Abstract
Background
Interventions are needed to reduce unnecessary antibiotic prescribing for respiratory tract infections (RTIs). Although community antibiotic prescribing appears to be decreasing in the UK, figures for out-of-hours (OOH) prescribing have substantially increased. Understanding the factors influencing prescribing in OOH and any perceived differences between general practitioner (GP) and nurse prescriber (NP) prescribing habits may enable the development of tailored interventions promoting optimal prescribing in this setting.
Objectives
To explore UK GP and NP views on and experiences of prescribing antibiotics for RTIs in primary care OOH services.
Methods
Thirty semi-structured interviews were conducted with GPs and NPs working in primary care OOH services. Inductive thematic analysis was used to analyse data.
Results
The research shows that factors particular to OOH influence antibiotic prescribing, including a lack of patient follow-up, access to patient GP records, consultation time, working contracts and implementation of feedback, audit and supervision. NPs reported perceptions of greater accountability for their prescribing compared with GPs and reported they had longer consultations during which they were able to discuss decisions with patients. Participants agreed that more complex cases should be seen by GPs and highlighted the importance of consistency of decision making, illness explanations to patients as well as a perception that differences in clinical training influence communication with patients and antibiotic prescribing decisions.
Conclusions
Environmental and social factors in OOH services and a mixed healthcare workforce provide unique influences on antibiotic prescribing for RTIs, which would need to be considered in tailoring interventions that promote prudent antibiotic prescribing in OOH services.
Introduction
Respiratory tract infections (RTIs) are usually brief, self-limiting conditions. Antibiotics have little or no clinical benefit in most cases, unless there is a serious underlying comorbidity.1 RTIs account for >60% of all prescriptions issued in UK primary care.1–3 In addition to the risk of side effects, the unnecessary prescription of antibiotics contributes to the spread of resistance.4,5 Antibiotic resistance may have catastrophic consequences and tackling rising resistance has been highlighted as an international priority.6
Although UK antibiotic prescribing rates have recently declined,7 it is recognized that more prudent prescribing is essential to slow the increase in resistant bacteria. The latest English Surveillance Programme for Antimicrobial Utilisation and Resistance (ESPAUR) report indicates that out-of-hours (OOH) accounts for 4.7% of prescribing in community settings.7 Understanding factors influencing prescribing in OOH may enable the tailoring of interventions to promote optimal prescribing in this setting.8,9
OOH in England are services provided outside of normal working hours (6.30pm–8.00am) and are accessed by patients either by calling NHS 111 or by visiting a specified centre such as urgent care services, an NHS walk-in centre or a minor injuries unit.10 General practice teams can choose whether to provide 24 h care for their patients or to transfer responsibility for OOH services to NHS England, who are responsible for providing a high-quality service for the local population. OOH services can be provided by NHS, private or private non-profit organizations and are commissioned by Clinical Commissioning Groups (CCGs). Previous research has shown that patients attending OOH are more likely to present with serious illness11 and the majority of antibiotics are prescribed to patients contacting the service at weekends, which presents a challenge when considering antibiotic prescribing as this may be due to antibiotic-seeking behaviour.12
One-fifth of adults in England who had an RTI in the last 6 months went on to visit their general practitioner (GP) surgery and 10.3% of these individuals expected to be prescribed an antibiotic, which may influence healthcare professionals’ decisions to prescribe.13 Other research14 has shown that GPs were more likely to prescribe when on call owing to lack of time, ability to follow up and absence of personal knowledge of the patient. In most cases of acute RTIs, no antibiotic is needed and no-prescribing strategies should be encouraged when infection is moderate; however, strategies such as a delayed prescription and self-care have been shown to provide similar benefits to an immediate antibiotic prescription and may be a more acceptable strategy for some clinicians and patients.8,15,16
A Cochrane Review highlighted that delayed prescribing may be a suitable compromise in place of immediate prescribing to significantly reduce unnecessary antibiotic use for RTIs and thereby reduce antibiotic resistance while maintaining patient safety and satisfaction levels.15 Studies have reported delayed antibiotic prescribing being used by GPs as a compromise to meet patient expectations, maintain relationships between the practitioner and patient, manage uncertainty and provide a safety net to safeguard against complication.17,18
Brookes-Howell et al.19 reported that clinician confidence in making a diagnosis was key in making prescribing decisions. Low confidence and low tolerance for uncertainty could lead to defensive medicine and prescribing ‘just in case’ and is associated with increased antibiotic prescribing.20,21 Other factors have been reported to impact antibiotic prescribing in the OOH setting, including a lack of record linkage and prior knowledge of patients as well as perceived additional patient demand.21
Prescribing habits may also vary between professional groups. Rowbotham et al.22 found that nurse prescribers (NPs) practice a no-prescribing approach when managing RTIs and have a repertoire of strategies to draw upon when dealing with patients, such as patient education, reinforcing the no-prescribing decision and addressing patient concerns. Although patients appreciate the extra time spent with an NP in-hours,23 it has been reported that this may increase costs in an already stretched service.24 Therefore, differences between the two professional groups are explored in this paper. Previous qualitative literature has largely focused on antibiotic prescribing in in-hours general practice and has not focused on the OOH setting, as this paper does.
Aims and objectives
Both GPs and NPs provide care for patients with RTIs in OOH. Therefore, the aim of this research is to explore the antibiotic prescribing practices of both groups. This study had two key objectives: (i) to identify GP and NP experiences of prescribing antibiotics for RTIs in OOH, to explore facilitators and barriers to reducing antibiotic prescribing; and (ii) to identify similarities and differences between GP and NP antibiotic prescribing.
Methods
Context
Two organizations were used to identify potential participants for interview: (i) the Clinical Research Network; and (ii) the Association for Prescribers. Both organizations advertised the study and provided a list of potential participants’ contact details. All invitees were e-mailed a participant information sheet, a reply slip and a consent form. All responses were sent to S. J. W. who then contacted participants. Once consent and eligibility were confirmed, a convenient date and time for a telephone interview was arranged. Participants taking part were each paid an honorarium of £50. Interviews were conducted between November 2015 and April 2016. The study was supported by a Patient and Public Involvement (PPI) representative (co-author K. P.) who was involved in study delivery and analysis and reviewed study rigour.
Participants
GPs and NPs working within primary care OOH services were recruited. NHS OOH services were defined as those that operated outside of normal daytime working hours (6.30pm–8.00am) that could be accessed by calling NHS 111 and walk-in services. To ensure diversity, purposive maximum variation sampling was used to identify participants.25 Snowball or chain sampling, a technique for locating further participants through existing ones,26 supported this sampling strategy. The primary sampling criteria were to ensure an equal mix of GPs and NPs who worked in rural and urban settings as well as staff from NHS, non-profit private and private OOH organizations. Secondary criteria sought to identify variation in whether prescribers worked solely in OOH or a mixture of in-hours practice and OOH, and number of years of clinical experience. Prescribers were excluded if individuals solely worked in secondary care OOH.
Interviews
A semi-structured interview guide was developed (available as Supplementary data at JAC Online) from existing literature on exploring in-hours GP antibiotic prescribing.18 Interview topics explored antibiotic prescribing for RTIs in OOH, the use of strategies to reduce unnecessary antibiotic prescribing, the influence of patient expectations on prescribing decisions and training in antibiotic management for healthcare professionals. The interviews were conducted by telephone for pragmatic reasons and to allow data collection with GPs and NPs from organizations across England. Interviews were completed by two experienced qualitative researchers (S. J. W. and A. V. H.) and were audio recorded. Interviews continued until data indicated saturation.
Analysis
Whilst interviews were taking place the team met regularly to discuss topics raised by participants and the interview guide was refined as the interviews continued. All interviews were transcribed verbatim. Transcripts were read and reread by S. J. W. both during and after the data collection period. An inductive thematic analysis approach27 was used to analyse data, drawing on methods of constant comparison.28 S. J. W. independently coded the first five interviews and a secondary analysis team (S. J. W., S. T.-C., A. V. H., K. P. and C. E.) met to agree on preliminary codes. Following coding of a further five transcripts, S. J. W. developed a draft coding frame that was discussed and agreed on by the full team. S. T.-C., A. V. H. and K. P. independently second-coded six transcripts (20%) using the coding frame; discrepancies were minor and changes were made following discussion. Codes were then grouped into themes in which both within- and between-participant variation was considered. Comparisons were also drawn between GP and NP experiences. Theme labelling and interpretation was continually discussed in regular team data meetings. NVivo 11 for Windows was used to manage data.
Our epistemological position is best characterized by subtle realism, in which the researchers assume that we can only know reality from our own perception of it.29 Our goal therefore was for a pragmatic analysis that would increase understanding of this area from a prescriber perspective, and lead to suggestions for future research and practice.
Ethics
This study was reviewed and approved by the NHS Health Research Authority (Ref 15/HRA/0101).
Results
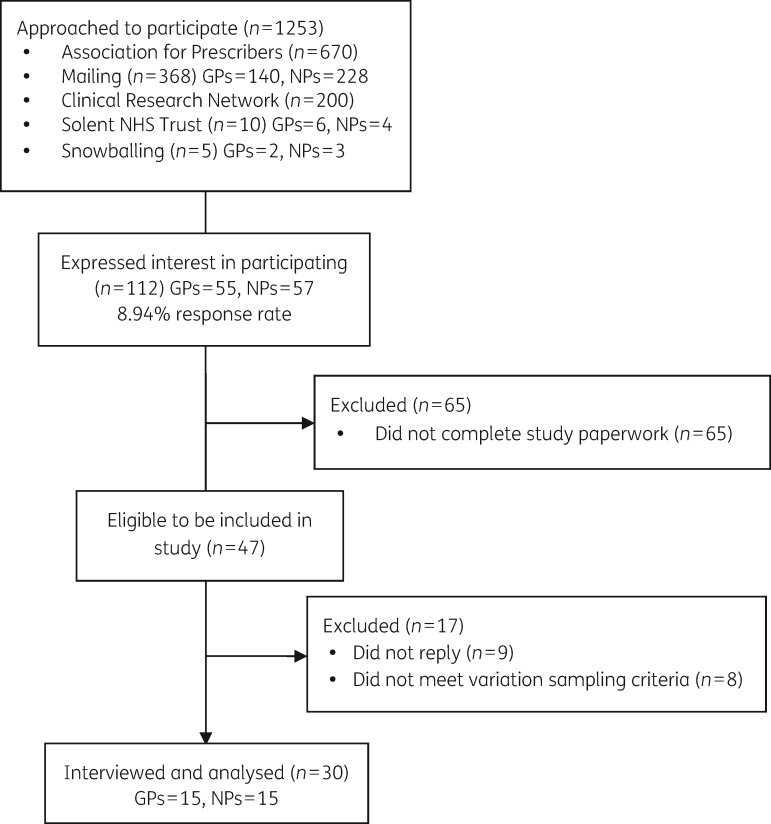
A total of 1253 prescribers were approached to take part in the study; 112 (8.94%) individuals responded to express an interest in participating in a telephone interview. See Figure 1 for recruitment details.
Figure 1.
UNITE CONSORT flow diagram.
Fifteen GPs and 15 NPs took part in interviews. The level of interest in the study allowed the team to purposefully select participants. Participant characteristics are detailed in Table 1.
Table 1.
Participant characteristics
| GPs | NPs | |
|---|---|---|
| Mean age (years) | 43 | 44 |
| Age range (years) | 30–67 | 32–63 |
| Gender ratio (male:female) | 8:7 | 4:11 |
| OOH provider | NHS: 8 | NHS: 6 |
| walk-in centre: 1 | walk-in centre: 4 | |
| private (non-profit): 1 | private (non-profit): 2 | |
| private: 5 | private: 3 | |
| No. of participants who work in-hours as well as OOH | 13 | 4 |
| Range of mean years qualified to prescribe | 0.5–42 | 0.5–14 |
| Mean years qualified | 18 | 22 |
| Mean years qualified as prescriber (NPs only) | 16 | |
| Mean years at OOH service | 7 | 8 |
| Urban/rural/mixture (practice area) | urban: 5 | urban: 9 |
| rural: 0 | rural: 2 | |
| mixture: 10 | mixture: 4 | |
| Mean deprivation score (practice area) | 7 | 5 |
Experience of antibiotic prescribing in OOH
Theme 1: managing RTIs in primary care OOH
Participants described the process of communicating decisions about treatment when patients did not require antibiotics. Participants identified three stages that were reported to be iterative in nature: managing patient expectations, negotiating treatment and safety netting. Participants described factors that both facilitated and hindered this process.
Managing patient expectations There were a number of elements of patient expectations that reportedly influenced the experience of antibiotic prescribing. Most practitioners reported high perceived or explicitly reported patient expectations of antibiotic treatment in OOH services; however, a minority suggested that they were in fact seeing fewer cases of patient demand for antibiotics than in previous years. Clinicians perceived a need to ‘break the cycle’ of expectation, which they felt could be achieved by not prescribing antibiotics when clinically unnecessary. However, some respondents did report ‘giving in’ to perceived patient demand in OOH when under pressure to see patients quickly.
GPs also discussed the cost to health services of antibiotic prescriptions and lengthy consultations, and how any demand for antibiotics needed to be weighed against consideration of the overall cost to the NHS or the organization for whom they worked. Financial comments came from both GPs and NPs, in particular those in managerial or directorial positions who may be more inclined to consider costs to the organization as part of their everyday role. Participants reported that, even though consideration of cost factored into their decision making, they were unlikely to discuss this with the patient, and cost implications to the patient were not raised.
NPs reported professional identity as a key influence in patient expectations. They described patient distrust that a no-prescribing decision was bound up with the profession of nursing and felt patients tended to believe that they would have been prescribed an antibiotic had they seen a doctor instead. NPs were more inclined to highlight the need for consistent prescribing across the professions to avoid the potential for patients to experience differing inter-professional prescribing practices.
“…I find it tricky because sometimes I feel the patients think I'm not giving them antibiotics because I'm a nurse and that if they saw a doctor they would get them instead […] Sometimes, unfortunately, if they have not been happy with not getting them, and they've re-booked to see a doctor, sometimes they are then given them. So the next time I see them, it just makes it that much harder all over again to try and convince them […]” NP 20/1001, Private OOH Organization
Negotiating treatment Participants described the second stage of the communication process as a negotiation about treatment. Participants reported normalizing patient symptoms in order to aid patient understanding of illness severity and duration in RTIs, and how important these subtle communication practices were perceived to be.
“[I tell patients]…’this is normal; this is normal. That's really good. Your temperature's normal,'…this is what they've got and what the normal duration of that illness is…there's no need for antibiotics…I try and present that as a positive so, ‘Oh, the good news is you don’t need any antibiotics. You can manage this yourself at home.' It's about how you give that message really.” GP 17/1002, Private OOH
Providing a safety net in OOH The third and final phase of the communication process was patient safety-netting. This included a thorough explanation of possible side effects of antibiotics (if prescribed), an explanation of red flag symptoms of further complications and signposting to another health service.
“…I probably will never see that patient again, it is really about thoroughly going through with them what you expect to happen with this illness, depending on whether you've prescribed or not. Just making sure that they understand anything that they need to be looking out for, which they need to be concerned about and what they need to do about that. Where they need to go… .it’s about being really specific in that information.” NP 25/1000, Private OOH
Participants reported higher prescribing rates at the weekend, although decisions to prescribe were reportedly used as an additional safety net, depending on the medical cover available the following day.
“…it depends what sort of medical cover you've got the following day. For example, I might see a [patient] on a Saturday morning, knowing that there isn't any Sunday medical cover, and so it's just a bit of uncertainty about which way their infection is going to go and their degree of vulnerability, and I would want them to start treatment perhaps a little earlier than I might do if I could follow them up the next day. You're seeing people as a snapshot sometimes and you're not sure quite where the continuity lies down the line, so that could be more complex, yes.” GP 07/1002, NHS OOH
Factors facilitating treatment decisions There was general agreement between GPs and NPs on the strategies they use to support decision making about treatment. Delayed prescribing was reported by GPs and NPs as a useful aid for dealing with patient demand for antibiotics as well as encouraging shared decision making, shared management and providing a tool for safeguarding against further complications.
“Assuming they are systemically well, and they've had a short duration of symptoms, I would nearly always try to persuade them that antibiotics aren't needed, but for those patients who are difficult to persuade quite often I use a delayed or a deferred prescription and allow them to use their judgement as to whether they actually do need to go onto antibiotics at a later date.” GP 04/1000, NHS OOH
Peer discussion and education played an important role in supporting treatment decisions, as prescribers had the opportunity to discuss alternative prescribing techniques as well as to validate their own prescribing decisions. Patient education leaflets were reportedly utilized as a tool to support explanations when an antibiotic was not prescribed. NPs described them as being used as a way to reinforce their message and enhance their epistemic stance with their patient.
“But it's an actual piece of paper rather than just saying to patients, ‘Look, you’ve got a virus, go and take some paracetamol and lie down'. […] The fact that it's endorsed by all the important people at the bottom just gives it a bit more welly.” NP 13/1000, NHS OOH
Prescribers working in OOH highlighted how raising public awareness outside of the consultation can positively influence consultations. Some participants did, however, emphasize that this should be in addition to explanations within a consultation, as this was viewed as providing an important opportunity to educate patients and was thought to be effective.
Factors hindering treatment decisions GPs and NPs reported three perceived barriers to communicating management decisions in OOH care: a legitimized need for an exchange between the patient and the prescriber, which has been termed here as a ‘consultation exchange’; lack of feedback on delayed prescriptions; and perceptions of other prescriber approaches.
Acknowledging patient illness and any effort made to attend OOH was reported as an important aspect of care management negotiations and was closely linked to the perceived need for a consultation exchange, in which a patient expects something in return for their effort, and the clinician in turn feels they should do something for the patient in order to meet that expectation. Giving advice alone was not, in a lot of cases, perceived as sufficient.
“Sometimes it's the perceived need to do something. Particularly if somebody has been through a telephone assessment, they've been given an appointment so they've been indicated, ‘You need to be seen today.’ They've made a journey. They've waited. They've been seen. They then expect to get something. So there's a great big sort of built-in expectation that is created by that process. That can translate then into the clinician then feeling that they need to give them something to make that journey worthwhile and to feel that they've got something that's going to help them get better.” NP 11/1000, Non-Profit OOH
Lack of feedback on what patients do with a delayed antibiotic prescription was described as a barrier to using the delayed strategy, owing to a perceived likelihood of the prescription being ‘cashed in’ against medical advice.
“…we can’t follow the patients up, we don’t follow them through, we have no idea whether they actually follow the instructions for delaying the prescription or whether they actually go and cash in their prescription and start the antibiotics straightaway.” NP 18/1000, NHS OOH
Inconsistent prescribing approaches between prescribers were repeatedly reported as a barrier to negotiating care management decisions, as patient expectations were raised owing to past experience of being given an antibiotic for an RTI. In turn, this could make it much harder for prescribers to explain that an antibiotic is unnecessary on subsequent occasions.
Prescribing approaches differed between GPs and NPs and as a result had an impact on professional identity. GPs who had worked with NPs observed that NPs were more likely to work to protocol, to which they felt there were benefits and drawbacks. NPs tended to agree with this definition and saw this in a positive light; that this protocol meant their decisions were made based on the facts before them and supported by local and national guidelines. GPs reported they would often prescribe differently from the guidelines and base their prescribing decisions on ‘gut feeling’. Both types of prescribers felt that GPs would be able to deal with more complex patients than NPs.
“I think it's quite complicated and a nurse will more likely work to a protocol, which is a good thing if you're looking at objective performance but also can be a difficulty for them if the protocol doesn't meet all the variables that the patient's presenting with…I don't actually quite know whether nurses prescribe more antibiotics than doctors. I bet they prescribe less actually.” GP 07/1002, NHS OOH
“…as I’ve become more experienced…I’m more aware now, I suppose, of the – the complexities of certain patients, I think that’s something that GPs would have more readily at their fingertips.” NP 16/1000, NHS OOH
Theme 2: factors influencing the decision to prescribe antibiotics in OOH
Organizational factors There were no differences between participants from private and NHS settings when describing organizational factors that influence prescribing. Access to patient GP records was variable; some reported no access whereas some prescribers reported having access to electronic patient records when general practices had agreed to allow such access. Those without access reported that it led to uncertainty and additional pressure to make the correct prescribing decisions.
“But, out of hours you're just seeing them on that spot, you're just seeing them once and somebody else is going to see them afterwards. Therefore you need to make the correct decision every time just once knowing that you might not see that patient, or the next thing you might see the GMC or the complaint. Therefore it just causes you more hassle for yourself eventually I guess. So that should be – yes, that should be the huge difference I guess.” GP 01/1000, NHS OOH
NPs reported having more time to spend with patients, whereas GPs highlighted how consultation time and the pressure to end a consultation influenced the likelihood of providing an antibiotic prescription during a busy OOH shift. Appointment time was reported to be variable between organizations as well as between GPs and NPs. When there was no appointment system, participants reported that they were still aware of the time they spent with each patient, especially during busy shifts when there was a long wait to be seen, and as such time remained a factor that influenced their decision to prescribe an antibiotic.
“…sometimes you're rushed, sometimes it can be easier to give the antibiotics rather than having a discussion with them each time.” GP 14/1000, NHS OOH
“We’re really, really fortunate here…our appointment times, if you’re booked into the nurse clinic, they’re half-hour appointments, so we can really spend time providing the education and explaining why we’re not giving antibiotics.” NP 13/1000, NHS OOH
Working contracts in OOH were reported to be challenging owing to a constantly changing workforce, in which clinicians all worked in different ways, including varying shift patterns. This was also reported to be different between GPs and NPs; NPs tended to be full-time members of staff and GPs reportedly worked on a bank or ad hoc basis. This changing workforce reportedly causes difficulty in maintaining consistency with regards to providing training and education, increasing the likelihood that antibiotics would be prescribed against local guidelines.
“…if you've got a transient clinical population, clinical workforce, you can't train them up, you can't educate them, you can't support them, they just come in and…I was going to say dole out antibiotics, I'm sure they don't do that, but it's easier if you're going to tootle off to another organization the next day.” GP 05/1000, Private Non-Profit OOH
A common perception across interviews with NPs was reports of their feeling more accountable for their prescribing than their GP counterparts.
“…I just don't think [doctors] see that it's not a problem right now rather than the future. So, that one prescription doesn't really matter, do you know what I mean? There's no accountability for it and no one is going to pull them up five years down the line and say, ‘You shouldn’t have given that prescription’, so the prescribing responsibility isn't there…part of being a responsible prescriber is sometimes not prescribing and I'll say that to my patients…it's not appropriate. It's not going to help. It's not going to help in the bigger picture at all'.” NP 13/1000, NHS OOH
GPs argued that their perception of accountability was linked to a lack of follow-up and a perceived need to ‘do something’ for the patient in the OOH setting.
“I think you're more likely to get prescribed antibiotics in the out-of-hours setting. One, is accountability, so you're not ever going to see that patient again in the out-of-hours setting. It's not really your issue. If you give them antibiotics and they go away, you can feel quite happy that you've done something […].” GP 17/1002, Private OOH
Audit, feedback and/or supervision were reported to be very important in OOH prescribing as this was thought to help inform future prescribing decisions and this was common across both GP and NP respondents. The amount of auditing described by some participants highlights that antibiotic prescribing is high on the OOH agenda.
“…it's something that's a piece of priority work for me and my team here, so we're doing a lot of work with our prescribers, both in terms of auditing, so we understand how much prescribing's going on. We also are looking at appropriateness of prescribing, so auditing case notes against the local guidelines and providing feedback to prescribers about how they're doing. So it's high up on our agenda.” NP 11/1000, Non-Profit OOH
Patient factors Participants reported that perceived patient anxiety in OOH, when compared with patients attending in-hours services, could lead to prescriber anxiety during a consultation influencing prescribing decisions, especially when considering more vulnerable patients such as children and the elderly.
“Amongst parents particularly that concern that they need to do something for their child and they have that anxiety that their child won't get better or will become very unwell. They bring that to the consultation saying, ‘Here’s my child. They're sick. I'm really worried about them. Do something for them please.' That fear perhaps that if you don't do something this might be the one child who got worse.” NP 11/1000, Private Non-Profit OOH
Participants reported a perception that patients are generally sicker when they attend OOH services than in-hours services. With an inability to follow up patients, this appeared to translate into a perceived higher clinical risk and therefore an increased likelihood of antibiotics being prescribed.
“…out-of-hours you are taking more risks in a way because there isn't quite the same sort of follow-up. You're generally tending to deal with sicker patients than you are on a day-to-day practice in general practice…therefore I think it probably makes you a little bit more cautious in out-of-hours.” GP 02/1000, Private OOH
A patient’s inability to reaccess OOH should they need to suggested an increased likelihood of antibiotics being prescribed, as prescribers described a preference to reduce risk whenever possible.
“…most general members of the public…they can come back if they need that prescription, so unless they were off travelling or if you've got like a really brittle asthmatic…but unless they're going abroad, unless they're going somewhere where they can't access a healthcare professional, then I'd be very reluctant.” NP 13/1000, NHS OOH
Patient–practitioner rapport in OOH was reported to be a particular challenge because prescribers have no prior relationship with their patients. Responses varied depending on the direction of influence, as some reported this would change their prescribing behaviour and others argued that their prescribing would not change regardless of prior knowledge of the patient.
“No, it doesn't matter who they are, whether I've built a rapport with them, whether I know them or not, it makes no difference whatsoever.” NP 22/1000, NHS OOH
“I think when you don't know them, it's not just about knowing about their medical history but also you don't know them as a person, I think it can be quite difficult to build up a rapport in a rushed setting…it's all about how they perceive you as a doctor I think and how you get on with them as well…” GP 14/1000, NHS OOH
Prescribers reported assessing patients to determine their awareness and understanding of the topic discussed within a consultation and that this assessment would influence their decision of whether or not to prescribe, particularly when dispensing a delayed antibiotic prescription.
“I don't like really giving delay prescriptions unless I really feel that they can take on board the information about using that.” NP 13/1000, NHS OOH
Discussion
Participants reported very similar barriers to prudent antibiotic prescribing as in previous literature that included clinicians working ‘in-hours’.30 This study, however, identifies the specific OOH contextual factors that also influence antibiotic prescribing. These include organizational factors such as access to patient GP records, which requires organizational change, and working contracts in which there is no consistency or team approach to prescribing, suggesting that interventions could encourage team clinical professional development in OOH staff groups. Implementation of feedback, audit and supervision is already done in primary care, but these findings suggest that prescribing advisers from local CCGs or similar groups could give feedback to OOH services and specify individual prescribers. More severe cases also tend to present in OOH, which needs to be recognized. When there is no prior relationship with or knowledge of the patient, practitioners may not gain a patient’s trust within a consultation, suggesting that good communication skills are vital in the OOH setting. Interventions with communication skill elements already exist and as such it may be prudent to tailor such interventions to the OOH setting. Similarities were noted in GP’s and NP’s experiences of making antibiotic prescribing decisions in OOH compared with those working in usual in-hours general practice, which were comparable with previous literature.30
The findings suggest that interventions being developed to promote prudent antibiotic prescribing should focus on ways to make this process more transparent in OOH, by providing such usage data to healthcare professionals and using communication tools to help reduce the impact of the barriers described above. Geographical and organizational location was not reported to impact antibiotic prescribing decisions; the only pattern in variability appeared to be between professional groups.
Differences between GP and NP antibiotic prescribing in OOH
NPs in this study highlighted the difficulties surrounding another clinician prescribing an antibiotic following a no-prescribing decision. Feeling a lack of trust from patients when they do not prescribe, NPs described providing evidence for their decision making through information materials, national guidance and explanations of the implications of over-prescribing in terms of side effects and the global issue of resistant bacteria. Any differences between types of healthcare professionals in their antibiotic prescribing can create problems between professions but inconsistent prescribing between individuals also sends mixed messages to patients. These findings therefore suggest a need to improve communication and closer working between all types of prescribers to help promote consistent practice.
Previous research14 has reported that a ‘fragmentation’ of workload for temporary or contract workers, in relation to in-hour GP practices, could contribute to clinicians being more likely to prescribe antibiotics. The current study suggests that small local changes in OOH services could help improve prudent prescribing decisions, utilizing experiences from OOH services that have implemented these changes.
The study findings are in line with previous research suggesting that improving accountability may help improve antibiotic prescribing should prescribing data be provided to individual prescribers.31 NPs felt the accountability placed on them via audit and feedback systems and clinical supervision improved their ability to make more prudent decisions around antibiotic prescribing and encouraged the implementation of good communication skills to provide advice rather than treat with a prescription. This finding highlights that NPs may currently receive more feedback about their prescribing than GPs, a model that could be applied to other healthcare professionals. This resonates with previous research that highlights that NPs are more concerned with justification of antibiotic prescribing owing to accountability and are therefore less likely to prescribe an antibiotic.17 NP participants in this study suggest that more complex cases should be seen by GPs and highlighted differences in clinical training between professions and how this affects communicating prescribing decisions. This suggests that both GPs and NPs could learn communication techniques from each other, which could be implemented via an intervention to improve prudent antibiotic prescribing.
Studies have indicated that attempts to reduce prescribing will also require clinicians to be receptive to change, to have confidence in their own decision making and to be prepared to invest time and effort into explaining their prescribing decision.19 Tailoring interventions that train clinicians in enhanced communication skills have been shown to be effective at reducing antibiotic prescribing in in-hours general practice and could also be useful for implementation in OOH.32,33
These findings suggest that clinicians would rather their patients reconsult in order to reduce the likelihood of further complication, but clinicians feared that patients would choose not to or would not be able to reconsult. Therefore, these factors should be given due consideration for any intervention being used in the OOH setting.
Patient expectations and a perceived need for a consultation exchange has been highlighted as a barrier to prescribing decisions. Involving the patient in decision making is useful in promoting appropriate antibiotic use.34 Participants suggest that more emphasis could be applied to providing advice to patients, whether in a consultation or via public health campaigns. This is an example of how organizational changes and interventions looking to improve prudent prescribing locally could have a positive influence on the number of antibiotic prescriptions given to patients.
Strengths and limitations
The study utilized purposive sampling of primary care OOH GPs and NPs in England and captured a broad view of antibiotic prescribing for RTIs in this setting. Individual- and service-level prescribing data were not available, which may have helped further ensure maximum variation of the sample. Recruitment was excellent and owing to a broad recruitment and sampling approach that allowed over 1000 prescribers the opportunity to participate, maximum variation sampling of a wide range of staff from across England was employed. The response rate was small (8.94%), however, which is typical for this type of research. The sample collected was varied according to key parameters and the findings resonate with other published research, which increases confidence in the face validity and transferability of the findings. The research adds novel findings to the literature and is the first of its kind to explore the views of GPs and NPs on antibiotic prescribing in NHS OOH services in primary care. The interviewers took a non-judgemental stance and all participants were able to discuss their antibiotic prescribing openly.
Future research
Following this study it is suggested that further qualitative research is warranted to explore other professions prescribing antibiotics for common infections in OOH (e.g. pharmacists and physiotherapists). It may also be beneficial to explore patient views and experiences of attending OOH for an RTI as well as patient satisfaction rates in primary care OOH. Finally, empirical insights into the conversations that practitioners have with their patients could help to understand the interactional challenges to prudent prescribing and will be the topic of further research. This research suggests a need to tailor existing interventions and trial these in an OOH setting and the publication of these novel data may be of use to other research teams developing such interventions.
Conclusions
OOH and a mixed healthcare workforce provide particular difficulties when prescribing antibiotics for RTIs, which would need to be considered in tailoring interventions to promote prudent antibiotic prescribing in this setting. The findings suggest that small organizational changes locally, such as improving access to patient GP records, encouraging training as an OOH team to promote consistent delivery of care to include all types of prescribers, individual audit and feedback for all prescribers, and communication skills training could improve prudent antibiotic prescribing at a local level when supported by OOH provider systems.
Supplementary Material
Acknowledgements
We would like to thank the NIHR Clinical Research Network and the Association for Prescribers for their support in disseminating study information to potential participants, which ultimately led to the successful completion of the study. We would also like to thank the health professionals who showed an interest in the study and to those who took the time to participate in interviews and share their views and experiences.
Funding
The UNITE study was funded by the National Institute of Health Research School for Primary Care Research (NIHR SPCR reference number 275).
Transparency declarations
None to declare.
Disclaimer
The views are those of the authors and not necessarily those of the NIHR, the NHS or the Department of Health.
Supplementary data
The interview guide is available as Supplementary data at JAC Online.
References
- 1. National Institute for Health and Care Excellence. Respiratory Tract Infections (Self-Limiting): Prescribing Antibiotics. London: NICE, 2008. https://www.nice.org.uk/guidance/cg69/resources/respiratory-tract-infections-selflimiting-prescribing-antibiotics-975576354757. [PubMed] [Google Scholar]
- 2. Public Health England. English Surveillance Programme for Antimicrobial Utilisation and Resistance (ESPAUR) Report 2010 to 2013. PHE, 2014.
- 3. Gulliford MC, Dregan A, Moore MV. et al. Continued high rates of antibiotic prescribing to adults with respiratory tract infection: survey of 568 UK general practices. BMJ Open 2014; 4: e006245.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Costelloe C, Metcalfe C, Lovering A. et al. Effect of antibiotic prescribing in primary care on antimicrobial resistance in individual patients: systematic review and meta-analysis. BMJ 2010; 340: c2096.. [DOI] [PubMed] [Google Scholar]
- 5. Dagan R, Leibovitz E, Greenberg D. et al. Dynamics of pneumococcal nasopharyngeal colonization during the first days of antibiotic treatment in pediatric patients. Pediatr Infect Dis J 1998; 17: 880–5. [DOI] [PubMed] [Google Scholar]
- 6. Davies S. Annual Report of the Chief Medical Officer 2011: Infections and the Rise of Antimicrobial Resistance London: Department of Health, 2011. [DOI] [PubMed]
- 7. Public Health England. English Surveillance Programme for Antimicrobial Utilisation and Resistance (ESPAUR) Report 2016 PHE, 2016.
- 8. Public Health England. Management and Treatment of Common Infections: Antibiotic Guidance for Primary Care: For Consultation and Local Adaptation Report 2017. PHE, 2017.
- 9. Spinks A, Glasziou PP, Del Mar CB.. Antibiotics for sore throat. Cochrane Database Syst Rev 2013; issue 11: CD0000023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. NHS England. About NHS Services. Emergency and Urgent Care Services http://www.nhs.uk/NHSEngland/AboutNHSservices/Emergencyandurgentcareservices/Pages/nhs-out-of-hours-services.aspx.
- 11. Huibers LAMJ, Moth G, Bondevik GT. et al. Diagnostic scope in out-of-hours primary care services in eight European countries: an observational study. BMC Fam Pract 2011; 12: 30.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hayward GN, Fisher RFR, Spence GT. et al. Increase in antibiotic prescriptions in out-of-hours primary care in contrast to in-hours primary care prescriptions: service evaluation in a population of 600000 patients. J Antimicrob Chemother 2016; 71: 2612–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. McNulty CAM, Nichols T, French DP. et al. Expectations for consultations and antibiotics for respiratory tract infection in primary care: the RTI clinical iceberg. Br J Gen Pract 2013; 63: e429–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Strandberg EA, Brorsson A, Hagstam C. et al. “I’m Dr Jekyll and Mr Hyde”: are GPs’ antibiotic prescribing patterns contextually dependent? A qualitative focus group study. Scand J Prim Health Care 2013; 31: 158–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Spurling GKP, Del Mar CB, Dooley L. et al. Delayed antibiotic prescriptions for respiratory infections. Cochrane Database Syst Rev 2017; issue 9: CD004417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Little P, Moore M, Kelly J. et al. Delayed antibiotic prescribing strategies for respiratory tract infections in primary care: pragmatic, factorial, randomised controlled trial. BMJ 2014; 348: g1606.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Peters S, Rowbotham S, Chisholm A. et al. Managing self-limiting respiratory tract infections: a qualitative study of the usefulness of the delayed prescribing strategy. Br J Gen Pract 2011; 61: e579–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Ryves R, Eyles C, Moore M. et al. Understanding the delayed prescribing of antibiotics for respiratory tract infection in primary care: a qualitative analysis. BMJ Open 2016; 6: e011882.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Brookes-Howell L, Hood K, Cooper L. et al. Understanding variation in primary medical care: a nine-country qualitative study of clinicians’ accounts of the non-clinical factors that shape antibiotic prescribing decisions for lower respiratory tract infection. BMJ Open 2012; 2: e000796.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. McIsaac W, Butler CC.. Does clinical error contribute to unnecessary antibiotic use? Med Decis Making 2000; 20: 33–8. [DOI] [PubMed] [Google Scholar]
- 21. Edelstein M, Raj T, Agbebiyi A. et al. “Just in case”: antibiotic prescribing behaviour among out-of-hours practitioners in England In: Abstracts of the Twenty-Sixth European Congress of Clinical Microbiology and Infectious Diseases, Amsterdam, The Netherlands, 2016. Abstract EP0129. ESCMID, Basel, Switzerland. [Google Scholar]
- 22. Rowbotham S, Chisholm A, Moschogianis S. et al. Challenges to nurse prescribers of a no-antibiotic prescribing strategy for managing self-limiting respiratory tract infections. J Adv Nurs 2012; 68: 2622–32. [DOI] [PubMed] [Google Scholar]
- 23. Courtney M, Rowbotham S, Lim R. et al. Antibiotics for acute respiratory tract infections: a mixed methods study of patient experiences of non-medical prescriber managements. BMJ Open 2017; 7: e013515.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Moth G, Huibers L, Vedsted P.. From doctor to nurse triage in Danish out-of-hours primary care service: simulated effects on costs. Int J Family Med 2013; 2013: 987834.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Patton MQ. Qualitative Evaluation and Research Methods, 2nd edn Newbury Park, CA: Sage Publication, 1990. [Google Scholar]
- 26. Patton MQ. Qualitative Research and Evaluation Methods, 3rd edn Thousand Oaks, CA: Sage Publications, 2002. [Google Scholar]
- 27. Braun V, Clarke V.. Using thematic analysis in psychology. Qual Res Psychol 2006; 3: 77–101. [Google Scholar]
- 28. Walker D, Myrick F.. Grounded theory: an exploration of process and procedure. Qual Health Res 2006; 16: 547–59. [DOI] [PubMed] [Google Scholar]
- 29. Hammersley M. What’s Wrong with Ethnography? London: Routledge, 1992. [Google Scholar]
- 30. Tonkin-Crine S, Yardley L, Little P.. Antibiotic prescribing for acute respiratory tract infections in primary care: a systematic review and meta-ethnography. J Antimicrob Chemother 2011; 66: 2215–23. [DOI] [PubMed] [Google Scholar]
- 31. Ivers N, Jamtvedt G, Flottorp S. et al. Audit and feedback: effects on professional practice and healthcare outcomes. Cochrane Database Syst Rev 2012; issue 6: CD000259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Little P, Stuart B, Francis N. et al. ; on behalf of the GRACE consortium. Effects of internet-based training on antibiotic prescribing rates for acute respiratory-tract infections: a multinational, cluster, randomised, factorial, controlled trial. Lancet 2013; 382: 1175–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Butler CC, Simpson SA, Dunstan F. et al. Effectiveness of multifaceted educational programme to reduce antibiotic dispensing in primary care: practice based randomised controlled trial. BMJ 2012; 344: d8173.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Butler CC, Rollnick S, Pill R. et al. Understanding the culture of prescribing: qualitative study of general practitioners’ and patients’ perceptions of antibiotics for sore throats. BMJ 1998; 317: 637–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.