Abstract
Background:
A review of the English literature over the least 43 years revealed only a total of 53 cases of Wassel types III, IV, and VII treated by the Bilhaut–Cloquet (B–C) procedure. Furthermore, the detailed results and range of motion were only given in 2 series (a total of 9 cases).
Methods:
Four cases of Wassel types III and IV thumb duplications with zigzag deformity were treated with a modified B–C procedure. The main modification was minimal central resections at the joints aiming for joint preservation to improve the postoperative range of motion of the new thumb.
Results:
The results showed an excellent overall functional score (Tada score of 5 of 5 in all cases). The mean range of motion at the metacarpophalangeal joint was excellent (60°), but the mean at the interphalangeal joint was only 20°. Cosmetically, all thumbs were “too wide” and a panel of 3 hand surgeons scored the cosmetic result (0–10 scoring system) between 5.7 and 6.7. No secondary procedures were done, and all parents were “very satisfied” despite the wide thumbs and split nails. This was attributed to the presence of an ugly preoperative zigzag appearance, and hence the comparative postoperative appearance was satisfactory.
Conclusion:
The modified B–C procedure gives a satisfactory function, but the cosmetic outcome is suboptimal.
INTRODUCTION
There are 4 types of surgical procedures for the correction of thumb polydactyly. “Simple excision” is usually done if one of the duplicates is floating or severely hypoplastic. Most cases are treated with “reconstruction”: the larger, more-functional duplicate is retained and reconstructed using techniques such as collateral ligament reconstruction, intrinsic muscle reattachment, intrinsic tendon balancing/reinsertion and soft-tissue augmentation from the excised smaller, less-functional duplicate. The third option is the “on-top plasty,” which is best suited for duplications with one thumb being adequate proximally and the other thumb containing a superior nail and pulp distally. Finally, the Bilhaut–Cloquet (B–C) procedure is occasionally done when both thumbs are equal in length and size but neither is thought to be sufficient for reconstruction on its own. In the B–C procedure, the central parts of the duplicates are discarded, and the outer parts are combined to from the new thumb.1
The use of the B–C procedure in thumb duplication has well-known drawbacks: the new thumb tends to be wider than normal, the new nail will be ridged in the center, and there is a variable degree of stiffness at the involved joints. Some hand surgeons clearly stated that the B–C procedure should be abandoned.2,3 Others recommended the B–C procedure for Wassel types I and II duplications and not for more proximal duplication types.4 Restricting the B–C procedure for Wassel types I and II results in stiffness at the interphalangeal joint (IPJ) only, which is well tolerated. In contrast, if the procedure is done for Wassel types III and IV, the resulting stiffness at both the IPJ and metacarpophalangeal joint (MPJ) is considered unacceptable. However, several authors still advocate the B–C procedure for types III, IV, and VII duplications.5–14 Except for the stiffness, these authors noted several advantages of the B–C procedure including better joint stability, alignment, and overall function.
The senior author (MMA) has used a modified B–C procedure in 4 cases of Wassel types III and IV zigzag thumb duplications aiming to minimize the stiffness at both IPJ and MPJ. The current communication describes the modification and reports on the results of these 4 cases.
PATIENTS AND METHODS
This is a retrospective study of a total of 4 cases of zigzag thumb polydactyly types III (n = 1) and IV (n = 3) treated with a modified B–C procedure. The aim of the modification was to minimize the stiffness at the IPJ and MPJ by minimizing resections at the joints. However, the modification was expected to result in wide thumbs. This disadvantage was explained to the parents before surgery.
Surgical Technique
In type III zigzag polydactyly (Fig. 1), the central cortices of the distal phalanges are removed. A closed wedge osteotomy is done at the level of the diaphysis of proximal phalanx, and the osteotomy is fixed with a single interosseous wire. Towel clips are applied to approximate the phalanges and correct the zigzag deformity, and transverse K-wires are used to maintain this approximation. The towel clips are removed, and a thumb spica cast is applied for 3 weeks. The transverse K-wires are removed in the clinic at time of cast removal.
Fig. 1.
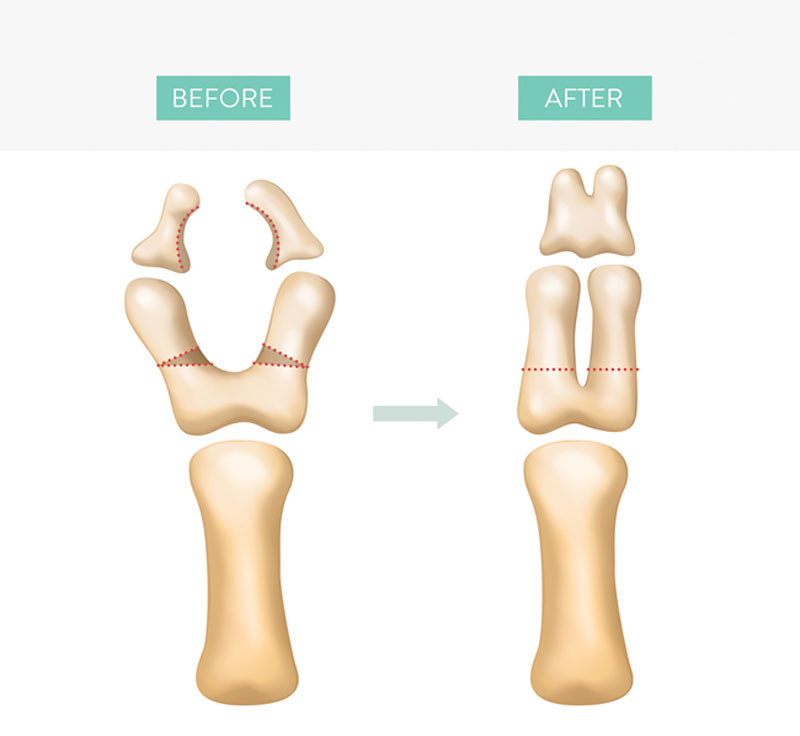
The modified B–C procedure for Wassel type III thumb polydactyly. The shaded areas are excised. Each closing wedge osteotomy is fixed with a single interosseous wire.
In type IV zigzag polydactyly (Fig. 2), the central cortices of the distal phalanges are removed. Central resections from the proximal phalanges are done at the level of the metaphysis, and lower diaphysis was also excised. Towel clips are applied to approximate the phalanges and correct the zigzag deformity, and transverse K-wires are used to maintain this approximation. The towel clips are removed, and a thumb spica cast is applied for 3 weeks. The K-wires are removed in the clinic at the time of cast removal.
Fig. 2.
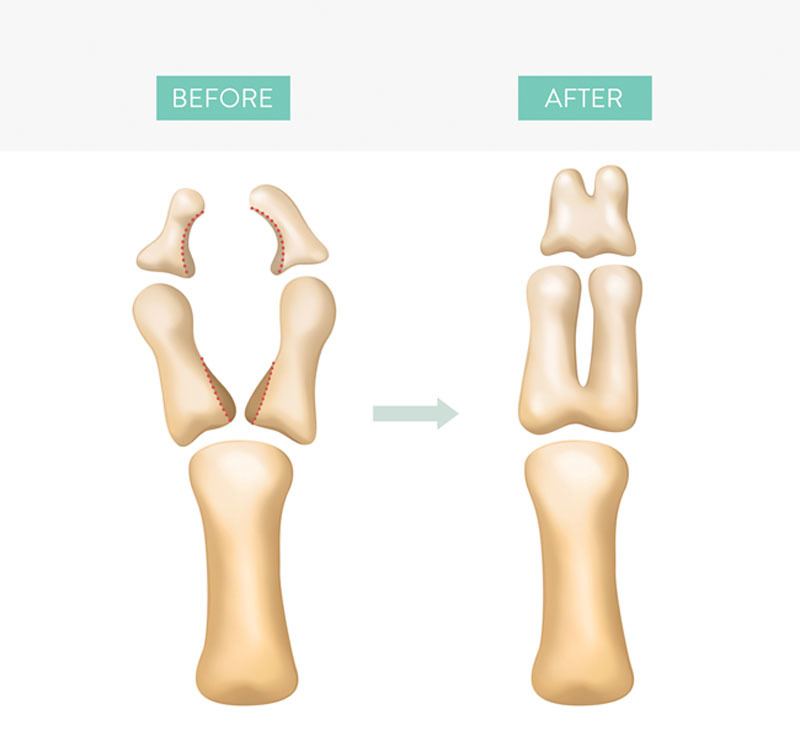
The modified B–C procedure for Wassel type IV thumb polydactyly. The shaded areas are excised.
In all cases, repair of the nail bed is done using absorbable sutures under magnification. No extrinsic tendon repositioning is done.
Assessment
Cosmetic and functional outcome measures were documented at final follow-up as shown in Tables 1 and 2. Furthermore, the overall functional outcome was measured using the scoring system of Tada et al. (1983) as shown in Table 3. Finally, the pre- and postoperative clinical and radiological illustrations of the 4 cases (Figs. 3–6) were shown to a panel of 3 hand surgeons. A list of 6 questions was given to the panel as shown in Table 4. The aim of the first 2 questions was to evaluate and score the overall cosmetic results. As mentioned in the introduction, the use of the B–C procedure for thumb polydactyly is a controversial issue. Hence, questions #3–6 were given to the panel to explore this controversial issue (Table 4). Finally, the parents were asked 2 questions regarding the use of the thumb in daily activities, and to assess the overall satisfaction as shown in Table 5.
Table 1.
Assessment of the Cosmetic Outcome
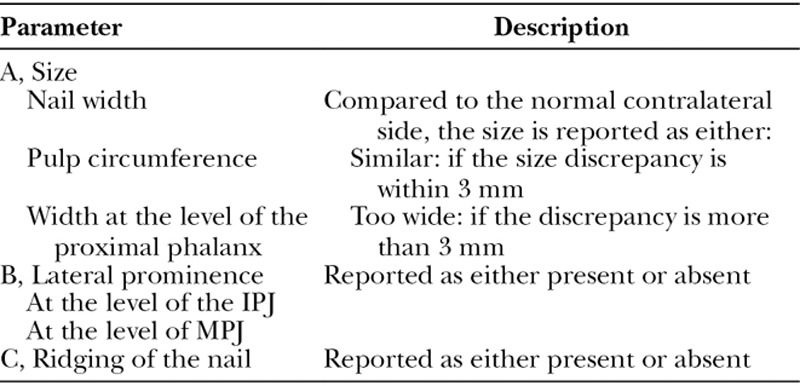
Table 2.
Functional Assessment
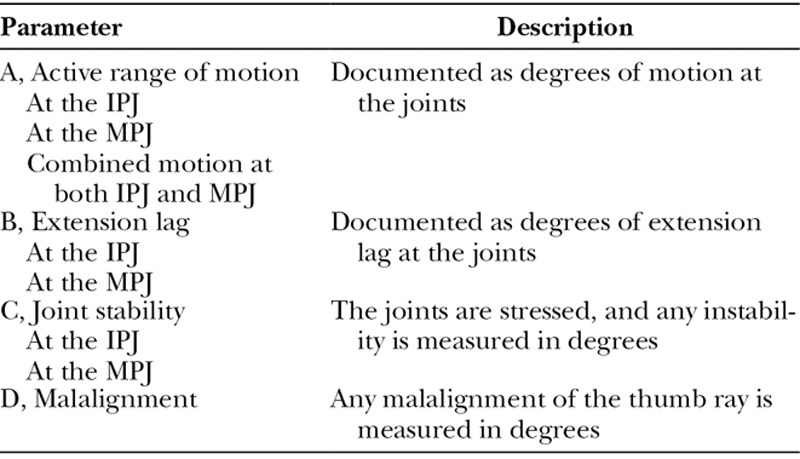
Table 3.
Tada Overall Functional Scoring for Treated Duplicate Thumbs
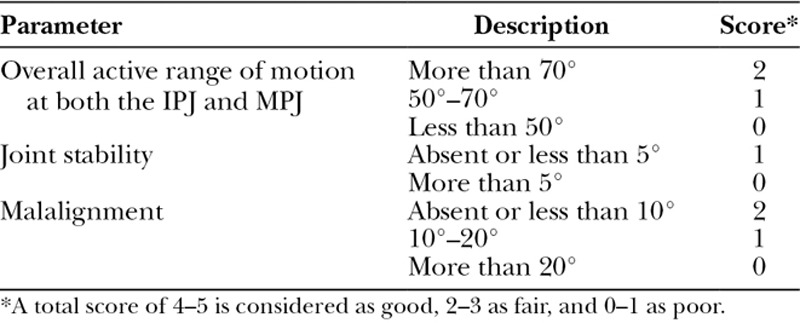
Fig. 3.

Case #1 with type IV duplication. A, Preoperative appearance, (B) marking, (C) immediate postoperative appearance, (D) final postoperative appearance, (E) preoperative X-ray, and (F) final postoperative X-ray. Note that bony union was obtained at the distal phalanges and not at the proximal phalanges.
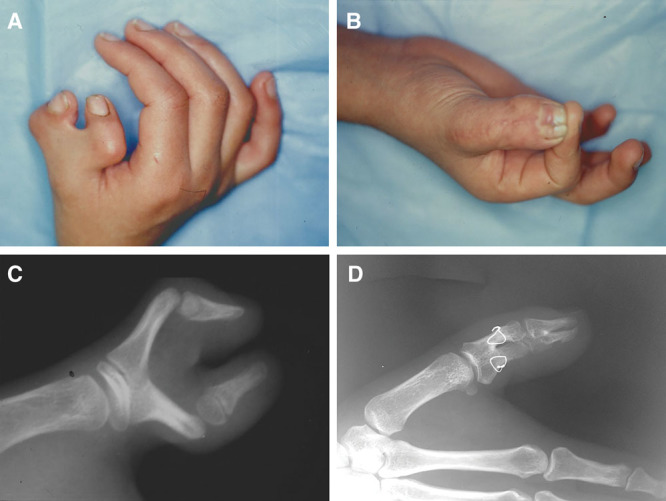
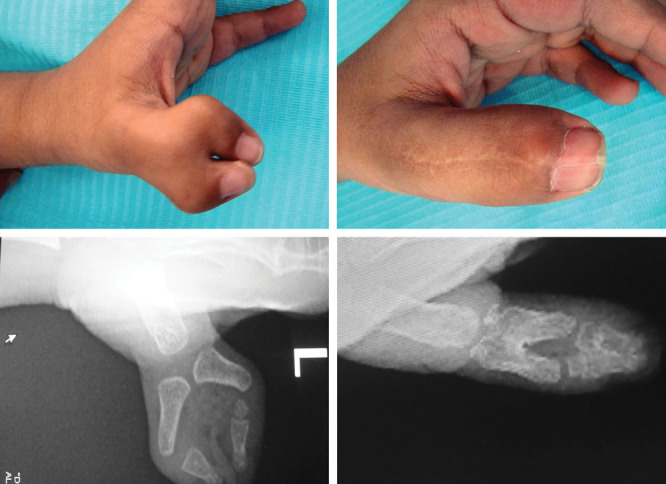
Fig. 6.

Case 4 with type IV duplication. A, Preoperative appearance, (B) final postoperative appearance, (C) preoperative X-ray, and (D) final postoperative X-ray. There was bony union at the distal phalanges only.
Table 4.
Questions Given to the Panel of Hand Surgeons
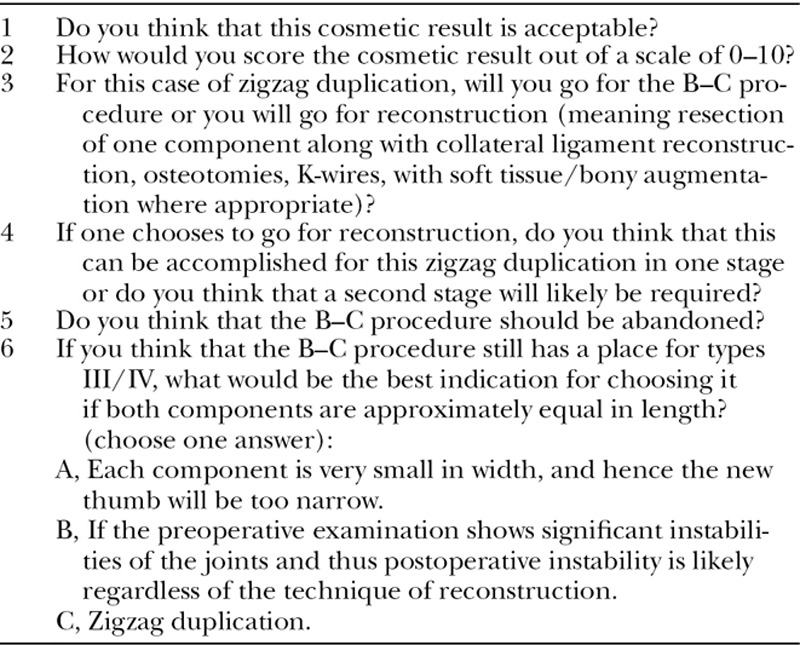
Table 5.
Questions Answered by the Parents
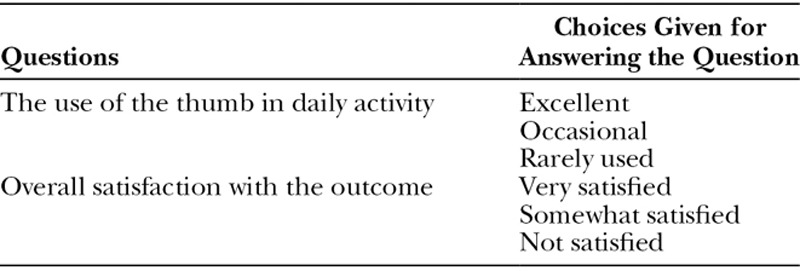
Fig. 4.
Case 2 with type III duplication. A, Preoperative appearance, (B) final postoperative appearance, (C) preoperative X-ray, and (D) final postoperative X-ray. There was bony union at the distal and proximal phalanges.
Fig. 5.
Case 3 with type IV duplication. A, Preoperative appearance, (B) final postoperative appearance, (C) preoperative X-ray, and (D) final postoperative X-ray. There was bony union at the distal and proximal phalanges.
RESULTS
Demographic data are shown in Table 6. The pre- and postoperative clinical and radiological illustrations are shown in Figures 3–6. Assessment of the cosmetic outcome (as per Table 1) was similar in all cases: all size parameters showed a discrepancy of more than 3 mm (ie, too wide). Note should be given that size comparison was not possible in case #1 because the contralateral thumb was hypoplastic, but the appearance was also judged as “too wide.” All 4 cases had lateral prominences at the IPJ. Case #2 also had a lateral prominence at the MPJ. Finally, the nail was ridged in all 4 cases.
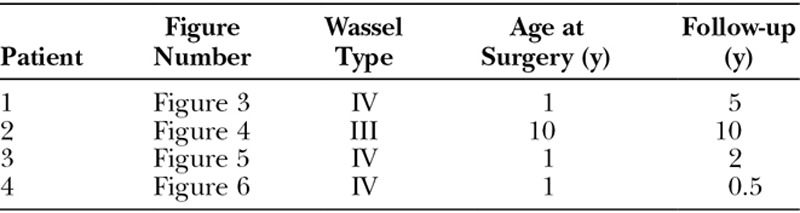
Table 6.
Demographic Data of the 4 Patients
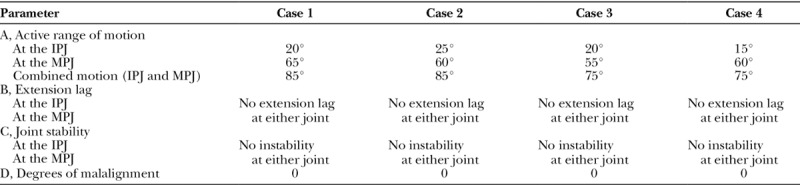
The functional results are shown in Table 7. Note should be given that none of the cases had an extension lag, joint instability, or malalignment. Because all cases showed a combined IPJ–MPJ active range of motion greater than 70° and none of the cases showed joint instability or malalignment, all cases qualified for a Tada score of 5 of 5 (as per Tada criteria3 in Table 3).
Table 7.
Functional Results in 4 Cases of Thumb Polydactyly Treated with the Modified B–C Procedure
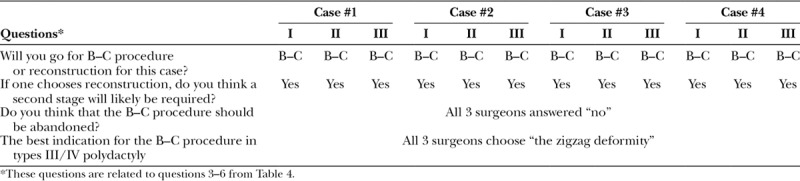
Tables 8 and 9 show the answers to the questions by the panel of hand surgeons. Although all surgeons considered the result cosmetically acceptable, the mean cosmetic scores (of 10) varied from 5.7 to 6.7 only, indicating that the overall cosmetic outcome was still suboptimal (Table 8). Table 9 shows that all 3 surgeons supported the use of the B–C procedure for the cases presented. Furthermore, all surgeons did not advocate the opinion of abandoning the B–C procedure and thought that the best indication of the procedure in Wassel types III and IV would be the zigzag deformity.
Table 8.
Assessment of the Cosmetic Results of the 4 Cases by 3 Hand Surgeons (Surgeons Are Labeled as I, II, III)
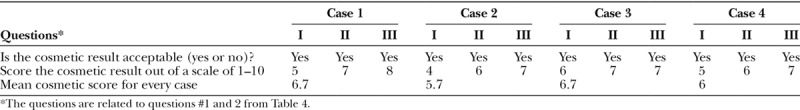
Table 9.
Panel Opinion for Questions Related to the Use of B–C Procedure in Thumb Polydactyly (the 3 Hand Surgeons in the Panel Are Labeled as I, II, III)
Finally, the parents of all cases reported the excellent use of the thumb in daily activities by all children, and all parents were “very satisfied.”
DISCUSSION
This article demonstrates an excellent functional outcome (Table 7) and a Tada functional score of 5 of 5 in all cases treated by the modified B–C procedure. Cosmetically, however, all thumbs were “too wide,” and the mean cosmetic score by the panel did not reach a score of 7 in any of the cases (Table 8). Yet, the panel thought that the overall cosmetic result is “acceptable” (Table 8), and all parents were “very satisfied” with the result. This may be due to the fact that all of our cases had an ugly zigzag deformity, and, in comparison, the postoperative appearance gives the impression of a good cosmetic outcome despite the excessive width and the split-nail appearance. We emphasize the importance of preoperative discussion with the family about what can be expected, with special attention regarding the aesthetic outcome. Furthermore, the importance of an informed consent of the possible complications, aesthetics, and long-term results/function is also emphasized in these cases.
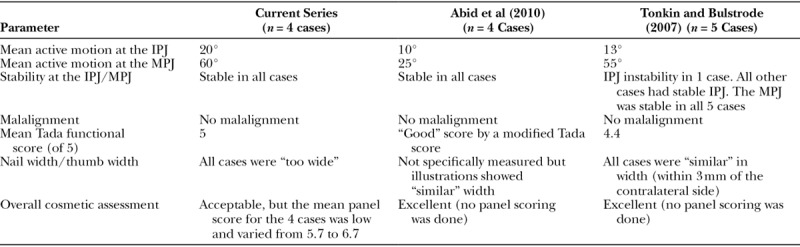
A review of the English literature over the least 43 years revealed only a total of 53 cases of Wassel types III, IV, and VII treated by the B–C procedure2,3,5,6,8,9,11,12,14–18, and these cases are summarized in Table 10. However, the detailed results and range of motion were only given in 3 series.2,5,14 Dijkman et al.2 reported the overall results in 8 cases (3 type II and 5 type IV cases) without specifying the results for the type IV cases, and hence we could not compare their results to ours. Table 11 compares our results to the results of the other 2 series.5,14 The 4 cases of Abid et al.5 had zigzag Wassel type IV thumb duplication. In all cases, only one nail was retained, and central bony excision was unequal at the distal phalanges and equal at the proximal phalanges. In the series of Tonkin and Bulstrode14 of 5 cases, 1 nail was retained (with unequal bony excision at the distal phalanges) in 1 case. The remaining 4 cases had classic B–C procedure with shared nails and equal bony excisions. However, Tonkin and Bulstrode14 made special attention to physeal matching and joint congruity to improve the range of motion. Table 11 clearly demonstrates that the cosmetic results in our series are inferior to the cosmetic results of the other 2 series. Functionally, however, our patients had better range of motion and better functional scores. The range of motion was severely restricted at both IPJ and MPJ in the series of Abid et al.5 However, the range motion was better in the series of Tonkin and Bulstrode,14 indicating that keeping special attention to joint congruity while doing the classic B–C procedure will improve the range of motion especially at the MPJ. In fact, the differences in range of motion between our series and their series are small and probably do not justify the “too wide” appearance of the thumbs in our series. The senior author has decided to stop using the modified technique and to start utilizing the Tonkin technique in future cases.
Table 10.
Wassel Types III, IV, and VII Treated by the B–C Procedure and Reported in the English Literature Since 1974
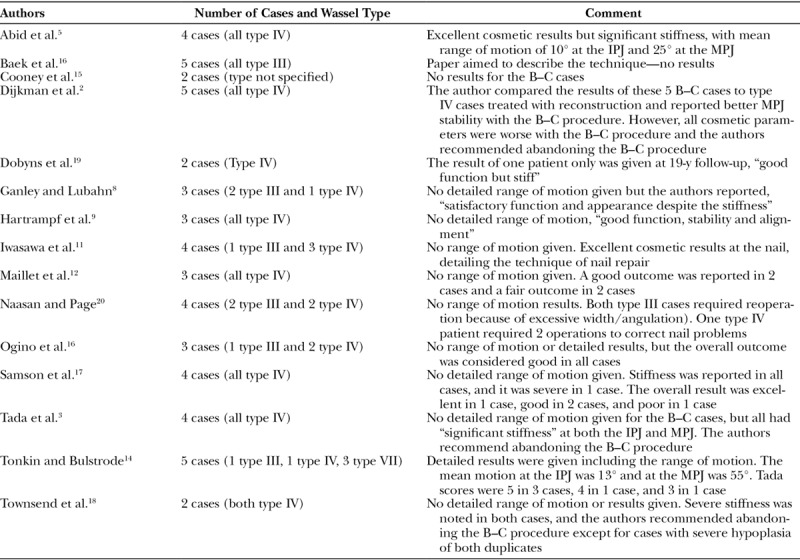
Table 11.
Comparison Between Our Results in the Current Series and the Results of Abid et al.5 and Tonkin and Bulstrode14
The senior author (MMA) believes that the main indication for using the B–C procedure in Wassel types III and IV is the presence of a zigzag deformity, and this was also the opinion of the panel. Although Wassel21 did not use the B–C procedure in his series, he stated that the B–C procedure is the best option for the zigzag deformity. Evans7 and Abid et al.5 also stressed that the B–C procedure was the technique of choice in zigzag types III and IV thumb duplications. Horii et al.22 treated 11 cases of type III thumb duplication with “reconstruction” and reported excellent results in all 11 cases, but none of the cases had a zigzag deformity. In contrast, Kawabata et al.23 treated the zigzag deformity with “reconstruction” and reported poor results (with regard to instability, malalignment, and extension log), despite doing secondary procedures in almost all patients. The need for secondary procedures if one elects to treat zigzag thumb duplications with “reconstruction” was also reported by our panel (Table 9).
Both Tada et al.3 and Dijkman et al.2 clearly stated that the B–C procedure should be abandoned. Other authors did not report a single case of B–C procedure in their series24 or only used it for types I and II duplications.4 We share the opinion of the panel (Table 9) that the B–C procedure has a place in the treatment of thumb polydactyly, and the best indication would be in zigzag deformities. Tonkin has also shown excellent results utilizing the classic B–C procedure for all types of thumb duplications.14,25
In conclusion, the aim of the modified B–C procedure in this series was to improve the range of motion, but at the expense of accepting a wide thumb. The modification obtained an excellent range of motion at the MPJ but a poor result at the IPJ. The reason for that is unclear, but it may be related to the presence of a severe preoperative joint incongruity at the IPJ. If one looks at the preoperative x-rays (Figs. 3–6), the base of the distal phalanx is articulating with the side of the head of the proximal phalanx because of the zigzag deformity. A simple joint reduction is not expected to produce a congruent IPJ. Failure to obtain a near-full range of motion and the relatively poor cosmetic outcome made the senior author decide to try the Tonkin technique in future patients with zigzag deformity and compare the results to the current series.
Footnotes
Supported by the College of Medicine Research Center, Deanship of Scientific Research, King Saud University, Riyadh, Saudi Arabia.
The study was approved by the Research Committee at Riyadh Care.
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the authors.
REFERENCES
- 1.Tonkin MA. Thumb duplication: concepts and techniques. Clin Orthop Surg. 2012;4:1–17.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dijkman RR, Selles RW, Hülsemann W, et al. A matched comparative study of the Bilhaut procedure versus resection and reconstruction for treatment of radial polydactyly types II and IV. J Hand Surg Am. 2016;41:e73–e83.. [DOI] [PubMed] [Google Scholar]
- 3.Tada K, Yonenobu K, Tsuyuguchi Y, et al. Duplication of the thumb. A retrospective review of two hundred and thirty-seven cases. J Bone Joint Surg Am. 1983;65:584–598.. [PubMed] [Google Scholar]
- 4.Andrew JG, Sykes PJ. Duplicate thumbs: a survey of results in twenty patients. J Hand Surg Br. 1988;13:50–53.. [DOI] [PubMed] [Google Scholar]
- 5.Abid A, Accadbled F, Knorr G, et al. Type IV-D thumb duplication: a new reconstruction method. Orthop Traumatol Surg Res. 2010;96:521–524.. [DOI] [PubMed] [Google Scholar]
- 6.Baek GH, Gong HS, Chung MS, et al. Modified Bilhaut-Cloquet procedure for Wassel type-II and III polydactyly of the thumb. J Bone Joint Surg Am. 2007;89:534–541.. [DOI] [PubMed] [Google Scholar]
- 7.Evans D. Polydactyly of the thumb. J Hand Surg Br. 1993;18:3–4.. [DOI] [PubMed] [Google Scholar]
- 8.Ganley TJ, Lubahn JD. Radial polydactyly: an outcome study. Ann Plast Surg. 1995;35:86–89.. [DOI] [PubMed] [Google Scholar]
- 9.Hartrampf CR, Vasconez LO, Mathes S. Construction of one good thumb from both parts of a congenitally bifid thumb. Plast Reconstr Surg. 1974;54:148–152.. [PubMed] [Google Scholar]
- 10.Iwasawa M, Hirose T. Nail plasty in the treatment of duplicated thumb. Ann Plast Surg. 1993;31:528–531.. [DOI] [PubMed] [Google Scholar]
- 11.Iwasawa M, Noguchi M, Mishima Y, et al. Long-term results of nail fusion plasty of the duplicated thumb. J Plast Reconstr Aesthet Surg. 2008;61:1085–1089.. [DOI] [PubMed] [Google Scholar]
- 12.Maillet M, Fron D, Martinot-Duquennoy V, et al. Results after surgical treatment of thumb duplication: a retrospective review of 33 thumbs. J Child Orthop. 2007;1:135–141.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ozalp T, Coşkunol E, Ozdemir O. [Thumb duplication: an analysis of 72 thumbs]. Acta Orthop Traumatol Turc. 2006;40:388–391.. [PubMed] [Google Scholar]
- 14.Tonkin MA, Bulstrode NW. The Bilhaut-Cloquet procedure for Wassel types III, IV and VII thumb duplication. J Hand Surg Eur Vol. 2007;32:684–693.. [DOI] [PubMed] [Google Scholar]
- 15.Cooney WP, Wolf J, Holtkamp K, et al. Congenital duplication of the thumb. Handchir Mikrochir Plast Chir. 2004;36:126–136.. [DOI] [PubMed] [Google Scholar]
- 16.Ogino T, Ishii S, Takahata S, et al. Long-term results of surgical treatment of thumb polydactyly. J Hand Surg Am. 1996;21:478–486.. [DOI] [PubMed] [Google Scholar]
- 17.Samson P, Salazard B, Magalon G. The “Bilhaut-Cloquet” technique for treatment of thumb duplication. Handchir Mikrochir Plast Chir. 2004;36:141–145.. [DOI] [PubMed] [Google Scholar]
- 18.Townsend DJ, Lipp EB, Jr, Chun K, et al. Thumb duplication, 66 years’ experience–a review of surgical complications. J Hand Surg Am. 1994;19:973–976.. [DOI] [PubMed] [Google Scholar]
- 19.Dobyns JH, Lipscomb PR, Cooney WP. Management of thumb duplication. Clin Orthop Relat Res. 1985; 195:26–44.. [PubMed] [Google Scholar]
- 20.Naasan A, Page RE. Duplication of the thumb. A 20-year retrospective review. J Hand Surg Br. 1994;19:355–360.. [DOI] [PubMed] [Google Scholar]
- 21.Wassel HD. The results of surgery for polydactyly of the thumb. A review. Clin Orthop Relat Res. 1969;64:175–193.. [PubMed] [Google Scholar]
- 22.Horii E, Hattori T, Koh S, et al. Reconstruction for Wassel type III radial polydactyly with two digits equal in size. J Hand Surg Am. 2009;34:1802–1807.. [DOI] [PubMed] [Google Scholar]
- 23.Kawabata H, Masatomi T, Shimada K, et al. Treatment of residual instability and extensor lag in polydactyly of the thumb. J Hand Surg Br. 1993;18:5–8.. [DOI] [PubMed] [Google Scholar]
- 24.Manske PR. Treatment of duplicated thumb using a ligamentous/periosteal flap. J Hand Surg Am. 1989;14:728–733.. [DOI] [PubMed] [Google Scholar]
- 25.Tonkin MA, Rumball KM. The Bilhaut-cloquet procedure revisited. Hand Surg. 1997; 2:67–74.. [Google Scholar]


