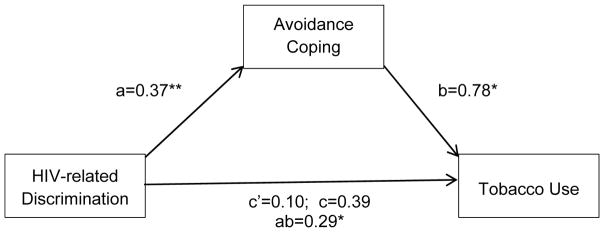
Results from multivariate analyses for all three mediation models are shown in Table 3. There was no evidence that race discrimination or sexual orientation discrimination was associated with avoidance coping, when controlling for the other forms of discrimination and demographic variables. Additionally, indirect effects were not significant for race discrimination or sexual orientation discrimination. There was a significant indirect effect of HIV-related discrimination on tobacco use, through its effect on avoidance coping (path coefficients are depicted in Figure 1). HIV-related discrimination was significantly associated with avoidance coping b(SE) = .37(.08), p<.001, 95% CI [.90, 2.59]. Avoidance coping was significantly associated with tobacco use, b(SE) = .78(.28), AOR=2.18, p=.006, 95% CI [.22, 1.34]. The odds of current tobacco use more than doubled for each point increase in avoidance coping. The bootstrap confidence intervals derived from 2000 samples indicated that the indirect effect of HIV-related discrimination on tobacco use through avoidance coping was significant b(SE) = .29(.14), 95% CI [.06, .62]. This finding suggests a significant mediation effect such that the odds of being a current smoker increase 34% for every point increase in HIV-related discrimination through its effect on avoidance coping, while controlling for demographic variables, race discrimination, and sexual orientation discrimination.
Table 3.
Multivariate analyses for three forms of discrimination on tobacco use, with mediation effect of avoidance coping.
| Outcome | ||||||||
|---|---|---|---|---|---|---|---|---|
| M (Avoidance Coping) | Y (Current Tobacco Use) | |||||||
|
| ||||||||
| Predictor | path | Coeff (SE) | p | 95% CI | path | Coeff (SE) | p | 95% CI |
| Model 1 | ||||||||
|
| ||||||||
| X (HIV Discrimination) | a | .37 (.08) | <.001 | .90 – 2.59 | C′ | .10 (.30) | .74 | −.49, .69 |
| M (Avoidance Coping) | --- | --- | --- | b | .78 (.28) | .006 | .22, 1.34 | |
| Total Effect | --- | --- | --- | c | .39 (.28) | .16 | −.15, .93 | |
| Indirect effect | --- | --- | --- | ab | .29 (.14) | .06, .62 | ||
|
| ||||||||
| Model 2 | ||||||||
|
| ||||||||
| X (Race Discrimination) | a | .03 (.06) | .58 | −.08 – .15 | c′ | −.34 (.24) | .16 | −.81, .13 |
| M (Avoidance Coping) | --- | --- | --- | b | .78 (.28) | .006 | .22, 1.34 | |
| Total Effect | --- | --- | --- | c | −.30 (.22) | .18 | −.75, .15 | |
| Indirect effect | --- | --- | --- | ab | .03 (.06) | −.07, .18 | ||
|
| ||||||||
| Model 3 | ||||||||
|
| ||||||||
| X (Sexual Orientation Discrimination) | a | .07 (.08) | .39 | −.09 – .22 | c′ | .03 (.28) | .91 | −.53, .59 |
| M (Avoidance Coping) | --- | --- | --- | b | .78 (.28) | .006 | .22, 1.34 | |
| Total Effect | --- | --- | --- | c | .08 (.28) | .78 | −.47, .63 | |
| Indirect effect | --- | --- | --- | ab | .05 (.08) | −.07, .23 | ||
Note: Indirect effects were calculated based on 2000 bootstrap samples. Coefficients are reported as unstandardized beta coefficients.
Paths a, b, c, and c′ are depicted (Model 1) in Figure 1.
The following covariates were included in all models: age, sex, race, sexual orientation, education.
Model 1 covariates also included: Race discrimination, sexual orientation discrimination.
Model 2 covariates also included: HIV discrimination, sexual orientation discrimination.
Model 3 covariates also included: HIV discrimination, race discrimination.
Figure 1.
Mediation model depicting the indirect effect of HIV-related discrimination on tobacco use through avoidance coping, controlling for age, sex, race, sexual orientation, education, racial discrimination, and sexual orientation discrimination.
Associations are presented as unstandardized path coefficients.
C′ is the direct effect, c is the total effect, ab is the indirect effect.
Statistical significance is noted as follows: **p<.001; *p<.05.
DISCUSSION
The present study examined the associations between different forms of discrimination, avoidance coping, and tobacco use in a sample of PLWH in the southeastern US. To date, reasons for the disproportionate rate of smoking in PLWH have not been well understood.36 In the present sample of PLWH recruited from an HIV clinic in Alabama, there was evidence that avoidance coping explains the relationship between HIV-related discrimination and current tobacco use, when controlling for demographic variables and other forms of discrimination (race and sexual orientation discrimination).
There has been consistent evidence of disparities in tobacco use over the course of the HIV epidemic,3,4,8,37–39 yet little progress has been seen in reducing the prevalence of use among PLWH. Thus, it is imperative to understand the factors that put PLWH at risk for tobacco use and that sustain tobacco use behavior. Results of this study suggest that HIV-related discrimination is a risk factor for tobacco use following previous research that has linked experiences of race discrimination and discrimination towards sexual minorities to tobacco use.15,16,18–20,40 Furthermore, results of the present study suggest that tobacco use is an outcome of an avoidant approach to cope with stress among people who experience discrimination.
HIV-related discrimination is related to tobacco use even when accounting for other forms of discrimination. This finding aligns with a previous investigation in which HIV-related discrimination was associated with depression when accounting for race and gender discrimination in a sample of African, Caribbean, and black women in Canada.41 One explanation Logie and colleagues made for their findings was that experiences of HIV discrimination likely varied more compared to the other forms of discrimination in their sample of women. On the other hand, Bogart and colleagues found that race discrimination predicted ART adherence when controlling for HIV and sexual orientation discrimination; and explained that African American men in their sample encounter race discrimination more because race is visible.12 It is possible that HIV-related discrimination is the most salient form of discrimination to PLWH in this sample of men and women in the southeastern US. Thus, it was HIV-related discrimination that drove the indirect effect on tobacco use compared to other forms of discrimination that have previously demonstrated associations with tobacco use. It is also possible that intersectionality (in this case, the degree to which race and sexual orientation shape one’s experience with HIV and related discrimination) makes it difficult to disentangle the unique effects of race or sexual orientation discrimination on tobacco use behavior when in the context of HIV-related discrimination.13,14
These findings should be interpreted in light of some limitations. Chiefly, these results are cross-sectional. The findings reported here are exploratory and should be interpreted as suggestions for potential causal paths that should be further investigated in prospective and longitudinal studies. Second, participants were recruited from an HIV primary care clinic in an urban area in the southeast US and may not represent the experiences of PLWH who receive care in other settings or geographical areas, or who are not connected with medical care. Tobacco use was a patient reported outcome at the clinic-level and abstracted from clinic records. As a result, the outcome is subject to social desirability bias and underreporting. Additionally, experiences of discrimination were measured in this study, and therefore these findings do not reflect effects of other dimensions of stigma (internalized stigma, anticipated stigma, community stigma) on tobacco use. Future research may help elucidate whether experiences of discrimination are unique in relation to tobacco use, or if there are differential effects of stigma dimensions on tobacco use behavior.
Three forms of discrimination were assessed using parallel items. This approach was chosen following previous research on the experiences of multiple forms of discrimination,12,41 but may reflect some response bias. Correlations between forms of discrimination were not exceedingly high in this sample, suggesting that results likely reflect participants’ true experiences. These results should be interpreted in light of participants’ perceived experiences of discrimination, rather than objective observations of discrimination. Another potential limitation is the exclusion of participants who were using other substances, as tobacco use may occur in the context of other drug use. Previous research has explored associations between HIV stigma and substance use (alcohol and stimulant use),42–44 and the present study offered the opportunity to examine associations between experiences of discrimination and tobacco use independent from other substance use. Future research should examine the roles of stigma and discrimination in polysubstance use, perhaps while also accounting for the potential stigma associated with tobacco and drug use.
These findings have implications for continued work on the implementation of stigma-reduction interventions to help address tobacco use and other health disparities among PLWH. A recent meta-analysis suggested that more rigorous empirical studies are needed, but stigma reduction interventions can have sustaining effects especially when implemented with professional samples (e.g., healthcare workers).45 Indeed, PLWH report greater likelihood of making a smoking quit attempt when it has been discussed with a health care provider.46,47 Healthcare providers stand to make greater impact on enhancing motivation to quit using tobacco when rapport is strong and they are attuned to the unique stressors their patients face.
Social and psychological determinants of tobacco use behavior must be accounted for in tobacco research and interventions. Pharmacological tobacco cessation approaches may not be sufficient in reducing tobacco use, as they do not replace the function of tobacco use behavior. Moreover, evidence for nicotine replacement and other medication therapies for tobacco cessation in PLWH is dependent upon access to therapies and motivation to quit.36 Mobile and web-based interventions have also shown good efficacy and acceptability for smoking cessation and allow for more potential access to interventions.36
Coping offers an accessible clinical focus for intervention. As such, tobacco use cessation programs can extend their reach by focusing on the unique stressors that PLWH face, and by identifying adaptive replacements for smoking that PLWH can access and use. Previous research suggests tobacco use may be a means for people to self-soothe and reduce distress in social situations where discrimination may be experienced.25 In cases where tobacco is used as a coping tool, contingencies will be needed to bolster motivation. In behavioral and motivation-based tobacco cessation approaches, the function of tobacco use should be validated; and appropriate, accessible, and effective replacements need to be addressed. Bolstering resilience coping resources may be most effective in response to HIV-related discrimination,41 as well as reducing avoidance coping approaches. Interventions appear to be most effective when they are tailored to the individual needs of PLWH, including mental health needs and socioeconomic barriers.48 The integration of psychologists, social workers, and other mental health professionals into the landscape of HIV care can help address motivation to quit, provide accessible interventions, and bolster support along with community-based resources (e.g., tobacco quit-lines, cessation groups embedded in gyms or churches) to supplement.
CONCLUSIONS
In summary, understanding unique risk factors for tobacco use among PLWH can help improve tobacco prevention and cessation programs. As we continue to see successes in reducing HIV transmission, our attention must shift to reducing morbidity and mortality among PLWH. By addressing the large disparity in tobacco use among PLWH, gains can be made in reducing acute and chronic health conditions that reduce health-related quality of life and decrease life expectancy. Future research on the associations between stigma and discrimination, coping, and tobacco use should utilize prospective and longitudinal designs to further explore the dynamics of these associations over time. At the individual-level interventionists should consider smoking as a functional behavior to cope with the potential stress of HIV-related discrimination, which may enhance tobacco prevention and cessation programs. At the structural and community level, more empirical work is needed to test the effectiveness of stigma and discrimination reduction interventions that could help reduce health disparities, including tobacco use, among PLWH.
Acknowledgments
Source of Funding
This research was supported by the University of Alabama at Birmingham Center for AIDS Research, a National Institutes of Health (NIH) funded program (P30 AI027767) that was made possible by the following institutes: NIAID, NCI, NICHD, NHLBI, NIDA, NIA, NIDDK, NIGMS, and OAR. K.B.C. and W.S.R. are supported by a T32 in Health Services and Outcomes Research (Agency for Healthcare Research and Quality [AHRQ] T32HS013852). Investigator support (B.T.) for this study was also provided by the National Institute of Mental Health (R01MH104114). The contents of this publication are the sole responsibility of the authors and do not represent the official views of the NIH or AHRQ.
Footnotes
Conflicts of Interest:
The authors have no conflicts of interest to declare.
References
- 1.Mdodo R, Frazier EL, Dube SR, et al. Cigarette smoking prevalence among adults with HIV compared with the general adult population in the United States: cross-sectional surveys. Ann Intern Med Mar 03. 2015;162(5):335–344. doi: 10.7326/M14-0954. [DOI] [PubMed] [Google Scholar]
- 2.Pacek LR, Sweitzer MM, McClernon FJ. Non-cigarette tobacco and poly-tobacco use among persons living with HIV drawn from a nationally representative sample. Drug Alcohol Depend. 2016;162:251–255. doi: 10.1016/j.drugalcdep.2016.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tamí-Maury I, Vidrine DJ, Fletcher FE, Danysh H, Arduino R, Gritz ER. Poly-Tobacco Use Among HIV-Positive Smokers: Implications for Smoking Cessation Efforts. Nicotine Tob Res. 2013;15(12):2100–2106. doi: 10.1093/ntr/ntt107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Reddy KP, Kong CY, Hyle EP, et al. Lung Cancer Mortality Associated With Smoking and Smoking Cessation Among People Living With HIV in the United States. JAMA Intern Med. 2017;177(11):1613–1621. doi: 10.1001/jamainternmed.2017.4349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Arcavi L, Benowitz NL. Cigarette smoking and infection. Arch Intern Med. 2004;164(20):2206–2216. doi: 10.1001/archinte.164.20.2206. [DOI] [PubMed] [Google Scholar]
- 6.Vidrine D. Cigarette smoking and HIV/AIDS: health implications, smoker characteristics and cessation strategies. AIDS Educ Prev. 2009;21(Suppl 3):3–13. doi: 10.1521/aeap.2009.21.3_supp.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Webb MS, Vanable PA, Carey MP, Blair DC. Cigarette smoking among HIV+ men and women: examining health, substance use, and psychosocial correlates across the smoking spectrum. J Behav Med Oct. 2007;30(5):371–383. doi: 10.1007/s10865-007-9112-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nahvi S, Cooperman NA. Review: the need for smoking cessation among HIV-positive smokers. AIDS Educ Prev. 2009;21(Suppl 3):14–27. doi: 10.1521/aeap.2009.21.3_supp.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Phelan JC, Link BG, Tehranifar P. Social conditions as fundamental causes of health inequalities: theory, evidence, and policy implications. J Health Soc Behav. 2010;51(Suppl 1):S28–S40. doi: 10.1177/0022146510383498. [DOI] [PubMed] [Google Scholar]
- 10.Earnshaw VA, Smith LR, Chaudoir SR, Amico KR, Copenhaver MM. HIV stigma mechanisms and well-being among PLWH: a test of the HIV stigma framework. AIDS Behav. 2013;17(5):1785–1795. doi: 10.1007/s10461-013-0437-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Turan B, Hatcher AM, Weiser SD, Johnson MO, Rice WS, Turan JM. Framing Mechanisms Linking HIV-Related Stigma, Adherence to Treatment, and Health Outcomes. Am J Public Health. 2017;107(6):863–869. doi: 10.2105/AJPH.2017.303744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bogart LM, Wagner GJ, Galvan FH, Klein DJ. Longitudinal relationships between antiretroviral treatment adherence and discrimination due to HIV-serostatus, race, and sexual orientation among African–American men with HIV. Ann Behav Med. 2010;40(2):184–190. doi: 10.1007/s12160-010-9200-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Logie CH, James L, Tharao W, Loutfy MR. HIV, gender, race, sexual orientation, and sex work: a qualitative study of intersectional stigma experienced by HIV-positive women in Ontario, Canada. PLoS Med. 2011;8(11):e1001124. doi: 10.1371/journal.pmed.1001124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bowleg L. The problem with the phrase women and minorities: intersectionality—an important theoretical framework for public health. Am J Public Health. 2012;102(7):1267–1273. doi: 10.2105/AJPH.2012.300750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Purnell JQ, Peppone LJ, Alcaraz K, et al. Perceived discrimination, psychological distress, and current smoking status: results from the Behavioral Risk Factor Surveillance System Reactions to Race module, 2004–2008. Am J Public Health. 2012;102(5):844–851. doi: 10.2105/AJPH.2012.300694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Corral I, Landrine H. Racial discrimination and health-promoting vs damaging behaviors among African-American adults. J Health Psychol. 2012;17(8):1176–1182. doi: 10.1177/1359105311435429. [DOI] [PubMed] [Google Scholar]
- 17.Lorenzo-Blanco EI, Cortina LM. Latino/a depression and smoking: An analysis through the lenses of culture, gender, and ethnicity. Am J Community Psychol. 2013;51(3–4):332–346. doi: 10.1007/s10464-012-9553-3. [DOI] [PubMed] [Google Scholar]
- 18.Pachankis JE, Hatzenbuehler ML, Starks TJ. The influence of structural stigma and rejection sensitivity on young sexual minority men’s daily tobacco and alcohol use. Soc Sci Med. 2014;103:67–75. doi: 10.1016/j.socscimed.2013.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Blosnich J, Lee JG, Horn K. A systematic review of the aetiology of tobacco disparities for sexual minorities. Tob Control. 2013;22(2):66–73. doi: 10.1136/tobaccocontrol-2011-050181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hatzenbuehler ML, Jun H-J, Corliss HL, Austin SB. Structural stigma and cigarette smoking in a prospective cohort study of sexual minority and heterosexual youth. Ann Behav Med. 2014;47(1):48–56. doi: 10.1007/s12160-013-9548-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lazarus RS, Folkman S. Coping and adaptation. The Handbook of Behavioral Medicine. 1984:282–325. [Google Scholar]
- 22.Moskowitz JT, Hult JR, Bussolari C, Acree M. What works in coping with HIV? A meta-analysis with implications for coping with serious illness. Psychol Bull. 2009;135(1):121–141. doi: 10.1037/a0014210. [DOI] [PubMed] [Google Scholar]
- 23.Pascoe EA, Smart Richman L. Perceived discrimination and health: a meta-analytic review. Psychol Bull. 2009;135(4):531–554. doi: 10.1037/a0016059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shadel WG, Mermelstein RJ. Cigarette smoking under stress: the role of coping expectancies among smokers in a clinic-based smoking cessation program. Health Psychol. 1993;12(6):443–450. doi: 10.1037//0278-6133.12.6.443. [DOI] [PubMed] [Google Scholar]
- 25.Reynolds NR, Neidig JL, Wewers ME. Illness representation and smoking behavior: a focus group study of HIV-positive men. J Assoc Nurses AIDS Care. 2004;15(4):37–47. doi: 10.1177/1055329003261969. [DOI] [PubMed] [Google Scholar]
- 26.Burkhalter JE, Springer CM, Chhabra R, Ostroff JS, Rapkin BD. Tobacco use and readiness to quit smoking in low-income HIV-infected persons. Nicotine Tob Res. 2005;7(4):511–522. doi: 10.1080/14622200500186064. [DOI] [PubMed] [Google Scholar]
- 27.Reif S, Safley D, McAllaster C, Wilson E, Whetten K. State of HIV in the US Deep South. J Community Health October 01. 2017;42(5):844–853. doi: 10.1007/s10900-017-0325-8. [DOI] [PubMed] [Google Scholar]
- 28.Reif S, Safley D, Wilson E, Whetten K. [Accessed October 13, 2017];HIV/AIDS in the US Deep South: Trends from 2008 to 2013. 2013 https://southernaids.files.wordpress.com/2011/10/hiv-aids-in-the-us-deep-south-trends-from-2008-2013.pdf.
- 29.Reif S, Sullivan K, Wilson E, Berger M, McAllaster C. [Accessed October 13, 2017]; [Accessed October 13, 2017];HIV/AIDS care and prevention infrastructure in the U.S. Deep South. 2016 https://southernaids.files.wordpress.com/2016/03/hiv-aids-care-and-prevention-infrastructure-in-the-u-s-deep-south1.pdf. https://southernaids.files.wordpress.com/2016/03/hiv-aids-care-and-prevention-infrastructure-in-the-u-s-deep-south1.pdf.
- 30.Darlington CK, Hutson SP. Understanding HIV-related stigma among women in the Southern United States: A literature review. AIDS Behav. 2017;21(1):12–26. doi: 10.1007/s10461-016-1504-9. [DOI] [PubMed] [Google Scholar]
- 31.CDC. [Accessed October 13, 2017];State Tobacco Activities Tracking and Evaluation (STATE) System. 2017 https://www.cdc.gov/statesystem/cigaretteuseadult.html.
- 32.Turan B, Fazeli PL, Raper JL, Mugavero MJ, Johnson MO. Social support and moment-to-moment changes in treatment self-efficacy in men living with HIV: Psychosocial moderators and clinical outcomes. Health Psychol. 2016;35(10):1126–1134. doi: 10.1037/hea0000356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Williams DR, Yu Y, Jackson JS, Anderson NB. Racial differences in physical and mental health: Socio-economic status, stress and discrimination. J Health Psychol. 1997;2(3):335–351. doi: 10.1177/135910539700200305. [DOI] [PubMed] [Google Scholar]
- 34.Vitaliano PP, Russo J, Carr JE, Maiuro RD, Becker J. The ways of coping checklist: Revision and psychometric properties. Multivariate Behav Res. 1985;20(1):3–26. doi: 10.1207/s15327906mbr2001_1. [DOI] [PubMed] [Google Scholar]
- 35.Hayes AF. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. Guilford Press; 2013. [Google Scholar]
- 36.Ledgerwood DM, Yskes R. Smoking Cessation for People Living With HIV/AIDS: A Literature Review and Synthesis. Nicotine & Tobacco Research. 2016;18(12):2177–2184. doi: 10.1093/ntr/ntw126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Niaura R, Shadel WG, Morrow K, Tashima K, Flanigan T, Abrams DB. Human immunodeficiency virus infection, AIDS, and smoking cessation: the time is now. Clin Infect Dis. 2000;31(3):808–812. doi: 10.1086/314048. [DOI] [PubMed] [Google Scholar]
- 38.Reynolds NR. Cigarette smoking and HIV: more evidence for action. AIDS Educ Prev. 2009;21(Suppl 3):106–121. doi: 10.1521/aeap.2009.21.3_supp.106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lifson AR, Lando HA. Smoking and HIV: prevalence, health risks, and cessation strategies. Curr HIV/AIDS Rep. 2012;9(3):223–230. doi: 10.1007/s11904-012-0121-0. [DOI] [PubMed] [Google Scholar]
- 40.Kendzor DE, Businelle MS, Reitzel LR, et al. Everyday discrimination is associated with nicotine dependence among African American, Latino, and White smokers. Nicotine Tob Res. 2014;16(6):633–640. doi: 10.1093/ntr/ntt198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Logie C, James L, Tharao W, Loutfy M. Associations between HIV-related stigma, racial discrimination, gender discrimination, and depression among HIV-positive African, Caribbean, and Black women in Ontario, Canada. AIDS Patient Care STDs. 2013;27(2):114–122. doi: 10.1089/apc.2012.0296. [DOI] [PubMed] [Google Scholar]
- 42.Edelman EJ, Lunze K, Cheng DM, et al. HIV Stigma and Substance Use Among HIV-Positive Russians with Risky Drinking. AIDS Behav. 2017;21(9):2618–2627. doi: 10.1007/s10461-017-1832-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lunze K, Lioznov D, Cheng DM, et al. HIV Stigma and Unhealthy Alcohol Use Among People Living with HIV in Russia. AIDS Behav. 2017;21(9):2609–2617. doi: 10.1007/s10461-017-1820-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Rendina HJ, Millar BM, Parsons JT. Situational HIV stigma and stimulant use: A day-level autoregressive cross-lagged path model among HIV-positive gay and bisexual men. Addict Behav. doi: 10.1016/j.addbeh.2018.01.003. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mak WW, Mo PK, Ma GY, Lam MY. Meta-analysis and systematic review of studies on the effectiveness of HIV stigma reduction programs. Soc Sci Med. 2017;188:30–40. doi: 10.1016/j.socscimed.2017.06.045. [DOI] [PubMed] [Google Scholar]
- 46.Berg CJ, Nehl EJ, Wang X, et al. Healthcare provider intervention on smoking and quit attempts among HIV-positive versus HIV-negative MSM smokers in Chengdu, China. AIDS Care. 2014;26(9):1201–1207. doi: 10.1080/09540121.2014.892565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Pacek LR, Rass O, Johnson MW. Positive smoking cessation-related interactions with HIV care providers increase the likelihood of interest in cessation among HIV-positive cigarette smokers. AIDS Care. 2017;10:1309–1314. doi: 10.1080/09540121.2017.1330532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Moscou-Jackson G, Commodore-Mensah Y, Farley J, DiGiacomo M. Smoking-cessation interventions in people living with HIV infection: a systematic review. J Assoc Nurses AIDS Care. 2014;25(1):32–45. doi: 10.1016/j.jana.2013.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]