Abstract
Background:
Phalloplasty with radial forearm flap is the gold standard for female-to-male sex reassignment surgery. However, it leaves a stigmatizing forearm scar, and as the new phallus is created with the forearm’s skin and fat, it does not look like that of a biological man. The aesthetic appearance of the donor site and the neophallus can be optimized after phalloplasty. In this study, we review refinement techniques (RTs) performed after radial forearm flap phalloplasty.
Methods:
We present a historical cohort of patients who underwent the following RTs: forearm fat grafting and localized laser in the forearm’s scars, and micropigmentation of the neophallus. Patient’s aesthetic satisfaction was evaluated using the Patient and Observer Scar Assessment Scale for the forearm’s refinements and the Male Genital Self-Image Scale for the neophallus.
Results:
Between January 2014 and January 2016, 8 patients underwent forearm fat grafting with localized laser, and 7 patients micropigmentation of the neophallus after radial flap phalloplasties. All Patient and Observer Scar Assessment Scale parameters showed a statistically significant reduction between preoperative and postoperative values. Male Genital Self-Image Scale survey showed that all patients felt positively about their genitals after micropigmentation. Patients who underwent refinement procedures were highly satisfied with the aesthetic outcome and felt more confident. They also claim that they would choose to have the refinement procedure done again.
Conclusions:
The proposed RTs are minimally invasive interventions to complement and enhance female-to-male sex reassignment surgery with very few complications and excellent aesthetic results of both the forearm scars and the constructed phallus.
INTRODUCTION
Phalloplasty is the sex reassignment surgery (SRS) proposed for male transsexual patients.1 Its goal is the creation of a phallus with an adequate length and thickness, tactility and erogenous sensitivity, and a functional urethra that should allow the patient to urinate while standing.2 In addition, and due to the physiological stress in which these individuals live, it is very important to achieve the best aesthetic results, resembling as much as possible to that of a biological man.
In recent years, both patients and surgeons have been striving for perfection; there is an increased interest in surgical refinements to improve aesthetic outcomes. What is more, patients have become more demanding in terms of aesthetic results.
Currently, the radial forearm free flap (RFFF) is considered the gold standard for phalloplasty.3,4 However, it leaves a visible scar in a very exposed area of the forearm, which can be stigmatizing for the male transsexual. For the coverage of the defect, it has been published that, provided an adequate graft is taken, full- and partial-thickness skin grafts have the same short-term and long-term outcomes in the repair of the RFFF donor sites.5–7 Similarly, the largest series published up to date indicates that no significant difference was found in patient’s satisfaction when comparing the use of a split-thickness versus a full-thickness skin graft.8 Even though most patients do not complain about their forearm’s scars, which they consider a worthwhile trade-off for the creation of a phallus,8 numerous studies report that scarring defects can be responsible for social and emotional problems, especially in this population.9
Autologous fat grafting is one of the available options proposed for the correction of scar-related defects.10 This technique, as proposed by Coleman,11 consists in free fat grafting, and has a volume-increasing effect, as well as it seems to stimulate the synthesis of collagen fibers, generating an increase in dermal thickness and improving the quality of the tissue.
Another viable option to address the scarring-related defects is laser. In the case of wounds covered with skin grafts, fractionated CO2 laser has demonstrated to increase dermal thickening and to improve the overall appearance and texture of the grafted skin.12 What is more, Stephan’s group has reported satisfactory results after the use of fractional CO2 laser in binding normal and grafted skin, observing tissue remodeling and collagen formation even up to 6 months after the laser application.13 Recently, different reports have demonstrated a synergistic effect in the cosmetic outcome of scar tissue through the combined use of fat grafts and laser.14
On the other hand, it is worth mentioning that in phalloplasty with radial flap, the phallus is recreated with the patient’s forearm skin and fat, meaning that the new phallus will have a different coloring and will lack the anatomical venous structures that males have in their genital area. In regard to this, the aesthetic appreciation of the new phallus by the patients and their sexual partners is of vital importance in terms of the psyche, social life, and masculine role development of the male transsexual patient.1
In recent years, micropigmentation has been introduced in the field of aesthetic medicine to correct the defects in skin coloration or recreate anatomical structures. After female-to-male (FTM) SRS, tattooing of the glans has been widely used and well documented in the literature.15 However, tattooing the full length of the phallus, and recreating male’s anatomical structures such as the dorsal vein of the penis, has not yet been reported.
In this context, we performed this study with the aim of reviewing the following aesthetic refinement techniques after RFFF phalloplasty: free fat grafting and the application of laser for the forearm’s scars; and micropigmentation for the neophallus. Our secondary aim was to evaluate the patient’s aesthetic perception after the aforementioned techniques.
PATIENTS AND METHODS
Design
All transgender men who underwent refinement techniques after RFFF phalloplasty between January 2014 and January 2016 at Institute of Plastic Surgery Dr. Iván Mañero (IM Clinic) were included. The exclusion criteria were patients who denied undergoing the refinement techniques after SRS, and patients lost to follow up.
The refinement techniques (RTs) offered were free fat grafting plus laser for the forearm’s scars, and/or micropigmentation for the neophallus. RTs were offered after complete healing had been achieved. Complete healing was defined as complete graph take, absence of wound dehiscences in the forearm donor site and the neophallus, and spontaneous urination, with absence of fistulas.
Surgical Technique
The SRS offered to male transsexual patients was phalloplasty with RFFF, as is described in literature.8,15,16 For the formation of the phallus, in all cases a radial flap from the forearm was used, elevated in the suprafascial plane and maintaining the antebrachial fascia intact. The neophallus and the urethra were formed with the radial forearm flap, using the tube in tube technique described by Chang and Hwang, maintaining its tactility and erogenous sensitivity by arterial, venous, and nerve anastomosis. In the same surgical procedure, the glans was made through de-epithelization of a circumferentially dermal flap at the level of the balanopreputial groove, rolling it up, and suturing the free end of the flap to its own base, generating the illusion of a relief, and then placing a partial skin graft from the groin in the de-epithelized area.17 The scrotum was recreated using the skin and the fat of the labia majora, after a complete vaginectomy.
The donor sites of the forearm were covered in the same surgical procedure with laminated partial skin grafts of the thigh, placing a splint on the forearm during the first 5 postoperatory days, to avoid their mobilization.
Once complete healing was achieved for each particular case, patients were offered the possibility of undergoing one of the following aesthetic RTs: for the forearm donor site defect, fat grafting and laser of the scars; and/or micropigmentation for the neophallus.
For the forearm’s fat grafting, patients were subjected to an outpatient intervention. In all cases, fat was obtained from liposuction of the lower abdomen. Subsequently, after washing and centrifuging the obtained material, the fat was transferred onto the forearm defect, following Coleman’s technique.11 The fat was transferred to the areas previously demarcated by 1 ml Luer Lock syringes, using lipo-injection cannulas. The fatty tissue was deposited under the skin grafts and antebrachial fascia, thus recreating subcutaneous fat tissue. Patients were discharged on the same day of the intervention with analgesics and antibiotic prophylaxis. An average of three interventions was required to achieve the amount of subcutaneous fat that the surgeon considered ideal in each case.
Later, an ablative fractional laser was administered to all the patients who underwent lipofilling of the forearm. The laser used was Erbium 1540 nm. A single physician carried out all laser treatments as recommended by the manufacturer. Parameters such as fluency, pulse duration, and number of passes were the same for all patients. As clinic protocol, the first laser session was applied 30 days after the last fat grafting surgery, followed by 2 other sessions applied on a monthly basis.
Patients who fulfilled the requirements to access aesthetic RTs of the neophallus and who agreed to have the micropigmentation technique performed were referred to an outpatient appointment with a tattooist trained in micropigmentation where, in addition to providing detailed information on the technique, sterilization methods, and current and future risks of the procedure, an agreement was made on how the final result of the phallus would be. Considering that each patient is anatomically different, no standard protocol was established; the operator was responsible for technical and artistic assessment throughout the whole procedure, with constant visual feedback to reach the planned result. Micropigmentation is based on the introduction of microdrops of pigment through the skin of the phallus and above the superficial dermis using a conventional tattooing device, which supports between 3 and 23 needles capable of moving at a speed of between 100 and 150 cps. It is a minimally invasive technique, carried out in outpatient clinics without the need of analgesia and with an extremely low complication rate, within which hypersensitivity to pigment, local infections in the site of puncture, and transmissions of infectious diseases stand out. The technique ends when the agreed aesthetic result has been achieved. More than 1 session may be required to achieve the optimal results.
Aesthetic Assessment of RTs
Patients who completed either of the RTs were scheduled for outpatient clinic visits at the 1st, 3rd, 6th, and 12th postoperatory months.
To rate the patient’s satisfaction with the aesthetic RTs employed, we used the Patient and Observer Scar Assessment Scale (POSAS v2.0) before and after the forearm’s RTs, and the Male Genital Self-Image Scale (MGSIS) after the micropigmentation of the phallus. Postoperatory evaluations were performed at the 3rd month follow-up visit.
The POSAS is a suitable, reliable, and complete scar evaluation tool. It consists of 2 scales, the patient scale (PSAS) and the observer scale (OSAS). The patient scores the following scar characteristics: color, pliability, thickness, relief, itching and pain, whereas the observer scores scar vascularization, pigmentation, pliability, thickness, and relief. Each item has a 10-step score, whereby the score 10 reflects the worst imaginable scar or sensation, and 1 reflects normal skin.18
The MGSIS conceptualizes male genital self-image as a construct primarily defined by appearance. The patient answers a survey considering his feelings about his genitals, and scores whether he strongly agrees, agrees, disagrees, or strongly disagrees with each one of the parameters.
Statistical Analysis
We used the program SPSS, version 20 for database and statistical analysis. The median and interquartile range (IQR) was used to describe quantitative variables. POSAS pre- and postoperative values were studied using a nonparametric test (Wilcoxon for paired samples). P values less than 0.05 were considered statistically significant.
Before the inclusion, all patients were duly informed of the study and signed the consent form for their inclusion.
RESULTS
From January 2010 to January 2014, 33 radial forearm free flap phalloplasties were performed at Ivan Mañero Clinic, Barcelona, Spain. Six patients were lost to follow-up. Overall, 20 patients had achieved complete healing by January 2014. Seven patients had urinary fistulas and were waiting either for its spontaneous resolution or for a secondary surgery. The median time from phalloplasty to complete healing was 7 (5–10) months.
From January 2014 to January 2016, 8 patients underwent the forearm’s RTs, and 7 patients micropigmentation of the neophallus after radial forearm free flap phalloplasty.
Refinement Techniques
After signing the corresponding informed consent form, eight patients were submitted to the aesthetic RTs of the forearm. Five of the 8 patients required 3 free fat grafting interventions to achieve the desired aesthetic result and 3 patients required 4 interventions. All the patients completed 3 fractional CO2 laser sessions. The first laser session was applied at least 30 days after the first outpatient intervention for a fat graft on the forearm, and the 2 following ones on a monthly basis.
Seven patients underwent the neophallus micropigmentation technique. Five patients completed the agreed objective in a single session, whereas the other 2 needed 2 sessions for its completion.
The median follow-up time after the aesthetic RTs was 9 months (IQR 6–10) after the last laser session for the donor site, and 7 months (IQR 5–10) for the neophallus.
No additional complications deriving from the use of neither fat free grafting nor micropigmentation were observed.
Evaluation of Aesthetic Satisfaction
All patients that were submitted to an RT completed the surveys.
In terms of the patient’s perception of the forearm’s scar, the PSAS revealed that after the Coleman and laser, the overall patient’s opinion of the defect compared with normal skin ranked from 2 to 5 (being 1 “as normal skin” and 10 “very different to normal skin”). None of the patients suffered from pain or itch the weeks before the evaluation. All PSAS parameters except itching and pain revealed a statistically significant reduction between preoperative and postoperative values. Itching and pain were not evaluated because neither of them was present before the RTs (Table 1).
Table 1.
Patient Scar Assessment Scale: Preoperative, Postoperative, and P Values
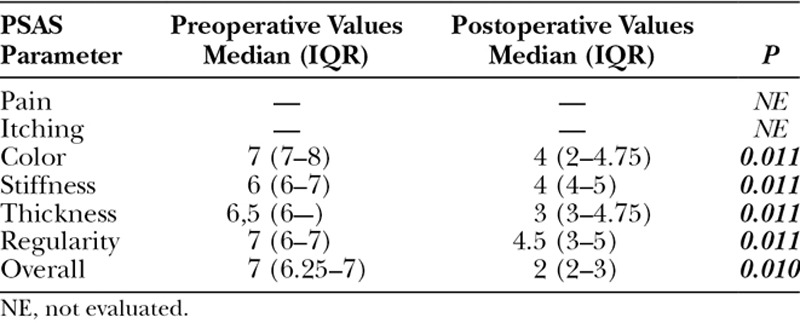
The same day, 1 observer completed the OSAS for each one of the patients. The overall opinion after the forearm’s RTs correlated well with the patient’s perception, ranking from 2 to 3. What is more, a significant reduction of all the OSAS parameters between preoperative and postoperative values was detected (Table 2, Figs. 1–3).
Table 2.
Observer Scar Assessment Scale: Preoperative, Postoperative, and P Values
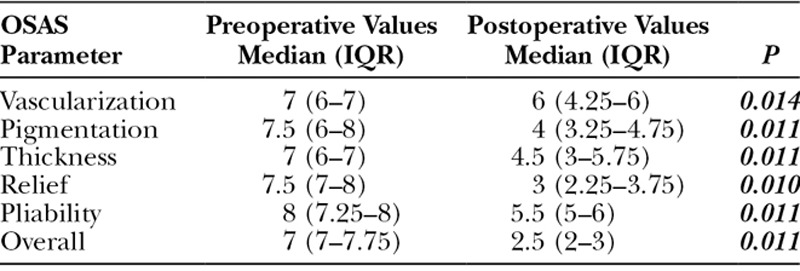
Fig. 1.
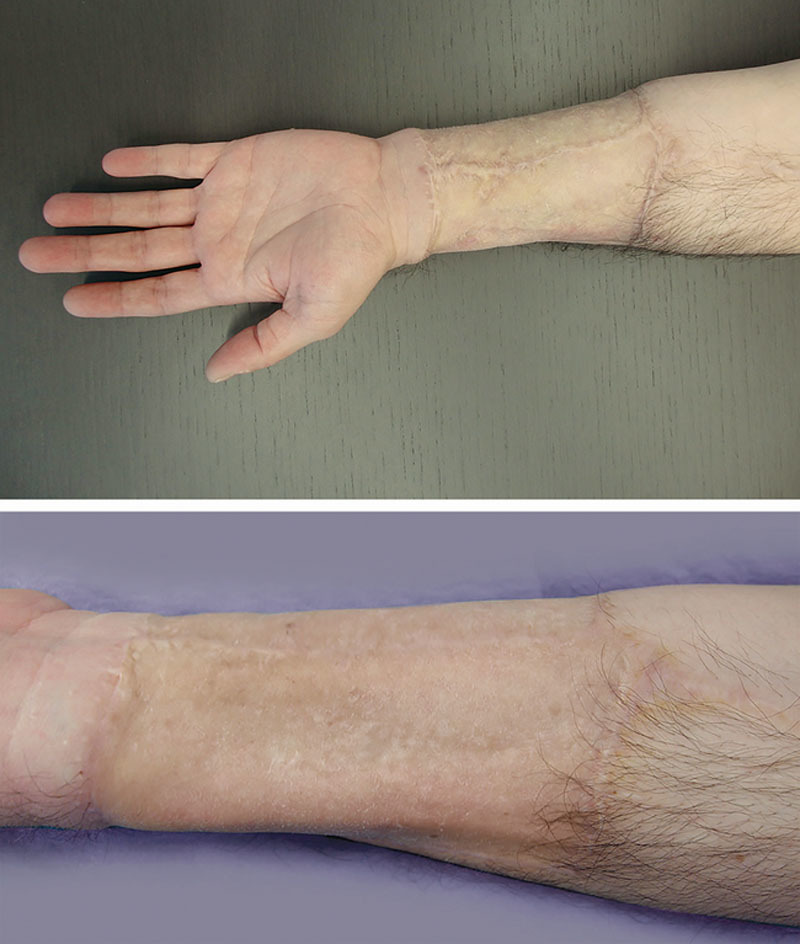
Forearm before and after Coleman + laser.
Fig. 3.

Forearm before and after Coleman + laser.
Fig. 2.

Forearm before and after Coleman + laser.
In addition, for the neophallus RT, MGSIS surveys after micropigmentation showed that all 7 patients who had undergone micropigmentation strongly agreed that they felt positively about their genitals and that they were satisfied with the appearance of their genitals (Table 3).
Table 3.
Male Genital Self-Image Scale
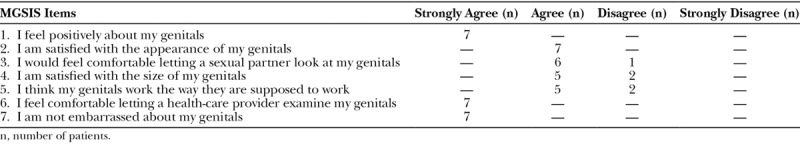
We did not do any assessment before the phallus micropigmentation. However, patients referred that they were uncomfortable with the idea of sharing showers with other men, or going to the sauna before the aforementioned technique, feelings that they did not experience afterward (Fig. 4).
Fig. 4.
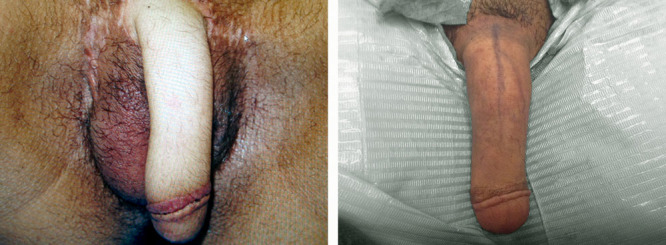
Phallus before and after micropigmentation.
All the patients who underwent an aesthetic RT assured that they would have it done again and that they currently feel more confident with their partners and in the social performance of their masculine role.
DISCUSSION
Our study has reviewed 3 aesthetic RTs after phalloplasty with RFFF in male transsexual patients, analyzing the patient’s aesthetic perception before and after the procedures.
Among our historical group of patients, 8 patients had fat grafting and laser on the scars in the donor site defect of the forearm. In all the cases, both interventions were performed on an outpatient basis and no inherent complications have been registered. When analyzing the scores given to the forearm’s scars by both clinician and patient, we detected a significant reduction of all POSAS parameters evaluated between preoperative and postoperative values, meaning that the overall aesthetic appearance of the donor site had been optimized. Consistently with prior published articles, our patients did not experience major functional problems such as bone fractures, chronic pain, itch and cold intolerance after RFFF, and, therefore, we did not evaluate those parameters.8
Our group considers that fat grafting above the skin grafts, ideally between the antebrachial fascia and the muscle, allows the hollow of the defect to be reduced, restoring volume deficits. It also contributes to better skin elasticity, increasing its thickness and, consequently, improving the forearm aesthetic outcome.
Laser application after fat grafting may have contributed to unify the coloration defects of the scars. Micro-perforations created by the laser may cause an increase in pliability of the scar tissue itself, which may be subsequently remodeled by the surrounding unaffected skin within the treatment area. Some studies have analyzed the histological impacts of fractional CO2 laser, where they distinguished areas of fibrosis, indicating new collagen formation was found after a single treatment session.19 In fact, procollagen chaperones like HSP70 and HSP47 that promote neocollagenesis rise after laser resurfacing and are responsible for the long-term efficacy of fractional CO2 laser.12 Thus, fractional CO2 laser could have allowed dermal thickening and improvement of the skin graft’s overall appearance and texture.
Likewise, micropigmentation of the phallus was performed in 7 patients, and the MGSIS scores after that RT were overall satisfactory. Even though we did not evaluate the patient’s perception before micropigmentation, all patients agreed that they did not feel comfortable about their genitals when going to saunas or showering with other men before the aforementioned technique, and that they now feel more confident with their genitals and masculine role development. We are aware that many surgeons perform tattooing of the glans immediately after phalloplasty, ideally before sensation returns to the penis.15 However, we added an additional aesthetic benefit when tattooing the whole length of the phallus, as well as recreating the dorsal vein of the penis. Micropigmentation may represent a nonsurgical therapeutic option for reducing the aesthetic defects of the neophallus. However, the longevity of the tattoo can vary depending on the place of the pigment deposit while its coloration depends on external factors, such as direct exposure from ultraviolet rays.20
One of the limitations of this study is the low number of cases in which we have been able to perform aesthetic RTs and hence, statistics have to be cautiously interpreted. This could be owed to the fact that it is a retrospective cohort and we had a high percentage of patients lost to follow-up after RFFF phalloplasty. On the other hand, some studies have shown that female-to-male transsexuals are very accepting of the donor-site scar, which they consider a worthwhile trade-off for the creation of a phallus,8 with over 75% of transsexual men being satisfied or neutral with the appearance of the scar.4 Following this line of thought, a self-selection bias could be accounted for, as only patients who were not satisfied with the donor site scar opted for these refinements. Second, the POSAS may be considered a subjective evaluation tool. Nevertheless, it is one of the most worldwide-used scales for the evaluation of the effectiveness of scar therapies. Regarding the MGSIS, it conceptualizes male genital self-image as a construct primarily defined by appearance. However, it can potentially miss other domains (such as function) that may influence the global genital self-image.21 Another limitation is the short-term follow-up after the RTs employed, which was 9 months for the forearm fat grafting and laser of the scars, and 7 months for the micropigmentation of the neophallus. In regard to this point, it is pertinent to remark that, although our patients have shown to be highly satisfied with the results of the aesthetic refinements offered, we do not know with any accuracy how long their effects will last.
Our work describes 3 aesthetic refinement techniques after phalloplasty with radial forearm flap, which have shown to improve the final aesthetic impression of both the phallus and the donor site. We consider that the visible scar in the donor site of the forearm could be perceived as a stigmatizing condition for male transsexuals. Furthermore, the aesthetic appearance of the neophallus is very important for the intimacy and masculine role development of the patients. Hence, disguising the forearms scars and making the neophallus as similar as possible to that of an XY could be offered to those patients who are not satisfied with their aesthetic appreciation after RFFF phalloplasty.
Finally, we consider further studies with larger cohorts and longer follow-up times to be important, in which aspects such as the durability of results, the complications of these interventions, and their long-term benefits should be evaluated.
CONCLUSIONS
The proposed RTs tend to improve the aesthetic appearance of both the forearm scar and the constructed phallus after SRS for female-to-male transgenders. Fat grafting plus laser and micro-pigmentation are effective minimally invasive techniques to complement female-to-male reassignment surgery with very low complications and high satisfaction rate. Aesthetic surgeons should continuously push the boundaries to optimize the patient’s quality of life.
ACKNOWLEDGMENT
We thank Dr. Ezequiel Mauro for comments that greatly improved our manuscript.
Footnotes
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the authors.
REFERENCES
- 1.Selvaggi G, Dhejne C, Landen M, et al. The 2011 WPATH standards of care and penile reconstruction in female-to-male transsexual individuals. Adv Urol. 2012;2012:581712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Monstrey SJ, Ceulemans P, Hoebeke P. Sex reassignment surgery in the female-to-male transsexual. Semin Plast Surg. 2011;25:229–244.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Monstrey S, Hoebeke P, Selvaggi G, et al. Penile reconstruction: is the radial forearm flap really the standard technique? Plast Reconstr Surg. 2009;124:510–518.. [DOI] [PubMed] [Google Scholar]
- 4.Van Caenegem E, Verhaeghe E, Taes Y, et al. Long-term evaluation of donor-site morbidity after radial forearm flap phalloplasty for transsexual men. J Sex Med. 2013;10:1644–1651.. [DOI] [PubMed] [Google Scholar]
- 5.Zuidam JM, Coert JH, Hofer SOP. Closure of the donor site of the free radial forearm flap: a comparison of full-thickness graft and split-thickness skin graft. Ann Plast Surg. 2005;55(6):612–616.. Available at: http://www.ncbi.nlm.nih.gov/pubmed/16327462. Accessed March 12, 2017. [DOI] [PubMed] [Google Scholar]
- 6.Sidebottom AJ, Stevens L, Moore M, et al. Repair of the radial free flap donor site with full or partial thickness skin grafts. A prospective randomised controlled trial. Int J Oral Maxillofac Surg. 2000;29(3):194–197.. Available at: http://www.ncbi.nlm.nih.gov/pubmed/10970081. Accessed March 12, 2017. [PubMed] [Google Scholar]
- 7.Ho T, Couch M, Carson K, et al. Radial forearm free flap donor site outcomes comparison by closure methods. Otolaryngol Head Neck Surg. 2006;134:309–315.. [DOI] [PubMed] [Google Scholar]
- 8.Selvaggi G, Monstrey S, Hoebeke P, et al. Donor-site morbidity of the radial forearm free flap after 125 phalloplasties in gender identity disorder. Plast Reconstr Surg. 2006;118:1171–1177.. [DOI] [PubMed] [Google Scholar]
- 9.Negenborn VL, Groen JW, Smit JM, et al. The use of autologous fat grafting for treatment of scar tissue and scar-related conditions: a systematic review. Plast Surg Nurs. 2016;36:131–143.. [DOI] [PubMed] [Google Scholar]
- 10.Klinger M, Caviggioli F, Klinger FM, et al. Autologous fat graft in scar treatment. J Craniofac Surg. 2013;24:1610–1615.. [DOI] [PubMed] [Google Scholar]
- 11.Coleman WP. Fat transplantation. Dermatol Clin. 1999;17(4):891–898, viii.. Available at: http://www.ncbi.nlm.nih.gov/pubmed/10526719. Accessed March 12, 2017. [DOI] [PubMed] [Google Scholar]
- 12.Katz B. Efficacy of a new fractional CO2 laser in the treatment of photodamage and acne scarring. Dermatol Ther. 2010;23:403–406.. [DOI] [PubMed] [Google Scholar]
- 13.Stephan FE, Habre MB, Helou JF, et al. Fractional CO2 laser treatment for a skin graft. J Cosmet Laser Ther. 2016;18:46–47.. [DOI] [PubMed] [Google Scholar]
- 14.Nita AC, Orzan OA, Filipescu M, Jianu D. Fat graft, laser CO2 and platelet-rich-plasma synergy in scars treatment. J Med Life. 2013;6(4):430–433.. Available at: http://www.ncbi.nlm.nih.gov/pubmed/24868255. Accessed March 12, 2017. [PMC free article] [PubMed] [Google Scholar]
- 15.Doornaert M, Hoebeke P, Ceulemans P, et al. Penile reconstruction with the radial forearm flap: an update. Handchir Mikrochir Plast Chir. 2011;43:208–214.. [DOI] [PubMed] [Google Scholar]
- 16.Chang TS, Hwang WY. Forearm flap in one-stage reconstruction of the penis. Plast Reconstr Surg. 1984;74(2):251–258.. Available at: http://www.ncbi.nlm.nih.gov/pubmed/6463150. Accessed March 12, 2017. [DOI] [PubMed] [Google Scholar]
- 17.Horton CE, Dean JA. Reconstruction of traumatically acquired defects of the phallus. World J Surg. 14(6):757–762.. Available at: http://www.ncbi.nlm.nih.gov/pubmed/2256347. Accessed March 12, 2017. [DOI] [PubMed] [Google Scholar]
- 18.Draaijers LJ, Tempelman FRH, Botman YAM, et al. The patient and observer scar assessment scale: a reliable and feasible tool for scar evaluation. Plast Reconstr Surg. 2004;113(7):1960-5 Available at: http://www.ncbi.nlm.nih.gov/pubmed/15253184. Accessed March 12, 2017. [DOI] [PubMed] [Google Scholar]
- 19.Magnani LR, Schweiger ES. Fractional CO2 lasers for the treatment of atrophic acne scars: a review of the literature. J Cosmet Laser Ther. 2014;16:48–56.. [DOI] [PubMed] [Google Scholar]
- 20.Rassman WR, Pak JP, Kim J, Estrin NF. Scalp micropigmentation: a concealer for hair and scalp deformities. J Clin Aesthet Dermatol. 2015;8(3):35–42.. Available at: http://www.ncbi.nlm.nih.gov/pubmed/25852813. Accessed March 12, 2017. [PMC free article] [PubMed] [Google Scholar]
- 21.Herbenick D, Schick V, Reece M, et al. The development and validation of the Male Genital Self-Image Scale: results from a nationally representative probability sample of men in the United States. J Sex Med. 2013;10:1516–1525.. [DOI] [PubMed] [Google Scholar]


