Abstract
Fractures of the lateral and the posterior processes of the talus are uncommon and frequently missed because of a low level of suspicion and difficulty in interpretation on plain radiographs. Missed fractures can lead to persistent pain and reduced function.
Lateral process fractures are usually a consequence of forced dorsiflexion and inversion of fixed pronated foot. These are also commonly known as snowboarder’s fractures.
The posterior process of the talus is composed of medial and lateral tubercles, separated by the groove for the flexor hallucis longus tendon.
The usual mechanism of injury is forced hyperplantarflexion and inversion causing direct compression of the posterior talus, or an avulsion fracture caused by the posterior talofibular ligament. CT scans are helpful in cases of high clinical suspicion.
There is a lack of consensus regarding optimal management of these fractures; however, management depends on the size, location and displacement of the fragment, the degree of cartilage damage and instability of the subtalar joint. Non-operative treatment includes immobilization and protected weight-bearing for six weeks. Surgical treatment includes open reduction and internal fixation or excision of the fragments, depending on the size.
Fractures of the lateral and the posterior processes of the talus are uncommon but important injuries that may result in significant disability in cases of missed diagnosis or delayed or inadequate treatment. Early diagnosis and timely management of these fractures help to avoid long-term complications, including malunion, nonunion or severe subtalar joint osteoarthritis.
Cite this article: EFORT Open Rev 2018;3:85-92. DOI: 10.1302/2058-5241.3.170040
Keywords: lateral process, posterior process, talar process
Introduction
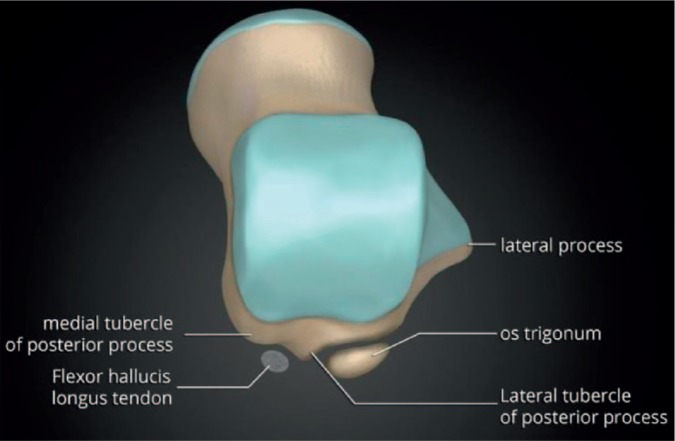
The talus is an incredible bone; despite its small size, it transmits considerable force during the normal gait cycle and even more significant force during impact activities. The talus is shaped like a truncated cone and is wider anteriorly than posteriorly. Approximately two-thirds of its surface area is covered with articular cartilage and it has a tenuous blood supply, similar to the scaphoid. The talus has seven articular surfaces and is divided into the head, neck and body, and two processes, the posterior process and the lateral process (Fig. 1). The posterior process is further subdivided into posterolateral and posteromedial tubercles. It is essential to understand these anatomical features of the talus in order to understand the anatomy of its fractures and their surgical management.
Fig. 1.
Anatomy of the talus (reproduced courtesy of Dr Matt. Skalski, Radiopaedia.org: https://radiopaedia.org/cases/anatomy-of-the-talus).
Fractures of the talus are uncommon and they comprise 3.4% of foot and ankle fractures and 0.32% of all fractures in the human body. Fractures of the lateral and posterior processes are considered to be peripheral talar fractures. They are uncommon and frequently missed due to difficulty in visualizing them on plain radiographs and low level of suspicion. Their management depends on the type, size of the fragment, degree of displacement, subtalar joint involvement and the articular surface lesion. Delayed diagnosis and treatment can potentially lead to poor outcomes, resulting in long-term pain, disability, nonunion and degenerative changes.1 Factors that can affect the outcomes of these fractures are the extent of initial articular damage, the accuracy of the reduction and the subtalar joint stability.2-4 This article aims to provide an overview of fractures of the lateral and posterior processes of the talus.
Fractures of the lateral process of the talus
Lateral process fractures of the talus are traditionally misdiagnosed as ankle sprains, and missed or untreated injuries can potentially lead to persistent symptoms.
Anatomy
The lateral process of the talus has a large base that articulates with the fibula dorsolaterally and contributes to maintaining the ankle mortise. It forms the lateral portion of the subtalar joint articulating with the posterior facet of the calcaneum inferomedially. The lateral talocalcaneal ligament originates from the tip of this process.5
Incidence
Despite being the second most common fracture, talar fractures are still rare. In a review of 1500 ankle injuries, only 0.86% were found to be lateral process fractures.6 Causative injuries include snowboarding injuries, falls from height, road traffic accidents, direct trauma, and football and rugby injuries.5 Their incidence among the general population is unknown; however, these are seen frequently in snowboarding-related injuries, hence they are also known as snowboarder’s fractures. In one large series, 2.3% of all snowboarding injuries were lateral process fractures, while some other studies have reported their incidence to be up to 6.3%.7,8 Not only is their incidence rising, but they are also increasingly recognized.
Mechanism
Lateral process fractures are usually a result of high-energy injuries. The suggested mechanism is thought to be a consequence of forced dorsiflexion and inversion of a fixed pronated foot.5 This results in a lateral shift of the talar head, an upward shift of the lateral process of the talus on the posterior articular surface of the calcaneum and loss of congruity of the posterior articulation.8 Boon et al, in their cadaveric study, proposed that some degree of external rotation is also required to produce this type of injury.9 Funk et al, in another cadaveric study, suggested that a combined eversion and dorsiflexion might also play an important role resulting in these fractures.10 However, there is no disagreement that dorsiflexion plays the key role at the time of injury. Hawkins postulated that the avulsion of the lateral process caused by the pull of the lateral talocalcaneal ligament might be another contributing mechanism; however, cadaveric and clinical studies do not clearly demonstrate this suggestion.11 One postulated reason behind their high incidence in snowboarders is the use of soft boots (70%), which results in more flexibility around the ankle joint leading to higher risk of foot and ankle injuries.12 However, Kirkpatrick et al reported a higher incidence of these fractures in snowboarders using hard boots as well.7 Therefore, the movement and the positioning of the ankle joint at the time of injury appear to be more important than the type of footwear being used.
Diagnosis
Clinically, up to 40% to 50% of lateral process fractures can be missed due to similar presentation as ankle sprains, even in the absence of distracting injuries.11,12 A history of ‘ankle sprain’ and the presence of associated acute localized tenderness, swelling and haematoma around the tip of the lateral malleolus, along with painful range of motion, should raise the suspicion of a lateral process fracture.5,13
Plain radiographs of the ankle in anteroposterior, lateral and mortise views should be performed routinely. A lateral process fracture is best seen on a mortise view or Broden’s view, but the chip fractures are best seen on the lateral view just above the Angle of Gissane.3,14 Presence of posterior subtalar effusion is highly suggestive of an occult lateral process fracture.15 A lateral radiograph with dorsiflexion and inversion of the ankle may assist in better visualization of the fracture fragment.16 Von Knoch et al described the appearance of an intact lateral process on a lateral radiograph as ‘symmetrically V-shaped’ and named the disruption of this appearance the ‘positive V-sign’.13 CT is considered to be the gold standard in cases of a high index of suspicion based on injury mechanism and clinical appearance (Figs 2a and 2b). The presence of accessory ossicles and osteophytes may make the diagnosis more difficult.17,18 Other associated injuries may be present including subtalar dislocations, talar neck fracture, malleolar fractures and lateral ligament injuries.5
Fig. 2.
Plain radiograph and CT images showing fracture of the lateral process of the talus.
Classification
Hawkins described three different patterns in his series of lateral process fractures.11
I. Simple fractures: extending from the talofibular articular surface to the posterior talocalcaneal articular surface of the subtalar joint.
II. Comminuted fractures: involving both the articular surfaces and the entire lateral process.
III. Chip fractures: arising from the anterior and inferior portion of the posterior articular process involving only the subtalar joint and not extending into the talofibular articulation.
Boack described a modified classification system that can be applied to fractures of either the lateral or the posterior processes.5 This classification includes four types of fracture, each type subdivided according to severity of bony injury, degree of chondral lesion and ligamentous stability. Based on their description, lateral and posterior process fractures are classified into four types.
Type 1: a small chip or avulsion fracture (< 0.5 cm):
1a - Small (extra-articular) fragment of the lateral process of the talus;
1b - Small fragment of the isolated medial tubercle of the posterior process;
1c - Small (intra-articular) fragment of the lateral process of the talus.
Type 2: an intermediate fragment (0.5 to 1.0 cm) with some displacement:
2a - Extends into the subtalar joint but not to the talofibular joint;
2b - Isolated fracture of the entire lateral tubercle of posterior process.
Type 3: a large fracture fragment (> 1 cm) with associated damage to both the ankle and the subtalar joints:
3a - Single large fragment of the lateral process extending from the talofibular articular surface to the posterior facet of the subtalar joint;
3b - Comminuted fracture of the entire lateral process;
3c - Fracture of the entire posterior process of the talus.
Type 4: a severe form of fracture of either of the processes and associated instability or dislocation of the subtalar joint.
Management
The literature lacks a consensus on the optimum management of lateral process fractures; however, management is aimed at restoring the anatomy of the talus and the articular surfaces in order to preserve the movement and stability of the subtalar joint.19 Appropriate management depends on the size, location and displacement of the fragment, the degree of articular cartilage damage and instability of the subtalar joint.5 When these fractures were described in initial reports, plaster cast immobilization was considered an adequate treatment. However, long-term follow-up in the largest individual series of 13 reported cases treated non-operatively showed that six months after sustaining an injury, nearly 50% of patients had symptoms severe enough to warrant subsequent surgical intervention.6
Management according to Hawkins classification
In cases of Hawkins type I fractures, previous reports have shown that those who were treated with open reduction and internal fixation had better outcomes than those treated non-operatively and had minimal or no symptoms at subsequent follow-up. It has also been reported that patients with type I fractures treated conservatively had 38% incidence of moderate or severe symptoms, with 47% of these requiring subsequent surgery, most commonly requiring subtalar arthrodesis (25%).8 Fractures that were missed or untreated for more than two weeks after sustaining injury have been associated with poor outcome, with long-term and persistent pain despite undergoing subsequent surgery, with up to 20% potentially requiring a subtalar fusion.8,11
In Hawkins type II fractures, an arthroscopic assessment is recommended and, depending on the chondral damage and size of the comminuted fragments, arthroscopic debridement is considered the most suitable treatment option. Missed or untreated fractures or type II fractures treated with plaster casting have been reported to result in poor functional outcomes requiring subtalar fusion.8,11
Hawkins type III fractures have been shown to have good outcome with non-operative treatment with plaster cast immobilization.8,11
Management according to Boack’s classification
Boack recommended that type 1a fractures with an extra-articular or undisplaced small avulsion fragment according to their classification system are better treated with a below-knee plaster cast and partial weight-bearing for a period of six weeks.2,20,21
It is recommended that all displaced fractures involving the articular surface should be treated surgically in order to reduce the risk of long-term degenerative changes.5,22 Even cases with minimally displaced fragments (Boack type 1c) can potentially lead to significant symptoms. These types of fractures should be treated with subtalar arthroscopy and excision, because the loose fragments may damage the articular surface.11,23,24 There have been no reports of instability of the subtalar or the ankle joints following the excision of these fragments.4
In Boack type 2 fractures, an arthroscopic assessment is recommended and, depending on the chondral damage and size of the comminuted fragments, arthroscopic debridement or arthroscopic-assisted reduction and internal fixation is preferred.1,2,5
In Boack type 3a fractures, the single large displaced fragment is best managed using arthroscopic or open reduction and anatomical fixation with headless compression screw, in order to achieve optimum outcome and avoid articular damage by the prominent head of the conventional screw (Figs 3a and 3b). Type 3b fractures require open reduction and internal fixation or excision of the comminuted fragments, depending on the size of the fragments.3,5,21,25,26 Factors determining the outcome are the presence of associated foot and ankle injury, the force injury, and late diagnosis.8
Fig. 3.
Fixation of the lateral process fracture.
In cases of an associated subtalar dislocation, up to 50% of patients may have an additional osteochondral injury. In these cases, emergency management is recommended to relocate the subtalar joint, and arthroscopic assessment should be used to visualize the articular surface and to excise any loose fragments, preventing subsequent problems.5,24,27 The treatment strategy based on Boack’s classification is summarized in Table 1.
Table I.
Management strategy for fractures of the lateral talar process
| Classification | Fracture characteristics | Management |
|---|---|---|
| 1a, 1b | < 0.5 cm, extra-articular |
Conservative |
| 1c | < 0.5 cm, displaced, intra-articular | Arthroscopic excision |
| 2a, 2b | 0.5-1 cm, displaced | Arthroscopic assessment of chondral lesion |
| 3a | > 1 cm single fragment | Arthroscopic assisted screw fixation |
| 3b | > 1 cm or multifragmentary | Open reduction and internal fixation |
| 3c | Entire process fracture | Open reduction and internal fixation |
| 4 | Fracture associated with subtalar dislocation | Emergency reduction, subsequent arthroscopic assessment of chondral lesion |
Surgical approach
The commonly preferred approach is through an anterolateral incision, just anterior and inferior to the tip of the lateral malleolus; however, a modified Ollier approach is an alternative.11,28 The dissection follows through the lateral part of the inferior extensor retinaculum just above the peroneal tendons, leaving the insertion of the short flexor muscles or cervical ligament undisturbed. It occasionally becomes necessary to detach the calcaneofibular ligament from the tip of the fibula.2,3,9
Complications and outcome
Timely diagnosis and management of these fractures are advised in order to prevent long-term complications. Surgical treatment of displaced fractures appears to be the most suitable choice to achieve a successful outcome. Suboptimal management is associated with pain and functional problems due to delayed healing, nonunion, degenerative changes and impingement. Patients with an associated subtalar dislocation have been reported to have the worst outcomes.5,29
Non-operative treatment has been reported to result in good outcomes in up to 60% of cases;4 however, a good outcome has been reported in all early and aggressively treated cases.4,6 Severe degenerative subtalar joint changes have been reported to occur in 10% to 15% of patients requiring subsequent subtalar arthrodesis.6,11,12,21 Nonunion has been reported in 60% of cases managed non-operatively,4,6 compared with 5% of cases following an early surgical intervention. Overall, nonunion can result in poor outcomes in 50% to 70% of cases.4 Further complications include an exostosis of the lateral process during bony healing, resulting in impingement against the calcaneus or the fibula.1,11,24
Fractures of the posterior process of the talus
The posterior process of the talus comprises medial and lateral tubercles, bearing the groove for the flexor hallucis longus tendon. The lateral tubercle, known as Stieda’s process, projects more posteriorly than medially. The lateral tubercle provides attachments to the posterior talocalcaneal and posterior talofibular ligaments. The medial tubercle is usually smaller but variable in size. It provides attachment to the posterior third of the deltoid ligament superiorly and the medial limb of the bifurcate talocalcaneal ligament inferiorly. The undersurface of the combined tubercles articulates with 25% of the posterior facet of the calcaneum.5,30,31
Fractures of the posterolateral process (Shepherd’s fracture)
Fractures of the posterolateral process can potentially be mistaken as os trigonum, which is the posterior process arising from a secondary ossification that failed to fuse with the body of the talus. An os trigonum appears rounded, corticated and is found in 7% to 10% of the normal population. It can also fracture and cause difficulty in diagnosis, but a CT or MRI scan can aid in differentiating the two conditions. Fractures of the lateral tubercle of the posterior process are known as Shepherd’s fracture and may be similar to ankle sprains in presentation but may demonstrate posterolateral tenderness with pain both on movement of the subtalar joint and on passive movement of the flexor hallucis longus (FHL) tendon.
Fractures of the posteromedial process (Cedell’s fracture)
Cedell first described fractures of the medial part of the posterior process of the talus.32 These can be misdiagnosed as ankle sprains if not included in the differential diagnosis of posteromedial ankle pain.
Fractures of the entire posterior process of the talus are very rare. There are only a few reported cases of entire process fractures.16,20,25,37,44
Mechanism
The causative injuries are similar to lateral process fractures. Two mechanisms have been postulated. The first is forced hyperplantarflexion and inversion causing direct compression of the posterior talus between the posterior tibial rim and the dorsal rim of the posterior facet of the calcaneum.5,31,33,34 The second assumption is that the posterior talofibular ligament causes an avulsion fracture of the lateral tubercle during hyperdorsiflexion and inversion motion.5,8,33,35 Cedell described the posteromedial tubercle fracture as an avulsion injury resulting from forced pronation and dorsiflexion of the foot.28,30,32 Other proposed mechanisms include direct trauma to the posteromedial facet, impingement of the sustentaculum tali in supination and forced dorsiflexion in cases of high-energy trauma.19,36
Diagnosis
Patients usually present with swelling and pain in the hindfoot area. The posterior talar impingement test is positive, with an increasing pain associated with active movements of the toe flexors or passive extension of the big toe.3,33
Plain radiographs of the ankle (anteroposterior, mortise and lateral views) are routinely obtained; however, the radiological features of minimal cortical breach and subtle lucency are not always easily identified (Fig. 4a).5,21 Broden’s view may aid in the assessment of subtalar joint involvement. It is taken by internally rotating the foot 45° while the beam is centered on the subtalar joint and angulated cephalad at a range of 10° to 40° from vertical.29 Ebraheim et al have suggested that two oblique views at 45° and 70° of external rotation may be helpful if the standard radiographs are inconclusive.37 Up to 40% of these fractures may be missed on initial presentation on plain radiographs.5,11,12,24 A high index of suspicion should be kept based on specific injury mechanisms and an urgent CT scan should be performed in order to identify the fracture, to assess the size, displacement and extent of the fracture fragmentation, or to differentiate the presence of accessory ossicles from acute fractures (Fig. 4b).2,17,20,22,31 These fractures may be associated with subtalar dislocations and may have osteochondral injuries in up to 50% of cases involving subtalar dislocations.3,19,24,27,28,37
Fig. 4.
Plain radiograph and sagittal CT images showing fracture of the posterior process of the talus.
Classification
Boack described his classification for the lateral process as well as for the posterior process of the talus as described in detail previously.5
Management
The principles of management are the same as per lateral process fractures. Undisplaced fractures can be managed in a plaster cast for six to eight weeks but surgical treatment is recommended either in the form of open reduction and internal fixation or excision of the fracture fragments, depending on their size, in order to minimize long-term pain.3,5,31
Surgical approach
Open reduction and internal fixation of posterior process fractures can be performed through a posterolateral or a posteromedial approach, depending on the location of the displaced fragments. The posteromedial approach involves a curved incision halfway between the medial malleolus and the margin of the Achilles tendon. The neurovascular bundle is mobilized for adequate access to the fracture fragments.2 Fracture fragments can be fixed using lag screws (1.5, 2.0 or 2.7 mm). The posterolateral approach involves a longitudinal incision between the lateral border of the fibula and the Achilles tendon. The fracture fragment is identified and fixed using the same techniques.38 It is essential to assess the stability of the subtalar joint and address it as needed to prevent long-term problems.39
Complications and outcome
Intra-articular fractures of the entire posterior process have been associated with a poor outcome due to the higher incidence of malunion and early degenerative changes.3,5,23,31,36 In conservatively treated cases, up to one-third may develop avascular necrosis.5 Up to 75% of patients initially treated conservatively may subsequently require excision of the fragments in case of posteromedial tubercle fractures. Displaced fractures, depending upon their size, can either be excised or fixed with small screws.
In cases of nonunion, malunion or exostosis resulting in impingement, excision of the fragments should be considered to eliminate the symptoms.11,24 In cases of significant and symptomatic subtalar joint arthritis, an arthrodesis may be required.40
Conclusion
Fractures of the lateral and the posterior processes of the talus are uncommon but significant injuries that may result in significant disability in cases of missed fractures, delayed diagnosis or inadequately treated fractures. A high index of suspicion is appropriate in cases of acute ankle sprains or persistent ankle pain after previous ankle injury. CT scanning is essential in all suspected cases and can aid in management planning. Early diagnosis and timely management of these fractures are useful in order to avoid long-term problems of malunion, nonunion or severe subtalar arthritis.
Footnotes
ICMJE Conflict of interest statement: None declared.
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- 1. Sanders TG, Ptaszek AJ, Morrison WB. Fracture of the lateral process of the talus: appearance at MR imaging and clinical significance. Skeletal Radiol 1999;28:236-239. [DOI] [PubMed] [Google Scholar]
- 2. Boack DH, Manegold S, Haas NP. [Treatment strategy for talus fractures]. Unfallchirurg 2004;107:499-514. [DOI] [PubMed] [Google Scholar]
- 3. Heckman JD, McLean MR. Fractures of the lateral process of the talus. Clin Orthop Relat Res 1985;(199):108-113. [PubMed] [Google Scholar]
- 4. Parsons SJ. Relation between the occurrence of bony union and outcome for fractures of the lateral process of the talus: a case report and analysis of published reports. Br J Sports Med 2003;37:274-276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Boack DH, Manegold S. Peripheral talar fractures. Injury 2004;35(suppl 2):SB23-SB35. [DOI] [PubMed] [Google Scholar]
- 6. Mukherjee SK, Pringle RM, Baxter AD. Fracture of the lateral process of the talus. A report of thirteen cases. J Bone Joint Surg Br 1974;56:263-273. [PubMed] [Google Scholar]
- 7. Kirkpatrick DP, Hunter RE, Janes PC, Mastrangelo J, Nicholas RA. The snowboarder’s foot and ankle. Am J Sports Med 1998;26:271-277. [DOI] [PubMed] [Google Scholar]
- 8. Perera A, Baker JF, Lui DF, Stephens MM. The management and outcome of lateral process fracture of the talus. Foot Ankle Surg 2010;16:15. [DOI] [PubMed] [Google Scholar]
- 9. Boon AJ, Smith J, Zobitz ME, Amrami KM. Snowboarder’s talus fracture. Mechanism of injury. Am J Sports Med 2001;29:333-338. [DOI] [PubMed] [Google Scholar]
- 10. Funk JR, Srinivasan SC, Crandall JR. Snowboarder’s talus fractures experimentally produced by eversion and dorsiflexion. Am J Sports Med 2003;31:921-928. [DOI] [PubMed] [Google Scholar]
- 11. Hawkins LG. Fracture of the lateral process of the talus. J Bone Joint Surg Am 1965;47:1170-1175. [PubMed] [Google Scholar]
- 12. Mills HJ, Horne G. Fractures of the lateral process of the talus. Aust N Z J Surg 1987;57:643-646. [DOI] [PubMed] [Google Scholar]
- 13. von Knoch F, Reckord U, von Knoch M, Sommer C. Fracture of the lateral process of the talus in snowboarders. J Bone Joint Surg Br 2007;89:772-777. [DOI] [PubMed] [Google Scholar]
- 14. Langer P, Nickisch F, Spenciner D, Fleming B, DiGiovanni CW. In vitro evaluation of the effect lateral process talar excision on ankle and subtalar joint stability. Foot Ankle Int 2007;28:78-83. [DOI] [PubMed] [Google Scholar]
- 15. Cimmino CV. Fracture of the lateral process of the talus. Am J Roentgenol Radium Ther Nucl Med 1963;90:1277-1280. [PubMed] [Google Scholar]
- 16. Bladin C, McCrory P. Snowboarding injuries. An overview. Sports Med 1995;19:358-364. [DOI] [PubMed] [Google Scholar]
- 17. Noble J, Royle SG. Fracture of the lateral process of the talus: computed tomographic scan diagnosis. Br J Sports Med 1992;26:245-246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Whitby EH, Barrington NA. Fractures of the lateral process of the talus–the value of lateral tomography. Br J Radiol 1995;68:583-586. [DOI] [PubMed] [Google Scholar]
- 19. Chen YJ, Hsu RW, Shih HN, Huang TJ. Fracture of the entire posterior process of talus associated with subtalar dislocation: a case report. Foot Ankle Int 1996;17:226-229. [DOI] [PubMed] [Google Scholar]
- 20. Ebraheim NA, Skie MC, Podeszwa DA, Jackson WT. Evaluation of process fractures of the talus using computed tomography. J Orthop Trauma 1994;8:332-337. [DOI] [PubMed] [Google Scholar]
- 21. McCrory P, Bladin C. Fractures of the lateral process of the talus: A clinical review. “Snowboarder's ankle”. Clin J Sport Med 1996;6:124–128. [DOI] [PubMed] [Google Scholar]
- 22. Ebraheim NA, Padanilam TG, Wong FY. Posteromedial process fractures of the talus. Foot Ankle Int 1995;16:734-739. [DOI] [PubMed] [Google Scholar]
- 23. Veazey BL, Heckman JD, Galindo MJ, McGanity PL. Excision of ununited fractures of the posterior process of the talus: a treatment for chronic posterior ankle pain. Foot Ankle 1992;13:453-457. [DOI] [PubMed] [Google Scholar]
- 24. Tucker DJ, Feder JM, Boylan JP. Fractures of the lateral process of the talus: two case reports and a comprehensive literature review. Foot Ankle Int 1998;19:641-646. [DOI] [PubMed] [Google Scholar]
- 25. Kettunen J, Waris P, Hermunen H, Hamalainen R. Fracture of the lateral talus process. A case report. Acta Orthop Scand 1992;63:356-357. [DOI] [PubMed] [Google Scholar]
- 26. Mallon WJ, Wombwell JH, Nunley JA. Intra-articular talar fractures: repair using the Herbert bone screw. Foot Ankle 1989;10:88-92. [DOI] [PubMed] [Google Scholar]
- 27. Bohay DR, Manoli A., II Occult fractures following subtalar joint injuries. Foot Ankle Int 1996;17:164-169. [DOI] [PubMed] [Google Scholar]
- 28. Nadim Y, Tosic A, Ebraheim N. Open reduction and internal fixation of fracture of the posterior process of the talus: a case report and review of the literature. Foot Ankle Int 1999;20:50-52. [DOI] [PubMed] [Google Scholar]
- 29. Letonoff EJ, Najarian CB, Suleiman J. The posteromedial process fracture of the talus: a case report. J Foot Ankle Surg 2002;41:52-56. [DOI] [PubMed] [Google Scholar]
- 30. Banks AS, Caldarella D. Fractures of the posteromedial process of the talus. J Am Podiatr Med Assoc 1994;84:66-70. [DOI] [PubMed] [Google Scholar]
- 31. Nyska M, Howard CB, Matan Y, et al. Fracture of the posterior body of the talus–the hidden fracture. Arch Orthop Trauma Surg 1998;117:114-117. [DOI] [PubMed] [Google Scholar]
- 32. Cedell CA. Rupture of the posterior talotibial ligament with the avulsion of a bone fragment from the talus. Acta Orthop Scand 1974;45:454-461. [DOI] [PubMed] [Google Scholar]
- 33. Higgins TF, Baumgaertner MR. Diagnosis and treatment of fractures of the talus: a comprehensive review of the literature. Foot Ankle Int 1999;20:595-605. [DOI] [PubMed] [Google Scholar]
- 34. Nasser S, Manoli A., II Fracture of the entire posterior process of the talus: a case report. Foot Ankle 1990;10:235-238. [DOI] [PubMed] [Google Scholar]
- 35. Baumhauer JF, Alvarez RG. Controversies in treating talus fractures. Orthop Clin North Am 1995;26:335-351. [PubMed] [Google Scholar]
- 36. Thermann H, Ansar M, Tscherne H. [Process fractures. A diagnostic problem in ankle injuries]. Orthopade 1999;28:518-528. [PubMed] [Google Scholar]
- 37. Ebraheim NA, Patil V, Frisch NC, Liu X. Diagnosis of medial tubercle fractures of the talar posterior process using oblique views. Injury 2007;38:1313-1317. [DOI] [PubMed] [Google Scholar]
- 38. Naranja RJ, Jr, Monaghan BA, Okereke E, Williams GR., Jr Open medial subtalar dislocation associated with fracture of the posterior process of the talus. J Orthop Trauma 1996;10:142-144. [DOI] [PubMed] [Google Scholar]
- 39. Berndt AL, Harty M. Transchondral fractures (osteochondritis dissecans) of the talus. J Bone Joint Surg [Am] 1959;41-A:988-1020. [PubMed] [Google Scholar]
- 40. Stefko RM, Lauerman WC, Heckman JD. Tarsal tunnel syndrome caused by an unrecognized fracture of the posterior process of the talus (Cedell fracture). A case report. J Bone Joint Surg [Am] 1994;76:116-118. [DOI] [PubMed] [Google Scholar]