Abstract
Background
Researchers have used various methods to describe and quantify the work of nurses. Many of these studies were focused on nursing in general care settings; therefore, less is known about the unique work nurses perform in intensive care units (ICUs).
Objectives
The aim of this study was to observe adult and pediatric ICU nurses in order to quantify and compare the duration and frequency of nursing tasks across four ICUs as well as within two discrete workflows: nurse handoffs at shift change and patient interdisciplinary rounds.
Methods
A behavioral task analysis of adult and pediatric nurses was used to allow unobtrusive, real-time observation. A total of 147 hours of observation were conducted in an adult medical-surgical, a cardiac, a pediatric, and a neonatal ICU at one rural, tertiary care community teaching hospital.
Results
Over 75% of ICU nurses’ time was spent on patient care activities. Approximately 50% of this time was spent on direct patient care, over 20% on care coordination, 28% on nonpatient care, and approximately 2% on indirect patient care activities. Variations were observed between units; for example, nurses in the two adult units spent more time using monitors and devices. A high rate and variety of tasks were also observed: Nurses performed about 125 activities per hour, averaging a switch between tasks every 29 seconds.
Discussion
This study provides useful information about how nurses spend their time in various ICUs. The methodology can be used in future research to examine changes in work related to, for example, implementation of health information technology.
Keywords: critical care, job task analysis, nurses, observation, work
The organization of nursing work (e.g., staffing ratios, workload) and characteristics of nurses (e.g., experience level, educational background) impact patient outcomes, quality of care, and nurse retention (Aiken, Clarke, Sloane, Sochalski, & Silber, 2002; Needleman, Buerhaus, Mattke, Stewart, & Zelevinsky, 2002; Tourangeau, Cranley, & Jeffs, 2006). Nursing personnel represent approximately 54% of all healthcare clinicians and serve a direct role in patient safety and quality of care. For example, nurses are responsible for the administration and monitoring phases of the medication use process, which is a frequently occurring and complex interdisciplinary care process estimated to be the source of 1.5 million patient injuries per year (Committee on the Work Environment for Nurses and Patient Safety Board, 2004). In addition, nurses play a major role in patient and family advocacy, care coordination, and system improvement. Therefore, the importance of the environments in which nurses work has been receiving widespread attention (Committee on the Work Environment for Nurses and Patient Safety Board, 2004). With the current nursing shortage expected to worsen through the year 2020 (Kuehn, 2007), it is important for organizations to improve the work life of nurses. One requirement for improving nurses’ work processes is to understand the details of nursing activities and the demands exerted upon them by the dynamic systems in which they work (Carayon et al., 2006). Therefore, accurate methods are needed to understand nurses’ work—the tasks they perform and the time spent performing those tasks.
The nurse behavioral task analysis described below was one component of a larger study examining the impact of electronic health record (EHR) implementation on clinicians in various intensive care units (ICUs). The overall study specifically focused on the effects of computerized provider order entry in multiple domains such as job task distribution, patient safety, and quality of care. The research team, composed primarily of human factors engineers and clinicians, utilizes a variety of investigational methods to understand and improve the design of the health systems (http://cqpi.engr.wisc.edu/cpoe_home).
Researchers have used a variety of observational methods to document the activities of anesthesiologists (Slagle & Weinger, 2009; Weinger, Herndon, & Gaba, 1997; Weinger, Slagle, & Reddy, 2004), primary care physicians (Overhage, Perkins, Tierney, & McDonald, 2001; Wetterneck et al., 2011), pharmacists (Rough, Reid-Ganske, Thielke, & Ploetz, 1996), and respiratory therapists (Conine & Neff, 1979). Measures of frequency, duration, and sequence of tasks and task categories were quantified in a number of studies (Battisto, Pak, Vander Wood, & Pilcher, 2009; Hendrich, Chow, Skierczynski, & Lu, 2008; Hendrickson, Doddato, & Kovner, 1990). Battisto et al. (2009) used job task analysis to measure the frequency of nine nurse activities in medical–surgical units at a large community hospital. Nurses spent 25% of their time on documentation and 55% of their time on direct patient care. Hendrich et al. (2008) studied the work of medical-surgical unit nurses in 36 U.S. hospitals using a work sampling technique in which nurses documented into a personal digital assistant which of 12 activities they were performing when the personal digital assistant randomly vibrated during their nursing shift. They found that nurses allocate about 75% of their time on direct nursing care. This total included the nonmutually exclusive categories of 35% on documentation, 19% on patient care activities, 17% on medication administration, and 17% on care coordination. Shively et al. (2011) used the work sampling technique to examine how nurses in three hospitals spent their time. The two most frequent work activities were direct care (36% for ICU nurses and 29% for nurses in acute care units) and communication (25% for ICU nurses and 28% for nurses in acute care units). The work of nurses includes not only direct patient care but also a range of other activities, such as documentation and care coordination.
The work of ICU nurses has been studied less. Wong et al. (2003) examined the types and distribution of ICU nursing tasks and compared the tasks both before and after the implementation of an ICU electronic information system. The proportion of time spent by surgical ICU nurses on documentation dropped from 35% to 24% after the implementation of an ICU information system (Quantitative Sentinel, Marquette Medical, Milwaukee, WI). Time spent by surgical ICU nurses on direct care (e.g., taking vital signs and patient treatments) increased from 31% to 40% while they spent the same amount of time (15%) on indirect care (e.g., conversation with patients, observing monitors) before and after the implementation of the new information system. This study was limited to a single ICU at a Veterans Affairs hospital, and 40 hours of observation were collected on 10 ICU nurses.
The methodologies described above relied on the development of behavioral taxonomies that were comprehensive representations of clinical tasks in various domains. Considerable effort was directed toward the identification of appropriate tasks and the organization of these tasks into logical categories. Consequently, observers could quickly locate tasks in real time, thereby directing more of their attention toward their participants and less toward the operation of the documentation tool. Observation methodologies also require standardization and procedural consistency to improve concordance between observers. Slagle, Weinger, Dinh, Brumer, and Williams (2002) and Schultz et al. (2006) discussed issues related to the validity and reliability of a direct observation methodology and outlined strategies to address these concerns.
Observation of ICU nursing work presents challenges not encountered in less acute situations. Rapidly changing patient conditions, a fast work pace, and a high-stimulus setting combine to create a complex milieu that may be intimidating and confusing to those unfamiliar with the environment. Furthermore, ICUs are not homogeneous workplaces. The patient characteristics that define various ICU populations (e.g., cardiovascular, surgical, neurological, pediatric, neonatal) create specialized patient needs that define the work performed by ICU nurses in these settings.
The objective of the behavioral task analysis used in this study was to observe activities performed by adult ICU (AICU) and pediatric ICU (PICU) nurses and compare the time they spent on various tasks across four different ICUs. Also evaluated were the tasks occurring during two critical, discrete, ICU workflows: nurse handoffs at shift change and patient interdisciplinary rounds.
Methods
Setting
Data were collected over a 3-month period in four ICUs of a 400-bed, rural, tertiary care community teaching hospital in the northeastern United States: a medical-surgical AICU, a cardiac ICU (CICU), a PICU, and a neonatal ICU (MCU). The 24-bed AICU uses a semiclosed ICU staffing model in which medical patients are managed by intensivists and surgical patients are comanaged by the ICU staff in consultation with surgeons. The AICU employs the largest number of registered nurses (n = 78) among the four ICUs and serves general critical care, trauma, and postsurgical patients. Residents rotate in the AICU under the supervision of critical care specialists (intensivists). The CICU comprises 18 beds and employs 65 nurses. Specialties are cardiothoracic surgery, cardiology critical care, and postoperative management of patients with liver transplants and serves as an adult critical care overflow. Cardiovascular fellows and physician assistants provide much of the patient care under the supervision of staff physicians, but it is an open-staff ICU in which the patient’s primary service (e.g., cardiology, cardiac surgery) retains responsibility for clinical management during the patient’s ICU stay. The PICU has 11 beds and employs 26 nurses. It is a closed-staff ICU that includes internal medicine and pediatric residents. The NICU has 38 beds, including 18 step-down beds for infants who need less intensive care. In this unit, 66 nurses rotate their care assignments between both groups of patients. The NICU has a closed staffing model in which the responsibility for clinical management of all patients resides with the ICU’s team of neonatologists and nurse practitioners. Pediatric residents who rotate through the MCU but cannot write orders assist them.
During this study, the state of the EHR implementation in the ICUs was limited with a few notable exceptions. For example, providers were using paper orders, but the organization was preparing to implement computerized provider order entry. Nursing clinical documentation functionality was in place, but nurses manually entered vital signs in the electronic nursing flowsheet because the bedside patient monitors were not networked with the EHR.
Data Collection Instrument
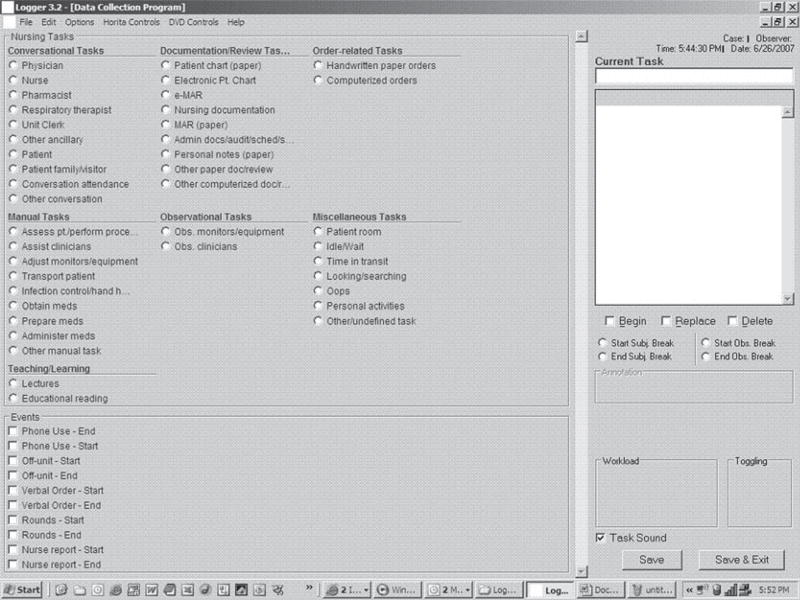
Nurses’ activities were observed and documented by researchers who used an existing software tool (Logger) on a portable tablet computer (Toshiba, New York, NY). The Logger is a noncommercial product that consists of a Microsoft Excel database with a graphical user interface created using the Microsoft Visual Basic programming language. The tool is customizable in that it utilizes domain-specific task lists developed by research teams (Schultz et al., 2006; Slagle et al., 2002). Before discussing the development of such a task list, it is helpful to first understand the software functionality Logger provided.
Observers documented tasks by selecting from a preconfigured task list using the tablet’s stylus (Figure 1). The software was programmed to record a start time when an activity was selected. Upon selection of the next task, the prior task was terminated and the task duration was calculated automatically (Schultz et al., 2006; Wong et al., 2003). Prior to observation, process rules were established to minimize documentation errors. When mistakes were made, the Logger offered a real-time correction feature as well as an annotation feature to insert a reminder that prompted the researcher to later correct the data entry. The data output was presented in a simple spreadsheet format that was exported in SPSS (version 20) for data analysis.
FIGURE 1.
Screenshot of data collection tool Nurse “Logger v 3.2”. Shown: task recording screen.
While the majority of tasks were sequential, there were inherent pauses between tasks during which time the nurse being observed appeared idle, inactive, or merely moving from one area to another. To address this, the observers utilized a specific group of activities categorized as in-between tasks (idle or waiting, transit time, and time searching for something). The task called transit time, for instance, implied movement without additional purpose other than to relocate; a nurse was in transit as he or she moved from one area to another. These transitional activities likely afforded the nurses time for cognitive activities such as planning; however, the behavioral observation method was not designed to document these processes.
The Logger software has two additional functions of relevance to this study: toggling and event marking. Toggling allowed observers to record simultaneous tasks (i.e., multitasking). Event marking allowed the observers to define specific contexts of interest and then document the occurrence of certain activities within those contexts. For example, two specific events were evaluated during this study: nurse handoffs performed face-to-face at the change of shift and interdisciplinary ICU rounds. When the observer recognized that one of these events was occurring, he or she would select the event on the Logger interface. Any nursing tasks occurring within that event would then be tagged for later analysis. Both events of interest were distinguished by unique cues. For example, the time of day (7 am, 3 pm, 7 pm, and 11 pm) and the presence of a new, incoming nurse typically indicated a change of shift handoff was impending. The gathering of a large group of clinical staff outside the door of an ICU patient’s room typically signaled the start of interdisciplinary rounds. When this event marker was turned on, subsequent tasks were tagged as belonging to that interdisciplinary round event. In practice, event indicators were often turned off and on because it was rare for a nurse to complete either a change of shift handoff or interdisciplinary rounds without being interrupted.
Development of the Nurse Taxonomy
Content Validity
Content validity “depends on the extent to which an empirical measurement reflects a specific domain of content” (Carmines & Zeller, 1979, p. 20). The research team relied significantly on the input of ICU nurses and physicians to ensure the content was representative of the ICU context. Development of the nurse job task list was an iterative process also involving human factors engineers from the research team. Engaging the multiple perspectives of different disciplines was useful throughout the development phase because it ensured the final taxonomy would be intuitive and understandable by non-nurse users. The process, which underwent approximately 10 iterations, began with the nurse task list developed by Wong et al. (2003). Four ICU nurses then refined this list further and added task definitions to ensure it would capture fully the clinical work found across multiple ICU settings. Furthermore, inclusion or exclusion of tasks in the broader categories was discussed among content experts and team members.
Early iterations of the task list were pilot-tested in ICUs by observers using paper prototypes. The tasks and their associated definitions were refined over 16 hours of pilot observations, debriefings, evaluation, and redesign until it was felt the task list was an exhaustive representation of ICU nurse work. The task list and categories were not integrated into the Logger tool until it was felt the taxonomy was representative of the entire content of nurse behavior in the ICU as suggested by Kerlinger and Lee (2000). A complete taxonomy of nurse tasks (n = 41), their definitions, and analysis categories are presented (see Table, Supplemental Digital Content 1, http://links.lww.com/NRES/A86).
Observer Training and Reliability
Two observers were used for data collection during this large observational study. There were many reasons for this; the most significant of which was efficiency. Several observers sharing the observation duties allowed the team to conclude the data collection phase within a reasonable time frame. This helped limit concerns regarding seasonal effects and minimized the influence of evolving circumstances within the ICUs and the organization itself. For instance, the hospital’s IT team was preparing to implement a full EHR technology in the upcoming year. Therefore, the research team gave considerable thought and effort toward the development of a process that would not only allow them to efficiently train multiple observers but, more importantly, to ensure consistency in the data collected across observers. One observer was both a masters-prepared registered nurse and human factors engineer. The second observer was a doctoral candidate in human factors engineering. This goal of achieving interobserver agreement is described by Robson (1993) as the “extent to which two or more observers obtain the same results when measuring the same behavior” (p. 340).
Achieving this goal required various approaches that progressed in difficulty during the training. Initially, there was an orientation phase (to both the observation tool and the ICU setting for the non-nurse) guided by a formal training manual developed by the research team. Subsequent activities involved progressively longer practice observation sessions in an ICU environment in an academic medical center affiliated with the research team’s university. Finally, the two observers performed a series of seven simultaneous observations, each lasting approximately 2 hours, during which they observed the same nurse and documented the tasks performed. At the end of the training period, the two observers achieved an interobserver agreement of 73% for capturing tasks within a 10-second window.
Data Collection Procedures
Observation periods ranged from 1.5 to 3 hours. The observations ran for a continuous period during which the researcher shadowed the nurse at a distance to see the nurse’s activities without interfering with natural movement, patient care, or workflow. Observers attempted to minimize interaction with the nurses. If family members were present or if the nurse was caring for an awake and alert patient, the observer asked the nurse to briefly explain the research study to give the family members and patient an opportunity to refuse to have their caregiver observed while caring for this patient. Observations were suspended during nurses’ personal time and when nurses were behind closed curtains with their patients. All observers underwent Health Insurance Portability and Accountability Act training and followed a set of behavioral rules of conduct developed by the University of Wisconsin’s Systems Engineering Initiative for Patient Safety research team, including infection control procedures. The institutional review boards of the university and the participating medical center approved the study. No protected health information about the patient and no identifying information about the nurses were collected.
Sample
The study participants were registered nurses employed in the four ICUs. Nurses were recruited through informational meetings, printed materials, and unit communications disseminated by unit leadership. To avoid causing disruptions, the observers prescheduled their observation sessions with the unit’s nurse manager, who then alerted the staff and charge nurse of the upcoming visit. Once on the unit, researchers coordinated their activities with the charge nurse, initially asking for her assessment that the unit was relatively stable (e.g., no impending disruptions such as fire drills or rapidly deteriorating patients) and requesting direction to nurses with typical ICU assignments. Nurses were then approached directly by the researcher, provided additional information about the project, and asked if they would participate. Five nurses refused to participate because it would have made them uncomfortable or they stated they were too busy. In-experienced nurses, nurses under preceptorship, and nurses who were involved primarily in nonclinical duties (charge nurses, nurse educators) did not participate. An effort was made to observe a variety of nurses with a range of patient assignments. In all ICUs, the observers shadowed nurses who were caring for critically ill patients. With the exception of a pool of per diem ICU staff, the nurses rarely floated to other ICUs. The research team utilized a purposeful sampling strategy that ensured that observations were conducted across all shifts and that all days of the week were represented in the sample.
Results
One hundred and forty-seven hours of observations were conducted by two observers over 3 months: 37 hours in the AICU, 35 hours in the CICU, 38 hours in the NICU, and 37 hours in the PICU. During the study period, patient census did not vary significantly in the AICU (23–24 patients), CICU (16–17 patients), or the NICU (22–29 patients); there was greater variation in the PICU (2–8 patients).
Data Analysis
The overwhelming majority of the nurses’ time comprised 17 individual tasks. These tasks were combined into four high-level task categories: (a) direct patient care, (b) care coordination, (c) indirect patient care, and (d) nonpatient care (Table 1). A human factors engineer and a physician classified the job tasks into high-level categories, in consultation with the director of critical care medicine at a large university hospital; this classification relies on previous research on nursing work, in particular the study of ICU nurses by Wong et al. (2003).
TABLE I.
List of Tasks and Task Categories
| Task categories | Tasks | Description of tasks |
|---|---|---|
| Direct patient care | Physical care of patient | Patient assessment, procedures, assisting clinicians, transporting patient, hand hygiene, obtaining or preparing medications, observing clinicians’ care activities |
| Use of monitors and devices | Adjusting medical devices, observing monitors and equipment | |
| Patient conversation | Conversing with patient | |
| Order management, including medications | Review and documentation of orders and medication administration records | |
| Clinical review and documentation | Review and documentation other than medications and orders, such as the patient chart, nursing documentation, and notes | |
| Care coordination | Conversation with physician | Conversing with physicians, including residents and physician assistants |
| Conversation with nurse | Conversing with other nurses | |
| Conversation with other ICU staff | Conversing with unit pharmacist, respiratory therapist, and unit desk clerk | |
| Conversation attendance | Standing, listening, not actively participating in conversation | |
| Conversation with patient’s family | Conversing with patient’s family | |
| Indirect patient care | Conversation with other non-ICU staff | Conversing with other ancillary clinical personnel, such as laboratory, radiology, physical therapy, or nutritionists |
| Administrative review and documentation | Review and documentation of other administrative documents | |
| Nonpatient care | Conversation with nonclinical staff | Conversing with nonclinical staff, such as housekeeping or IT, or unidentified people, including unidentified telephone calls. |
| Nonclinical manual tasks | Other nonclinical manual tasks | |
| In-between tasks | Idle or waiting, time in transit, looking, or searching | |
| Education and learning | Lectures, reading | |
| Other tasks | Other undefined tasks |
The time-coded data were analyzed to describe the amount of time spent on specific tasks as well as categories of tasks (Tables 2 and 3). For this analysis, the data from each of the 58 observation periods were aggregated and percentages of time were calculated. In addition, the number of individual occurrences of the individual tasks was examined. The percentage of the total observed time that each nurse spent on each task or category of tasks was calculated, and the degree to which differences in nurses’ task distribution varied by the unit in which they worked (AICU, CICU, NICU, or PICU) was assessed. Statistical comparisons of the four ICUs were made using a measure of effect sizes (η2) instead of F tests because of the large number of comparisons and the high likelihood of type I errors. Eta-square (η2) estimates the proportion of the variability explained by unit; a relatively large eta-square means that the effect of unit was larger (Trusty, Thompson, & Petrocelli, 2004). To correct for non-normal distributions, the dependent variables were log-transformed before Eta-square was calculated. Similar analyses were performed on the rate of task occurrences per hour.
TABLE 2.
Time Spent by Intensive Care Unit Nurses on Tasks
| AICU (%) | CICU (%) | NICU (%) | PICU (%) | Total (%) | η2 | Cohen’s d | |
|---|---|---|---|---|---|---|---|
| Total direct patient care | 51.28 | 58.69 | 49.90 | 47.07 | 51.77 | .112 | 0.710 |
| Physical care of patient | 14.52 | 14.12 | 23.19 | 17.08 | 17.12 | .209 | 1.028 |
| Use of monitors and devices | 10.25 | 12.16 | 7.27 | 5.60 | 8.84 | .149 | 0.837 |
| Patient conversation | 2.32 | 3.41 | 0.52 | 2.22 | 2.15 | .238 | 1.118 |
| Order management, including medications | 3.97 | 2.97 | 2.58 | 4.27 | 3.47 | .036 | 0.386 |
| Clinical review and documentation | 20.22 | 26.03 | 16.34 | 17.90 | 20.19 | .121 | 0.742 |
| Total care coordination | 21.14 | 21.86 | 20.05 | 28.37 | 22.91 | .069 | 0.545 |
| Conversation with physician | 3.01 | 3.51 | 1.67 | 3.70 | 3.00 | .128 | 0.766 |
| Conversation with nurse | 12.29 | 12.59 | 10.70 | 17.01 | 13.19 | .018 | 0.271 |
| Conversation with other ICU staff | 1.51 | 1.63 | 1.39 | 2.18 | 1.68 | .025 | 0.320 |
| Conversation attendance | 1.35 | 1.20 | 3.59 | 2.63 | 2.17 | .054 | 0.478 |
| Conversation with patient’s family | 2.97 | 2.94 | 2.69 | 2.85 | 2.87 | .055 | 0.482 |
| Total indirect patient care | 2.93 | 1.78 | 1.79 | 1.00 | 2.09 | .159 | 0.870 |
| Conversation with other non-ICU staff | 1.97 | 1.60 | 0.53 | 0.20 | 1.09 | .111 | 0.707 |
| Administrative review and documentation | 0.96 | 0.18 | 1.26 | 0.30 | 0.66 | .113 | 0.714 |
| Total nonpatient care | 24.65 | 17.67 | 28.26 | 24.05 | 23.57 | .155 | 0.857 |
| Conversation with nonclinical staff | 3.83 | 4.21 | 9.77 | 7.28 | 6.21 | .028 | 0.339 |
| Nonclinical manual tasks | 5.27 | 5.57 | 7.78 | 4.46 | 5.73 | .075 | 0.570 |
| In between tasks | 9.55 | 6.31 | 7.00 | 9.03 | 7.99 | .057 | 0.412 |
| Education and learning | 0.57 | 0.00 | 0.66 | 0.80 | 0.50 | .038 | 0.398 |
| Other tasks | 5.44 | 1.57 | 3.05 | 2.48 | 3.14 | .045 | 0.434 |
| Total | 100.00 | 100.00 | 100.00 | 100.00 | 100.00 |
Note. Eta-square estimates the proportion of the variability explained by unit (Trusty et al., 2004). Cohen’s d is also provided for use in meta-analyses. ICU = intensive care unit; AICU = adult intensive care unit; CICU = cardiac intensive care unit; NICU = neonatal intensive care unit; PICU = pediatric intensive care unit.
TABLE 3.
Rate of Intensive Care Unit Nurses’ Activities per Hour
| AICU | CICU | NICU | PICU | Total | η2 | Cohen’s d | |
|---|---|---|---|---|---|---|---|
| Total direct patient care | 73.31 | 88.08 | 59.63 | 41.70 | 65.79 | .269 | 1.213 |
| Physical care of patient | 18.98 | 17.12 | 18.32 | 13.74 | 17.02 | .103 | 0.678 |
| Use of monitors or devices | 22.99 | 32.05 | 17.30 | 8.99 | 20.38 | .314 | 1.353 |
| Conversation with patient | 4.01 | 6.54 | 0.72 | 2.52 | 3.50 | .302 | 1.316 |
| Order management including medications | 5.08 | 4.54 | 5.80 | 4.74 | 5.03 | .007 | 0.168 |
| Clinical review and documentation | 22.26 | 27.83 | 17.48 | 11.72 | 19.86 | .193 | 0.978 |
| Total care coordination | 24.19 | 25.79 | 16.02 | 22.67 | 22.28 | .097 | 0.655 |
| Conversation with physician | 4.05 | 5.15 | 1.73 | 3.21 | 3.57 | .122 | 0.746 |
| Conversation with nurse | 12.81 | 13.80 | 9.17 | 12.72 | 12.18 | .031 | 0.358 |
| Conversation with other ICU staff | 2.00 | 2.31 | 1.47 | 1.99 | 1.95 | .043 | 0.424 |
| Conversation attendance | 2.39 | 1.29 | 2.34 | 1.75 | 1.93 | .009 | 0.191 |
| Conversation with patient’s family | 2.93 | 3.23 | 1.31 | 3.01 | 2.64 | .073 | 0.561 |
| Total indirect patient care | 3.07 | 3.99 | 1.25 | 0.60 | 2.24 | .259 | 1.182 |
| Conversation with other non-ICU staff | 2.50 | 3.51 | 0.73 | 0.39 | 1.80 | .131 | 0.776 |
| Administrative review and documentation | 0.57 | 0.48 | 0.52 | 0.21 | 0.44 | .106 | 0.689 |
| Total nonpatient care | 42.45 | 40.65 | 32.06 | 25.13 | 35.13 | .078 | 0.582 |
| Conversation with nonclinical staff | 2.12 | 2.59 | 2.00 | 2.11 | 2.21 | .026 | 0.327 |
| Nonclinical manual tasks | 11.30 | 13.21 | 12.89 | 7.30 | 11.14 | .111 | 0.707 |
| In-between tasks | 26.99 | 23.22 | 16.46 | 14.49 | 20.36 | .052 | 0.468 |
| Education and learning | 0.14 | 0.00 | 0.19 | 0.12 | 0.11 | .069 | 0.544 |
| Other tasks | 1.90 | 1.63 | 0.51 | 1.11 | 1.30 | .165 | 0.889 |
| Rate of occurrences, all tasks | 143.02 | 158.51 | 108.96 | 90.10 | 125.44 | .031 | 0.358 |
Note. Eta-square estimates the proportion of the variability explained by unit (Trusty et al., 2004). Cohen’s d is also provided for use in meta-analyses. ICU = intensive care unit; AICU = adult intensive care unit; CICU = cardiac intensive care unit; NICU = neonatal intensive care unit; PICU = pediatric intensive care unit.
Across the four ICUs, nurses spent 52% of their time on direct patient care, 23% on care coordination, 2% on indirect patient care activities, and 24% on nonpatient care (Table 2). The individual tasks on which nurses spent the most time were review and documentation of clinical information (20% of nurses’ time), physical care of the patient (17%), conversation with other nurses (13%), and in-between tasks (8%). The idle or waiting time and the time in transit were typically observed between other tasks and provided the nurse with time to transition to the next task.
Multitasking accounted for less than 5% of the total time observed and almost always involved conversation combined with other tasks. These conversations were most frequently with other nurses or with patients and their families (52% and 23% of multitasking occurrences, respectively). The tasks most frequently performed concurrently with conversation were assessing the patient (21% of multitasking occurrences), clinical documentation (14%), and adjusting monitors and devices (12%).
Time spent by nurses on various tasks was examined across the four ICUs. The largest differences (i.e., highest η2 scores) were observed for the following tasks: patient conversation (η2 = .238), physical care of patients (η2 = .209), use of monitors and devices (η2 = .149), conversation with physicians (η2 = .128), and clinical review and documentation (η2 = .121). Nurses in the PICUs, in particular the NICU, spent more time physically caring for patients (23% for NICU and 17% for PICU) as compared with nurses in the AICU and CICU (14%). The opposite pattern was observed for the use of monitors and devices (12% for CICU, 10% for AICU, 7% for NICU, and 6% for PICU) and for the clinical review and documentation task (26% for CICU, 20% for AICU, 18% for PICU, and 16% for NICU). Nurses spent a small amount of time talking to patients (CICU 3%, PICU 2%, AICU 2%, and NICU 1%). They also spent very little total time talking to physicians (4% PICU, 3% AICU and CICU, and 2% NICU).
The discrete activities performed by ICU nurses (the recording of each task in the electronic observation tool) were used to calculate the number of activities per hour. The average number of nurse activities per hour across all ICUs was 125; it was highest in the CICU (158 activities per hour), followed by the AICU (143), the NICU (109), and the PICU (90). This means that ICU nurses were switching between tasks on average every 29 seconds: every 23 seconds in the CICU, 25 seconds in the AICU, 33 seconds in the NICU, and every 40 seconds in the PICU. The most frequent task occurrences were using monitors and equipment, clinical review and documentation, and in-between tasks (20 activities per hour each), followed by physical care of the patient (17 activities per hour) and nurse conversation (12 activities per hour; Table 3).
During nurse handoffs, ICU nurses spent most of their time performing care coordination tasks (79% of nurses’ time compared with 21% of time outside of shift-change report). Tasks performed less often by ICU nurses during shift change report include direct patient care (17% during shift change compared with 53% outside of shift change) and nonpatient care (4% during shift change compared to 24% outside of shift change). The ICU nurses did not perform any indirect patient care tasks during shift change. A similar pattern was found for time spent by ICU nurses during interdisciplinary rounds: 80% of that time was spent on care coordination (as opposed to 22% of time spent on care coordination outside of rounds).
Discussion
During the 147 hours of observation, most of the ICU nurses’ work was patient care tasks, in particular direct patient care and care coordination. Nonpatient care tasks took a large amount of nurses’ time (24%), but ICU nurses spent most of their time caring for patients, with 76% of nurses’ time spent on patient care (direct care, care coordination, and indirect patient care). This finding is similar to the finding of Hendrich et al. (2008) that medical–surgical hospital nurses spend 75% of their time on patient care. The total amount of time that nurses spend talking to patients and explaining things in medical–surgical units is likely higher than in the ICU, but nurses tend to spend more time observing monitors and administering medications in the ICU (Cullen et al., 1997). In the current study, ICU nurses spent about 24% of their time on review and documentation (including 20% on clinical review and documentation and 4% on order management); this is similar to the amount of time spent by ICU nurses on documentation after the implementation of an electronic documentation system in the study by Wong et al. (2003) and the time spent by medical surgical nurses using computers for documentation in Battisto et al. (2009). In Wong et al. (2003), before the electronic documentation system was implemented, nurses spent 35% of their time on documentation. This is similar to the findings of Hendrich et al. (2008) in medical–surgical units without electronic documentation. In the current study, ICU nurses used an EHR system for charting (i.e., nursing flowsheets). The results confirm results of other studies that ICU nurses spend about one quarter of their time on review and documentation tasks. This time is unlikely to decrease given the increasing pressure from regulatory agencies to document care activities.
The distribution of nurses’ task time varied substantially between the ICUs for some tasks such as physical care of patient, use of monitors and devices, patient conversation, and clinical review and documentation. In general, nurses in the two AICUs spent more time on clinical review and documentation and in their use of monitors and devices than nurses in the NICU or PICU. On the other hand, nurses in the PICUs spent more time on physical care of the patient. In general, nurses in all four ICUs spent similar amounts of time on care coordination, indirect patient care, and nonpatient care tasks.
Individual nursing tasks were rarely sustained for long time periods. The high number and large variety of nursing activities within short time periods suggest that the ICU nurses’ work is unremittingly busy and frequently changing. This finding is consistent with research by Ebright, Patterson, Chalko, and Render (2003) and Wolf et al. (2006), who showed how nurses stack activities in anticipation or preparation for problems they expect to encounter. Stacking of activities involves rapid changes in activities to manage priorities and other work challenges such as interruptions (Wolf et al., 2006). These rapid and frequent changes in activities may contribute to ICU nursing workload, a well-known job stressor and contributor to medical errors (Carayon & Gürses, 2005). The potential links between activity rate and workload among ICU nurses should be examined in future research.
Highly complex ICU work processes are supported by many tasks other than direct patient care: care coordination occupied 23% of nurses’ time and documentation and review 20% of their time. As expected, care coordination occupied about 80% of ICU nurses’ time during handoffs at shift change and during patient rounds. Nurses’ work frequently demands interaction, planning, and consulting with a variety of clinicians and ancillary staff. There was a high frequency and variety of communication tasks that occurred in all ICUs, in particular during shift change and rounds. It cannot be ascertained from these observations, however, the nature of the team interactions and to what extent the communication supports effective collaboration or efficient care processes.
The work of caring for critically ill patients is a team effort in which nurses play a central role. It is not, however, a system dominated by synchronous face-to-face interaction of the physician–nurse dyad as relatively little physician–nurse communication activity was observed: 3% of nurses’ time was spent in conversations with ICU physicians and 2% of their time was spent on conversation attendance that occurred during rounds with ICU physicians. The current study was limited by the inability to reliably identify with whom nurses were speaking during telephone conversations. It is likely that the physicians’ orders and goals for patient care are communicated in other asynchronous ways, such as through paper-based orders and physician documentation. Furthermore, nurses’ specialized skills and protocol-based practices of the specialized ICUs enables more autonomy in nursing practice. This may contribute as well to the observation that clinical review and documentation was one of the most frequently observed nurse tasks (20% of nurses’ time). A great deal of information must be reviewed and documented, including physician orders, clinical details, quality improvement reports, and the fulfillment of compliance and legal requirements.
The prevalence and necessity of life support or monitoring equipment extends the boundary of the patient to include a variety of technology-mediated, asynchronous, and remote care interventions. The approximately 9% of nurses’ time spent interacting with clinical equipment and monitors is congruent with the highly technical and specialized environment of ICUs.
The observational methodology used has limitations, the most important being that the cognitive work performed by ICU nurses is not measured. To understand the cognitive demands experienced by ICU nurses, other methods, such as interviews and questionnaires, would need to be performed. The current study showed that ICU nurses perform about 125 distinguishable activities per hour; however, it is important to understand that this hourly activity rate also depends on how broadly the tasks were defined. The task list created here is much more detailed than previously designed task lists. Because data collection was limited to four ICUs in a single hospital, results cannot be generalized to other ICUs.
This observational method proved effective for gaining an understanding of the nature of ICU nurses’ work activities and offers greater understanding of the ICU as a unique work environment. The observational methodology provides more specific, quantitative information about time spent by ICU nurses on various tasks. This job task information can be used by administrators and managers in a variety of ways; for example, to evaluate staffing needs, to assess training needs, to understand workload, or to understand how nursing work changes when technologies are introduced into the work setting. This information can be used to evaluate the added value of job tasks performed by ICU nurses. Such data can be the input to other methods aimed at analyzing and redesigning processes and improving quality.
Supplementary Material
Footnotes
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s Web site (www.nursingresearchonline.com).
Note: Information about the Logger and Task Analysis Programs can be obtained from Jason.Slagle@Vanderbilt.edu.
The authors have no conflicts of interest to disclose.
Contributor Information
Stephen Douglas, University of Wisconsin Hospital and Clinics, Madison..
Randi Cartmill, Center for Quality and Productivity Improvement, University of Wisconsin-Madison..
Roger Brown, School of Nursing, University of Wisconsin-Madison..
Peter Hoonakker, Center for Quality and Productivity Improvement, University of Wisconsin-Madison..
Jason Slagle, Center for Research and Innovation in Systems Safety, Department of Anesthesiology, Vanderbilt University School of Medicine, Nashville, Tennessee..
Kara Schultz Van Roy, Research Fellow, Center for Quality and Productivity Improvement, University of Wisconsin-Madison, and Doctoral Recipient, Department of Industrial and Systems Engineering, University of Wisconsin-Madison..
James M. Walker, Geisinger Medical Center, Danville, Pennsylvania..
Matthew Weinger, Center for Research and Innovation in Systems Safety, Department of Anesthesiology, Vanderbilt University School of Medicine, Nashville, Tennessee..
Tosha Wetterneck, Department of Medicine, University of Wisconsin School of Medicine and Public Health, and Center for Quality and Productivity Improvement, University of Wisconsin-Madison..
Pascale Carayon, Director, Center for Quality and Productivity Improvement, University of Wisconsin-Madison, and Professor, Department of Industrial and Systems Engineering, University of Wisconsin-Madison..
References
- Aiken LH, Clarke SP, Sloane DM, Sochalski J, Silber JH. Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. Journal of the American Medical Association. 2002;288:1987–1993. doi: 10.1001/jama.288.16.1987. [DOI] [PubMed] [Google Scholar]
- Battisto D, Pak R, Vander Wood MA, Pilcher JJ. Using a task analysis to describe nursing work in acute care patient environments. Journal of Nursing Administration. 2009;39:537–547. doi: 10.1097/NNA.0b013e3181c1806d. [DOI] [PubMed] [Google Scholar]
- Carayon P, Gürses AP. A human factors engineering conceptual framework of nursing workload and patient safety in intensive care units. Intensive and Critical Care Nursing. 2005;21:284–301. doi: 10.1016/j.iccn.2004.12.003. [DOI] [PubMed] [Google Scholar]
- Carayon P, Schoofs Hundt A, Karsh BT, Gurses AP, Alvarado CJ, Smith M, Flatley Brennan P. Work system design for patient safety: The SEIPS model. Quality and Safety in Health Care. 2006;15:i50–i58. doi: 10.1136/qshc.2005.015842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carmines EG, Zeller RA. Reliability and validity assessment. Beverly Hills, CA: Sage; 1979. [Google Scholar]
- Committee on the Work Environment for Nurses and Patient Safety Board. Keeping patients safe: Transforming the work environment of nurses. Washington, DC: Author; 2004. [Google Scholar]
- Conine TA, Neff P. Productivity of respiratory therapy personnel. Respiratory Care. 1979;24:314–320. [PubMed] [Google Scholar]
- Cullen DJ, Sweitzer BJ, Bates DW, Burdick E, Edmondson A, Leape LL. Preventable adverse drug events in hospitalized patients: A comparative study of intensive care and general care units. RCritical Care Medicine. 1997;25:1289–1297. doi: 10.1097/00003246-199708000-00014. [DOI] [PubMed] [Google Scholar]
- Ebright PR, Patterson ES, Chalko BA, Render ML. Understanding the complexity of registered nurse work in acute care settings. Journal of Nursing Administration. 2003;33:630–638. doi: 10.1097/00005110-200312000-00004. [DOI] [PubMed] [Google Scholar]
- Hendrich A, Chow M, Skierczynski BA, Lu Z. A 36-hospital time and motion study: How do medical-surgical nurses spend their time? The Permanente Journal. 2008;12:25–34. doi: 10.7812/tpp/08-021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hendrickson G, Doddato TM, Kovner CT. How do nurses use their time? Journal of Nursing Administration. 1990;20:31–37. doi: 10.1097/00005110-199003000-00008. [DOI] [PubMed] [Google Scholar]
- Kerlinger FN, Lee HB. Foundations of behavioral research. 4. Belmont, CA: Wadsworth; 2000. [Google Scholar]
- Kuehn BM. No end in sight to nursing shortage: Bottleneck at nursing schools a key factor. Journal of the American Medical Association. 2007;298:1623–1625. doi: 10.1001/jama.298.14.1623. [DOI] [PubMed] [Google Scholar]
- Needleman J, Buerhaus P, Mattke S, Stewart M, Zelevinsky K. Nurse-staffing levels and the quality of care in hospitals. New England Journal of Medicine. 2002;346:1715–1722. doi: 10.1056/NEJMsa012247. [DOI] [PubMed] [Google Scholar]
- Overhage JM, Perkins S, Tierney WM, McDonald CJ. Controlled trial of direct physician order entry: Effects on physicians’ time utilization in ambulatory primary care internal medicine practices. Journal of the American Medical Informatics Association. 2001;8:361–371. doi: 10.1136/jamia.2001.0080361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robson C. Real world research—A resource for social scientists and practitioner-researchers. Oxford, UK: Blackwell; 1993. [Google Scholar]
- Rough SS, Reid-Ganske LM, Thielke TS, Ploetz PA. Work redesign and role restructuring in a pharmacy department with pharmacist assistants. American Journal of Health-System Pharmacy. 1996;53:1928–1933. doi: 10.1093/ajhp/53.16.1928. [DOI] [PubMed] [Google Scholar]
- Schultz K, Slagle J, Brown R, Douglas S, Frederick B, Lakhani M, Carayon P. Development of a job task analysis tool for assessing the work of physicians in the intensive care unit. In: In The Human Factors and Ergonomics Society, editor. Proceedings of the human factors and ergonomics society 50th annual meeting. Santa Monica, CA: Author; 2006. pp. 1469–1473. [Google Scholar]
- Shively M, Rutledge T, Rose BA, Graham P, Long R, Stucky E, Dresselhaus T. Real-time assessment of nurse work environment and stress. Journal for Healthcare Quality. 2011;33:39–48. doi: 10.1111/j.1945-1474.2010.00093.x. [DOI] [PubMed] [Google Scholar]
- Slagle JM, Weinger MB. Effects of intraoperative reading on vigilance and workload during anesthesia care in an academic medical center. Anesthesiology. 2009;110:275–283. doi: 10.1097/ALN.0b013e318194b1fc. [DOI] [PubMed] [Google Scholar]
- Slagle JM, Weinger MB, Dinh MT, Brumer VV, Williams K. Assessment of the intrarater and interrater reliability of an established clinical task analysis methodology. Anesthesiology. 2002;96:1129–1139. doi: 10.1097/00000542-200205000-00016. [DOI] [PubMed] [Google Scholar]
- Tourangeau AE, Cranley LA, Jeffs L. Impact of nursing on hospital patient mortality: A focused review and related policy implications. Quality and Safety in Health Care. 2006;15:4–8. doi: 10.1136/qshc.2005.014514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trusty J, Thompson B, Petrocelli JV. Practical guide for reporting effect size in quantitative research. Journal of Counseling and Development. 2004;82:107–110. [Google Scholar]
- Weinger MB, Herndon OW, Gaba DM. The effect of electronic record keeping and transesophageal echocardiography on task distribution, workload, and vigilance during cardiac anesthesia. Anesthesiology. 1997;87:144–155. doi: 10.1097/00000542-199707000-00019. [DOI] [PubMed] [Google Scholar]
- Weinger MB, Reddy SB, Slagle JM. Multiple measures of anesthesia workload during teaching and nonteaching cases. Anesthesia and Analgesia. 2004;98:1419–1425. doi: 10.1213/01.ane.0000106838.66901.d2. [DOI] [PubMed] [Google Scholar]
- Wetterneck TB, Lapin JA, Krueger DJ, Holman GT, Beasley JW, Karsh BT. Development of a primary care physician task list to evaluate workflow. BMJ Quality and Safety. 2011;21:47–53. doi: 10.1136/bmjqs-2011-000067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolf LD, Potter P, Sledge JA, Boxerman SB, Grayson D, Evanoff B. Describing nurses’ work: Combining quantitative and qualitative analysis. Human Factors. 2006;48:5–14. doi: 10.1518/001872006776412289. [DOI] [PubMed] [Google Scholar]
- Wong DH, Gallegos Y, Weinger MB, Clack S, Slagle J, Anderson CT. Changes in intensive care unit nurse task activity after installation of a third-generation intensive care unit information system. Critical Care Medicine. 2003;31:2488–2494. doi: 10.1097/01.CCM.0000089637.53301.EF. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.