Abstract
Background
Echinocandins are recommended as first-line therapy against Candida glabrata infections, although increased resistance to this class has been reported worldwide and they are currently only available for parenteral administration. SCY-078 is an investigational glucan synthase inhibitor that is orally available.
Objectives
To evaluate the in vivo efficacy of SCY-078 in an experimental model of invasive candidiasis due to WT and echinocandin-resistant C. glabrata isolates.
Methods
Neutropenic ICR mice were inoculated intravenously with a WT isolate (SCY-078 and caspofungin MICs 0.25 and 0.125 mg/L, respectively) or an echinocandin-resistant isolate (SCY-078 and caspofungin MICs 1 and 0.5 mg/L, respectively). Treatment with placebo, SCY-078 (8, 30 or 40 mg/kg orally every 12 h) or caspofungin (1 mg/kg by intraperitoneal injection once daily) began 24 h later. Kidney fungal burden was measured on day 8 post-inoculation.
Results
Significant reductions in kidney fungal burden were observed with 30 mg/kg SCY-078 against both isolates and with the 40 mg/kg dose against the echinocandin-resistant isolate. These results were supported by SCY-078 plasma concentration data at the higher doses, where levels above the MICs for both isolates were observed 12 h after the last oral dose. Reductions in fungal burden were also observed with caspofungin against the WT isolate, but not against the resistant isolate.
Conclusions
SCY-078 demonstrated in vivo efficacy against infections caused by both WT and echinocandin-resistant C. glabrata isolates in this experimental model. This orally available glucan synthase inhibitor has potential as a therapy against echinocandin-resistant C. glabrata infections.
Introduction
In the USA, the second most prevalent species associated with invasive infection is Candida glabrata.1,2 Current treatment strategies for invasive infections caused by C. glabrata include the use of azoles, amphotericin B or echinocandins. Although effective, each of these classes has drawbacks that may limit clinical responses. For example, amphotericin B formulations are associated with nephrotoxicity and are only available intravenously. The echinocandins, although clinically safer than the polyenes, are also only available for intravenous administration, which may limit their use in outpatients. Fluconazole has been a safe and effective treatment option for many years for patients with invasive candidiasis and this antifungal is available in both oral and intravenous formulations. However, recent epidemiological studies have also demonstrated that fluconazole and echinocandin resistance in C. glabrata is increasing at many centres in the USA and worldwide.3–6 Thus, the development of new therapeutic strategies for invasive candidiasis, including those infections caused by C. glabrata, is of paramount importance.
SCY-078 is an investigational glucan synthase inhibitor that has potent in vitro activity against Candida species, including isolates with mutations in fks1 hot-spot regions that confer resistance to echinocandins.7 This agent is also being developed for oral administration and thus may also overcome the limitation of the need for intravenous administration. The objective of this study was to evaluate the in vivo efficacy of SCY-078 administered orally against invasive candidiasis caused by both WT and echinocandin-resistant C. glabrata isolates.
Materials and methods
Antifungals
SCY-078 (Scynexis, Inc., Jersey City, NJ, USA) was provided in a methylcellulose formulation for oral administration. The pharmaceutical formulation of caspofungin was used in the in vivo model. For in vitro susceptibility testing, powders of both agents were dissolved in DMSO and further dilutions were prepared in RPMI medium buffered with 0.165 M MOPS (pH 7.0).
Isolates
Both a susceptible WT C. glabrata isolate (05-761) and an echinocandin-resistant isolate (05-62; R1379S Fks2p amino acid substitution) were used. Antifungal susceptibility testing was performed per the CLSI M27-A3 methods with MICs read after 24 h of incubation at 50% inhibition of growth for both SCY-078 and caspofungin.8 Prior to use in the in vivo model, isolates were subcultured at 37 °C for 48 h on Sabouraud dextrose agar three times before being washed in sterile saline with 0.1% Tween 20. Inoculum viability was determined by serially diluting an aliquot and plating it on Sabouraud dextrose agar to determine the number of cfu after incubation at 37 °C.
Murine model
We utilized our established murine models of invasive candidiasis.9–12 Outbred ICR male mice (Harlan) were housed five per cage and were rendered neutropenic with a single dose of 5-fluorouracil (150 mg/kg) administered intravenously 1 day prior to infection. Although this immunosuppression is temporary, mice are rendered neutropenic (<2 × 109 neutrophils/L with a nadir of <1 × 109/L) on days 1–8 post-inoculation, which corresponds to the duration of treatment and fungal burden analysis in this model. On the day of inoculation, animals were infected intravenously with 0.2 mL of C. glabrata with the number of Candida cells per animal adjusted to body weight (e.g. 4 × 106C. glabrata cells/g = 1.0 × 108 cells per mouse for a 25 g mouse). Mice were monitored at least twice daily throughout the study to prevent and minimize unnecessary pain or distress post-inoculation. One day after inoculation, therapy was started with a placebo (methylcellulose), SCY-078 (8, 30 or 40 mg/kg by oral gavage every 12 h) or caspofungin (1 mg/kg by intraperitoneal injection once daily) and continued for 7 days. This dose of caspofungin was chosen based on our previous experience with this echinocandin against invasive candidiasis caused by resistant Candida species,9,13,14 and the extensive tissue exposure that is achieved with repeated dosing, which exceeds the MIC90 for C. glabrata.15,16 Mice were humanely euthanized on day 8, ∼12 h after the last dose of SCY-078. The kidneys were aseptically removed, weighed and homogenized, and serial dilutions of the homogenates were plated on Sabouraud dextrose agar. After 24 h of incubation, the number of cfu/g was calculated. Blood was also collected from the anaesthetized mice treated with SCY-078 via cardiac puncture. The plasma was separated and SCY-078 concentrations were measured. All animals were maintained in accordance with the Association for the Assessment and Accreditation of Laboratory Animal Care and this study was approved by the Institutional Animal Care and Use Committee at UTHSCSA (protocol no. 16038x).
SCY-078 plasma concentrations
Plasma samples were analysed by LC-MS/MS after protein precipitation as previously described.17
Data analysis
Differences in kidney fungal burden (cfu/g) and plasma concentrations among the groups were assessed for significance by ANOVA with Tukey’s post-test for multiple comparisons. A P value of ≤0.05 was considered statistically significant for all comparisons.
Results
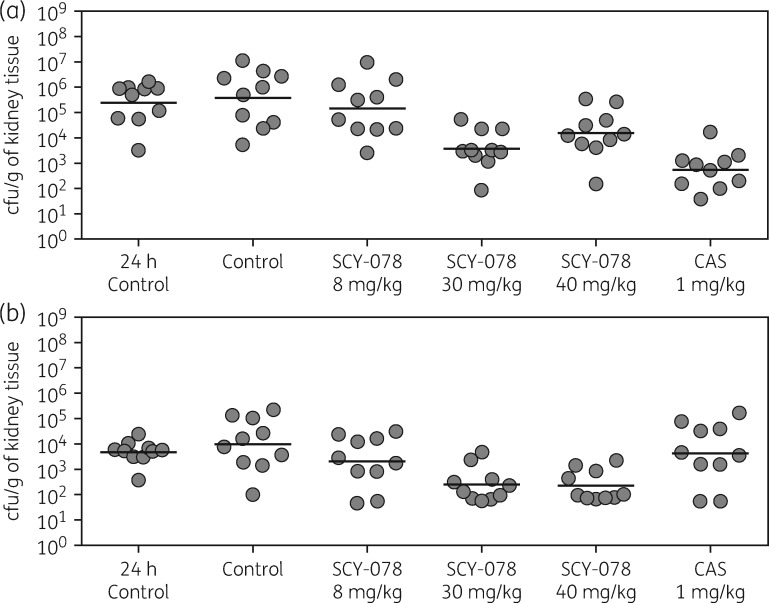
Fungal burden: WT isolate
SCY-078 was effective at reducing kidney fungal burden in this experimental model of invasive candidiasis caused by C. glabrata. Oral administration of SCY-078 at doses of 30 mg/kg significantly reduced the number of cfu (mean log10 cfu/g ± SD 3.57 ± 0.79) in the kidneys of mice infected with the WT isolate compared with both fungal burden measured prior to the start of therapy (24 h post-inoculation, 5.38 ± 0.85 log10 cfu/g) and on day 8 in mice administered a placebo (5.58 ± 1.11 log10 cfu/g; P < 0.01 for both comparisons) (Figure 1a). Caspofungin also resulted in a significant reduction in the fungal burden compared with that observed prior to the start of therapy and in the placebo group on day 8 (2.74 ± 0.76 log10 cfu/g; P < 0.01 for both comparisons). Neither SCY-078 at 8 mg/kg nor 40 mg/kg significantly reduced the fungal burden, although there was a trend with the higher dose compared with the placebo group (4.18 ± 0.96 log10 cfu/g; P = 0.074).
Figure 1.
Kidney fungal burden in mice infected with (a) the WT C. glabrata isolate and (b) the echinocandin-resistant isolate at 24 h post-inoculation just prior to the start of therapy and on day 8 in mice treated with placebo, SCY-078 or caspofungin. CAS, caspofungin.
Fungal burden: echinocandin-resistant isolate
SCY-078 was also effective against infection caused by the echinocandin-resistant isolate (Figure 1b). Both the 30 and 40 mg/kg doses of SCY-078 significantly reduced the fungal burden (2.38 ± 0.66 and 2.34 ± 0.60 log10 cfu/g, respectively) compared with that measured prior to the start of therapy (3.66 ± 0.46 log10 cfu/g; P ≤ 0.03 for both comparisons) and in the placebo group on day 8 (3.99 ± 1.04 log10 cfu/g; P < 0.01 for both comparisons). As expected, caspofungin was ineffective against infection caused by the resistant isolate, as the fungal burden remained unchanged (3.61 ± 1.22 log10 cfu/g). As observed against the WT isolate, 8 mg/kg SCY-078 was ineffective.
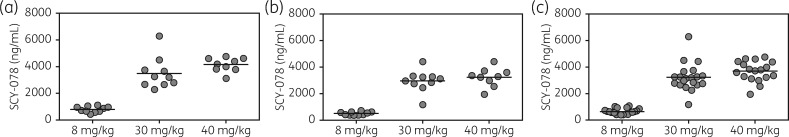
SCY-078 plasma concentrations
Bloodstream levels of SCY-078 were also elevated in mice treated with the 30 and 40 mg/kg doses. As shown in Figure 2, plasma concentrations at these two doses remained higher than the MICs for both the WT (SCY-078, 0.25 mg/L; caspofungin, 0.125 mg/L) and echinocandin-resistant (SCY-078, 1 mg/L; caspofungin, 0.5 mg/L) isolates 12 h after dosing had stopped (combined mean 3.225 ± 1.023 and 3.683 ± 0.761 mg/L, respectively). These concentrations were significantly higher than those achieved with the 8 mg/kg dose, which were similar to the MICs for the isolates used in this study (0.645 ± 0.221 mg/L; P < 0.01). The plasma concentrations for SCY-078 were also consistent between the experiments involving the WT and resistant isolates.
Figure 2.
SCY-078 plasma concentrations at ∼12 h after the last dose in mice infected with (a) the WT C. glabrata isolate and (b) the echinocandin-resistant isolate. (c) Combined results.
Discussion
SCY-078 is an investigational semi-synthetic derivative of enfumafungin that inhibits glucan synthase, leading to a decrease in (1,3)-β-d-glucan polymers and a weakening of the fungal cell wall.18 This agent is structurally different from the echinocandins, which act in the same fashion. Unlike the echinocandins, SCY-078 is also absorbed from the gastrointestinal track following oral administration. Potent in vitro activity for SCY-078 has been reported against Candida species, including some isolates that harbour fks1 and fks2 point mutations that cause echinocandin resistance.18 Efficacy has also been reported in an established murine model of infection caused by Candida albicans, C. glabrata and Candida tropicalis.19 In this previous study, the SCY-078 MICs for the C. glabrata isolates ranged from 0.03 to 0.25 mg/L and it is unknown whether any of these were echinocandin-resistant or harboured fks mutations.
The results of our study support the in vitro findings that SCY-078 maintains activity against echinocandin-resistant C. glabrata isolates. This agent was effective at reducing the kidney fungal burden against both WT and resistant isolates in our established neutropenic murine model. At the most effective oral dose used, SCY-078 resulted in a 1.28–1.81 log10 cfu/g reduction in fungal burden compared with that measured prior to the start of therapy and a 1.61–2.01 log10 cfu/g reduction compared with that of mice administered placebo. These results were supported by the plasma concentrations that were achieved 12 h after the last oral dose of SCY-078 and result in exposures that are achievable in humans.17,20 Interestingly, the highest dose of SCY-078 did not result in a statistically significant reduction in fungal burden against the WT isolate. Although paradoxical reductions in activity have been reported for the echinocandins at higher concentrations against Candida species, which also target the production of (1,3)-β-d-glucan polymers, this has not been observed against C. glabrata,21,22 and was not observed when SCY-078 was tested in vitro against the WT isolate in this study. Thus, the lack of a statistically significant reduction in fungal burden at the highest dose used against this isolate may be due to model variability, as there was a trend toward a reduction in fungal burden (P = 0.074 as reported above).
Overall, these results suggest that SCY-078 may be potentially useful for the treatment of invasive C. glabrata infections, including those caused by echinocandin-resistant isolates. One limitation of this study is the use of a resistant isolate with a relatively rare fks mutation compared with other more frequent mutations that lead to higher echinocandin MICs (e.g. Fks1p S629P, Fks2p S663P, F659S and F659del).4,5,23,24 Thus, it cannot be extrapolated that SCY-078 would maintain in vivo efficacy against all fks mutations. However, in another experiment conducted by our group, SCY-078 did maintain in vitro activity compared with caspofungin against two resistant C. glabrata isolates, including one harbouring a S629P amino acid change in Fks1p and the other a F659del in Fks2p (SCY-078 MICs 1 and 0.5 mg/L versus caspofungin MICs >8 and 8 mg/L, respectively). Thus, further in vivo studies with other isolates harbouring different fks mutations are warranted.
Acknowledgments
Funding
This project utilized preclinical services funded by the National Institute of Allergy and Infectious Diseases, National Institutes of Health, Department of Health and Human Services, under Contract Nos. HHS272201000018I and HHSN272201000038I - Task Orders A10 and A93, respectively.
Transparency declarations
N. P. W. has received research support to the UT Health San Antonio from Astellas, bioMérieux, F2G, Merck, Revolution Medicines and Viamet, and has served on advisory boards for Merck, Astellas, Toyama and Viamet. L. K. N. has received travel support from Viamet Pharmaceuticals, Inc. T. F. P. has received research grants to UT Health San Antonio from Astellas, Merck and Revolution Medicines, and has served as a consultant for Astellas, Merck, Revolution Medicines, Toyama, Viamet and Scynexis. All other authors: none to declare.
References
- 1. Pappas PG, Rex JH, Lee J. et al. A prospective observational study of candidemia: epidemiology, therapy, and influences on mortality in hospitalized adult and pediatric patients. Clin Infect Dis 2003; 37: 634–43. [DOI] [PubMed] [Google Scholar]
- 2. Yapar N. Epidemiology and risk factors for invasive candidiasis. Ther Clin Risk Manag 2014; 10: 95–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Pham CD, Iqbal N, Bolden CB. et al. Role of FKS mutations in Candida glabrata: MIC values, echinocandin resistance, and multidrug resistance. Antimicrob Agents Chemother 2014; 58: 4690–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Beyda ND, John J, Kilic A. et al. FKS mutant Candida glabrata: risk factors and outcomes in patients with candidemia. Clin Infect Dis 2014; 59: 819–25. [DOI] [PubMed] [Google Scholar]
- 5. Alexander BD, Johnson MD, Pfeiffer CD. et al. Increasing echinocandin resistance in Candida glabrata: clinical failure correlates with presence of FKS mutations and elevated minimum inhibitory concentrations. Clin Infect Dis 2013; 56: 1724–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Vallabhaneni S, Cleveland AA, Farley MM. et al. Epidemiology and risk factors for echinocandin nonsusceptible Candida glabrata bloodstream infections: data from a large multisite population-based candidemia surveillance program, 2008-2014. Open Forum Infect Dis 2015; 2: ofv163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Jimenez-Ortigosa C, Paderu P, Motyl MR. et al. Enfumafungin derivative MK-3118 shows increased in vitro potency against clinical echinocandin-resistant Candida species and Aspergillus species isolates. Antimicrob Agents Chemother 2014; 58: 1248–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Clinical and Laboratory Standards Institute. Reference Method for Broth Dilution Antifungal Susceptibility Testing of Yeasts—Third Edition: Approved Standard M27-A3. CLSI, Wayne, PA, USA, 2008. [Google Scholar]
- 9. Wiederhold NP, Najvar LK, Bocanegra R. et al. In vivo efficacy of anidulafungin and caspofungin against Candida glabrata and association with in vitro potency in the presence of sera. Antimicrob Agents Chemother 2007; 51: 1616–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Brzankalski GE, Najvar LK, Wiederhold NP. et al. Evaluation of aminocandin and caspofungin against Candida glabrata including isolates with reduced caspofungin susceptibility. J Antimicrob Chemother 2008; 62: 1094–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Najvar LK, Bocanegra R, Wiederhold NP. et al. Therapeutic and prophylactic efficacy of aminocandin (IP960) against disseminated candidiasis in mice. Clin Microbiol Infect 2008; 14: 595–600. [DOI] [PubMed] [Google Scholar]
- 12. Wiederhold NP, Najvar LK, Fothergill AW. et al. The novel arylamidine T-2307 demonstrates in vitro and in vivo activity against echinocandin-resistant Candida glabrata. J Antimicrob Chemother 2016; 71: 692–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Wiederhold NP, Najvar LK, Bocanegra RA. et al. Caspofungin dose escalation for invasive candidiasis due to resistant Candida albicans. Antimicrob Agents Chemother 2011; 55: 3254–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Wiederhold NP, Najvar LK, Jaramillo R. et al. The novel antifungal VL-2397 demonstrates efficacy in an in vivo model of invasive candidiasis caused by wild-type and multi-drug resistant Candida glabrata In: Abstracts of ASM Microbe, New Orleans, LA, USA, 2017. Abstract 3299. American Society for Microbiology, Washington, DC, USA.
- 15. Louie A, Deziel M, Liu W. et al. Pharmacodynamics of caspofungin in a murine model of systemic candidiasis: importance of persistence of caspofungin in tissues to understanding drug activity. Antimicrob Agents Chemother 2005; 49: 5058–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Pfaller MA, Boyken L, Hollis RJ. et al. In vitro susceptibilities of Candida spp. to caspofungin: four years of global surveillance. J Clin Microbiol 2006; 44: 760–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Wring SA, Randolph R, Park S. et al. Preclinical pharmacokinetics and pharmacodynamic target of SCY-078, a first-in-class orally active antifungal glucan synthesis inhibitor, in murine models of disseminated candidiasis. Antimicrob Agents Chemother 2017; 61: e02068-16.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Pfaller MA, Messer SA, Motyl MR. et al. Activity of MK-3118, a new oral glucan synthase inhibitor, tested against Candida spp. by two international methods (CLSI and EUCAST). J Antimicrob Chemother 2013; 68: 858–63. [DOI] [PubMed] [Google Scholar]
- 19. Lepak AJ, Marchillo K, Andes DR.. Pharmacodynamic target evaluation of a novel oral glucan synthase inhibitor, SCY-078 (MK-3118), using an in vivo murine invasive candidiasis model. Antimicrob Agents Chemother 2015; 59: 1265–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Trucksis M, Garrett G, Bautmans A. et al. A phase I multi-rising dose study evaluating safety, tolerability, and pharmacokinetics of MK-3118, oral glucan synthase inhibitor in healthy volunteers. In: Abstracts of the Fifty-first Interscience Conference on Antimicrobial Agents and Chemotherapy, Chicago, IL, USA, 2011. Abstract F1-1390. American Society for Microbiology, Washington, DC, USA.
- 21. Chamilos G, Lewis RE, Albert N. et al. Paradoxical effect of echinocandins across Candida species in vitro: evidence for echinocandin-specific and candida species-related differences. Antimicrob Agents Chemother 2007; 51: 2257–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Wiederhold NP. Attenuation of echinocandin activity at elevated concentrations: a review of the paradoxical effect. Curr Opin Infect Dis 2007; 20: 574–8. [DOI] [PubMed] [Google Scholar]
- 23. Garcia-Effron G, Lee S, Park S. et al. Effect of Candida glabrata FKS1 and FKS2 mutations on echinocandin sensitivity and kinetics of 1,3-β-d-glucan synthase: implication for the existing susceptibility breakpoint. Antimicrob Agents Chemother 2009; 53: 3690–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Arendrup MC, Perlin DS, Jensen RH. et al. Differential in vivo activities of anidulafungin, caspofungin, and micafungin against Candida glabrata isolates with and without FKS resistance mutations. Antimicrob Agents Chemother 2012; 56: 2435–42. [DOI] [PMC free article] [PubMed] [Google Scholar]