Abstract
Background
Due to the alarming rise in opioid-related overdose deaths, a public health emergency was declared in British Columbia (BC). In this study, we examined the relationship between illicit fentanyl and heroin found in seized drugs and illicit overdose deaths in BC.
Methods
An observational cross-sectional survey was conducted using BC data from Health Canada's Drug Analysis Service, which analyzes drug samples seized by law enforcement agencies, and non-intentional illicit overdoses from the BC Coroner's Service, from 2000 to 2016. Initial scatter plots and subsequent multivariate regression analysis were performed to describe the potential relationship between seized illicit fentanyl samples and overdose deaths and to determine if this differed from seized heroin and overdose deaths. Fentanyl samples were analyzed for other drug content.
Results
Fentanyl is increasingly being found combined with other opioid and non-opioid illicit drugs. Strong positive relationships were found between the number of seized fentanyl samples and total overdose deaths (R2 = 0.97) as well as between seized fentanyl and fentanyl-detected overdose deaths (R2 = 0.99). A positive association was found between the number of seized heroin samples and total overdose deaths (R2 = 0.78).
Conclusion
This research contributes to the expanding body of evidence implicating illicit fentanyl use (often combined with heroin or other substances) in overdose deaths in BC. Policy makers and healthcare providers are urged to implement drug treatment and harm reduction strategies for people at risk of overdose associated with current trends in illicit opioid use.
Keywords: Fentanyl, Heroin, Drug Overdose, Substance-Related Disorders, Opioid-Related disorders, Law Enforcement
1. Introduction
Misuse of opioids from both diverted prescriptions and illicitly manufactured sources is a well-documented and rising phenomenon in North America, and numerous studies report increasing opioid-related deaths in both Canada and the United States (Fischer and Argento, 2012; Lake et al., 2015; Manchikanti et al., 2012; Paulozzi et al., 2006; Suzuki and El-Haddad, 2017). Fentanyl, a synthetic opioid 50–100 times more potent than morphine with significantly cheaper production costs than heroin, has come under considerable scrutiny as a prominent contributor to the recent surge in overdose (OD) deaths seen across North America (Frank and Pollack, 2017). British Columbia (B.C.) has historically been the Canadian province with the highest rates of opioid use and opioid-related deaths (Canadian Centre on Substance Abuse, 2015; CBC News; Dauvergne, 2009; Health Canada, 2014). In B.C., total illicit drug overdose deaths increased from 269 in 2012 to 931 in 2016 (British Columbia Coroner’s Service, 2017a). Furthermore, recent studies and anecdotal reports suggest that many people who use drugs are unaware that their opioid source may be contaminated with fentanyl, either because the drugs are intentionally mislabeled as a different substance or because fentanyl may be surreptitiously assimilated into the primary drug of consumption (Amlani et al., 2015; Klar et al., 2016; McKee et al., 2015). The overall escalation in opioid-related unintentional deaths has led to a public health emergency being declared in B.C. by the Provincial Health Officer (B.C. Gov. News, 2016).
While the relationship between illicit fentanyl (synthesized from clandestine laboratories or diverted prescribed fentanyl) and fentanyl-related1 OD deaths has been well established in certain American reports (CDC, 2008; Denton et al., 2008; Gladden, 2016; Hull et al., 2007; Suzuki and El-Haddad, 2017), Canadian data is limited. Although there have been studies suggesting that fentanyl use and fentanyl-related deaths are both increasing across Canada (B.C. Gov. News, 2014; British Columbia Coroner’s Service, 2017b; Canadian Centre on Substance Abuse, 2015), there are currently no studies examining a possible association between the prevalence of illicit fentanyl on the black market and either the overall rate of OD deaths or of fentanyl-detected2 OD deaths. Though there is considerable data detailing the past association between non-fentanyl opioids, such as heroin, and total OD deaths in B.C., there are no data on the relationship with illicit drug seizure (Dauvergne, 2009; Fischer and Argento, 2012; Health Canada, 2014; Lake et al., 2015).
The purpose of the current study is to examine the relationship between seized fentanyl samples (including illicitly manufactured fentanyl along with prescribed fentanyl that is distributed/diverted) and total as well as fentanyl-detected unintentional OD deaths in B.C. Also examined is the relationship between seized heroin and total unintentional OD deaths in the province.
2. Methods
Publicly available data detailing the number of fentanyl and heroin exhibits seized by law enforcement in B.C. per year, from January 1, 2000 to December 31, 2016, were obtained from the Canadian Drug Analysis Service (DAS). The DAS is a federal laboratory that determines the chemical content of non-marijuana samples seized by Canadian law enforcement agencies when a not guilty plea is entered by an accused. Seized drugs are not tested if the accused pleads guilty. Fentanyl and fentanyl free-base were included in the analysis, but fentanyl analogues were not. Detection threshold using liquid chromatography mass spectrometry (LC/MS) was 1 µg/ml. The fentanyl data were further stratified to elucidate the number of exhibits that also contained other illicit drugs (morphine, oxycodone, hydromorphone, cocaine/crack, methamphetamine, but excluding cannabis). We used data detailing seizures of fentanyl and heroin exhibits by law enforcement in B.C. as a surrogate marker for the prevalence of these substances on the black market.
Data regarding the number of illicit drug unintentional OD deaths in B.C., from January 1, 2000 to December 31, 2016, were obtained from the B.C. Coroners Service (BCCS). These data include accidental overdose deaths attributed to street drugs, deliberate misuse of prescription medications including those obtained by diversion, drugs of unknown origin, and any combination of these sources. These data exclude overdose deaths deemed by the coroner to be intentional from history or circumstance (e.g., note found). Data detailing the number of fentanyl-detected unintentional overdose deaths in B.C., from January 1, 2012 (the first year fentanyl-detected OD deaths were identified in BC) to December 31, 2016, were also obtained from the BCCS (British Columbia Coroner’s Service, 2017a, 2017b). Fentanyl-detected deaths reported included the metabolite norfentanyl, but fentanyl analogues were not tested for. Detection threshold for both fentanyl and norfentanyl using LC/MS was 1 µg/ml. Because both of the data sources used in this study (DAS and BCCS) were publicly available, ethics approval was not required for this project.
Scatter plots were first utilized to establish temporal trends for seized fentanyl, seized heroin, overall OD deaths, and fentanyl-detected OD deaths. A regression analysis was then performed using R2 as a measure of association to determine if there was an association between the number of seized fentanyl samples and total OD deaths, seized fentanyl and fentanyl-detected OD deaths, and seized heroin and total OD deaths. All calculations were performed using Microsoft Excel for Macintosh, version 15.32.
3. Results
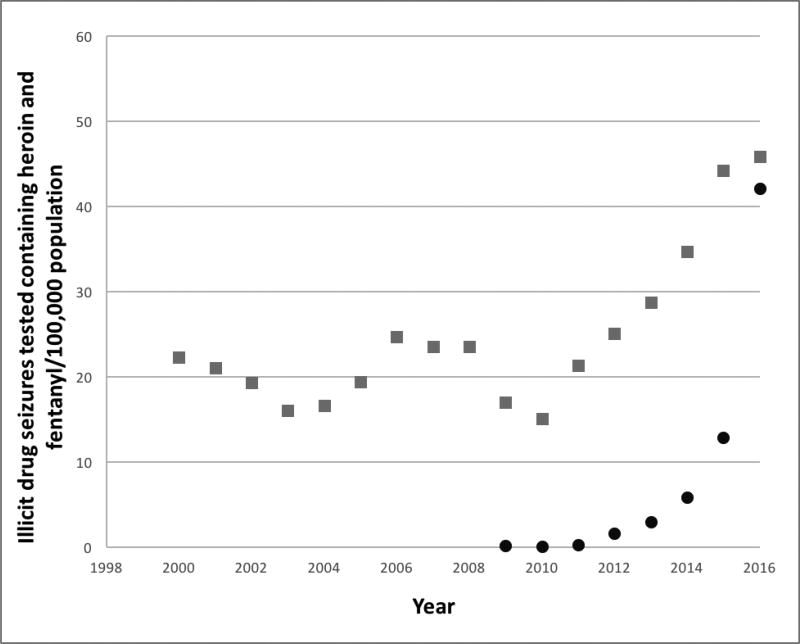
The number of seized heroin exhibits in B.C. fluctuated between 2000 and 2010, but it has been increasing steadily since then and tripled from 2010 to 2016 (Figure 1). Since seized illicit fentanyl in B.C. was first reported by the DAS in 2009, the number of samples has increased exponentially from 6 samples reported in 2009 to 1,997 in 2016 (Figure 1). Similarly, the number of seized fentanyl exhibits that are combined with other illicit drugs has been increasing since 2009, as has the variety of different illicit drug types with which fentanyl has being found, primarily mixed with heroin (Table 1). In addition, there is a notable rise in the finding of fentanyl mixed with stimulants (cocaine/crack and methamphetamine) in seized samples from 2016.
Figure 1.
Illicit drug seizures tested and containing heroin and fentanyl in British Columbia from 2006–2016.
* Data obtained from the Health Canada Drug Analysis Service. Circle = Fentanyl, square = heroin.
Table 1.
Number of seized drug exhibits tested and found to contain illicit substances from 2009–2016
| Year | Heroin | Fentanyl | Fentanyl + heroin |
Fentanyl + morphine |
Fentanyl + cocaine/crack |
Fentanyl + methamph† |
Fentanyl + oxycodone |
Fentanyl + hydromor†† |
|---|---|---|---|---|---|---|---|---|
| 2000 | 899 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 2001 | 856 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 2002 | 791 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 2003 | 661 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 2004 | 690 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 2005 | 813 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 2006 | 1047 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 2007 | 1008 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 2008 | 1021 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 2009 | 748 | 6 | 0 | 0 | 1 | 0 | 0 | 0 |
| 2010 | 674 | 5 | 1 | 0 | 1 | 0 | 0 | 0 |
| 2011 | 960 | 10 | 0 | 0 | 0 | 0 | 0 | 0 |
| 2012 | 1139 | 73 | 3 | 0 | 2 | 0 | 0 | 0 |
| 2013 | 1318 | 134 | 49 | 2 | 17 | 1 | 0 | 0 |
| 2014 | 1608 | 273 | 67 | 5 | 21 | 9 | 0 | 0 |
| 2015 | 2072 | 603 | 262 | 13 | 44 | 18 | 4 | 0 |
| 2016 | 2178 | 1997 | 1349 | 28 | 179 | 174 | 0 | 1 |
methamphetamine,
hydromorphone
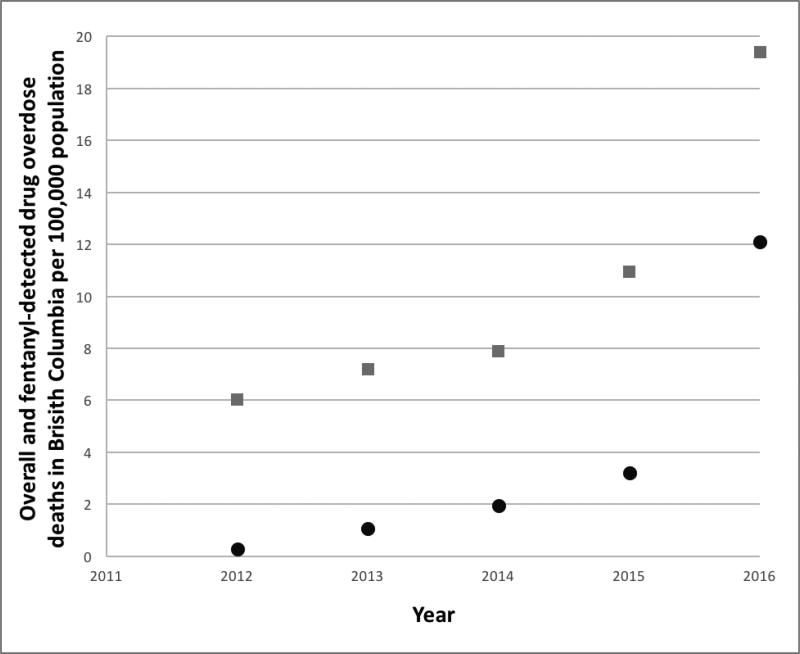
Similarly, the rate of overall OD deaths in B.C. fluctuated between 2000 and 2008 but tripled between 2012 and 2016 to a new high of 19.4 deaths per 100,000 population (Figure 2). Also, since fentanyl-detected OD deaths were first documented in B.C. in 2012, they have increased more than 40-fold from 0.3 to 12.1 per 100,000 people in 2012 and 2016 respectively (Figure 2). Furthermore, the proportion of OD deaths in which fentanyl was detected increased from 4% to 62% over that same period of time.
Figure 2.
Overall and fentanyl-detected illicit drug overdose deaths in British Columbia from 2012–2016.
*Data obtained from the BC Coroner’s Service. Circle = fentanyl-detected, square = overall
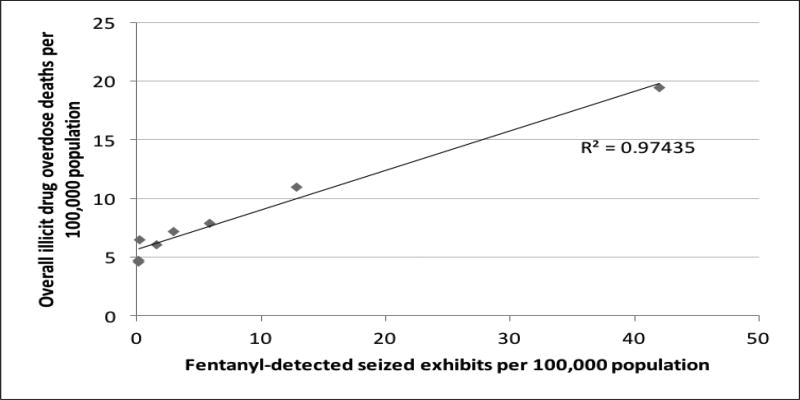
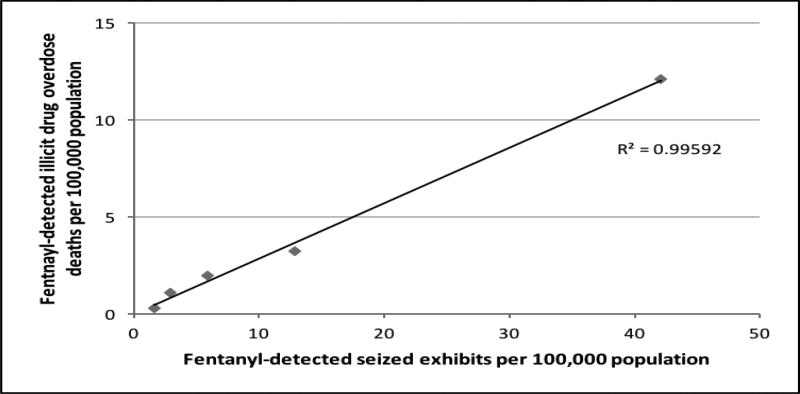
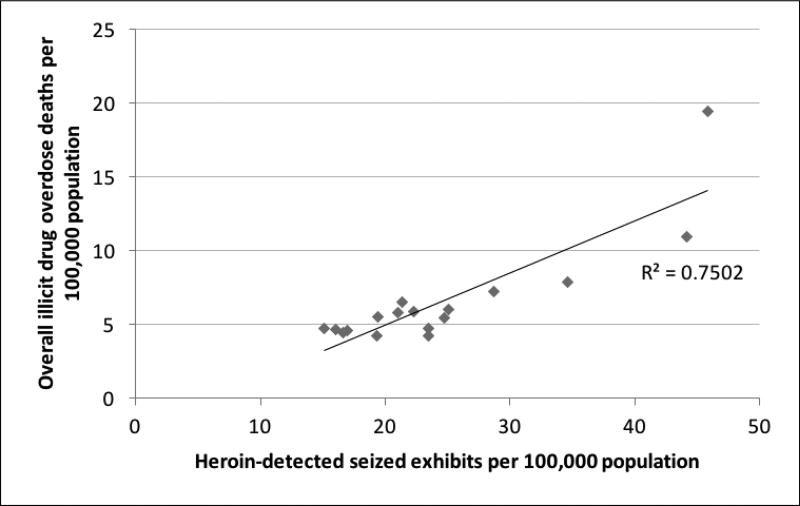
The scatter plots with associated trend lines and R2 values are shown in Figures 3–5. The regression analysis revealed that there is a strong positive relationship between the number of seized fentanyl samples and total OD deaths (R2 = 0.97) as well as a between seized fentanyl and fentanyl-detected OD deaths (R2 = 0.99). There was also an association between the number of seized heroin samples and total OD deaths (R2 = 0.75).
Figure 3.
Overall illicit drug overdose deaths and fentanyl-detected seized exhibits per 100,000 population
Figure 5.
Fentanyl-detected illicit drug overdose deaths and fentanyl-detected seized drug exhibits per 100,000 population
4. Interpretation
The numbers of seized fentanyl and heroin samples, as well as both total illicit drug OD deaths and fentanyl-detected OD deaths, have all been rising rapidly in B.C. since 2009. We have identified a positive association between seized fentanyl and total unintentional OD deaths that is stronger than the relationship between seized heroin and total unintentional OD deaths. This suggests that, though both may be contributing, illicit fentanyl use may be more closely related than illicit heroin use to the increase in OD deaths seen in B.C. from 2009–2016.
We identified a strong association between the number of tested samples of seized drugs where fentanyl was detected and unintentional OD deaths in which fentanyl was detected. Our findings are consistent with the findings in the US that illicit fentanyl use is becoming more prevalent, and OD is correlated to illicit drug seizure of fentanyl but not related to fentanyl prescribing rates (Gladden, 2016; Suzuki and El-Haddad, 2017). Also, in a recent study from a supervised injection site in Sydney, Australia, fentanyl injections had approximately four and half times the risk of resulting in OD than heroin and prescription opioid injections combined (Latimer et al., 2016).
Previous studies have shown a significant proportion of drug users are unintentionally ingesting fentanyl, unaware of its presence in the substances they are taking (Amlani et al., 2015; Klar et al., 2016). The current study complements this finding by showing fentanyl was detected with a large variety of illicit drug classes in samples analyzed by the DAS, particularly stimulants. In 2016, 96% of OD deaths in B.C. contained methamphetamine, 46% cocaine/crack, and 30% heroin, yet it remains unclear if the people involved took these combinations knowingly. Furthermore, the exponential increase in tested seized fentanyl and fentanyl-detected OD deaths since 2012, and the strong association between the two variables, suggests that concerns regarding the current perceived threat of illicit fentanyl use are warranted. Previous studies have identified the potency of fentanyl and resulting easy concealment and transportation, in addition to its low production cost, as key factors leading to its expanding presence on the black market (Suzuki and El-Haddad, 2017). According to the US Drug Enforcement Agency, fentanyl-laced pills can be sold as counterfeit oxycodone for $10–20 a pill, which means that a kilogram of pure fentanyl purchased from illicit overseas suppliers for a few thousand dollars can be turned into revenue as high as $20 million dollars (Drug Enforcement Administration, 2016). Such financial incentives will likely continue to drive the production of counterfeit pills containing illicitly manufactured fentanyl (Suzuki and El-Haddad, 2017).
The information derived from this study may be of particular interest to family physicians, emergency room physicians, nurse practitioners, and first responders in British Columbia, who are often the initial point of health care contact for persons who use illicit drugs. Given the clear trend in increasing fentanyl detected in seized drug samples and fentanyl-detected OD deaths, it is recommended that health care providers discuss the possible harms of fentanyl use with their patients who are most at risk. This should include a discussion of the risk of unknowingly consuming fentanyl in patients who use any illicit recreational drugs (particularly heroin or stimulants), the potential for lethality with fentanyl use, and measures to mitigate this harm. It is imperative that evidence-based treatment and harm reduction strategies be offered including opioid agonist therapies (buprenorphine/naloxone, methadone, extended release morphine), antagonist therapy (oral or injectable naltrexone), addiction counseling, outpatient and/or residential programs, take-home naloxone kits, and supervised injection sites (Bird et al., 2016; Drucker et al., 2016; Lee et al., 2016; Mattick et al., 2008, Mattick et al., 2009; McAuley et al., 2015; Minozzi et al., 2011; Tanum et al., 2017; Veilleux et al., 2010; Volkow, 2017). Point of care urine drug screening may allow drug users to gain feedback as to the content of drugs they have ingested recently. Access to consumer testing of drug samples, although yet to be studied with much rigor, has been a recent strategy employed in B.C. to increase awareness with the intention of reducing the risk of harm (Sherren, 2015).
There are several potential limitations to this study. Gaps exist in knowledge with regards to the actual composition of illicit drugs available for purchase on the black market. It is unclear how accurately the drug seizure composition data provided by the DAS represents the actual content of illicit drugs being consumed by drug users across the province. The data do not include analogues of fentanyl, and thus they may underestimate related ODs and seized drug content. Further, the DAS was unable to provide regionally stratified data within B.C., whether samples were submitted by the Canada Border Services Agency or by local law enforcement agencies, or the quantity of drugs seized for each exhibit. In addition, the DAS requests that exhibits be submitted for testing only when verification of the substances in question is required for court or other purposes, and multiple exhibits may be submitted from the same drug seizure. As a result of all of these limitations, the DAS expressed in a statement that “exhibits analyzed by DAS likely represent a subset of the substances seized by law enforcement agencies, which would also be a subset of the substances found on the illicit market” (Petts, 2016). Furthermore, it is difficult to determine if the increases in the number of seized illicit drugs identified in this study represent a change in the pattern of what is available for purchase on the black market or a change in law enforcement practices. From these data we are unable to determine what proportion of the people who died had an opioid use disorder and what proportion were casual or experimental users. These challenges highlight the difficulty of studying illicit substance use and suggest a need for developing more rigorous methods of sampling and analyzing the content of the illicit drugs that are being consumed from the black market. While caution should be applied when extrapolating the analyses of seized drug data to represent the composition of street drugs, these data reflect the best available information about what may be present in the illicit market in B.C. at the present time.
The current study supports public health concerns regarding the increasing prevalence of illicit fentanyl use and associated unintentional OD mortality. It also validates reports that fentanyl is being combined with other substances and may be consumed unknowingly by individuals who use other illicit substances. An array of treatment and harm reduction strategies need to be implemented to potentially curb the rise in opioid-related deaths in BC.
Figure 4.
Overall illicit drug overdose deaths and heroin-detected seized exhibits
Highlights.
This study compares illicit drug seizure content to BC opioid deaths from 2009–16.
Fentanyl seizure and overall opioid-detected deaths were highly correlated.
Heroin seizure and overall opioid-detected deaths were highly correlated.
Seized fentanyl exhibits were increasingly found to contain other illicit drugs.
Illicit fentanyl, often mixed with other drugs, contributed to overdose deaths in BC.
Acknowledgments
Role of Funding Source
At the time of the initiation of the research, Drs. Baldwin, Gray and Goel were family medicine residents supported by Vancouver Coastal Health and the UBC Department of Family Practice, and Dr. Rieb was a Canadian Addiction Medicine Research Fellow through St. Paul’s Hospital supported by a US National Institute of Drug Abuse (R25 DA037756-02). Dr. Wood is supported in part by a Tier 1 Canada Research Chair in Inner-City Medicine award. The funders had no role in the design and conduct of this study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
The authors wish to thank staff at DAS and BCCS for providing the raw data used in this analysis, Dr. Rita McCracken for encouragement, and Dr. Jonathan Berkowitz for statistical guidance.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
“Fentanyl-related” OD death is the term typically used in the US and elsewhere in Canada to indicate fentanyl found on biologic testing, and attributes the cause of death to fentanyl.
“Fentanyl-detected” OD death is the term typically preferred by the B.C. coroner service (instead of “fentanyl-related”) since it does not presume definitive attribution of the cause of death.
Contributors
The principal investigator and corresponding author, Dr. Rieb, supervised and helped to formulate the research question with the three Family Medicine Residents, Drs. Baldwin, Gray, and Goel. Dr. Gray ran the statistics and generated the tables and figures. All four doctors and the other co-authors, Drs. Buxton and Wood, assisted with conceptual development, interpretation, and manuscript writing. All authors have read and approved of the final version of the manuscript.
Conflict of interest
The authors have no conflicts of interest to declare.
References
- Amlani A, McKee G, Khamis N, Raghukumar G, Tsang E, Buxton JA. Why the FUSS (Fentanyl Urine Screen Study)? A cross-sectional survey to characterize an emerging threat to people who use drugs in British Columbia, Canada. Harm. Reduct. J. 2015;12 doi: 10.1186/s12954-015-0088-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- British Columbia Government, Office of the Surgeon General. B.C. Coroners Service warns of deaths related to illicit fentanyl use. 2014 Accessed at: https://news.gov.bc.ca/06336.
- Bird SM, McAuley A, Perry S, Hunter C. Effectiveness of Scotland’s national naloxone program for reducing opioid-related deaths: A before (2006–10) versus after (2011–13) comparison. Addict. Abingdon Engl. 2016;111:883–891. doi: 10.1111/add.13265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- B.C. Coroner’s Service. Illicit drug overdose deaths in B.C. January 1, 2007 – March 31 2017. Victoria: British Columbia Coroner’s Service; 2017a. [Google Scholar]
- B.C. Coroner’s Service. Fentanyl-detected illicit drug overdose deaths January 1, 2012 – February 28, 2017. Victoria: British Columbia Coroner’s Service; 2017b. [Google Scholar]
- B.C. Gov. News. Provincial Health Officer declares public health emergency. 2016 Accessed at: https://news.gov.bc.ca/releases/2016HLTH0026-000568.
- Canadian Centre on Substance Abuse. CCENDU Bulletin: Deaths involving fentanyl in Canada, 2009–2014. Ottawa: Canadian Centre on Substance Abuse; 2015. [Google Scholar]
- CBC News Interactive: Canada - Substance abuse. CBC News. Accessed at: http://www.cbc.ca/news2/interactives/map-canada-substance-abuse.
- CDC. Nonpharmaceutical Fentanyl-Related Deaths - Multiple States, April 2005–March 2007. Center for Disease Control; Atlanta: 2008. [PubMed] [Google Scholar]
- Drug Enforcement Administration. Counterfeit prescription pills containing fentanyls: A global threat. 2016 DEA-DCT-DIB-021-16. [Google Scholar]
- Dauvergne M. Trends in police-reported drug offences in Canada. Ottawa: Statistics Canada; 2009. [Google Scholar]
- Denton JS, Donoghue ER, McReynolds J, Kalelkar MB. An epidemic of illicit fentanyl deaths in Cook County, Illinois: September 2005 through April 2007. J. Forensic Sci. 2008;53:452–454. doi: 10.1111/j.1556-4029.2008.00669.x. [DOI] [PubMed] [Google Scholar]
- Drucker E, Anderson K, Haemmig R, Heimer R, Small D, Walley A, Wood E, van Beek I. Treating addictions: Harm reduction in clinical care and prevention. J. Bioethical Inq. 2016 doi: 10.1007/s11673-016-9720-6. [DOI] [PubMed] [Google Scholar]
- Fischer B, Argento E. Prescription opioid related misuse, harms, diversion and interventions in Canada: A review. Pain Physician. 2012;15:ES191–203. [PubMed] [Google Scholar]
- Frank RG, Pollack HA. Addressing the fentanyl threat to public health. N. Engl. J. Med. 2017;376:605–607. doi: 10.1056/NEJMp1615145. [DOI] [PubMed] [Google Scholar]
- Gladden RM. Fentanyl law enforcement submissions and increases in synthetic opioid–involved overdose deaths — 27 States, 2013–2014. MMWR Morb. Mortal. Wkly. Rep. 2016;65 doi: 10.15585/mmwr.mm6533a2. [DOI] [PubMed] [Google Scholar]
- Health Canada. Canadian Alcohol and Drug Use Monitoring Survey. 2014 Accessed at: https://www.canada.ca/en/health-canada/services/health-concerns/drug-prevention-treatment/canadian-alcohol-drug-use-monitoring-survey.html.
- Hull MJ, Juhascik M, Mazur F, Flomenbaum MA, Behonick GS. Fatalities associated with fentanyl and co-administered cocaine or opiates. J. Forensic Sci. 2007;52:1383–1388. doi: 10.1111/j.1556-4029.2007.00564.x. [DOI] [PubMed] [Google Scholar]
- Klar SA, Brodkin E, Gibson E, Padhi S, Predy C, Green C, Lee Vi. Furanyl-fentanyl overdose events caused by smoking contaminated crack cocaine — British Columbia, Canada, July 15–18, 2016. MMWR Morb. Mortal. Wkly. Rep. 2016;65 doi: 10.15585/mmwr.mm6537a6. [DOI] [PubMed] [Google Scholar]
- Lake S, Wood E, Buxton J, Dong H, Montaner J, Kerr T. Prescription opioid use and non-fatal overdose in a cohort of injection drug users. Am. J. Drug Alcohol Abuse. 2015;41:257–263. doi: 10.3109/00952990.2014.998366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Latimer J, Ling S, Flaherty I, Jauncey M, Salmon AM. Risk of fentanyl overdose among clients of the Sydney medically supervised injecting centre. Int. J. Drug Policy. 2016;37:111–114. doi: 10.1016/j.drugpo.2016.08.004. [DOI] [PubMed] [Google Scholar]
- Lee JD, Friedmann PD, Kinlock TW, Nunes EV, Boney TY, Hoskinson RAJ, Wilson D, McDonald R, Rotrosen J, Gourevitch MN, Gordon M, Fishman M, Chen DT, Bonnie RJ, Cornish JW, Murphy SM, O’Brien CP. Extended-release naltrexone to prevent opioid relapse in criminal justice offenders. N. Engl. J. Med. 2016;374:1232–1242. doi: 10.1056/NEJMoa1505409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manchikanti L, Helm S, Fellows B, Janata JW, Pampati V, Grider JS, Boswell MV. Opioid epidemic in the United States. Pain Physician. 2012;15:ES9–38. [PubMed] [Google Scholar]
- Mattick RP, Breen C, Kimber J, Davoli M. Methadone maintenance therapy versus no opioid replacement therapy for opioid dependence. Cochrane Database Syst. Rev. 2009;8:CD002209. doi: 10.1002/14651858.CD002209. [DOI] [PubMed] [Google Scholar]
- Mattick RP, Kimber J, Breen C, Davoli M. Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence. Cochrane Database Syst. Rev. 2004;3:CD002207. doi: 10.1002/14651858.CD002207.pub2. [DOI] [PubMed] [Google Scholar]
- McAuley A, Aucott L, Matheson C. Exploring the life-saving potential of naloxone: A systematic review and descriptive meta-analysis of take home naloxone (THN) programs for opioid users. Int. J. Drug Policy. 2015;26:1183–1188. doi: 10.1016/j.drugpo.2015.09.011. [DOI] [PubMed] [Google Scholar]
- McKee G, Amiani A, Buxton J. Illicit fentanyl: An emerging threat to people who use drugs in B.C. B. C. Med. J. 2015;57:235. [Google Scholar]
- Minozzi S, Amato L, Vecchi S, Davoli M, Kirchmayer U, Verster A. Oral naltrexone maintenance treatment for opioid dependence. Cochrane Database Syst. Rev. 2011;13:CD001333. doi: 10.1002/14651858.CD001333.pub2. [DOI] [PubMed] [Google Scholar]
- Paulozzi LJ, Budnitz DS, Xi Y. Increasing deaths from opioid analgesics in the United States. Pharmacoepidemiol. Drug Saf. 2006;15:618–627. doi: 10.1002/pds.1276. [DOI] [PubMed] [Google Scholar]
- Petts L. UBC Family Practice Research Project. Data Request 2016 [Google Scholar]
- Sherren R. Why some music festivals are vetting rather than banning drugs. CBC News. 2015 Accessed at: http://www.cbc.ca/news/health/why-some-music-festivals-are-vetting-rather-than-banning-drugs-1.3193954.
- Suzuki J, El-Haddad S. A review: Fentanyl and non-pharmaceutical fentanyls. Drug Alcohol Depend. 2017;171:107–116. doi: 10.1016/j.drugalcdep.2016.11.033. [DOI] [PubMed] [Google Scholar]
- Tanum L, Solli KK, Latif Z-E-H, Benth JŠ, Opheim A, Sharma-Haase K, Krajci P, Kunøe N. The effectiveness of injectable extended-release naltrexone vs daily buprenorphine-naloxone for opioid dependence: A randomized clinical noninferiority trial. JAMA Psychiatry. 2017;74:1197–1205. doi: 10.1001/jamapsychiatry.2017.3206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Veilleux JC, Colvin PJ, Anderson J, York C, Heinz AJ. A review of opioid dependence treatment: Pharmacological and psychosocial interventions to treat opioid addiction. Clin. Psychol. Rev. 2010;30:155–166. doi: 10.1016/j.cpr.2009.10.006. [DOI] [PubMed] [Google Scholar]
- Volkow ND. Medications for opioid use disorder: Bridging the gap in care. Lancet. 2017;391:285–287. doi: 10.1016/S0140-6736(17)32893-3. [DOI] [PubMed] [Google Scholar]