Abstract
Patients describe experiencing personal recovery despite ongoing symptoms of psychosis. The aim of the current research was to perform a meta-analysis investigating the relationship between clinical and personal recovery in patients with schizophrenia spectrum disorders. A comprehensive OvidSP database search was performed to identify relevant studies. Correlation coefficients of the relationship between clinical and personal recovery were retrieved from primary studies. Meta-analyses were performed, calculating mean weighted effect sizes for the association between clinical and personal recovery, hope, and empowerment. Additionally, associations between positive, negative, affective symptoms, general functioning, and personal recovery were investigated. The results show that heterogeneity across studies was substantial. Random effect meta-analysis of the relationship between symptom severity and personal recovery revealed a mean weighted correlation coefficient of r = −.21 (95% CI = −0.27 to −0.14, P < .001). We found the following mean weighted effect size for positive symptoms r = −.20 (95% CI = −0.27 to −0.12, P < .001), negative symptoms r = −.24 (95% CI = −0.33 to −0.15, P < .001), affective symptoms r = −.34 (95% CI = −0.44 to −0.24, P < .001) and functioning r = .21 (95% CI = −0.09 to 0.32, P < .001). The results indicate a significant small to medium association between clinical and personal recovery. Psychotic symptoms show a smaller correlation than affective symptoms with personal recovery. These findings suggest that clinical and personal recovery should both be considered in treatment and outcome monitoring of patients with schizophrenia spectrum disorders.
Keywords: schizophrenia, psychosis, psychotic disorder, personal recovery, hope, empowerment
Introduction
Recovery has become an increasingly important aspect of care in mental health services all over the world.1 Recovery-oriented practices have especially emerged for schizophrenia, which has traditionally been seen as a condition with an unfavorable course.2 Since the second half of the 20th-century patient organizations have challenged the assumption that people with schizophrenia cannot live a productive and satisfying life. Patients have emphasized that recovery can occur even when psychotic symptoms are persistent.3 Scientific- and patient-based influences have resulted in a clinical and a personal definition of recovery in schizophrenia.2
The clinical definition includes remission of symptoms and functional improvement. The Remission in Schizophrenia Working Group (RSWG) defines remission as improvements in core signs and symptoms to the extent that they are of such low intensity that they no longer interfere significantly with behavior.4 Operational criteria include a score of mild or less on specific items of a symptom scale over a 6-month period, eg, the Positive and Negative Syndrome Scale (PANSS) or the Brief Psychiatric Rating Scale (BPRS). The RSWG describes that recovery, besides being relatively free of disease-related psychopathology, implies the ability to function in the community, socially and vocationally. The RSWG states that recovery is a more demanding and longer-term phenomenon than remission and that remission is a necessary but not sufficient step toward recovery. Moreover, the RSWG writes that consensus regarding operational criteria for recovery, in particular, cognition or psychosocial functioning, was considered outside its scope, because more research is needed on this topic.4 Other authors have also included living independently, having friends5 and scores of >65 on the Global Assessment of Functioning (GAF) to the criteria of clinical recovery.6
The patient-based definition of recovery has been developed based on narratives of individuals who have experienced mental illness.7,8 Stories from the patient movement have shown that people with psychosis have the possibility of living a productive and satisfying life, despite ongoing symptoms.3 The most frequently cited patient-based definition is: “the development of new meaning and purpose in one’s life, as one grows beyond the catastrophic effects of mental illness.”9 Recovery from schizophrenia is not a uniform process but varies from person to person.10 The term personal recovery has been widely used in literature to describe the patient-based definition of recovery.11
Because personal recovery is different for every individual, it is hard to define common characteristics. Nonetheless, several authors have tried to capture important aspects of personal recovery in qualitative research. Andresen et al,12 by reviewing published experiential accounts of recovery by people with schizophrenia, have identified 4 key processes of personal recovery: finding hope; re-establishment of identity; finding meaning in life; and taking responsibility for recovery. Leamy et al13 have identified similar categories of personal recovery processes, namely connectedness, hope, identity, meaning, and empowerment (also known by the acronym “CHIME”). In a more recent study, this framework has been validated as a defensible theoretical base for clinical and research purposes.14 Law and Morrison15 have found comparable elements in their Delphi study among individuals experiencing symptoms of psychosis. Several instruments have been developed, based on the experience of patients, to assess personal recovery,16–19 hope,20 and empowerment.21
In the treatment of patients with schizophrenia, the primary goal traditionally is clinical recovery. So far, inconsistent findings regarding the association between clinical and personal recovery have been published, from large22 to very small correlations,23 usually negative, but also positive correlations.24 Insight into this association is important because if clinical and personal domains do not overlap, this may inform mental health services to consider extending their treatment strategies beyond clinical goals to promote personal recovery. Moreover, it would support the implementation of instruments to measure personal recovery in outcome monitoring.25
In this meta-analysis, we aim to investigate the strength of the relationship between clinical and personal recovery in patients with schizophrenia spectrum disorders. Because connectedness, hope, and empowerment have most consistently been identified as relevant categories of personal recovery, we will also assess the relationship between these concepts and clinical measures.13
Methods
Literature Search
A comprehensive online OvidSP database search was performed, including Embase, MEDLINE, PsycINFO, EBM Reviews, and the Ovid Nursing database from the inception of the individual databases to February 2017, without limits concerning publication status or language domain. The following search terms were used: (“schizophrenia” OR “psychosis” OR “psychotic disorder”) AND ((“recovery” AND (“personal” OR “subjective”)) OR (“connectedness” OR “hope” OR “empowerment”)). In addition, the reference lists of articles that met inclusion criteria were used for further study identification.
The title and abstract of each article were manually screened according to the following criteria: (1) the article possibly investigates the relationship between clinical and personal recovery, or between aspects of both; (2) the article includes quantitative data. After the screening, the full texts of the remaining studies were obtained.
Study Selection
To be considered for inclusion in the meta-analysis, studies had to meet the following inclusion criteria:
DSM diagnosis of schizophrenia spectrum disorder in >90% of the study sample. The current DSM-5 definition of the schizophrenia spectrum was used, which includes the following diagnoses: schizophrenia, schizoaffective disorder, schizophreniform disorder, brief psychotic disorder, and schizotypal (personality) disorder. The “other psychotic disorders,” including substance/medication-induced psychotic disorder, psychotic disorder due to another medical condition, catatonia, and other specified and unspecified schizophrenia spectrum and psychotic disorders were excluded.26
Clinical recovery was defined as severity of psychotic symptoms, measured with a valid clinical instrument, such as the Positive and Negative Syndrome Scale (PANSS); and/or as severity of emotional distress measured with a valid instrument such as the Calgary Depression Scale (CDS); and/or as functioning assessed with measures such as the GAF.
A valid measure was used to assess personal recovery (eg, Recovery Assessment Scale [RAS]), hope (eg, Beck Hopelessness Scale [BHS]), empowerment (eg, Empowerment Scale [ES]) or connectedness (eg, Social Connectedness Scale [SCS]).
Effect sizes or data that enabled effect size calculation or estimation were reported.
We excluded studies without original data (ie, articles which used the same patient sample), or not published in peer-reviewed journals (ie, reviews, conference abstracts, book chapters).
Data Collection and Items
Data were collected directly from the text, correlation matrixes, or other statistical tables from the included studies. Sample size, mean age, gender, primary diagnosis, country of origin of the study, clinical setting, stage of the disorder (early psychosis or chronic), the mean duration of illness, clinical outcome measure used, personal recovery measure used, and effect sizes of the relationships between clinical and personal measures were extracted. Unfortunately, most studies did not report on the phase of the disorder (ie, active or remission).
Risk of Bias in Studies and Study Quality
The methodological quality of individual studies was assessed by the Agency for Healthcare Research and Quality (AHRQ) assessment tool. This specific tool has been used in multiple reviews of observational studies.27–30 We used the version of the tool adapted by Taylor et al,31 which judges parameters such as sample selection, description of the cohort, and adequate reporting. We excluded 4 out of 10 items because these were only applicable for studies with comparison groups. We added 2 items, to assess whether the association between clinical and personal recovery was a primary or secondary outcome of the study, and to assess the method by which a diagnosis was made. This resulted in 8 items. For every study, we calculated a total quality score, see table 1.
Table 1.
Studies on the Relationship Between Clinical Recovery and Personal Recovery, Hope and Empowerment in Schizophrenia Spectrum Disorders
| Study | N | Age, Mean (SD) | Gender, %M/%F | Origin | Setting | Stage of Disorder | Duration of Illness in Years, Mean (SD) | Clinical Recovery Instrument | Personal Recovery Instrument | Quality Score (0–12) |
|---|---|---|---|---|---|---|---|---|---|---|
| Andresen et al25 | 110 | 39.5 (11.3) | 54/46 | Australia | Outpatient | Mixed | <5: 14.2% ≥5: 71.8% Unknown: 14.1 % |
HoNOS K-10 GAF | RAS, MHRM | 5 |
| Armstronget al32 | 795 | 54.3 (9.4) | 92/8 | USA | Outpatient | Chronic | ? | BPRS, GAF | MHRM | 8 |
| Berry et al33 | 325 | 37.9 (9.7) | 86.5/13.5 | UK | Outpatient | Chronic | 12.1 (0.24) | PANSS, GAF | MDES | 9 |
| Castelein et al21 | 50 | 31.4 (13) | 72/28 | Netherlands | Mixed | Mixed | 6.5 (6.3) | CAPE | ES, PES, MHCS | 10 |
| Cavelti et al34 | 156 | 44.5 (11.7) | 66/34 | Switzerland | Outpatient | Chronic | 17.9 (11.7) | PANSS, BDI CDS, GAF | RAS | 10 |
| Chou et al35 | 190 | 44.9 (11.6) | 50/50 | Taiwan | Outpatient | Chronic | 21.9 (10.4) | PSS | ES | 9 |
| Díaz-Mandado et al36 | 43 | 36.7 (8.1) | 74.4/25.6 | Spain | Outpatient | Chronic | 24.3 (6.6) | PANSS | RAS | 9 |
| Giusti et al24 | 76 | 45.8 (12.7) | 57.9/42.1 | Italy | Inpatient | Chronic | 20.5 (10.9) | PANSS, BPRS | RAS | 11 |
| Gottschalk37 | 23 | ? | ? | USA | ? | ? | ? | BPRS, HRSD | GHS | 7 |
| Hofer et al38 | Japan: 60 Austria: 52 |
J: 45.9 (10.0) A: 44.4 (10.7) |
J: 37/63 A: 52/48 |
Japan and Austria | Outpatient | Chronic | J: 18.9 (10.6) A: 15.4 (10.5) |
PANSS | BHS | 11 |
| Jahn et al39 | 169 | 51.9 (8.5) | 87.5/12.5 | USA | Outpatient | Chronic | Range: 3 or more | PANSS, BSI | MARS | 6 |
| Jørgensen et al40 | 101 | 37.5 (12.6) | 47/53 | Denmark | Outpatient | Chronic | 10 | PANSS | RAS | 9 |
| Kukla et al41 | 119 | 47.6 (8.8) | 74/26 | USA | Outpatient | ? | ? | PANSS | RAS, SHS | 9 |
| Kukla et al42 | 68 | 50.2 (11.0) | 94.1/5.9 | USA | Outpatient | Chronic | 20 | PANSS | RAS | 10 |
| Landeen et al43 | 55 | 34.9 | 75/25 | Canada | Outpatient | Chronic | 12.7 (range 2–26) | PANSS | MHS | 10 |
| Landeen et al44 | 70 | 31.1 (6.3) | 60/40 | Canada | Mixed | Chronic | 7.4 (4.7) | PANSS, BDI | MHS | 11 |
| Law et al45 | 335 | 36.0 (11.6) | 66.3/33.7 | UK | Mixed | Mixed | ? | PANSS, CDS | QPR, BHS | 8 |
| Law et al46 | 110 | 37.3 (11.6) | 69/31 | UK | Mixed | Mixed | ? | PANSS, GAF | QPR | 6 |
| Lecomte et al47 | 150 | 25.0 (6.4) | 61/39 | Canada | Outpatient | Early psychosis | Range: 0–2 | BPRS | LOT | 10 |
| Lysaker et al48 | 52 | 44 | 100/0 | USA | Outpatient | Chronic | 22 | PANSS | BHS (inverted) | 10 |
| Lysaker et al49 | 25 | 50.7 (10.2) | 96/4 | USA | Outpatient | Chronic | 25 | PANSS | STAND | 9 |
| Lysaker et al50 | 143 | 46.8 (9.6) | 92/8 | USA | Outpatient | Chronic | 20 | PANSS | BHS (inverted) | 10 |
| Macpherson et al51 | 403 | 44 (11) | 64/36 | UK | Outpatient | Chronic | 16 | BPRS, GAF | QPR, HHI, MHCS | 8 |
| Morrison et al52 | 122 | 35.5 (11.5) | 88/34 | UK | Mixed | Mixed | 3.1 | PANSS, HADS | QPR | 9 |
| Norman et al53 | 84 | 28 (7.4) | 69/31 | Canada | Outpatient | Early psychosis | 4.7 (3.7) | SAPS, SANS | RAS | 11 |
| Oliveira-Maia et al54 | 101 | 52.2 (13.8) | 76.2/23.8 | Portugal | Outpatient | Chronic | 24.4 (11.9) | GAF | MHRM | 8 |
| Resnick et al55 | 825 | 44.6 (12) | 71.6/28.4 | USA | Mixed | ? | ? | SCL-90 | “Recovery orientation, hope and empowerment” | 7 |
| Ringer et al56 | 52 | 46.6 (9.2) | 100/0 | USA | Outpatient | Chronic | 15 | PANSS | BHS | 9 |
| Roe et al23 | 159 | 43.2 (10.7) | 66.7/33.3 | Israel | Outpatient | Chronic | 20 | BPRS, GAF | RAS | 9 |
| Schrank et al57 | 200 | 40.3 (12.2) | 62.5/37.5 | Austria | Mixed | Chronic | 15.9 (12.6) | PANSS, ADS | IHS | 10 |
| Schrank et al58 | 284 | 39.9 (12.6) | 58.1/41.9 | Austria | Mixed | Chronic | 15.2 (12.8) | PANSS, ADS | IHS | 10 |
| Sibitz et al59 | 157 | 37.3 (11.9) | 54.5/45.5 | Austria | Mixed | Chronic | 13.6 (10.6) | ADS | ES | 9 |
| Snyder et al60 | 104 | ? | ? | USA | Inpatient | ? | ? | BSI, GAF | Several measures, including MHRM | 5 |
| Vass et al22 | 80 | 39.2 (11.6) | 61.3/38.7 | UK | Outpatient | Mixed | ? | PANSS | QPR BHS | 7 |
| Wciórka et al61 | 110 | 38.3 (11.4) | 39/61 | Poland | Mixed | Mixed | 13 (8.7) | BPRS, CDS | STORI | 9 |
| Wciórka et al62 | 110 | 38.3 (11.4) | 39/61 | Poland | Mixed | Mixed | 13 (10.4) | BPRS, CDS | ES | 9 |
| Wood and Irons63 | 52 | 37.0 (13.0) | 59.6/40.4 | UK | Mixed | Mixed | ? | PANSS, CDS | QPR | 7 |
Note: ADS, Allgemeine Depressionsskala: German version of the widely used CES-D (Center for Epidemiological Studies Depression Scale); BDI, Beck Depression Inventory; BHS, Beck Hopelessness Scale; BPRS, Brief Psychiatric Rating Scale; BSI, Brief Symptom Inventory; CAPE, Community Assessment of Psychic Experiences; CDS, Calgary Depression Scale; ES, Empowerment Scale; GAF, Global Assessment of Functioning; GHS, Gottschalk Hope Scale; HADS, Hospital Anxiety and Depression Scale; HHI, Herth Hope Index; HoNOS, Health of the Nation Outcome Scale; HRSD, Hamilton Rating Scale for Depression; IHS, Integrative Hope Scale; K-10, Kessler Psychological Distress Scale; LOT, Life Orientation Test; MARS, Maryland Assessment of Recovery in People With Serious Mental Illness; MDES, Making Decisions and Empowerment Scale; MHCS, Mental Health Confidence Scale; MHRM, Mental Health Recovery Measure; MHS, Miller Hope Scale; PANSS, Positive and Negative Syndrome Scale; PES, Personal Empowerment Scale; PSS, Psychiatric Symptoms Scale; QPR, Questionnaire about the Process of Recovery; RAS, Recovery Assessment Scale; SAPS, Scale for the Assessment of Positive Symptoms; SANS, Scale for the Assessment of Negative Symptoms; SCL-90, Symptom CheckList; SHS, Snyder Hope Scale; STAND, Scale to Assess Narrative Development; STORI, Stages of Recovery Instrument; ?, no data available.
Data Analysis
Effect Size Calculation.
To assess the strength of the relationship between measures of clinical and personal recovery, Pearson’s correlation coefficient r was used as the measure of effect size. According to Cohen, r = .10 is considered a small effect, explaining 1% of the total variance); r = .30 a medium effect, accounting for 9% of the total variance) and r = .50 a large effect, accounting for 25% of the variance.64
When correlation coefficients were not given, they were either calculated from reported data according to Lipsey and Wilson65 or estimated from reported standardized regression coefficients.
Regarding the personal recovery category of hope, the direction of the reported correlation coefficient was reversed wherever necessary, such that all included effect sizes represented the association between clinical recovery and hope, instead of hopelessness.
Integration of Dependent Effect Sizes.
To ensure that every study only contributed one effect size to the analysis, we calculated average effect sizes within one study if multiple effect sizes were reported on similar outcomes.66–68 This was the case if 2 or more measures were used to assess overall symptom severity, or (an aspect of) personal recovery. When studies only reported the outcome of assessed subscales and not of the total score, we averaged effect sizes of subscales to estimate an overall effect size. For example, reported correlation coefficients between personal recovery and positive symptoms, negative symptoms and general psychopathology of the PANSS were averaged, to calculate an overall correlation between personal recovery and symptom severity.
Meta-analysis Procedure.
To account for expected heterogeneity between studies, random-effects models according to Hedges and Vevea69 were calculated to obtain a combined effect weighted for sample size. The relationships between symptom severity on the one hand and personal recovery, hope, and empowerment, on the other hand, were investigated separately. In addition to the analyses of overall symptom severity, separate analyses were conducted for positive, negative, and affective symptoms and general functioning, if possible.
The presence of heterogeneity was evaluated by calculating the I2 metric, ie, the percentage of between-study variance due to systematic heterogeneity rather than chance.70 Data analysis was performed with SPSS version 23.71 Figures were plotted using comprehensive meta-analysis software.72
Heterogeneity was further explored by evaluating the effect of moderator variables. We were interested if estimated study quality as assessed with the AHRQ would affect reported effect sizes and/or cause heterogeneity. Furthermore, we planned to include age and illness duration or stage of illness as moderators. However, because the information was missing on these variables in a substantial part of the studies (table 1), only age could be added to the model. Meta-regression analyses were performed using SPSS 23 software, with macros provided by Lipsey and Wilson.65
Publication bias was examined by computing Rosenthal’s fail safe N and a funnel plot, which displays effect sizes plotted against the standard errors.67,73 Data points on the funnel plot are ideally evenly distributed around the mean effect size, with asymmetry suggesting a publication bias.
Results
Study Selection
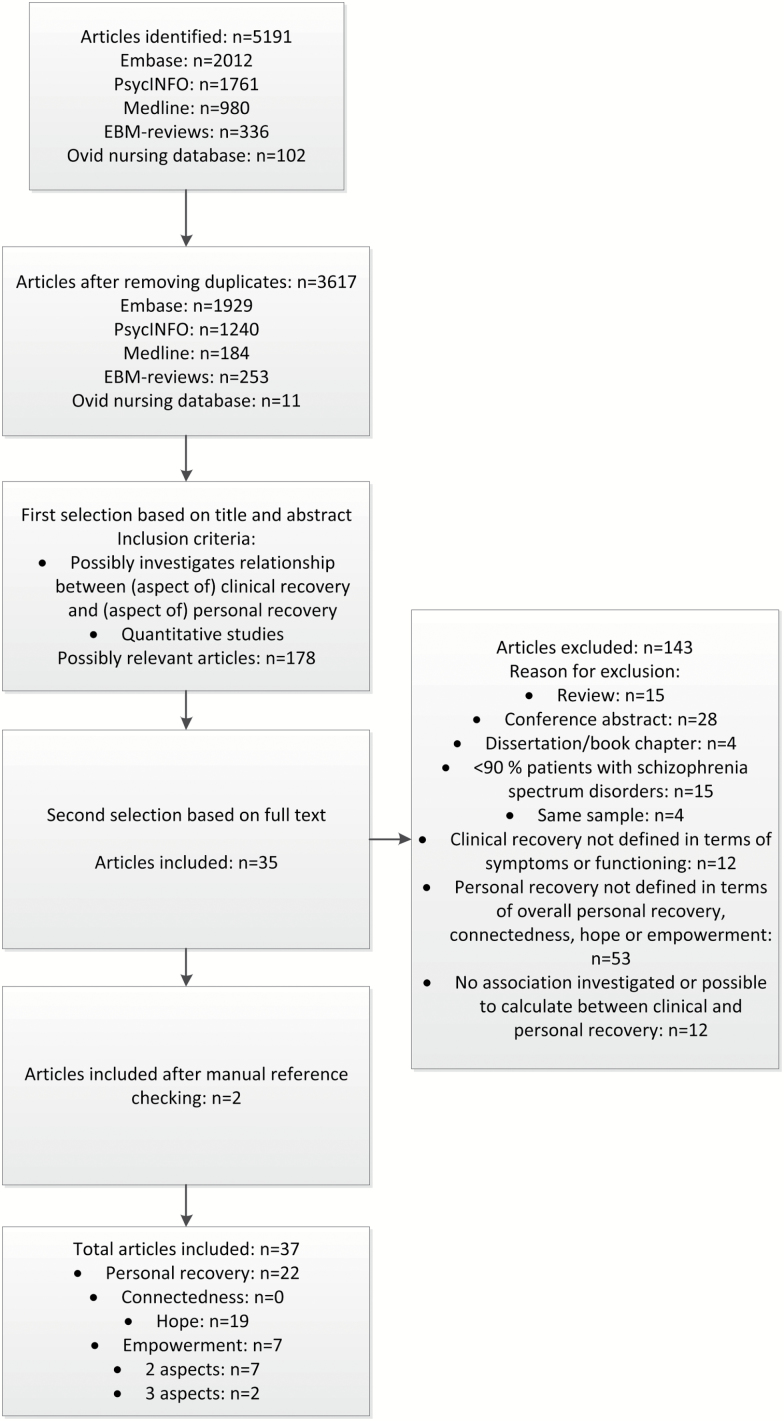
Figure 1 shows the flow chart of the process of selecting relevant articles. The literature search resulted in 5191 publications, of which 3617 remained after removal of duplicates. A total of 178 publications were selected on the basis of title and abstract. Eventually, 35 studies from the literature search were included. By reviewing the references of the included publications, we found an additional 2 relevant articles.25,51 Within the total of 37 included publications, 22 addressed overall personal recovery, 19 hope, and 7 empowerment. No relevant articles were found concerning connectedness. See table 1 for study characteristics.
Fig. 1.
Flow diagram study selection.
Results of the Meta-analysis
Clinical and Personal Recovery.
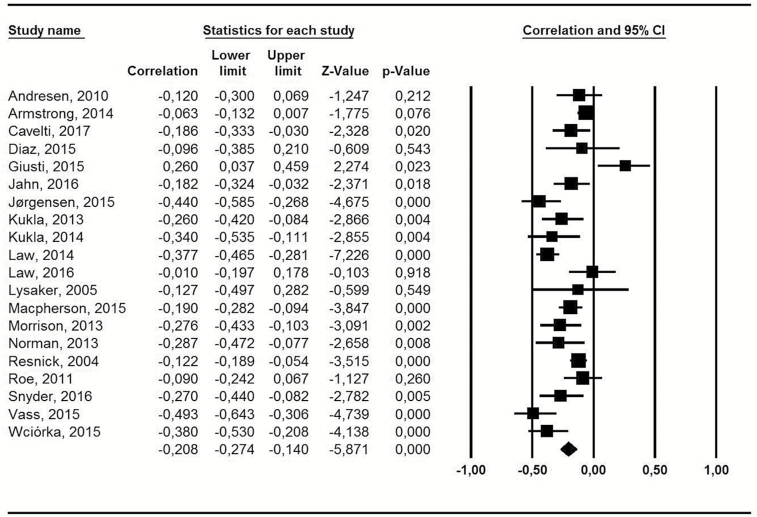
The meta-analysis that investigated the relationship between overall symptom severity and overall personal recovery in patients with schizophrenia spectrum disorders included 20 studies, with a total of 3994 participants, most of which were male (70.4%) and outpatients. The mean age was 42.4, with an age range from 28.0 to 54.3. One study did not report on gender and age.60 Individual sample sizes ranged from 25 to 825. Most studies reported on chronic patients, only one study specifically investigated early psychosis patients.53
The heterogeneity across studies was substantial (I2 = 75.8, 95% CI = 62.7–84.3).74 Random effect meta-analysis of the relationship between overall symptom severity and personal recovery revealed a significant mean weighted correlation coefficient of r = −.21 (95% CI = −0.27 to −0.14, P < .001) (supplementary table 1). This implies that patients with higher severity of overall psychopathology reported slightly lower personal recovery. Figure 2 shows the forest plot of effect sizes and 95% confidence intervals, as well as z and P values, which provide an indication of the statistical significance of the association.
Fig. 2.
Meta-analysis of the association between symptom severity and personal recovery.
Of the 20 studies, the majority reported on the association between personal recovery and different symptom domains: positive symptoms (k = 17, n = 3319), negative symptoms (k = 15, n = 2442), affective symptoms (k = 12, n = 2442). In addition to the association between personal recovery and overall psychopathology, we performed separate meta-analyses for all of these domains. The meta-analyses of positive and affective symptoms included one additional study, which only reported data on the association between these symptoms domains and personal recovery.63 One additional study only reported on the association between personal recovery and the GAF54 resulting in 8 studies which reported on the association with general functioning (n = 1938). Again, heterogeneity was substantial across studies assessing positive symptoms (I2 = 74.8, 95% CI = 59.3–84.3), negative symptoms (I2 = 76.7, 95% CI = 61.8–85.8), and affective symptoms (I2 = 84.5, 95% CI = 74.4–90.6). Random effect meta-analyses revealed a significant negative mean weighted effect size for positive symptoms r = −.20 (95% CI = −0.27 to −0.12, P < .001), negative symptoms r = −.24 (95% CI = −0.33 to −0.15, P < .001) and affective symptoms r = −.34 (95% CI = −0.44 to −0.24, P < .001). A small significant positive effect size was found for the association with general functioning r = .21 (95% CI = −0.09 to 0.32, P < .001) ( supplementary table 1).
Meta-regression Analysis
We conducted a meta-regression analysis to evaluate if age or study quality potentially explained differences in reported effect sizes among studies and caused heterogeneity. A nonsignificant tendency for age to correlate with the effect size (B = .010, SE = .005, P = .056) was found and no effect for study quality. Together they only explained 14.5% of the variation between studies.
Furthermore, no significant moderation effects were found in meta-regression analyses conducted for the different symptom domains. Differences in age and study quality explained 27.6% of the variation observed in the association with positive symptoms, 6.2% for negative symptoms, and 29.8% for affective symptoms.
Sensitivity Analysis
Rosenthal Fail-Safe N = 913 suggests that there would need to exist more than 900 negative unpublished studies to turn the estimated significant population effect-size into a nonsignificant result. The funnel plot does not indicate publication bias (supplementary material).
Clinical Recovery and Hope.
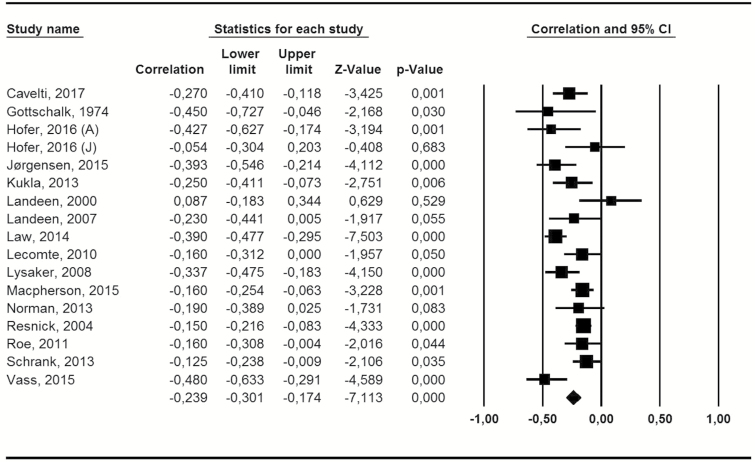
Seventeen studies were included in the meta-analysis of the relationship between overall symptom severity and hope, with one publication included twice, because it reported on 2 studies in different populations (in Austria and Japan). Three thousand ninety-nine participants were analyzed, most were male (60.1%) and outpatients. The mean age was 37.2. One study did not report on gender and age.37 The majority of studies mainly included patients with longer duration of psychosis, only 2 specifically investigated patients with early psychosis.47,53
Heterogeneity across studies was substantial (I2 = 64.9, 95% CI = 41.2–79.0). Results showed a significant mean weighted correlation coefficient of r = −.24 (95% CI = −0.30 to −0.187, P < .001) (supplementary table 1). Figure 3 shows the forest plot of effect sizes and 95% confidence intervals for the association between overall symptom severity and hope in the included individual studies.
Fig. 3.
Meta-analysis of the association between symptom severity and hope.
Subsequently, meta-analyses of the 3 separate symptom domains positive symptoms (k = 12, n = 2364), negative symptoms (k = 11, n = 1539), and affective symptoms (k = 14, n = 2669) were conducted. The meta-analyses of affective symptoms included 3 additional studies, which only reported data on the association between hope and affective symptoms.48,56,57 Again, heterogeneity between studies included in these analyses was substantially high for positive symptoms (I2 = 77.4, 95% CI = 60.7–87.0) and affective symptoms (I2 = 81.7, 95% CI = 70.4–88.7). Results showed significant negative mean weighted effect sizes for positive symptoms r = −.14 (95% CI = −0.23 to −0.05, P = .004), negative symptoms r = −.26 (95% CI = −0.32 to −0.19, P < .001), and affective symptoms r = −.43 (95% CI = −0.51 to −0.35, P < .001). There were not enough studies to conduct a meta-analysis of general functioning.
Meta-regression Analysis
Meta-regression analyses, which integrated age and study quality as potential predictors of the heterogeneity between studies, showed no significant effects. Together they only explained 4.7% of the variation observed regarding overall symptom severity, 25.4% regarding positive symptoms, 9.0% in the association with negative symptoms, and 17.4% in affective symptoms.
Sensitivity Analysis
Rosenthal Fail-Safe N = 869 suggests that there would need to be more than 800 negative unpublished studies included in the meta-analysis to result in a nonsignificant population effect size. The funnel plot does not suggest publication bias (supplementary material).
Clinical Recovery and Empowerment.
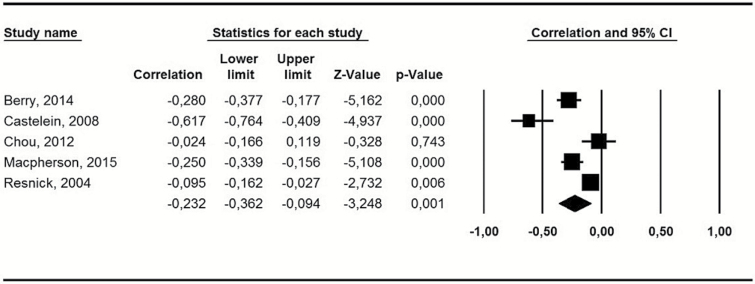
Seven studies investigated the relationship between symptom severity and empowerment. Five of 7 studies (n = 1793) could be included in the meta-analysis, since in 2 studies it was not possible to calculate an effect size of the relationship between overall psychopathology and empowerment.59,62 Of the 1793 participants, most were male (68.8%) and outpatients. The mean age was 40.6. All studies reported mainly on patients with longer duration of psychosis.
Again, heterogeneity across studies was substantial (I2 = 86.7, 95% CI = 71.2–93.9, Q = 30.1, P > .001). The random effect meta-analysis revealed a significant mean weighted correlation coefficient of r = −.23 (95% CI = −0.36 to −0.09, P < .001). Figure 4 shows the forest plot of individual effect sizes and 95% confidence intervals for the association between overall symptom severity and empowerment. Due to the small number of included studies, no additional subsample analyses regarding different symptom domains and functioning, or meta-regression analyses were conducted.
Fig. 4.
Meta-analysis of the association between symptom severity and empowerment.
Sensitivity Analysis
Rosenthal Fail-Safe N = 118 suggests that there would need to be more than 100 negative unpublished studies included in the meta-analysis to result in a nonsignificant population effect size. The funnel plot does not suggest publication bias (supplementary material).
Discussion
Main Findings
To our knowledge, this is the first meta-analysis investigating the relationship between clinical and personal recovery. Results show that there is only a small to medium negative correlation between symptom severity and personal recovery in patients with schizophrenia spectrum disorders. This also is the case for the relationship between symptom severity and hope and empowerment, 2 important categories of personal recovery processes.13 No studies have been found considering the relationship between symptom severity and connectedness, the third category of personal recovery. When subdomains of clinical recovery are taken into consideration, it becomes apparent that affective symptoms show a medium strength correlation with personal recovery and hope. Positive and negative symptoms demonstrate a small to medium association with personal recovery and hope. Moreover, only a small positive association was found between general functioning, as measured with the GAF, and personal recovery. Previous studies on the relationship of clinical outcome with subjective quality of life, a concept related to personal recovery, show a similar modest correlation and also strengthen the importance of affective symptoms within this association.75,76
In the current meta-analysis, heterogeneity of the studies was substantial. Furthermore, a tendency of a moderating effect of age was found in meta-regression analyses: the younger the patient, the higher the negative correlation between symptom severity and personal recovery. Lastly, the sensitivity analysis suggests that the risk of publication bias is low.
Implications
Implications for Clinical Practice.
Given the small to medium association between overall symptom severity and personal recovery, explicit attention for personal recovery within treatment could better fit the needs of patients. Besides that, our findings suggest that current outcome measures in clinical practice, which mainly focus on symptom remission and functioning,25 should be extended to include personal recovery.
Our findings highlight the relative importance of affective symptoms for personal recovery. This is in line with studies of patients with affective disorders.77–79 A key component of depression is that everything is perceived as pointless and hope is lost. The question is whether treatment of affective symptoms will promote personal recovery, or that promoting personal recovery, in general, will relieve feelings of depression.
On the other hand, this meta-analysis shows that positive symptoms were only slightly related to personal recovery. This may imply that an emphasis on reducing positive symptoms might not result in improved personal recovery.
Although few studies were found that investigated the relationship between general functioning and personal recovery, the results show a small correlation between these 2 outcomes (r = .21). This is remarkable because one would expect that better functioning, for instance having a house, work and relationships would increase the perceived level of recovery. A possible explanation is that the GAF is scored by the professional and personal recovery by the patient. Possibly, the GAF does not reflect important aspects of functioning from the perspective of patients. Also, symptom and functioning ratings are both part of the GAF and it is known from the literature that GAF ratings are highly correlated with ratings of symptoms in schizophrenia.80 A higher correlation (r = .36) between personal recovery and social functioning, measured by the social functioning scale (SFS) has been found.81
Several empirically validated personal recovery-oriented practices have already been developed, eg, peer support workers, wellness recovery action planning, recovery colleges, and mental health trialogues, but implementation in mental health systems, remains limited.82 To make recovery-oriented practices a success, professional and organizational commitment toward supporting subjective outcome measures such as personal recovery is needed. The relative emphasis of the evidence-based medicine paradigm on objective (clinical) outcomes,83 possibly together with an implicit idea that individuals with mental health problems do not qualify as equal partners in the evaluation of treatment, might have been the reason that earlier findings of a small relationship between objective and subjective domains of outcome have not resulted in implementation of effective practices on a larger scale.82
Implications for Future Research.
Clinical, as well as personal recovery, change over time. Because most of the selected studies did not investigate these concepts longitudinally, the current meta-analyses focused on cross-sectional associations. Longitudinal research gives additional information about the process of personal recovery and whether or not this relates to the reduction of symptoms and if so, which symptoms in particular. It would also be possible to investigate how clinical recovery changes according to stages of recovery.12,84 Few studies have been performed to investigate changes in personal recovery and symptom severity over time. Some studies showed no correlation between the changes of personal recovery scales and symptom-focused scales60,85 and others showed that there is some degree of alignment between clinical and personal outcomes.22,40,46,51 Similar to what was found in the current cross-sectional meta-analysis, affective symptoms were more strongly associated with personal recovery over time than psychotic symptoms.40,46 More studies are needed to understand the longitudinal interaction between clinical and personal recovery.
Because some studies did not report the stage of the disorder of the subjects included and only 2 studies were found that explicitly investigated patients with early psychosis, it was not possible to integrate stage of disorder in the meta-regression analyses. Because age showed a tendency to correlate with the effect size, it is imaginable that the stage of the disorder would also play a role. In future research, it would be helpful to investigate the relationship between clinical and personal recovery in homogeneous groups of early and chronic patients to evaluate the potential difference between these groups of patients.
The few studies that investigated the relationship between personal recovery and functioning used the GAF. This general measure might not be the best fit to assess functional outcome (see Implications for clinical practice section). For future research, agreement about the instrument best suitable to measure functional recovery is needed.86
Cognitive deficits are an important aspect of schizophrenia.87 Although a consensus measure for cognitive deficits in schizophrenia is available,88 the 3 studies we found on the relationship between cognition and personal recovery used heterogeneous measures. In future research on personal recovery and cognition, consistent application of the consensus measure is needed.89–91
Furthermore, international agreement concerning a measure to evaluate personal recovery is necessary. This starts with the definition of personal recovery and which aspects are most important to measure. We would suggest using the CHIME-framework of Leamy et al as a basis of this definition.13,14 According to existing evidence, the RAS seems to be a good choice as a personal recovery scale for regular use, because it was developed with patient involvement, maps relatively well on the CHIME-framework, appears to be sensitive to change over time, is easy to administer and shows good internal consistency (α = .70–.93), test–retest reliability, and interrater reliability.16,17,19,92–94
Our findings imply that patients, who still experience symptoms might nevertheless report good personal recovery. This results in the question which factors are specifically helpful to achieve personal recovery. Building on existing research on the domains of personal recovery, qualitative studies asking patients what exactly was helpful for their personal recovery, could provide useful information on the ingredients of interventions in clinical and other domains that promote personal recovery.14,15,95
Limitations
A first limitation is the application of a specific definition of personal recovery, which limits the generalizability of our results to otherwise defined concepts of personal recovery. Besides the CHIME framework, mentioned in the introduction, several other concepts are used, such as resilience, self-determination, self-esteem, stigma, spirituality, and life-satisfaction.13 Furthermore, we are not able to report on the relationship between clinical recovery and 2 aspects of CHIME, “identity” and “meaning,” as we chose to confine our search to the processes of personal recovery most frequently named by patients.13 The values of I2 indicate substantial heterogeneity of included studies, which probably reflects the use of multiple measures of personal recovery with different operationalisations of the concept,16 and/or heterogeneity in the study population.
To avoid the problem that multiple dependent effect sizes from the same study could potentially bias the results, we calculated an average effect size within each study before analyses.67,73 Although this method of calculating a simple mean effect size to summarize a set of nonindependent effect sizes is commonly applied, this procedure may have led to over- of underestimation, especially in case of small correlations between averaged outcome measures.96 We tried to partially account for this problem by reporting separate meta-analysis for the different symptom domains.
Another limitation relates to the possible negative association between insight and personal recovery. Interestingly, one study found a positive association between severity of psychopathology and personal recovery, whereas a negative correlation was reported between personal recovery and cognitive insight and self-reflectiveness. The authors conclude that perception of personal recovery is correlated with a lower awareness of symptomatology, which they call a “cognitive trap.”24 Apparently, patients can consider themselves recovered and lead a fulfilling life, while not being aware of symptoms. However, some patients consider acknowledging and accepting illness as an important step in their recovery process.95
Because study quality was variable, we investigated a possible effect in the meta-regression analyses, but did not find a significant confounding effect.
Because only a few studies were found on the link between symptom severity and empowerment and between general functioning and personal recovery, the results on these subjects must be interpreted with caution.
Conclusion
Overall, the association between clinical and personal recovery is small to medium. Our meta-analysis shows that symptom severity only partially explains personal recovery. Moreover, psychotic symptoms are moderately associated with personal recovery, while affective symptoms are more closely linked to personal recovery. Therefore, clinical and personal recovery need their own attention in treatment and outcome monitoring of patients with schizophrenia spectrum disorders, with a special focus on the interaction between affective symptoms and personal recovery.
Supplementary Material
Supplementary data are available at Schizophrenia Bulletin online.
Supplementary Material
Acknowledgments
The authors have declared that there are no conflicts of interest in relation to the subject of this study.
References
- 1. Schrank B, Slade M. Recovery in psychiatry. Psychiatr Bull. 2007;31:321–325. [Google Scholar]
- 2. Slade M, Amering M, Oades L. Recovery: an international perspective. Epidemiol Psichiatr Soc. 2008;17:128–137. [DOI] [PubMed] [Google Scholar]
- 3. Bellack AS. Scientific and consumer models of recovery in schizophrenia: concordance, contrasts, and implications. Schizophr Bull. 2006;32:432–442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Andreasen NC, Carpenter WT Jr, Kane JM, Lasser RA, Marder SR, Weinberger DR. Remission in schizophrenia: proposed criteria and rationale for consensus. Am J Psychiatry. 2005;162:441–449. [DOI] [PubMed] [Google Scholar]
- 5. Liberman RP, Kopelowicz A, Ventura J, Gutkind D. Operational criteria and factors related to recovery from schizophrenia. Int Rev Psychiatry. 2002;14:256–272. [Google Scholar]
- 6. Torgalsbøen A. What is recovery in schizophrenia? In: Provencher HL, Keyes CLM, eds. Severe Mental Illness, Research Evidence and Implications for Practice. Boston, MA: Boston University; 2013:302–315. [Google Scholar]
- 7. Deegan PE. Recovery as a self-directed process of healing and transformation. Occup Ther Ment Health. 2002;17:5–21. [Google Scholar]
- 8. Mead S, Copeland ME. What recovery means to us: consumers’ perspectives. Community Ment Health J. 2000;36:315–328. [DOI] [PubMed] [Google Scholar]
- 9. Anthony WA. Recovery from mental illness: the guiding vision of the mental health service system in the 1990s. Psychosocial Rehabil J. 1993;16:11–23. [Google Scholar]
- 10. Lysaker PH, Roe D, Buck KD. Recovery and wellness amidst schizophrenia: definitions, evidence, and the implications for clinical practice. J Am Psychiatr Nurses Assoc. 2010;16:36–42. [DOI] [PubMed] [Google Scholar]
- 11. Slade M. Personal Recovery and Mental Illness. A Guide for Mental Health Professionals. Cambridge, UK: Cambridge University Press; 2009. [Google Scholar]
- 12. Andresen R, Oades L, Caputi P. The experience of recovery from schizophrenia: towards an empirically validated stage model. Aust N Z J Psychiatry. 2003;37:586–594. [DOI] [PubMed] [Google Scholar]
- 13. Leamy M, Bird V, Le Boutillier C, Williams J, Slade M. Conceptual framework for personal recovery in mental health: systematic review and narrative synthesis. Br J Psychiatry. 2011;199:445–452. [DOI] [PubMed] [Google Scholar]
- 14. Bird V, Leamy M, Tew J, Le Boutillier C, Williams J, Slade M. Fit for purpose? Validation of a conceptual framework for personal recovery with current mental health consumers. Aust N Z J Psychiatry. 2014;48:644–653. [DOI] [PubMed] [Google Scholar]
- 15. Law H, Morrison AP. Recovery in psychosis: a Delphi study with experts by experience. Schizophr Bull. 2014;40:1347–1355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Shanks V, Williams J, Leamy M, Bird VJ, Le Boutillier C, Slade M. Measures of personal recovery: a systematic review. Psychiatr Serv. 2013;64:974–980. [DOI] [PubMed] [Google Scholar]
- 17. Law H, Morrison A, Byrne R, Hodson E. Recovery from psychosis: a user informed review of self-report instruments for measuring recovery. J Ment Health. 2012;21:192–207. [DOI] [PubMed] [Google Scholar]
- 18. Burgess P, Pirkis J, Coombs T, Rosen A. Assessing the value of existing recovery measures for routine use in Australian mental health services. Aust N Z J Psychiatry. 2011;45:267–280. [DOI] [PubMed] [Google Scholar]
- 19. Sklar M, Groessl EJ, O’Connell M, Davidson L, Aarons GA. Instruments for measuring mental health recovery: a systematic review. Clin Psychol Rev. 2013;33:1082–1095. [DOI] [PubMed] [Google Scholar]
- 20. Schrank B, Bird V, Rudnick A, Slade M. Determinants, self-management strategies and interventions for hope in people with mental disorders: systematic search and narrative review. Soc Sci Med. 2012;74:554–564. [DOI] [PubMed] [Google Scholar]
- 21. Castelein S, van der Gaag M, Bruggeman R, van Busschbach JT, Wiersma D. Measuring empowerment among people with psychotic disorders: a comparison of three instruments. Psychiatr Serv. 2008;59:1338–1342. [DOI] [PubMed] [Google Scholar]
- 22. Vass V, Morrison AP, Law H et al. How stigma impacts on people with psychosis: the mediating effect of self-esteem and hopelessness on subjective recovery and psychotic experiences. Psychiatry Res. 2015;230:487–495. [DOI] [PubMed] [Google Scholar]
- 23. Roe D, Mashiach-Eizenberg M, Lysaker PH. The relation between objective and subjective domains of recovery among persons with schizophrenia-related disorders. Schizophr Res. 2011;131:133–138. [DOI] [PubMed] [Google Scholar]
- 24. Giusti L, Ussorio D, Tosone A et al. Is personal recovery in schizophrenia predicted by low cognitive insight?Community Ment Health J. 2015;51:30–37. [DOI] [PubMed] [Google Scholar]
- 25. Andresen R, Caputi P, Oades LG. Do clinical outcome measures assess consumer-defined recovery?Psychiatry Res. 2010;177:309–317. [DOI] [PubMed] [Google Scholar]
- 26. Schizophrenia Spectrum and Other Psychotic Disorders. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. American Psychiatric Association; 2013. [Google Scholar]
- 27. Williams JW, Plassman BL, Burke J, Benjamin S. Preventing Alzheimer’s disease and cognitive decline. Evid Rep Technol Assess. 2010:1–727. [PMC free article] [PubMed] [Google Scholar]
- 28. Wang C, Chung M, Lichtenstein A et al. Effects of omega-3 fatty acids on cardiovascular disease. Evid Rep Technol Assess. 2004:1–8. [PMC free article] [PubMed] [Google Scholar]
- 29. Myers ER, McCrory DC, Mills AA, Price TM, Swamy GK, Tantibhedhyangkul J, Wu JM, Matchar DB. Effectiveness of assisted reproductive technology (ART). Evid Rep Technol Assess. 2008:1–195. [PMC free article] [PubMed] [Google Scholar]
- 30. Dudley R, Taylor P, Wickham S, Hutton P. Psychosis, delusions and the “jumping to conclusions” reasoning bias: a systematic review and meta-analysis. Schizophr Bull. 2016;42:652–665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Taylor P, Hutton P, Dudley R. Rationale and protocol for a systematic review and meta-analysis on reduced data gathering in people with delusions. Syst Rev. 2014;3:44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Armstrong NP, Cohen AN, Hellemann G, Reist C, Young AS. Validating a brief version of the Mental Health Recovery Measure for individuals with schizophrenia. Psychiatr Serv. 2014;65:1154–1159. [DOI] [PubMed] [Google Scholar]
- 33. Berry K, Allott R, Emsley R, Ennion S, Barrowclough C. Perceived empowerment in people with a dual diagnosis of schizophrenia spectrum disorder and substance misuse. Soc Psychiatry Psychiatr Epidemiol. 2014;49:377–384. [DOI] [PubMed] [Google Scholar]
- 34. Cavelti M, Wirtz M, Corrigan P, Vauth R. Recovery assessment scale: examining the factor structure of the German version (RAS-G) in people with schizophrenia spectrum disorders. Eur Psychiatry. 2017;41:60–67. [DOI] [PubMed] [Google Scholar]
- 35. Chou KR, Shih YW, Chang C et al. Psychosocial rehabilitation activities, empowerment, and quality of community-based life for people with schizophrenia. Arch Psychiatr Nurs. 2012;26:285–294. [DOI] [PubMed] [Google Scholar]
- 36. Díaz-Mandado O, Nieto-Moreno M, Montorio I, Periáñez JA. Predictores de recuperación subjetiva en la esquizofrenia. Revista de Psicopatología y Psicología Clínica. 2015;20:14. [Google Scholar]
- 37. Gottschalk LA. A Hope scale applicable to verbal samples. Arch Gen Psychiatry. 1974;30:779–785. [DOI] [PubMed] [Google Scholar]
- 38. Hofer A, Mizuno Y, Frajo-Apor B et al. Resilience, internalized stigma, self-esteem, and hopelessness among people with schizophrenia: cultural comparison in Austria and Japan. Schizophr Res. 2016;171:86–91. [DOI] [PubMed] [Google Scholar]
- 39. Jahn DR, DeVylder JE, Drapalski AL, Medoff D, Dixon LB. Personal recovery as a protective factor against suicide ideation in individuals with schizophrenia. J Nerv Mental Dis. 2016;204:827–831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Jørgensen R, Zoffmann V, Munk-Jørgensen P et al. Relationships over time of subjective and objective elements of recovery in persons with schizophreni. Psychiatry Res. 2015;228:14–19. [DOI] [PubMed] [Google Scholar]
- 41. Kukla M, Salyers MP, Lysaker PH. Levels of patient activation among adults with schizophrenia: associations with hope, symptoms, medication adherence, and recovery attitudes. J Nerv Ment Dis. 2013;201:339–344. [DOI] [PubMed] [Google Scholar]
- 42. Kukla M, Lysaker PH, Roe D. Strong subjective recovery as a protective factor against the effects of positive symptoms on quality of life outcomes in schizophrenia. Compr Psychiatry. 2014;55:1363–1368. [DOI] [PubMed] [Google Scholar]
- 43. Landeen J, Pawlick J, Woodside H, Kirkpatrick H, Byrne C. Hope, quality of life and symptom severity in individuals with schizophrenia. Psychiatr Rehabil J 2000;23:364–369. [Google Scholar]
- 44. Landeen JL, Seeman MV, Goering P, Streiner D. Schizophrenia: effect of perceived stigma on two dimensions of recovery. Clin Schizophr Relat Psychoses 2007;1:64–68. [Google Scholar]
- 45. Law H, Neil ST, Dunn G, Morrison AP. Psychometric properties of the questionnaire about the process of recovery (QPR). Schizophr Res. 2014;156:184–189. [DOI] [PubMed] [Google Scholar]
- 46. Law H, Shryane N, Bentall RP, Morrison AP. Longitudinal predictors of subjective recovery in psychosis. Br J Psychiatry. 2016;209:48–53. [DOI] [PubMed] [Google Scholar]
- 47. Lecomte T, Corbiere M, Theroux L. Correlates and predictors of optimism in individuals with early psychosis or severe mental illness. Psychosis. 2010;2:122–133. [Google Scholar]
- 48. Lysaker PH, Davis LW, Hunter NL. Neurocognitive, social and clinical correlates of two domains of hopelessness in schizophrenia. Schizophr Res. 2004;70:277–285. [DOI] [PubMed] [Google Scholar]
- 49. Lysaker PH, Wickett A, Davis LW. Narrative qualities in schizophrenia: associations with impairments in neurocognition and negative symptoms. J Nerv Ment Dis. 2005;193:244–249. [DOI] [PubMed] [Google Scholar]
- 50. Lysaker PH, Salyers MP, Tsai J, Spurrier LY, Davis LW. Clinical and psychological correlates of two domains of hopelessness in schizophrenia. J Rehabil Res Dev. 2008;45:911–919. [DOI] [PubMed] [Google Scholar]
- 51. Macpherson R, Pesola F, Leamy M et al. The relationship between clinical and recovery dimensions of outcome in mental health. Schizophr Res. 2016;175:142–147. [DOI] [PubMed] [Google Scholar]
- 52. Morrison AP, Shryane N, Beck R et al. Psychosocial and neuropsychiatric predictors of subjective recovery from psychosis. Psychiatry Res. 2013;208:203–209. [DOI] [PubMed] [Google Scholar]
- 53. Norman RM, Windell D, Lynch J, Manchanda R. Correlates of subjective recovery in an early intervention program for psychoses. Early Interv Psychiatry. 2013;7:278–284. [DOI] [PubMed] [Google Scholar]
- 54. Oliveira-Maia AJ, Mendonça C, Pessoa MJ, Camacho M, Gago J. The mental health recovery measure can be used to assess aspects of both customer-based and service-based recovery in the context of severe mental illness. Front Psychol. 2016;7:1679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Resnick SG, Rosenheck RA, Lehman AF. An exploratory analysis of correlates of recovery. Psychiatr Serv. 2004;55:540–547. [DOI] [PubMed] [Google Scholar]
- 56. Ringer JM, Buchanan EE, Olesek K, Lysaker PH. Anxious and avoidant attachment styles and indicators of recovery in schizophrenia: associations with self-esteem and hope. Psychol Psychother. 2014;87:209–221. [DOI] [PubMed] [Google Scholar]
- 57. Schrank B, Woppmann A, Grant Hay A, Sibitz I, Zehetmayer S, Lauber C. Validation of the integrative hope scale in people with psychosis. Psychiatry Res. 2012;198:395–399. [DOI] [PubMed] [Google Scholar]
- 58. Schrank B, Amering M, Hay AG, Weber M, Sibitz I. Insight, positive and negative symptoms, hope, depression and self-stigma: a comprehensive model of mutual influences in schizophrenia spectrum disorders. Epidemiol Psychiatr Sci. 2014;23:271–279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Sibitz I, Amering M, Unger A et al. The impact of the social network, stigma and empowerment on the quality of life in patients with schizophrenia. Eur Psychiatry. 2011;26:28–33. [DOI] [PubMed] [Google Scholar]
- 60. Snyder M, Young S, Schactman L. Early dynamics of recovery from psychotic spectrum disorder within a therapeutic recovery community: patterns and dynamics. Psychosis. 2016;8:23–36. [Google Scholar]
- 61. Wciórka J, Świtaj P, Anczewska M. The stages of recovery in relation to the other subjective and objective aspects of psychosis. Psychiatry Res. 2015;225:613–618. [DOI] [PubMed] [Google Scholar]
- 62. Wciórka J, Switaj P, Anczewska M. The sense of empowerment in the early stage of recovery from psychosis. Psychosis. 2015;7:249–260. [Google Scholar]
- 63. Wood L, Irons C. Exploring the associations between social rank and external shame with experiences of psychosis. Behav Cogn Psychother. 2015;44:527–538. [DOI] [PubMed] [Google Scholar]
- 64. Cohen J. A power primer. Psychol Bull. 1992;112:155–159. [DOI] [PubMed] [Google Scholar]
- 65. Lipsey MW, Wilson DB.. Practical Meta-Analysis . Thousand Oaks, CA: SAGE Publications, Inc; 2000. [Google Scholar]
- 66. Hedges LV, Olkin I.. Statistical Methods for Meta-analysis. Orlando, FL: Academic Press; 1985. [Google Scholar]
- 67. Rosenthal R. Meta-analytic Procedures for Social Research. 2nd ed. Newbury Park, CA: Sage; 1991. [Google Scholar]
- 68. Turner HM, Bernard RM. Calculating and synthesizing effect sizes. Contemp Issues Commun Sci Disord. 2006;33:42–55. [Google Scholar]
- 69. Hedges LV, Vevea JL. Fixed- and random-effects models in meta-analysis. Psychol Methods. 1998;3:486–504. [Google Scholar]
- 70. Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–1558. [DOI] [PubMed] [Google Scholar]
- 71. IBM SPSS Statistics for Windows, Version 23.0 [computer program]. Armonk, NY: IBM Corp; 2015. [Google Scholar]
- 72. Comprehensive Meta-analysis Software [computer program]. Version 2. Englewood, NJ: Biostat. [Google Scholar]
- 73. Field AP, Gillett R. How to do a meta-analysis. Br J Math Stat Psychol. 2010;63:665–694. [DOI] [PubMed] [Google Scholar]
- 74. Higgins JPT, Green S. 9.5.2 Identifying and measuring heterogeneity. In: Cochrane Handbook for Systematic Reviews of Interventions. Version 5.1.0. London, UK: The Cochrane Collaboration; 2011. [Google Scholar]
- 75. Priebe S, McCabe R, Junghan U et al. Association between symptoms and quality of life in patients with schizophrenia: a pooled analysis of changes over time. Schizophr Res. 2011;133:17–21. [DOI] [PubMed] [Google Scholar]
- 76. Eack SM, Newhill CE. Psychiatric symptoms and quality of life in schizophrenia: a meta-analysis. Schizophr Bull. 2007;33:1225–1237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Brown C, Rempfer M, Hamera E. Correlates of insider and outsider conceptualizations of recovery. Psychiatr Rehabil J. 2008;32:23–31. [DOI] [PubMed] [Google Scholar]
- 78. Shahar G, Davidson L. Depressive symptoms erode self-esteem in severe mental illness: a three-wave, cross-lagged study. J Consult Clin Psychol. 2003;71:890–900. [DOI] [PubMed] [Google Scholar]
- 79. Aloba O, Akinsulore A, Mapayi B et al. The Yoruba version of the Beck Hopelessness Scale: psychometric characteristics and correlates of hopelessness in a sample of Nigerian psychiatric outpatients. Compr Psychiatry. 2015;56:258–271. [DOI] [PubMed] [Google Scholar]
- 80. Startup M, Jackson MC, Bendix S. The concurrent validity of the Global Assessment of Functioning (GAF). Br J Clin Psychol. 2002;41:417–422. [DOI] [PubMed] [Google Scholar]
- 81. Drapalski AL, Medoff D, Dixon L, Bellack A. The reliability and validity of the Maryland Assessment of Recovery in Serious Mental Illness Scale. Psychiatry Res. 2016;239:259–264. [DOI] [PubMed] [Google Scholar]
- 82. Slade M, Amering M, Farkas M et al. Uses and abuses of recovery: implementing recovery-oriented practices in mental health systems. World Psychiatry. 2014;13:12–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Faulkner A, Thomas P. User-led research and evidence-based medicine. Br J Psychiatry. 2002;180:1–3. [DOI] [PubMed] [Google Scholar]
- 84. Spaniol L, Wewiorski NJ, Gagne C, Anthony WA. The process of recovery from schizophrenia. Int Rev Psychiatry. 2002;14:327–336. [Google Scholar]
- 85. Cavelti M, Homan P, Vauth R. The impact of thought disorder on therapeutic alliance and personal recovery in schizophrenia and schizoaffective disorder: an exploratory study. Psychiatry Res. 2016;239:92–98. [DOI] [PubMed] [Google Scholar]
- 86. Mausbach BT, Moore R, Bowie C, Cardenas V, Patterson TL. A review of instruments for measuring functional recovery in those diagnosed with psychosis. Schizophr Bull. 2009;35:307–318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Kahn RS, Keefe RS. Schizophrenia is a cognitive illness: time for a change in focus. JAMA Psychiatry. 2013;70:1107–1112. [DOI] [PubMed] [Google Scholar]
- 88. Velligan DI, Fredrick M, Mintz J et al. The reliability and validity of the MATRICS functional assessment battery. Schizophr Bull. 2014;40:1047–1052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Green MF, Nuechterlein KH, Gold JM et al. Approaching a consensus cognitive battery for clinical trials in schizophrenia: the NIMH-MATRICS conference to select cognitive domains and test criteria. Biol Psychiatry. 2004;56:301–307. [DOI] [PubMed] [Google Scholar]
- 90. Green MF, Schooler NR, Kern RS et al. Evaluation of functionally meaningful measures for clinical trials of cognition enhancement in schizophrenia. Am J Psychiatry. 2011;168:400–407. [DOI] [PubMed] [Google Scholar]
- 91. Nuechterlein KH, Green MF, Kern RS et al. The MATRICS Consensus Cognitive Battery, part 1: test selection, reliability, and validity. Am J Psychiatry. 2008;165:203–213. [DOI] [PubMed] [Google Scholar]
- 92. Corrigan PW, Salzer M, Ralph RO, Sangster Y, Keck L. Examining the factor structure of the recovery assessment scale. Schizophr Bull. 2004;30:1035–1041. [DOI] [PubMed] [Google Scholar]
- 93. Cavelti M, Kvrgic S, Beck EM, Kossowsky J, Vauth R. Assessing recovery from schizophrenia as an individual process. A review of self-report instruments. Eur Psychiatry. 2012;27:19–32. [DOI] [PubMed] [Google Scholar]
- 94. Salzer MS, Brusilovskiy E. Advancing recovery science: reliability and validity properties of the Recovery Assessment Scale. Psychiatr Serv. 2014;65:442–453. [DOI] [PubMed] [Google Scholar]
- 95. Young SL, Ensing DS. Exploring recovery from the perspective of people with psychiatric disabilities. Psychiatr Rehabil J. 1999;3:219–231. [Google Scholar]
- 96. Marín-Martínez F, Sánchez-Meca J. Averaging dependent effect sizes in meta-analysis: a cautionary note about procedures. Span J Psychol. 1999;2:32–38. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.