Abstract
Mechanical or anatomical alignment techniques create a supposedly ‘biomechanically friendly’ but often functionally limited prosthetic knee.
Alternative techniques for alignment in total knee arthroplasty (TKA) aim at being more anatomical and patient-specific, aiming to improve functional outcomes after TKA.
The kinematic alignment (KA) technique for TKA has shown good early clinical outcomes. Its role in extreme anatomical variation remains to be defined.
The restricted KA technique for TKA might be a reasonable option for patients with extreme anatomical variation.
While unicompartmental knee arthroplasty (UKA) has many advantages over TKA, the revision rate remains higher compared with TKA. One major explanation is the relative ease with which a UKA can be converted to a TKA, compared with revising a TKA. This can be considered as an additional advantage of UKA. Another reason is that surgeons favour revising a UKA to a TKA in cases of degeneration of the other femorotibial compartment rather than performing a relatively simple re-operation of the knee by doing an additional UKA (staged bi-UKA).
Cite this article: EFORT Open Rev 2018;3:1–6. DOI: 10.1302/2058-5241.3.170021
Keywords: knee arthroplasty, kinematic alignment technique, mechanical alignment technique
Introduction
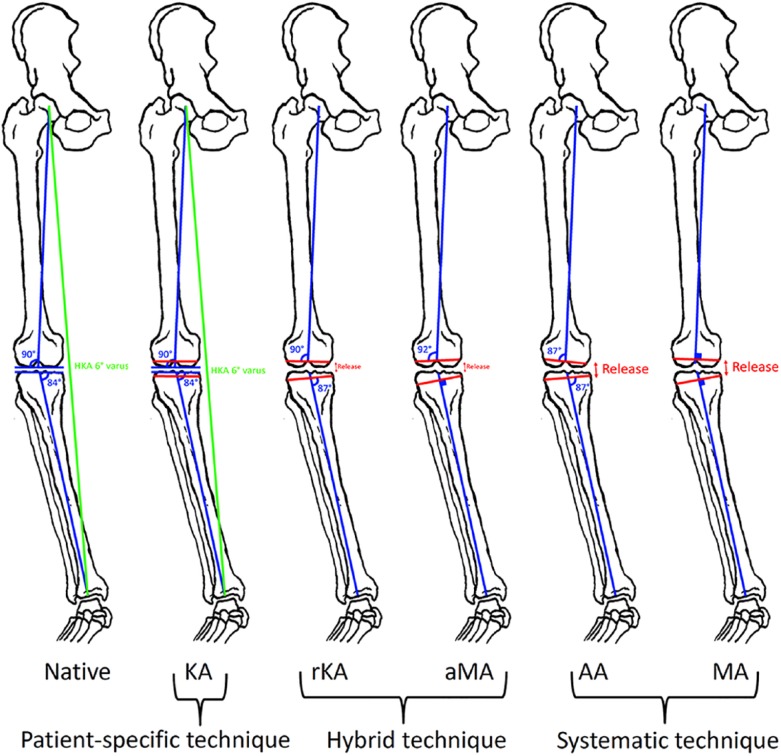
Knee arthroplasty surgery is becoming more common with an increasing prevalence of osteoarthritis (OA) and increasing life expectancy.1 Knee arthroplasty can be either partial (PKA) or total (TKA), depending on the extent of joint disease, with both approaches having shown favourable long-term survivorship and functional outcomes.2,3 However, by comparison with total hip arthroplasty, TKA provides overall inferior functional outcomes with a high prevalence of residual symptoms and lower patient satisfaction.4-6 Technological advances leading to better implant design and surgical precision have unfortunately not helped to significantly improve TKA patients’ functional outcomes.7,8 Considering this and other improvements such as better wear-resistance with modern polyethylene and better cementation, some authors have started to challenge the basics of the mechanical alignment (MA) technique and recently developed and tested more anatomy-friendly techniques for TKA.9 Because the optimal knee soft-tissue tension10 and component alignment in TKA remain a matter of debate,9 this instructional review aims to classify the multiple techniques (systematic, patient-specific and hybrid alignment techniques) for knee implant positioning (Fig. 1) and to summarize the evidence behind each one.
Fig. 1.
Different techniques for aligning total knee arthroplasty implants on a patient with 6° constitutional varus limb alignment. From left to right, kinematic alignment (KA), restricted KA (rKA), adjusted mechanical alignment (aMA), anatomical alignment (AA), mechanical alignment (MA). Excepting the KA technique, all techniques necessitate varying amounts of soft-tissue release (more so for systematic techniques than hybrid techniques).
Systematic alignment techniques for knee arthroplasty
A systematic implant positioning results in implants being always positioned in the same way for every patient, which disregards patient-specific knee joint anatomy. This has been described as ‘biomechanically-friendly’. In order to optimize implant survivorship by reducing the risk of accelerated polyethylene wear, early implant loosening and patella instability, the recommended positioning for TKA implants has been to create a straight limb with a perpendicular tibiofemoral joint line (TFJL). In order to do so, as initially described by Insall et al, implants were systematically positioned perpendicular to the mechanical axis of the femur and tibia in the frontal plane.11,12 This systematic positioning, the MA technique, does not take into account patient-specific knee anatomy and generated a similar biomechanically-friendly but non-physiological prosthetic knee geometry for almost every patient. Traditionally, the axial rotational alignment of the femoral component was suggested to be systematically externally rotated 3° relative to the posterior condylar line (measured resection technique) in order to compensate for the frequent varus orientation (3° on average in the Caucasian population) of the proximal tibia joint line.12 However, because the proximal tibia joint line orientation varies between patients, this frequently resulted in the necessity for balancing a non-rectangular flexion gap. However, the technical demands of properly balancing a TKA and the frequently observed post-operative clinically deleterious knee imbalances generated by this conventional technique3,13 led to the development of the gap-balancing technique to adjust the axial rotational alignment of the femoral component.14
Patient-specific femoral implant rotation enables adjustment of the flexion gap to equal the extension gap and therefore significantly improves the prosthetic knee balance. Unfortunately this technique does not respect the physiological lateral knee laxity, which seems to be beneficial for knee biomechanics and potentially for clinical TKA outcomes.15
Because the average TFJL frontal orientation in the population is 3° valgus,16,17 a technique for positioning TKA implants trying to create a systematic 3° valgus orientated TFJL, namely the anatomical alignment (AA) technique,18 was developed in parallel with the MA technique. The goal of this technique is to simplify human anatomy by aiming at the mean value for all patients with the theoretical advantage (compared with the MA technique) of reducing the risk of stretching the lateral retinaculum during deep flexion and therefore potentially reducing the risk of anterior knee pain and abnormal patellar tracking by optimizing the patella biomechanics.19 Hungerford, Kenna and Krackow18 promoted this philosophy in the 1980s; however, the poor precision of initial instrumentation, which risked ending up with supposedly clinically deleterious excessive varus orientation of the tibial implant,20,21 limited its widespread use. Over the last decade, new implant designs with a built-in oblique TFJL have been developed, and their mechanical positioning enables the creation of a systematic oblique TFJL, reproducing the effect of the AA technique.22-24 The MA of those new implants therefore generated an AA-like technique with MA bone cuts. Published results using the AA and AA-like techniques have shown good mid- to long-term results.18,23,24 However, there is still no definitive scientific evidence that the AA technique provides improvement compared with the traditional MA technique.25,26
As the recommended frontal alignment with MA technique is neutral (0°+/-3°)27 and constitutional limb alignment in the population varies from valgus to varus,17 the idea of aligning the TKA to slightly reproduce the constitutional limb deformity was promoted.28-31 To achieve this goal, an adjustment relative to the frontal mechanical axis of the femur with the femoral component positioning in slight (2° to 3°) varus (patient with constitutional varus limb) or slight valgus (patient with constitutional valgus limb) while keeping the tibial component perpendicularly aligned to the frontal mechanical axis of the tibia has been proposed.28-31 This approach could be thought of as a hybrid technique, as it is an adjusted version of the MA technique (aMA) aiming at respecting more of the patient’s anatomy and therefore at helping to obtain ligamentous balance in extension. One study reported excellent functional outcomes with aMA-TKAs for patients with constitutionally varus knees,30 and another has shown good long-term clinical outcomes for patients with constitutionally valgus knees.31
Patient-specific alignment techniques for knee arthroplasty
Patient-specific alignment can be achieved with either the use of PKA or TKA implants.
Kinematic alignment (KA) technique for TKA
Following the results of a couple of studies suggesting that the standing post-operative limb alignment was of poor value in predicting clinical outcomes for patients with prosthetic knees,27,28 the idea of preserving the constitutional knee alignment has arisen. The concept of preserving the entire constitutional knee alignment has been developed by Howell and Hull32 since 2007 with the KA technique. KA aims to respect the 3D anatomy of the TFJL and aims at aligning the implants with the kinematic axis of the knee around which the tibia moves around the femur. Put simply, the KA technique is a true resurfacing of the femorotibial joint aiming at restoring its pre-arthritic (or constitutional) articular surfaces and soft-tissue laxity.32 It is important to understand that the KA technique is not an adjustment of the MA or AA techniques, but rather a new surgical technique for TKA, with nothing in common with the MA technique except the sagittal positioning of the femoral component. The KA technique can be performed with the use of navigation33 or patient-specific instrumentation,34 or manual instrumentation using the measured resection technique.35 Recently, implant manufacturers have developed specific KA manual instrumentation.35 A prospective cohort study36 and a systematic review37 found that the KA technique generated excellent overall outcomes up until six years follow-up. Randomized controlled trials comparing MA and KA TKA have shown faster recovery with KA TKA,34,42 no significant difference in complications38-40 and significant early (one to two years average follow-up) clinical improvements with KA TKA using patient-reported outcomes such as Oxford Knee Scores and Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) Scores.34,38,40,42 A meta-analysis43 also concluded that KA TKAs provide a better functional outcome (Oxford Knee Score and Knee Society Score) and a similar complication rate compared with MA TKA at two years of follow-up. Longer-term outcomes are needed in order to define the best indication for the KA technique as it is likely that some patients with extreme variation in constitutional knee anatomy (severe pathoanatomy) may not benefit from restoring it.44
UKA – another way of restoring constitutional knee anatomy and kinematics
Although it is widely accepted that generalized (tricompartmental) OA is best treated with TKA, OA localized to one or two compartments can be treated with either PKA or TKA.2,45 For varus patients with medial TF OA, replacing the disease-free lateral TF and patellofemoral compartments, and potentially removing the anterior and posterior cruciate ligaments, alter the knee kinematics and proprioception.46 Therefore, partial knee resurfacing techniques confined to the damaged and symptomatic compartments have been suggested.47,48 These ligament- and bone-sparing methods attempt to restore the constitutional knee anatomy (like KA TKA), improve knee stability and preserve joint proprioception.49
Studies have shown excellent functional outcomes and long-term survival after medial UKA with minimal wear, even in the context of constitutional deformity.45,50,51-54 Therefore, indications for medial UKA have been progressively widened, with constitutional frontal limb deformity no longer being considered a contraindication, and UKA is now being estimated to be a valuable treatment option for 30% to 80% of patients requiring a knee arthroplasty.45 However, the reality is that PKA usually represents less than 10% of a surgeon’s knee arthroplasties, mostly due to the surgeon’s preference,55 their fear of having an increased revision rate50,56 and the different ways of interpreting the current literature.50 Surprisingly, although medial UKA results in better clinical outcomes compared with MA TKA, with better efficacy (faster recovery, better functional scores, higher satisfaction) and safety (lower rates of morbidity and mortality and fewer complications),38,39,45,50,53 national joint registries still show a substantially higher revision rate for medial UKA compared with MA TKA.5,56,57 This is mainly because UKA fixation may be more challenging (small implant surface), because of disease progression in other native compartments and because a medial UKA is easier to revise compared with a TKA, and therefore surgeons have a lower threshold for revising a UKA (for a similar disappointing functional outcome, UKAs are more likely to be revised than TKAs).50,57
Hybrid alignment techniques for knee arthroplasty
Patients can have wide-ranging variation in knee anatomy and performing KA TKA can lead to a high rate of limb alignment and implant positioning which would traditionally be considered as at risk of failure.39 Therefore, some cautious authors33 have described performing a KA TKA when there was no significant pathoanatomy (constitutional limb and TFJL alignments) while slightly correcting in more severe cases, by adjusting the position of either the tibial or femoral component and following a specific algorithm.58 In doing so, it is hoped that a patient’s supposed safe range of alignment will be achieved; a hip-knee-ankle angle within 3° (varus or valgus) and frontal implants positioning within 5° of femoral or tibial mechanical axis.33,58 This technique has been referred to as restricted KA (rKA) (as authors restrict the indication of a full KA technique)58 and has been shown to generate good early clinical outcomes.33 Surgeons willing to do the rKA technique need to assess the patient’s anatomy (limb alignment, joint line obliquity) pre- or intraoperatively, in order to adjust the positioning of implants if needed. The rKA technique is therefore best performed with the use of intraoperative computer-assisted navigation or with the use of preoperative planning and the subsequent generation of patient-specific instruments.33
Conclusions
The positioning of knee implants and the ‘systematic approach’ (patient’s anatomy adapted to a fixed implant orientation) versus the ‘patient-specific approach’ (implant positioning to replicate the pre-arthritic patient’s anatomy) is currently largely debated. Systematic and biomechanically-friendly alignment techniques such as the MA and AA techniques have successfully demonstrated good long-term survival but with some functional limitations. The patient-specific and anatomically-friendly KA technique has emerged and has shown promising results; however, this technique might not be suitable for extreme anatomical variants which may be considered as pathoanatomies. In the latter situation, the hybrid rKA technique seems to be an attractive option. However, alignment and implant orientation probably only explain in part some of our unsatisfactory TKA results, as patient’s preoperative disease status and chronic pain syndrome installation may also play a significant role. Also, in all TKAs, whatever the technique of positioning, significant anatomical and kinematic modifications are made secondary to meniscus removal, changing the conforming cartilaginous surface to a rigid polyethylene, removal of cruciate ligament(s) with compensatory implant design(s) (central post, polyethylene lips and congruency, etc), which make it very challenging to restore normal knee function. Further research is needed to improve functional outcomes of TKA by defining the true value and best indications for each alignment technique and implant design.
Footnotes
ICMJE Conflict of interest statement: Mr Rivière declares board membership of FORTE; consultancy for Depuy, activities outside the submitted work. Mr Boughton declares grants from the Royal College of Surgeons of England and Dunhill Medical Trust Clinical Research Fellowship, activity relating to the submitted work; travel and expenses from the Royal College of Surgeons of England Capener Travelling Fellowship, activity outside the submitted work. Mr Cobb declares board membership of Embody Orthopaedic; grants from Zimmer Biomet; lecture fees from Microport; patents from Imperial Innovations; royalties from Matortho; stock options from Embody Orthopaedic; travel expenses from Zimmer Biomet, activities outside the submitted work.
Funding
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- 1. Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg [Am] 2007;89-A:780-785. [DOI] [PubMed] [Google Scholar]
- 2. Bonnin MP, Saffarini M, Bossard N, Dantony E, Victor J. Morphometric analysis of the distal femur in total knee arthroplasty and native knees. Bone Joint J 2016;98-B:49-57. [DOI] [PubMed] [Google Scholar]
- 3. Le DH, Goodman SB, Maloney WJ, Huddleston JI. Current modes of failure in TKA: infection, instability, and stiffness predominate. Clin Orthop Relat Res 2014;472:2197-2200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Williams DP, Blakey CM, Hadfield SG, et al. Long-term trends in the Oxford knee score following total knee replacement. Bone Joint J 2013;95-B:45-51. [DOI] [PubMed] [Google Scholar]
- 5. Liddle AD, Pandit H, Judge A, Murray DW. Patient-reported outcomes after total and unicompartmental knee arthroplasty: a study of 14,076 matched patients from the National Joint Registry for England and Wales. Bone Joint J 2015;97-B:793-801. [DOI] [PubMed] [Google Scholar]
- 6. Nam D, Nunley RM, Barrack RL. Patient dissatisfaction following total knee replacement: a growing concern? Bone Joint J 2014;96-B(Suppl A):96-100. [DOI] [PubMed] [Google Scholar]
- 7. Sassoon A, Nam D, Nunley R, Barrack R. Systematic review of patient-specific instrumentation in total knee arthroplasty: new but not improved. Clin Orthop Relat Res 2015;473:151-158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Xie C, Liu K, Xiao L, Tang R. Clinical Outcomes After Computer-assisted Versus Conventional Total Knee Arthroplasty. Orthopedics 2012;35:e647-e653. [DOI] [PubMed] [Google Scholar]
- 9. Cherian JJ, Kapadia BH, Banerjee S, et al. Mechanical, anatomical, and kinematic axis in TKA: concepts and practical applications. Curr Rev Musculoskelet Med 2014;7:89-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Roth JD, Howell SM, Hull ML. Native knee laxities at 0 degrees, 45 degrees, and 90 degrees of flexion and their relationship to the goal of the gap-balancing alignment method of total knee arthroplasty. J Bone Joint Surg [Am] 2015;97:1678-1684. [DOI] [PubMed] [Google Scholar]
- 11. Sharkey PF, Hozack WJ, Rothman RH, Shastri S, Jacoby SM. Insall Award paper. Why are total knee arthroplasties failing today? Clin Orthop Relat Res 2002;404:7-13. [DOI] [PubMed] [Google Scholar]
- 12. Whiteside LA. Soft tissue balancing: the knee. J Arthroplasty 2002;17(Suppl 1):23-27. [DOI] [PubMed] [Google Scholar]
- 13. Gu Y, Roth JD, Howell SM, Hull ML. How frequently do four methods for mechanically aligning a total knee arthroplasty cause collateral ligament imbalance and change alignment from normal in white patients? AAOS Exhibit Selection. J Bone Joint Surg [Am] 2014;96:e101, 1-9. [DOI] [PubMed] [Google Scholar]
- 14. Daines BK, Dennis DA. Gap balancing vs. measured resection technique in total knee arthroplasty. Clin Orthop Surg 2014;6:1-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Matsumoto T, Shibanuma N, Takayama K, et al. The influence of intraoperative soft tissue balance on patellar pressure in posterior-stabilized total knee arthroplasty. Knee 2016;23:540-544. [DOI] [PubMed] [Google Scholar]
- 16. Nam D, Shah RR, Nunley RM, Barrack RL. Evaluation of the 3-dimensional, weight-bearing orientation of the normal adult knee. J Arthroplasty 2014;29:906-911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Bellemans J, Colyn W, Vandenneucker H, Victor J. The Chitranjan Ranawat award: is neutral mechanical alignment normal for all patients? The concept of constitutional varus. Clin Orthop Relat Res 2012;470:45-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Hungerford DS, Kenna RV, Krackow KA. The porous-coated anatomic total knee. Orthop Clin North Am 1982;13:103-122. [PubMed] [Google Scholar]
- 19. Ghosh KM, Merican AM, Iranpour-Boroujeni F, Deehan DJ, Amis AA. Length change patterns of the extensor retinaculum and the effect of total knee replacement. J Orthop Res 2009;27:865-870. [DOI] [PubMed] [Google Scholar]
- 20. Ritter MA, Davis KE, Meding JB, et al. The effect of alignment and BMI on failure of total knee replacement. J Bone Joint Surg [Am] 2011;93-A:1588-1596. [DOI] [PubMed] [Google Scholar]
- 21. Srivastava A, Lee GY, Steklov N, et al. Effect of tibial component varus on wear in total knee arthroplasty. Knee 2012;19:560-563. [DOI] [PubMed] [Google Scholar]
- 22. Schwechter EM, Fitz W. Design rationale for customized TKA: a new idea or revisiting the past? Curr Rev Musculoskelet Med 2012;5:303-308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ishii Y, Matsuda Y, Sakata S, Onda N, Omori G. Primary total knee arthroplasty using the Genesis I total knee prosthesis: a 5- to 10-year follow-up study. Knee 2005;12:341-345. [DOI] [PubMed] [Google Scholar]
- 24. Ahmed I, Salmon LJ, Waller A, et al. Total knee arthroplasty with an oxidised zirconium femoral component: ten-year survivorship analysis. Bone Joint J 2016;98-B:58-64. [DOI] [PubMed] [Google Scholar]
- 25. Yim JH, Song EK, Khan MS, Sun ZH, Seon JK. A comparison of classical and anatomical total knee alignment methods in robotic total knee arthroplasty: classical and anatomical knee alignment methods in TKA. J Arthroplasty 2013;28:932-937. [DOI] [PubMed] [Google Scholar]
- 26. Mugnai R, Digennaro V, Ensini A, Leardini A, Catani F. Can TKA design affect the clinical outcome? Comparison between two guided-motion systems. Knee Surg Sports Traumatol Arthrosc 2014;22:581-589. [DOI] [PubMed] [Google Scholar]
- 27. Parratte S, Pagnano MW, Trousdale RT, Berry DJ. Effect of postoperative mechanical axis alignment on the fifteen-year survival of modern, cemented total knee replacements. J Bone Joint Surg [Am] 2010;92-A:2143-2149. [DOI] [PubMed] [Google Scholar]
- 28. Vanlommel L, Vanlommel J, Claes S, Bellemans J. Slight undercorrection following total knee arthroplasty results in superior clinical outcomes in varus knees. Knee Surg Sports Traumatol Arthrosc 2013;21:2325-2330. [DOI] [PubMed] [Google Scholar]
- 29. Victor JM, Bassens D, Bellemans J, et al. Constitutional varus does not affect joint line orientation in the coronal plane. Clin Orthop Relat Res 2014;472:98-104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. De Muylder J, Victor J, Cornu O, Kaminski L, Thienpont E. Total knee arthroplasty in patients with substantial deformities using primary knee components. Knee Surg Sports Traumatol Arthrosc 2015;23:3653-3659. [DOI] [PubMed] [Google Scholar]
- 31. Ranawat AS, Ranawat CS, Elkus M, et al. Total knee arthroplasty for severe valgus deformity. J Bone Joint Surg [Am] 2005;87(Pt 2)(suppl 1):271-284. [DOI] [PubMed] [Google Scholar]
- 32. Howell SM, Hull ML. Kinematic alignment in total knee arthroplasty. In: Norman Scott W. Insall and Scott Surgery of the Knee (5th edition). London: Churchill Livingston, 2011:1255-1269. [Google Scholar]
- 33. Hutt JR, LeBlanc MA, Massé V, Lavigne M, Vendittoli PA. Kinematic TKA using navigation: surgical technique and initial results. Orthop Traumatol Surg Res 2016;102:99-104. [DOI] [PubMed] [Google Scholar]
- 34. Waterson HB, Clement ND, Eyres KS, Mandalia VI, Toms AD. The early outcome of kinematic versus mechanical alignment in total knee arthroplasty: a prospective randomised control trial. Bone Joint J 2016;98-B:1360-1368. [DOI] [PubMed] [Google Scholar]
- 35. Howell SM, Hull ML. Kinematic alignment in total knee arthroplasty. Definition, history, principle, surgical technique, and results of an alignment option for TKA. Arthropaedia 2014;1:44-53. [Google Scholar]
- 36. Howell SM, Papadopoulos S, Kuznik K, Ghaly LR, Hull ML. Does varus alignment adversely affect implant survival and function six years after kinematically aligned total knee arthroplasty? Int Orthop 2015;39:2117-2124. [DOI] [PubMed] [Google Scholar]
- 37. Lee YS, Howell SM, Won YY, et al. Kinematic alignment is a possible alternative to mechanical alignment in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 2017;25:3467-3479. [DOI] [PubMed] [Google Scholar]
- 38. Dossett HG, Swartz GJ, Estrada NA, LeFevre GW, Kwasman BG. Kinematically versus mechanically aligned total knee arthroplasty. Orthopedics 2012;35:e160-e169. [DOI] [PubMed] [Google Scholar]
- 39. Young SW, Walker ML, Bayan A, et al. The Chitranjan S. Ranawat Award: no difference in 2-year functional outcomes using kinematic versus mechanical alignment in TKA: a randomized controlled clinical trial. Clin Orthop Relat Res 2016;475:9-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Calliess T, Bauer K, Stukenborg-Colsman C, et al. PSI kinematic versus non-PSI mechanical alignment in total knee arthroplasty: a prospective, randomized study. Knee Surg Sports Traumatol Arthrosc 2016;96:e8175. [DOI] [PubMed] [Google Scholar]
- 41. Matsumoto T, Takayama K, Ishida K, et al. Radiological and clinical comparison of kinematically versus mechanically aligned total knee arthroplasty. Bone Joint J 2017;99-B:640-646. [DOI] [PubMed] [Google Scholar]
- 42. Dossett HG, Estrada NA, Swartz GJ, LeFevre GW, Kwasman BG. A randomised controlled trial of kinematically and mechanically aligned total knee replacements: two-year clinical results. Bone Joint J 2014;96-B:907-913. [DOI] [PubMed] [Google Scholar]
- 43. Courtney PM, Lee GC. Early Outcomes of Kinematic Alignment in Primary Total Knee Arthroplasty: A Meta-Analysis of the Literature. J Arthroplasty 2017;32:2028-2032.e1. [DOI] [PubMed] [Google Scholar]
- 44. Rivière C, Auvinet E, Vendittoli PA, Cobb J, Parratte S. Alignment options for total knee arthroplasty: a systematic review. Orthop Traumatol Surg Res 2017;103:1047-1056. [DOI] [PubMed] [Google Scholar]
- 45. Berend KR, Berend ME, Dalury DF, et al. Consensus Statement on Indications and Contraindications for Medial Unicompartmental Knee Arthroplasty. J Surg Orthop Adv 2015;24:252-256. [PubMed] [Google Scholar]
- 46. Dennis DA, Mahfouz MR, Komistek RD, Hoff W. In vivo determination of normal and anterior cruciate ligament-deficient knee kinematics. J Biomech 2005;38:241-253. [DOI] [PubMed] [Google Scholar]
- 47. Parratte S, Pauly V, Aubaniac JM, Argenson JN. Survival of bicompartmental knee arthroplasty at 5 to 23 years. Clin Orthop Relat Res 2010;468:64-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Ollivier M, Abdel MP, Parratte S, Argenson JN. Lateral unicondylar knee arthroplasty (UKA): contemporary indications, surgical technique, and results. Int Orthop 2014;38:449-455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Wünschel M, Lo J, Dilger T, Wülker N, Müller O. Influence of bi- and tri-compartmental knee arthroplasty on the kinematics of the knee joint. BMC Musculoskelet Disord 2011;12:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Murray DW, Liddle AD, Dodd CA, Pandit H. Unicompartmental knee arthroplasty: is the glass half full or half empty? Bone Joint J 2015;97-B(Suppl A):3-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Kendrick BJ, Simpson DJ, Kaptein BL, et al. Polyethylene wear of mobile-bearing unicompartmental knee replacement at 20 years. J Bone Joint Surg [Br] 2011;93-B:470-475. [DOI] [PubMed] [Google Scholar]
- 52. Kendrick BJ, Longino D, Pandit H, et al. Polyethylene wear in Oxford unicompartmental knee replacement: a retrieval study of 47 bearings. J Bone Joint Surg [Br] 2010;92-B:367-373. [DOI] [PubMed] [Google Scholar]
- 53. Lustig S, Lording T, Frank F, et al. Progression of medial osteoarthritis and long term results of lateral unicompartmental arthroplasty: 10 to 18 year follow-up of 54 consecutive implants. Knee 2014;21(Suppl 1):S26-S32. [DOI] [PubMed] [Google Scholar]
- 54. Cobb JP. Patient safety after partial and total knee replacement. Lancet 2014;384:1405-1407. [DOI] [PubMed] [Google Scholar]
- 55. Willis-Owen CA, Brust K, Alsop H, Miraldo M, Cobb JP. Unicondylar knee arthroplasty in the UK National Health Service: an analysis of candidacy, outcome and cost efficacy. Knee 2009;16:473-478. [DOI] [PubMed] [Google Scholar]
- 56. Niinimäki T, Eskelinen A, Mäkelä K, et al. Unicompartmental knee arthroplasty survivorship is lower than TKA survivorship: a 27-year Finnish registry study. Clin Orthop Relat Res 2014;472:1496-1501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Rothwell AG, Hooper GJ, Hobbs A, Frampton CM. An analysis of the Oxford hip and knee scores and their relationship to early joint revision in the New Zealand Joint Registry. J Bone Joint Surg [Br] 2010;92-B:413-418. [DOI] [PubMed] [Google Scholar]
- 58. Almaawi AM, Hutt JRB, Masse V, Lavigne M, Vendittoli PA. The impact of mechanical and restricted kinematic alignment on knee anatomy in total knee arthroplasty. J Arthroplasty 2017;32:2133-2140. [DOI] [PubMed] [Google Scholar]