Abstract
Objectives
The UK Five Year Antimicrobial Resistance (AMR) Strategy was published in September 2013 and recommended a One Health approach emphasizing the importance of collaboration to tackle AMR. We describe the inauguration of what we believe to be the first regional One Health group established in the UK. The purpose of the group was to ensure the implementation of a coordinated Cornwall-wide response to the UK AMR Strategy and we describe the outputs of the group to date.
Methods
The Cornwall Antimicrobial Resistance Group was set up as a sub-group of the Health & Wellbeing Board’s Health Protection Committee. Stakeholders reviewed the key objectives set out within the Five Year AMR strategy, identified local priorities and existing work streams within Cornwall, and completed a gap analysis. The annual work plan was developed from the gap analysis and provided a foundation for improved coordination of One Health antimicrobial stewardship (AMS) activity in Cornwall.
Results
To date, outputs from the group can be arranged under the following themes: education and engagement with the public; education and engagement with healthcare workers and veterinarians; and a comprehensive AMS programme for all sectors. The group continues to grow in size with wider stakeholder engagement and increased variety of work streams.
Conclusions
This unique group facilitates discussions across sectors, which has enabled the sharing of knowledge, ideas and resources, stimulated local AMS initiatives, and ensured a platform for the development of future AMR and AMS work.
Introduction
Cornwall is a rural county with a population of over 500 000 with pockets of high deprivation.1 Deprivation has been linked to higher rates of antibiotic prescribing.2 Resistance to key antibacterials is increasing in Cornwall, as it is in the UK and elsewhere.3,4 Of particular local concern is the increased resistance amongst Escherichia coli blood culture isolates to: piperacillin/tazobactam (30/285, 11% non-susceptible), co-amoxiclav (126/285, 44% non-susceptible) and ciprofloxacin (61/285, 21% non-susceptible), and the increased resistance in Klebsiella pneumoniae to piperacillin/tazobactam (6/33, 18% non-susceptible) (unpublished data).
The UK Department of Health (DH) and the Department for Environment Food and Rural Affairs published the UK Five Year Antimicrobial Resistance (AMR) Strategy in September 2013.5 The strategy sets out the following three aims: (i) to improve the knowledge and understanding of AMR; (ii) to conserve and steward the effectiveness of existing treatments; and (iii) to stimulate the development of new antibiotics, diagnostics and novel therapies.
The strategy called for a One Health approach and emphasized the importance of a collaborative approach by experts, health professionals and the public to change the practices that have contributed to the rapid development of AMR. Here we describe the inauguration of the Cornwall Antimicrobial Resistance Group (CARG), which we believe to be the first One Health group established in the UK, and the outputs of the group to date.
Methods
CARG was set up as a sub-group of the Health & Wellbeing Board’s Health Protection Committee with the purpose of implementing a coordinated Cornwall-wide response to the UK Strategy.5 The Chief Pharmacist of Royal Cornwall Hospital Trust and the Medical Director of NHS England Devon and Cornwall and Isles of Scilly Area Team initially wrote to the identified stakeholder organizations shown in Table 1 to notify them of the group’s formation and seek representation.
Table 1.
Identified stakeholder organizations
| Sector | Representative at group inception (January 2014) | Current representatives (October 2016) |
|---|---|---|
| Royal Cornwall Hospital (secondary care provider) | Nurse Consultant Infection Prevention and Control (DIPC) | Medical Microbiology Consultant |
| Microbiology Biomedical Scientist | ||
| Microbiologist (antimicrobial lead) | Consultant and DIPC | |
| Antimicrobial Pharmacist | Chief Pharmacist | |
| Medical Consultant and DIPC | Infection Prevention and Control Consultant Nurse DIPC | |
| Consultant Antimicrobial Pharmacist | ||
| Kernow (Cornwall) Clinical Commissioning Group | Medical Lead and Responsible Officer | GP and Clinical lead |
| Infection Prevention and Control Consultant Nurse | Nurse Consultant Infection Prevention (DIPC) | |
| Pharmaceutical Advisor | ||
| Pharmaceutical Advisor | ||
| Cornwall Foundation Trust (Community Hospital) | Director of Quality and Governance (DIPC) | Pharmaceutical Advisor |
| Director of Quality and Governance (DIPC) | ||
| Infection Prevention and Control Nurse | ||
| Cornwall Health (out of hours GP service) | Medical Director (out-of-hours GP service) | Consultant Paramedic and lead clinician |
| Community pharmacy | Chief Officer Local Pharmaceutical Committee | Chief Officer Local Pharmaceutical Committee |
| Veterinary and farm services | Veterinary representative | Animal and Plant Health Agency Veterinarian |
| Cornwall Veterinary Association | ||
| Duchy Agriculture College | ||
| Public Health England | Consultant in Health Protection | Consultant in Health Protection |
| Academia | Academic from the University of Exeter Medical School working on the environmental dimension of AMR | European Centre for Environment and Human Health |
| University of Exeter Medical School | ||
| University of Plymouth School of Nursing | ||
| Innovation Development Manager and mathematical modeller | ||
| Dean of Plymouth School of Dentistry | ||
| University of Bristol Veterinary School | ||
| Dental | Dental Practice representative | |
| Local Dental Committee representative | ||
| Public Health | Director of Public Health (chair) | |
| Educators | Wellcome Trust Innovation Fund ‘Drug and Bug’ Project Educators | |
| Community and Schools Healthier Lifestyles Support Worker | ||
| Public representation | Health Watch representative |
DIPC, Director of Infection Prevention and Control.
The inaugural CARG convened on 23 January 2014 when the initial stakeholders were divided into small groups and tasked with identifying work streams locally that met the objectives of the UK strategy. Areas of the UK strategy that were not met and deemed not achievable by the group were recorded as such, and objectives within the UK strategy that were not met but were within the capabilities of the committee went on to form the annual work plan.
The work plan focused on three of the seven key areas outlined by the UK strategy where the group felt it could be of most value. These were: (i) improving professional education, training and public engagement; (ii) optimizing prescribing practice; and (iii) better access to and use of surveillance data.
The remaining key areas were not included in the local work plan. Of these, three were determined to require national actions led by the DH: developing new drugs, treatments and diagnostics; better identification and prioritization of AMR research needs; and strengthened international collaboration. The remaining key area, improving infection prevention and control strategies, was a key local priority that was already well embedded into practice in the wake of the Clostridium difficile and MRSA epidemics in the first decade of this century. The work plan provided a foundation for improved coordination of One Health antimicrobial stewardship (AMS) activities in Cornwall. The group hopes that other unidentified stakeholders will be identified, or make themselves known as the group becomes more widely recognized, thus providing support for individuals to facilitate broader AMS outcomes.
Results
At the time of writing the group has grown in size with far-reaching representation and collaboration. The current stakeholder membership is shown in Table 1.
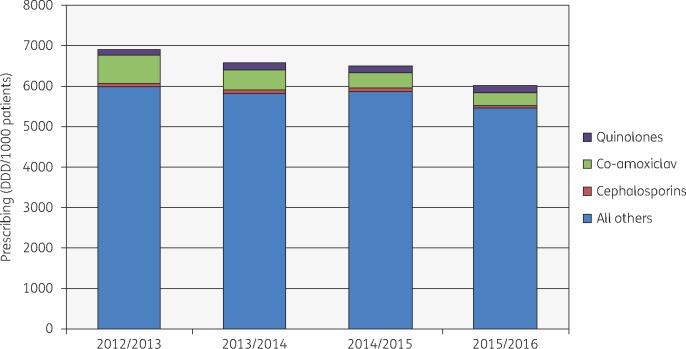
Antibiotic consumption in primary care in Cornwall fell by 12.8% in total from 2012/13 to 2015/16, with the proportion of broad-spectrum antibiotics (cephalosporins, quinolones and co-amoxiclav) falling by 3.9%. Co-amoxiclav consumption fell by 56% over the same time period (Figure 1). The main driver for this reduction was implementation of the TARGET antibiotics toolkit; all GP practices carried out the self-assessment checklist as part of the incentive scheme in 2014/15 and utilized the ‘Treat Your Infection’ patient leaflet from 2014 onwards. NHS England introduced the Quality Premium in 2015 with antibiotic prescribing targets.6 NHS Kernow (Cornwall) Clinical Commissioning Group (CCG) achieved both targets: total antibacterial items/Specific Therapeutic group Age-sex Related Prescribing Unit (STAR-PU) ≤ 1.172, and the proportion of co-amoxiclav, cephalosporins and quinolones for the 12 months to March 2016 <11.3%.
Figure 1.
NHS Kernow, primary care prescribing (British National Formulary 5.1). Data from electronic prescribing analysis and cost, NHS Business Services Authority. This figure appears in colour in the online version of JAC and in black and white in the print version of JAC.
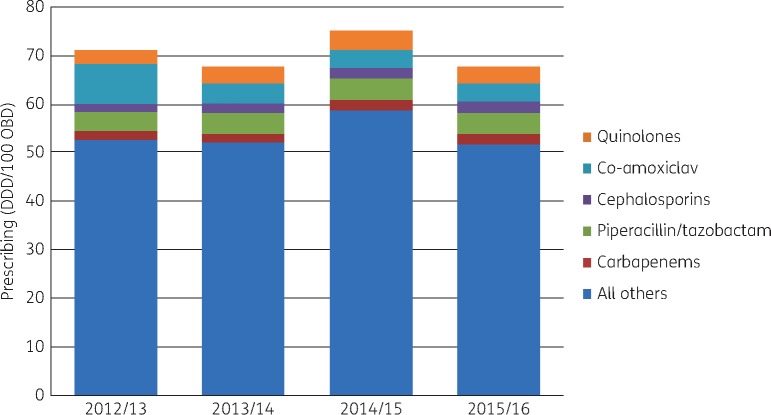
Between 2012/13 and 2015/16 the following changes in prescription rates were seen in secondary care in Cornwall (Figure 2): piperacillin/tazobactam, +11.33%; cephalosporins, +40.76%; quinolones, +34.98%; carbapenems, +25.70%; co-amoxiclav, −54.8%; and total antibiotics, −2.22%. With the introduction of the NHS England Antibiotic Stewardship CQUIN7 we have embarked on a programme of activity which attempts to reduce consumption of piperacillin/tazobactam and meropenem, at the same time reducing total antibiotic consumption.
Figure 2.
Secondary care data. OBD, occupied bed days. This figure appears in colour in the online version of JAC and in black and white in the printed version of JAC.
Outputs of the group
Interdisciplinary collaboration between multiple organizations has enabled wide-ranging outputs through sharing of resources and facilitating networking. Many of these outputs were successful due either to CARG initiating the action or through the support of the group. We feel this range of outputs would be more laborious and therefore difficult to achieve without such a collaborative approach.
Education and engagement with the public
CARG representatives have raised public awareness of AMR on BBC Radio Cornwall (158 000 listeners a week, reaching 38.4% of the county’s population)8 and other local radio stations Heart FM and Pirate FM, BBC local television news and through public engagement at the Eden Project (8471 visitors over 3 days) and the Royal Cornwall Show (approximately 120 000 visitors over 3 days).
Leaflets, posters and stickers have been developed locally with key AMR messages and distributed widely to GP practices, community hospitals, children’s centres and community pharmacies. e-Bug material has been promoted in 13 of the 235 primary schools in Cornwall. Local schools entered a ‘design a bug’ and ‘design a poster’ competition promoting prudent antibiotic use prior to the annual Healthy Schools Awards day, with the winner being presented with a toy e-Bug.9
Education and engagement with healthcare workers and vets
Outputs are as follows:
The inaugural AMR One Health conference hosted by CARG at the Eden Project for healthcare professionals in Cornwall representing nine disciplines across the health community; GPs, nurses, podiatrists, pharmacists, medical microbiologists, radiographers, hospital doctors, veterinarians and public health workers.
Two ‘Drug and Bug’ nurse educators funded by the Wellcome Innovation Fund provided infection prevention and control and AMS education in care homes.
AMS initiatives are discussed regularly with GPs at local quarterly GP Prescribing Lead meetings.
The veterinarian representative made the group aware of the drivers and restrictions for prescribing antibiotics in animals, improving awareness of AMS issues in this sector.
The veterinarian representative keeps the group up-to-date with national and european veterinary reports on antimicrobial resistance and utilization (e.g. European Surveillance of Veterinary Antimicrobial Consumption report and UK Veterinary Antimicrobial Resistance and Sales Surveillance report).
A human health member of the CARG committee delivered an AMR education session at the local Cornwall Veterinary Association’s annual conference in 2015.
Education on AMR from a One Health perspective was delivered to the Cornwall Veterinary Association at its annual conference.
Promotion of the Antibiotic Guardian Campaign10 on European Antibiotics Awareness day and World Antibiotic Awareness Week across primary care, secondary care, local dental, medical and nursing universities and the public. Devon, Cornwall and the Isles of Scilly NHS Area Team have recorded 32.25 antibiotic guardians per 100 000 population, almost twice the England average rate of 17.2.11
Comprehensive antimicrobial stewardship programme for all sectors
Achievements are as follows:
Recommendation that NHS Kernow CCG implement the TARGET toolkit in primary care as part of the GP prescribing quality scheme for 2014/15, which was done successfully in all practices across Cornwall.12
Coordinated regular review of secondary and primary care antibiotic consumption data.
Exploration of a C-reactive protein (CRP) point-of-care testing pilot in community pharmacies to aid the diagnosis of bacterial respiratory tract infection.
A review of the evidence for point-of-care CRP testing with a view to pilot in GP surgeries. Funding was not forthcoming but a plan to pilot testing in out-of-hours clinics and an Urgent Care Centre was proposed.
A review of the evidence for improved patient outcomes in laboratories utilizing MALDI-TOF/MS resulted in the submission of a business case for the Medical Microbiology Department.
Community hospital antibiotic point prevalence audit format amended to incorporate collection of 72 h review data and report to CARG.
First place in regional secondary care antibiotic point prevalence benchmarking audit on AMS performance.
A review of Cornish farmer and veterinarian participation in national veterinary and farm stewardship programmes.
Others
The Group registered as a stakeholder for the NICE Good Practice Guidance on Antimicrobial Stewardship and the NICE Guidance on Managing Common Infections.
Discussion
We are aware of the success of local One Health AMR groups in Sweden, which in 2008 reported a reduction in antibiotic use and lowered AMR rates over 10 years, without measurable negative consequences.13 More recently the inauguration of a One Health AMR inter-agency AMS strategy was described in Minnesota, USA. We wait to hear the successes of this group.14
Since the founding of CARG and sharing of knowledge within England we are aware of three other local AMR strategy implementation groups in: (i) Cheshire and Merseyside; (ii) Leeds; and (iii) Bath and Northeast Somerset. In common with other local AMR groups and the early Swedish examples, we too rely on personal commitment from local AMR healthcare leaders without funding or a formal mandate. It is hoped that as the successes of these groups are recognized others will follow and funding will be secured, as occurred in Sweden where a growing number of groups are now financially supported.
NHS England’s Sustainability and Transformation Plans15 provide an opportunity for local healthcare systems to further develop integrated primary and secondary care antibiotic stewardship activities, facilitating the inauguration of local One Health groups and bridging the gap between animal and human health practice, which is key to the local delivery of the national AMR strategy.
Conclusions
The group provides a forum for the local implementation of a coordinated AMR strategy, delivering the national strategy locally. This forum facilitates discussions across boundaries, which enables the sharing of knowledge, ideas and support, stimulating the development of work around AMR. With the emergence of local One Health groups in the UK and worldwide we need to share experiences, learn from successes and secure funding, thus enabling expansion of this model nationwide.
Acknowledgements
We thank Tracey Nicholls (Personal Assistant to the Chief Pharmacist) and Laura Mellow (Personal Assistant to Public Health Director) for their administrative support for these meetings.
Funding
This study was carried out as part of our routine work.
Transparency declarations
None to declare.
Disclaimer
The views expressed are those of the authors and not necessarily those of the NHS, the NIHR, PHE or the Department of Health.
References
- 1. IMD Data 2015. https://www.cornwall.gov.uk/council-and-democracy/data-and-research/data-by-topic/deprivation/.
- 2. Wise J. Antibiotic prescribing is higher in deprived areas of England. BMJ 2015; 351: h6117.. [DOI] [PubMed] [Google Scholar]
- 3. PHE. English Surveillance Programme for Antimicrobial Utilisation and Resistance (ESPAUR), Report2016. https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/575626/ESPAUR_Report_2016.pdf.
- 4. WHO. Antimicrobial Resistance: Global Report on Surveillance, 2014. http://www.who.int/drugresistance/documents/surveillancereport/en/.
- 5. Department of Health and Department for Environment Food and Rural Affairs (DEFRA). UK Five Year Antimicrobial Resistance (AMR) Strategy 2013-2018 https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/244058/20130902_UK_5_year_AMR_strategy.pdf.
- 6. NHS England. Quality Premium: 2015/16 Guidance for CCGs.https://www.england.nhs.uk/wp-content/uploads/2013/12/qual-prem-guid.pdf.
- 7. NHS England. Commissioning for Quality and Innovation Guidance for 2016/17 2016. https://www.england.nhs.uk/wp-content/uploads/2016/03/cquin-guidance-16-17-v3.pdf.
- 8. BBC Press Office. Radio Cornwall RAJAR Quarter 1, 2014 http://www.bbc.co.uk/pressoffice/pressreleases/stories/2002/05_may/09/radiocornwall_rajarq1.shtml.
- 9. e-Bug. http://www.e-bug.eu/.
- 10. PHE. Antibiotic Guardian http://antibioticguardian.com/.
- 11. Bhattacharya A, Hopkins S, Sallis S. et al. Process evaluation of the UK-wide Antibiotic Guardian campaign: developing engagement on antimicrobial resistance. J Public Health 2016; doi:10.1093/pubmed/fdw059. [DOI] [PubMed] [Google Scholar]
- 12. TARGET Toolkit http://www.rcgp.org.uk/targetantibiotics.
- 13. Mölstad S, Erntell M, Hanberger H. et al. Sustained reduction of antibiotic use and low bacterial resistance: 10-year follow-up of the Swedish Strama programme. Lancet Infect Dis 2008; 8: 125–32. [DOI] [PubMed] [Google Scholar]
- 14. Tomczyk S, Lynfield R. One health approach to antibiotic stewardship strategic planning in Minnesota. In: CSTE Conference 2016 Abstract. https://cste.confex.com/cste/2016/webprogram/Paper6647.html.
- 15. NHS England. Sustainability and Transformation Plan Footprints. 2016 https://www.england.nhs.uk/wp-content/uploads/2016/02/stp-footprints-march-2016.pdf.