Abstract
Background:
Closing of defects of the lower limb after skin cancer excision poses a challenge in lower limb skin. Although the concept of relaxed skin tension lines has been established as ideal on the face, on the lower limb there remains confusion between Langer’s lines and wrinkle lines, and this study was done with the task of identifying and mapping biodynamic excisional skin tension (BEST) lines on the lower limb.
Methods:
Following studies on BEST lines elsewhere on the body, the author investigated BEST lines on the lower limb. Using a specially designed tensiometer, inherent skin tension (pretension) and wound-closing tension were studied along with the force needed to bring the wound edges together after excision of a lesion in 23 cases with defects ranging from 1.5 to 4.5 cm in diameter. Skin tension measurements of skin lines (relaxed skin tension lines (RSTL) versus BEST) and vertical closure (BEST) versus vertical closure with a parallel relaxing incision were undertaken and followed by statistical analyses utilizing the paired t test and the unpaired Student’s t tests.
Results:
BEST lines run in the vertical direction on the lower limb, that is, closure in a vertical direction resulted in a statistically significant reduction in closing tension when compared with other directions. Using a parallel relaxing incision can offer further reduction in tension, if needed.
Conclusion:
BEST lines of the lower limb are discussed, and a new technique of using parallel relaxing incisions to achieve closure of larger defects is also presented as an alternative to cutaneous flaps or grafts in the lower limb.
INTRODUCTION
The goal of lower extremity reconstruction (after skin cancer excision, for example) is the complete removal of tumors and the coverage of resultant defects, to deliver patients a healed wound and to let them resume work and leisure activities.1 When wounds are small, primary closure is feasible; however, when wounds are too large to be closed primarily, in addition to traditional partial and full-thickness skin grafts,2 halo grafts,3 perforator island flaps such as the Keystone Flap4 and reducing opposed multilobed flaps5 have been described previously. For wounds that cannot be closed primarily and the option of a local flap or skin graft is not feasible, free tissue transfer6 is sometimes employed.
Although closure of wounds under least tension is well known to result in best outcomes to do with both wound healing and scar formation, the lines of excision that result in least tension have often been contentious. It has been noted that many textbooks depict skin tension lines such as Langer’s lines differently, and there may be a “lack of science behind skin lines currently used for surgical excisions.”7
Borges8 first described the concept of using relaxed skin tension lines (RSTL) for excisions of skin lesions on the face. RSTL are based on the concept that when skin is relaxed, furrows are formed—and these lines are made more noticeable by pinching skin and noting the direction of furrows and ridges.8 However, on the rest of the body or areas such as the lower limb, Borges8 generally referred to Kraissl’s lines,9 which are essentially wrinkle lines. Recently, after studies on wound tension in surgical wounds, this author proposed the hypothesis that incisional and excisional lines need to be considered differently.10 Wrinkle lines that may be suitable for surgical incisions many not be load-bearing enough to allow them to handle the increased loads of excisional surgery.11
Although the medical view considers skin our largest organ, a biomaterial engineering perspective considers skin as a composite material that behaves elastically only at low-load levels. In areas like the lower limb and feet, due to increased weight-bearing functions, skin reveals increased viscoelastic behavior, that is, strain becomes a function of load and time.11 In sun-damaged lower limbs, although changes due to age are visible to the observer, the underlying elastin network also shows a degree of degradation over time.12
On the lower limb, especially below the knee, the consequence of improperly oriented initial excision-lines is significant, as it may mean the difference between primary closure or the need for a skin graft with its associated longer healing time and suboptimal cosmetic result. Therefore, getting the orientation of an ellipse correct while planning excisional surgery is of paramount importance. In this study, the author set out to study the best orientation of ellipses on the lower limb (below knee) for skin lesion excisions and investigated a new technique of lowering excisional wound tension using parallel relaxing incisions.
MATERIALS AND METHODS
A formal study on patients was undertaken, after obtaining all the necessary ethics approvals [New Zealand Health and Disability Ethics Committee (HDEC Reference number 15/CEN/113); Australia: University of Queensland Institutional Human Ethics (Approval No. 2015001550)]. This study was carried out in accordance with the recommendations of the ethics committees listed above, with written informed consent from all subjects. All subjects gave written informed consent in accordance with the Declaration of Helsinki. All patients presented for skin cancer surgery and were operated upon by a single surgeon (in this case the author). Twenty-one consecutive patients underwent 23 procedures. Two patients had 2 lesions (and 1 of them had identical-sized lesions on both pretibial regions allowing for a biomechanical comparison between the parallel fascia-relaxing incision and a type 1 keystone island perforator flap4 that was used on the other limb).
Surgical Procedure
This study was done using a tensiometer to measure tension after defects were cut out in a circular fashion, with no predetermined direction of closure. Once tension measurements were taken, the wound was closed in the direction that would result in the least wound tension (BEST lines). Ultimately, the study ended up a test of this hypothesis: Vertically-oriented excisions have less wound-closing tension when compared with oblique or RSTL/wrinkle line wound closures. When the wound closure was still under tension, a parallel relaxing incision was used (as detailed below). This was extended through the fascial layer only when further reduction in tension was deemed necessary by the surgeon. All cases were operated upon by 1 surgeon, the author, to ensure technical consistency.
Tensiometer
The development and design of the tensiometer used for this study (Fig. 1) have been described in detail in a previous article.10 The device is made up of 4 main elements, a linear actuator, a force sensor, signal conditioning hardware, and embedded software: The linear actuator provides a consistent force that is applied to the skin to measure wound tension, with a special focus on wound closing tension. The force sensor is a strain-element force-sensor and has a sensing range of 0–10 Newton’s (N) that has been deemed an adequate range in previous skin tension studies.10 The force needed to bring the wound edges together after a defect is created is converted to a proportional voltage potential and passed through signal conditioning software. The embedded software provides control for the linear actuator and converts the signal voltage from the force sensor into measurable tension, that is displayed on the instrument panel for ease of recording. This device is bidirectional, that is, the user can measure inward and outward forces by flicking the switch to change the direction of measurement. This allows us to measure any inherent skin tension (pretension) and understand both skin tension and relaxation lines.10
Fig. 1.

Measuring tension along different directions using a specially designed tensiometer.
Twenty-three circular lower limb defects (14 males and 9 females; age range, 50–88) with diameters ranging from 1.5 to 4.5 cm were studied as detailed in Table 1. Statistical analysis was done using unpaired Student’s t test (R programming language) as the statistical team felt it was felt the most powerful method available to test these data.
Table 1.
Wound Tension Measurements Comparing RSTL/Wrinkle Lines and Vertical Lines

Closing wound tension was measured before and after the wounds were excised in a circular fashion, and pretension was also measured before the excision (Fig. 1). The measurements were compared along the RSTL and the vertical planes because these were the 2 directions that had the 2 lowest tension measurements consistently, compared with other directions—confirming that in areas like the lower limb, skin exhibits orthotropy rather than anisotropy.
RESULTS
Twenty-one patients aged between 50 and 88 years underwent 23 operations. There were 13 males and 8 female patients. All excisions were for sizeable skin neoplasms, and the diameters of the circular defects created are noted in Table 1.
The tension force measurements are noted in Newtons (N) in Table 1. A detailed statistical analysis was undertaken. Numbers 1 and 2 were the same patient, a 69-year-old male who had a 3.5-cm lesions that could not be closed primarily over his pretibial regions. On one limb, he underwent a fascial release technique (after a vertically orientated elliptical excision) and on the other, a type 1 keystone design island perforator flap. We did not find any biomechanical advantage in a keystone flap (with its fascia-relaxing incision) when compared with a vertical closure (and a parallel fascia-relaxing incision). There were no wound infections, and one case of wound dehiscence was managed by dressings alone and did not need secondary closure.
Statistical Analyses
Detailed statistical analyses were undertaken at the statistics and mathematics sciences department. The team decided to use the paired t test (a, b, paired = TRUE) and the unpaired Student’s t test [programming software was from R Core Team (2017)].
Detailed statistical analysis using the paired t test [Student’s t distribution, t = 8.9154, df = 22, P value = 9.338e-09 (95% CI); mean of the differences, 0.4130435] showed a significant reduction in wound-closure tension using BEST lines when compared with RSTL/wrinkle lines.
A similar analysis using the paired t test [Student’s t distribution, t = 8.7781, df = 22, P value = 1.223e-08 (95% CI); mean of the differences, 0.2304348] showed an additional reduction in tension when using a parallel relaxing incision (also in the vertical plane).
The surface markings for the parallel relaxing incisions are as follows: for a medially placed incision, the line runs from the medial condyle of tibia to the medial malleolus, and for a laterally placed incision the line runs from the head of the fibula to the lateral malleolus. The site of the relaxing incisions (medial or lateral) is chosen depending on where the lesion is located (anterior or posterior), and the closest location is chosen. In general, the relaxing incision is one-third the length of the ellipse. Care is taken while making the incision through skin and fascia to avoid underlying nerves and blood vessels, and fascia is released only if the wound is unable to be closed with the parallel relaxing skin incision extending only up to the subcutis.
In all cases, the BEST lines appeared to run in a vertical direction. In summary, closure in the vertical direction, that is, orientating the ellipse vertically (Figs. 2, 3) reduced tension when compared with closure along the RSTL/wrinkle lines of the lower leg by an average of 15.82%. The study confirmed that when it comes to the lower limb, Biodynamic Excisional Skin Tension (BEST) lines (Figs. 4, 5) run in the vertical direction. There was no reduction in tension between a keystone design island perforator flap and a vertical parallel incision in the patient who had lesions of similar diameter and wound tension. However, using a parallel relaxing incision (Fig. 6) reduced tension on vertically (BEST line) closed wounds by approximately 10% (average further reduction in tension was 10.4%), indicating the usefulness of this technique, the full operative technical details of which will be the subject of another article.
Fig. 2.

Skin crease lines (RSTL) and incision along vertical (BEST) lines.
Fig. 3.

Wound closure in vertical plane (BEST lines) has least tension.
Fig. 4.
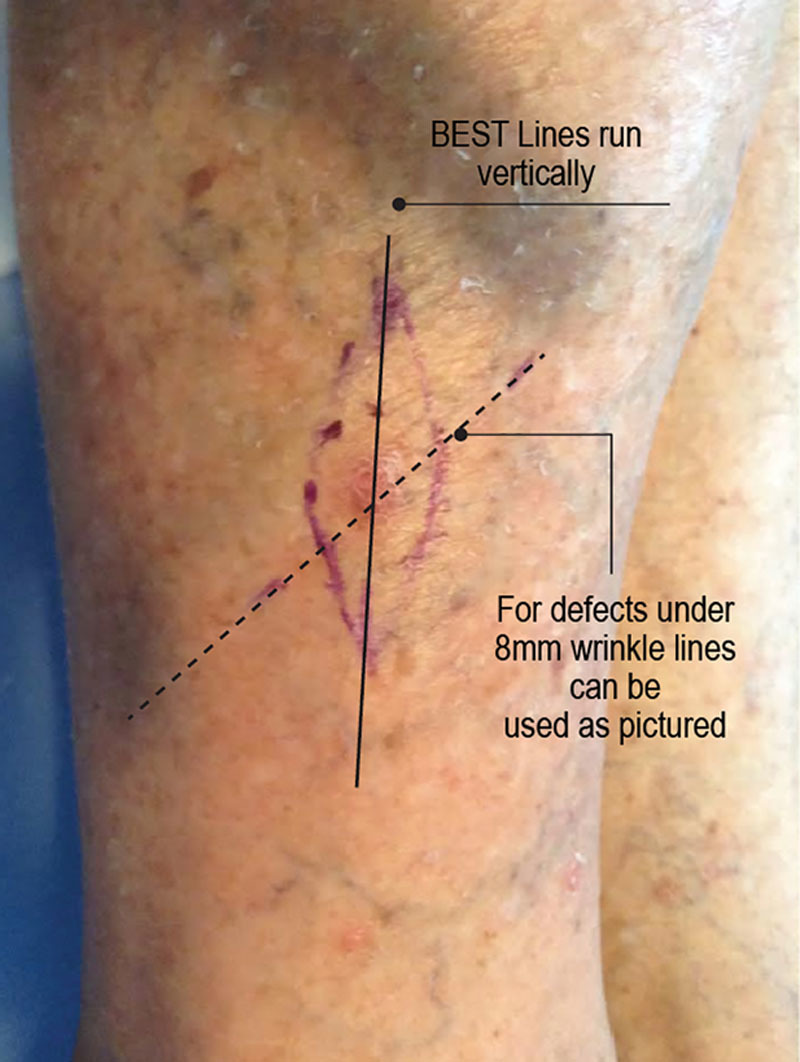
BEST lines and wrinkle/RSTL lines leg illustrated in a clinical image.
Fig. 5.

BEST lines, RSTL, and location of lesions in this study.
Fig. 6.

Elliptical excision and parallel relaxing incision technique.
DISCUSSION
Studies using this tensiometer on different body sites have already shown that under a diameter of 7–8 mm, there is very little differences in wound-closing tension.13 Although it has been often discussed that skin is anisotropic, in areas close to the bone like the pretibial region, it does exhibit orthotropy, that is, a degree of symmetry with respect to 2 normal planes, which is thought to be due to the preferential orientation of collagen fibers.14 Use of this tensiometer in other regions like the scalp also revealed a strong directional preference with regard to lowered closing tension.
Lower limb, especially below-knee skin cancer excisions pose a problem due to actinic-damaged thin skin that is friable in older patients. When incorrectly oriented ellipses are marked while planning excisions, the end result is often a skin graft with its associated poor cosmetic appearance. As authors such as Borges8 have noted, Langer’s lines were first studied in cadavers stiffened with rigor mortis so they can hardly be considered lines of relaxation.8 However, in the lower limb, Borges8 deferred to wrinkle lines. In anatomical locations other than the face, Borges’s lines indeed follow Langer’s lines, and in directions against Langer’s lines, they are impeded by the skin tension that ends up making them irregular.15 One of the other problems has been that different textbooks have marked out Langer’s lines on the lower limb differently, adding to the confusion during planning excisions.7
We used Borges method of determining RSTL, that is, pinching skin and noting both furrows and ridges—because when contour lines are produced by muscle of joint action, one only notes furrows7 and therefore this may be confusing. Using this technique, RSTL and wrinkle lines, that is, skin lines that we observe on our legs at rest seem to lie in the same oblique–horizontal plane (Fig. 4). In this study, BEST lines for wound closure were noted to be in the vertical plane (Fig. 2).
In areas like the pretibial region of the lower limb, Langer’s lines are aligned along elastin fibers—and studies have suggested that 76% of these elastin fibers are in the direction of Langer lines, and 5.1% perpendicular.16 Another study using a multiphoton microscopic camera has demonstrated that under low-load levels such as during incisional surgery, elastin stretches, and collagen buckles, the reverse of what occurs at high-load levels during excisional surgery.17 Given this differential interplay between elastin and collagen based on low and high loads of tension, the importance of differentiating incisional and excisional lines has been suggested,18 and this may be most important on the lower limb. As this study has shown, BEST lines lie in the vertical direction and are best adopted for lower limb excisional surgery. Additional reduction in tension can be afforded by using parallel relaxing incisions, and the details and the surface markings for this specific technique are detailed below.
Parallel Relaxing Incisions to Decrease Wound Tension
Anatomical studies on vascularity of the lower limb have suggested that the surgical plane lies deep to the fascia layer.19 Dye-injection studies on cadavers showed that the fascial plexus communicates with the subdermal plexus and sometimes with a vascular plexus on the underside of the deep fascia.19 Fascial release as an adjunct to wound closure has been described previously, but in the technique advocated by Dumanian et al.20, the facial release was performed via the main surgical wound, that is, these fascial releasing incisions resulted in 2 bipedicled fascial flaps attached to the overlying skin. This technique is not dissimilar to the galeal scoring technique that has been used in scalp surgery to reduce wound tension—a method that has been described as “separating components” of skin.21
One patient, a 69-year-old male, had identical 3.5-cm lesions on both legs and 1 limb; he underwent a fascial release technique (after vertical excision) and on the other, a type 1 keystone design island perforator flap. We did not find any biomechanical advantage in a keystone flap (with a fascia-relaxing incision) when compared with a vertical closure (and a parallel fascia-relaxing incision) indicating that the main advantage of the Keystone flap may not be biomechanics but vascularity. In this case, the parallel relaxing fascial incision achieved a greater reduction in tension. As detailed in the table, the use of a parallel relaxing incision reduced tension on vertically closed wounds (on average) by an additional 10.4%. Although conducting this study, the author noted that pinching the skin (the usual method advocated to find RSTL was often inaccurate indicating that the pinch technique may be unreliable on the lower limb to detect best excisional skin tension lines. Wounds that were felt to be too tight to close using the pinch method were easily closed using the parallel relaxing incision technique (Figs. 7, 8). This parallel relaxing incisional technique has the added advantage of not being limited to a specific site on the leg—as the surface markings the author has described allows the closure of both anterior and posterior leg wounds. Therefore, this technique is presented as a viable alternative to skin grafts or flap closures for difficult defects.
Fig. 7.

Clinical images of closure using BEST lines and parallel relaxing incisions.
Fig. 8.

Clinical images of closure using BEST lines and parallel relaxing incisions; the “pinch” method of assessing skin tension can lead to erroneous conclusions on the lower limb.
CONCLUSIONS
This study has confirmed that BEST lines that allow the wound to be closed under least tension lie in the vertical direction in the lower limb, and are best adopted for lower limb excisional surgery. Additional reduction in tension can be achieved by using parallel relaxing incisions, through fascia if needed, also in the vertical plane. The findings of this study suggest that the technique of using parallel relaxing incisions can help achieve the closure of lower limb defects (that cannot be closed primarily) without utilizing a flap or a skin graft, and is therefore being presented to the wider plastic surgical community.
ACKNOWLEDGMENTS
This article resulted from a study that formed part of my PhD research project at the University of Queensland’s School of Medicine, and I acknowledge my supervisors, Associate Professor Cliff Rosendahl, University of Queensland, and Professor John Windsor, University of Auckland. I thank Ryan Butler, Auckland University of Technology, for his help with photography to document this experiment and Dr Robin Hankin of the Mathematical Sciences departments of the Auckland University of Technology for help with statistical methods.
I thank Ryan Butler for his help with photography to document this experiment and Dr Robin Hankin of the Mathematical Sciences departments of the Auckland University of Technology with help with statistical methods.
Footnotes
Ethics approvals for clinical study were obtained from New Zealand Health and Disability Ethics Committee (HDEC Reference number 15/CEN/113) and University of Queensland Institutional Human Ethics (Approval No. 2015001550), Australia.
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the authors.
REFERENCES
- 1.Parrett BM, Pribaz JJ. Lower extremity reconstruction. Rev Med Clin Condes 2010; 21:66–75.. [Google Scholar]
- 2.Oganesyan G, Jarell AD, Srivastava M, et al. Efficacy and complication rates of full-thickness skin graft repair of lower extremity wounds after Mohs micrographic surgery. Dermatol Surg. 2013;9:1334–1339.. [DOI] [PubMed] [Google Scholar]
- 3.Paul SP. “Halo” grafting—a simple and effective technique of skin grafting. Dermatol Surg. 2010;36:115–119.. [DOI] [PubMed] [Google Scholar]
- 4.Behan FC. The keystone design perforator island flap in reconstructive surgery. ANZ J Surg. 2003;73:112–120.. [DOI] [PubMed] [Google Scholar]
- 5.Dixon AJ, Dixon JB. Reducing opposed multilobed flaps results in fewer complications than traditional repair techniques when closing medium-sized defects on the leg after excision of skin tumor. Dermatol Surg. 2006;32:935–942.. [DOI] [PubMed] [Google Scholar]
- 6.Miyamoto S, Kayano S, Fujiki M, et al. Early mobilization after free-flap transfer to the lower extremities: preferential use of flow-through anastomosis. Plast Reconstr Surg Glob Open. 2014;2:e127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Paul SP. Biodynamic Excisional Skin Tension (BEST) lines: revisiting Langer’s lines, skin biomechanics, current concepts in cutaneous surgery, and the (lack of) science behind skin lines used for surgical excisions. J Dermatol Res. 2017;2:77–87.. [Google Scholar]
- 8.Borges AF. Relaxed skin tension lines (RSTL) versus other skin lines. Plast Reconstr Surg. 1984;73:144–150.. [DOI] [PubMed] [Google Scholar]
- 9.Maranda EL, Heifetz R, Cortizo J, et al. Kraissl lines—a map. JAMA Dermatol. 2016;152:1014. [DOI] [PubMed] [Google Scholar]
- 10.Paul SP, Matulich J, Charlton N. A new skin tensiometer device: computational analyses to understand biodynamic excisional skin tension lines. Sci Rep. 2016;6:30117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Daly CH, Odland GF. Age-related changes in the mechanical properties of human skin. J Invest Dermatol. 1979;73:84–87.. [DOI] [PubMed] [Google Scholar]
- 12.Escoffier C, de Rigal J, Rochefort A, et al. Age-related mechanical properties of human skin: an in vivo study. J Invest Dermatol. 1989;93:353–357.. [PubMed] [Google Scholar]
- 13.Paul SP. Revisiting Langer’s lines, introducing BEST lines, and studying the biomechanics of scalp skin. Spectrum Dermatologie. 2017;2:8–11.. [Google Scholar]
- 14.Lanir Y. A structural theory for the homogeneous biaxial stress-strain relationships in flat collagenous tissues. J Biomech. 1979;12:423–436.. [DOI] [PubMed] [Google Scholar]
- 15.Barbenel JC. Serup J, Jemec GBE. Identification of Langer’s lines. In: Handbook of Non-invasive Methods and the Skin. 1995:Boca Raton, Fla.: CRC Press; 341–344.. [Google Scholar]
- 16.Zahouani H, Djaghloul M, Vargiolu R, et al. Contribution of human skin topography to the characterization of dynamic skin tension during senescence: morpho-mechanical approach. J Phys Conf Ser 2014;483:012012. [Google Scholar]
- 17.Paul SP. Are incisional and excisional skin tension lines biomechanically different? Understanding the interplay between elastin and collagen during surgical procedures. IJBM. 2017;7:111–114.. [Google Scholar]
- 18.Paul SP. The use of zigs and zags to reduce scarring over “keloid triangles” during excisional surgery: biomechanics, review and recommendations. Surg Sci. 2017;8:240–255.. [Google Scholar]
- 19.Haertsch P. The surgical plane in the leg. Br J Plast Surg. 1981;34:464–469.. [DOI] [PubMed] [Google Scholar]
- 20.Dumanian GA, Llull R, Edington H. Fascial release as an adjunct to wound closure. Br J Plast Surg. 1996;49:64–66.. [DOI] [PubMed] [Google Scholar]
- 21.Ramirez OM, Ruas E, Dellon AL. “Components separation” method for closure of abdominal-wall defects: an anatomic and clinical study. Plast Reconstr Surg. 1990;86:519–526.. [DOI] [PubMed] [Google Scholar]


