Abstract
ADHD is associated with automobile crashes, traffic fatalities, and serious road trauma, but it is unclear whether this risk is (a) driven by ADHD symptoms specifically, and (b) unique to ADHD or transdiagnostic across psychiatric disabilities, such as depression, that also have concentration problems as core symptoms. The current study provides the first prospective, continuously-monitored evaluation of crash risk related to ADHD symptoms, including the first on-road comparison of ADHD with another high-prevalence psychiatric disability (depression). A probability-based sample of 3,226 drivers from six U.S. sites, including subsamples with self-reported ADHD (n=274) and depression (n=251), consented to have their vehicles outfitted with sophisticated data acquisition technologies to continuously monitor real-world, day-to-day driving from ‘engine-on to engine-off’ for 1-2 years (Mean=440 consecutive days/driver, Mean=9,528 miles/driver). Crashes and near-crashes were objectively identified via software-based algorithms and double-coded manual validation (blinded to clinical status). Miles driven, days monitored, age, gender, education, and marital status were controlled. ADHD symptoms portended 5% increased crash risk per increase in symptom severity score (IRR=1.05). This risk corresponded to approximately 1 biennial crash and 1 annual near-crash per driver with ADHD; crash risk doubled for drivers reporting ADHD symptom severity near the sample’s maximum. Analyses based on self-reported clinical status indicated similarly elevated rates for ADHD (IRR=1.46) and depression (IRR=1.34) that may be related, in part, to both groups’ inattention/concentration symptoms. Risk was not attenuated by ADHD usual treatment, but varied according to antidepressant medication status. Previous studies have significantly underestimated the risk for traffic crashes conveyed by ADHD and depression.
Keywords: ADHD, Depression, Motor Vehicle Driving, Accidents, Prospective, SHRP-2
Motor vehicle crashes are a leading cause of death in the U.S.1 and occur disproportionately among individuals with high-prevalence psychiatric disorders such as ADHD2 and Depression.3 Converging evidence indicates that drivers with ADHD4,5,6,7 and drivers with Depression8,9 have higher rates of adverse driving outcomes than healthy control drivers across a broad range of metrics that include crashes, citations, insurance claims, loss of licenses, serious crash-related injuries, and traffic fatalities.6,10,11,12,13 These findings have major public health implications when juxtaposed with the high prevalence of adult ADHD (4%)14 and Depression (7%–13%).15
Meta-analytic evidence supports a robust link between ADHD (RR=1.23-1.88), Depression (RR=1.67-1.90) and motor vehicle crash risk.5,16,45 However, the veracity of these estimates has been questioned due to uncontrolled confounds5 and the paucity of prospective, on-road data.2,17 As a result, there is significant evidence that the magnitude of these links has been both overestimated5 and underestimated.7 For example, the most recent meta-analysis concluded that ADHD’s true risk was modest, and conveyed in large part by extra-disorder factors including greater exposure, demographic risk factors (e.g., male gender), and/or concomitant transdiagnostic risk factors.5 In contrast, emerging evidence suggests that ADHD’s true risk may have been significantly underestimated. Only one study has prospectively assessed ADHD’s crash risk using objective, in-car monitoring of routine driving (N=17), and found that over 60% of crashes involving drivers with ADHD were not reported to authorities/insurance companies18. Similarly, additional evidence suggests that drivers with ADHD may systematically underreport their driving errors in self-report studies.19,20
Official police/government records have been used to address these concerns, but are limited to crashes on public roads and decisions to report the crash (drivers), send an officer (police dispatch), and file an official report (officer).21 Further, national registers and hospital database reviews have been limited to crashes that involve death or severe road trauma.10,12 Simulator studies and standardized on-road driving tests address some of these limitations, but provide time-limited evaluation of driving skills under ideal conditions that may not correspond to day-to-day driving habits and in-car distractions.8,22,23 In addition, fewer than 50% of studies report miles driven, despite the known association between exposure and crash risk.4 Finally, the correspondence between retrospective self-report and prospective crash risk is unknown.
An additional limitation of this literature is the paucity of empirical studies directly comparing multiple forms of high prevalence psychiatric disability.7 These comparisons are particularly critical for understanding ADHD-related risk given the nonspecific nature of core ADHD symptoms,2,11 and questions regarding the extent to which ADHD specifically, or psychiatric disability in general, portends risk for adverse driving outcomes.5 For example, Depression is another high prevalence psychiatric disability associated with both attention/concentration problems and increased crash risk.9,24, 25 In the only empirical study to date, to our knowledge, that directly compared ADHD and Depression, Aduen and colleagues found that only ADHD was associated with multiple collisions and violations, whereas only Depression was associated with self-reported injury following a collision.11 However, Aduen relied exclusively on retrospective self-report data, despite concerns regarding the reliability of self-reported driving outcomes for these groups.19,20
The current study prospectively follows the large cohort of drivers from Aduen11 and is well positioned to address issues related to both overestimation and underestimation of crash risk via (1) robust control for exposure and multiple risk factors for crashes26 that are also correlates of ADHD,4,7 and (2) large-scale, continuous-monitoring of adverse outcomes during routine driving as a function of ADHD symptom severity and clinical status. This multisite sample of 3,226 drivers was surveyed for ADHD symptoms, psychiatric status, and prior crash involvement. Their driving was then monitored continuously using in-car technologies that recorded, on average, 9,500 miles of routine driving from ‘engine-on to engine-off’ over a span of 440 consecutive days per driver (totaling >5.5 million recorded trips).
Primary analyses focused on prospective crash risk portended by ADHD symptom severity. Exploratory analyses examined risk as a function of clinical group designations identified at study entry,11 medication treatment assessed at study entry and exit, and correspondence between retrospective self-report and prospective crash risk. We hypothesized that ADHD symptom severity would portend increased risk for future adverse driving outcomes.4,5,6 Based on the retrospective self-report data from this sample,11 we expected the exploratory clinical group analyses to show increased crash risk for ADHD but not Depression. We also expected medication to attenuate crash risk, such that medicated drivers with ADHD/Depression would show lower crash risk relative to unmedicated drivers with ADHD/Depression.6,8,9,18 Finally, we expected retrospective self-report to predict prospective crash risk for healthy control drivers, but made no predictions regarding these relations among drivers with ADHD and Depression given the paucity of previous research.
Method
Design and Overview
Probability-based sampling was employed to obtain a representative sample of 3,600 licensed drivers (3,226 were followed prospectively, including 2,329 of the 2,354 drivers assigned to a clinical/comparison group by Aduen).11 Drivers were oversampled for younger and older drivers across 6 U.S. sites: Florida (Tampa), Indiana (Bloomington), North Carolina (Durham), New York (Buffalo), Pennsylvania (State College), and Washington (Seattle). Sample demographics are shown in Table 1, and were controlled in all analyses based on prior evidence that each covariate is associated with adverse driving outcomes (age, gender, education/socioeconomic status, marital status, miles driven, and days of study monitoring).23,27 Detailed sample descriptives and population-based comparisons with U.S. licensed drivers are provided in Antin (2015).28 Comparisons indicate close approximation to U.S. drivers for the sample. Technical reporting of the Strategic Highway Research Program Naturalistic Driving Study (SHRP-2) study design, recruitment, and methodological plans are found in Antin (2011).29
Table 1.
Sample demographics.
| Overall Sample (N=3,226) | ADHD (N=274) | Depression (N=249) | Healthy Control (N=1,806) | Clinical Subgroup Chi-square | |||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| M | SD | M | SD | M | SD | M | SD | ||
| Miles Driven | 9527.9 | 7315.8 | 9874.2 | 7346.9 | 9716.6 | 6846.1 | 9390.9 | 7510.0 | p=.53, ns |
| Days Monitored | 440.49 | 210.65 | 423.39 | 202.68 | 442.17 | 210.34 | 439.85 | 213.36 | p=.46, ns |
| BAQS ADHD Score | 3.20 | 2.18 | 7.43 | 2.57 | 3.39 | 1.63 | 1.86 | 1.01 | p<.0005 |
| Percent involved in | |||||||||
| No crashes | 70.3% | 58.8% | 64.7% | 72.8% | p<.001 | ||||
| Single crash | 19.9% | 23.4% | 21.7% | 19.1% | |||||
| Multiple crashes | 9.8% | 17.9% | 13.7% | 8.1% | |||||
| No near-crashes | 61.7% | 52.2% | 52.2% | 64.4% | p<.001 | ||||
| Single near-crash | 21.7% | 25.5% | 24.5% | 20.8% | |||||
| Multi. near-crashes | 16.6% | 22.3% | 23.3% | 14.8% | |||||
| Age Group | N | % | N | % | N | % | N | % | p<.005 |
| 16-17 | 258 | 8.0 | 40 | 14.7 | 13 | 5.2 | 126 | 7.0 | |
| 18-20 | 520 | 16.1 | 71 | 26.0 | 39 | 15.7 | 248 | 13.8 | |
| 21-25 | 597 | 18.5 | 77 | 28.2 | 53 | 21.3 | 280 | 15.5 | |
| 26-35 | 327 | 10.1 | 25 | 9.2 | 25 | 10.0 | 192 | 10.6 | |
| 36-50 | 349 | 10.8 | 25 | 9.2 | 38 | 15.3 | 198 | 11.0 | |
| 51-65 | 383 | 11.9 | 11 | 4.0 | 37 | 14.9 | 234 | 13.0 | |
| 66-75 | 345 | 10.7 | 12 | 4.4 | 28 | 11.2 | 213 | 11.8 | |
| 75+ | 442 | 13.7 | 12 | 4.4 | 16 | 6.4 | 312 | 17.3 | |
| Not reported | 5 | 0.2 | 1 | 0.004 | 0 | 0.0 | 3 | 0.002 | |
| Gender | p<.005 | ||||||||
| Male | 1537 | 47.6 | 131 | 48.3 | 75 | 30.4 | 900 | 50.3 | |
| Female | 1661 | 51.5 | 140 | 51.7 | 172 | 69.6 | 890 | 49.7 | |
| Not Reported | 28 | 0.9 | 3 | 0.01 | 2 | 0.001 | 16 | 0.001 | |
| Education | p<.005 | ||||||||
| Some high school | 271 | 8.4 | 39 | 14.3 | 14 | 5.7 | 126 | 7.0 | |
| H.S. graduate | 1241 | 38.5 | 118 | 43.2 | 100 | 40.5 | 660 | 36.8 | |
| College degree + | 1692 | 52.4 | 116 | 42.5 | 133 | 53.8 | 1006 | 56.1 | |
| Not reported | 22 | 0.7 | 1 | 0.003 | 2 | 0.001 | 14 | 0.008 | |
| Marital Status | p<.005 | ||||||||
| Not Married | 1989 | 61.7 | 211 | 77.9 | 162 | 65.3 | 1054 | 58.9 | |
| Married | 1207 | 37.4 | 60 | 22.1 | 86 | 34.7 | 734 | 41.1 | |
| Not reported | 30 | 0.9 | 3 | 0.01 | 1 | 0.004 | 18 | 0.001 | |
| Annual Income | p=.04 | ||||||||
| Under $29K | 556 | 17.2 | 60 | 21.9 | 52 | 20.9 | 282 | 15.6 | |
| $30K to $39K | 378 | 11.7 | 26 | 9.5 | 27 | 10.8 | 233 | 12.9 | |
| $50K to $69K | 537 | 16.6 | 36 | 13.1 | 39 | 15.7 | 297 | 16.4 | |
| $70K to $99K | 551 | 17.1 | 36 | 13.1 | 44 | 17.7 | 316 | 17.5 | |
| $100K to $149K | 462 | 14.3 | 37 | 13.5 | 36 | 14.5 | 258 | 14.3 | |
| $150K or higher | 219 | 6.8 | 28 | 10.2 | 14 | 5.6 | 133 | 7.4 | |
| Not reported | 523 | 16.2 | 51 | 18.6 | 37 | 14.9 | 287 | 15.9 | |
Note: BAQS = Barkley Adult ADHD Quick Screen.
Continuous Monitoring and Event Triggers
Each driver’s car was outfitted with five high-speed video cameras, speed/brake monitors, accelerometers, and GPS to continuously capture routine driving from engine-on to engine-off for 1-2 consecutive years per driver (5,512,900 individual trips that occurred between 2010 and 2013).29 Software-based trigger algorithms with 100% double-coded manual validation identified 4,254 safety-critical events (SCEs; 1,549 crashes, 2,705 near-crashes). These software-based algorithms used kinematic and behavioral signatures previously identified as present with high probability during crashes (e.g., longitudinal deceleration < −0.65g, lateral acceleration >0.75g).28,29 Detailed data reduction methods, software-based trigger algorithms and validation, vehicle sensor calibration, data reductionist training, and reliability are provided in Hankey (2016).30
All SCEs were verified by comparing event videos with pre-recorded index images to ensure the consented participant was driving. Manual video review then verified if an SCE occurred. Verified events were coded by extensively trained data reductionists (100% SCEs coded by >2 coders; reliability=91%).28,29 Coders were blind to driver clinical status.29
Prospective Driving Outcomes
Primary outcomes included number of crashes (SCEs involving any contact between participant vehicle and fixed or moving object, at any speed where kinetic energy is measurably transferred or dissipated) and near-crashes (SCEs requiring a rapid, evasive maneuver by participant vehicle to avoid an imminent crash) recorded during prospective on-road monitoring.
Barkley Adult ADHD Quick Screen (BAQS)
After enrollment, all participants completed the BAQS, a 6-item self-report questionnaire that assesses ADHD symptoms in adults on a 4-point scale (0=never/rarely, 1=sometimes, 2=often, 3=very often; range=0-18). Scores are summed across the six items and correlate .97 with scores from full, 18-item DSM-IV symptom checklists.31 Psychometric support includes high internal consistency (α=.90) and concurrent validity for self-reported (r=.97) and other-report (r=.68) 18-item ADHD symptom checklists. The predictive validity is adequate for self-reported (r=.87) and other-reported impairment (r=.67), in addition to high sensitivity (.93) and specificity (.97) for differentiating adults with ADHD from neurotypical adults based on a clinical cut-off score of ≥7.31
Clinical Groups
Overview
Exploratory clinical group analyses were conducted using the diagnostic groups defined for this sample at study entry.11 Briefly, Aduen (2015)11 identified 275 drivers with ADHD and 1,828 drivers with no known psychopathology (Healthy Controls) based on self-reported current clinical status and symptoms at study entry. They also identified 251 drivers with Depression, who are included here to provide the first on-road comparison of ADHD with another high-prevalence psychiatric disorder32 associated with attention/concentration problems24,33 and adverse driving outcomes.25 Clinical group comparisons were conducted using these psychiatric diagnoses,11 and are considered exploratory because the naturalistic study design precluded clinical interviewing or tracking illness course/treatment efficacy during the prospective monitoring of driving outcomes.
Group assignment
Group membership at study entry was defined by Aduen11 from an initial sample of 3,259 participants as follows: Participants were included in the ADHD Group with a positive BAQS screen (>7) and/or self-reported ADHD, alone (n=229) or comorbid with anxiety (n=46; total n =275). Participants with positive BAQS screens who reported other clinical disorders but not ADHD (n=52) were excluded from the ADHD group as recommended because 83% of mood disorders screen positive on the BAQS.31 Participants were included in the Depression Group if they endorsed Depression, alone (n=170) or comorbid with anxiety (n=81)a, but not ADHD (total n=251); no BAQS criteria were set for the Depression Group. Individuals with self-reported anxiety were included given its high comorbidity with both adult ADHD and Depression.31 Individuals were assigned to the Healthy Control Group (no known psychopathology) based on negative BAQS screen (< 4) and no self-reported psychological diagnoses (n=1,828). Participants were excluded from all groups if they self-reported personality, psychotic, or bipolar disorders (n=32). The remaining 821 cases were excluded for failing to meet any group criteria (i.e., no self-reported Depression and BAQS scores of 4-6 that fell between the Healthy Control maximum and ADHD minimum).
Psychiatric Treatment
ADHD and antidepressant medications were queried at study entry and exit29 and used as a proxy for active treatment.18 Consistent with epidemiological estimates,34,35 20.8% and 61.0% of drivers with ADHD and Depression, respectively, reported disorder-specific medication treatment at one or both time points. Exploratory analyses were conducted by subdividing the ADHD and Depression groups into mutually exclusive categories: Unmedicated (no reported medication that treats their identified disorder at either time point), Started (reported at exit but not entry), Stopped (reported at entry not exit), and Medicated (reported at both time points).
Cell sizes were sufficient for exploratory analyses of antidepressant time course for the Depression group (Unmedicated=99; Started=98; Stopped=24; Medicated=30). ADHD medication was dichotomized based on medication at either time point (No=218; Yes=57) due to insufficient cell counts (Unmedicated=218; Started=43; Stopped=12; Medicated=2). The naturalistic study design precluded monitoring of perceived medication efficacy, emergent effects, or timing in relation to crashes. Nevertheless, these analyses reflect the most extensive examination to date of the protective effects of medication treatment against crashes during real-world, day-to-day driving.
Data Analysis Overview
Negative binomial regressions predicted the maximum likelihood (MLE) conditional probability (incident rate ratios; IRR with Wald 95%CIs)36 of crash and near-crash counts as a function of ADHD symptom severity scores, controlling for miles driven, days of continuous monitoring (exposure), age, gender, education, and marital status. Separate models were run for crashes and near-crashes. To aid interpretation, IRRs are supplemented with estimates of annual risk per driver by computing estimated marginal means with time set to 365.25 days and miles driven set to the U.S. national average of 15,000 annual miles driven.37
Exploratory analyses repeated these models, first substituting the categorical clinical groups11 (ADHD, Depression, Healthy Control) for BAQS scores, and finally subdividing the ADHD and Depression groups by medication status.
All models were superior to the null model (all omnibus likelihood ratio χ2[14]≥218.01, all p<.0005) and demonstrated adequate goodness-of-fit (all χ2/df =1.07-1.24). The dispersion coefficient (negative binomial) was significantly greater than 0.0 for all models (all 95%CIs exclude 0.0), supporting use of the negative binomial over Poisson distribution models.
Ethics Statement
Participants gave informed consent before participating. Participants were protected by a national Certificate of Confidentiality and not required to surrender study-related materials to authorities.29
Results
Preliminary Analyses
Missing data ranged from 0.1-0.9% for gender, age, education, and marital status and did not vary by clinical group (p=.60), supporting Missing at Random (MAR) assumptions. Education served as a proxy for socioeconomic status.26 Sample retention was excellent: 3,226 cases (89.6%) were followed prospectively and included in analyses. Of the 2,354 drivers assigned to a clinical or control group at study entry,11 2,329 (98.9%) were retained including 274 of 275 drivers with ADHD (99.6%), 249 of 251 drivers with Depression (99.2%), and 1,806 of 1,828 Healthy Control drivers (98.8%). These groups did not differ in miles driven (mean=9,527.90 miles; p=.53), days of study participation (mean=440.49 days; p=.46), or performance on a driving knowledge questionnaire (meancorrect=79.74%; p=.14). Group differences in demographics are detailed in Aduen,11 and include differences in gender (more females in the Depression group), age (ADHD overrepresented in the youngest age groups and underrepresented in the oldest age groups), marital status (ADHD drivers less likely to be married), and education (ADHD drivers less likely to have a high school diploma or college degree). These demographic variables were included as covariates in all subsequent analyses.
ADHD Symptoms
Greater ADHD symptoms at study entry portended 5%–6% increased risk per increase in symptom severity score for crashes (IRR=1.05, 95%CI=1.02-1.09, p<.0005), and near-crashes (IRR=1.06, 95%CI=1.03-1.09, p<.0005). Annual number of expected crashes/near-crashes as a function of BAQS ADHD symptom severity score is depicted in Figure 1. Notably, risk increases per ADHD symptom severity endorsement;b for example, a BAQS score of 17 predicts approximately 1 annual crash per driver (0.99 crashes/driver), while a BAQS score of 0 predicts 1 crash per 2.4 drivers (0.41 crashes/driver). Figure 2 shows these estimates as a function of age group.
Figure 1.
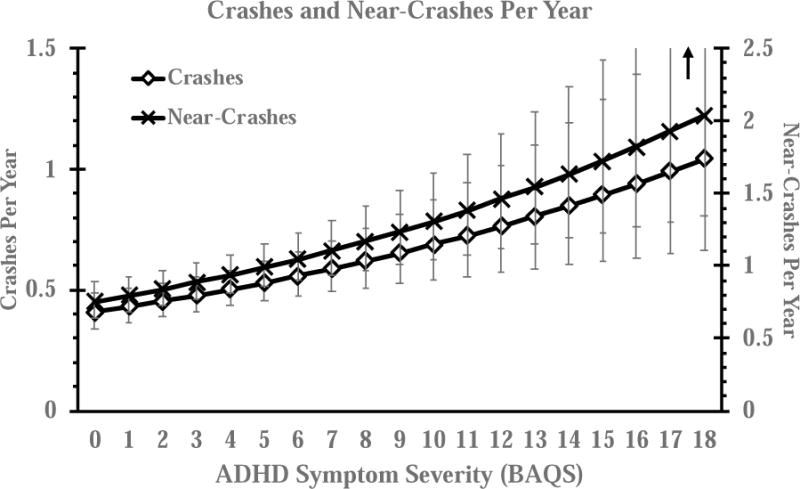
Crash and near-crash risk as a function of BAQS ADHD symptom severity scores. Values reflect estimated marginal means for incidents per year, controlled for age, gender, education, and marital status. Per year was defined for days of continuous monitoring=365.25 and total miles driven=15,000. Error bars reflect 95% Wald confidence intervals (CIs).
Figure 2.
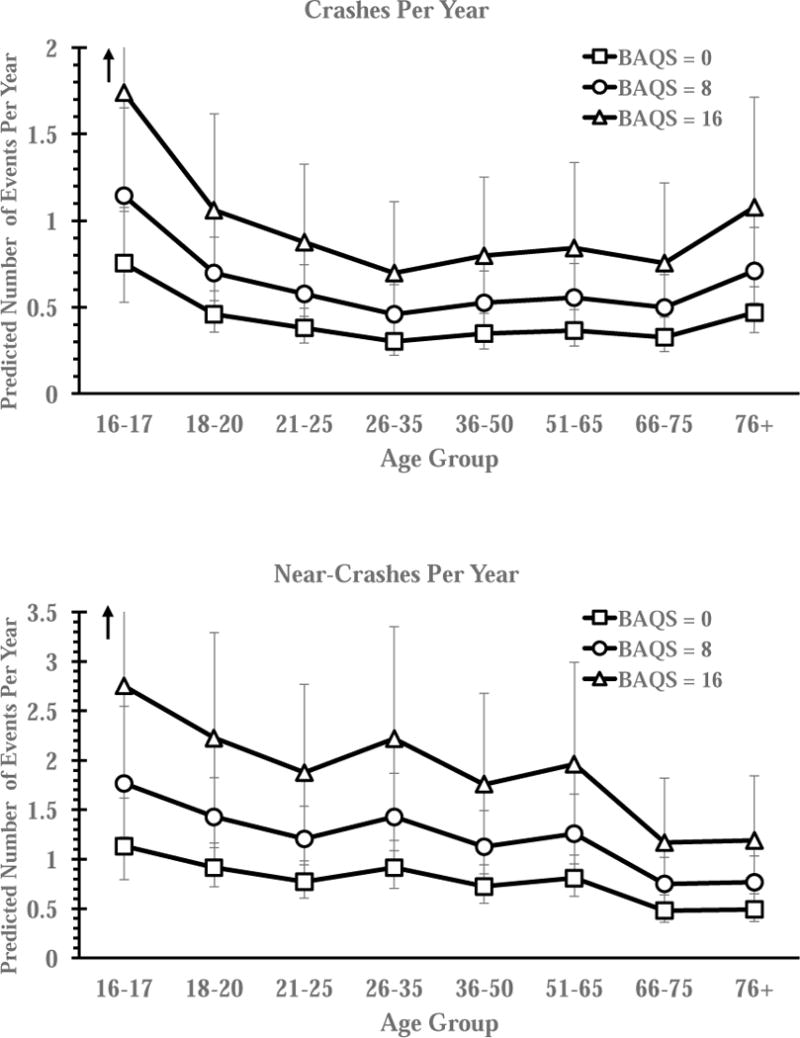
Crash and near-crash risk as a function of ADHD symptoms (BAQS) and age group. BAQS scores were selected to be representative and equidistant. BAQS=0 indicates no ADHD symptoms, BASQ=8 exceeds the clinical cut-off for ADHD of >7, and BAQS=16 indicates high severity ADHD symptoms. Values reflect estimated marginal means for incidents per year, controlled for gender, education, and marital status. Per year was defined for days of continuous monitoring=365.25 and total miles driven=15,000. Error bars reflect 95% Wald CIs.
Clinical Groups
ADHD designation at study entry portended 46% increased risk for crashes (IRR=1.46, 95%CI=1.17-1.83, p=.001) and 28% increased risk for near-crashes (IRR=1.28, 95%CI=1.04-1.58, p=.02). These data correspond, on average, to 0.65 annual crashes and 1.08 annual near-crashes per driver with ADHD. Figures 3 and 4 show these estimates as a function of miles driven and age groups.
Figure 3.
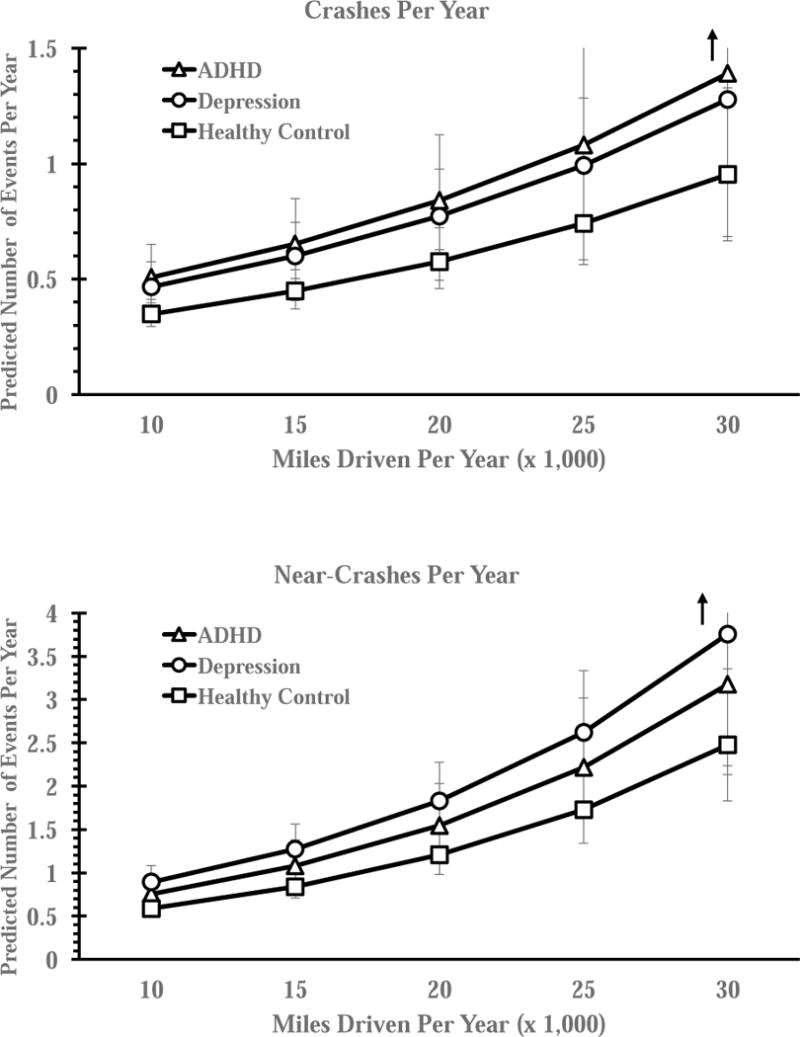
Crash and near-crash risk as a function of clinical group and exposure (miles driven per year), controlled for age, gender, education, and marital status. Values reflect estimated marginal means for incidents per year, defined for days of continuous monitoring=365.25. Error bars reflect 95% Wald confidence intervals.
Figure 4.
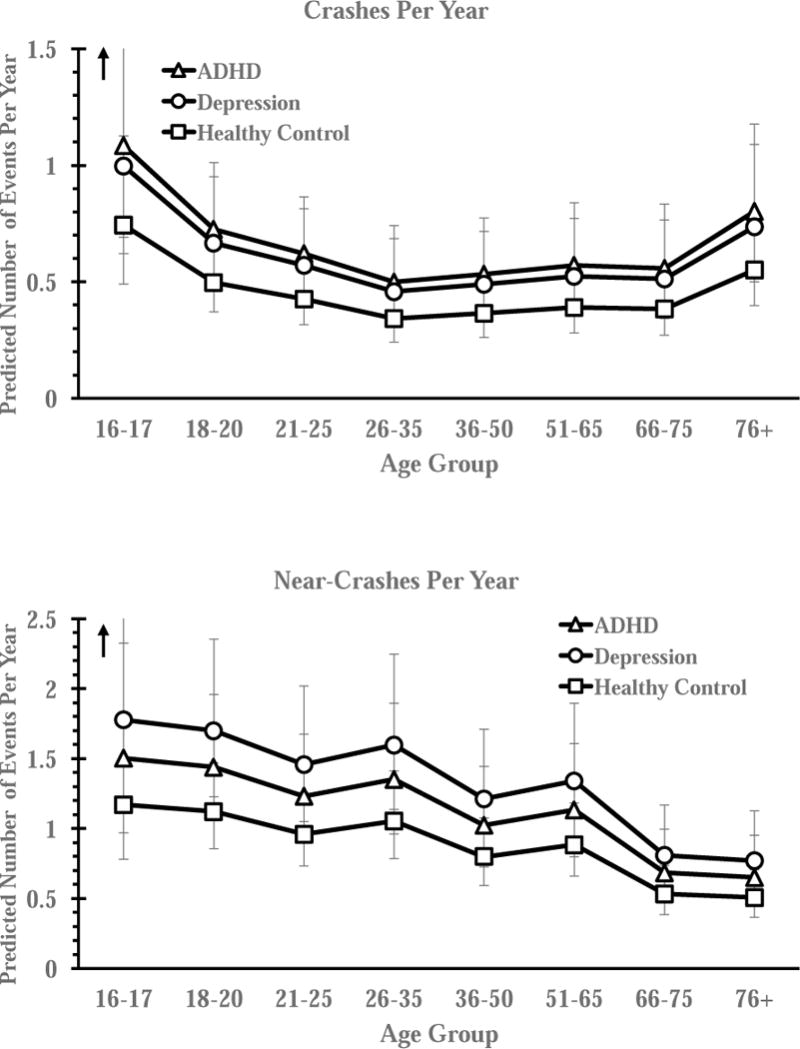
Crash and near-crash risk as a function of clinical group and age group, controlled for age, gender, education, and marital status. Values reflect estimated marginal means for incidents per year, defined for days of continuous monitoring =365.25 and miles driven =15,000. Error bars reflect 95% Wald confidence intervals.
Depression at study entry portended 34% increased risk for crashes (IRR=1.34, 95%CI=1.05-1.71, p=.02) and 52% increased risk for near-crashes (IRR=1.52, 95%CI=1.22-1.88, p<.0005). These data predict, on average, 0.60 annual crashes and 1.28 annual near-crashes per driver with Depression (Figures 3–4). Drivers with ADHD did not significantly differ from drivers with Depression on crashes (IRR=0.92, 95%CI=0.68-1.25, p=.59) or near-crashes (IRR=1.18, 95%CI=0.90,1.56, p=.23).
Treatment Status
ADHD
Exploratory analyses indicated that medication treatment for ADHD did not attenuate driving risk, as evidenced by increased crash risk for both untreated (IRR=1.36, 95%CI=1.06-1.75, p=.02) and treated (IRR=1.86, 95%CI=1.22-2.82, p=.004) drivers with ADHD relative to Healthy Control drivers. The treated and untreated ADHD subgroups did not differ (IRR=1.33, 95%CI=0.85-2.08, p=.21).
Depression
Results indicated reduced crash risk for medicated drivers with Depression, such that crash risk relative to Healthy Controls was detected only for the subgroup who discontinued antidepressants during the study (IRR=2.35, 95%CI=1.29-4.27, p=.005; all other subgroups p>.24). Drivers with Depression who discontinued medication also showed increased risk relative to unmedicated drivers with Depression (IRR=2.05, 95%CI=1.13-3.71, p=.02; all other between-subgroup comparisons p>.23).
Assessing Crash Risk: Retrospective Self-Report vs. Prospective Monitoring
A final comparison was made by comparing the retrospective self-report data for this sample at study entry from Aduen (2015)11 with the current study’s prospective in-car monitoring. Partial correlations adjusted for miles driven, days of continuous monitoring, and driver demographics indicated that self-reported crash counts at study entry predicted crash counts during prospective monitoring for healthy control drivers (r=.10, p<.0005, n=1,743), but were poor predictors of prospectively-identified crashes for drivers in the ADHD (r=-.002, p=.98, n=260) and Depression groups (r=-.01, p=.85, n=236).
Discussion
The current study was the first prospective, continuously-monitored assessment of real-world crash risk as a function of ADHD symptoms, controlling for a host of established risk factors.38 Prospective monitoring indicated a robust association between ADHD symptoms and adverse driving outcomes. The 5%–6% increased risk per ADHD symptom severity endorsement indicates that, on average, drivers who screen positive for ADHD are expected to have at least one biennial crash and one annual near-crash. This risk increases substantially as ADHD symptom severity increases, and doubles to predict approximately one crash per year for drivers reporting the most severe ADHD symptoms. Similarly, ADHD clinical status at study entry portended large magnitude risk for experiencing a crash (IRR=1.46).11 Examination of the confidence intervals indicates that these estimates were higher than expected based on the most recent meta-analysis (RR=1.23).5 Thus, our dimensional and categorical findings confirm that ADHD portends adverse driving outcomes,2,4,5,7 and extends previous findings by suggesting that this risk is higher than previously estimated at both the symptom and clinical group levels.
Importantly, however, this risk did not appear unique to ADHD, but occurred at elevated rates for drivers with Depression. Depression is another high-prevalence psychiatric disability associated with attention/concentration problems,16,24,25,33 and this group also reported elevated ADHD symptoms relative to controls in the current study. We propose both inattentive and impulsive/hyperactive behavior as potential transdiagnostic mechanisms, given their status as core symptoms of both ADHD and Depression (reified for the latter as ‘concentration problems’ and ‘psychomotor agitation observable to others’).2,3,24 Combined with the finding that crash risk increases proportionately with each increase in ADHD symptom severity (Figure 1), these findings suggest that symptom frequency/severity may be more important than clinical status per se when assessing motor vehicle crash risk. At the same time, drivers with Depression may have been somewhat better able to avoid imminent crashes than drivers with ADHD (near-crash: IRRDepression=1.28 vs. IRRADHD=1.52). Beyond the elevated but less severe ADHD symptoms exhibited by the Depression group, this result suggests potential disorder-specific differences in successfully recovering from presumed attentional lapses12,13 in time to avoid an imminent crash.
The association between Depression and crash risk appears inconsistent with retrospective self-report from this sample,11 which documented this risk for ADHD but not Depression. The reason for this incongruence is not clear, but may be related to the overall poor correspondence between prior crashes and future crashes among drivers in the Depression and ADHD groups. Alternatively, exploratory analyses linked crash risk specifically to members of the Depression group who discontinued antidepressants during prospective monitoring. Medication results must be considered tentative, but protective effects of antidepressant treatment9 could explain this discrepancy given that these drivers were by definition taking medication when reporting prior crashes at study entry. We also considered Depression-specific explanations, but these appeared unlikely given evidence that these drivers appraise their driving performance more negatively than other drivers.39,40 Notably, the poor predictive validity of self-reported crashes for both clinical groups indicates that patient education is warranted irrespective of patients’ self-reported crash history (i.e., self-reported safe driving is not a protective factor against future crashes for drivers with ADHD and Depression).
Medication was not associated with reduced risk for drivers with ADHD, with relatively wide confidence intervals that limit comparative statements regarding crash risk between medicated and unmedicated ADHD subgroups. Although there is evidence that certain psychostimulant formulations may increase crash risk in certain environments,17,41 placebo-controlled studies are consistent in documenting reduced crash risk when medication is metabolically active.17,18 Because ADHD medication has well-documented benefits for motor vehicle driving,42 the equivocal results for ADHD medication may reflect inconsistent adherence, interactions between unmedicated symptom severity and treatment status, and/or driving events that occurred when medication was not metabolically active.4,6 Alternatively, the trend toward increased risk in medicated drivers may reflect effects of unmeasured factors rather than causes, such that 75% of medicated drivers with ADHD (n=43 of 57) began treatment during the study monitoring period.
For the Depression group, the higher prevalence of medication treatment allowed us to separate medication status based on time course. We found that the increased risk for crashes was seen exclusively for drivers who discontinued antidepressant treatment during the study (IRR=2.35). To our knowledge, there have been no controlled studies documenting vehicular crash rates among patients who discontinue antidepressants. In the absence of such data, we suggest that the current findings call for patient education and routine consideration of driving risk during treatment planning – particularly when patients discontinue antidepressant medication.
Limitations
The current study was the first to prospectively track crash risk as a function of ADHD symptoms in a large sample of drivers using continuous, on-road monitoring. The following caveats must be considered. ADHD symptom severity was based on a well-validated ADHD screening measure (93% sensitivity, 99% specificity)31 whereas clinical group assignment was based on self-reported current diagnosis rather than gold-standard psychiatric interviewing. We were unable to track symptom course during prospective vehicle monitoring, and the proportion of females in the ADHD group (51%) was somewhat higher than expected based on current prevalence estimates. Although these methods are comparable to other large-scale epidemiological studies,12 generalization is limited to clinically- rather than research-defined ADHD and Depression.7 Thus, while the results exhort patient education and consideration of driving risk in treatment planning, implications for putative etiological mechanisms are less clear. Participants were protected by a national Certificate of Confidentiality; thus, correspondence with police, hospital, and/or Department of Motor Vehicle recordkeeping is unknown.
Further, we were unable to track the course of Depression during prospective monitoring. Epidemiological evidence indicates that 20% of Depression cases are chronic across the two-year period covered in the current study,43 and an additional 33%–50% experience recurrent episodes in a given year.15 Nevertheless, the proportion of these drivers who were depressed and/or medicated at the time of a crash/near-crash is unknown, and uncertainty regarding medication and symptom time course precludes causal attributions. Still, epidemiological studies frequently use prescription data as a proxy for active treatment.9,17 For clinical practice, we interpret these findings to indicate that clinicians should educate patients regarding crash risk irrespective of self-reported crash history and potential symptom remission.
Finally, we were unable to examine proximal risk factors for crashes, such as in situ driver behaviors, cell phones, alcohol and substance use, or whether medication was active at the time of a crash. Thus, additional work is needed to identify the mechanisms by which ADHD confers crash risk (e.g., increased risk for substance use is a known outcome of ADHD as well as a risk factor for crashes).6 The naturalistic study design precluded clinical interviewing regarding perceived medication efficacy, emergent effects, or timing in relation to crashes, and thus informs protective effects of medication treatment rather than optimal dosing. Nevertheless, these analyses reflect the most extensive examination to date of the protective effects of medication treatment on prospective, objectively documented motor vehicle crashes.
Clinical and Research Implications
Results confirm that ADHD and Depression are significant risk factors for adverse driving outcomes,9,44 and indicate that this risk is greater than previously estimated – particularly for being involved in, and culpable for, crashes and near-crashes. Notably, this risk appears proportional to ADHD symptom severity, rather than an outcome of clinical status per se. Clinically, patient education regarding driving risk is warranted, particularly when considering medication changes. Psychostimulants and manual transmission vehicles may reduce but not eliminate risk for ADHD drivers,4 and assessing daily driving routines (e.g., afternoon/evening vs. late night) has important implications for selecting among psychostimulant formulations.17 Future studies are needed to identify specific, in-car behaviors that portend this risk, and determine why drivers with elevated but less severe ADHD symptoms – such as those with Depression – may have greater success executing evasive actions that avoid imminent crashes. Determining whether similar behaviors precede crashes between clinical groups and across ADHD severity levels will be helpful for developing transdiagnostic and disorder-specific interventions to reduce adverse driving outcomes45. In particular, the omnipresence of cellphones46, social media access, and WiFi-connected vehicles may simultaneously provide both serious risk (e.g., distracted driving) and golden public health opportunity for intervention (e.g., real-time monitoring/intervention).47,48,49
Supplementary Material
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Self-reported anxiety did not predict crashes or near-crashes when added as an exploratory predictor in the clinical group models below (all p > .79; all 95%CIs included 1.0), and its inclusion did not change the significance or interpretation of any results. Exploratory analyses indicated also that crash and near-crash rates did not vary significantly (all p>.34; all 95%CIs included 1.0) as a function of the criteria for ADHD group membership (n=48 self-reported an ADHD diagnosis but did not meet the BAQS cutoff, n=169 met the BAQS cut-off but did not self-report an ADHD diagnosis, n=58 self-reported an ADHD diagnosis and met the BAQS criteria). Results are therefore reported for the combined ADHD group and without anxiety included to most closely match the retrospective report from this sample from Aduen et al. (2015).
Per ADHD symptom severity endorsement refers to an increase of 1 point on the BAQS (e.g., a change from ‘sometimes’ to ‘often’ on a single item). The range of BAQS scores in the sample was 0-17 (0-18 possible). A BAQS score of 0 reflects responses of never/rarely for all 6 items, whereas BAQS=17 occurs when 5 of 6 symptoms occur very often, and 1 symptom occurs often. A BAQS score of 8 would exceed the questionnaire’s clinical screening cutoff of 7, and could be obtained via several item endorsement combinations (e.g., endorsements of Often on 4 items and Never on the remaining two items, endorsements of Often on 2 items and Sometimes on the remaining 4 items). This score of 8 predicts 0.62 crashes (1 crash per 1.61 drivers) and 1.17 near-crashes per year.
Contributor Information
Paula A. Aduen, University of Virginia, Curry School of Education
Michael J. Kofler, Florida State University, Department of Psychology
Dustin E. Sarver, University of Mississippi Medical Center, Center for Advancement of Youth
Erica L. Wells, Florida State University, Department of Psychology
Elia F. Soto, Florida State University, Department of Psychology
Daniel J. Cox, University of Virginia Health Sciences Center, Center for Behavioral Medicine Research
References
- 1.Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. Web-based Injury Statistics Query and Reporting System (WISQARS) Fatal Injury Data. 2016 Accessed from https://www.cdc.gov/injury/wisqars/overview/key_data.html 08/31/2017.
- 2.Fuermaier AB, Tucha L, Evans BL, et al. Driving and attention deficit hyperactivity disorder. J Neural Transm. 2015:1–13. doi: 10.1007/s00702-015-1465-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bulmash EL, Moller HJ, Kayumov L, Shen J, Wang X, Shapiro CM. Psychomotor disturbance in depression: assessment using a driving simulator paradigm. J Affect Disord. 2006;93(1):213–218. doi: 10.1016/j.jad.2006.01.015. [DOI] [PubMed] [Google Scholar]
- 4.Cox DJ, Madaan V, Cox BS. Adult attention-deficit/hyperactivity disorder and driving: why and how to manage it. Curr Psychiatry Rep. 2011;13(5):345–50x. doi: 10.1007/s11920-011-0216-0. [DOI] [PubMed] [Google Scholar]
- 5.Vaa T. ADHD and relative risk of accidents in road traffic: A meta-analysis. Accident Anal Prev. 2014;62:415–425. doi: 10.1016/j.aap.2013.10.003. [DOI] [PubMed] [Google Scholar]
- 6.Barkley RA, Cox D. A review of driving risks and impairments associated with attention-deficit/hyperactivity disorder and the effects of stimulant medication on driving performance. J Safety Res. 2007;38(1):113–28. doi: 10.1016/j.jsr.2006.09.004. [DOI] [PubMed] [Google Scholar]
- 7.Jerome L, Habinski L, Segal A. Attention-deficit/hyperactivity disorder (ADHD) and driving risk: a review of the literature and a methodological critique. Curr Psychiatry Rep. 2006;8(5):416–26. doi: 10.1007/s11920-006-0045-8. [DOI] [PubMed] [Google Scholar]
- 8.Brunnauer A, Laux G, David I, Fric M, Hermisson I, Möller HJ. The impact of reboxetine and mirtazapine on driving simulator performance and psychomotor function in depressed patients. J Clin Psychiatry. 2008;69(12):1880–1886. doi: 10.4088/jcp.v69n1205. [DOI] [PubMed] [Google Scholar]
- 9.Wingen M, Ramaekers JG, Schmitt JA. Driving impairment in depressed patients receiving long-term antidepressant treatment. J Psychopharmacol. 2006;188(1):84–91. doi: 10.1007/s00213-006-0471-7. [DOI] [PubMed] [Google Scholar]
- 10.Swensen A, Birnbaum HG, Ben Hamadi R, et al. Incidence and costs of accidents among attention-deficit/hyperactivity disorder patients. J Adolesc Health. 2004;35:346. [PubMed] [Google Scholar]
- 11.Aduen PA, Kofler MJ, Cox DJ, et al. Motor vehicle driving in high incidence psychiatric disability: Comparison of drivers with ADHD, depression, and no known psychopathology. J Psychiatr Res. 2015;64:59–66. doi: 10.1016/j.jpsychires.2015.03.009. [DOI] [PubMed] [Google Scholar]
- 12.Chang Z, Lichtenstein P, D’Onofrio BM, et al. Serious transport accidents in adults with attention-deficit/hyperactivity disorder and the effect of medication: A population-based study. JAMA Psychiatry. 2014;71(3):319–325. doi: 10.1001/jamapsychiatry.2013.4174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Redelmeier DA, Chan WK, Lu H. Road trauma in teenage male youth with childhood disruptive behavior disorders: a population based analysis. PLoS Med. 2010;7(11) doi: 10.1371/journal.pmed.1000369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Polanczyk G, de Lima MS, Horta BL, et al. The worldwide prevalence of ADHD: a systematic review and metaregression analysis. Am J Psychiatry. 2007;164(6):942–8. doi: 10.1176/ajp.2007.164.6.942. [DOI] [PubMed] [Google Scholar]
- 15.Hasin DS, Goodwin RD, Stinson FS, Grant BF. Epidemiology of major depressive disorder: results from the National Epidemiologic Survey on Alcoholism and Related Conditions. Arch Gen Psychiatry. 2005;62(10):1097–1106. doi: 10.1001/archpsyc.62.10.1097. [DOI] [PubMed] [Google Scholar]
- 16.Hill LL, Lauzon VL, Winbrock EL, Li G, Chihuri S, Lee KC. Depression, antidepressants and driving safety. Inj Epidimiol. 2017;4:10. doi: 10.1186/s40621-017-0107-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Merkel RL, Jr, Nichols JQ, Fellers JC, Hidalgo P, Martinez LA, Putziger I, Burket RC, Cox DJ. Comparison of on-road driving between young adults with and without ADHD. J Atten Disord. 2016 Mar;20(3):260–9. doi: 10.1177/1087054712473832. [DOI] [PubMed] [Google Scholar]
- 18.Cox DJ, Davis M, Mikami AY, Singh H, Merkel RL, Burket R. Long-acting methylphenidate reduces collision rates of young adult drivers with attention-deficit/hyperactivity disorder. J Clin Pharmacol. 2012;32(2):225–30. doi: 10.1097/JCP.0b013e3182496dc5. [DOI] [PubMed] [Google Scholar]
- 19.Knouse LE, Bagwell CL, Barkley RA, et al. Accuracy of self-evaluation in adults with ADHD evidence from a driving study. J Atten Disord. 2005;8(4):221–234. doi: 10.1177/1087054705280159. [DOI] [PubMed] [Google Scholar]
- 20.Wåhlberg AE, Dorn L. How reliable are self-report measures of mileage, violations and crashes? Saf Sci. 2015;76:67–73. [Google Scholar]
- 21.McCartt AT, Solomon MG. Tracking traffic citations through court adjudications to posting to public driver records. Traffic Inj Prev. 2004;5(2):93–100. doi: 10.1080/15389580490434863. [DOI] [PubMed] [Google Scholar]
- 22.Biederman J, Fried R, Monuteaux MC, et al. A laboratory driving simulation for assessment of driving behavior in adults with ADHD: a controlled study. Ann Gen Psychiatry. 2007;6:4. doi: 10.1186/1744-859X-6-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Barkley RA, Murphy KR, O’Connell T, et al. Effects of two doses of methylphenidate on simulator driving performance in adults with attention deficit hyperactivity disorder. J Safety Res. 2005;36(2):121–31. doi: 10.1016/j.jsr.2005.01.001. [DOI] [PubMed] [Google Scholar]
- 24.Austin MP, Mitchell P, Goodwin GM. Cognitive deficits in depression. Br J Psychiatry. 2001;178(3):200–6. doi: 10.1192/bjp.178.3.200. [DOI] [PubMed] [Google Scholar]
- 25.Wickens CM, Smart RG, Mann RE. The impact of depression on driver performance. Int J Ment Health. 2014;12(4):524–37. [Google Scholar]
- 26.Di Milia L, Smolensky MH, Costa G, et al. Demographic factors, fatigue, and driving accidents: An examination of the published literature. Accident Anal Prev. 2011;43(2):516–532. doi: 10.1016/j.aap.2009.12.018. [DOI] [PubMed] [Google Scholar]
- 27.Whitlock G, Norton R, Clark T, Jackson R, MacMahon S. Motor vehicle driver injury and marital status: a cohort study with prospective and retrospective driver injuries. Inj Prev. 2004;10(1):33–6. doi: 10.1136/ip.2003.003020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Antin J, Stulce K, Eichelberger L, et al. Naturalistic driving study: Descriptive comparison of the study sample with national data. Transportation Research Board; 2015. Accessible at https://www.nap.edu/download/22196. [Google Scholar]
- 29.Antin J, Lee S, Hankey J, et al. Design of the in-vehicle driving behavior and crash risk study. Transportation Research Board; 2011. Accessible at https://www.nap.edu/download/14494. [Google Scholar]
- 30.Hankey J, Perez MA, McClafferty J. Description of the SHRP 2 Naturalistic Database and the Crash, Near-Crash, and Baseline Data Sets. Transportation Research Board; 2016. Accessible at: https://www.nap.edu/download/22196. [Google Scholar]
- 31.Barkley RA, Murphy KR, Fischer M. ADHD in adults: What the science says. Guilford Press; 2010. [Google Scholar]
- 32.Kessler RC, Bromet EJ. The epidemiology of depression across cultures. Annu Rev Public Health. 2013;34:119–138. doi: 10.1146/annurev-publhealth-031912-114409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Paelecke-Habermann Y, Pohl J, Leplow B. Attention and executive functions in remitted major depression patients. J Affect Disord. 2005;89(1):125–35. doi: 10.1016/j.jad.2005.09.006. [DOI] [PubMed] [Google Scholar]
- 34.Kessler R, Adler L, Barkley R, et al. The prevalence and correlates of adult ADHD in the United States: Results from the national comorbidity survey replication. Am J Psychiatry. 2006;163:716–723. doi: 10.1176/appi.ajp.163.4.716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Harman JS, Edlund MJ, Fortney JC. Trends in antidepressant utilization from 2001 to 2004. Psychiatr Serv. 2015 doi: 10.1176/ps.2009.60.5.611. [DOI] [PubMed] [Google Scholar]
- 36.Valentine JC, Aloe AM, Lau TW. Life after NHST: How to describe your data without “ping” everywhere. Basic Appl Soc Psych. 2015;37(5):260–273. [Google Scholar]
- 37.National Center for Statistics and Analysis. Annual Vehicle- Miles of Travel, 1980-2015 National Summary. Washington, DC: National Highway Traffic Safety Administration; 2015. (Highway Statistics Series). [Google Scholar]
- 38.Mannuzza S, Klein RG, Bessler A, et al. Adult outcome of hyperactive boys: Educational achievement, occupational rank, and psychiatric status. Arch Gen Psychiatry. 1993;50(7):565–576. doi: 10.1001/archpsyc.1993.01820190067007. [DOI] [PubMed] [Google Scholar]
- 39.Dorn L, Matthews G. Prediction of mood and risk appraisals from trait measures: Two studies of simulated driving. Eur J Pers. 1995;9:25–42. [Google Scholar]
- 40.Thames AD, Becker BW, Marcotte TD, et al. Depression, cognition, and self-appraisal of functional abilities in HIV: An examination of subjective appraisal versus objective performance. Clin Neuropsychol. 2011;25(2):224–43. doi: 10.1080/13854046.2010.539577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Randell NJ, Charlton SG, Starkey NJ. Driving with ADHD performance effects and environment demand in traffic. J Atten Disord. 2016 doi: 10.1177/1087054716658126. 1087054716658126. [DOI] [PubMed] [Google Scholar]
- 42.Chang Z, Quinn PD, Hur K, Gibbons RD, Sjölander A, Larsson H, D’Onofrio BM. Association between medication use for attention-deficit/hyperactivity disorder and risk of motor vehicle crashes. JAMA Psychiatry. 2017;74(6):597–603. doi: 10.1001/jamapsychiatry.2017.0659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Spijker J, De Graaf R, Bijl RV, et al. Duration of major depressive episodes in the general population: Results from the Netherlands mental health survey and incidence study. British J Psychiat. 2002;181:208–213. doi: 10.1192/bjp.181.3.208. [DOI] [PubMed] [Google Scholar]
- 44.Stavrinos D, Garner AA, Franklin CA, et al. Distracted driving in teens with and without attention-deficit/hyperactivity disorder. Pediatr Nurs. 2015;30(5) doi: 10.1016/j.pedn.2015.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Vaa T. Deliverable R1.1 of EU-project IMMORTAL. Institute of Transport Economics; Oslo: 2003. Impairments, diseases, age and their relative risks of accident involvement: Results from meta- analysis. (TØI-Report 690). [Google Scholar]
- 46.O’Connor SS, Shain LM, Whitehill JM, Ebel BE. Measuring a conceptual model of the relationship between compulsive cell phone use, in-vehicle cell phone use, and motor vehicle crash. Accid Anal Prev. 2017 Feb 28;99:372–8. doi: 10.1016/j.aap.2016.12.016. [DOI] [PubMed] [Google Scholar]
- 47.El Farouki K, Lagarde E, Orriols L, et al. The increased risk of road crashes in Attention Deficit Hyperactivity Disorder (ADHD) adult drivers: Driven by distraction? Results from a responsibility case-control study. Plos ONE. 2014;9(12):1–15. doi: 10.1371/journal.pone.0115002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Jenkins S, Codjoe J, Alecsandru C, Ishak S. Advances in Human Aspects of Transportation. Springer International Publishing; 2017. Exploration of the SHRP 2 NDS: Development of a Distracted Driving Prediction Model; pp. 231–242. [Google Scholar]
- 49.Reimer B, Mehler B, D’Ambrosio LA, et al. The impact of distractions on young adult drivers with attention deficit hyperactivity disorder (ADHD) Accid Anal Prev. 2010;42(3):842. doi: 10.1016/j.aap.2009.06.021. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


