Abstract
Graft size in hamstring autograft anterior cruciate ligament (ACL) surgery is an important factor directly related to failure. Most of the evidence in the field suggests that the size of the graft in hamstring autograft ACL reconstruction matters when the surgeon is trying to avoid failures.
The exact graft diameter needed to avoid failures is not absolutely clear and could depend on other factors, but newer studies suggest than even increases of 0.5 mm up to a graft size of 10 mm are beneficial for the patient. There is still no evidence to recommend the use of grafts > 10 mm.
Several methods – e.g. folding the graft in more strands – that are simple and reproducible have been published lately to address the problem of having an insufficient graft size when performing an ACL reconstruction. Due to the evidence presented, we think it is necessary for the surgeon to have them in his or her arsenal before performing an ACL reconstruction.
There are obviously other factors that should be considered, especially age. Therefore, a larger graft size should not be taken as the only goal in ACL reconstruction.
Cite this article: EFORT Open Rev 2018;3:93-97. DOI: 10.1302/2058-5241.3.170038
Keywords: knee, ACL, graft size, hamstring, re-rupture
Introduction
Anterior cruciate ligament (ACL) ruptures have been estimated to occur in 200 000 persons annually in the United States.1 Most of these patients eventually undergo ACL reconstruction based on continued instability symptoms or desire for future participation in cutting or pivoting sports. There are multiple graft options for ACL reconstruction including bone-patellar tendon-bone (BPTB) autograft, quadriceps tendon autograft, hamstring tendon autograft and several allograft sources.2 Recently, the use of hamstring autograft has increased due to similarly good results as any other graft, while also resulting in decreased donor site morbidity and improved fixation methods.3-6 The most frequently used hamstring graft configuration is a four-strand graft consisting of doubled semitendinosus (ST) and gracilis tendons (G). Biomechanical studies have shown that these grafts have equivalent or superior strength in time when compared with BPTB grafts.7,8 Also, randomized controlled clinical trials have shown no significant differences in clinical outcomes between BPTB and hamstring autografts.9-11 Several authors report the mean graft diameter of four-strand hamstring grafts to be in the range of 7.7 mm to 8.5 mm.7,8,12 However, both clinical experience and MRI evidence show significant variability in hamstring size across the population.11,12 Although difficult to predict accurately, hamstring autograft diameter has been shown to correlate with patient sex, height, body mass index (BMI) and thigh circumference.12-16 Biomechanical studies have demonstrated that the strength of a graft tendon is related to its size and that the smaller the size of the tendon, the greater the likelihood of a weaker and more unstable graft tendon.17
The relationship of graft size with ACL reconstruction failures: early evidence
In 2012, Magnussen et al18 published the first clinical study connecting graft size and revision rates in hamstring autograft ACL surgery. They prospectively collected data from 256 hamstring autograft ACL reconstructions with a mean follow-up of 14 months (6 to 47). All the grafts were prepared as four-strand doubled ST-G grafts. The overall revision ACL surgery of the study was 7%. When they subdivided the number of revisions depending on graft size, they found that in grafts > 8 mm (grafts of ⩾ 8.5 mm in diameter) the rate of revision ACL surgery was 1.7% (1 in 58 patients). On the other hand, when the graft size was 7.5 mm to 8 mm, 9 of 139 patients (6.5%) required a revision ACL surgery, respectively, compared with 8 of 59 patients (13.6%) with grafts of ⩽ 7 mm in diameter. They also evaluated age as a potential risk factor for revision surgery, concluding that age < 20 years had increased rates of revision. Finally, they concluded that the use of hamstring autografts ⩽ 8 mm in diameter in patients aged < 20 years is associated with higher revision rates.
It is not mentioned in the study, but according to how the results were displayed (in 0.5-mm increments between graft sizes), the most probable method they used to measure the grafts was using sizing tubes with 0.5-mm differences in diameter. Also, it is important to note that a misunderstanding of the conclusions could lead to the interpretation that 8 mm is the cut-off point to achieve better or worse revision rates. However, reading it correctly, what the paper really means is that grafts ⩾ 8.5 mm had fewer chances of needing a revision surgery, so the real cut-off point should be 8.5 mm, at least according to this study.
In 2013, Park et al2 reported on 296 patients that underwent hamstring autograft ACL reconstruction and were followed for a minimum of two years. They prepared the grafts as a four-strand doubled ST-G and measured them using a tube-shaped sizing device (Acufex, Smith & Nephew, Norwood, MA, USA) calibrated to 0.5 mm. The study showed a 4% failure rate defined as revision ACL surgery (one patient) or IKDC grade C or D (11 patients). They analysed every 0.5-mm graft size from 5 mm to 9.5 mm. Statistically significant differences were not observed except when patients were classified as < 8.0 mm and as ⩾ 8.0 mm, where a 5.2% failure rate was found for graft diameters < 8 mm compared with 0% in grafts ⩾ 8 mm.
In the same year, Kamien et al19 presented a study of 98 patients that underwent doubled ST-G four-strand autograft ACL reconstruction with at least 24 months of follow-up. Failure was defined as any grade of pivot shift, a 2+ Lachman grade (with no palpable end-point), 5 mm or larger side-to-side differences in KT-1000 arthrometer testing and/or revision surgery. Graft sizing tubes (Smith & Nephew) with 0.5-mm increments were used. They found 15 failures (15.3%) in the study. As in Magnussen et al,18 they found that younger patients, in this case aged < 25 years, had a significantly higher failure rate (12 of 48; 25.0%) compared with patients aged > 25 years (3 of 50; 6.0%) (p = 0.009). They also found out that the level of activity (objectified as Tegner Score) was associated with an increased risk of failure. However, unlike the two previous studies,2,18 when they assessed the failures regarding graft size, they did not find any correlation between the diameter of the graft and failure rates.
At the end of 2013, Mariscalco et al20 presented the results of the MOON cohort regarding graft size influence in patient-reported outcomes and the risk of revision after hamstring autograft ACL reconstruction. They analysed data of 263 patients from two academic medical centres. In this study, four-strand grafts were used in every patient but some of them (number not specified) were quadrupled ST and some doubled ST-G grafts. They did not specify the device used to measure the grafts, but it is understood that they used sizing tubes with 0.5-mm calibration. They found that a 1-mm increase in graft size was noted to correlate with a 3.3-point increase in the KOOS pain subscale (p = 0.003), a 2.0-point increase in the KOOS activities of daily living subscale (p = 0.034), a 5.2-point increase in the KOOS sport/recreation function subscale (p = 0.004) and a 3.4-point increase in the subjective IKDC score (p = 0.026). They had an overall 5.3% revision rate in their study. Of this number, revision was required in 0 of 64 patients (0.0%) when grafts were > 8 mm in diameter and in 14 of 199 patients (7.0%) when grafts were ⩽ 8 mm in diameter (p = 0.037).
Summarizing the evidence available from those first four studies on the topic, Conte et al21 developed a systematic review published in mid-2014. They concluded that there was a strong correlation among the previous studies when a meta-analysis was performed for the group, with a 6.8 times greater relative risk of failure for grafts ⩽ 8 mm in diameter (p = 0.008). It can be concluded that to decrease the risk of having a failure in hamstring ACL reconstruction, a graft of at least 8.5-mm should be used.
The relationship of graft size with ACL reconstruction failures: recent evidence
After the systematic review previously cited, studies on the topic of graft size in hamstring ACL surgery had focused on more specific results, trying to locate a safe zone with a low risk of failure instead of absolute values as the first studies. In 2016, Spragg et al22 published a multicentre, case-control study of 132 revised hamstring ACL reconstructions matched with 396 controls. Graft diameters were measured at 0.5-mm intervals. As the study comes from registry data (Kaiser Permanente ACLR Registry), they do not describe the surgical technique because it varies between centres. In their results, they reported that the likelihood of a patient requiring revision was 0.82 times lower (95% confidence interval (CI) 0.68 to 0.98) for every 0.5-mm increase in the graft diameter from 7.0 to 9.0 mm after primary ACL reconstruction with a hamstring autograft (p = 0.026). They calculated the number needed to treat to harm as 86.64. This number can be interpreted as the following: for approximately every 87 cases with 7-mm grafts instead of 8-mm grafts, one additional revision is yielded. It can be concluded from this study that even when it is not possible to obtain larger grafts, an increase as small as 0.5 mm from a 7-mm diameter could be beneficial for the patient.
The same year, Marchand et al23 reported on the laximetric outcomes (using GNRB® [Genourob, Laval, France] as a measurement tool) of 88 hamstring ACL reconstruction patients operated using a four-strand isolated ST or a doubled ST-G 4-strand graft with an average follow-up of 26 months. The diameter of the central portion of the graft prepared was measured using a calibrator. No graft had a diameter < 8 mm in the study. They did not have any ACL failures and, from their results, it can be concluded that any increase in the diameter of the graft over 8 mm does not improve the laximetric results of an ACL reconstruction. Therefore, harvesting and adding further tissue to increase the diameter of the graft would not be beneficial for the patient.
Schlumberger et al,24 in a recently published study of 2448 cases of four-strand doubled ST-G ACL reconstructions, reported 73 ruptures (3%). When they assessed graft size influence in the re-rupture rate they did not find statistically significant differences between groups (non-rupture versus re-rupture) nor when they compared grafts > 8 mm or < 8 mm. They did not report how grafts were measured in the study. Finally, Snaebjörnsson et al25 published a study on 2240 patients using data from the Swedish National Knee Ligament Registry. A total of 560 were cases (patients who underwent hamstring ACL reconstruction and finally were revised) and 1680 were controls. As Spragg et al22 data came from a registry, they did not describe the surgical technique because it varied between centres. In their results, they reported that a graft diameter between 7.0 mm and 7.5 mm consistently had a higher proportion of cases requiring revision. Contrarily, a graft diameter between 9.0 mm and 10.0 mm consistently had a higher proportion of no revisions. In their cohort, the likelihood of revision for every 0.5-mm increase in the hamstring autograft diameter between 7.0 mm and 10.0 mm was 0.86 (95% CI 0.75 to 0.99; p = 0.03). Accordingly, for every 0.5-mm increment in the graft diameter between 7.0 mm and 10.0 mm, the likelihood of a patient requiring revision surgery after primary ACL reconstruction with a hamstring autograft was 0.86 times lower.
Summary and recommendations from the evidence
After reviewing the evidence available on this topic, several conclusions and recommendations can be made:
The majority of the evidence on the topic suggests that the size of the graft in hamstring autograft ACL reconstruction matters when the surgeon is trying to avoid failures. Of the eight studies available at this point, only two have not found a relationship between smaller grafts and failures.
The exact graft diameter needed to avoid failures is not absolutely clear and could depend on other factors (for example, patient size), but newer studies suggest than even increases of 0.5 mm up to a graft size of 10 mm are beneficial for the patient. There is still no evidence to recommend the use of grafts > 10 mm.
There are obviously other factors that should be considered, especially age18,19,23 (probably the most important risk factor for revision). Therefore, a larger graft size should not be taken as the unique single goal in ACL reconstruction.
Authors’ preferred method to manage patients with an insufficient graft
Several techniques to address an insufficient graft (when the graft size is smaller than would be preferred for the individual patient) have been published in recent years.26-29 Our treatment algorithm consists of converting any hamstring graft prepared as a four-strand doubled ST-G < 8.5 mm to a five-strand ST-G. The preparation technique has been previously published30 and consists of tripling the ST and adding the G on top (Fig. 1). A requirement of the technique is the use of a cortical button as femoral fixation, because the graft is prepared around it, and to have a ST of at least 21 cm in length if the surgeon wants to fix the tibia with intra-tunnel devices (for example, interference screws). In grafts where the ST tendon is < 21 cm, cortical fixation in both ends is possible31 thanks to newly introduced devices, although this event is very infrequent.
Fig. 1.
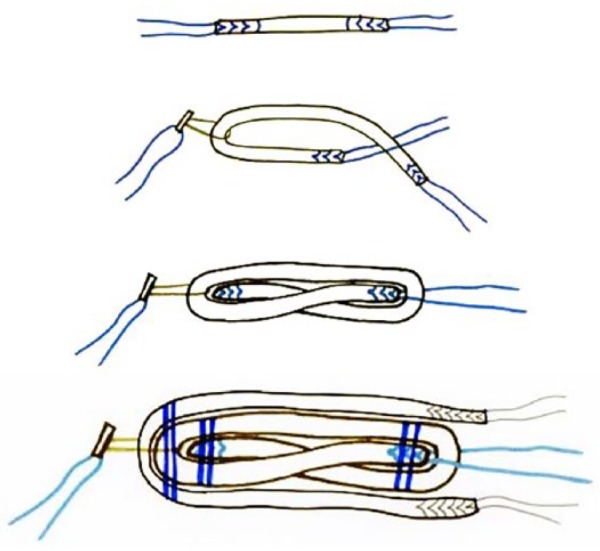
Five-strand graft preparation technique.
Conclusions
Graft size in hamstring autograft ACL surgery is an important factor directly related to failure, but the exact graft size recommended to avoid a risk of failure is still a topic of debate. Several methods that are simple and reproducible have been published lately to address this potential event when performing an ACL reconstruction. Due to the evidence presented, we think it is relevant for the surgeon to have them in his or her arsenal before performing an ACL reconstruction.
Footnotes
ICMJE Conflict of interest statement: D. Figueroa declares board membership of SLARD; consultancy, payment for lectures, and payment for development of educational presentations for Stryker, activities outside the submitted work.
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- 1. Hewett TE, Schultz SJ, Griffin LY, eds. Understanding and preventing noncontact ACL injuries. Champaign, IL: Human Kinetics; 2007. [Google Scholar]
- 2. Park SY, Oh H, Park S, et al. Factors predicting hamstring tendon autograft diameters and resulting failure rates after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 2013;21:1111-8. [DOI] [PubMed] [Google Scholar]
- 3. Ejerhed L, Kartus J, Sernert N, Köhler K, Karlsson J. Patellar tendon or semitendinosus tendon autografts for anterior cruciate ligament reconstruction? A prospective randomized study with a two-year follow-up. Am J Sports Med 2003;31:19-25. [DOI] [PubMed] [Google Scholar]
- 4. Feller JA, Webster KE. A randomized comparison of patellar tendon and hamstring tendon anterior cruciate ligament reconstruction. Am J Sports Med 2003;31:564-73. [DOI] [PubMed] [Google Scholar]
- 5. Freedman KB, D’Amato MJ, Nedeff DD, Kaz A, Bach BR., Jr Arthroscopic anterior cruciate ligament reconstruction: a metaanalysis comparing patellar tendon and hamstring tendon autografts. Am J Sports Med 2003;31:2-11. [DOI] [PubMed] [Google Scholar]
- 6. Laxdal G, Kartus J, Hansson L, et al. A prospective randomized comparison of bone-patellar tendon-bone and hamstring grafts for anterior cruciate ligament reconstruction. Arthroscopy 2005;21:34-42. [DOI] [PubMed] [Google Scholar]
- 7. Hamner DL, Brown CH, Jr, Steiner ME, Hecker AT, Hayes WC. Hamstring tendon grafts for reconstruction of the anterior cruciate ligament: biomechanical evaluation of the use of multiple strands and tensioning techniques. J Bone Joint Surg Am 1999;81:549-57. [DOI] [PubMed] [Google Scholar]
- 8. Wilson TW, Zafuta MP, Zobitz M. A biomechanical analysis of matched bone-patellar tendon-bone and double-looped semitendinosus and gracilis tendon grafts. Am J Sports Med 1999;27:202-7. [DOI] [PubMed] [Google Scholar]
- 9. Maletis GB, Cameron SL, Tengan JJ, Burchette RJ. A prospective randomized study of anterior cruciate ligament reconstruction: a comparison of patellar tendon and quadruple-strand semitendinosus/gracilis tendons fixed with bioabsorbable interference screws. Am J Sports Med 2007;35:384-94. [DOI] [PubMed] [Google Scholar]
- 10. Sajovic M, Vengust V, Komadina R, Tavcar R, Skaza K. A prospective, randomized comparison of semitendinosus and gracilis tendon versus patellar tendon autografts for anterior cruciate ligament reconstruction: five-year follow-up. Am J Sports Med 2006;34:1933-40. [DOI] [PubMed] [Google Scholar]
- 11. Samuelsson K, Andersson D, Karlsson J. Treatment of anterior cruciate ligament injuries with special reference to graft type and surgical technique: an assessment of randomized controlled trials. Arthroscopy 2009;25:1139-74. [DOI] [PubMed] [Google Scholar]
- 12. Tuman JM, Diduch DR, Rubino LJ, et al. Predictors for hamstring graft diameter in anterior cruciate ligament reconstruction. Am J Sports Med 2007;35:1945-9. [DOI] [PubMed] [Google Scholar]
- 13. Calvo R, Melean P, Figueroa D, et al. Does patient weight and height correlate with the length and diameter of the semitendinosus graft? Rev Esp Cir Ortop Traumatol 2011;55:2-8. [Google Scholar]
- 14. Ma CB, Keifa E, Dunn W, Fu FH, Harner CD. Can pre-operative measures predict quadruple hamstring graft diameter? Knee 2010;17:81-3. [DOI] [PubMed] [Google Scholar]
- 15. Schwartzberg R, Burkhart B, Lariviere C. Prediction of hamstring tendon autograft diameter and length for anterior cruciate ligament reconstruction. Am J Orthop (Belle Mead NJ) 2008;37:157-9. [PubMed] [Google Scholar]
- 16. Treme G, Diduch DR, Billante MJ, Miller MD, Hart JM. Hamstring graft size prediction: a prospective clinical evaluation. Am J Sports Med 2008;36:2204-9. [DOI] [PubMed] [Google Scholar]
- 17. Pagnani MJ, Warner JJ, O’Brien SJ, Warren RF. Anatomic considerations in harvesting the semitendinosus and gracilis tendons and a technique of harvest. Am J Sports Med 1993;21:565-71. [DOI] [PubMed] [Google Scholar]
- 18. Magnussen RA, Lawrence JT, West RL, et al. Graft size and patient age are predictors of early revision after anterior cruciate ligament reconstruction with hamstring autograft. Arthroscopy 2012;28:526-31. [DOI] [PubMed] [Google Scholar]
- 19. Kamien PM, Hydrick JM, Replogle WH, Go LT, Barrett GR. Age, graft size, and Tegner activity level as predictors of failure in anterior cruciate ligament reconstruction with hamstring autograft. Am J Sports Med. 2013;41:1808-12. [DOI] [PubMed] [Google Scholar]
- 20. Mariscalco MW, Flanigan DC, Mitchell J, et al. The influence of hamstring autograft size on patient-reported outcomes and risk of revision after anterior cruciate ligament reconstruction: a Multicenter Orthopaedic Outcomes Network (MOON) Cohort Study. Arthroscopy 2013;29:1948-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Conte EJ, Hyatt AE, Gatt CJ, Jr, Dhawan A. Hamstring autograft size can be predicted and is a potential risk factor for anterior cruciate ligament reconstruction failure. Arthroscopy 2014;30:882-90. [DOI] [PubMed] [Google Scholar]
- 22. Spragg L, Chen J, Mirzayan R, Love R, Maletis G. The effect of autologous hamstring graft diameter on the likelihood for revision of anterior cruciate ligament reconstruction. Am J Sports Med 2016;44:1475-81. [DOI] [PubMed] [Google Scholar]
- 23. Marchand JB, Ruiz N, Coupry A, Bowen M, Robert H. Do graft diameter or patient age influence the results of ACL reconstruction? Knee Surg Sports Traumatol Arthrosc 2016;24:2998-3004. [DOI] [PubMed] [Google Scholar]
- 24. Schlumberger M, Schuster P, Schulz M, et al. Traumatic graft rupture after primary and revision anterior cruciate ligament reconstruction: retrospective analysis of incidence and risk factors in 2915 cases. Knee Surg Sports Traumatol Arthrosc 2017;25(5):1535-41. [DOI] [PubMed] [Google Scholar]
- 25. Snaebjörnsson T, Hamrin Senorski E, Ayeni OR, et al. Graft diameter as a predictor for revision anterior cruciate ligament reconstruction and KOOS and EQ-5D values: a cohort study from the Swedish National Knee Ligament Register based on 2240 patients. Am J Sports Med 2017;45:2092-7. [DOI] [PubMed] [Google Scholar]
- 26. Lavery KP, Rasmussen JF, Dhawan A. Five-strand hamstring autograft for anterior cruciate ligament reconstruction. Arthrosc Tech 2014;3:e423-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Lee RJ, Ganley TJ. The 5-strand hamstring graft in anterior cruciate ligament reconstruction. Arthrosc Tech 2014;3:e627-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Burrus MT, Werner BC, Crow AJ, et al. Increased failure rates after anterior cruciate ligament reconstruction with soft-tissue autograft-allograft hybrid grafts. Arthroscopy 2015;31:2342-51. [DOI] [PubMed] [Google Scholar]
- 29. Darnley JE, Léger-St-Jean B, Pedroza AD, et al. Anterior cruciate ligament reconstruction using a combination of autograft and allograft tendon: a MOON cohort study. Orthop J Sports Med 2016;4:2325967116662249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Calvo R, Figueroa D, Figueroa F, et al. Five-strand hamstring autograft versus quadruple hamstring autograft with graft diameters 8.0 millimeters or more in anterior cruciate ligament reconstruction: clinical outcomes with a minimum 2-year follow-up. Arthroscopy 2017;33:1007-13. [DOI] [PubMed] [Google Scholar]
- 31. Fritsch B, Figueroa F, Semay B. Graft preparation technique to optimize hamstring graft diameter for anterior cruciate ligament reconstruction. Arthrosc Tech 2017;6:e2169-75. [DOI] [PMC free article] [PubMed] [Google Scholar]


