Abstract
Background:
This study aims to report the changes in sunken eyes combined with blepharoptosis after levator resection.
Methods:
Analysis involved 60 eyes from 32 patients with sunken eyes combined with blepharoptosis. Advancement of the levator aponeurosis and the Müller’s muscle complex (levator resection) was performed in these patients. Area of upper eyelid sulcus (AES) was defined as the area of the upper eyelid shadow. The digital images were converted to black and white using image-processing software (Adobe Photoshop), and the AES was calculated using ImageJ software. In addition, margin reflex distance, eyebrow height (EBH), and AES were measured before and 3 months after surgery to assess the changes in the eyelids.
Results:
Preoperative AES was significantly correlated to age (P < 0.0001; r = 0.8062). Sunken eyes were remarkably improved after levator resection in all patients. Mean margin reflex distance significantly increased, whereas mean EBH and mean AES significantly decreased at 3 months after surgery (P < 0.0001). The AES change was significantly correlated to the EBH change (P < 0.0001; r = 0.5184).
Conclusions:
The principal aim of levator resection is to improve upper eyelid height and visual fields; however, this technique can alter the location of the eyebrow and upper orbital fat. The effects fill the hollowness of the upper eyelid and can remarkably improve sunken eyes.
INTRODUCTION
Sunken eye (the deepened upper eyelid sulcus or skeletonized eyes) is a cosmetic problem that results in an older and unnatural appearance. The causes of sunken eyes are decreased orbital fatty tissue due to aging,1,2 massive weight loss, trauma, surgery,3 and anti-glaucoma eye drops.4–8 In addition, age-related sunken eye is strongly associated with upper eyelid ptosis.9,10 Autologous fat grafting or orbital fat transposition had been reported to treat sunken eyes.11–15 Sunken eyes combined with blepharoptosis are often improved after blepharoptosis surgery;2,16 however, the effects were not fully documented.
Herein, we analyze the upper eyelid position and sulcus before and after levator resection and investigate the changes in sunken eyes combined with blepharoptosis.
PATIENTS AND METHODS
Subjects
This study included 60 eyes from 32 patients who had clinically significant sunken eyes combined with blepharoptosis. All patients underwent levator resection at Igo Ophthalmic Clinic, between August 2015 and February 2017. One man and 31 women with a mean age of 61.3 years (range, 39–81 years) were recruited. Twenty-nine patients had bilateral blepharoptosis, and three had unilateral blepharoptosis.
The causes of blepharoptosis in our patient cohort included the prolonged use of hard contact lens (47 eyes, 78.3%), aging (11 eyes, 18.3%), and glaucoma eye drops (2 eyes, 3.3%).
This study was conducted in accordance with the Declaration of Helsinki and with the approval of the Igo Ophthalmic Clinic’s ethical review board, and prior informed consent was obtained from each patient.
Surgical Procedures (Levator Resection)
Our surgical procedures have been previously described.17 In brief, after the eyelid was fixed with S-485 Entropion Forceps Kuhnt (Inami & Co., LTD., Tokyo, Japan), the levator aponeurosis and Müller’s muscle complex was separated and advanced by 8–10 mm at 2 points by mattress suturing using 6-0 Vicryl (Ethicon Inc., Somerville, N.J.). Intraoperative quantification was performed while the patient was sitting. After the resection of redundant skin for 5–12 mm, a double eyelid fold was formed, and the skin was closed with 6-0 nylon. Fat grafting or fat transfer was not performed in any patient.
All patients required eye drops for dry eyes during the early postoperative period, although the condition improved steadily over time, and no patients exhibited persistent postoperative lagophthalmos. Two eyes exhibited skin redundancy following surgery, and thus required additional skin dermabrasion.
Image Processing and Outcome Measures
Upper eyelid height before and after surgery was assessed using margin reflex distance-1 (MRD-1), which is defined as the distance from the central pupil reflex to the upper eyelid margin, with eyes in the primary position. Eyebrow height (EBH) is defined as the distance from the central pupil reflex to the lowest eyebrow margin in the midpupillary line. Digital images were analyzed by ImageJ software (version 1.41, NIH). The corneal diameter was used as the standard scale of 11 mm.
Area of upper eyelid sulcus (AES) is defined as the area of the upper eyelid shadow. Digital images were converted to black and white using an image-processing software (Adobe Photoshop). The threshold of black and white balance was decided where the border of cornea and conjunctiva was clear. The area of the upper eyelid shadow was manually traced, and it was automatically calculated by ImageJ software. MRD-1, EBH, and AES measurements taken preoperatively and 3 months postoperatively were compared.
Statistical Analysis
Statistical analyses were performed using JMP version 13.1 (SAS Institute Inc., Cary, N.C.). The significance of the differences between the preoperative and postoperative values of MRD-1, EBH, and AES was determined by Student’s paired t tests. P < 0.01 was considered statistically significant.
The correlation between age and preoperative values of MRD-1, EBH, and AES was analyzed by Spearman’s rank correlation coefficient. Furthermore, the correlation between the MRD-1 change and the EBH change, the MRD-1 change and the AES change, and the EBH change and the AES change was analyzed by Spearman’s rank correlation coefficient.
RESULTS
Mean (± SD) MRD-1 significantly increased from 1.06 ± 0.81 mm (range, -1 to 2 mm) preoperatively to 3.49 ± 0.46 mm (range, 2 to 4 mm) at 3 months, postoperatively (paired t test; P < 0.001). No reductions in MRD-1 were observed during follow-up in any patients.
Mean EBH significantly decreased from 21.19 ± 3.18 mm (range, 15.5–25.5 mm) preoperatively to 17.33 ± 2.96 mm (range, 11.0–24.0 mm) at 3 months, postoperatively (paired t test; P < 0.001).
Mean AES significantly decreased from 79.83 ± 56.66 mm2 (range, 20.1–258.4 mm2) preoperatively to 22.37 ± 32.88 mm2 (range, 0–167.7 mm2) at 3 months, postoperatively (paired t test; P < 0.001).
The correlation between age and preoperative values of MRD-1, EBH, and AES is presented in Figure. 1A–C. In particular, the correlation between preoperative AES is significantly correlated to age (P < 0.0001; r = 0.8062).
Fig. 1.
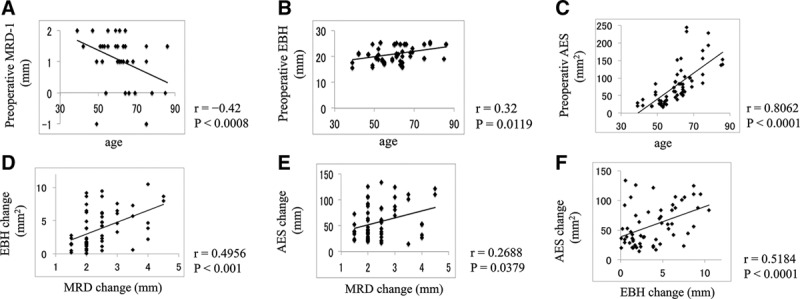
A–C, Correlation between age and preoperative values of MRD-1 (A), EBH (B), and AES (C). D–F, Correlation between the MRD-1 change and the EBH change (D), the MRD-1 change and the AES change (E), and the EBH change and the AES change (F).
The correlation between the MRD-1 change and the EBH change, the MRD-1 change and the AES change, and the EBH change and the AES change is presented in Fig. 1D–F. The EBH change is significantly and positively correlated to the MRD change (P < 0.001; r = 0.4956). The AES change is significantly and positively correlated to the EBH change (P < 0.0001; r = 0.5184).
AES are surrounded by red line in the black and white photographs (Fig. 2, Table 1). The severity of sunken eye evidently correlated with AES. AES and EBH were remarkably decreased after levator resection.
Fig. 2.
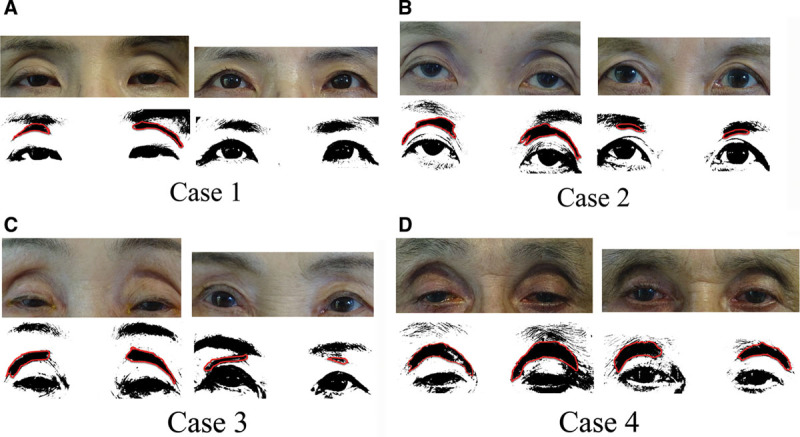
AES are surrounded by red line in the black and white photographs. The severity of sunken eye evidently correlated with AES. AES and EBH were remarkably decreased after levator resection. Case 1: A 49-year-old woman with hard contact lens wear-induced blepharoptosis (A). Case 2: A 63-year-old woman with hard contact lens wear-induced blepharoptosis (B). Case 3: A 75-year-old woman with age-related involutional blepharoptosis (C). Case 4: A 66-year-old man with glaucoma eye drops-induced blepharoptosis (D).
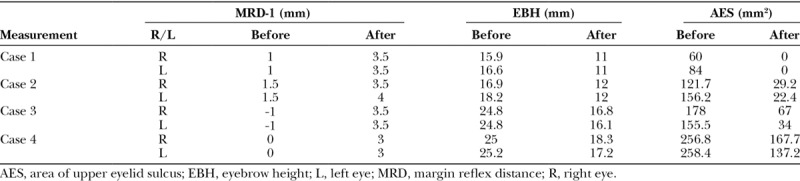
Table 1.
MRD-1, EBH, and AES before and 3 Months after Levator Resection in Cases 1–4
DISCUSSION
Our results showed that the AES before surgery are significantly and positively correlated with age, which is due to lipoatrophy and age-related decrease in the volume of upper eyelid fat.1,2,9 Patients with blepharoptosis sometimes have a deepened upper eyelid sulcus,9,10 and the sunken eyes combined with blepharoptosis are often improved after blepharoptosis surgery.2,16 Therefore, we quantitatively analyzed the change in the upper eyelid after levator resection using image-processing software (Adobe Photoshop) and image-analyzing software (ImageJ).
We measured AES as the shadow of the upper eyelid sulcus in the black and white photographs, and mean AES significantly decreased after surgery. This finding seems to occur more likely for the following reasons: First, the orbital septum attached on the levator aponeurosis18,19 and disinsertion or dehiscence of the levator aponeurosis can also cause ptosis.20 As a result, the orbital fat and orbital septum move toward the back of the eyeball, which increases the upper eyelid sulcus (Fig. 3B).10 Advancement of the levator aponeurosis and the Müller’s muscle complex causes the orbital fat and orbital septum to move forward, and we speculate that these effects fill the hollowness of the upper eyelid sulcus (Fig. 3C); second, to improve the visual fields, the position of the eyebrow in patients with blepharoptosis is significantly higher than those in healthy subjects.21 Excessive use of the frontalis muscle results in higher EBH and deep wrinkles in the forehead.16 Drooping of the eyebrow has been reported after Müller’s muscle conjunctiva resection surgery,22 levator advancement,16,23 and levator resection.24 These procedures revealed a significant reduction in brow position of almost 4 mm after ptosis surgery, and similar results were obtained in our study. In addition, we showed that the AES change is significantly and positively correlated to the EBH change. We speculate that a higher EBH makes the subcutaneous tissue thinner; subsequently, the upper eyelid sulcus becomes more evident (Fig. 3B). Therefore, the subcutaneous tissue becomes thicker after surgery, and the effects can fill the hollowness of the upper eyelid sulcus (Fig. 3C).
Fig. 3.
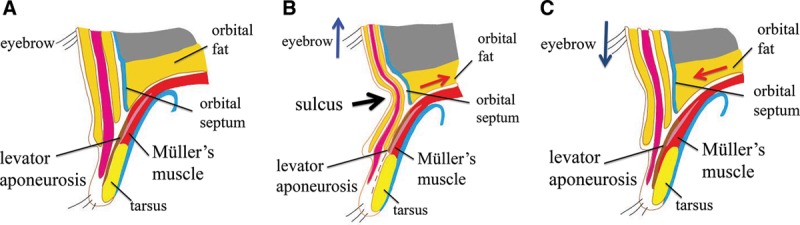
Schematic representation of the upper eyelid in normal eye (A), sunken eyes combined with blepharoptosis (B), and sunken eyes combined with blepharoptosis after levator resection (C).
Glaucoma eye drops (prostaglandin analogs) are believed to be the cause of sunken eyes combined with blepharoptosis in 2 cases. Fat atrophy can be considered a mechanism of upper eyelid sulcus deepening in patient’s using topical prostaglandin analogs.5–8 In addition, periocular muscle atrophy,25 or decreased thickness of periorbital soft tissues,26 had been reported to be associated with using prostaglandin analogs. Nakakura et al.8 reported that the sunken eye appearance can be reduced by discontinuing or switching eyedrops. However, discontinuing or switching eye drops is often difficult in cases of severe glaucoma. In case 4, measuring the intraocular pressure with the Goldmann applanation tonometer is very difficult because of tight eyelids. Therefore, blepharoptosis surgery was believed to be necessary for careful attention to intraocular pressure control in the case. As far as we know, there were no reports about the quantitative assessment of the upper eyelid sulcus in glaucoma patients. Our quantitative measurement of the upper eyelid sulcus may be useful to assess the side effects of glaucoma eye drops.
Autologous fat grafting or orbital fat transposition had been reported for the treatment of sunken eyes11–14; however, complication such as acute embolization with vision loss had been reported.27,28 Therefore, careful attention should be paid to the treatment of sunken eyes. In cases of sunken eyes combined with blepharoptosis, blepharoptosis surgeries are thought to be the first choice of treatment.
In conclusion, we quantitatively analyzed the change in the upper eyelid after levator resection and showed significant reduction of EBH and AES. The principal aim of levator resection is to improve upper eyelid height and visual fields; however, this technique can alter the location of the eyebrow and upper orbital fat. The effects fill the hollowness of the upper eyelid and can remarkably improve sunken eyes.
Footnotes
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the authors.
REFERENCES
- 1.Oh SR, Chokthaweesak W, Annunziata CC, et al. Analysis of eyelid fat pad changes with aging. Ophthal Plast Reconstr Surg. 2011;27:348–351.. [DOI] [PubMed] [Google Scholar]
- 2.Park DD. Aging Asian upper blepharoplasty and brow. Semin Plast Surg. 2015;29:188–200.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tung TC, Tsai TR, Yu CC, et al. Simultaneous fat removal with suture upper blepharoplasty. Aesthetic Plast Surg. 2012;36:842–845.. [DOI] [PubMed] [Google Scholar]
- 4.Peplinski LS, Albiani Smith K. Deepening of lid sulcus from topical bimatoprost therapy. Optom Vis Sci. 2004;81:574–577.. [DOI] [PubMed] [Google Scholar]
- 5.Park J, Cho HK, Moon JI. Changes to upper eyelid orbital fat from use of topical bimatoprost, travoprost, and latanoprost. Jpn J Ophthalmol. 2011;55:22–27.. [DOI] [PubMed] [Google Scholar]
- 6.Taketani Y, Yamagishi R, Fujishiro T, et al. Activation of the prostanoid FP receptor inhibits adipogenesis leading to deepening of the upper eyelid sulcus in prostaglandin-associated periorbitopathy. Invest Ophthalmol Vis Sci. 2014;55:1269–1276.. [DOI] [PubMed] [Google Scholar]
- 7.Jayaprakasam A, Ghazi-Nouri S. Periorbital fat atrophy—an unfamiliar side effect of prostaglandin analogues. Orbit. 2010;29:357–359.. [DOI] [PubMed] [Google Scholar]
- 8.Nakakura S, Tabuchi H, Kiuchi Y. Latanoprost therapy after sunken eyes caused by travoprost or bimatoprost. Optom Vis Sci. 2011;88:1140–1144.. [DOI] [PubMed] [Google Scholar]
- 9.Guyuron B, Harvey D. Periorbital and orbital aging: senile enophthalmos as a cause of upper eyelid ptosis. Plast Reconstr Surg. 2016;138:31e–37e.. [DOI] [PubMed] [Google Scholar]
- 10.Nakakura S, Terao E, Nagatomi N, et al. Cross-sectional study of the association between a deepening of the upper eyelid sulcus-like appearance and wide-open eyes. PLoS One. 2014;9:e96249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Maniglia JJ, Maniglia RF, Jorge dos Santos MC, et al. Surgical treatment of the sunken upper eyelid. Arch Facial Plast Surg. 2006;8:269–272.. [DOI] [PubMed] [Google Scholar]
- 12.Chen CC, Chen SN, Huang CL. Correction of sunken upper-eyelid deformity in young Asians by minimally-invasive double-eyelid procedure and simultaneous orbital fat pad repositioning: a one-year follow-up study of 250 cases. Aesthet Surg J. 2015;35:359–366.. [DOI] [PubMed] [Google Scholar]
- 13.Ciuci PM, Obagi S. Rejuvenation of the periorbital complex with autologous fat transfer: current therapy. J Oral Maxillofac Surg. 2008;66:1686–1693.. [DOI] [PubMed] [Google Scholar]
- 14.Tonnard PL, Verpaele AM, Zeltzer AA. Augmentation blepharoplasty: a review of 500 consecutive patients. Aesthet Surg J. 2013;33:341–352.. [DOI] [PubMed] [Google Scholar]
- 15.Park S, Kim B, Shin Y. Correction of superior sulcus deformity with orbital fat anatomic repositioning and fat graft applied to retro-orbicularis oculi fat for Asian eyelids. Aesthetic Plast Surg. 2011;35:162–170.. [DOI] [PubMed] [Google Scholar]
- 16.Lee JM, Lee TE, Lee H, et al. Change in brow position after upper blepharoplasty or levator advancement. J Craniofac Surg. 2012;23:434–436.. [DOI] [PubMed] [Google Scholar]
- 17.Mawatari Y, Fukushima M. Predictive images of postoperative levator resection outcome using image processing software. Clin Ophthalmol. 2016;10:1877–1881.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kakizaki H, Leibovitch I, Selva D, et al. Orbital septum attachment on the levator aponeurosis in Asians: in vivo and cadaver study. Ophthalmology. 2009;116:2031–2035.. [DOI] [PubMed] [Google Scholar]
- 19.Goldberg RA, Wu JC, Jesmanowicz A, et al. Eyelid anatomy revisited. Dynamic high-resolution magnetic resonance images of Whitnall’s ligament and upper eyelid structures with the use of a surface coil. Arch Ophthalmol. 1992;110:1598–1600.. [DOI] [PubMed] [Google Scholar]
- 20.Finsterer J. Ptosis: causes, presentation, and management. Aesthetic Plast Surg. 2003;27:193–204.. [DOI] [PubMed] [Google Scholar]
- 21.Nishihira T, Ohjimi H, Eto A. A new digital image analysis system for measuring blepharoptosis patients’ upper eyelid and eyebrow positions. Ann Plast Surg. 2014;72:209–213.. [DOI] [PubMed] [Google Scholar]
- 22.Rootman DB, Karlin J, Moore G, et al. The effect of ptosis surgery on brow position and the utility of preoperative phenylephrine testing. Ophthal Plast Reconstr Surg. 2016;32:195–198.. [DOI] [PubMed] [Google Scholar]
- 23.Zheng X, Kakizaki H, Goto T, et al. Digital analysis of eyelid features and eyebrow position following CO2 laser-assisted blepharoptosis surgery. Plast Reconstr Surg Glob Open. 2016;4:e1063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kokubo K, Katori N, Hayashi K, et al. Evaluation of the eyebrow position after levator resection. J Plast Reconstr Aesthet Surg. 2017;70:85–90.. [DOI] [PubMed] [Google Scholar]
- 25.Wang PX, Koh VT, Cheng JF. Periorbital muscle atrophy associated with topical bimatoprost therapy. Clin Ophthalmol. 2014;8:311–314.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Goh AS, Nassiri N, Kohn JC, et al. Prostaglandin eyedrops are associated with decreased thicknesses of eyelid dermis and orbicularis oculi muscle: ultrasonographic findings. Ophthal Plast Reconstr Surg. 2016;32:337–341.. [DOI] [PubMed] [Google Scholar]
- 27.Dreizen NG, Framm L. Sudden unilateral visual loss after autologous fat injection into the glabellar area. Am J Ophthalmol. 1989;107:85–87.. [DOI] [PubMed] [Google Scholar]
- 28.Lee CM, Hong IH, Park SP. Ophthalmic artery obstruction and cerebral infarction following periocular injection of autologous fat. Korean J Ophthalmol. 2011;25:358–361.. [DOI] [PMC free article] [PubMed] [Google Scholar]


