Abstract
BACKGROUND
Double-orifice mitral valve (DOMV) is an extremely rare cardiac malformation. It has been found to be accompanied by congenital anomalies (CAs), however, it can be detected as an isolated anomaly. The clinical findings of a DOMV are variable and depend predominantly on the associated cardiac abnormalities, particularly atrioventricular septal defects or mitral valve (MV) regurgitation and/or stenosis.
CASE REPORT
In this regard, we describe an isolated DOMV in an 18-year-old young girl who complained of a short-term nonspecific chest pain. She underwent transthoracic and transesophageal echocardiographic examinations. The examinations revealed a DOMV without any valvular or structural malformations. Other examinations were unremarkable. The patient did need neither medical nor surgical interventions.
CONCLUSION
The isolated cases of DOMV do not need therapy and might be only followed up using echocardiographic examinations. However, a careful echocardiographic examination for detection of concomitant structural malformations would be of great importance in the management of such cases.
Keywords: Echocardiography, Heart Valve Disease, Mitral Valve, Congenital Heart Defects
Introduction
Double-orifice mitral valve (DOMV) is an extremely rare congenital anomaly (CA) diagnosed by the detection of two orifices in the left mitral valve (MV) area, as separated chordal attachment to the papillary muscle. This cannot be attributable to the endocardial cushions and abnormal development of the MV originating from the primitive left ventricle.1 The DOMV is usually associated with CAs, however, it is also detected as an isolated malformation.2,3
The majority of cases are detected by 2-dimensional transthoracic echocardiography (2D TTE),2 however, transesophageal echocardiography (TEE) also provides more detailed analysis of both the structures and functions of the MV.4,5 This report describes an isolated DOMV identified using both 2D TTE and TEE imaging modalities.
Case Report
An 18-year-old girl patient was referred to the outpatient clinic of Rajaie Cardiovascular Medical and Research Center, Tehran, Iran, complaining of an atypical chest pain during the past one month. Her physical examination was unremarkable and her pulse rate was regular, with a blood pressure of 110/70 mmHg. She had a normal heart auscultation with no abnormal sounds. Moreover, the electrocardiography and chest roentgenography tests revealed no abnormalities.
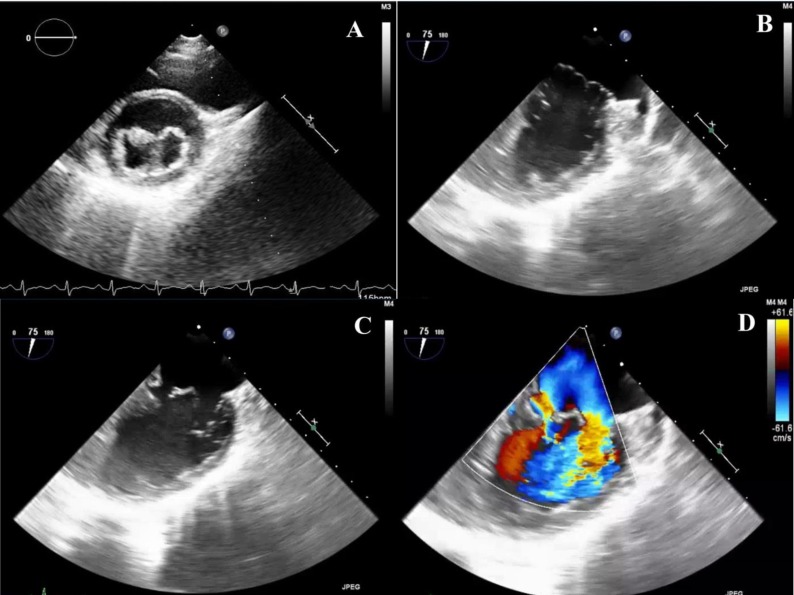
She also underwent a routine echocardiographic examination. The 2D TTE revealed 2 separate orifices in the MV location in parasternal short-axis view (PSAV) during diastole with a posteromedial and anterolateral orifice (Figure 1). The sizes of the 4 cardiac chambers were normal. There were neither heart valve diseases, including regurgitation or stenosis, nor regional wall motion abnormalities.
Figure 1.
Short-axis transthoracic view showing complete bridge type of double-orifice mitral valve (DOMV)
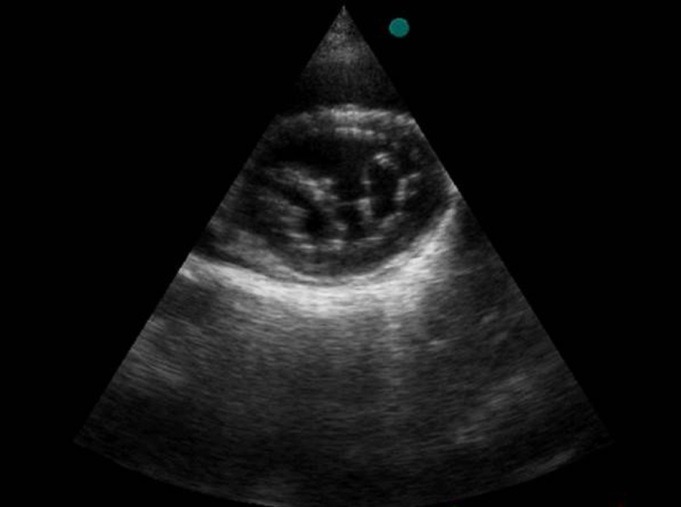
The left and right ventricular ejection fractions were normal. Furthermore, no pericardial effusion was detected. No CAs were also diagnosed. A TEE-based examination was also performed in order to evaluate the MV comprehensively to provide more precise information regarding this lesion. In addition, the TEE-based examination revealed two orifices in the MV area with separate leaflets (Figure 2). The color Doppler imaging (CDI) also showed two different blood flows thorough different valves (Figure 2 and Video 1). No other abnormalities were identified. The findings were consistent with a diagnosis of DOMV without any cardiac malformations. Therefore, the patient was discharged without any specific treatment.
Figure 2.
Transesophageal echocardiographic (TEE) images showing (A) double-orifice mitral valve (DOMV), two anatomical mitral valve (MV) leaflets in (B) systolic and (C) diastolic state, and (D) Doppler echocardiography of concomitant flows through two valves
Discussion
In this report, we described a rare form of DOMV in a young girl who complained of a short-term nonspecific chest pain. We did not find any valvular involvements in this case except an isolated DOMV which did not require neither medical nor surgical interventions.
DOMV is a rare CA which may be either an isolated malformation or concomitant with other CAs like endocardial cushion defect, bicuspid aortic valve, coarctation of aorta (CoA or CoAo), and patent ductus arteriosus (PDA).6 The most common associated anomaly is partial atrioventricular septal defect. Occasionally, some other anomalies were rarely reported, particularly right-to-left shunting anomalies.7 Moreover, the presence of DOMV associated with other syndromes has also been reported, including down syndrome,8,9 Kabuki syndrome,10 and Cornelia de Lange syndrome.11 According to the coexistence of these syndromes and DOMV, we should consider other extra cardiac anomalies in such cases, including limb anomalies, facial defects, gastrointestinal defects, and neurological manifestations. In addition, in the present case, there was neither intra cardiac nor extra cardiac anomalies.
The exact incidence of DOMV is still unknown; however, in two retrospective studies on the evaluation of the echocardiographic findings of two referral centers, the incidence of DOMV has been found to be approximately 0.04% and 0.01% among children12 and adult individuals, respectively.4 The clinical findings of the DOMV are variable and depend predominantly on the associated cardiac abnormalities. Patients with an isolated DOMV usually have mild symptoms including chest pain and palpitation similar to the present case and are found incidentally at echocardiographic assessment for nonspecific symptoms.2,13
Trowitzsch et al.14 described 3 various types of DOMV according to 2D TTE examination: hole type, accounting for approximately 85% of such cases detected as a small accessory orifice placed at either the anterolateral or posteromedial commissure, detectable at the mid-leaflet level view; complete bridge type, accounting for about 15% of DOMVs, with a central bridge of fibrous connecting the 2 leaflets associated with normal papillary muscles of each orifice; and incomplete bridge type, including a partial connection at the leaflet edge. The MV can operate normally among approximately 50% of patients with DOMV.15 The presence of separated leaflet chordae for both valve openings distinguishes DOMV from acquired lesions, including perforation, fusion of MV leaflets by inflammation, perforated aneurysm of a leaflet, trauma, and iatrogenic.12
Echocardiography is the method of choice for detecting and monitoring the progression of DOMV. Other concomitant congenital heart defects are detected during echocardiographic examination. PSAV in TTE is the best view for showing the numbers of MV leaflets and orifices. Long-axis and off-axis views can be used to define the chordal attachments to their respective papillary muscles. Pulse wave, continuous wave, and color Doppler technologies can also be implemented to evaluate the functional status of structural anomalies.2,4 Three-dimensional echocardiography has also been used for more comprehensive evaluation in suspected cases.5 This modality may be helpful to detect the anomalous relationship between the papillary muscles and mitral chordae among patients with the DOMV diagnosis.
The management of DOMV depends on the severity of involvement and concomitant anomalies. All patients with significant mitral stenosis and/or insufficiency need medical management to relieve pulmonary congestion and to stabilize them before any required interventions. Surgical approaches are implemented in cases with severe MV stenosis and/or regurgitation or among patients with concomitant cardiac anomalies, particularly septal defects. The type of surgical interventions depends on the detailed anatomical and functional characteristics of the MV abnormality. The MV repair procedure is treatment of choice unless the valve is markedly abnormal or malfunctioned where the valve replacement is needed.13 Other asymptomatic cases, particularly isolated ones, need neither medical therapies nor surgical correction and may be followed up using echocardiographic examinations. Based on the experience obtained in the present case, we emphasize the importance of careful echocardiographic examination to detect any valvular or structural malformations in such cases to determine the best treatment.
Video 1.
Acknowledgments
None.
Footnotes
Conflicts of Interest
Authors have no conflict of interests.
REFERENCES
- 1.Erdemli O, Ayik I, Karadeniz U, Yamak B, Birincioglu CL, Caglar K. A double-orifice atrioventricular valve case: Intraoperative transesophageal echocardiography in diagnosis and treatment. Anesth Analg. 2003;97(3):650–3. doi: 10.1213/01.ANE.0000078580.22176.B0. [DOI] [PubMed] [Google Scholar]
- 2.Han J, He Y, Li Z, Zhang Y, Chen J, Wang L, et al. Isolated double-orifice mitral valve anomaly on 3-dimensional transesophageal echocardiography. J Ultrasound Med. 2009;28(11):1589–92. doi: 10.7863/jum.2009.28.11.1589. [DOI] [PubMed] [Google Scholar]
- 3.Khani M, Rohani A. Double-orifice mitral valve associated with bicuspid aortic valve. Asian Cardiovasc Thorac Ann. 2017;25(5):386–7. doi: 10.1177/0218492316638607. [DOI] [PubMed] [Google Scholar]
- 4.Wojcik A, Klisiewicz A, Szymanski P, Rozanski J, Hoffman P. Double-orifice mitral valve-echocardiographic findings. Kardiol Pol. 2011;69(2):139–43. [PubMed] [Google Scholar]
- 5.Ender J, Sgouropoulou S. Value of transesophageal echocardiography (TEE) guidance in minimally invasive mitral valve surgery. Ann Cardiothorac Surg. 2013;2(6):796–802. doi: 10.3978/j.issn.2225-319X.2013.10.09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bano-Rodrigo A, Van Praagh S, Trowitzsch E, Van Praagh R. Double-orifice mitral valve: A study of 27 postmortem cases with developmental, diagnostic and surgical considerations. Am J Cardiol. 1988;61(1):152–60. doi: 10.1016/0002-9149(88)91322-7. [DOI] [PubMed] [Google Scholar]
- 7.Zalzstein E, Hamilton R, Zucker N, Levitas A, Gross GJ. Presentation, natural history, and outcome in children and adolescents with double orifice mitral valve. Am J Cardiol. 2004;93(8):1067–9. doi: 10.1016/j.amjcard.2004.01.015. [DOI] [PubMed] [Google Scholar]
- 8.Formigari R, Di Donato RM, Gargiulo G, Di Carlo D, Feltri C, Picchio FM, et al. Better surgical prognosis for patients with complete atrioventricular septal defect and Down's syndrome. Ann Thorac Surg. 2004;78(2):666–72. doi: 10.1016/j.athoracsur.2003.12.021. [DOI] [PubMed] [Google Scholar]
- 9.Marino B, Vairo U, Corno A, Nava S, Guccione P, Calabro R, et al. Atrioventricular canal in Down syndrome. Prevalence of associated cardiac malformations compared with patients without Down syndrome. Am J Dis Child. 1990;144(10):1120–2. doi: 10.1001/archpedi.1990.02150340066025. [DOI] [PubMed] [Google Scholar]
- 10.Digilio MC, Marino B, Toscano A, Giannotti A, Dallapiccola B. Congenital heart defects in Kabuki syndrome. Am J Med Genet. 2001;100(4):269–74. doi: 10.1002/ajmg.1265. [DOI] [PubMed] [Google Scholar]
- 11.Chatfield KC, Schrier SA, Li J, Clark D, Kaur M, Kline AD, et al. Congenital heart disease in Cornelia de Lange syndrome: Phenotype and genotype analysis. Am J Med Genet A. 2012;158A(10):2499–505. doi: 10.1002/ajmg.a.35582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Das BB, Pauliks LB, Knudson OA, Kirby S, Chan KC, Valdes-Cruz L, et al. Double-orifice mitral valve with intact atrioventricular septum: Aan echocardiographic study with anatomic and functional considerations. J Am Soc Echocardiogr. 2005;18(3):231–6. doi: 10.1016/j.echo.2004.12.001. [DOI] [PubMed] [Google Scholar]
- 13.Anwar AM, McGhie JS, Meijboom FJ, Ten Cate FJ. Double orifice mitral valve by real-time three-dimensional echocardiography. Eur J Echocardiogr. 2008;9(5):731–2. doi: 10.1093/ejechocard/jen149. [DOI] [PubMed] [Google Scholar]
- 14.Trowitzsch E, Bano-Rodrigo A, Burger BM, Colan SD, Sanders SP. Two-dimensional echocardiographic findings in double orifice mitral valve. J Am Coll Cardiol. 1985;6(2):383–7. doi: 10.1016/s0735-1097(85)80176-5. [DOI] [PubMed] [Google Scholar]
- 15.van Buuren F, Faber L, Bogunovic N. Double orifice mitral valve with normal function: An echocardiography and MRI study of a rare finding. Eur Heart J. 2011;32(2):137. doi: 10.1093/eurheartj/ehq350. [DOI] [PubMed] [Google Scholar]