Abstract
Background
Low efficacy of miltefosine in the treatment of visceral leishmaniasis was recently observed in Eastern Africa.
Objectives
To describe the pharmacokinetics and establish a pharmacokinetic/pharmacodynamic relationship for miltefosine in Eastern African patients with visceral leishmaniasis, using a time-to-event approach to model relapse of disease.
Methods
Miltefosine plasma concentrations from 95 patients (48 monotherapy versus 47 combination therapy) were included in the population pharmacokinetic model using non-linear mixed effects modelling. Subsequently a time-to-event model was developed to model the time of clinical relapse. Various summary pharmacokinetic parameters (various AUCs, Time > EC50, Time > EC90), normalized within each treatment arm to allow simultaneous analysis, were evaluated as relapse hazard-changing covariates.
Results
A two-compartment population model with first-order absorption fitted the miltefosine pharmacokinetic data adequately. Relative bioavailability was reduced (−74%, relative standard error 4.7%) during the first week of treatment of the monotherapy arm but only the first day of the shorter combination regimen. Time to the relapse of infection could be described using a constant baseline hazard (baseline 1.8 relapses/year, relative standard error 72.7%). Miltefosine Time > EC90 improved the model significantly when added in a maximum effect function on the baseline hazard (half maximal effect with Time > EC90 6.97 days for monotherapy).
Conclusions
Miltefosine drug exposure was found to be decreased in Eastern African patients with visceral leishmaniasis, due to a (transient) initial lower bioavailability. Relapse hazard was inversely linked to miltefosine exposure. Significantly lower miltefosine exposure was observed in children compared with adults, further urging the need for implementation of dose adaptations for children.
Introduction
Visceral leishmaniasis (VL) is generally ranked as one of the most neglected tropical diseases, afflicting only the poorest of the poor and to a large extent children, particularly in Eastern Africa.1,2 Global incidence has recently been estimated to be up to 400000 cases annually and Eastern Africa is one of the world’s main endemic regions, representing ∼15% of the global burden, with pockets of endemicity present in Eritrea, Ethiopia, Kenya, Somalia, Sudan, South Sudan and Uganda.3
Drug treatment is effective and leads to initial clinical response in most patients with VL, but some patients may eventually relapse as a result of recrudescent Leishmania parasites. This risk of relapse is the main reason for the recommended 6–12 month follow-up period4 before confirming cure or failure. Miltefosine was developed two decades ago as the first oral treatment for VL, based on clinical trials solely conducted on the Indian subcontinent.5 Very recent data from Kenya and Sudan demonstrated relatively poor efficacy rates for miltefosine in the Eastern African region, both for a shortened combination regimen together with liposomal amphotericin B (LAmB) [77% (95% CI 64%–90%)] as well as for the standard 28 day monotherapy [72% (95% CI 60%–85%)], mainly attributable to relapses during the follow-up period.6 This is in line with experiences from other antileishmanial medicines indicating a consistently lower therapeutic efficacy in Eastern Africa compared with the Indian subcontinent.7,8 The reason behind this disparity is still to be elucidated, but host-related factors such as pharmacokinetics and host immunity are expected to play an important role.
The pharmacokinetics of miltefosine have been described previously in patient cohorts from the Netherlands, India, Colombia and Nepal.5,9–12 Miltefosine disposition is generally characterized by a large volume of distribution and a low apparent clearance, resulting in a long biphasic elimination (typical initial half-life ∼7 days).9,11 To date, no data are available on the population pharmacokinetic properties of miltefosine from Eastern Africa. Miltefosine drug exposure in children was significantly lower compared with adults, when receiving the 2.5 mg/kg/day regimen.4,9 In Nepalese patients, lower drug exposure has been linked to a reduced clinical response: the time miltefosine concentrations were above a high in vitro intracellular amastigote susceptibility value (EC90) was significantly associated with eventual relapse during the 12 month follow-up period.10 No further pharmacokinetic/pharmacodynamic relationship has been established for miltefosine.
The aim of this study was to describe the population pharmacokinetics of miltefosine in Eastern African patients with VL using non-linear mixed effects modelling and to establish and describe in more detail the miltefosine exposure–effect relationship on relapse of the infection, using a time-to-event approach.
Materials and methods
Study site and ethics approval
The pharmacokinetic data were collected in an open-label randomized multicentre study that was carried out at three VL treatment hospitals: one in Baringo district in Kenya (Kimalel health centre) and two in Gedaref State in Sudan (Dooka and Kassab hospitals). Clinical data of this study are reported in full elsewhere.6 The study was registered with ClinicalTrials.gov with the identifier NCT01067443. Additional details on the ethics approval can be found in Supplementary Methods (available as Supplementary data at JAC Online).
Drug regimens
Patients were randomized to one of three different treatment arms. Two arms that contained miltefosine were included in the current pharmacokinetic/pharmacodynamic analysis: (i) combination therapy arm: a combination of a single dose of intravenous LAmB (AmBisome®, 10 mg/kg; Gilead Pharmaceuticals, USA) on day 1 followed by 10 days of oral miltefosine (Impavido®, 2.5 mg/kg/day, maximum 150 mg/day; Paladin, Canada) from day 1 to 10; (ii) monotherapy arm ‘MIL’: a miltefosine monotherapy for 28 days (2.5 mg/kg/day, maximum 150 mg/day). All treatment was directly observed. Additional details can be found in Supplementary Methods.
Blood samples
Potassium EDTA blood samples were collected through venepuncture. During treatment, blood samples were nominally collected in the combination therapy arm prior to treatment initiation and thereafter at 4, 8 h and 2, 5, 9 days (patients ≥12 years of age) or 4, 8 h and 5, 9 days (patients <12 years of age) after the first miltefosine dose; and in the miltefosine arm prior to the first dose and thereafter at 4, 8 h and 2, 6, 13, 20, 27 days (patients ≥12 years of age) or 4, 8 h, and 6, 13, 27 days (patients <12 years of age) after the first dose. Except for the first treatment-day, all samples were collected prior to the first dose that day. Additional blood samples were drawn on days 60 and 210. Additional details on processing and transport of the blood samples can be found in Supplementary data.
Bioanalysis
Miltefosine was quantified by LC-MS/MS, as described previously with small adaptations.13 The lower limit of quantification (LLOQ) was set at 4.00 ng/mL for miltefosine in human blood plasma.13
Population pharmacokinetic analysis
Estimation of miltefosine population pharmacokinetic parameters was performed using non-linear mixed effects modelling with the first-order conditional estimation method with interaction as implemented in NONMEM (version 7.3; ICON Development Solutions, USA).14 Dataset management and graphical analysis was performed in R (version 3.1.2).15 The modelling process was further automated by the use of Perl-speaks-NONMEM (PsN, version 4.3.7), Pirana (version 2.9.0) and the R-package Xpose (version 4.5.3).16 Model development was initially guided by physiological and biological plausibility, the objective function value (OFV) as computed by NONMEM and standard goodness of fit plots. A ΔOFV of –3.84 (for 1 d.f., χ2 distribution) corresponded with a significance level of P = 0.05. Concentrations below the LLOQ were censored and handled using the M3 method, in which likelihood is maximized simultaneously for both the continuous and categorical censored data.17,18
A previously developed two-compartment disposition model with first-order absorption and elimination to and from the central compartment11 was used as the base structural model. Clearances and volumes of distribution were modelled using allometric scaling with power exponents of 0.75 and 1.00, respectively, using fat-free mass as the body size descriptor.19 Between-subject variability was modelled exponentially as:
| (1) |
in which Θi is the individual parameter estimate for the ith individual, Θ is the typical population parameter value, and ηi,Θ is the between-subject random variability with a mean of 0 and a variance of ω2. Between-occasion variability was evaluated for all structural parameter values. For instance for bioavailability (F):
| (2) |
where Fij is the relative bioavailability for the ith individual at the jth nominal sampling occasion, F is the typical bioavailability fixed at 100%, and κj,F is the between-occasion variability in F, for which each sampling window was considered an occasion. The residual variability was modelled with a combined fixed additive and proportional error on observed concentrations. A limited number of possible covariates were investigated based on data inspection and plausibility, which included: time on treatment, treatment centre and country; fat-free mass was already included in the base model.
Model evaluation was first of all guided by the OFV and further done based on basic goodness-of-fit plots. Bootstrapping (n = 1000) was performed on final models to evaluate model robustness and obtain non-parametric confidence intervals of all parameter estimates. Both numerical and graphical visual predictive checks were performed based on 1000 model-based simulations to compare observed data to simulated data and evaluate the predictive performance of the final model.
Pharmacodynamic analysis
Using the final pharmacokinetic model, individual estimates of secondary pharmacokinetic parameters for miltefosine were calculated, based on the individual predicted concentration–time curves: the AUC from 0 till the end of treatment, i.e. 10 days for the combination therapy and 28 days for the monotherapy regimen (AUC0–10/28d) and the time that the miltefosine concentration was either over the in vitro intracellular susceptibility value EC50 or EC90 (Time > EC50 and Time > EC90). For EC50 and EC90, values were selected based on intracellular amastigote in vitro susceptibility testing of clinical Leishmania donovani isolates from the Eastern African region (Sudan and northern Ethiopia). The chosen values represented the highest, non-outlier, susceptibility values from various repeated experiments: an EC50 of 4.95 μM (2.01 μg/mL) and an EC90 of 25.9 μM (10.6 μg/mL) (V. Yardley, LSHTM, personal communication). To allow model identifiability as well as exploration of the influence of varying miltefosine exposure, miltefosine exposure covariates were normalized relative to the mean value within their respective treatment arm (normalized mean equalled 1). Times to recrudescent VL infection were based on the initiation of administration of any rescue treatment. Patients with no relapse were right-censored at the time of the last time point of follow-up (day 210). This relapse dataset was analysed with a time-to-event model in NONMEM using exact maximal likelihood estimation. The hazard [h(t)] was modelled using a constant hazard model (Eq. 3):
| (3) |
where λ is the baseline hazard. Since the relapse hazard was assumed to be 0 during treatment, cumulative hazard was integrated over time from end-of-treatment until relapse or end-of-follow-up. The inhibitory effect of miltefosine exposure and additionally of co-treatment with LAmB in the combination arm was implemented as a maximum effect (Emax) function and a proportional effect, respectively, on the baseline hazard, as follows:
| (4) |
where h(t)i is the individual hazard at time t, h(t) is the baseline hazard at time t, MILi is the predicted individual miltefosine exposure, I50 is the exposure value that leads to 50% reduction in hazard and AmB is the proportional decrease in relapse hazard due to co-administration of LAmB.
The development of the pharmacodynamic model was initially guided by the OFV. Simulation-based diagnostics were used to evaluate the final model through Kaplan–Meier visual predictive check plots based on 1000 simulations of the final model. The parameter estimate precisions were obtained through bootstrapping (n = 1000 samples), stratified on the treatment arm.
Results
Patients and samples
Plasma samples (n = 711 both pre- and post-dose samples) were collected and analysed for their miltefosine concentration from a total of 96 enrolled patients. One patient was excluded from the final population pharmacokinetic analysis, as there was only a single unreliable concentration available. Finally, 608 concentrations (excluding pre-dose samples) from 95 patients were included in the pharmacokinetic analysis of which 28 (4.6%) post-dose concentrations were below LLOQ. Demographic characteristics of the included patients are presented in Table 1. A large proportion of the patients were children, with almost half (43.2%) of the patients having an age of ≥7 (the inclusion threshold) and <12 years. Patients were enrolled in three treatment centres in Kenya and Sudan, with approximately half of the patients recruited in each country. As the aim of the pharmacodynamic analysis was to establish and describe the relationship between miltefosine exposure and VL relapse, four patients who received rescue treatment early (before or around the nominal time point when initial cure was assessed, i.e. day 28) were further excluded from the pharmacodynamic analysis; two of four patients who received rescue treatment had not finished the assigned miltefosine treatment regimen, due to lack of treatment response or adverse events. A total of 91 patients was thus subsequently included in the pharmacodynamic analysis.
Table 1.
Demographics and treatment details of the patients included in the population pharmacokinetic study of miltefosine in Eastern African patients with VL, all values are given as median (range), unless stated otherwise
| Parameter | Monotherapy arm | Combination therapy arm | Both arms |
|---|---|---|---|
| Total no. of patients | 48 | 47 | 95 |
| Female patients, n (%) | 7 (14.6) | 6 (12.8) | 13 (13.7) |
| Total dose of miltefosine (mg/kg) | 72.6 (62.22–93.3) | 20.8 (6.78–25.0) | NA |
| Daily dose of miltefosine (mg/kg/day) | 2.59 (2.02–3.33) | 2.63 (2.08–3.33) | 2.61 (2.02–3.33) |
| Number of days on miltefosine | 28 (14–28) | 10 (3–10) | NA |
| Patients with unfinished regimen, n (%) | 1 (2) | 2 (4) | 3 (3) |
| Paediatric patients (<12 years), n (%) | 19 (39.6) | 22 (46.8) | 41 (43.2) |
| Age (years) | 13 (7–41) | 12 (7–30) | 13 (7–41) |
| Body weight (kg) | 33.5 (16–65) | 32 (15–59) | 32 (15–65) |
| Height (cm) | 150 (107–185) | 146 (115–176) | 150 (107–185) |
| Fat-free mass (kg) | 31.4 (15.3–55.9) | 31.9 (15.2–48.5) | 29.9 (15.2–55.9) |
| Body mass index (kg/m2)a | 17.7 (15.4–21.7) | 17.7 (15.9–21.0) | 17.9 (15.4–21.7) |
| Body mass index-for-age (z-score)b | –2.45 (–4.01 to 0.46) | –1.87 (–4.05 to 1.00) | –1.88 (–4.05 to 1.00) |
| Malnourished patients, n (%)c | 27 (56.3) | 22 (45.8) | 49 (51.0) |
| Patients with initial failure, n (%) | 2 (4.17) | 2 (4.25) | 4 (4.21) |
| Patients with relapse, n (%) | 9 (18.8) | 6 (12.8) | 15 (15.7) |
| Treatment centres | |||
| Kimalel, Kenya, n (%) | 24 (50.0) | 25 (53.1) | 49 (51.6) |
| Kassab, Sudan, n (%) | 7 (14.6) | 6 (12.8) | 13 (13.7) |
| Dooka, Sudan, n (%) | 17 (35.4) | 16 (34.0) | 33 (34.7) |
NA, not applicable.
Calculated for patients of ≥ 18 years of age.
Calculated for patients <18 years of age, using the WHO Growth Reference 2007 data (http://www.who.int/growthref/en/).
Definitions for malnourishment: BMI <18.5 for patients of ≥ 18 years of age and BMI-for-age z-score < −2 for patients <18 years of age.
Pharmacokinetics of miltefosine
Plasma concentration–time profiles of miltefosine were best described by a two-compartment disposition structural model with first-order absorption into and first-order elimination from the central compartment. A model with three disposition compartments was not supported by the data. As the absolute F of miltefosine is unknown, all disposition parameters were relative to F.
During the initial model building, an over-prediction of miltefosine concentrations throughout the first days of treatment was observed. A step-function to model time as a covariate effect on the pharmacokinetic parameters was used to explore the time-varying shape of every structural pharmacokinetic parameter. Time-varying ka and F gave comparable substantial improvements in fit, giving a better fit than, e.g. time-varying CL/F (ΔOFV +70), eventually F was chosen because of better physiological plausibility. Finally, the model was parameterized in such a way that F was ‘normal’ (fixed to 1) at the end of treatment and during follow-up, and the decrease in F was estimated with a single step relative to this fixed F for the first week (0 < day ≤7) of monotherapy arm but only for the first day (0 < day ≤ 1) of combination therapy (ΔOFV –105, 1 d.f. extra). The basal F value was 74.3% (4.68% relative standard error, RSE) lower than F at the end of treatment, which was assumed to be 100%. No other covariates could further be identified: treatment centre and country of origin did not appear to affect the pharmacokinetic parameters further.
Owing to sparseness of the data, between-subject variabilities could only be identified for CL/F and ka, in combination with implementation of between-occasion variability on the relative bioavailability (ΔOFV –40.6). In addition, between-subject variability on the temporary decrease in F was high and improved the fit significantly (96.4%; ΔOFV –76).
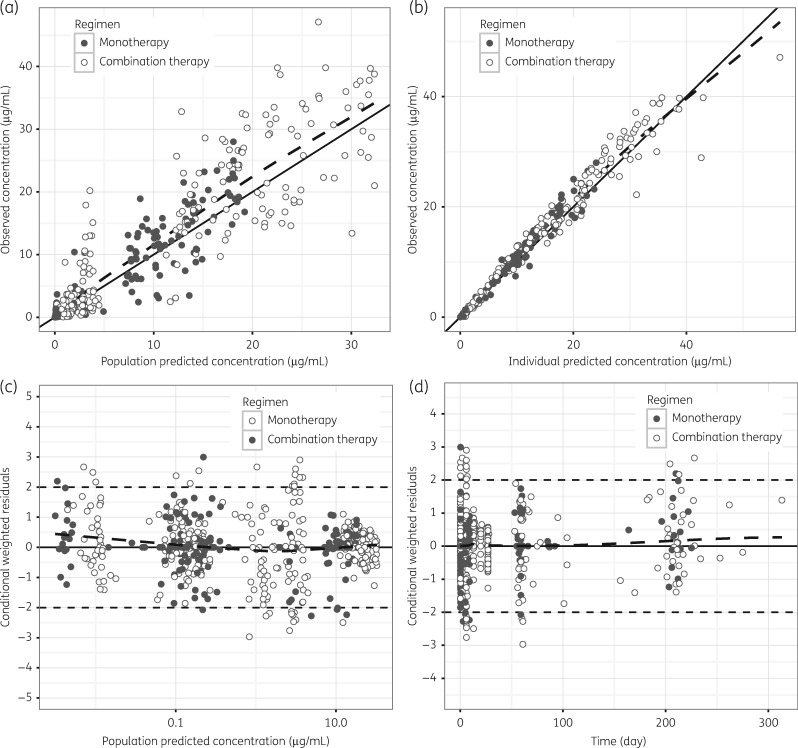
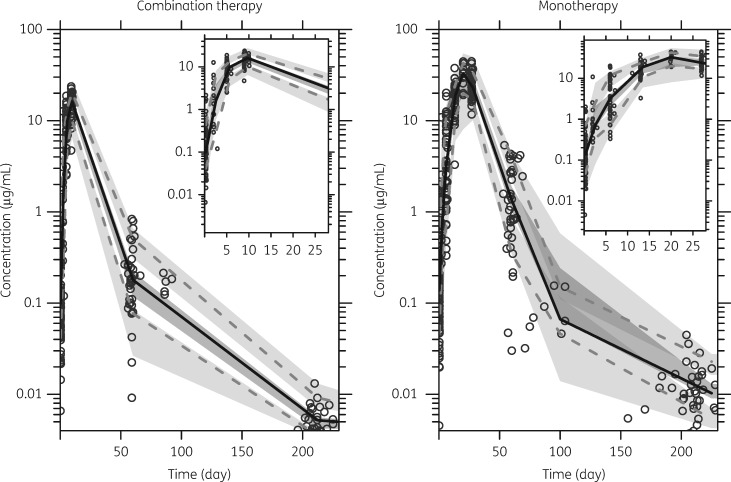
Basic goodness-of-fit plots are shown in Figure 1 and the final model parameter estimates are given in Table 2. A visual predictive check was used to assess the simulation performance of the final model and showed no major deviations, following most trends in the observations (Figure 2).
Figure 1.
Goodness-of-fit plots for the final miltefosine population pharmacokinetic model. Observed concentrations versus (a) population predicted concentrations and (b) individual predicted concentrations. Conditional weighted residuals versus (c) population predicted concentrations and (d) time. Solid line represents the line of identity or unity and the broken line is the locally weighted least square regression line to indicate trends.
Table 2.
Parameter estimates of the final miltefosine population pharmacokinetic and pharmacodynamic model in Eastern African patients with VL treated with either miltefosine monotherapy or combination therapy
| Parametera | Population estimate (% RSEc) | Between-subject variability (% RSEc) | Between-occasion variability (% RSEc) |
|---|---|---|---|
| Pharmacokinetics | |||
| Absorption rate, ka (/day) | 1.49 (17.7) | 68.0 (24.5) | |
| Clearance, CL/F (L/day)b | 4.29 (3.22) | 17.0 (23.3) | |
| Central volume of distribution, Vc/F (L)b | 51.7 (4.33) | NE | |
| Intercompartmental clearance, Q/F (L/day) | 0.0266 (40.7) | NE | |
| Peripheral volume of distribution, Vp/F (L) | 2.25 (14.1) | NE | |
| F (%, at end of treatment) | 100 fixed | NE | 30.1 (41.3) |
| Residual proportional error (%) | 31.0 (5.74) | ||
| Residual additive error (μg/mL) | 0.001 fixed | ||
| Reduction in F at baselined (% change from end of treatment) | –74.3 (4.68) | 96.4 (19.5) | |
| Pharmacodynamics | |||
| Baseline hazard of relapse (infections/year) | 1.84 (72.7) | ||
| I50 miltefosine Time > EC90 for monotherapy arm (day) | 6.97 (80.5) | ||
| I50 miltefosine Time > EC90 for combination therapy arm (day) | 2.00 (80.5) | ||
| Hazard reduction by liposomal amphotericin B (%) | 63.6 (39.0) |
ka, absorption rate, CL/F, oral clearance; Vc/F, central volume of distribution; Q/F, intercompartmental clearance; Vp/F, peripheral volume of distribution; F, relative bioavailability; I50, exposure value that leads to 50% reduction in hazard; NE, not estimated.
All clearances and volumes were allometrically scaled (power exponents of 0.75 and 1, respectively) based on fat-free mass. Values reported are normalized to a standard fat-free mass of 53 kg.
Calculated as: 100 × (SD/mean value), based on 1000 bootstrap samples.
Duration of the reduction in F was empirically determined to be from >0 to ≤ 7 days for the monotherapy regimen and from >0 to ≤ 1 day for the combination therapy regimen.
Figure 2.
Visual predictive check of the final miltefosine population pharmacokinetic model in Eastern African patients with VL receiving 10 days of miltefosine (2.5 mg/kg/day) in combination therapy (left plot) or 28 days of miltefosine (2.5 mg/kg/day) monotherapy (right plot). Insets in the top right corner show a magnification of the same plot during the initial treatment period (0–28 days). Circles represent the observed concentrations, the solid line the 50th percentile of the observed data and the dashed lines the 10th and 90th percentiles of the observed data. Shaded areas indicate the simulated 95% CI of the 10th and 90th (light grey) and 50th (dark grey) percentiles of the simulations (n = 1000 simulations).
Using the final model, secondary pharmacokinetic parameters relating to miltefosine exposure were calculated based on the model-predicted individual concentration–time curves (Table 3). For both treatment arms there was a significant difference in all calculated exposure values between children (<12 years of age) and adolescent/adults (≥12 years of age). The median AUC0–∞, AUC0–10/28d, Time > EC50 and Time > EC90 in the monotherapy arm were 1.49 (P < 0.01), 1.41 (P < 0.01), 1.10 (P < 0.05) and 1.26 (P < 0.01) times higher in adults than in children, respectively, while in the combination therapy arm they were 1.59 (P < 0.01), 1.38 (P < 0.05), 1.20 (P < 0.05) and 3.13 (P < 0.01) times higher, respectively.
Table 3.
Secondary pharmacokinetic parameters of miltefosine in Eastern African patients with VL treated with either miltefosine monotherapy or combination therapy
| Secondary parametera [median (range)] |
|||||
|---|---|---|---|---|---|
| Monotherapy (28 days miltefosine) | Total (n = 48) | Paediatricb (n = 19) | Adultb (n = 29) | Diff (%)c | P value |
| Initial half-life (days) | 7.05 (4.02–10.9) | 7.02 (4.02–8.45) | 7.18 (5.35–10.9) | –2 | 0.258 |
| Terminal half-life (days) | 79.4 (49.9–103) | 77.8 (54.9–95.6) | 81.3 (49.9–103) | –4 | 0.073 |
| AUC0–∞ (μg·day/mL) | 713 (237–1482) | 545 (314–1080) | 812 (237–1482) | –33 | 0.006d |
| AUC0–28d (μg·day/mL) | 423 (191–767) | 352 (232–593) | 497 (191–767) | –29 | 0.002d |
| Time > EC50 (days) | 51.4 (30.5–77.1) | 48.3 (36.3–62.4) | 52.9 (30.5–77.1) | –9 | 0.024e |
| Time > EC90 (days) | 27.0 (4.29–43.8) | 22.1 (11.0–34.2) | 27.8 (4.29–43.8) | –21 | 0.005d |
| Combination therapy (10 days miltefosine) | Total (n = 47) | Paediatricb (n = 22) | Adultb (n = 25) | Diff (%)c | P value |
| Initial half-life (days) | 7.39 (5.41–10.3) | 6.76 (5.58–9.00) | 7.52 (5.41–10.3) | –12 | 0.031e |
| Terminal half-life (days) | 78.5 (62.4–98.6) | 76.7 (66.0–98.6) | 79.7 (62.4–93.7) | –4 | 0.231 |
| AUC0–∞ (μg·day/mL) | 290 (70.1–496) | 197 (136–496) | 313 (70.1–483) | –37 | 0.004d |
| AUC0–10 (μg·day/mL) | 87.9 (31.1–136) | 69.5 (31.1–129) | 95.9 (32.3–136) | –28 | 0.004d |
| Time > EC50 (days) | 31.2 (14.2–46.9) | 28.5 (23.1–43.0) | 34.1 (14.2–46.9) | –16 | 0.013e |
| Time > EC90 (days) | 8.98 (0–16.8) | 3.17 (0–16.8) | 9.93 (0–16.2) | –68 | 0.002d |
Time > EC50, time the miltefosine concentration was above the in vitro susceptibility value EC50; Time > EC90, time the miltefosine concentration was above the in vitro susceptibility value EC90; P value, calculated based on Mann–Whitney U-test.
Paediatric defined as having an age <12 years and adult defined as having an age ≥12 years.
Percentage difference between the median adult and paediatric ([paediatric – adult]/adult) pharmacokinetic parameter.
Below significance level of P < 0.01.
Below significance level of P < 0.05.
Pharmacodynamics of miltefosine in monotherapy and combination therapy
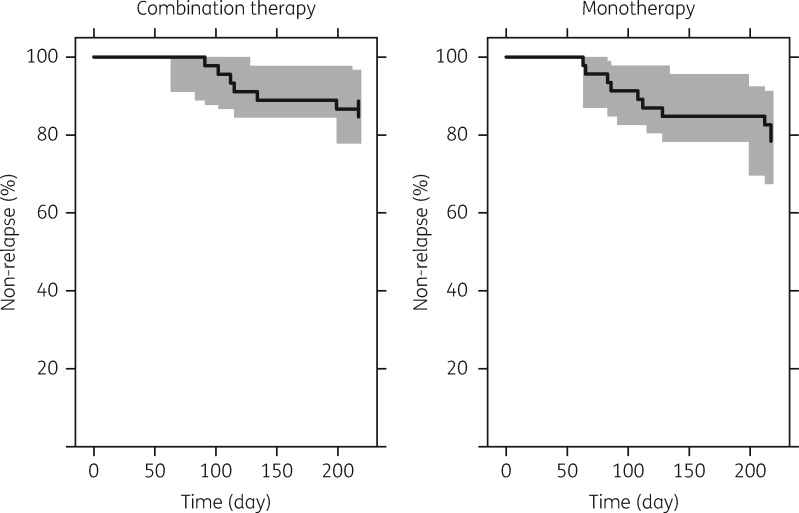
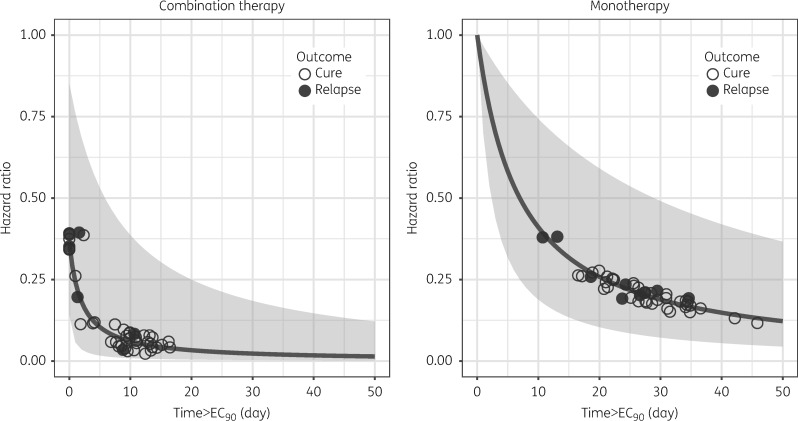
Fifteen of 91 patients (16.5%) included in the pharmacodynamic analysis presented with a clinical and parasitological confirmed relapse of VL during the follow-up period, for which they received rescue treatment at a median (range) of 112 days (63–217 days); with 108 days (63–217 days, n = 6) and 113.5 days (91–199 days, n = 9) for the monotherapy and combination therapy, respectively. All relapses were confirmed parasitologically by microscopy-positive aspirates of lymph node, bone marrow or spleen. The constant hazard model resulted in an adequate fit of the time to relapse data, with no added value of a Weibull function (ΔOFV = –2.24, 1 d.f. extra). Adding an inhibitory effect of normalized miltefosine Time > EC90 on the baseline hazard function resulted in a significantly better description of the data, when combined with a proportional inhibitory effect of LAmB (ΔOFV = –7.09, 2 d.f. extra, P = 0.03). The other tested miltefosine exposure parameters, i.e. AUC0–10/28d and Time > EC50, did not improve the hazard model fit significantly. Final model parameter estimates are given in Table 2. The Kaplan–Meier plots of observed time to relapse data together with the visual predictive checks simulated from the final model are shown in Figure 3. The relative hazard for both treatment regimens compared with the baseline hazard (without treatment effects) is depicted in Figure 4.
Figure 3.
Visual predictive check of the final time-to-event model with an inhibitory effect of miltefosine exposure (Time > EC90) on the hazard function. Left plot depicts the combination therapy regimen (10 days of miltefosine), the right plot the monotherapy arm (28 days of miltefosine). Solid black line is the Kaplan–Meier plot of the observed relapses of visceral leishmaniasis during the follow-up period, and the grey area is the 95% prediction interval of the simulated time to the relapse of disease (n = 1000 simulations).
Figure 4.
Hazard ratio versus the duration of miltefosine concentration >EC90 (Time > EC90). Lines indicate the estimated hazard ratios for the combination therapy (left panel) and miltefosine monotherapy (right panel). Grey areas represent the respective computed 90% CI. Circles represent the observed individuals: open circles represent cured patients, while filled circles represent patients who relapsed and received rescue treatment.
Discussion
This study is the first description of the pharmacokinetic properties of miltefosine in VL patients in Eastern Africa. This population pharmacokinetic model has been extended into a pharmacokinetic/pharmacodynamic model to describe the effect of miltefosine treatment both in mono- and combination therapy on relapse of disease during the follow-up period to explain the overall treatment efficacy of the treatment regimens.
Pharmacokinetics
The overall structural two-compartment model and the population pharmacokinetic model parameter estimates in this study were comparable and in the same range as estimates we published previously from pooled analyses in Indian adults and children, and European adults,9,11 except for the extent (F) and rate (ka) of absorption and the magnitude of variability in these parameters.
The current analysis indicated a typical absorption rate constant of 1.25 day−1. Previous estimates of miltefosine ka were ∼0.4 day−1. This might be an artefact finding related to the very sparse samples informing estimation of ka. Other potential reasons could be type of concomitant food intake and/or underlying malnourishment (51% of our population, Table 1). Clinically more relevant, given the continued accumulation of miltefosine during treatment, is the observation that the extent of absorption F, was highly decreased (−73.4%) during the first part of the treatment period. This decreased bioavailability and its subsequent recovery, previously unobserved, might indicate disease-specific absorption-limiting factors, which could be more pronounced in Eastern Africa. Gastrointestinal adverse events (vomiting, diarrhoea) related to miltefosine intake were most prominent in the first week of treatment,6 but were similar to previous reports.5 Other possible relevant factors could include dietary differences between populations and the aforementioned malnutrition, despite per-protocol exclusion of severe forms of malnourishment. Protein-energy malnutrition can affect drugs’ bioavailability by a generalized malabsorption due to decreased gastrointestinal mucosal functionality, which normally improves rapidly (within days) after re-initiation of a nutritional diet, affecting protein binding.20,21 Decreased bioavailability in malnourished patients has e.g. been shown for chloramphenicol, chloroquine, lopinavir and efavirenz.22–24 To the best of our knowledge it is unknown whether malnutrition-related malabsorption could be more prevalent in Eastern African versus Indian patients with VL.
None the less, the transiently decreased bioavailability resulted in a substantial decrease in accumulation of miltefosine in our patient cohort. For comparison, previously mean (95% CI) AUC0–28d in a typical adult Indian patient cohort with a comparable body weight distribution [mean (95% CI): 35 (16–54) kg] following a similar dosing regimen (2.5 mg/kg/day, 28 days) was estimated at 675 μg/mL (377–1080 μg/mL), corresponding to an average 30% higher exposure than achieved in our population [median (range): 423 (191–767) μg/mL].9 The lower exposure might explain, at least in part, the lower cure rates for the miltefosine monotherapy in Eastern Africa compared with the Indian subcontinent, although additional factors on the parasite- or host-level cannot be excluded.
The faster recovery time of bioavailability for the combination therapy could be due to a quicker improvement of the patients’ overall physiological state after the LAmB injection. An underlying drug–drug interaction between the two drugs can also not be excluded and has been observed previously in vitro.25 Free miltefosine could theoretically be incorporated into the liposomes encapsulating AmB,26 making it unavailable for further disposition and metabolism. While this phenomenon would effectively increase observed plasma concentrations, masking the reduced oral bioavailability, high protein binding of miltefosine (>95%) would probably largely limit this theoretical interaction. Additionally, miltefosine and AmB compete with the same cholesterol-enriched domain of cell membranes.27 Membrane pre-saturation with AmB could therefore explain a better miltefosine bioavailability in the blood.
This model-based analysis confirmed lower miltefosine exposure in children versus adults, while receiving the same mg/kg dose, due to faster clearance, in accordance with well-established allometric scaling of the elimination clearance rate.28 Almost all exposure values were significantly decreased in the paediatric population for both treatment arms, with the largest differences observed for AUC0–∞, AUC0–10/28d and Time > EC90. Children were probably more prone to failure on miltefosine-based therapy than adults in Eastern Africa.6 Twelve of 15 (87%) relapsing patients in this cohort were <14 years. Higher failure rates for children with VL on miltefosine therapy have been observed previously in other regions.4,29 The current analysis reinforces the urgent need to adapt the miltefosine dosing algorithm in children, such as the allometric dosing regimen we proposed previously.9 Adaptation of the paediatric miltefosine dosage might be more crucial in Eastern Africa, as the overall response and drug exposure were lower in Eastern African patients compared with the Indian subcontinent.
Pharmacodynamics
Initial cure is achieved in most patients with treated VL: in this pharmacokinetic cohort, only 4 of 95 patients experienced initial failure within the first 28 days. For a successful treatment, drug exposure is thought to decrease the parasite load during the treatment period below a critical level, sufficient to prevent recrudescence of the parasite, e.g. by suppression due to the patient’s own (re-)activated immune system. The VL relapses were successfully modelled using a time-to-event approach, where both LAmB as well as the Time > EC90 for miltefosine affected time until relapse. The reduction in relapse hazard by a single LAmB infusion was substantial (64%), in itself equivalent to the hazard reduction resulting from Time > EC90 of 12.2 days for miltefosine monotherapy, according model-based estimates. This substantial contribution is corroborated by the fact that this regimen has some efficacy as monotherapy.7 Based on the individually obtained Time > EC90 values, empirical pharmacokinetic targets can be proposed. For the combination arm, no relapses occurred in patients with Time > EC90 >10.7 days [15 of 39 (30%) cured patients reached this value], while for the monotherapy arm only a single relapse occurred in patients with Time > EC90 29.5 days [15 of 37 (41%) of cured patients reached this value] (Figure 4). While these values are not definitive thresholds to be reached and are highly dependent on both the EC90 used and the patient population, they do provide a pharmacokinetic window for future miltefosine dose optimization. In a previous study in Nepal, we also identified Time > 10 × EC50 (corresponding with Time > EC90) affecting the probability of relapse on miltefosine.10 These findings might indicate that the effect of miltefosine is driven to a large extent by time-dependent killing.10 Nevertheless, a high concentration threshold appears to be pivotal as well, which could be due to less than optimal penetration of miltefosine into the Leishmania infection sites.
Conclusions
For the first time, the population pharmacokinetic properties of miltefosine in Eastern African patients with VL were successfully described by a two-compartment disposition non-linear mixed-effects model. The relative bioavailability of miltefosine was substantially reduced at the initiation of therapy and recovered faster for the combination therapy arm than for the monotherapy arm. This resulted in ∼30% reduction in miltefosine exposure in Eastern African adult patients receiving 2.5 mg/kg/day compared with historic data from India. The data presented here indicate that a dose adjustment is warranted for Eastern African patients with VL, particularly in children. An exposure–effect relationship was established for the Time > EC90 of miltefosine, which affected the relapse time and empirical pharmacokinetic targets were suggested.
An effective, safe, oral, field-adapted treatment is urgently needed for VL in Eastern Africa. Miltefosine, the sole currently available oral treatment for VL, is considered an interesting option for combination with new oral candidate compounds. The data presented here will be critical to guide a rationale for future development of combination treatments in Eastern Africa containing miltefosine.
Supplementary Material
Acknowledgements
We sincerely thank the VL patients and parents of the paediatric patients for their willingness to be enrolled in this study and their cooperation. We also thank the clinical study teams and all laboratory technicians at the clinical sites in Dooka, Kassab and Kimalel, and the DNDi Africa Data Center for their professional assistance. This study was conducted within the context of the Leishmania East Africa Platform (LEAP), in collaboration with the trial sites, and coordinated, implemented and funded by the Drugs for Neglected Diseases initiative (DNDi). This paper is published with permission from the Director KEMRI.
Funding
This work was supported through DNDi by the Médecins Sans Frontières International; the Medicor Foundation; Department for International Development (DFID), UK; the Ministry of Foreign and European Affairs (MAEE), France; the Spanish Agency of International Cooperation for Development (AECID), Spain; the Dutch Ministry of Foreign Affairs (DGIS), the Netherlands; Federal Ministry of Education and Research (BMBF) through KfW, Germany; and Swiss Agency for Development and Cooperation (SDC), Switzerland. T. D. was supported by the Netherlands Organisation for Scientific Research (NWO/ZonMw) through Veni project no. 91617140.
Transparency declarations
None to declare.
Author contributions
Designed the study: T. P. C. D., M. B., S. J. E., A. H., J. O., A. M. M., M. W. and E. A. G. K. Enrolled patients: B. M. Y., S. N., G. K., A. M. M. and E. A. G. K. Responsible for bioanalysis: A. E. K. and J. H. B. Performed pharmacometric analysis: T. P. C. D. and M. O. K. Wrote the first draft of the manuscript: T. P. C. D. Contributed to the interpretation of study findings: all authors. Agree with the manuscript’s results and conclusions: all authors.
Supplementary data
Supplementary Methods appear as Supplementary data at JAC Online.
References
- 1. Harhay MO, Olliaro PL, Vaillant M. et al. Who is a typical patient with visceral leishmaniasis? Characterizing the demographic and nutritional profile of patients in Brazil, East Africa, and South Asia. Am J Trop Med Hyg 2011; 84: 543–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Boelaert M, Meheus F, Sanchez A. et al. The poorest of the poor: a poverty appraisal of households affected by visceral leishmaniasis in Bihar, India. Trop Med Int Health 2009; 14: 639–44. [DOI] [PubMed] [Google Scholar]
- 3. Alvar J, Vélez ID, Bern C. et al. Leishmaniasis worldwide and global estimates of its incidence. PLoS One 2012; 7: e35671.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Rijal S, Ostyn B, Uranw S. et al. Increasing failure of miltefosine in the treatment of Kala-azar in Nepal and the potential role of parasite drug resistance, reinfection, or noncompliance. Clin Infect Dis 2013; 56: 1530–8. [DOI] [PubMed] [Google Scholar]
- 5. Dorlo TP, Balasegaram M, Beijnen JH. et al. Miltefosine: a review of its pharmacology and therapeutic efficacy in the treatment of leishmaniasis. J Antimicrob Chemother 2012; 67: 2576–97. [DOI] [PubMed] [Google Scholar]
- 6. Wasunna M, Njenga S, Balasegaram M. et al. Efficacy and safety of AmBisome in combination with sodium stibogluconate or miltefosine and miltefosine monotherapy for african visceral leishmaniasis: phase II randomized trial. PLoS Negl Trop Dis 2016; 10: e0004880.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Khalil EA, Weldegebreal T, Younis BM. et al. Safety and efficacy of single dose versus multiple doses of AmBisome for treatment of visceral leishmaniasis in eastern Africa: a randomised trial. PLoS Negl Trop Dis 2014; 8: e2613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Musa A, Khalil E, Hailu A. et al. Sodium stibogluconate (SSG) & paromomycin combination compared to SSG for visceral leishmaniasis in East Africa: a randomised controlled trial. PLoS Negl Trop Dis 2012; 6: e1674.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Dorlo TP, Huitema AD, Beijnen JH. et al. Optimal dosing of miltefosine in children and adults with visceral leishmaniasis. Antimicrob Agents Chemother 2012; 56: 3864–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Dorlo TP, Rijal S, Ostyn B. et al. Failure of miltefosine in visceral leishmaniasis is associated with low drug exposure. J Infect Dis 2014; 210: 146–53. [DOI] [PubMed] [Google Scholar]
- 11. Dorlo TP, van Thiel PP, Huitema AD. et al. Pharmacokinetics of miltefosine in Old World cutaneous leishmaniasis patients. Antimicrob Agents Chemother 2008; 52: 2855–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Castro MD, Gomez MA, Kip AE. et al. Pharmacokinetics of miltefosine in children and adults with cutaneous leishmaniasis. Antimicrob Agents Chemother 2017; 61: doi:10.1128/AAC.02198-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Dorlo TP, Hillebrand MJ, Rosing H. et al. Development and validation of a quantitative assay for the measurement of miltefosine in human plasma by liquid chromatography-tandem mass spectrometry. J Chromatogr B 2008; 865: 55–62. [DOI] [PubMed] [Google Scholar]
- 14. Beal SL, Sheiner LB, Boeckmann AJ. et al. NONMEM User’s Guides. Ellicott City, MD: Icon Development Solutions, 2009. [Google Scholar]
- 15. R Development Core Team. R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing, 2014. [Google Scholar]
- 16. Keizer RJ, Karlsson MO, Hooker A. Modeling and simulation workbench for NONMEM: tutorial on Pirana, PsN, and Xpose. CPT Pharmacometrics Syst Pharmacol 2013; 2: e50.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Beal SL. Ways to fit a PK model with some data below the quantification limit. J Pharmacokinet Pharmacodyn 2001; 28: 481–504. [DOI] [PubMed] [Google Scholar]
- 18. Ahn JE, Karlsson MO, Dunne A. et al. Likelihood based approaches to handling data below the quantification limit using NONMEM VI. J Pharmacokinet Pharmacodyn 2008; 35: 401–21. [DOI] [PubMed] [Google Scholar]
- 19. Janmahasatian S, Duffull SB, Ash S. et al. Quantification of lean bodyweight. Clin Pharmacokinet 2005; 44: 1051–65. [DOI] [PubMed] [Google Scholar]
- 20. Krishnaswamy K. Drug metabolism and pharmacokinetics in malnourished children. Clin Pharmacokinet 1989; 17 Suppl 1: 68–88. [DOI] [PubMed] [Google Scholar]
- 21. Viteri FE, Flores JM, Alvarado J. et al. Intestinal malabsorption in malnourished children before and during recovery. Relation between severity of protein deficiency and the malabsorption process. Am J Dig Dis 1973; 18: 201–11. [DOI] [PubMed] [Google Scholar]
- 22. Walker O, Dawodu AH, Salako LA. et al. Single dose disposition of chloroquine in kwashiorkor and normal children—evidence for decreased absorption in kwashiorkor. Br J Clin Pharmacol 1987; 23: 467–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Bartelink IH, Savic RM, Dorsey G. et al. The effect of malnutrition on the pharmacokinetics and virologic outcomes of lopinavir, efavirenz and nevirapine in food insecure HIV-infected children in Tororo, Uganda. Pediatr Infect Dis J 2015; 34: e63–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Eriksson M, Paalzow L, Bolme P. et al. Chloramphenicol pharmacokinetics in Ethiopian children of differing nutritional status. Eur J Clin Pharmacol 1983; 24: 819–23. [DOI] [PubMed] [Google Scholar]
- 25. Ménez C, Buyse M, Besnard M. et al. Interaction between Miltefosine and amphotericin B: consequences for their activities towards intestinal epithelial cells and Leishmania donovani promastigotes in vitro. Antimicrob Agents Chemother 2006; 50: 3793–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Papagiannaros A, Hatziantoniou S, Dimas K. et al. A liposomal formulation of doxorubicin, composed of hexadecylphosphocholine (HePC): physicochemical characterization and cytotoxic activity against human cancer cell lines. Biomed Pharmacother 2006; 60: 36–42. [DOI] [PubMed] [Google Scholar]
- 27. Saint-Pierre-Chazalet M, Ben Brahim M, Le Moyec L. et al. Membrane sterol depletion impairs miltefosine action in wild-type and miltefosine-resistant Leishmania donovani promastigotes. J Antimicrob Chemother 2009; 64: 993–1001. [DOI] [PubMed] [Google Scholar]
- 28. Anderson BJ, Holford NH. Mechanistic basis of using body size and maturation to predict clearance in humans. Drug Metab Pharmacokinet 2009; 24: 25–36. [DOI] [PubMed] [Google Scholar]
- 29. Ostyn B, Hasker E, Dorlo TP. et al. Failure of miltefosine treatment for visceral leishmaniasis in children and men in South-East Asia. PLoS One 2014; 9: e100220. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.