Abstract
[Purpose] To investigate the effect of heel height on the distribution of plantar foot force and heel pain in patients with a heel spur. [Subjects and Methods] Plantar force was measured using 8 force sensors in 16 patients (3 men, 13 women), with symptomatic heel spur for 4 heel heights (0–4 cm). Sensors were located at the hallux (T1); medial to lateral metatarsals (M1 through M3), mid-foot (MF); and at the central, lateral, and medial heel (CH, LH, and MH). Pain was evaluated using the minimum compression force that caused pain and was measured using an algometer. [Results] Load bearing shifted from the heel (CH) to the mid-foot (MF) and hallux (T1) with increasing heel height. Raising the heel from 2 to 3 cm reduced the magnitude of load bearing, relative to the minimum compression force for pain, by 3.70% at the LH and 2.35% at the MH. Excellent clinical outcomes, defined by a 70–100% decrease in pain, were achieved in 10/16 participants with the use of a 2-cm and 3-cm heel height in men and women, respectively. [Conclusion] Increasing heel height effectively decreases the plantar force on the heel during weight-bearing activities.
Key words: Calcaneal spur, Heel height shoe, Algometer
INTRODUCTION
Heel pain is a problem frequently seen in orthopedic practice, and treatment is mostly disappointing. Clinically, pain is the chief presenting complaint that causes difficulty in weight-bearing functions, such as walking and standing, thereby restricting work and sport activities1, 2). Treatment for this syndrome is usually conservative and is directed toward decreasing the pain via a nonsteroidal anti-inflammatory drug and a reduction in activity level3). Several studies have attempted to decrease pain in the heel compared to this type of conservative treatment using extracorporeal shock wave4) or pulsed radio frequency energy5) as well as conservative treatment in combination with extracorporeal shockwave therapy6, 7) or with contrast baths, stretching exercises, or wearing low-heeled shoes8). During treatment, the level of pain in each patient was determined using a telephone survey3) or by manual palpation1).
The pain felt by the calcanea spur patients is due to considerable load in the heel area during weight-bearing activities2, 9). This high loading commonly leads to the development of calcaneal (heel) spurs and pain10). Orthotics is generally prescribed to manage the pain associated with heel spurs, to reduce load bearing on the heel by increasing the height of the shoe11,12,13,14,15). Goske et al.16) noted that high conformity of the orthotic to the heel was essential to increasing the contact surface between the heel and the orthotic. This could then reduce the magnitude of the weight-bearing load on the heel. Thicker and softer orthotics further decreased the calcaneal loads, although the effect of the material used was not as important as the appropriate sizing and thickness of the orthotic.
We add to the results of these previous studies by measuring the pressure pain threshold (PPT) in the heels of patients experiencing plantar heel pain syndrome. The pain level was measured using a pressure algometer, which indicates the PPT in a quantitative manner17), as described in Saban et al18). In that study, the researchers divided the heel region into 5 sites and pressed each site using an algometer probe. However, the exact location of pain suppression was not specified.
In the study presented herein, we assessed 7 pain suppression points that were set around the site of the spur growth. In doing so, we sought to systematically evaluate the effects of increasing the heel height of a shoe on the distribution of forces on the heel during standing and the subsequent pain among patients with a symptomatic heel spur. A priori, we hypothesized that increasing the height of the shoe would decrease the peak compressive forces that were exerted on the heel during standing.
SUBJECTS AND METHODS
Sixteen patients with symptomatic heel spurs were recruited from the RSUD (local public hospital) Tugurejo in Semarang. Volunteers were healthy, without notable asymmetries on lower limbs alignment and without history of orthopedic trauma based on the check up by an orthopedic specialist. The patient characteristics are shown in Table 1. The study was approved by the institutional review board and all patients provided informed consent. Reporting was in accordance with the proposed guidelines for the reporting of reliability and agreement studies (GRRAS)19).
Table 1. Subject characteristics.
| Parameter | Range of Value | Mean and SD |
|---|---|---|
| Age (years) | 27–73 | 55 ± 12 |
| Gender (male:female) | 3:13 | |
| Weight (kg) | 49–84.6 | 61.9 ± 9.5 |
| Height (cm) | 144–172 | 155 ± 7 |
| Body Mass Index (BMI) (kg/m2) | 19.1–33.5 | 25.6 ± 3.7 |
Each patient was asked to perform loaded and unloaded scanning of the foot. Loaded scanning of the foot using a digital footprint was used to determine foot width (FW) and foot length (FL). The footprint image was then used to map the location of pain suppression points around the spur growth. FL is the direct distance from the pterion point to the most anterior point of the longest toe (first or second) and is measured parallel to the foot axis. FW is the horizontal distance between the tibial metatarsal to the fibular metatarsal20). The digital footprint was generated using a modified flatbed document scanner and was designed to scan one foot at a time. The scanning process occurs when the research subject is standing in an upright posture above the platform, as shown in Fig. 1a. To obtain the footprint image, the portions of the foot that are not in direct contact with the platform (Fig. 1b) are removed using MATLAB, which results in the final image as shown in Fig. 1c. The FW and FL are calculated using MATLAB as the difference between the nearest and furthest points at the x and y coordinates, respectively, where x represents the horizontal coordinates and y represents the vertical coordinates.
Fig. 1.
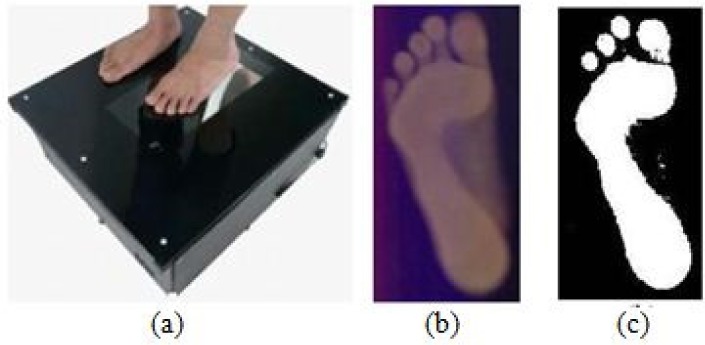
Loaded scanning of a foot using a digital footprint.
The location of the bone spur was obtained from standing plain radiographs, where S is the distance between the back of the heel and the base of the spur and L is the length of the spur (Fig. 2a). By mapping the results of this radiograph on the footprint image (Fig. 1c), the location and dimensions of the bone spur can be seen in plantar view. The 7 points used for pain assessment could then be localized, with point 7 being placed at the base of the spur. The remaining 6 points were distributed along the circumference of a circle, with the base of the spur at its center, and the radius of the circle being equal to the length of the spur plus 1 cm (Fig. 2b). In all cases, the base of the spur was assumed to be in the heel center line, which was a line drawn from the center of the heel to the tip of the second toe (Fig. 2c)21).
Fig. 2.
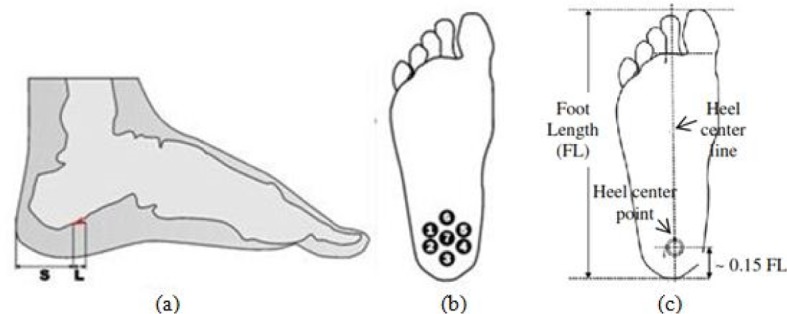
Determination of the 7 points location of pain test.
The heel center point was placed at 0.15 of the FL from the back of the heel, as described by Rodrigo et al.22)
To measure PPT, the patient lays supine in a relaxed position, and the measurements were performed using a mechanical pressure algometer (FDIX 25, Wagner Instruments, Greenwich, CT, USA), as shown in Fig. 3a. This device consists of a flat rubber tip probe of 1 cm in diameter, which is applied perpendicular to the skin. The voltage signal is transduced and amplified and the output is displayed in Newtons or kilograms. The pain test is conducted as follows: 1) mark the 7 pressure points in the heel area to be assessed (Fig 2b); 2) press the skin at point 7 first; 3) increase the pressure gradually and stop until the patient’s face expression looks like a level 6 or 7, as shown in Fig. 3b23); 4) take a note of the force value that causes pain; 5) apply the same procedure to the remaining points 1–6. Suppression at the end of the spur (around point 6) should produce a minimum compressive force since it is identical to the cantilever construction. Using the pain test results at those 7 points, it is possible to reveal the pain minimum compressive force and the point location in each patient.
Fig. 3.
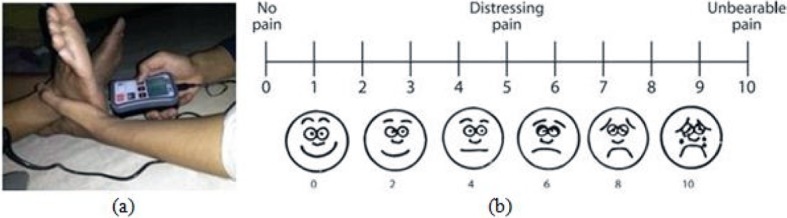
Pain test and the patient’s facial expression to pain.
The distribution of plantar forces, between the foot and the shoe was measured using an 8-sensor array (402 FSR, Interlink Electronics, Camarillo, CA, USA). Determination of the location of each sensor was performed using an unloaded foot scan that was produced using a 3D foot scanner (ScanPod 3D, Vismach Technology Ltd., Hong Kong, China). In particular, we scanned around the area with the greater z-value coordinates, as shown in the red color image (Fig. 4a). Sensors were positioned at the following 8 locations: T1, hallux (sensor 1); M1, metatarsal 1 (sensor 2); M2, metatarsal 2 (sensor 3); M3, metatarsal 3 (sensor 4); MF, midfoot (sensor 5); LH, lateral heel (sensor 6); CH, center of heel (sensor 7); and MH, medial heel (sensor 8), as shown in Fig. 4b. Sensor 7 was always placed at the center of heel, which estimated to be located at 0.15 x FL (Fig. 2c)22). The standardized position of the 8 sensors was embedded in a fabricated orthotic to measure the plantar force between the foot and the shoe (Fig. 4c). For analysis, only the force recorded in the greater z-value of the sensors positioned at the center, medial, and lateral heel was used (3 of the 8 sensors of the array).
Fig. 4.
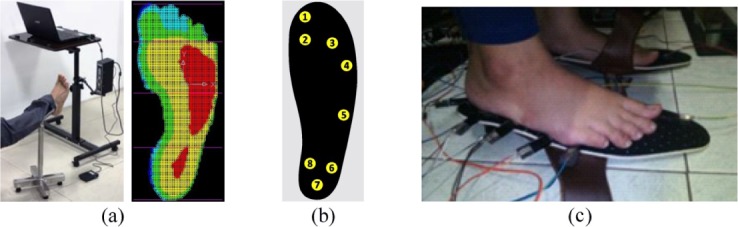
Determination of the 8 points location of the plantar forces distribution measurement.
Each participant was fitted with an appropriate shoe size, with custom heel heights of 0 cm, 2 cm, 3 cm, and 4 cm (Fig. 5a). To provide foot stability and comfort in the shoe, a custom insole, without contour (flat) or arch support was included. The outer covering was made of Microcel Puff EVA foam (7 mm), with the inner cushion made of Poron cushioning (3 mm)16) (Fig. 5b). Heel wedges of different heights could be inserted into the shoes. Starting with a heel height of 0 cm, the load on the soles of the patient’s feet was measured using FSR sensors. If the peak load in the heel area F was still greater than the minimum pain force F* or F>F *, patient was asked to use a shoe with a higher heel. The peak load in the heel area was measured again. This process repeated until F≤F *. All measurements for each heel height shoe are performed when patient is standing in an upright posture guided by the operator
Fig. 5.
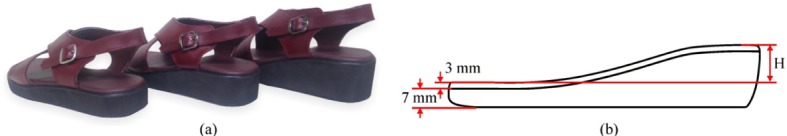
Test shoes with 3 heel heights variation (2 cm, 3 cm, and 4 cm).
RESULTS
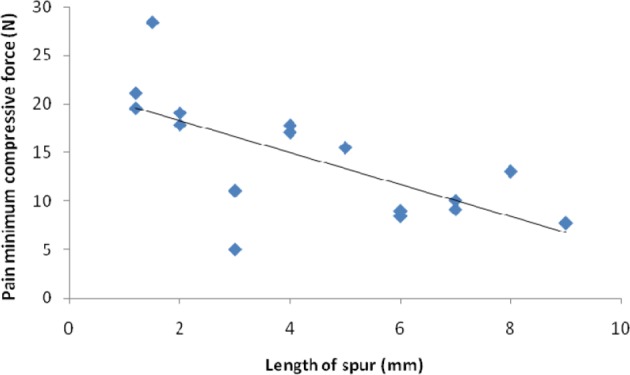
Among the 16 patients in our study group, 7 had symptomatic bilateral heel spurs. Since compressive pain was measured bilaterally in these patients, a total of 23 feet were evaluated. The length of the heel spur ranged between 1.2 and 9 mm. The compressive pain force ranged between 5.04 and 28.40 N. We observed a linear relationship (correlation coefficient: 0.68) between the length of the spur and the minimum compression force for pain, as shown in Fig. 6. According to the BMI classification from WHO24), there was a relationship between BMI classification and the minimum compression force for pain (i.e., as BMI increased, the minimum compression force for pain decreased). In the normal weight group (BMI between 18.5–24.9 kg/m2), the average minimum compression force for pain was 18.07 ± 5.75 N. In the overweight group (BMI between 25.0–29.9 kg/m2), the average minimum compression force for pain was 12.02 ± 4.57 N. In the obese group (BMI ≥30 kg/m2), the average minimum compression force for pain was 8.42 ± 3.08 N.
Fig. 6.
The relationship between length of the spur and pain minimum compressive force.
The minimum compression force for pain, at each reference point around the heel spur, was as follows: point 1, pain in 11 feet (7.03–28.4 N); point 2, pain in 2 feet (13.06–17.85 N); point 3, pain in 1 foot (9.0 N); point 4, no cases identified; point 5, pain in 1 foot (8.45 N); point 6, pain in 7 feet (5.04–25.10 N); and point 7, pain in 1 foot (17.8 N). When considering the smallest pain force in the patients with bilateral heel spurs, we found that the average minimum compressive force for pain was 14.37 ± 6.20 N.
The distribution of load bearing on the plantar surface of the foot, expressed as a proportion of body weight (z-force/BW, %), is reported in Table 2 for the different heel heights. As heel height increased, peak force shifted away from the heel to the mid-foot (MF) and fore-foot. Loading on the MF increased as a function of increasing heel height, from 1.06% at the baseline (0 cm) heel height to 10.01% for the 2-cm height, 10.68% for the 3-cm height, and 11.43% for the 4-cm height. The hallux (T1) supported the highest proportion of load bearing, with peak magnitudes sustained with a heel height of 4 cm. In comparison, the proportion of load bearing was lowest on the medial forefoot (M1) for all heel heights in comparison to all other regions of the foot, and this for all heel heights from baseline. The load bearing on the metatarsal region (M2) increased from 0.95% (0 cm) to a peak magnitude of 9.45% (3 cm), while load bearing on the M3 region increased from 2.45% (0 cm) to a peak magnitude of 6.10% (2 cm), decreasing to below the baseline magnitude with heel heights of 3 and 4 cm (0.77% and 0.87%, respectively). With regard to load bearing specifically on the heel, the proportion of load bearing increased generally as a function of heel height on the medial (MH) and lateral (LH) heel, compared to baseline (0 cm), with the peak magnitudes sustained on the LH and MH with the 4-cm heel height. For the central heel (CH), the peak load bearing was at baseline (0 cm), with a marked decrease with increasing heel height, from 14.32% (0 cm) to 1.36% (2 cm), 0.91% (3 cm), and 0.89% (4 cm). The distribution of loading on the MH, LH, and CH for the 4 heel heights is summarized in Fig. 7. The force applied at the CH was lower than the minimum pain force (F*) with increasing heel height from 0 cm, while the magnitude of force on the LH was comparable to F* at heel heights of 2 cm (5.45% of F*) and 3 cm (1.75% of F*). Load bearing magnitudes were significantly greater than F* on the MH, at 2 cm (33.65% of F*) and 3 cm (31.30% of F*). The magnitude of force both on the LH and MH were significantly increased with a heel height of 4 cm.
Table 2. Average of load/BW (%) for each region of the foot.
| Region (Sensor) | 0-cm heel | 2-cm heel | 3-cm heel | 4-cm heel |
|---|---|---|---|---|
| T1 (1) | 1.02 ± 0.14 | 11.47 ± 0.23 | 13.19 ± 0.13 | 15.74 ± 0.14 |
| M1 (2) | 1.05 ± 0.13 | 1.11 ± 0.09 | 0.97 ± 0.02 | 1.53 ± 0.02 |
| M2 (3) | 0.95 ± 0.03 | 7.39 ± 0.59 | 9.45 ± 0.44 | 8.45 ± 0.32 |
| M3 (4) | 2.45 ± 0.02 | 6.10 ± 0.55 | 0.77 ± 0.04 | 0.87 ± 0.01 |
| MF (5) | 1.06 ± 0.12 | 10.01 ± 0.42 | 10.68 ± 0.51 | 11.43 ± 0.83 |
| LH (6) | 1.23 ± 0.04 | 8.66 ± 0.17 | 6.87 ± 0.22 | 10.13 ± 0.42 |
| CH (7) | 14.32 ± 0.21 | 1.36 ± 0.11 | 0.91 ± 0.04 | 0.89 ± 0.01 |
| MH (8) | 11.45 ± 0.92 | 11.55 ± 0.47 | 9.84 ± 0.17 | 13.79 ± 0.07 |
Values are express as the mean ± standard deviation of the proportion of body weight.
Fig. 7.
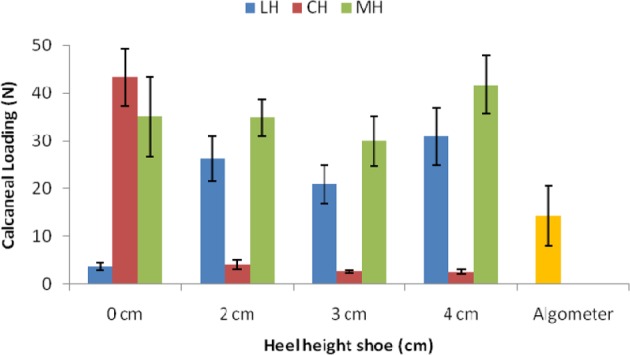
Calcaneal loading during standing for the 4 heel heights, compared to the minimum compressive force for pain measured using the algometer (mean ± SD).
The reference measurements of the foot for the location of the sensor at CH are summarized in Table 3, including the difference between the center point of the heel (used for force measurement) and the base of the spur (used for pain measurement). For some participants, this difference was negative, thereby indicating that the CH sensor was posterior to the base of the spur. The greater distance difference was seen in patients no. 3 and no. 15 (i.e. 5.9 and 6.9 mm, respectively). However, the average difference between the center point of the heel and the base of the spur in these cases was small (1.17 ± 2.79 mm) or −1.6 to 3.9 mm. Overall, the sensor was localized close to the base of the heel spur (−1.5 to 2.3 mm), except for 2 cases with a difference of 5.9 and 6.9 mm.
Table 3. The difference between the center of the heel and the base of the heel spur.
| Subject number | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| FL (mm) | 249 | 242 | 266 | 237 | 254 | 240 | 252 | 249 | 276 | 237 | 251 | 240 | 240 | 270 | 273 | 234 |
| FW (mm) | 98 | 118 | 118 | 106 | 108 | 91 | 100 | 101 | 108 | 96 | 102 | 94 | 100 | 100 | 99 | 90 |
| Shoe size | 40 | 39 | 42 | 38 | 38 | 38 | 40 | 40 | 43 | 38 | 40 | 38 | 39 | 40 | 42 | 37 |
| Spur length (mm) | 5.0 | 1.5 | 9.0 | 1.2 | 1.2 | 4.0 | 6.0 | 2.0 | 2.0 | 4.0 | 6.0 | 8.0 | 4.0 | 2.0 | 3.0 | 7.0 |
| Distance difference (mm) | −0.6 | 1.3 | 5.9 | 1.6 | 1.1 | −2 | −1.2 | 0.4 | 0.4 | 0.6 | −1.3 | 6 | −2 | 1.5 | 6.9 | 0.1 |
DISCUSSION
The highest number of pain points were identified at points 1 and 6, just anterior and anterolateral to the heel spur. This is consistent with our original assumption that pressure applied to the end of the spur would be associated with the greatest magnitude of pain. The average minimum compression force for pain at points 5 and 6 (i.e., 8.5 N and 14.5 N, respectively), were lower than at points 1 and 2 (i.e., 16.5 N and 15.5 N, respectively). This result is in accordance with the study of Saban et al.18), except at point 7 in the base of the spur, which noted that the minimum compressive force for pain at sites medially posterior, medially anterior, and center, were significantly lower than at sites laterally anterior and laterally posterior. He concludes that this is due to the aggregation of anatomic structure at this location, particularly the nervous tissues. The patients that Saban et al. recruited experienced plantar heel pain syndrome and were not specifically mentioned due to the presence of a calcaneal spur and since the exact location of pain suppression points 1–5 were not specified. In this study, in reference to the spur, point 7 was placed at the base, point 6 was placed at the end, points 1 and 2 were placed laterally anterior and laterally posterior, and points 4 and 5 were placed medially posterior and medially anterior. Based on the placement of the 7 points for pain assessment, it is reasonable if the minimum compression force for pain at point 7 is higher than at the other points.
The relationship between BMI and the minimum compression force for pain indicated that patients with excessive body weight experience more pain25). Meanwhile, the relationship between the length of the spur and the minimum compression force for pain shows that the compression force for pain is lower when the length of spur is higher. This agrees with the research of Ozdemir et al.8) and Rome et al26). Ozdemir et al. noted that, as spur size increased, the heel pad compressibility index (HPCI) value increased, while Rome et al. demonstrated that heel pad thickness and HPCI were all significantly greater in patients with plantar heel pain than in normal subjects.
Our measurement of the distribution and magnitudes of forces on the plantar surface of the foot provides additional insights into the forces at the foot-shoe interface. With increasing heel height, we identified a redistribution of plantar force, both in terms of magnitude and location, with increasing load bearing on the mid-foot region. Therefore, the increase in the downward slope of the foot with higher heel height shifts load bearing from the heel to the mid- and fore-foot regions15). This redistribution is characterized by a shift in the proportion of load bearing from CH to M2, which is indicative of increased pronation of the fore-foot with increasing heel height13), with an increase in peak plantar force under the hallux (T1 region) with the 4-cm heel height. These findings agree with those previously reported by Kim et al.14) and Hessert et al27). Compared to flat shoes, Speksnijder et al. reported an increase of 27% in the plantar force on the medial fore-foot at M1, 13% in the central fore-foot (M2), and 27% at the hallux (T1) with high-heeled shoes, with the same redistribution identified during walking, although the peak magnitudes of force were greater28). Increasing heel height also forces the fore-foot into pronation, with a decrease in rear-foot pronation11), which we found resulted in an 89% increase in the proportion of load bearing on the MH, relative to the LH, in comparison to the baseline (0 cm) heel height.
Our comparison of average calcaneal loading to the average pain minimum compressive force indicated a decrease in load bearing on the CH with a 2-cm heel height which is smaller than the average pain minimum compressive force, but without decrease in load bearing on the LH and MH. Therefore, there is still a potential for heel pain. However, raising the heel height from 2 to 3 cm reduced the proportion of load bearing on the LH by 3.70% and on the MH by 2.35% in comparison to the minimum compressive force for pain.
The average difference between the location of the heel center point and the location of the base of the spur was 1.17 mm. Therefore, the position of the CH sensory was relatively accurate since, at the very least, the edge of the sensor was able to compress the spur. This allowed us to compare the peak load applied to the minimum compression force for pain.
We found that the use of a 2-cm heel height for men and 3-cm heel height for women was sufficient to decrease calcaneal pain and improve comfort during standing and walking. Participants wore their custom shoes from early August to the end of September 2016, for ≥4 h/day over a duration of 8 weeks29). Without the use of local anesthetic, the following clinical outcomes were obtained: a decrease in pain from 100% to 70% in 10 individuals (excellent clinical outcome); decrease from 70% to 30% in 3 individuals (very good outcome); and a decrease of <30% (satisfactory outcome) in 3 individuals. None of the participants reported an increase in pain or unsatisfactory results. Therefore, increasing heel height provides an effective strategy to decrease the plantar force on the heel during weight-bearing activities.
Acknowledgments
This work was supported by an Application and Development Research Grant from the UNDIP (2015) Contract No. DIPA: 023.04.2.1898.152013 and (2016) Contract No. SP DIPA: 042.01.2.400898/2016.
REFERENCES
- 1.Alshami AM, Souvlis T, Coppieters MW: A review of plantar heel pain of neural origin: differential diagnosis and management. Man Ther, 2008, 13: 103–111. [DOI] [PubMed] [Google Scholar]
- 2.Giddings VL, Beaupré GS, Whalen RT, et al. : Calcaneal loading during walking and running. Med Sci Sports Exerc, 2000, 32: 627–634. [DOI] [PubMed] [Google Scholar]
- 3.Wolgin M, Cook C, Graham C, et al. : Conservative treatment of plantar heel pain: long-term follow-up. Foot Ankle Int, 1994, 15: 97–102. [DOI] [PubMed] [Google Scholar]
- 4.Rompe JD, Hopf C, Nafe B, et al. : Low-energy extracorporeal shock wave therapy for painful heel: a prospective controlled single-blind study. Arch Orthop Trauma Surg, 1996, 115: 75–79. [DOI] [PubMed] [Google Scholar]
- 5.Michel R: Treatment of chronic plantar fasciitis with pulsed radio frequency energy therapy. Foot, 2009, 19: 239–241. [DOI] [PubMed] [Google Scholar]
- 6.Buch M, Knorr U, Fleming L, et al. : [Extracorporeal shockwave therapy in symptomatic heel spurs. An overview]. Orthopade, 2002, 31: 637–644 (in German). [DOI] [PubMed] [Google Scholar]
- 7.Lee GP, Ogden JA, Cross GL: Effect of extracorporeal shock waves on calcaneal bone spurs. Foot Ankle Int, 2003, 24: 927–930. [DOI] [PubMed] [Google Scholar]
- 8.Ozdemir H, Söyüncü Y, Ozgörgen M, et al. : Effects of changes in heel fat pad thickness and elasticity on heel pain. J Am Podiatr Med Assoc, 2004, 94: 47–52. [DOI] [PubMed] [Google Scholar]
- 9.Chia KK, Suresh S, Kuah A, et al. : Comparative trial of the foot pressure patterns between corrective orthotics,formthotics, bone spur pads and flat insoles in patients with chronic plantar fasciitis. Ann Acad Med Singapore, 2009, 38: 869–875. [PubMed] [Google Scholar]
- 10.Thomas JL, Christensen JC, Kravitz SR, et al. American College of Foot and Ankle Surgeons Heel Pain Committee: The diagnosis and treatment of heel pain: a clinical practice guideline-revision 2010. J Foot Ankle Surg, 2010, 49: S1–S19. [DOI] [PubMed] [Google Scholar]
- 11.Shimizu M, Andrew PD: Effect of heel height on the foot in unilateral standing. J Phys Ther Sci, 1999, 11: 95–100. [Google Scholar]
- 12.Xiaohong J, Rencheng W, Lee W: Effects of shoe heel height on loading and muscle activity for trans-tibial amputees during standing. Tsinghua Sci Technol, 2009, 14: 281–286. [Google Scholar]
- 13.Cong Y, Cheung JT, Leung AK, et al. : Effect of heel height on in-shoe localized triaxial stresses. J Biomech, 2011, 44: 2267–2272. [DOI] [PubMed] [Google Scholar]
- 14.Kim JS, Fell DW, Cha YJ, et al. : Effects of different heel heights on plantar foot pressure distribution of older women during walking. J Phys Ther Sci, 2012, 24: 1091–1094. [Google Scholar]
- 15.Petrofsky J, Khowailed IA, Burtnett BN, et al. : Balance and pressure distribution under the foot during standing and walking with no orthotics compared to custom and off the shelf orthotics, a pilot study. Clin Res Foot Ankle, 2014, 3: 161. [Google Scholar]
- 16.Goske S, Erdemir A, Petre M, et al. : Reduction of plantar heel pressures: insole design using finite element analysis. J Biomech, 2006, 39: 2363–2370. [DOI] [PubMed] [Google Scholar]
- 17.Geber C, Klein T, Azad S, et al. : Test-retest and interobserver reliability of quantitative sensory testing according to the protocol of the German Research Network on Neuropathic Pain (DFNS): a multi-centre study. Pain, 2011, 152: 548–556. [DOI] [PubMed] [Google Scholar]
- 18.Saban B, Masharawi Y: Pain threshold tests in patients with heel pain syndrome. Foot Ankle Int, 2016, 37: 730–736. [DOI] [PubMed] [Google Scholar]
- 19.Kottner J, Audigé L, Brorson S, et al. : Guidelines for Reporting Reliability and Agreement Studies (GRRAS) were proposed. J Clin Epidemiol, 2011, 64: 96–106. [DOI] [PubMed] [Google Scholar]
- 20.Lee YC, Lin G, Wang MJ: Comparing 3D foot scanning with conventional measurement methods. J Foot Ankle Res, 2014, 7: 44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cavanagh PR, Rodgers MM: The arch index: a useful measure from footprints. J Biomech, 1987, 20: 547–551. [DOI] [PubMed] [Google Scholar]
- 22.Rodrigo AS, Goonetilleke RS, Xiong S: Load distribution to minimise pressure-related pain on foot: a model. Ergonomics, 2013, 56: 1180–1193. [DOI] [PubMed] [Google Scholar]
- 23.Holy Redeemer. Pain Level Chart. http://www.holyredeemer.com/Uploads/Public/Documents/2011%20Pain%20 Level%20Chart.pdf (Accessed Apr. 23, 2017)
- 24.World Health Organization: Obesity: preventing and managing the global epidemic. Geneva 2000. World Health Organ Tech Rep Ser, 894. [PubMed] [Google Scholar]
- 25.Hill J, Cutting PJ: Heel pain and body weight. Foot Ankle Int, 1989, 9: 254–255. [DOI] [PubMed] [Google Scholar]
- 26.Rome K, Campbell R, Flint A, et al. : Heel pad thickness—a contributing factor associated with plantar heel pain in young adults. Foot Ankle Int, 2002, 23: 142–147. [DOI] [PubMed] [Google Scholar]
- 27.Hessert MJ, Vyas M, Leach J, et al. : Foot pressure distribution during walking in young and old adults. BMC Geriatr, 2005, 5: 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Speksnijder CM, Munckhof RJH, Moonen SAFCM, et al.: The higher the heel the higher the forefoot-pressure in ten healthy women. Foot, 2005, 15: 17–21. [Google Scholar]
- 29.Chen TH, Chou LW, Tsai MW, et al. : Effectiveness of a heel cup with an arch support insole on the standing balance of the elderly. Clin Interv Aging, 2014, 9: 351–356. [DOI] [PMC free article] [PubMed] [Google Scholar]


