Abstract
Psychosocial interventions have significant but modest impact on negative symptoms and functioning in schizophrenia. Identifying mechanisms of change in these interventions can inform treatment targets to strengthen these interventions. A number of studies have found associations between dysfunctional attitudes negative symptoms and functioning in schizophrenia. We previously found improvement in experiential negative symptoms and functioning in cognitive-behavioral social skills training (CBSST) in participants with schizophrenia (N = 149), and the present study examined whether improvements in CBSST in that trial were mediated by the group effect on defeatist performance attitudes and asocial beliefs. In multilevel mediation analyses, the effect of treatment group on experiential negative symptoms and functioning was mediated prospectively through defeatist attitudes but asocial beliefs only mediated effects on experiential negative symptoms. The findings suggest that cognitive-behavioral therapy interventions that target dysfunctional attitudes can lead to improvement in negative symptoms and functioning in schizophrenia.
Keywords: dysfunctional beliefs, motivation, experiential negative symptoms, CBT, CBSST, schizophrenia
Introduction
Schizophrenia is one of the top 10 causes globally of profound functional disability,1 and negative symptoms of schizophrenia account for much of the poor functional outcome.2 Negative symptoms include 2 separate factors of reduced expressive (eg, facial affect, voice tone) and experiential (eg, amotivation, asociality) symptoms.2–5 Experiential negative symptoms are particularly important to treat, because they are more strongly associated with all aspects of functioning.5–8 Unfortunately, available pharmacological and psychosocial interventions have only limited benefits for negative symptoms and functioning.9,10 Psychosocial interventions like cognitive-behavioral therapy (CBT) and social skills training (SST) have been shown to provide partial benefit for negative symptoms and impaired functioning in schizophrenia, with effect sizes in meta-analyses ranging from small to moderate (d = 0.38–0.44).11–14 However, more recent CBT trials show smaller effects on negative symptoms than earlier studies (Velthorst et al15), even for trials that specifically target negative symptoms as the primary outcome.
It may be possible to strengthen the impact of psychosocial interventions on negative symptoms by targeting dysfunctional attitudes. Beck and colleagues16–18 proposed that cognitions like defeatist performance attitudes (eg, “Why try, I always fail”) and asocial beliefs (eg, “I’m better off alone”) contribute to negative symptoms and poor functioning in schizophrenia. The Beck model proposes that discouraging everyday failure experiences (eg, poor grades in school, poor work performance, social rejection) due to illness-related factors like neurocognitive impairment and stigma can lead to low expectations for success and defeatist attitudes, which, in turn, lead to negative symptoms like amotivation and asociality, and ultimately poor functioning. Similarly, in social learning theory,19 self-competency beliefs are central to motivation for achievement and engagement in goal-directed functioning activities.
Several studies have found that dysfunctional attitudes are endorsed more strongly by participants with schizophrenia than healthy controls and are associated with negative symptoms (especially experiential negative symptoms) and poor functioning, even after accounting for depression.17,20–24 A recent meta-analysis25 found relationships between defeatist performance beliefs and negative symptoms across 10 studies and functioning across 8 studies. Some studies have found stronger associations with these outcomes for defeatist attitudes than for asocial beliefs, although asocial beliefs may show stronger associations with social functioning, relative to other forms of functioning.26 There is also some evidence that defeatist attitudes show stronger associations with experiential negative symptoms than with functioning, and the pathway from defeatist attitudes to functioning may be mediated by experiential (motivation) negative symptoms (ie, defeatist attitudes → diminished motivation → functioning).23,24,26
Dysfunctional attitudes can be targeted in CBT to improve negative symptoms and functioning. Grant and colleagues27 found that a CBT intervention designed in part to address defeatist attitudes led to greater reduction in avolition/apathy negative symptoms and global functioning relative to standard treatment in low-functioning participants with schizophrenia. A large (N = 198) RCT comparing CBT with cognitive remediation found comparable significant improvements in negative symptoms in both interventions in participants with schizophrenia,28 although the CBT intervention did not specifically target defeatist attitudes. An open trial by Staring and colleagues29 of a CBT intervention specifically designed to target different types of dysfunctional beliefs found significant reduction in negative symptoms and dysfunctional beliefs in schizophrenia, and change in dysfunctional beliefs partially mediated change in negative symptoms. A pilot RCT of MOtiVation and Enhancement (MOVE) training by Velligan and colleagues30 compared standard care with a 9-month individual home-based intervention that bundled CBT for defeatist attitudes, environmental supports and skills training for participants with schizophrenia with persistent negative symptoms found significantly greater improvement in negative symptoms in the active treatment. Another open CBT trial found improvement in both dysfunctional attitudes and negative symptoms in a sample of participants with psychotic disorders who were not taking antipsychotic medications.31 Thus, there is mounting evidence from clinical trials that dysfunctional attitudes are a mechanism of change in psychosocial interventions targeting negative symptoms and functioning in schizophrenia.
We32 developed Cognitive-Behavioral Social Skills Training (CBSST), which is a bundled intervention that combines CBT, SST, and problem-solving training to target negative symptoms and functioning in schizophrenia. The CBT components of CBSST target defeatist performance attitudes and asocial beliefs that interfere with functioning goals. In 3 clinical trials,33–35 participants with schizophrenia in CBSST showed better functional outcome relative to standard care and a goal-focused supportive contact (GFSC) condition. In the most recent trial,35 participants with schizophrenia also showed significantly greater reduction in severity of both experiential negative symptoms and defeatist performance attitudes relative to GFSC. The present study is a secondary analysis of data from this most recent CBSST trial, which examined whether the treatment group effect on negative symptoms and functioning was mediated by the group effect on defeatist performance attitudes and asocial beliefs. We predicted that these dysfunctional attitudes would mediate the group effect on both negative symptoms and functioning, but given prior research,23,24,26 we predicted stronger mediation effects would be found for negative symptoms relative to functioning and for defeatist attitudes relative to asocial beliefs.
Methods
Design
This study is a secondary analysis of data from a prior randomized clinical trial.35 All study procedures were approved by the institutional review board of the Veterans Affairs San Diego Healthcare System. After providing informed consent and completing baseline assessments, eligible participants were randomly assigned to 1 of 2 treatment conditions: CBSST or GFSC. Participants were then treated for 9 months and followed for 12 months after treatment, with baseline, 4.5-month (mid-treatment), 9-month (end-of-treatment), 15-month (mid-follow-up), and 21-month (1-year post-treatment) follow-up assessments. Assessors were blind to treatment allocation.
Participants
Inclusion criteria were: (1) Age >18, (2) diagnosis of schizophrenia (N = 117) or schizoaffective disorder (N = 32) based on the Structured Clinical Interview for the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (SCID)36 and available medical record review, and (3) capacity to provide informed consent. The minimal exclusion criteria consisted of: (1) Prior exposure to CBT or SST during the previous 5 years, and (2) level of care required at baseline that would interfere with participation in outpatient therapy groups or assessments (eg, disabling medical problems, or current hospitalization for medical, psychiatric, or substance abuse problems). Sample characteristics are shown in table 1.
Table 1.
Sample Characteristics
| Variable | GFSC (N = 76) | CBSST (N = 73) | Statistical Analysis | ||||
|---|---|---|---|---|---|---|---|
| N | % | N | % | χ2 | df | P | |
| Male | 53 | 70 | 46 | 63 | 0.76 | 1 | .385 |
| Caucasian | 44 | 58 | 41 | 56 | 0.05 | 1 | .831 |
| M | SD | M | SD | t | df | P | |
| Age (y) | 41.6 | 9.2 | 41.1 | 10.4 | 0.33 | 147 | .742 |
| Education (y) | 12.3 | 1.8 | 12.3 | 2.0 | 0.04 | 147 | .967 |
| Duration of illness (y) | 21.4 | 10.6 | 21.3 | 11.5 | 0.05 | 147 | .961 |
| PANSS total | 73.3 | 20.0 | 71.5 | 16.6 | 0.59 | 146 | .556 |
Note: GFSC, Goal-Focused Supportive Contact; CBSST, Cognitive Behavioral Social Skills Training; PANSS, Positive and Negative Syndrome Scale.
Interventions
Participants in both treatment conditions were offered a total of 36 weekly group therapy sessions (9 months) during a treatment phase, which was followed by monthly booster group sessions during the follow-up period (12 sessions). In both conditions, group therapy sessions were 2 hours, with a lunch or snack break mid-way, and both groups were also offered individual goal-setting sessions at baseline and every 3 months thereafter.
Cognitive-Behavioral Social Skills Training.
CBSST32 was delivered in 3, 6-session modules that were intended to be completed twice, for a total of 36 weekly sessions. The 3 CBSST modules were Cognitive Skills, Social Skills, and Problem-Solving Skills. Training thought challenging skills was the exclusive focus of the Cognitive Skills Module, but thought challenging was also used throughout the other 2 modules. Group members were introduced to the general concepts of CBT, including the relationship between thoughts, actions and feelings (generic cognitive model), automatic thoughts, thought challenging through behavioral experiments and examining evidence for beliefs, and mistakes in thinking. The primary thought challenging skill trained was the 3C’s: Catch It, Check It, Change It (“It” is an unhelpful thought).
The primary goal of the Social Skills Module was to improve communication skills through behavioral role plays, including active listening, expressing positive and negative feelings and making positive requests. Important role plays included assertive interactions with co-workers, friends and family, making new friends, and effectively interacting with case managers, doctors, and other support persons.
Basic problem-solving skills were trained in the Problem-Solving Skills Module using the acronym, SCALE – Specify the problem, Consider all possible solutions, Assess the best solution, Lay out a plan, and Execute and Evaluate the outcome. The focus was on developing specific, feasible plans to solve real-world problems, including scheduling pleasant activities, improving living situations, finances, using public transportation, finding a volunteer or paid job, and enrolling in classes.
Goal-Focused Supportive Contact.
The GFSC intervention was an enhanced supportive contact control condition with a primary focus, like CBSST, on setting and achieving functioning goals. Sessions included components of psychoeducation, empathy, and nondirective reinforcement of health, coping, and symptom management behaviors, which grew out of group discussions about goals, with minimal therapist guidance.
Assessment Measures
Clinical Symptoms.
The Positive and Negative Syndrome Scale (PANSS),37 and the Scale for the Assessment of Negative Symptoms (SANS)38 were administered. Based on factor analytic studies of the SANS,3,5 the SANS-Diminished Motivation (SANS-DM) factor was defined as the average of Avolition-Apathy and Anhedonia-Asociality global ratings (Items 17, 22). Inter-rater reliability (interclass correlation) was .88 for PANSS and .83 for SANS. The SANS-DM was administered at all assessment points.
Functioning.
Self-reported instrumental functioning was assessed using the Independent Living Skills Survey (ILSS).39 The ILSS is a 51-item, self-report measure which was administered in an interview format to assess multiple domains of functioning. A composite score was computed as the average of scores (rated 1 = yes, performed; 0 = no, not performed) on 5 relevant functional domains (appearance and clothing, personal hygiene, health maintenance, transportation, and leisure and community activities; range = 0–1). The ILSS was administered at all assessment points.
Performance-based social competence was assessed using the Maryland Assessment of Social Competence (MASC).40 The MASC is a structured behavioral role play assessment that measures the ability to resolve interpersonal problems through conversation scenarios (1 conversation initiation; 2 assertion), during which the participant interacts with a live confederate who plays a role (eg, boss) in a problem-oriented situation (eg, asking for a work shift change). The measure has 3 parallel sets of scenarios for multiple administrations. Videotaped role plays are coded by blinded raters on dimensions of verbal content, nonverbal communication behavior, and an overall effectiveness score, which was the primary MASC variable. Inter-rater reliability (interclass correlation) was .86 for the MASC. The MASC was not administered at mid-treatment or mid-follow-up assessments.
Dysfunctional Attitudes (Mediators).
The Defeatist Performance Attitude Scale (DPAS) is a 15-item self-report subscale derived from factor analysis of the commonly-used Dysfunctional Attitude Scale.41 The DPAS indexes endorsement of defeatist attitudes about one’s ability to perform goal-directed tasks (eg, “If you cannot do something well, there is little point in doing it at all,” “If I fail at my work, then I am a failure as a person,” “People will probably think less of me if I make mistakes and fail”). Items are rated on a 1–7 Likert scale with higher total scores (range = 15–105) indicating more severe defeatist performance attitudes.
The Asocial Beliefs Scale (ABS) is a 15-item scale derived from the Revised Social Anhedonia Scale (RSAS).42 In order to specifically tap attitudes of social disinterest, rather than emotional experiences, Grant and Beck42 selected 15 RSAS items with face validity for assessing social disinterest in interacting with others, including “I attach very little importance to having close friends” and “I could be happy living all alone in a cabin in the woods or mountains.” Items that reflected frequency of actual social interactions and emotional aspects of social satisfaction and pleasure or general emotional dysregulation were not included. Items are rated true or false with higher scores (range = 0–15) indicating more severe asocial beliefs. The ABS was administered at all time points.
Statistical Analysis
Mediation analyses were conducted to test the hypothesized relations between treatment group (CBSST vs GFSC), mediators (DPAS; ABS), and outcome variables (SANS-DM; ILSS; MASC).43 Multilevel mediation models were used to include multiple nested time points within individuals and to model variables at the levels of both person (treatment group) and time (mediators, outcomes), with random person-level intercepts. Mediator variables were incorporated as time-varying predictors. All available data were included via maximum likelihood estimation, a preferred estimation method when missing data are assumed missing-at-random.44 The missing-at-random assumption was supported by analyses showing that the subsample with complete follow-up data did not differ from those with any missing data on ethnicity, Χ2(1) = 0.28, P = .59, education level, Χ2(2) = 1.25, P = .54, gender, Χ2(1) = 0.03, P = .86, age at baseline, F(1,145) = 3.26, P = .07, or baseline levels of any mediators or outcome variables, including negative symptoms (F values 0.00–1.95, P values .16–.95). Preliminary models also revealed no statistically-significant confounding differences between treatment groups on study variables at baseline. We expected to see better levels of outcomes associated with greater session attendance, so session attendance and time were included as covariates for all models. All mediators and outcome variables were standardized (to baseline levels) to improve interpretation. All analyses were conducted in Stata 14.0.45
Mediation analyses were conducted in 3 sequential steps, which restricted the number of potential analyses by eliminating candidate mediation paths in a stepwise manner. Hypothesized mediation paths were first examined with the test of joint significance, in which separate multilevel models test the “a path” (group effect to mediator) and the “b path” (mediator to outcome) with mediators used to predict outcomes at concurrent time points. Mediation paths passing this test were then examined further by directly estimating the mediated effect with the products-of-coefficients approach and determining statistical significance with bias-corrected asymmetric 95% confidence limits estimated with a bootstrap procedure.46 These methods have been shown to have greater accuracy and power to detect mediated effects than alternative approaches.47 Mediation effect sizes were reported with the proportion of the total effect (ie, treatment group difference in the outcome) explained by the mediated effect.46 All statistically-significant concurrent mediation effects were then examined further to test temporal precedence. In prospective multilevel models, mediation effects were re-estimated with outcome variables predicted by lagged (ie, prior visit) mediators controlling for treatment group, session attendance, and time. Each set of analyses (concurrent and prospective) offers some unique information with distinct strengths. One weakness of the prospective mediation model is that in order to test lagged effects, it restricts the outcome data to the final 3 follow-ups, while the concurrent mediation model uses outcome data from all 4 follow-ups. The concurrent mediation analysis provides the best opportunity to identify mediation using all available data, and also highlights potential early changes in outcomes (by mid-treatment) that are not captured by the prospective mediation analysis. The strength of the prospective mediation is that the temporally-precedent effects provide an additional layer of support for establishing these mediators as mechanisms of change.
Results
Group Effects on Mediators
Descriptive data for all outcome and mediator variables are shown in table 1. As reported in the parent clinical trial,35 effect sizes for the difference between model-estimated means of the 2 treatment groups at final follow-up ranged from small to very large (SANS Diminished Motivation = .52; ILSS = 1.00; DPAS = .90; ABS = .14). Results of multilevel models estimating the “a path” (group effect to mediator), “b path” (mediator to outcome) and mediated effects (ab) of treatment group (CBSST vs GFSC) on negative symptoms and functioning through dysfunctional attitudes (DPAS, ABS) at concurrent time points are shown in table 1. The “a path” analyses examined the effect of CBSST on the post-baseline mediator variable. As compared to GFSC, participants in the CBSST group had significantly lower DPAS (a = −0.40, SE = 0.17, P < .05) but not significantly lower ABS (a = −0.07, SE = 0.17, P = .69) (tables 2 and 3). The correlation between ABS and DPAS was, r = .258, P = .002, suggesting a significant but modest association between the constructs.
Table 2.
Descriptive Statistics for Available Data on All Measures at Each Assessment Point for Each Treatment Group
| Measure | Group | Baseline | 4 Months | End of Treatment | 6-Month Follow-up | 12-Month Follow-up | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| N | M (SD) | N | M (SD) | N | M (SD) | N | M (SD) | N | M (SD) | ||
| ILSS | CBSST | 72 | 0.73 (0.10) | 41 | 0.74 (0.10) | 35 | 0.72 (0.10) | 23 | 0.73 (0.12) | 24 | 0.71 (0.11) |
| GFSC | 76 | 0.70 (0.10) | 50 | 0.71 (0.11) | 44 | 0.71 (0.10) | 31 | 0.69 (0.12) | 31 | 0.69 (0.11) | |
| MASC | CBSST | 63 | 3.4 (1.0) | — | — | 35 | 3.8 (0.9) | — | — | 24 | 3.5 (0.8) |
| GFSC | 74 | 3.2 (1.2) | — | — | 42 | 3.4 (1.1) | — | — | 28 | 3.3 (1.0) | |
| SANS Dim Mot | CBSST | 71 | 2.26 (1.11) | 39 | 2.33 (1.14) | 36 | 2.06 (1.06) | 24 | 2.02 (1.12) | 25 | 1.74 (0.81) |
| GFSC | 76 | 2.11 (1.17) | 49 | 2.11 (1.16) | 45 | 2.29 (0.91) | 33 | 2.26 (1.31) | 31 | 2.27 (1.15) | |
| DPAS | CBSST | 71 | 51.1 (17.2) | 42 | 51.6 (15.7) | 36 | 49.8 (14.6) | 24 | 46.2 (16.9) | 25 | 44.2 (13.3) |
| GFSC | 76 | 56.0 (17.2) | 52 | 56.2 (19.4) | 45 | 54.1 (18.3) | 33 | 54.3 (17.9) | 32 | 54.8 (17.7) | |
| ABS | CBSST | 71 | 5.9 (2.9) | 42 | 6.5 (3.4) | 36 | 5.6 (3.0) | 23 | 5.3 (2.9) | 25 | 6.0 (2.7) |
| GFSC | 76 | 6.2 (2.9) | 52 | 6.1 (2.6) | 45 | 7.1 (2.8) | 33 | 5.8 (2.3) | 32 | 6.5 (2.7) | |
Note: CBSST, Cognitive Behavioral Social Skills Training; GFSC, Goal-Focused Supportive Contact; ILSS, Independent Living Skills Survey; MASC, Maryland Assessment of Social Competence (MASC; not administered at mid-treatment or mid-follow-up); SANS, Scale for Assessment of Negative Symptoms Diminished Motivation and Diminished Expression factors; DPAS, Defeatist Performance Attitude Scale; ABS, Asocial Beliefs Scale. Groups did not differ significantly at baseline on any outcome measure.
Table 3.
Results of Multilevel Analyses Estimating the Concurrent Mediated Effects (ab) of Treatment Group (CBSST vs GFSC) on Negative Symptoms and Functioning Through Defeatist Performance Attitudes Scale (DPAS) and Asocial Beliefs Scale (ABS)
| Mediator | Outcome | a Path Group→ Attitudes | b Path Attitudes→ Outcome | ab Mediation Effect | ab Effect 95% CI | % of Total Effect |
|---|---|---|---|---|---|---|
| DPAS | SANS-DM | −0.40* | 0.16* | −0.06* | −0.11, −0.03 | 30% |
| ILSS | −0.40* | −0.12* | 0.05* | 0.01, 0.08 | 12% | |
| MASC | −0.40* | −0.26** | 0.11* | 0.06, 0.17 | 39% | |
| ABS | SANS-DM | −0.07 | 0.23** | −0.02* | −0.04, −0.001 | 8% |
| ILSS | −0.07 | −0.04 | 0.003 | −0.003, 0.009 | 0.7% | |
| MASC | −0.07 | −0.20* | 0.01 | −0.04, 0.06 | 7% |
Note: CBSST, Cognitive-Behavioral Social Skills Training; GFSC, Goal-Focused Supportive Contact; SANS-DM, Scale for Assessment of Negative Symptoms-Diminished Motivation; ILSS, Independent Living Skills Survey; MASC, Maryland Assessment of Social Competence.
*P < .05, **P < .001.
Mediator Relations With Outcome Variables
The “b path” analyses, which examined associations between time-varying mediators and outcomes, revealed several statistically significant associations. Greater DPAS was associated with greater diminished motivation (b = 0.16, SE = 0.06, P < .05) and poorer functioning on both the ILSS (b = −0.12, SE = 0.06, P < .05) and MASC (b = −0.26, SE = 0.08, P < .001). Greater ABS was also associated with greater diminished motivation (b = 0.23, SE = 0.06, P < .001) and poorer functioning on the MASC (b = −0.20, SE = 0.08, P < .05), but not the ILSS (b = −0.04, SE = 0.06, P = .49).
Estimation of Mediated Effects
Mediation effects (ab) and associated 95% CIs were directly estimated. The CBSST condition had superior outcomes in several domains, which were significantly mediated by DPAS, and to some extent by ABS. Specifically, lower DPAS in CBSST (compared to GFSC) significantly mediated the effects of CBSST on lower diminished motivation (ab = −0.06, P < .05), greater instrumental functioning on the ILSS (ab = 0.05, P < .05), and greater social competence on the MASC (ab = 0.11, P < .05). The effects of CBSST on lower diminished motivation were also significantly mediated by lower ABS, as this mediation effect was statistically significant (ab = −0.024, P < .05). The mediation effects from CBSST through ABS was not statistically significant for functioning on the ILSS (ab = 0.003, P > .05) or social competence on the MASC (ab = 0.01, P > .05).
Prospective Mediation Effects
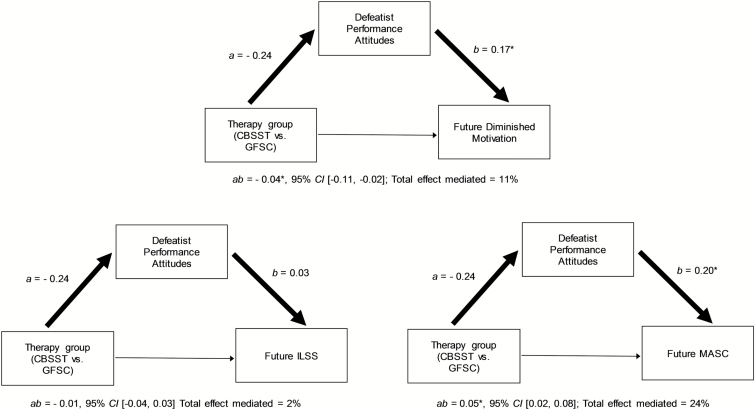
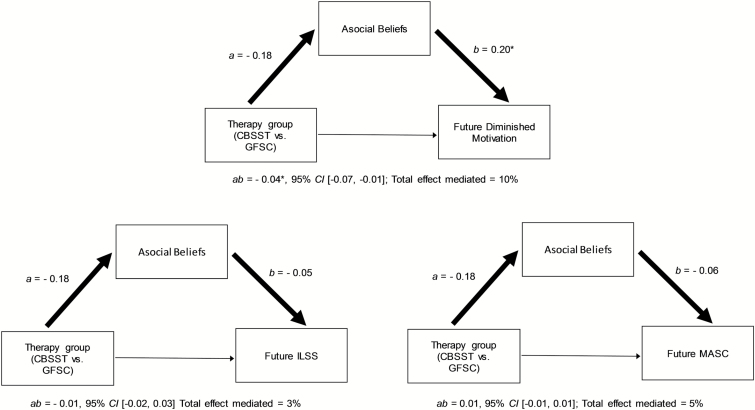
The criteria for establishing potential causal mechanisms of change include both statistical mediation and temporal precedence. To test temporal precedence, further analyses examined whether the significant mediation paths through DPAS and ABS would persist when tested prospectively. In these models prior or “lagged” post-baseline mediators (month 4, 9, and 15) were used to predict subsequent outcomes (month 9, 15, and 21) in multilevel models. As shown in figure 1, the effects of CBSST on DPAS prospectively mediated effects on lower diminished motivation and greater social competence on the MASC, but not instrumental functioning on the ILSS. As shown in figure 2, the effects of CBSST on lower ABS also prospectively mediated the effects on lower diminished motivation, but not functioning (ILSS or MASC). These results provided evidence that the advantages of CBSST for reducing experiential negative symptoms and improving social functioning were both mediated and temporally preceded by lower levels of DPAS, and lower ABS for experiential negative symptoms.
Fig. 1.
Results of models estimating the prospective mediation effects of treatment group on Diminished Motivation (Scale for Assessment of Negative Symptoms [SANS]) and functioning (Independent Living Skills Survey [ILSS] and Maryland Assessment of Social Competence [MASC]) through prior defeatist performance attitudes (Defeatist Performance Attitudes Scale [DPAS]). *P < .05.
Fig. 2.
Results of models estimating the prospective mediation effects of treatment group on Diminished Motivation (Scale for Assessment of Negative Symptoms [SANS]) and functioning (Independent Living Skills Survey [ILSS], Maryland Assessment of Social Competence [MASC]) through prior asocial beliefs (Asocial Beliefs Scale [ABS]). *P < .05.
Discussion
Specific psychosocial interventions like CBSST can lead to modest improvements in negative symptoms and functioning in schizophrenia. Identifying mechanisms of change in these interventions can inform treatment targets to strengthen the impact of psychosocial interventions on these outcomes. The present study examined whether reduction in severity of dysfunctional attitudes mediated improvements in experiential negative symptoms and functioning a secondary analysis of data from a recent CBSST clinical trial.35 Consistent with hypotheses, dysfunctional attitudes mediated the group effect on both experiential negative symptoms and functioning. Also, consistent with hypotheses and prior research,23,24,26 mediation effects were more consistently found for negative symptoms relative to functioning and for defeatist performance attitudes relative to asocial beliefs. Importantly, the longitudinal findings from this study support causal relationships in the direction from dysfunctional attitudes to negative symptoms and functioning, filling a gap in the predominantly cross-sectional literature.25 Another recent longitudinal study26 also supported the directionality of these relationships in schizophrenia, and found different patterns of relationships for defeatist vs asocial beliefs.
The CBT components of CBSST target defeatist performance attitudes and asocial beliefs that interfere with functioning goals.33–35 Participants with schizophrenia in CBSST showed better functional outcome and greater reduction in severity of experiential negative symptoms and defeatist performance attitudes relative to GFSC.35 Other clinical trials of CBT for schizophrenia have also found significant reductions in dysfunctional attitudes29,48 and one trial found evidence for partial mediation of improvements in negative symptoms by dysfunctional attitudes.29 The findings from the present study further suggest that modification of dysfunctional attitudes may be an important treatment target in CBT interventions like CBSST for schizophrenia, whereby reduction in dysfunctional attitudes contributes to improved motivation and effort devoted to goal-directed functioning tasks.
Mediation effects were more robust for experiential negative symptoms than for functioning outcomes. For experiential negative symptoms, significant concurrent and prospective ab mediation paths were found for both DPAS and ABS, but for functioning, a significant prospective ab mediation path was found only for DPAS and performance-based social competence but not self-reported instrumental functioning, and ABS did not mediate either type of functioning outcome. The findings may suggest that dysfunctional attitudes are more strongly associated with negative symptoms than with functioning, which would be expected if the pathway from dysfunctional attitudes to functioning is mediated by amotivation.23,24,26 This would lead to stronger associations between dysfunctional attitudes and experiential negative symptoms than functioning further downstream. Finally, the finding that DPAS prospectively mediated social functioning on the MASC, but not instrumental functioning on the ILSS, may be due to the different types of functioning tapped by the tasks or due to the psychometric properties of the tasks, because performance-based measures like the MASC may be more reliable and valid measures of functioning than self-report measures like the ILSS.49,50
DPAS and ABS also showed a different pattern mediation effects. Mediation of experiential negative symptoms and functioning was found for DPAS, whereas ABS mediated experiential negative symptoms but not functioning. It is possible that more generalized defeatist beliefs contribute to amotivation and performance of instrumental and social role behaviors, whereas social disinterest beliefs contribute more specifically to asociality and social functioning.26 The psychometrics of the DPAS and ABS scales may have also influenced the strength of associations found, given that DPAS items are rated on a 7-point Likert scale resulting in a broad range of scores, while ABS items, which are rated true/false, have a more limited range of possible scores (table 2). Future research might address this by using a Likert scale for the ABS measure. In addition, if the CBSST intervention is modified in future research to strengthen aspects that target socialization, such as growing social networks, greater impact of asocial beliefs on social outcomes may be found. Finally, future research might also benefit from better outcome measures. For example, ecological momentary assessment (EMA) of the frequency and quality of social interactions using smartphones to sample real-time, real-world activities multiple times a day for 1 or 2 weeks may provide a more sensitive measure of social functioning that could show stronger associations with asocial beliefs. Future research may also benefit from newer negative symptom measures, like the Clinical Assessment Interview for Negative Symptoms (CAINS; Kring et al8), which was developed to better capture motivation and pleasure deficits and relies less on behavioral or performance deficits that overlap with functioning measures. The CAINS, therefore, may help identify which types of dysfunctional beliefs are more specifically linked to motivational negative symptoms.
This study had several limitations. As described in the parent report of this clinical trial,35 this clinical trial had a high dropout rate (46%), which limits interpretation of results, because group differences found might reflect a selective bias in who remained in the study. Several steps were taken to address this and increase confidence in the results. First, the multilevel mediation models used do not require complete data and participants with missing data were included in analyses. In addition, the 2 treatment groups did not differ significantly in drop-out rates, and the missing-at-random assumption was supported by analyses showing that the subsample with complete follow-up data did not differ significantly from those with any missing data on any demographic, outcome or mediator variable, including negative symptoms. Session attendance was also included as a covariate in the models. These analyses provided no evidence that drop-out rates introduced a systematic bias into the sample. Typical of schizophrenia research, the sample was also predominantly male and had been ill for over 20 years on average, so findings may not generalize to younger first-episode samples. We are aware of at least 1 study, however, that found associations between dysfunctional attitudes and negative symptoms and functioning in a recent-onset sample.51 Finally, the severity of negative symptoms in the sample was on average relatively mild. Thus, floor effects may have contributed to the modest effects found for change in negative symptoms during treatment. A clinical trial specifically targeting negative symptoms and recruiting patients with persistent moderate to severe negative symptoms may show more robust effects or such a trial may find that CBSST is not as effective for participants with more severe negative symptoms.
Despite these limitations, identifying treatments to reduce negative symptom severity and improve functioning in schizophrenia is of high public health significance. The results of this study suggest that novel interventions like CBSST,32 Recovery-Oriented Cognitive Therapy (CT-R),27 MOtiVation and Enhancement Training (MOVE),30 and Cognitive Behavioral Therapy for negative symptoms (CBT-n)29 that target dysfunctional attitudes can improve experiential negative symptoms and functioning outcomes in schizophrenia.
Funding
Research reported in this publication was supported by the Department of Veterans Affairs, Veterans Health Administration, Office of Research and Development, Rehabilitation Research and Development Service, the National Institute of Mental Health of the National Institutes of Health (grant R01MH071410 to E.G.), and the National Institute on Drug Abuse (K23DA039348 to M.W.). The content is solely the responsibility of the authors and does not necessarily represent the official views of the Department of Veterans Affairs or National Institutes of Health.
Acknowledgments
We thank the participants who volunteered for this study. E.G. has an equity interest in Granholm Consulting, Inc., a company that may potentially benefit from the research results as he receives income from the company for CBSST workshops and consulting. The terms of this arrangement have been reviewed and approved by the University of California, San Diego in accordance with its conflict of interest policies. Trial Registry: ClinicalTrials.gov #NCT 00338975.
References
- 1. Wu EQ, Birnbaum HG, Shi L et al. The economic burden of schizophrenia in the United States in 2002. J Clin Psychiatry. 2005;66:1122–1129. [DOI] [PubMed] [Google Scholar]
- 2. Kirkpatrick B, Fenton WS, Carpenter WT Jr, Marder SR. The NIMH-MATRICS consensus statement on negative symptoms. Schizophr Bull. 2006;32:214–219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Blanchard JJ, Cohen AS. The structure of negative symptoms within schizophrenia: implications for assessment. Schizophr Bull. 2006;32:238–245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Marder SR, Kirkpatrick B. Defining and measuring negative symptoms of schizophrenia in clinical trials. Eur Neuropsychopharmacol. 2014;24:737–743. [DOI] [PubMed] [Google Scholar]
- 5. Sayers SL, Curran PJ, Mueser KT. Factor structure and construct validity of the scale for the assessment of negative symptoms. Psychol Assess. 1996;8:269–280. [Google Scholar]
- 6. Dowd EC, Barch DM. Anhedonia and emotional experience in schizophrenia: neural and behavioral indicators. Biol Psychiatry. 2010;67:902–911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Strauss GP, Horan WP, Kirkpatrick B et al. Deconstructing negative symptoms of schizophrenia: avolition-apathy and diminished expression clusters predict clinical presentation and functional outcome. J Psychiatr Res. 2013;47:783–790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kring AM, Gur RE, Blanchard JJ, Horan WP, Reise SP. The clinical assessment interview for negative symptoms (CAINS): final development and validation. Am J Psychiatry. 2013;170:165–172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kreyenbuhl J, Buchanan RW, Dickerson FB, Dixon LB. The schizophrenia patient outcomes research team (PORT): updated treatment recommendations 2009. Schizophr Bull. 2010;36:94–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Singh SP, Singh V, Kar N, Chan K. Efficacy of antidepressants in treating the negative symptoms of chronic schizophrenia: meta-analysis. Br J Psychiatry. 2010;197:174–179. [DOI] [PubMed] [Google Scholar]
- 11. Kurtz MM, Mueser KT. A meta-analysis of controlled research on social skills training for schizophrenia. J Consult Clin Psychol. 2008;76:491–504. [DOI] [PubMed] [Google Scholar]
- 12. Wykes T, Steel C, Everitt B, Tarrier N. Cognitive behavior therapy for schizophrenia: effect sizes, clinical models, and methodological rigor. Schizophr Bull. 2008;34:523–537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Thase ME, Kingdon D, Turkington D. The promise of cognitive behavior therapy for treatment of severe mental disorders: a review of recent developments. World Psychiatry. 2014;13:244–250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Turner DT, van der Gaag M, Karyotaki E, Cuijpers P. Psychological interventions for psychosis: a meta-analysis of comparative outcome studies. The American Journal of Psychiatry. 2014;171:523–538. [DOI] [PubMed] [Google Scholar]
- 15. Velthorst E, Koeter M, van der Gaag M et al. Adapted cognitive-behavioural therapy required for targeting negative symptoms in schizophrenia: meta-analysis and meta-regression. Psychol Med. 2015;45:453–465. [DOI] [PubMed] [Google Scholar]
- 16. Beck AT, Rector NA, Stolar NM, Grant PM.. Schizophrenia: Cognitive Theory, Research, and Therapy. New York, NY: Guilford Press; 2009. [Google Scholar]
- 17. Grant PM, Beck AT. Defeatist beliefs as a mediator of cognitive impairment, negative symptoms, and functioning in schizophrenia. Schizophr Bull. 2009;35:798–806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Rector NA, Beck AT, Stolar N. The negative symptoms of schizophrenia: a cognitive perspective. Can J Psychiatry. 2005;50:247–257. [DOI] [PubMed] [Google Scholar]
- 19. Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Englewood Cliffs, NJ: Prentice-Hall; 1986. [Google Scholar]
- 20. Avery R, Startup M, Calabria K. The role of effort, cognitive expectancy appraisals and coping style in the maintenance of the negative symptoms of schizophrenia. Psychiatry Res. 2009;167:36–46. [DOI] [PubMed] [Google Scholar]
- 21. Couture SM, Blanchard JJ, Bennett ME. Negative expectancy appraisals and defeatist performance beliefs and negative symptoms of schizophrenia. Psychiatry Res. 2011;189:43–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Horan WP, Rassovsky Y, Kern RS et al. Further support for the role of dysfunctional attitudes in models of real-world functioning in schizophrenia. J Psychiatr Res. 2010;44:499–505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Green MF, Hellemann G, Horan WP, Lee J, Wynn JK. From perception to functional outcome in schizophrenia: modeling the role of ability and motivation. Arch Gen Psychiatry. 2012;69:1216–1224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Quinlan T, Roesch S, Granholm E. The role of dysfunctional attitudes in models of negative symptoms and functioning in schizophrenia. Schizophr Bull. 2014;157:182–189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Campellone TR, Sanchez AH, Kring AM. Defeatist performance beliefs, negative symptoms, and functional outcome in schizophrenia: a meta-analytic review. Schizophr Bull. 2016;42:1343–1352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Thomas EC, Luther L, Zullo L, Beck AT, Grant PM. From neurocognition to community participation in serious mental illness: the intermediary role of dysfunctional attitudes and motivation. Psychol Med. 2016;47:1–15. [DOI] [PubMed] [Google Scholar]
- 27. Grant PM, Huh GA, Perivoliotis D, Stolar NM, Beck AT. Randomized trial to evaluate the efficacy of cognitive therapy for low-functioning patients with schizophrenia. Arch Gen Psychiatry. 2012;69:121–127. [DOI] [PubMed] [Google Scholar]
- 28. Klingberg S, Wölwer W, Engel C et al. Negative symptoms of schizophrenia as primary target of cognitive behavioral therapy: results of the randomized clinical TONES study. Schizophr Bull. 2011;37(suppl 2):S98–S110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Staring AB, Ter Huurne MA, van der Gaag M. Cognitive behavioral therapy for negative symptoms (CBT-n) in psychotic disorders: a pilot study. J Behav Ther Exp Psychiatry. 2013;44:300–306. [DOI] [PubMed] [Google Scholar]
- 30. Velligan DI, Roberts D, Mintz J et al. A randomized pilot study of MOtiVation and Enhancement (MOVE) Training for negative symptoms in schizophrenia. Schizophr Res. 2015;165:175–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Morrison AP, Turkington D, Wardle M et al. A preliminary exploration of predictors of outcome and cognitive mechanisms of change in cognitive behaviour therapy for psychosis in people not taking antipsychotic medication. Behav Res Ther. 2012;50:163–167. [DOI] [PubMed] [Google Scholar]
- 32. Granholm EL, McQuaid JR, Holden JL.. Cognitive-behavioral Social Skills Training for Schizophrenia: A Practical Treatment Guide. New York, NY: The Guilford Press; 2016. [Google Scholar]
- 33. Granholm E, McQuaid JR, McClure FS et al. A randomized, controlled trial of cognitive behavioral social skills training for middle-aged and older outpatients with chronic schizophrenia. Am J Psychiatry. 2005;162:520–529. [DOI] [PubMed] [Google Scholar]
- 34. Granholm E, Holden J, Link PC, McQuaid JR, Jeste DV. Randomized controlled trial of cognitive behavioral social skills training for older consumers with schizophrenia: defeatist performance attitudes and functional outcome. Am J Geriatr Psychiatry. 2013;21:251–262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Granholm E, Holden J, Link PC, McQuaid JR. Randomized clinical trial of cognitive behavioral social skills training for schizophrenia: improvement in functioning and experiential negative symptoms. J Consult Clin Psychol. 2014;82:1173–1185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. First MB, Spitzer R, Gibbon M, Williams J.. Structured Clinical Interview for DSM-IV Axis I Disorders - Patient Edition (SCID-I/P, Version 2.0). New York, NY: New York State Psychiatric Institute, Biometrics Research Department; 1996. [Google Scholar]
- 37. Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13:261–276. [DOI] [PubMed] [Google Scholar]
- 38. Andreasen NC. Negative symptoms in schizophrenia. Definition and reliability. Arch Gen Psychiatry. 1982;39:784–788. [DOI] [PubMed] [Google Scholar]
- 39. Wallace CJ, Liberman RP, Tauber R, Wallace J. The independent living skills survey: a comprehensive measure of the community functioning of severely and persistently mentally ill individuals. Schizophr Bull. 2000;26:631–658. [DOI] [PubMed] [Google Scholar]
- 40. Bellack AS, Sayers M, Mueser KT, Bennett M. Evaluation of social problem solving in schizophrenia. J Abnorm Psychol. 1994;103:371–378. [DOI] [PubMed] [Google Scholar]
- 41. Cane DB, Olinger LJ, Gotlib IH, Kuiper NA. Factor structure of the dysfunctional attitude scale in a student population. J Clin Psychol. 1986;42:307–309. [Google Scholar]
- 42. Grant PM, Beck AT. Asocial beliefs as predictors of asocial behavior in schizophrenia. Psychiatry Res. 2010;177:65–70. [DOI] [PubMed] [Google Scholar]
- 43. Krull JL, MacKinnon DP. Multilevel modeling of individual and group level mediated effects. Multivariate Behav Res. 2001;36:249–277. [DOI] [PubMed] [Google Scholar]
- 44. Schafer JL, Graham JW. Missing data: our view of the state of the art. Psychol Methods. 2002;7:147–177. [PubMed] [Google Scholar]
- 45. Stata Statistical Software: Release 14 [computer program]. College Station, TX: StataCorp LP; 2015. [Google Scholar]
- 46. MacKinnon DP. Introduction to statistical mediation analysis. New York, NY: Lawrence Erlbaum Associates; 2008. [Google Scholar]
- 47. MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V. A comparison of methods to test mediation and other intervening variable effects. Psychol Methods. 2002;7:83–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Morrison AP, French P, Stewart SL et al. Early detection and intervention evaluation for people at risk of psychosis: multisite randomised controlled trial. BMJ. 2012;344:e2233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Harvey PD, Raykov T, Twamley EW et al. Validating the measurement of real-world functional outcomes: phase I results of the VALERO study. The American Journal of Psychiatry. 2011;168:1195–1201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Bowie CR, Twamley EW, Anderson H, Halpern B, Patterson TL, Harvey PD. Self-assessment of functional status in schizophrenia. J Psychiatr Res. 2007;41:1012–1018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Ventura J, Subotnik KL, Ered A et al. The relationship of attitudinal beliefs to negative symptoms, neurocognition, and daily functioning in recent-onset schizophrenia. Schizophr Bull. 2014;40:1308–1318. [DOI] [PMC free article] [PubMed] [Google Scholar]