Abstract
Background
Heroin use is increasing in the US. Heroin use may predispose users towards injection routes of drug administration as compared to other illicit substances.
Objective
To explore the relationship between heroin use and drug injection, we compared time from first use to first injection (referred to as time to injection onset by drug [TTIOD]) of heroin, methamphetamine/speed, cocaine, and crack cocaine among people who inject drugs (PWID).
Methods
Age of first use and first injection by drug was collected from 776 PWID. Survival analyses were used to determine TTIOD and to examine demographic factors associated with TTIOD. Cox regression analysis was used to determine demographic factors associated with drug-specific injection onset.
Results
The eventual injection onset rate by the drug was 99% for participants who used heroin, 85% for participants who used methamphetamine/speed, 80% for participants who used powder cocaine, and 38% for participants who used crack cocaine. Hazard ratios for injection use within one year of first use by drug were: 1.37 (median survival time [MST]=0.61 years) for heroin, 0.66 (MST=1.10 years) for methamphetamine/speed, 0.50 (MST=2.93 years) for powder cocaine, and 0.12 (MST=39.59 years) for crack cocaine. Demographic differences in TTIOD were found for each drug. Demographic differences were found for eventual injection by drug for all substances except heroin.
Conclusion
Among PWID, heroin use was associated with a more rapid transition to injection and a higher rate of eventual heroin injection regardless of demographics. More robust, innovative efforts to reduce heroin use and prevent injection initiation are urgently needed.
Keywords: Heroin, PWID, injection drugs, epidemiology, time to injection onset
1. Introduction
1.1. Global and US Trends in Opioids and Heroin
Of the estimated 35 million people who used opioids in 2015, 17.7 million people used heroin or opium (UNODC, 2017). Opioids are the primary drug of concern for people entering treatment in Asian and Europe and the second drug of concern in North America and Africa (UNODC, 2017). The health consequences of opioid use have led the United Nations Office on Drugs and Crime (UNODC) to conclude that opioids, including heroin, are “the most harmful drug type.” (UNODC, 2017) The UNODC and others have also concluded that increasing overdose deaths are strongly related with increased heroin and synthetic opioids (especially fentanyl) use and that this phenomenon is a special concern in North America (Global, 2017; UNODC, 2017). In the global context, understanding drug use practices related to heroin use appears warranted.
In the US, increases in past year heroin use have been documented. Between 2002-04 and 2011-14 heroin use increased from 1.6 to 2.6 per thousand (Jones et al., 2015). Per capita past year heroin use doubled for people aged 18 to 25 between the years of 2002 to 2014 and increased for people aged 26 and older (Center, 2015). Comparison of heroin use and heroin use disorder from the National Epidemiologic Survey on Alcohol and Related Condition from 2001-02 to 2012-13, showed significant increases in lifetime heroin use and disorder during this period, with statistically significant increases among non-Hispanic Whites and those aged 18 to 29 (Martins et al., 2017). Heroin-related treatment admissions have also increased dramatically overall and among non-Hispanic whites and individuals aged 45 years of age and older (Compton et al., 2016; Kolodny et al., 2015).
1.2. Heroin Use and Transitions to Injection Drug Use
One potential consequence of heroin use is increased drug injection. Reasons for this are multiple. Some types of heroin (i.e., black tar heroin) are difficult to use without injection (Maxwell and Spence, 2006). In addition, as compared to ingestion through other routes, heroin injection typically provides a lower-cost per dose with a stronger euphoric drug effect, more rapid onset and longer effect as compared to snorting or smoking heroin (Fitzgerald et al., 1999; Goldsamt et al., 2010; Kermode et al., 2009; McBride et al., 2001; Sherman et al., 2002; Swift et al., 1999). Other research indicates that these effects appear more salient for heroin than other common injectable drugs such as methamphetamines/speed (referred to as meth/speed hereafter) and powder cocaine (Gossop et al., 1992). Perhaps for this reason 50% of people who used heroin in the NSHUD report injecting as compared to 13% of people who use meth/speed and 3% for people who use cocaine (Novak and Kral, 2011). Understanding the implications of increased heroin use for drug injection patterns is important given the elevated risk associated with drug injection (Larney et al., 2016; UNODC, 2017)
1.3. Time to Injection Initiation by Drug
Previously, we examined birth cohort differences in time to injection initiation (TTII) -defined as years between first illicit drug use and first injection drug use (Bluthenthal et al., 2017). Along with race and gender differences, we also found that PWID born in the 1980s and later, who came of age during the prescription opioid epidemic, had a shorter TTII as compared to those born in the 1970s who came of age during the cocaine/crack cocaine epidemics (Bluthenthal et al., 2017).
As a follow-up to that study, we now examine time to injection onset by drug (TTIOD), defined as years between first use of a particular drug and first injection of that drug. We hypothesize that heroin use would result in a more rapid transition to injection once used as compared to meth/speed, powder cocaine, and crack-cocaine. Given recent national data on changing trends in heroin use by sub-populations (Cicero et al., 2014; Jones et al., 2015), our prior research finding on TTII (Bluthenthal et al., 2017), and sexual orientation vulnerability to methamphetamine (Marshall et al., 2011), we also consider if demographic characteristics are associated with injection onset of heroin, meth/speed, cocaine, and crack cocaine. To our knowledge, this type of comparative examination of TTIOD has not been previously undertaken.
2. Methods
2.1. Study Procedures, Eligibility, and Recruitment
Data for these analyses come from a mixed-method, life course study of injection initiation among PWID in Los Angeles and San Francisco, California from 2011 to 2013 (Arreola et al., 2014; Wenger et al., 2016). Study recruitment was accomplished using targeted sampling methods (Bluthenthal and Watters, 1995; Kral et al., 2010; Watters and Biernacki, 1989). Participant eligibility criteria included self-reported injection drug use in the last 30 days (as verified by visible signs of venipuncture), 18 years of age or older, and ability to provide informed consent. A total of 776 participants were eligible and completed a 30-minute, quantitative survey using computer-assisted personal interviewing software (Questionnaire Development System, Nova Research, Bethesda, MD) with a trained research interviewer in a private setting. Participants received $15 USD for completing the quantitative survey. The institutional review boards approved study procedures at RTI International and the University of Southern California.
2.2. Key Study Domains and Variables
Guided by Life Course Theory (Elder, 1994), we were interested in the time between critical events; in this case the first use of a specific drug and first injection of that same drug. While we asked for information on 12 injectable drugs (i.e., heroin, powder cocaine, crack cocaine, meth/speed, prescription opioids, stimulants, sedatives, tranquilizers, methadone, buprenorphine, speedballs [heroin/cocaine mixture], and goofball [heroin/meth/speed mixture]), we limited our investigation to heroin, meth/speed, powder cocaine and crack cocaine. We excluded prescription opioids because we did not ask details on which kind of prescription opioid was used. In the last 50 years, prescription opioid formulations have changed three times, with short-acting formulations being available throughout, followed by the introduction of extended-release formulations in the mid-nineties, and then abuse-deterrent formulations in 2010 (Manchikanti et al., 2012). The abuse potential and routes of administration of these prescription opiate formulations differ significantly (Butler et al., 2011; Butler et al., 2013; Havens et al., 2014). Unfortunately, our questions on prescription opioids did not include items that would allow us to distinguish between types of prescription opioids (short-acting, extended-releases, abuse-deterrent) and so we cannot reliably examine prescription opioid TTIOD in our sample. We have also excluded other prescription drugs (i.e., stimulants, sedative, tranquilizers, methadone, and buprenorphine) because fewer than 10% of our sample had ever injected these substances.
To determine first use and first injection of heroin, meth/speed, powder cocaine, and crack cocaine, we asked the following questions. “Have you ever used [drug type]?” For those responding affirmatively, the next question was, “How old were you when you first used [drug type]?” Participants were then asked if they had ever injected the drug. For those responding affirmatively, they were asked the age at first injection use. To determine TTIOD, we subtracted age of the first injection of a drug from the age of first use. TTIOD result of zero indicates that the participant first used and first injected a drug at the same age. All other numbers indicate the years between first use and first injection.
Changes in drug-using subpopulations led us to consider the following demographic variables as covariates: gender by sexual orientation (heterosexual male, heterosexual female, gay or bisexual male, lesbian or bisexual female), age (measured as birth cohort), and race/ethnicity (White, African American, Latino, and all others).
2.3. Sample Size and Statistical Analyses
Participants contributed data for analyses if they ever used crack cocaine, powder cocaine, meth/speed or heroin (n=776). Therefore, analyses related to heroin use included 94% of the sample. The proportion included for the other drugs was: 87% for crack cocaine, 86% for powder cocaine, and 73% for meth/speed.
Survival analysis techniques were used to describe years to first injection by drug. Cumulative survival proportions by year were generated for each drug. Using survival tables, we determined hazard ratios and median survival TTIOD for each drug as well. To assess if TTIOD differed by demographics, we used Kaplan-Meier comparison of means. Lastly, we used Cox regression analysis to determine if demographic factors were associated with eventual uptake of injection for heroin, meth/speed, powder cocaine, and crack cocaine. For all statistical tests, we used p<0.05 to establish significance. Data analysis was conducted using IBM© SPSS© version 24.
3. Results
3.1 Sample characteristics
Selected sample characteristics are presented in Table 1. This sample is diverse (∼30% white and African American, 25% Latino; 25% female), older (50% were ≥ 50 years of age; mean age=47.59 [standard deviation=11.44]), low income (80% earned income < $1,350 per month), and unstably housed (62% homeless). In terms of drug use, most had used heroin (94%) and marijuana (93%) at least once. Over three-quarters had ever used cocaine, and nearly three quarters had used meth/speed. While all participants were recent injectors, rates of ever injecting a drug varied. For instance, heroin was ever injected by 93% of the sample as compared to 69% for powder cocaine, 62% for meth/speed, and 33% for crack-cocaine. Mean age of first injection was 21.72 years (standard deviation = 8.58; median = 19).
Table 1.
Selected demographic, socioeconomic, and drug use characteristics of sample (N=776).
| Characteristic | N (%) |
|---|---|
|
| |
| Study Site | |
| Los Angeles | 397 (51%) |
| San Francisco | 380 (49%) |
|
| |
| Gender by sexual orientation | |
| Heterosexual male | 495 (64%) |
| Heterosexual Female | 164 (21%) |
| Gay or bisexual male | 77 (10%) |
| Lesbian or bisexual female | 39 (5%) |
|
| |
| Age | |
| <29 | 80 (10%) |
| 30 to 39 | 86 (11%) |
| 40-49 | 223 (29%) |
| 50 or higher | 388 (50%) |
|
| |
| Birth Cohort | |
| Pre-Sixties | 339 (44%) |
| Sixties | 243 (31%) |
| Seventies | 104 (13%) |
| Eighties or later | 91 (12%) |
|
| |
| Race/ethnicity | |
| White | 265 (34%) |
| African American | 233 (30%) |
| Hispanic | 192 (25%) |
| All others | 82 (11%) |
|
| |
| High school or equivalent education or more – Yes | 499 (64%) |
|
| |
| Currently homeless – Yes | 484 (62%) |
|
| |
| Monthly income | |
| <$1,351 | 627 (81%) |
| $1,351 plus | 150 (19%) |
|
| |
| Years of drug injection | |
| <10 years | 126 (16%) |
| 10 to 19 years | 128 (17%) |
| 20 or more years | 522 (67%) |
|
| |
| Ever used | |
| Crack cocaine | 677 (87%) |
| Powder cocaine | 669 (86%) |
| Methamphetamine | 566 (73%) |
| Heroin | 732 (94%) |
| Opiate prescription medication | 492 (63%) |
| Stimulant prescription medication | 168 (22%) |
| Tranquilizers prescription medication | 451 (58%) |
| Sedative prescription medication | 159 (20%) |
| Marijuana | 723 (93%) |
|
| |
| Ever injected | |
| Crack cocaine | 254 (33%) |
| Powder cocaine | 537 (69%) |
| Methamphetamine | 480 (62%) |
| Heroin | 727 (94%) |
| Opiate prescription medication | 250 (32%) |
|
| |
| First drug injected | |
| Heroin | 460 (59%) |
| Methamphetamine/Speed | 163 (21%) |
| Cocaine | 84 (11%) |
| Goofball/Speedball | 33 (4%) |
| Prescription opioids | 28 (4%) |
| Other prescription drugs | 4 (1%) |
|
| |
| Injection frequency, last 30 days | |
| Less than once a day | 362 (47%) |
| Once or twice a day | 214 (27%) |
| Three times or more a day | 201 (26%) |
3.2. Survival Analysis of TTIOD for Heroin, Meth/Speed, and Powder Cocaine
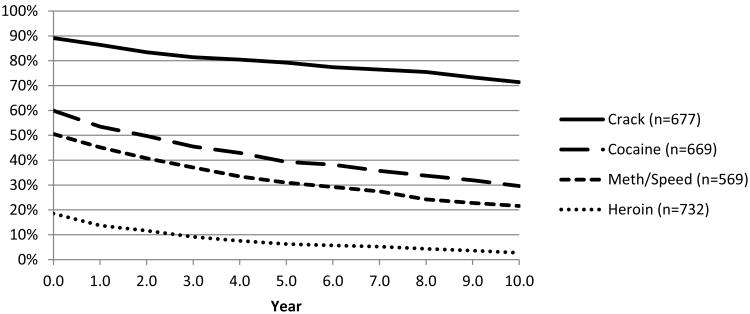
Figure 1 illustrates the cumulative survival proportions by year since first use for each drug. For people using heroin, only 19% had NOT initiated injection use within one year of first use. These proportions were 51% for people using meth/speed, 60% for powder cocaine, and 89% for crack cocaine. Within 10 years of first use, 3% of people using heroin had NOT injected it as compared to 22% of people that had used meth/speed, 30% of people that had used powder cocaine, and 71% of people who had used crack cocaine. The one-year hazard ratios by drug were 1.37 for heroin (standard error [SE]=0.04; median survival time = 0.61 year), 0.66 for meth/speed (SE=0.04; median survival time =1.10 years), 0.50 for powder cocaine (SE=0.03; median survival time = 2.93 years), and 0.12 for crack cocaine (SE=0.01; median survival time = 39.59 years).
Figure 1.
Ten-year cumulative survival: Proportion having not injected by year from first use for heroin, meth/speed, cocaine, and crack cocaine among PWID, 2011-13.
3.3. Kaplan-Meier Comparison of Means Of TTIOD
Using Kaplan-Meier techniques, we examined demographic (sex, birth cohort, sexual orientation, and race) differences in TTIOD (Table 2). For heroin, we found differences in survival curves such that Latinos had statistically significant shorter TTIOD and PWID born in the 1970s had longer TTIOD. For meth/speed, we found that gay/bisexual men had a shorter TTIOD while Latinos had longer TTIOD. For cocaine, PWID born in the pre-sixties birth cohort and women had longer TTIOD. For crack cocaine, whites and the 1980s or later birth cohort had shorter TTIOD.
Table 2.
Kaplan-Meier results for demographic variables associated with time to injection onset by drug (TTIOD).
| Heroin Mean in years (95% ∼CI) | Meth/Speed Mean in years (95% ∼CI) | Cocaine Mean in years (95% ∼CI) | Crack Cocaine Mean in years (95% ∼CI) | |
|---|---|---|---|---|
|
| ||||
| Sex by sexual orientation | ||||
| Heterosexual male | 1.15 (0.82, 1.42) | 8.07 (6.39, 9.75) | 10.88 (8.97, 12.80) | 30.17 (27.84, 32.51) |
| Heterosexual female | 1.03 (0.41, 1.67) | 8.84 (6.37, 11.30) | 14.14 (11.16, 17.12)* | 28.10 (25.26, 30.94) |
| Gay/bisexual | 0.79 (0.34, 1.24) | 2.52 (1.62, 3.42)* | 10.64 (7.16, 14.13) | 21.57 (17.01, 26.12) |
| Lesbian/bisexual | 1.07 (0.24, 1.90) | 7.61 (4.39, 10.83) | 11.72 (6.86, 16.58) | 22.60 (17.34, 27.85) |
|
| ||||
| Birth cohort | ||||
| Pre-1960s | 0.84 (0.45, 1.23) | 10.37 (7.69, 13.05) | 11.73 (9.23, 14.22) | 33.45 (30.77, 36.13) |
| 1960s | 1.16 (0.66, 1.65) | 5.66 (4.18, 7.14) | 9.81 (8.01, 11.61) | 25.00 (22.92, 27.08) |
| 1970s | 1.75 (1.00, 2.49)* | 6.38 (4.80, 7.96) | 9.53 (7.51, 11.56) | 15.40 (13.13, 17.67) |
| 1980s or later | 1.12 (0.58, 1.65) | 4.58 (3.49, 5.67) | 7.63 (6.15, 9.11)* | 8.36 (6.56, 10.17)* |
|
| ||||
| Race | ||||
| White | 1.13 (0.73, 1.52) | 5.43 (4.15, 6.71)* | 9.02 (7.38, 10.66) | 20.10 (17.90, 22.32)* |
| African American | 1.50 (0.88, 2.13) | 9.52 (6.39, 12.66) | 12.87 (10.04, 15.71) | 32.24 (29.13, 35.35) |
| Latino | 0.55 (0.15, 0.94)* | 12.91 (8.96, 16.87) | 10.25 (7.72, 12.78) | 29.55 (26.97, 32.12) |
| Other | 1.07 (0.41, 1.73) | 6.08 (3.74, 8.43) | 15.82 (9.97, 21.68) | 33.02 (27.93, 38.12) |
∼CI= Confidence Interval;
p<0.05 based on Log Rank (Mantel-Cox)
3.4. Cox Regression Analysis of Factors Associated with Injection Uptake
Lastly, we examined demographic factors associated with transitioning into injection by drug (Table 3). Eventual injection by drug was as follows: 99% for heroin, 85% for meth/speed, 80% for powder cocaine, and 38% for crack cocaine. Due to the high rate of eventual injection among people who used heroin, no demographic differences in injection uptake were noted for this drug. Gay men were more likely to initiate meth/speed injection while Latinos were less likely to initiate meth/speed injection. For cocaine, heterosexual women and PWID born in the 1980s were less likely to initiate powder cocaine injection. Factors associated with crack cocaine injection included PWID born in the 1970s and 1980s while Latinos were less likely to inject crack cocaine.
Table 3.
Cox regression models of demographic factors associated with injection uptake by drug.
| Variables | Meth/Speed AOR (95% CI) | P= | Cocaine AOR (95% CI) | P= | Crack Cocaine AOR (95% CI) | P= |
|---|---|---|---|---|---|---|
|
| ||||||
| Gender by sexual orientation | Referent | Referent | NS | |||
| Heterosexual male | 0.85 (0.66, 1.08) | 0.18 | 0.73 (0.58, 0.91) | 0.01 | ||
| Heterosexual female | 1.37 (1.05, 1.79) | 0.02 | 0.86 (0.64, 1.16) | 0.33 | ||
| Gay/bisexual male | 0.82 (0.54, 1.25) | 0.36 | 0.84 (0.56, 1.26) | 0.40 | ||
| Lesbian/bisexual female | ||||||
|
| ||||||
| Race | ||||||
| White | Referent | NS | Referent | |||
| Black | 0.86 (1.68, 1.08) | 0.20 | 0.71 (0.51, 0.98) | 0.04 | ||
| Latino | 0.71 (0.55, 0.91) | 0.01 | 0.51 (0.35, 0.74) | 0.01 | ||
| Other | 0.96 (0.72, 1.28) | 0.78 | 0.64 (0.40, 1.01) | 0.05 | ||
|
| ||||||
| Birth cohort | ||||||
| Pre-1960s | Referent | Referent | ||||
| 1960s | NS | 0.92 (0.76, 1.12) | 0.40 | 1.30 (0.95, 1.78) | 0.10 | |
| 1970 | 0.82 (0.62, 1.07) | 0.20 | 2.12 (1.45, 3.10) | 0.01 | ||
| 1980 or later | 0.69 (0.50, 0.95) | 0.03 | 3.06 (1.95, 4.81) | 0.01 | ||
AOR=Adjusted Odds Ratio; CI=Confidence Interval; ns=Not significant.
4. Discussion
4.1. Heroin TTIOD and Injection Uptake
The rapid transition from first use to the first injection of heroin is our principal finding. This transition occurred more rapidly as compared to crack cocaine, powder cocaine, and meth/speed as measured by mean and median years to TTIOD, 1 and 10 years thresholds, and hazard ratio. These findings are in line with one study which reported that people who use heroin were more likely to become regular injectors and to progress to regular injection more quickly than users of cocaine, methamphetamine, and prescription stimulants and opioids (O'Keefe et al., 2016). Taken together, these data point to the elevated risk of injection for people who use heroin compared to people who use meth/speed, cocaine, and crack cocaine. This lead us to conclude that the increase in heroin use in the US is likely to be accompanied by a surge in people who inject drugs.
Local case reports and national surveillance data on ailments common to drug injection indicate that injection drug use is increasing rapidly in the US. For instance, data from the National Inpatient Sample found that injection drug use-related infective endocarditis (IDU-IE) cases increased from 7% in 2000 to 12.1% of cases in 2013 (Wurcel et al., 2016). A twelve-fold increase in hospitalizations for infective endocarditis was reported in North Carolina between 2010 and 2015 (Fleischauer et al., 2017). Similarly, a single center study of a tertiary care facility in North Carolina reported that IDU-IE cases rose from 14% to 56% of all IE cases between 2009 and 2014 (Hartman et al., 2016). At the University of Cincinnati Medical Center, investigators documented a two-fold increase in infective endocarditis and a three-fold increase in HCV that they linked to injection drug use over a 10-year period (Keeshin and Feinberg, 2016). Lastly, significant increases in HCV infections among people under the age of 30 have been linked to injection drug use in Kentucky, Massachusetts, Tennessee, Virginia, and West Virginia (CDC, 2011; Zibbell et al., 2015) and acute HCV incidence increased in 30 states between 2006 and 2012 (Suryaprasad et al., 2014).
4.2. Demographic Differences in Injection Uptake
Demographic characteristics were related to more rapid TTIOD. For instance, we found that TTIOD for heroin and crack cocaine varied by birth cohort, aligning with our prior work that reported TTII (years between first illicit use of any drug and first injection of any drug) differed between those born in the 1970s versus those born in the 1980s or later (Bluthenthal et al., 2017). We also found that meth/speed TTIOD was significantly shorter for gay men. A large literature has documented the elevated use of amphetamines, methamphetamine, and crystal methamphetamine among gay men (Halkitis et al., 2001; Shoptaw, 2006). In addition, studies have also found that methamphetamine injection among gay men is higher than other groups (Inglez-Dias et al., 2008; Jin et al., 2014). Shorter TTIOD and higher odds of injection uptake among gay PWID might be expected. While the health risk, particularly HIV, for drug injection among gay men has been widely reported (CDC, 2013; Kral et al., 2001; Patrick et al., 1997; Strathdee et al., 2001), factors associated with transitions to drug injection among gay men are not well understood (Deacon et al., 2013; Dowsett et al., 2005; Nakamura et al., 2009). These demographic differences in injection by drug type are worthy of additional study. Such future work should consider factors such as cultural, socioeconomic, generational norms, and use patterns shaped by racial segregation or by subpopulation lifestyles (such as those observed for gay men) that might indicate a susceptibility to drug injection (Bourgois, 2003; Bourgois et al., 2006; Denham, 2008; McCoy et al., 2005).
4.3. Limitations
Research design limitations include the following. Data are based on participant self-reports and are subject to recall bias. However, recall measures for this study have been found to be reliable (Dyal et al., 2015). Our retrospective, cross-sectional study design allowed us to examine birth cohort differences, but studies that examine injection onset by drug type among prospective cohorts of people who use non-injection drugs are needed. Further, studies examining TTII and TTIOD in other locales are required to determine if the patterns observed in our studies are replicated elsewhere. Our sample should not be considered representative of PWID in Los Angeles and San Francisco, although our sampling approach has been found to yield comparable results to those employing respondent-driven sampling (Kral et al., 2010). Our sample was also older, and new studies with larger proportions of younger injectors are needed to determine if our findings are generalizable to younger cohorts of PWID.
Regarding our substantive findings, it is possible that black tar heroin – the predominant form that heroin is sold in the west of the Mississippi - accelerates transitions to drug injection because it is more difficult to sniff than the East Coast Colombian-sourced powder forms of heroin (Maxwell and Spence, 2006). However, national data on heroin use indicates that rates of injection are lower in the Western US than in other regions despite the high prevalence of black tar heroin on the West Coast (Muhuri et al., 2013). Nonetheless, studies examining TTIOD in cities where powder heroin forms are sold are needed (Ciccarone and Bourgois, 2003; Mars et al., 2016; Summers et al., 2017). Lastly, our data do not allow us to consider drug potency. Drug potency can vary substantially even over short periods of time and might influence the route of drug administration changes and overdose rates as indicated in other studies (Cunningham et al., 2008; Hempstead and Yildirim, 2014; Strang et al., 1997). Future studies that carefully examine the logistics of drug form, potency fluctuations, as well as cultural norms and political-economic contexts shaping patterns of drug use across vulnerable population subgroups are needed to more fully examine these relationships to explore the potential for population-level prevention interventions.
5. Conclusion
These data and our analysis of TTII in general (Bluthenthal et al., 2017), lead us to conclude that increased use of heroin in the US is highly likely to lead to more people injecting drugs. Increasing heroin use and drug injection present significant public health challenges. Shorter TTIOD reduces the opportunity for treatment and prevention systems to intervene with people who use drugs prior to the escalation to more dangerous ingestion modes. Efforts to engage people who use drugs while still early in their drug use career should be prioritized, and specific interventions aimed at engagement in treatment (Kelley and Chitwood, 2004) and preventing transitions into injection should be implemented (Werb et al., 2013). Programs to consider in this latter area include the Sniffer intervention that was developed for users of powder heroin (Casriel et al., 1990; Des Jarlais et al., 1992), and the distribution foil (for smoking heroin) (Pizzey and Hunt, 2008) and other non-injection equipment with the aim of preventing transitions to injection (Bridge, 2010; Hunt, 1999).
Focus on active PWID as agents of injection prevention intervention should also be considered (Werb et al., 2017). Empirical studies have found that injection initiation is often a social learning process (Khobzi et al., 2008; Stillwell et al., 1999) that involves repeated exposure to injection, advice on how to injection, and actual assistance with first injection (Bluthenthal et al., 2014; Kolla et al., 2015). There are community (Hunt et al., 1998) and individual-level (Strike et al., 2014) interventions that attempt to discourage active PWID from interacting with non-injectors in a way that would prompt the latter to learn about injection or ask for assistance initiating injection (Bluthenthal et al., 2015; Rotondi et al., 2014). Safe drug consumption sites might also serve this purpose by permitting PWID to use in private settings that do not expose non-injectors to injection drug use (McNeil and Small, 2014; Potier et al., 2014). These approaches should be implemented where feasible.
Finally, to address other health risk associated with injection a robust public health response is needed and should include long-standing, evidence-based interventions such as syringe exchange programs (MacArthur et al., 2014), wound and abscess care clinics (Grau et al., 2002), primary care screening, vaccinations, and treatments (Burr et al., 2014; Heinzerling et al., 2006; Perlman et al., 2001), and overdose prevention education and naloxone distribution among other health promoting strategies (CDC, 2012). Heroin and drug injection-related harms are increasing, and our data suggest the need for public health to improve its understanding of the complex supply/demand/sociocultural and economic parameters that have shaped changing generational preferences for drugs and their relationship to routes of administration. This would enable the field to supplement these evidence-based risk reduction approaches with more innovative, culturally-appropriate upstream structural interventions among the vulnerable populations most affected by this emerging crisis.
Highlights.
Heroin use leads to injection more rapidly than other drugs
Population increases in heroin use could lead to more drug injection.
Demographic differences in trajectories to injection differed by drug.
Public health responses to emerging trends in drug injection are urgently needed.
Acknowledgments
The research was supported by NIDA (grant # R01DA027689: Program Official, Elizabeth Lambert and grant # R01 DA038965) and in part by the National Cancer Institute (grant # P30CA014089). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. We thank the participants who took part in this study. The following research staff and volunteers also contributed to the study and are acknowledged here: Sonya Arreola, Vahak Bairamian, Soo Jin Byun, Jose Collazo, Jacob Curry, David-Preston Dent, Karina Dominguez, Jahaira Fajardo, Richard Hamilton, Frank Levels, Luis Maldonado, Askia Muhammad, Brett Mendenhall, Stephanie Dyal-Pitts, James Thing, and Michele Thorsen.
Role of Funding Source: The research was supported by NIDA (grant # R01DA027689: Program Official, Elizabeth Lambert and grant # R01 DA038965: Program Official Richard Jenkins) and in part by grant #s DA010164, DA037820, UL1TR001881, and National Cancer Institute (grant # P30CA014089).
Footnotes
Contributors: Ricky Bluthenthal designed the study (along with Alex Kral), conducted the statistical analysis, and prepared drafts of the manuscript. Ricky Bluthenthal, Philippe Bourgois, and Lynn Wenger managed the literature searches and summaries of previous related work. Lynn Wenger managed the study protocol. All authors contributed to and have approved the final manuscript.
Conflict of Interest: No conflict declared.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Arreola S, Bluthenthal RN, Wenger L, Chu D, Thing J, Kral AH. Characteristics of people who initiate injection drug use later in life. Drug Alcohol Depend. 2014;138:244–250. doi: 10.1016/j.drugalcdep.2014.02.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bluthenthal RN, Watters JK. Multimethod research from targeted sampling to HIV risk environments. NIDA Res Monogr. 1995;157:212–230. [PubMed] [Google Scholar]
- Bluthenthal RN, Wenger L, Chu D, Bourgois P, Kral AH. Drug use generations and patterns of injection drug use: Birth cohort differences among people who inject drugs in Los Angeles and San Francisco, California. Drug Alcohol Depend. 2017;175:210–218. doi: 10.1016/j.drugalcdep.2017.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bluthenthal RN, Wenger L, Chu D, Lorvick J, Quinn B, Thing JP, Kral AH. Factors associated with being asked to initiate someone into injection drug use. Drug Alcohol Depend. 2015;149:252–258. doi: 10.1016/j.drugalcdep.2015.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bluthenthal RN, Wenger L, Chu D, Quinn B, Thing J, Kral AH. Factors associated with initiating someone into illicit drug injection. Drug Alcohol Depend. 2014;144:186–192. doi: 10.1016/j.drugalcdep.2014.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bourgois P. In search of respect: Selling crack in el barrio. 2nd. Cambridge University Press; New York: 2003. [Google Scholar]
- Bourgois P, Martinez A, Kral A, Edlin BR, Schonberg J, Ciccarone D. Reinterpreting ethnic patterns among white and African American men who inject heroin: a social science of medicine approach. PLoS Med. 2006;3:e452. doi: 10.1371/journal.pmed.0030452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bridge J. Route transition interventions: potential public health gains from reducing or preventing injecting. Int J Drug Policy. 2010;21:125–128. doi: 10.1016/j.drugpo.2010.01.011. [DOI] [PubMed] [Google Scholar]
- Burr CK, Storm DS, Hoyt MJ, Dutton L, Berezny L, Allread V, Paul S. Integrating health and prevention services in syringe access programs: a strategy to address unmet needs in a high-risk population. Public Health Rep. 2014;129(1):26–32. doi: 10.1177/00333549141291S105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butler SF, Black RA, Cassidy TA, Dailey TM, Budman SH. Abuse risks and routes of administration of different prescription opioid compounds and formulations. Harm Reduct J. 2011;8:29. doi: 10.1186/1477-7517-8-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butler SF, Cassidy TA, Chilcoat H, Black RA, Landau C, Budman SH, Coplan PM. Abuse Rates and Routes of Administration of Reformulated Extended-Release Oxycodone: Initial Findings From a Sentinel Surveillance Sample of Individuals Assessed for Substance Abuse Treatment. J Pain. 2013;14:351–358. doi: 10.1016/j.jpain.2012.08.008. [DOI] [PubMed] [Google Scholar]
- Casriel C, Des Jarlais DC, Rodriguez R, Friedman SR, Stepherson B, Khuri E. Working with heroin sniffers: clinical issues in preventing drug injection. J Subst Abuse Treat. 1990;7:1–10. doi: 10.1016/0740-5472(90)90031-k. [DOI] [PubMed] [Google Scholar]
- CDC Hepatitis C virus infection among adolescents and young adults: Massachusetts, 2002-2009. MMWR: Morb Mortal Wkly Rep. 2011;60:537–541. [PubMed] [Google Scholar]
- CDC. Community-based opioid overdose prevention programs providing Naloxone -- United States, 2010. MMWR: Morb Mortal Wkly Rep. 2012;61:101–105. [PMC free article] [PubMed] [Google Scholar]
- CDC. Estimated percentages and characteristics of men who have sex with men and use injection drugs -- United States, 1999-2011. MMWR: Morbi Mortal Wkly Rep. 2013;62:757–762. [PMC free article] [PubMed] [Google Scholar]
- Center for Behavioral Health Statistics and Quality. ehavioral health trends in the United States: Results from the 2014 National Survey on Drug use and Health. Substance Abuse and Mental Health Services Administration; 2015. p. 64. [Google Scholar]
- Ciccarone D, Bourgois P. Explaining the geographical variation of HIV among injection drug users in the United States. Subst Use Misuse. 2003;38:2049–2063. doi: 10.1081/JA-120025125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cicero TJ, Ellis MS, Surratt HL, Kurtz SP. The changing face of heroin use in the United States: a retrospective analysis of the past 50 years. JAMA Psychiatry. 2014;71:821–826. doi: 10.1001/jamapsychiatry.2014.366. [DOI] [PubMed] [Google Scholar]
- Compton WM, Jones CM, Baldwin GT. Relationship between Nonmedical Prescription-Opioid Use and Heroin Use. New Engl J Med. 2016;374:154–163. doi: 10.1056/NEJMra1508490. [DOI] [PubMed] [Google Scholar]
- Cunningham JK, Liu LM, Muramoto M. Methamphetamine suppression and route of administration: precursor regulation impacts on snorting, smoking, swallowing and injecting. Addiction. 2008;103:1174–1186. doi: 10.1111/j.1360-0443.2008.02208.x. [DOI] [PubMed] [Google Scholar]
- Deacon RM, Mooney-Somers J, Treloar C, Maher L. At the intersection of marginalised identities: lesbian, gay, bisexual and transgender people's experiences of injecting drug use and hepatitis C seroconversion. Health Soc Care Community. 2013;21:402–410. doi: 10.1111/hsc.12026. [DOI] [PubMed] [Google Scholar]
- Denham BE. Folk devils, news icons, and the construction of moral panics. Journalism Studies. 2008;9:945–961. [Google Scholar]
- Des Jarlais D, Casriel C, Freidman SR, Rosenblum A. AIDS and the transition to illicit drug injection -- results of a randomized trial prevention program. Br J Addict. 1992;87:493–498. doi: 10.1111/j.1360-0443.1992.tb01950.x. [DOI] [PubMed] [Google Scholar]
- Dowsett GW, Wain D, Keys D. Good gay men don't get “Messy”: Injecting drug use and gay community. Sex Res Social Policy. 2005;2:22–36. [Google Scholar]
- Dyal SR, Kral AH, Dominguez Gonzalez K, Wenger LD, Bluthenthal RN. Consistency of self-reported drug use events in a mixed methods study of people who inject drugs. Am J Drug Alcohol Abuse. 2015;41:332–338. doi: 10.3109/00952990.2015.1037842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elder GH. Time, human agency, and social change: Perspectives on the life course. Soc Psychol Q. 1994;57:4–15. [Google Scholar]
- Fitzgerald JL, Louie R, Rosenthal D, Crofts N. The meaning of the rush for initiates to injecting drug user. Contemp Drug Probl. 1999;26:481–504. [Google Scholar]
- Fleischauer AT, Ruhl L, Rhea S, Barnes E. Hospitalizations for endocarditis and associated health care costs among persons with diagnosed drug dependence — North Carolina, 2010–2015. MMWR: Morb Mortal Wkly Rep. 2017;66:569–573. doi: 10.15585/mmwr.mm6622a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Global Commission on Drug Policy. The opioid crisis in North America. Geneva, Switzerland: 2017. p. 20. [Google Scholar]
- Goldsamt LA, Harocopos A, Kobrak P, Jost JJ, Clatts MC. Circumstances, pedagogy and rationales for injection initiation among new drug injectors. J Community Health. 2010;35:258–267. doi: 10.1007/s10900-010-9231-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gossop M, Griffiths P, Powis B, Strang J. Severity of dependence and route of administration of heroin, cocaine and amphetamines. Br J Addict. 1992;87:1527–1536. doi: 10.1111/j.1360-0443.1992.tb02660.x. [DOI] [PubMed] [Google Scholar]
- Grau LE, Arevalo S, Catchpool C, Heimer R. Expanding harm reduction services through a wound and abscess clinic. Am J Public Health. 2002;92:1915–1917. doi: 10.2105/ajph.92.12.1915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halkitis PN, Parsons JT, Stirratt MJ. A double epidemic: Crystal methamphetamine drug use in relation to HIV transmission. J Homosex. 2001;41:17–35. doi: 10.1300/J082v41n02_02. [DOI] [PubMed] [Google Scholar]
- Hartman L, Barnes E, Bachmann L, Schafer K, Lovato J, Files DC. Opiate Injection-associated Infective Endocarditis in the Southeastern United States. Am J Med Sci. 2016;352:603–608. doi: 10.1016/j.amjms.2016.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Havens JR, Leukefeld CG, DeVeaugh-Geiss AM, Coplan P, Chilcoat HD. The impact of a reformulation of extended-release oxycodone designed to deter abuse in a sample of prescription opioid abusers. Drug Alcohol Depend. 2014;139:9–17. doi: 10.1016/j.drugalcdep.2014.02.018. [DOI] [PubMed] [Google Scholar]
- Heinzerling KG, Kral AH, Flynn NM, Anderson RL, Scott A, Gilbert ML, Asch SM, Bluthenthal RN. Unmet need for recommended preventive health services among clients of California syringe exchange programs: Implications for quality improvement. Drug Alcohol Depend. 2006;81:167–178. doi: 10.1016/j.drugalcdep.2005.06.008. [DOI] [PubMed] [Google Scholar]
- Hempstead K, Yildirim EO. Supply-side response to declining heroin purity: Fentanyl overdose episode in New Jersey. Health Econ. 2014;23:688–705. doi: 10.1002/hec.2937. [DOI] [PubMed] [Google Scholar]
- Hunt N, Stillwell G, Taylor C, Griffiths P. Evaluation of a brief intervention to prevent initiation into injecting. Drugs: Educ Prev Policy. 1998;5:185–194. [Google Scholar]
- Hunt PG, Southwell Mathew, Stillwell Garry, Strang John, Neil Preventing and curtailing injecting drug use: A review of opportunities for developing and delivering ‘route transition interventions’. Drug Alcohol Rev. 1999;18:441–451. [Google Scholar]
- Inglez-Dias A, Hahn JA, Lum PJ, Evans J, Davidson P, Page-Shafer K. Trends in methamphetamine use in young injection drug users in San Francisco from 1998 to 2004: the UFO Study. Drug Alcohol Rev. 2008;27:286–291. doi: 10.1080/09595230801914784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jin H, Huriaux E, Loughran E, Packer T, Raymond HF. Differences in HIV risk behaviors among people who inject drugs by gender and sexual orientation, San Francisco, 2012. Drug and Alcohol Depend. 2014;145:180–184. doi: 10.1016/j.drugalcdep.2014.10.015. [DOI] [PubMed] [Google Scholar]
- Jones CM, Logan J, Gladden RM, Bohm MK. Vital Signs: Demographic and substance use trends among heroin users - United States, 2002-2013. MMWR: Morb Mortal Wkly Rep. 2015;64:719–725. [PMC free article] [PubMed] [Google Scholar]
- Keeshin SW, Feinberg J. Endocarditis as a marker for new epidemics of injection drug use. Am J Med Sci. 2016;352:609–614. doi: 10.1016/j.amjms.2016.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelley MS, Chitwood DD. Effects of drug treatment for heroin sniffers: A protective factor against moving to injection? Soc Sci Med. 2004;58:2083–2092. doi: 10.1016/j.socscimed.2003.08.006. [DOI] [PubMed] [Google Scholar]
- Kermode M, Longleng V, Singh BC, Bowen K, Rintoul A. Killing time with enjoyment: A qualitative study of initiation into injecting drug use in north-east India. Subst Use Misuse. 2009;44:1070–1089. doi: 10.1080/10826080802486301. [DOI] [PubMed] [Google Scholar]
- Khobzi N, Strike C, Cavalieri W, Bright R, Myers T, Calzavara L, Millson M. Initiation into injection: Necessary and background processes. Addict Res Theory. 2008;17:1–14. [Google Scholar]
- Kolla G, Strike C, Roy E, Altenberg J, Balian R, Silver R, Hunt N. Initiation stories: An examination of the narratives of people who assist with a first injection. Subst Use Misuse. 2015;50:1619–1627. doi: 10.3109/10826084.2015.1023456. [DOI] [PubMed] [Google Scholar]
- Kolodny A, Courtwright DT, Hwang CS, Kreiner P, Eadie JL, Clark TW, Alexander GC. The prescription opioid and heroin crisis: A public health approach to an epidemic of addiction. Annu Rev Public Health. 2015;36:559–574. doi: 10.1146/annurev-publhealth-031914-122957. [DOI] [PubMed] [Google Scholar]
- Kral AH, Bluthenthal RN, Lorvick J, Gee L, Bacchetti P, Edlin BR. Sexual transmission of HIV-1 among injection drug users in San Francisco, USA: Risk-factor analysis. Lancet. 2001;357:1397–1401. doi: 10.1016/S0140-6736(00)04562-1. [DOI] [PubMed] [Google Scholar]
- Kral AH, Malekinejad M, Vaudrey J, Martinez AN, Lorvick J, McFarland W, Raymond HF. Comparing respondent-driven sampling and targeted sampling methods of recruiting injection drug users in San Francisco. J Urban Health. 2010;87:839–850. doi: 10.1007/s11524-010-9486-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larney S, Peacock A, Mathers BM, Hickman M, Degenhardt L. A systematic review of injecting-related injury and disease among people who inject drugs. Drug Alcohol Depend. 2016;171:39–49. doi: 10.1016/j.drugalcdep.2016.11.029. [DOI] [PubMed] [Google Scholar]
- MacArthur GJ, van Velzen E, Palmateer N, Kimber J, Pharris A, Hope V, Taylor A, Roy K, Aspinall E, Goldberg D, Rhodes T, Hedrich D, Salminen M, Hickman M, Hutchinson SJ. Interventions to prevent HIV and hepatitis C in people who inject drugs: A review of reviews to assess evidence of effectiveness. Int J Drug Policy. 2014;25:34–52. doi: 10.1016/j.drugpo.2013.07.001. [DOI] [PubMed] [Google Scholar]
- Manchikanti L, Helms S, Fellows B, Janata W, Pampati V, Grider JS, Boswell MV. Opioid epidemic in the United States. Pain Physician. 2012;15(3 suppl):ES9–38. [PubMed] [Google Scholar]
- Mars SG, Bourgois P, Karandinos G, Montero F, Ciccarone D. The textures of heroin: User prespectives on “Black Tar” and powder heroin in two U.S. cities. J Psychoactive Drugs. 2016;48:270–278. doi: 10.1080/02791072.2016.1207826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall BD, Wood E, Shoveller JA, Patterson TL, Montaner JS, Kerr T. Pathways to HIV risk and vulnerability among lesbian, gay, bisexual, and transgendered methamphetamine users: A multi-cohort gender-based analysis. BMC Public Health. 2011;11:20. doi: 10.1186/1471-2458-11-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martins SS, Sarvet A, Santaella-Tenorio J, Saha T, Grant BF, Hasin DS. Changes in us lifetime heroin use and heroin use disorder: Prevalence from the 2001-2002 to 2012-2013 national epidemiologic survey on alcohol and related conditions. JAMA Psychiatry. 2017;74:445–455. doi: 10.1001/jamapsychiatry.2017.0113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maxwell JC, Spence RT. An exploratory study of inhalers and injectors who used black tar heroin. J Maint Addict. 2006;3:61–82. doi: 10.1300/J126v03n01_06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McBride AJ, Pates RM, Arnold K, Ball N. Needle fixation, the drug user's perspective: A qualitative study. Addiction. 2001;96:1049–1058. doi: 10.1046/j.1360-0443.2001.967104914.x. [DOI] [PubMed] [Google Scholar]
- McCoy K, McGuire J, Curtis R, Spunt B. White chicks on dope: Heroin and identity dynamics in New York in the 1990s. J Drug Issues. 2005;35:817–841. [Google Scholar]
- McNeil R, Small W. ‘Safer environment interventions’: A qualitative synthesis of the experiences and perceptions of people who inject drugs. Soc Sci Med. 2014;106:151–158. doi: 10.1016/j.socscimed.2014.01.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muhuri PK, Gfroerer JC, Davies MC. CBHSQ Data Review. Substance Abuse and Mental Health Administration; 2013. Associations of nonmedical pain reliever use and initiation of heroin use in the United States; pp. 1–17. [Google Scholar]
- Nakamura N, Semple SJ, Strathdee SA, Patterson TL. Methamphetamine initiation among HIV-positive gay and bisexual men. AIDS Care. 2009;21:1176–1184. doi: 10.1080/09540120902729999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Novak SP, Kral AH. Comparing injection and non-injection routes of administration for heroin, methamphetamine, and cocaine users in the United States. J Addict Dis. 2011;30:248–257. doi: 10.1080/10550887.2011.581989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Keefe D, Horyniak D, Dietze P. From initiating injecting drug use to regular injecting: Retrospective survival analysis of injecting progression within a sample of people who inject drugs regularly. Drug and Alcohol Depend. 2016;158:177–180. doi: 10.1016/j.drugalcdep.2015.11.022. [DOI] [PubMed] [Google Scholar]
- Patrick DM, Strathdee SA, Archibald CP, Ofner M, Craib KJ, Cornelisse PG, Schechter MT, Rekart ML, O'Shaughnessy MV. Determinants of HIV seroconversion in injection drug users during a period of rising prevalence in Vancouver. Int J STD AIDS. 1997;8:437–445. doi: 10.1258/0956462971920497. [DOI] [PubMed] [Google Scholar]
- Perlman DC, Gourevitch MN, Trinh C, Salomon N, Horn L, Des Jarlais DC. Cost-effectiveness of tuberculosis screening and observed preventive therapy for active drug injectors at a syringe-exchange program. J Urban Health. 2001;78:550–567. doi: 10.1093/jurban/78.3.550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pizzey R, Hunt N. Distributing foil from needle and syringe programmes (NSPs) to promote transitions from heroin injecting to chasing: An evaluation. Harm Reduct J. 2008;5:24. doi: 10.1186/1477-7517-5-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Potier C, Laprévote V, Dubois-Arber F, Cottencin O, Rolland B. Supervised injection services: What has been demonstrated? A systematic literature review Drug Alcohol Depend. 2014;145:48–68. doi: 10.1016/j.drugalcdep.2014.10.012. [DOI] [PubMed] [Google Scholar]
- Rotondi NK, Strike C, Kolla G, Rotondi MA, Rudzinski K, Guimond T, Roy E. Transition to injection drug use: the role of initiators. AIDS Behav. 2014;18:486–494. doi: 10.1007/s10461-013-0693-8. [DOI] [PubMed] [Google Scholar]
- Sherman SG, Strathdee S, Smith L, Laney G. Spheres of influence in transitioning to injection drug use: A qualitative study of young injectors. Int J Drug Policy. 2002;13:113–120. [Google Scholar]
- Shoptaw S. Methamphetamine use in urban gay and bisexual populations. Top HIV Med. 2006;14:84–87. [PubMed] [Google Scholar]
- Stillwell G, Hunt N, Taylor C, Griffiths P. The modelling of injecting behavior and initiation into injection. Addict Res. 1999;7:447–459. [Google Scholar]
- Strang J, Griffiths P, Gossop M. Heroin in the United Kingdom: Different forms, different origins, and the relationship to different routes of administration. Drug Alcohol Rev. 1997;16:329–337. doi: 10.1080/09595239700186711. [DOI] [PubMed] [Google Scholar]
- Strathdee SA, Galai N, Safaiean M, Celentano DD, Vlahov D, Johnson L, Nelson KE. Sex differences in risk factors for HIV seroconversion among injection drug users a 10-year perspective. Arch Intern Med. 2001;161:1281–1288. doi: 10.1001/archinte.161.10.1281. [DOI] [PubMed] [Google Scholar]
- Strike C, Rotondi M, Kolla G, Roy E, Rotondi NK, Rudzinski K, Balian R, Guimond T, Penn R, Silver RB, Millson M, Sirois K, Altenberg J, Hunt N. Interrupting the social processes linked with initiation of injection drug use: Results fro a pilot study. Drug Alcohol Depend. 2014;137:48–54. doi: 10.1016/j.drugalcdep.2014.01.004. [DOI] [PubMed] [Google Scholar]
- Summers PJ, Struve IA, Wilkes MS, Rees VW. Injection-site vein loss and soft tissue abscesses associated with black tar heroin injection: A cross-sectional study of tw distinct populations in USA. Int J Drug Policy. 2017;39:21–27. doi: 10.1016/j.drugpo.2016.08.006. [DOI] [PubMed] [Google Scholar]
- Suryaprasad AG, White JZ, Xu F, Eichler BA, Hamilton J, Patel A, Hamdounia SB, Church DR, Barton K, Fisher C, Macomber K, Stanley M, Guilfoyle SM, Swee K, Liu S, Iqbal K, Tohme R, Sharapov U, Kupronis BA, Ward JW, Holmberg SD. Emerging Epidemic of hepatitis C virus infections among young nonurban Persons who inject drugs in the United States, 2006–2012. Clin Infect Dis. 2014;59:1411–1419. doi: 10.1093/cid/ciu643. [DOI] [PubMed] [Google Scholar]
- Swift W, Maher L, Sunjic S. Transitions between routes of heroin administration: A study of Caucasian and Indochinese heroin users in south-western Sydney, Australia. Addiction. 1999;94:71–82. doi: 10.1046/j.1360-0443.1999.941714.x. [DOI] [PubMed] [Google Scholar]
- UNODC. World Drug Report 2017. United Nations Publication; Vienna, Austria: 2017. [Google Scholar]
- Watters JK, Biernacki P. Targeted sampling: Options for the study of hidden populations. Soc Probl. 1989;36:416–430. [Google Scholar]
- Wenger LD, Lopez AM, Kral AH, Bluthenthal RN. Moral ambivalence and the decision to initiate others into injection drug use: A qualitative study in two California cities. Int J Drug Policy. 2016;37:42–51. doi: 10.1016/j.drugpo.2016.07.008. [DOI] [PubMed] [Google Scholar]
- Werb D, Bluthenthal RN, Kolla G, Strike C, Kral AH, Uuskula A, Des Jarlais D. Preventing injection drug use initiation: State of the evidence and opportunities for the future. J Urban Health. 2017 doi: 10.1007/s11524-017-0192-8. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Werb D, Buxton J, Shoveller J, Richardson C, Rowell G, Wood E. Interventions to prevent the initiation of injection drug use: A systematic review. Drug Alcohol Depend. 2013;133:669–676. doi: 10.1016/j.drugalcdep.2013.08.017. [DOI] [PubMed] [Google Scholar]
- Wurcel AG, Anderson JE, Chui KKH, Skinner S, Knox TA, Snydman DR, Stopka TJ. Increasing infectious endocarditis admissions among young people who inject drugs. Open Forum Infect Dis. 2016;3:ofw157–ofw157. doi: 10.1093/ofid/ofw157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zibbell J, Iqbal K, Patel RC, Suryaprasad AG, Sanders KJ, Moore-Moravian L, Serrechia J, Blankenship S, Ward JM, Holtzman D. Increases in hepatitis C virus infection related to injection drug use among persons aged < 30 years - Kentucky, Tennessee, Virginia, and West Virginia, 2006-2012. MMWR: Morb Mortal Wkly Rep. 2015;64:453–458. [PMC free article] [PubMed] [Google Scholar]